Abstract
Cancer is the second leading cause of death among Hispanics. Most of the cancer statistics available both at the state and national levels report cancer statistics for all Hispanics as an aggregate group. The goal of this paper is to provide a population-based overview of cancer mortality among Hispanics (Cubans, Mexicans, Puerto Ricans and other Hispanics) in Florida from 1990 to 2000 and to explore the demographic diversity of this growing ethnic group. The study population consisted of Hispanics and White non-Hispanics who died from cancer. Cancer mortality rates and proportion of cancer deaths by type and age at death for the selected racial/ethnic groups were calculated. Our findings indicate that the cancer death rates of the Hispanic subgroups compared favorably with those of White non-Hispanics and that cancer rates often presented for all Hispanics mask important differences between the different ethnic subgroups that fall under the Hispanic umbrella.
Keywords: Hispanics, Hispanic Americans, Neoplasms, Cancer mortality, Epidemiology, Florida, Cubans, Puerto Ricans, Mexicans
Introduction
Cancer is the second leading cause of death among adult Hispanics. Cancer occurrences vary across Hispanic subgroups because of regional, demographic, geographic, socioeconomic, behavioral and/or genetic differences [1-3]. From epidemiologic, public health, cancer control and social science perspectives, it is important to identify populations that differ in disease patterns, risk patterns and disease outcomes [4]. However, most of the data available, both at the national and state level, report cancer statistics for all Hispanics as an aggregate group [3], masking important heterogeneity in overall mortality across subgroups that fall under the Hispanic label [5].
Hispanics are the fastest growing and largest minority group in the United States (13% vs. 11% of African-Americans) [6]. By the year 2050, an estimated 102 million Hispanics will reside in the United States representing nearly 25% of the total U.S. population. Florida has one of the highest percentages of Hispanics in the nation—nearly 20% of the state population [7]. From 1990 to 2000, the Florida Hispanic population experienced a 70% increase and is the fastest growing ethnic group in the state.
The term Hispanic, created by the U.S. Office of Management and Budget (OMB) in the 1970s, is a socially and politically constructed term first used in the 1980 census [8]. With this inclusion, U.S. Hispanics gained political and economic leverage to advance and exert influence over state and national policies [9, 10]. The OMB acknowledges that there are no anthropological or biological bases to support these classifications and that they are sociopolitical constructs [11, 12].
Overall, Florida residents experience similar illness burden and mortality as the general U.S. population. However, the state economy and demographic population composition distinguish the state in several important ways giving rise to a unique set of public health and clinical considerations. Florida’s large population is diverse with regard to age, ethnicity and international immigration. These features shape the population’s general literacy level, English language proficiency and employment opportunities, which in turn are key variables that affect health status and access to health care. As a gateway to Latin America and the Caribbean, Florida also has a diverse foreign-born population (12.9 % in 1990, and 16.7% of the population in 2000 compared to 11.1% nationally) [13], with 72.8% of this population born in Latin America. And this is a different experience than other states with large Hispanic populations such as California and Texas. In 1990, the foreign born population in California and Texas were 17.3% and 8.7%, respectively. By 2000, California and Texas had increased their foreign born population to 23.5% and 13%, respectively. In 2000, Hispanics comprised over 54.8% of the foreign born population in California, whereas in Texas Hispanics comprised 74.7% of the foreign born. In total, Hispanics comprise over 30% of the populations of California and Texas. The overwhelming majority of Hispanics are of Mexican descent (83% in Texas and California vs. 16% in Florida) [7] underscoring the need to make state-by-state inter-ethnic comparisons.
Hispanics in Florida have a similar annual death rate to Hispanics nationwide for all cancer sites combined (130.6/100,000 vs. 129.1/100,000, respectively). While morbidity and mortality rates for all-cancer sites in Florida are similar to the general U.S. population, some cancer-specific morbidity and mortality rates differ. For example, cervical cancer incidence is higher in Florida than in the United States [14]. The breast cancer mortality rate in Florida is the third highest in the nation [14]. Even though the average annual age-adjusted death rates for lung, breast and colorectal cancer are lower for Hispanics compared to other ethnic groups, the rates are higher for Hispanics in Florida than the national Hispanic averages [15]. In 1999, during the study period, cancer accounted for 24% of all deaths in Florida [16].
Similar to other cancer data collection systems, the Florida Cancer Data System (FCDS) relies on medical records which often do not include information on country of origin for Hispanic patients. The surveillance, epidemiology and end results (SEER) datasets collected by the National Cancer Institute categorize individuals as Hispanic using a variety of methods including birthplace, last name, and self-identification of Hispanic ethnicity. However, cancer incidence rates from SEER for Hispanic subgroups are generally not available. To date, several studies have explored cancer incidence and mortality differentials between all Hispanics and White non-Hispanics in Florida [2, 3, 17-19]. By drawing no distinction among the different Hispanic subgroups researchers extrapolate data from one Hispanic subgroup to another where this extrapolation may not always be valid and, in fact, may be misleading [20].
However, none of these studies has compared all site cancer mortality rates among Cuban, Mexican, Puerto Rican, all other Hispanic and White non-Hispanic racial/ethnic groups in Florida. Our study is the first to disaggregate Florida Hispanic groups and reveal considerable differences in the mortality experience of Florida Hispanics. Specifically, it will provide answers to the following questions: (1) Do cancer mortality rates differ between Cubans, Mexicans, Puerto Ricans and all other Hispanics and (2) How do the cancer mortality rates of each of these Hispanic subgroups compare to those of non-Hispanic Whites?
Given the complexity of these categories, the U.S. Hispanic population serves as an illustrative example to explore heterogeneity found within ethnic groups. Despite shared characteristics (language and relative youth), considerable differences exist among Hispanics, particularly with regard to median age, household size, education and family income [21]. In Florida, Cubans are the largest Hispanic group (32%) followed by Puerto Ricans (18%), Mexicans (13%), and other Hispanics. During the 1990s, the numbers of immigrants from other Latin American countries increased (Columbians, Dominicans, Nicaraguans), further diversifying the Hispanic population of the state [6]. In 1993 all states began recording Hispanic ethnicity on death certificates, except for Oklahoma, which began in 1997 [3]. Despite some studies showing a Hispanic favorable advantage in cancer mortality compared to White non-Hispanics [5, 21-24], there is no single source of reliable data on cancer rates, mortality or survival for Hispanic subgroups [25]. We seek to fill this gap and compare cancer mortality rates across Hispanic subgroups and non-Hispanic Whites.
Methods
Study Population
The study population consists of Florida residents aged 25 years and older, who died from cancer between 1990 and 2000, who are classified as Cuban, Mexican, Puerto Rican, other Hispanic (i.e., Central and South Americans, Dominicans and other Hispanic groups excluding Cubans, Puerto Rican, Mexicans) or as White non-Hispanic on their death certificate. We obtained U.S. Census Bureau data to glean demographic characteristics of Florida Hispanics with the 1990 census. The 1990 U.S. Census provided accurate demographic data collected while the reported decedents were still alive (Table 1).
Table 1.
Decedent demographics 1990–2000
| Hispanics |
|||||
|---|---|---|---|---|---|
| Cuban | Mexican | Puerto Rican | Other Hispanic | White non-Hispanic | |
| Number of decedents | 17,907 | 636 | 3,218 | 4,963 | 339,989 |
| Women | 7832 (44%) | 263 (41%) | 1,473 (46) | 2,461 (50%) | 156,515 (46%) |
| Men | 10,075 (56%) | 373 (59%) | 1,745 (54) | 2,502 (50%) | 183,474 (54%) |
| Median age | |||||
| Women | 71 | 60 | 67 | 66 | 72 |
| Men | 70 | 62 | 67 | 69 | 72 |
| Place of birth (%) | |||||
| Mexico | 0.01 | 53.14 | 0 | 0.12 | 0.02 |
| Puerto Rico | 0.01 | 0.47 | 91.14 | 0.97 | 0.07 |
| Cuba | 97.84 | 0.16 | 0.09 | 2.94 | 0.14 |
| Florida | 1.51 | 2.2 | 0.31 | 7.56 | 8.66 |
| Other | 0.63 | 44.03 | 8.46 | 88.41 | 91.2 |
| Educational attainment (%) | |||||
| Elementary/none | 40 | 51 | 32 | 26 | 11 |
| Some High School/High School Grad | 37 | 32 | 47 | 44 | 56 |
| Some College/College Grad | 23 | 17 | 21 | 30 | 33 |
| Race (%) | |||||
| White | 98 | 99 | 98 | 93 | 100 |
| Black | 2 | 0 | 2 | 6 | 0 |
Note: If percent <.5 rounded to 0
Social characteristics of decedents 25 years and older with underlying cause of death reported as cancer in Florida 1990–2000
Data Sources
Death certificates for the years 1990–2000 were obtained from the National Vital Statistics System supported by the NCHS and deaths were defined with International Classification of Disease codes (ICD) according to the ICD-9 for the years 1990–1998 and then with ICD-10 codes for date from 1999 to 2000. Age, race, Hispanic ethnicity and origin, educational attainment, place of birth, and marital status were retrieved electronically for each cancer death identified. Identification of Hispanic ethnicity is based on the information recorded on the death certificate following one of two formats recommended by the National Center for Health Statistics [26]. For the group classified as all other Hispanics, the following death certificate categories were combined; “Central or South American” and “other or unknown Hispanic”. It is estimated that more than 99% of deaths occurring in the U.S. are registered in this system. However, Hispanic mortality rates are slightly understated (by less than 10%) because of net underreporting of Hispanic origin on the death certificate [27].
Calculation of Rates and Analysis
We calculate cancer mortality rates using the direct age adjustment method. State specific mortality rates for cancer deaths were calculated from all cancers types combined for each ethnic group in this study. Annual cancer deaths (numerators) and population counts (denominator) for 5-year age groups beginning with individuals 25 years of age were summed for the selected ethnic groups by gender for the study period 1990–2000. These data were calculated using the 2000 standardized population age distribution [28]. Average annual age adjusted cancer mortality rates for the years 1990–2000 were also calculated. In addition, descriptive statistics on the demographics of decedents were calculated.
We then calculated proportions of cancer deaths due to the top cancers for all years combined (1990 through 2000) for each ethnic group and reported for the decedents. By comparing cancer mortality rates of each Hispanic ethnic group to those of a reference population, such as White non-Hispanics, we are able to assess the burden of cancer among Hispanics as compared to White non-Hispanics. We used SAS statistical software (Cary, NC) for our analyses. Human subjects IRB approval was obtained from the University of South Florida Institutional Review Board.
Results
During 1990–2000, 26,724 Hispanic cancer deaths were identified. Of these, 67% (n = 17,907) were reported to be Cuban, 2.37% (n = 636) were Mexican, 12% (n = 3, 218) as Puerto Rican with the remainder (4,963) reporting to be “other” Hispanic. Although Cubans comprise 32% of the Hispanic population in Florida, they accounted for 67% of cancer deaths among Hispanics in Florida, 1990–2000. During this same time period, 339,989 White non-Hispanics died from cancer in Florida (See Table 1).
Differences in Hispanic Mortality
Considerable demographic differences exist among the Hispanic decedents. The median age at death was 72 years for White non-Hispanic women and men whereas it was 60 years for Mexican women. Death certificate data show that the majority of Cubans (98%), and Puerto Ricans (91%) were born in their homeland compared to 53% of Mexicans. Among Cuban decedents, 40% report having an elementary education or less and 37% report having some high school or high school diploma. Consistent with other studies, Mexicans had the least educational attainment with 51% report having an elementary education or less. A large majority of the decedents in the Hispanic subgroups were categorized as White (98% of Cubans, 99% of Mexicans, 98% of Puerto Ricans, 93% of other Hispanics). In Table 2, the percent change refers to the extent to which the rate increases or decreases over the 10 year period. The figures are arrived at by comparing the initial (or before), e.g., 1990 rate and final (or after) 2000 rate.
Table 2.
Average annual age-adjusted cancer mortality rates by ethnicity 1990–2000
| Rate | Confidence interval |
SE | Percent change (%) |
|
|---|---|---|---|---|
| Women | ||||
| White non-Hispanic | 253.3 | 252.0–254.5 | 10.6 | 0.5 |
| Puerto Rican | 161.5 | 153.3–169.8 | 21.5 | −10.9 |
| Other Hispanic | 144.6 | 138.9–150.3 | 12.4 | 33.1 |
| Mexican | 108.6 | 95.5–121.8 | 24.3 | 23.1 |
| Cuban | 184.5 | 180.4–188.5 | 6.5 | 1.8 |
| Hispanica | 170.5 | 167.5–173.6 | 6.6 | 10.9 |
| Men | ||||
| White non-Hispanic | 376.4 | 374.6–378.1 | 22.5 | −15.4 |
| Puerto Rican | 258.1 | 246.0–270.2 | 22.2 | 33.8 |
| Other Hispanic | 212.9 | 204.6–221.2 | 31.8 | −22.1 |
| Mexican | 163.4 | 146.8–179.9 | 56.4 | 81.7 |
| Cuban | 327.5 | 321.1–333.9 | 16.1 | 0.6 |
| Hispanica | 290.2 | 285.5–294.9 | 12.1 | −1.1 |
All Hispanic ethnic groups comibed
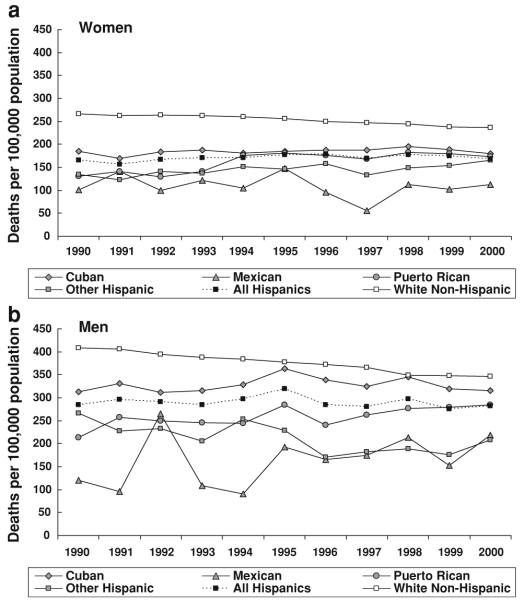
Age-adjusted cancer mortality rates for our Hispanic groups ranged from 56 to 363 deaths per 100,000 (See Fig. 1a and b). For each group, the cancer death rates were higher for men than for women. Cuban men have the highest cancer mortality rates compared to White non-Hispanic men. Of all the Hispanic groups, Mexican women and men have the lowest death rates (Fig. 1a and b). Overall, the cancer death rates of the subgroups compare favorably with those of White non-Hispanics but given the range of mortality rates for the subgroups, it is clear that important differences exist between the different Hispanic ethnic subgroups.
Fig. 1.
(a) Age-adjusted cancer mortality rates for Hispanic subgroups compared with White non-Hispanics, Florida 1990–2000. (b) Age-adjusted cancer mortality rates for Hispanic subgroups compared with White non-Hispanics, Florida 1990–2000
White non-Hispanic men had the highest cancer mortality rates which show a steady decline since 1992. The mortality rate for White non-Hispanic women is higher than the death rate for all Hispanic women; however, for all Hispanic women the rate shows a steady downward trend. Cancer rates for Mexican men and women peak sharply in 1991/1992 and 1995 for men and women followed by a steady decline until 1997. At this point, rates start to increase again. The lack of a discernable pattern could be attributed to the relative small number (n = 636) of Mexican decedents.
Death Rates by Anatomic Cancer Site for Hispanic Subgroups
Our Hispanic subgroups substantially varied in terms of deaths by anatomic cancer site. Mexican women had the highest percentage (9.1%) of cancer deaths due to cervical cancer compared to the women in the other ethnic groups (1.6–4.3%). The proportions of cancer deaths due to breast cancer were similar across our Hispanic subgroups (17.7–20.5%) (Table 3).
Table 3.
Proportion of deaths by selected cancer type, 1990–2000
| Hispanic |
|||||
|---|---|---|---|---|---|
| Cuban | Mexican | Puerto Rican |
Other Hispanic |
White non- Hispanic |
|
| Men | |||||
| Total number of decedents, n | 10,075 | 373 | 1,745 | 2502 | 183,474 |
| Lung | 30.1 | 23.6 | 23.2 | 23.7 | 34.2 |
| Prostate | 13.3 | 8.6 | 11.7 | 15.3 | 11.8 |
| Colorectal | 10.7 | 10.2 | 12.1 | 9.3 | 10 |
| Pancreas | 4.7 | 4.8 | 4.6 | 5.3 | 4.8 |
| Liver and intrahepatic bile duct | 3.5 | 4.8 | 6.4 | 4.4 | 2.2 |
| Bladder | 3.5 | 1.3 | 1.9 | 3.6 | 3.2 |
| Stomach | 2.9 | 4.8 | 6 | 5.7 | 2.5 |
| Brain and other nervous system | 2.5 | 2.9 | 2.2 | 2.9 | 2.3 |
| Lip, oral cavity and pharynx | 2.5 | 2.7 | 2.6 | 1.4 | 2 |
| Kidney-renal | 1.9 | 2.4 | 1.5 | 1.6 | 1.9 |
| All other cancers | 24.3 | 33.8 | 27.7 | 26.7 | 25 |
| Women | |||||
| Total number of decedents, n | 7,832 | 263 | 1,473 | 2,461 | 156,515 |
| Breast | 18.8 | 20.5 | 18.3 | 17.7 | 15.5 |
| Colorectal | 15.1 | 7.2 | 11.3 | 11.2 | 10.9 |
| Lung | 13.4 | 8.7 | 13.3 | 11.9 | 28.1 |
| Pancreas | 6.3 | 6.1 | 6.2 | 6.4 | 5.6 |
| Ovary | 5.6 | 4.6 | 6.2 | 5.4 | 5.4 |
| Liver and intrahepatic bile duct | 3.4 | 5.7 | 2.8 | 3.5 | 1.4 |
| Brain and other nervous system | 2.6 | 2.3 | 2.8 | 2.4 | 2.2 |
| Stomach | 2.6 | 5.3 | 5 | 4.9 | 1.8 |
| Cervix | 1.6 | 9.1 | 3.1 | 4.3 | naa |
| Kidney and renal pelvis | 1.2 | 3.8 | naa | naa | 1.4 |
| Bladder | naa | naa | naa | 1.2 | 1.6 |
| All other cancers | 29.4 | 26.6 | 29.5 | 31.1 | 26.1 |
“na” indicates not available. In this table, we list the top 10 cancers in each ethnic group. If that particular cancer was not one of the top 10 cancers it was not listed and thus is included in the proportion for “all other cancers” category. For example, deaths due to cancer of the cervix were not in the top 10 for the White non-Hispanic group, thus the cell contains “na” and the proportion of cancer deaths due to cancer of the cervix is included within the “all other cancers” category
White non-Hispanic women had the highest percentage of cancer deaths due to lung cancer (28.1%) compared to Hispanics. Hispanic women have differing percentages of death due to lung cancer—Cuban (13.4%), Mexican (8.7%), Puerto Rican (13.3%) and all other Hispanic women (11.9%). The proportion of cancer deaths due to lung cancer were highest for White non-Hispanic men (34.2%), followed by Cuban (30.1%), other Hispanic (23.6%), Mexican (23.2%) and Puerto Ricans (23.7%).
Cuban women had the highest percentage of cancer deaths due to colorectal cancer (15.1%) compared to Mexican (7.2%), Puerto Rican (11.3%), other Hispanic (11.2%) and White non-Hispanic women (10.9%). Among men, the percentage of cancer deaths varied considerably as well. Mexican men (8.6%) had the lowest percentage of cancer deaths due to prostate cancer compared to Cuban (13.3%), Puerto Rican (11.7%), other Hispanic (15.3%) and White non-Hispanic men (11.8%). Puerto Rican (6%) and other Hispanic (5.7) men had highest percentage of cancer deaths due to stomach cancer compared to Cuban (2.9%), Mexican (4.8%), and White non-Hispanic men (3%). These results must be interpreted with caution because although the proportion of deaths due to a certain cancer may be higher for particular subgroups, it does not mean the age-adjusted rates will be higher.
Cancer Mortality and Age
Cancer death rates considerably increase with age, but a different pattern emerges when Hispanics are disaggregated (Fig. 2). The proportions of cancer deaths by age group were similar for both men and women and are reported together. Among White non-Hispanics 8.9% of cancer deaths occurred before the age of 55 compared to 31.5% of Mexicans, 19.7% of Puerto Ricans, 20.8% all other Hispanics and 10.8% of Cubans. An even higher proportion of Mexicans (11.8%) died before the age of 40 compared to all other racial/ethnic groups.
Fig. 2.
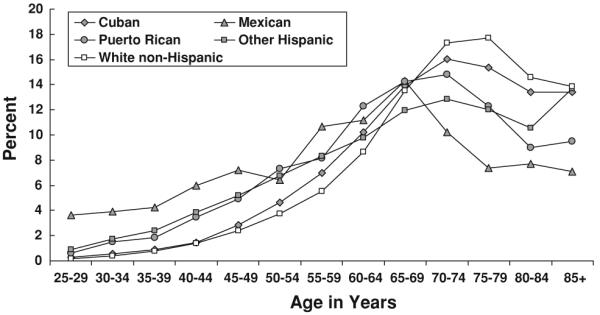
Age distribution of cancer deaths for men and women combined, Hispanic subgroups compared with White non-Hispanics, Florida 1990–2000
Discussion
To our knowledge, our study is the first to disaggregate Florida Hispanic groups and to reveal considerable differences in cancer mortality. Our findings are congruent with other research results that compared mortality rates among some of the selected Hispanic subgroups outside of Florida [5, 22-24, 29-34]. The highest cancer mortality rates were among White non-Hispanic men followed by Cuban men; whereas the lowest mortality rates were found among Mexican women. Overall, Cubans displayed a cancer mortality profile similar to White non-Hispanics.
Observed mortality differentials may be partly explained by differences in cancer screening rates across Latino subgroups [35, 36]. Mexican women report the lowest rates of recent screening [37] which may contribute to the higher proportion of deaths due to cervical cancer and higher rates of cancer death at younger ages found in our Florida sample of Mexican women. This is in stark contrast to the situation reported when Hispanics are aggregated in one group as reported by the Florida Behavioral Risk Factor Surveillance Survey (BRFSS). In 2004, the Florida BRFSS reported that 89% of Hispanic women have had a pap smear [38]. In terms of mammography screening, the same report shows that 57% of Hispanic women have had a mammogram. As access to care is one of the strongest predictors of regular screening and early detection of cervical cancer, the excess mortality experienced by this group may be partly explained by the fact that Mexicans have the least access to health care coverage and services of all Hispanic groups [25].
Mortality patterns among subgroups must be considered within the context of political economics and culture. Cuban, Puerto Rican and Mexican immigration patterns are distinct from one another and reflect important changes in U.S. migration policy. For example, a recent study found that nearly two thirds of Puerto Ricans, 67.5% of Cubans, 55.6% of Mexicans and 53.1% of all Hispanics had lived in the United States for over 15 years [39]. Researchers suggest that lifestyle and diet changes are attributable to acculturation to mainstream U.S. culture and that changes in health related behaviors as acculturation increases are associated with higher health risks [40, 41]. Rosenwaike suggests that lower cancer mortality among selected Hispanic subgroups relative to White non-Hispanics persist because of healthier lifestyle patterns [21] or death at younger ages before many cancers are detectable.
Current research highlights that most peer-reviewed literature focuses on socio-cultural and behavioral factors that impact health [34, 35, 42-44]. Although Hispanics have lower incidence rates for cancers they are more likely to have larger tumors and/or metastatic disease at the time of diagnosis [3, 45]. Possible explanations for late stage diagnoses include low rate of medical insurance coverage [45, 46], lack of knowledge about services, limited access to and use of cancer screening programs [36, 45-48] poverty and other complex sociocultural and geographic factors that contribute to healthcare disparities [49, 50]. A recent study found that relative to non-Hispanic Whites, Mexicans, South and Central Americans and Puerto Ricans had a 1.4- to 3.6-fold greater risk of presenting with stage IV [51]. Moreover, Ramirez et al. [52] examined women’s breast and cervical cancer knowledge, attitudes and screening behaviors in various Hispanic subgroups [46]. Study findings indicated that Puerto Ricans had the least knowledge about Papanicolaou smear guidelines and found that knowledge was significantly related to age, income, education, language and recent screening history.
Regarding health behaviors important variations among the Hispanic subgroups have also been noted in the literature. For example, smoking preferences and frequencies have been reported to vary between Latinos and Anglos [53, 54] and within Latinos (30% of Cuban women are smokers versus 14% of Puerto Ricans and 9% of Mexicans) [55]. There is also evidence of differences in alcohol consumption patterns [56, 57]. Recent studies have observed an increase in body weight during the year after cancer diagnosis which is linked to recurrence and reduced survival [58-63]. Obesity is higher among Latinas than non-Hispanic Whites but also varies substantially by country of origin (19% of Cubans are obese versus 32% of Puerto Ricans and Mexicans versus 21% of non Hispanic whites) [55].
Without disaggregated analyses, initiatives in cancer control and prevention are fated to be misdirected and misinformed. To illustrate, the cancer mortality rate (all sites combined) for Hispanic men for 1997 was 285 per 100,000 but for Mexicans it was 180 per 100,000 whereas it was 262 per 100,000 for Puerto Ricans and 328 per 100,000 for Cubans. Cancer mortality rates among Mexicans in our sample were similarly lower than rates for White non-Hispanics Cubans, Puerto Ricans, and all Hispanics combined, despite the reported lower life expectancy, access to care, educational attainment and socioeconomic status. The second lowest mortality rates were found among Other Hispanics. These findings partly support the “salmon bias” migratory hypothesis proposed to explain the lower U.S. Hispanic mortality rates compared to White non-Hispanics [64]. According to this hypothesis, seriously ill Hispanics may return to their country of origin to die which would result in “statistically immortal” [65]. Hispanics as the U.S. does not keep record of foreign deaths. The hypothesis has received partial support from some researchers, especially regarding foreign-born Mexican and Other Hispanics [66] but not from others [67]. This underscores the importance of collecting relevant data on Hispanics (e.g., country of origin, birthplace) and of reporting health statistics by meaningful subgroups (e.g., foreign-born versus not) in order to get an accurate picture of health outcomes of diverse ethnic groups such as the U.S. Hispanic population.
Limitations
Misclassification of ethnicity is always a potential methodological problem [68]. The findings reported in this paper are subject to the following limitations. First, comparison of cancer death rates between racial and ethnic groups, particularly those involving groups other than Whites or Blacks, should be interpreted with caution because ethnicity and race are rarely classified uniformly on medical records or death certificates [69]. Thus, cancer rates are biased downward, leading to an under-representation of cancer for the population [70, 71]. Second, the data on death certificates are usually provided by the funeral director or physician who reports the race/ethnicity of the individual with information from a family member or from observation [72]. However, a recent study found a high accuracy of birthplace information that was obtained from death certificates for Hispanics [73]. Third, it has also been reported that causes of deaths for minorities are more likely to be misclassified as “symptoms, signs, and ill-defined conditions” than they are for Whites [74, 75]. Fourth, the National Longitudinal Mortality Study (NLMS) indicated an underreporting of deaths for Hispanics, including Mexicans, Cubans and Puerto Ricans [72]. Fifth, mortality rates for Hispanics are also affected by under coverage of the population during the census [25, 70, 71, 76]. Sixth, accuracy in the cause of death in cancer patients may also contribute to misclassification bias [77, 78]. Another limitation is that some of the rates are based on small number of cases, which should be interpreted with caution, and that the descriptive cancer statistics reported here are only for the state of Florida and may not be generalizable to all Hispanics in the United States.
Implications for Researchers and Clinicians
From 1990 to 2000, there was a 70% increase in the Hispanic population in Florida. The largest percent increase was seen among Mexicans and Hispanics from Central and South America. Population estimates indicate that the Hispanic population in Florida could be over 4 million in 2010. Due to the fast growth of the Hispanic population, the categories used to report cancer data and statistics need to expand and include other information for Hispanic subgroups living in Florida and the United States because their demographics and socioeconomic status differ, and these differences affect health [70]. Our future research will include the exploration cancer site-specific mortality rates for each of the selected ethnic groups and calculation of national cancer death rates to have a more complete picture of the state of cancer mortality among various Hispanic subgroups.
Many cancer interventions and research programs are guided by cancer incidence and mortality statistics. In 1991, Rosenwaike stressed the “pressing need for more accurate, current, and comprehensive data for specific ethnic groups” [21]. Discerning cancer incidence and mortality rates by ethnic subgroup is a first step in determining the cancer prevention and control activities that are needed to better address the cancer needs of all Hispanics. Healthy People 2010 reports the cancer death rate per 100,000 for Hispanics was 123.7 using 1998 as baseline with a goal of overall reduction in cancer deaths by 21%. Consideration of intra-ethnic heterogeneity in cancer control prevention efforts can possibly hasten the goals of Healthy People 2010 and also provide a more culturally competent approach to cancer control and prevention.
Acknowledgements
We would like to thank Dr. Latetia Moore and Dr. Jihyun Lee for their assistance with data preparation and analysis as well as Dr. Cathy Meade and Janelle Menard for their support and editorial comments. Dr. Barnett Pathak was supported in part by an Established Investigator Grant from the American Heart Association. Dr. Soler-Vilá was supported in part by a Mentored Research Scholar Award from the American Cancer Society. Dr. Flores was supported in part by Project EXPORT from the National Center on Minority Health and Health Disparities/National Institutes of Health.
Contributor Information
Dinorah Martinez-Tyson, Health Outcomes and Behavior, H. Lee Moffitt Cancer Center & Research Institute, FOW-EDU, 12902 Magnolia Drive, Tampa, FL 33612-9497, USA.
Elizabeth Barnett Pathak, Department of Epidemiology and Biostatistics, College of Public Health, The University of South Florida, 13201 Bruce B. Downs Blvd, MDC 56, Tampa, FL 33647, USA.
Hosanna Soler-Vila, Epidemiology and Public Health & Sylvester Comprehensive Cancer Center, Leonard M. Miller School of Medicine, University of Miami, Room 308 Fox Cancer Center, 1550 NW 10th Avenue, Miami, FL 33136, USA.
Ann Marie Flores, Department of Orthopaedics & Rehabilitation, Rehabilitation Oncology Program, Vanderbilt University Medical Center, 1215 21st Avenue South, Suite 3220 MCE, Nashville, TN 37232-5677, USA.
References
- 1.American Cancer Society . Cancer facts and figures for Hispanics/Latinos 2003–2005. Atlanta: 2003. [Google Scholar]
- 2.American Cancer Society . Cancer facts and figures for Hispanics/Latinos 2006–2008. Atlanta: 2006. [Google Scholar]
- 3.O’Brien K, Cokkinides V, Jemal A, et al. Cancer statistics for Hispanics, 2003. CA Cancer J Clin. 2003;53(4):208–26. doi: 10.3322/canjclin.53.4.208. [DOI] [PubMed] [Google Scholar]
- 4.North American Association of Central Cancer Registries . Final Report of Atlanta Symposium: North American Association of Central Cancer Registries. Uniform data standards committee subcommittee on methodologic issues of measuring cancer among Hispanics. n.d. [Google Scholar]
- 5.Hummer R, Rogers R, Amir SH, Forbes D, Frisbie WP. Adult mortality differentials among Hispanic subgroups and non-Hispanic Whites. Soc Sci Quart. 2000;81(1):459–76. [PubMed] [Google Scholar]
- 6.U.S. Census Bureau [Accessed 07 Jun 2004];U.S. Census 2000. 2002 Junuary 25; http://www.census.gov.
- 7.U.S. Census Bureau [Accessed 10 Aug 2007];American community survey. 2003 Summary Tables; generated by Dinorah Martinez-Tyson; using American FactFinder; < http://factfinder.census.gov>.
- 8.Hayes-Bautista DE, Chapa J. Latino terminology: conceptual bases for standardized terminology. Am J Public Health. 1987;77(1):61–8. doi: 10.2105/ajph.77.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sommers LK. Inventing Latinismo: The creation of “Hispanic” panethnicity in the United States. J Am Folklore. 1991;104(411):32–53. [Google Scholar]
- 10.Trueba ET. Latinos Unidos. Rowman & Littlefield Publishing; Lanham: 1998. [Google Scholar]
- 11.Grieco EM, Cassidy RC. Overview of race and Hispanic origin: census 2000 brief. US Department of Commerce, US Census Bureau; Washington, DC: 2001. United States census 2000. [Google Scholar]
- 12.Oppenheimer GM. Paradigm lost: race, ethnicity, and the search for a new population taxonomy. Am J Public Health. 2001;91(7):1049–1055. doi: 10.2105/ajph.91.7.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.U.S. Census Bureau [Accessed 07 June 2004];Florida quick facts. 2004 May 26; http://quickfacts.census.gov/qfd/states/12000.html.
- 14.Dyer JG. The black cloud over the sunshine state: Health disparities in South Florida. J Cult Div. 2003;10(2):50–5. [PubMed] [Google Scholar]
- 15.The National Cancer Institute N [Accessed 02 June 2004];State Cancer Profiles. http://statecancerprofiles.cancer.gov/
- 16.CDC [Accessed 18 Aug 2003];The burden of chronic disease and their risk factors: national and state perspectives chronic diseases, risk factors, and preventive services, Florida. Section IV. http://apps.nccd.cdc.gov/BurdenBook/DeathCause.asp?state=fl.
- 17.Trapido EJ. The epidemiology of cancer in Florida. Cancer Contr. 1998;5(3 Suppl 1):15–6. doi: 10.1177/107327489800503S05. [DOI] [PubMed] [Google Scholar]
- 18.Wilkinson JD, Wohler-Torres B, Trapido E, Fleming LE, MacKinnon J, Peace S. Cancer among Hispanic women in South Florida: an 18-year assessment: a report from the Florida Cancer Data System. Cancer. 2002;95(8):1752–8. doi: 10.1002/cncr.10834. [DOI] [PubMed] [Google Scholar]
- 19.Wilkinson JD, Wohler-Torres B, Trapido E, et al. Cancer trends among Hispanic men in South Florida, 1981–1998. Cancer. 2002;94(4):1183–90. [PubMed] [Google Scholar]
- 20.Modiano MR, Villar-Werstler P, Meister J, Figueroa-Valles N. Cancer in Hispanics: issues of concern. J Natl Cancer Inst Monogr. 1995;(18):35–9. [PubMed] [Google Scholar]
- 21.Rosenwaike I. Mortality of Hispanic populations: Mexicans, Puerto Ricans, and Cubans in the United States and in their home countries. Greenwood Press; Westport, CT: 1991. Mortality experience of Hispanic populations. [Google Scholar]
- 22.Diaz-Briquets S. Mortality patterns of Cubans in the United States. In: Rosenwaike I, editor. Mortality of Hispanic populations: Mexicans, Puerto Ricans, and Cubans in the United States and in the home countries. Greenwood Press; New York: 1991. pp. 111–32. [Google Scholar]
- 23.Mallin K, Anderson K. Cancer mortality in Illinois Mexican and Puerto Rican immigrants, 1979–1984. Int J Cancer. 1988;41(5):670–6. doi: 10.1002/ijc.2910410506. [DOI] [PubMed] [Google Scholar]
- 24.Rosenwaike I. Mortality differentials among persons born in Cuba, Mexico, and Puerto Rico residing in the United States, 1979–81. Am J Public Health. 1987;77(5):603–6. doi: 10.2105/ajph.77.5.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Department of Health and Human Services National Cancer Institute . Cancer in women of color monograph. Bethesda, MD: Jan, 2003. [Google Scholar]
- 26.NCHS . Vital and health statistics: quality of death rates by race and Hispanic origin a summary of current research. Department of Health and Human Services. Centers for Disease Control and Prevention; 1999. Publication No. (PHS) 99–1328. [Google Scholar]
- 27.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat. 1999;2(128):1–13. [PubMed] [Google Scholar]
- 28.Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47(3):1–16. 20. [PubMed] [Google Scholar]
- 29.Rosenwaike I. Cancer mortality among Puerto Rican-born residents in New York City. Am J Epidemiol. 1984;119(2):177–85. doi: 10.1093/oxfordjournals.aje.a113736. [DOI] [PubMed] [Google Scholar]
- 30.Rosenwaike I, Hempstead K. Mortality among three Puerto Rican populations. In: Rosenwaike I, editor. Mortality of Hispanic populations: Mexicans, Puerto Ricans, and Cubans in the United States and in their home countries. Greenwood Press; Westport, CT: 1991. [Google Scholar]
- 31.Althuis MD, Dozier JM, Anderson WF, Devesa SS, Brinton LA. Global trends in breast cancer incidence and mortality 1973–1997. Int J Epidemiol. 2005;34(2):405–12. doi: 10.1093/ije/dyh414. [DOI] [PubMed] [Google Scholar]
- 32.Anderson RN, Kochanek KD, Murphy SL. Monthly vital statistics report. 11, supp 2. Vol. 45. National Center for Health Statistics; Hyattsville, Maryland: 1997. Report of final mortality statistics, 1995. [Google Scholar]
- 33.Bosetti C, Malvezzi M, Chatenoud L, Negri E, Levi F, La Vecchia C. Trends in cancer mortality in the Americas, 1970–2000. Ann Oncol. 2005;16(3):489–511. doi: 10.1093/humrep/mdi086. [DOI] [PubMed] [Google Scholar]
- 34.Ramirez AG, McAlister A, Villarreal R, et al. Prevention and control in diverse Hispanic populations. Cancer Suppl. 1998;83(8):1825–9. [Google Scholar]
- 35.Gorin SS, Heck JE. Cancer screening among Latino subgroups in the United States. Prev Med. 2005;40(5):515–26. doi: 10.1016/j.ypmed.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 36.Zambrana RE, Breen N, Fox SA, Gutierrez-Mohamed ML. Use of cancer screening practices by Hispanic women: analyses by subgroup. Prev Med. 1999;29(6 Pt 1):466–77. doi: 10.1006/pmed.1999.0566. [DOI] [PubMed] [Google Scholar]
- 37.Ramirez AG, Suarez L. The impact of cancer on Latino populations. In: Guirre-Molina, Molina, Zambrana, editors. Health issues in the Latinor community. Jossey-Bass; San Francisco, CA: 2001. [Google Scholar]
- 38.Florida Department of Health [Accessed 10 Aug 2007];Office of planning, evaluation & data analysis. BRFSS Statewide report of core variables: section 15: Women’s Health. Generated by Dinorah-Martinez-Tyson; using Community health Assessment Resource Tool Set, http://www.floridacharts.com/charts/brfss.aspx.
- 39.Hajat A, Lucas JB, Kington R. Health outcomes among Hispanic subgroups: data from the National Health Interview Survey, 1992–95. Adv Data. 2000;310:1–14. [PubMed] [Google Scholar]
- 40.Cairney J, Ostbye T. Time since immigration and excess body weight. Cancer J Public Health. 1999;90(2):120–4. doi: 10.1007/BF03404114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Palinkas LA, Pickwel SM. Acculturation as a risk factor for chronic disease among Cambodian refugees in the United States. Soc Sci Med. 1995;40(12):1643–53. doi: 10.1016/0277-9536(94)00344-s. [DOI] [PubMed] [Google Scholar]
- 42.Chavez LR, Hubbell FA, Mishra SI. Ethnography and breast cancer control among Latinas and Anglo women in southern California. In: Baer H, editor. Anthropology in public health: bridging differences in culture and society. Oxford University Press; Oxford: 1999. pp. 117–41. [Google Scholar]
- 43.O’Malley AS, Kerner J, Johnson AE, Melblatt J. Acculturation and breast cancer screening among Hispanic women in New York City. Am J Public Health. 1999;89(2):219–27. doi: 10.2105/ajph.89.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ramirez AG, Suarez L, McAlister A, Villarreal R, Trapido E, Talavera GA, et al. Cervical cancer screening in regional Hispanic populations. Am J Public Health Behav. 2000;24(3):181–92. doi: 10.1093/her/15.5.559. [DOI] [PubMed] [Google Scholar]
- 45.Huerta EE. Cancer statistics for Hispanics, 2003: good news, bad news, and the need for a health system paradigm change. CA Cancer J Clin. 2003;53(4):205–7. doi: 10.3322/canjclin.53.4.205. [DOI] [PubMed] [Google Scholar]
- 46.Ramirez AG, McAlister A, Villarreal R, et al. Prevention and control in diverse Hispanic populations. Cancer Suppl. 1998;83(8):1825–9. [Google Scholar]
- 47.Hiatt RA, Pasick RJ, Stewart S, et al. Community-based cancer screening for underserved women: design and baseline findings from the Breast and Cervical Cancer Intervention Study. Prev Med. 2001;33(3):190–203. doi: 10.1006/pmed.2001.0871. [DOI] [PubMed] [Google Scholar]
- 48.O’Malley AS, Kerner J, Johnson AE, Mandelblatt J. Acculturation and breast cancer screening among Hispanic women in New York City. Am J Public Health. 1999;89(2):219–27. doi: 10.2105/ajph.89.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chavez LR, Hubbell FA, Mishra SI. Ethnography and breast cancer control among Latinas and Anglo women in southern California. In: Hahn RA, editor. Anthropology in public health. Oxford University Press; New York: 1999. pp. 117–41. [Google Scholar]
- 50.Huerta EE, Macario E. Communicating health risk to ethnic groups: reaching Hispanics as a case study. J Natl Cancer Inst Monogr. 1999;25:23–6. doi: 10.1093/oxfordjournals.jncimonographs.a024202. [DOI] [PubMed] [Google Scholar]
- 51.Li CI, Malone KE, Daling JR. Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med. 2003;163(1):49–56. doi: 10.1001/archinte.163.1.49. [DOI] [PubMed] [Google Scholar]
- 52.Ramirez AG, Suarez L, Laufman L, Barroso C, Chalela P. Hispanic women’s breast and cervical cancer knowledge, attitudes, and screening behaviors. Am J Health Promot. 2000;14(5):292–300. doi: 10.4278/0890-1171-14.5.292. [DOI] [PubMed] [Google Scholar]
- 53.Hymowitz N, Corle D, Royce J, et al. Smokers’ baseline characteristics in the COMMIT trial. Prev Med. 1995;24(5):503–8. doi: 10.1006/pmed.1995.1080. [DOI] [PubMed] [Google Scholar]
- 54.Perez-Stable EJ, Marin G, Posner SF. Ethnic comparison of attitudes and beliefs about cigarette smoking. J Gen Intern Med. 1998;13(3):167–74. doi: 10.1046/j.1525-1497.1998.00051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Howe HL, Wu X, Ries LA, et al. Annual report to the nation on the status of cancer, 1975–2003, featuring cancer among U.S. Hispanic/Latino populations. Cancer. 2006;107(8):1711–2. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- 56.Lee DJ, Markides KS, Ray LA. Epidemiology of self-reported past heavy drinking in Hispanic adults. Ethn Health. 1997;2(1–2):77–88. doi: 10.1080/13557858.1997.9961817. [DOI] [PubMed] [Google Scholar]
- 57.Marin G, Posner SF. The role of gender and acculturation on determining the consumption of alcoholic beverages among Mexican-Americans and Central Americans in the United States. Int J Addict. 1995;30(7):779–94. doi: 10.3109/10826089509067007. [DOI] [PubMed] [Google Scholar]
- 58.Irwin ML, Crumley D, McTiernan A, et al. Physical activity levels before and after a diagnosis of breast carcinoma: the health, eating, activity, and lifestyle (HEAL) study. Cancer. 2003;97(7):1746–57. doi: 10.1002/cncr.11227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Irwin ML, McTiernan A, Baumgartner RN, et al. Changes in body fat and weight after a breast cancer diagnosis: influence of demographic, prognostic, and lifestyle factors. J Clin Oncol. 2005;23(4):774–82. doi: 10.1200/JCO.2005.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Irwin ML, McTiernan A, Bernstein L, et al. Physical activity levels among breast cancer survivors. Med Sci Sports Exerc. 2004;36(9):1484–91. [PMC free article] [PubMed] [Google Scholar]
- 61.Irwin ML, McTiernan A, Bernstein L, et al. Relationship of obesity and physical activity with C-peptide, leptin, and insulin-like growth factors in breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2005;14(12):2881–88. doi: 10.1158/1055-9965.EPI-05-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mock V, Frangakis C, Davidson NE, et al. Exercise manages fatigue during breast cancer treatment: a randomized controlled trial. Psychooncology. 2005;14(6):464–77. doi: 10.1002/pon.863. [DOI] [PubMed] [Google Scholar]
- 63.Thune I, Brenn T, Lund E, Gaard M. Physical activity and the risk of breast cancer. N Engl J Med. 1997;336(18):1269–75. doi: 10.1056/NEJM199705013361801. [DOI] [PubMed] [Google Scholar]
- 64.Shai D, Rosenwaike I. Mortality among Hispanics in metropolitan Chicago: an examination based on vital statistics data. J Chronic Dis. 1987;40(5):445–51. doi: 10.1016/0021-9681(87)90178-0. [DOI] [PubMed] [Google Scholar]
- 65.Pablos-Mendez A. Mortality among Hispanics. JAMA. 1994;271(16):1237. [PubMed] [Google Scholar]
- 66.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 67.Abraido-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543–8. doi: 10.2105/ajph.89.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Winkleby MA, Rockhill B. Comparability of self-reported Hispanic ethnicity and Spanish surname coding. Hispanic J Behav Sci. 1992;14:487–95. [Google Scholar]
- 69.American Cancer Society . Cancer facts & figures for Hispanics 2000–2001. American Cancer Society; Atlanta: 2000. [Google Scholar]
- 70.Canto MT, Chu KC. Annual cancer incidence rates for Hispanics in the United States: surveillance, epidemiology, and end results, 1992–1996. Cancer. 2000;88(11):2642–52. doi: 10.1002/1097-0142(20000601)88:11<2642::aid-cncr29>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 71.Swallen KC, West DW, Stewart SL, Glaser SL, Horn-Ross PL. Predictors of misclassification of Hispanic ethnicity in a population-based cancer registry. Ann Epidemiol. 1997;7(3):200–6. doi: 10.1016/s1047-2797(96)00154-8. [DOI] [PubMed] [Google Scholar]
- 72.Department of Health and Human Services. Centers for Disease Control and Prevention . Vital and health statistics: quality of death rates by race and Hispanic origin a summary of current research. National Center for Health Statistics; 1999. Publication no. (PHS) 99–1328. [Google Scholar]
- 73.Gomez SL, Glaser SL, Kelsey JL, Lee MM. Bias in completeness of birthplace data for Asian groups in a population-based cancer registry (United States) Cancer Causes Control. 2004;15(3):243–53. doi: 10.1023/B:CACO.0000024244.91775.64. [DOI] [PubMed] [Google Scholar]
- 74.Becker TM, Wiggins CL, Key CR, Samet JM. Symptoms, signs, and ill-defined conditions: a leading cause of death among minorities. Am J Epidemiol. 1990;131(4):664–8. doi: 10.1093/oxfordjournals.aje.a115550. [DOI] [PubMed] [Google Scholar]
- 75.Kircher T, Anderson RE. Cause of death. Proper completion of the death certificate. J Am Med Rec Assoc. 1987;58(11):47–51. [PubMed] [Google Scholar]
- 76.Zambrana RE, Carter-Pokras O. Health data issues for Hispanics: implications for public health research. J Health Care Poor Underserved. 2001;12(1):20–34. doi: 10.1353/hpu.2010.0547. [DOI] [PubMed] [Google Scholar]
- 77.Gomez SL, Glaser SL. Misclassification of race/ethnicity in a population-based cancer registry (United States) Cancer Causes Control. 2006;17(6):771–81. doi: 10.1007/s10552-006-0013-y. [DOI] [PubMed] [Google Scholar]
- 78.Welch G, Black C. Are deaths within 1 month of cancer-directed surgery attributed to cancer? J Natl Cancer Inst. 2002;94:1066–70. doi: 10.1093/jnci/94.14.1066. [DOI] [PubMed] [Google Scholar]