Abstract
Two distinct genetic clades of seasonal influenza A(H1N1) viruses have cocirculated in the recent seasons: clade 2B oseltamivir-resistant and adamantane-susceptible viruses, and clade 2C viruses that are resistant to adamantanes and susceptible to oseltamivir. We tested seasonal influenza A(H1N1) viruses collected in 2008-2010 from the United States and globally for resistance to antivirals approved by the Food and Drug Administration. We report 28 viruses with both adamantane and oseltamivir (dual) resistance from 5 countries belonging to 4 distinct genotypes. Because of limited options for antiviral treatment, emergence of dual-resistant influenza viruses poses a public health concern, and their circulation needs to be closely monitored.
Since the 2007–2008 influenza season, seasonal (prepandemic) influenza A(H1N1) viruses with resistance to both classes of licensed antiviral drugs, M2 blockers (adamantanes) and neuraminidase inhibitors (NAIs), have been reported in the United States and globally (http://www.cdc.gov/flu/weekly/fluactivity.htm).
The markers of resistance to adamantanes are well established and include mutations at residues 26, 27, 30, 31, and 34 in the M2 protein [1, 2]; each change confers resistance to both adamantanes: amantadine and rimantadine. High levels of resistance to adamantanes have been reported globally since 2005 [3]; however, adamantane resistance in US seasonal influenza A(H1N1) viruses has been relatively low in recent seasons: 10.7% and .7% for the 2007–2008 and 2008–2009 seasons, respectively (http://www.cdc.gov/flu/weekly/). Conversely, adamantane resistance in southeast Asia has remained elevated (33%–100%) since 2007 [4]. Phylogenetically, the M genes of adamantane-susceptible and resistant seasonal influenza A(H1N1) viruses form 2 distinct clades: 2B and 2C, respectively [3]. Among recent viruses, clade 2C viruses carry the S31N mutation, the most commonly detected adamantane resistance marker. If adamantane resistance is detected in the primarily adamantane-susceptible clade 2B viruses, it is generally linked with the development of resistance during adamantane treatment [1, 2].
Rise in resistance to the NAI oseltamivir, due to the H275Y mutation (H274Y in N2 numbering) in the neuraminidase (NA), was first noted among seasonal influenza A(H1N1) viruses in 2007–2008 [5, 6]. Prevalence of oseltamivir-resistant influenza A(H1N1) viruses increased to approximately 100% in many countries during 2008–2009 [6]. These viruses, belonging to clade 2B, retained susceptibility to adamantanes and to the other licensed NAI, zanamivir [5, 6]. Interestingly, in some geographic regions, including China, the prevalence of oseltamivir-resistant seasonal influenza A(H1N1) viruses was lower [7].
Because only 2 classes of antiviral agents are licensed, the detection of viruses with resistance to drugs in both classes of antiviral agents is concerning. Recently, a growing number of seasonal influenza A(H1N1) viruses with resistance to both oseltamivir and adamantanes were reported from Hong Kong [8, 9]. We performed detailed analysis of 28 seasonal influenza A(H1N1) viruses with resistance to both oseltamivir and adamantanes (ie, dual-resistant) identified from global surveillance to gain insight into possible mechanisms for the emergence of these viruses.
MATERIALS and METHODS
Viruses.
During the 2008–2009 and 2009–2010 influenza seasons, US public health laboratories and National Influenza Centers from other countries submitted influenza virus isolates to the US Centers for Disease Control and Prevention (CDC) for virus strain characterization and antiviral resistance surveillance [5].
Pyrosequencing.
Pyrosequencing was conducted for the detection of the H275Y mutation in the NA and for markers of adamantane resistance in the M2 gene [3].
Conventional sequencing.
Full genome sequencing (PB2, PB1, PA, HA, NP, NA, M, and NS gene segments) of dual-resistant viruses was performed using the Sanger sequencing method on the 3730 xl DNA Analyzer (Applied Biosystems). RNA extraction and reverse-transcription polymerase chain reaction (RT-PCR) setup were performed using the same kits as for pyrosequencing [3]. RT-PCR products were cleaned up using ExoSAP-IT (USB Corporation). Sequencing reactions were prepared with the BigDye Terminator kit (version 3.1) and purified with the BigDye XTerminator kit (Applied Biosystems).
Phylogenetic analysis.
Gene sequences were aligned using BioEdit (version 7.0.9.0). The gene sequences of dual-resistant influenza viruses were deposited into GISAID. Phylogenetic analysis of each gene (data not shown) was performed using the Neighbor-Joining method, nucleotide model Tamura-Nei, MEGA version 4 [10].
Epidemiological investigation.
For US surveillance isolates, state health departments were asked to obtain epidemiological and clinical information for each patient (data not shown); the collection of information was deemed to be for surveillance purposes and not research.
RESULTS
Antiviral susceptibility surveillance for seasonal A(H1N1) viruses.
From 1 October 2008 to 30 September 2009 (the 2008–2009 influenza season), of the 1157 seasonal (prepandemic) influenza A(H1N1) viruses submitted from US public health laboratories, 1146 (99.0%) were resistant to oseltamivir and all were susceptible to zanamivir (http://www.cdc.gov/flu/weekly/). Of the 275 viruses submitted from other countries, 182 (66.2%) were resistant to oseltamivir and all were susceptible to zanamivir. Eight (7%) of 1157 viruses collected in the United States and 100 (34.8%) of 287 foreign viruses were resistant to adamantanes. From 1 October 2009 to 20 January 2010 (part of the 2009-2010 influenza season), 25 seasonal influenza A(H1N1) viruses collected globally were tested, and all were susceptible to both NAIs with the exception of one US virus that was resistant to oseltamivir. Of these 25 viruses, 18 (72%) were adamantane-resistant (Table 1).
Table 1.
Antiviral data and genetic clades for influenza A(H1N1) viruses with dual resistance to oseltamivir and adamantanes, 2008–2010
| Strain designation | Collection date | Country | NA mutation | M2 mutation | Antiviral exposure | Passage history* | PB2 | PB1 | PA | HA | NP | NA | M | NS | Genotype |
| A/Texas/38/2009ab | 02/08/09 | US | H275Y | V27A | Yes | X/C2 | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 1 |
| A/West Virginia/02/2009 | 03/18/09 | US | H275Y | S31N | No | R1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 1 |
| A/Kentucky/08/2009ab | 05/11/09 | US | H275Y | V27A | Yes | E1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 1 |
| A/Alberta/RV2859/2009 | 09/24/09 | Canada | H275Y | V27A | Unknown | C1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 1 |
| A/Kenya/1720/2009 | 08/14/09 | Kenya | H275Y | L26F | Unknown | X/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 2B | 1 |
| A/Fujian-Gulou/1581/2009 | 05/27/09 | China | H275Y | S31N | Unknown | E2/E1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hunan-Changning/52/2009 | 07/06/09 | China | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/4458/2009 | 07/06/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/4508/2009 | 07/10/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Fujian-Gulou/1896/2009 | 07/16/09 | China | H275Y | S31N | Unknown | E2/E1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Vietnam/2036/2009 | 07/22/09 | Vietnam | H275Y | S31N | Unknown | X/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/14775/2009 | 08/08/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Texas/57/2009a | 08/12/09 | US | H275Y | S31N | Yes | M1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Jiangsu-Quanshan/377/2009 | 09/07/09 | China | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/26547/2009 | 09/07/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Beijing-Chaoyang/1792/2009 | 09/09/09 | China | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/26552/2009 | 09/11/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Zhejiang-Liandu/1339/2009 | 09/23/09 | China | H275Y | S31N | Unknown | C1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Sichuan-Xiqu/325/2009 | 09/23/09 | China | H275Y | S31N | Unknown | C3/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Beijing-Chaoyang/11230/2009 | 10/15/09 | China | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Beijing-Chaoyang/11263/2009 | 10/17/09 | China | H275Y | S31N | Unknown | C1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/33773/2009 | 10/17/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/33774/2009 | 10/21/09 | Hong Kong | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Fujian-Shanghang/523/2009 | 10/22/09 | China | H275Y | S31N | Unknown | C1/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Hong Kong/33775/2009 | 10/23/09 | Hong Kong | H275Y | S31N | Unknown | C2/C2 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Sichuan-Dongqu/1836/2009 | 11/02/09 | China | H275Y | S31N | Unknown | C2/C1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2B | 2 |
| A/Guangdong-Zhuangzuyaozuzizhi/51/2009 | 03/13/09 | China | H275Y | S31N | Unknown | E1/E1 | 2B | 2B | 2B | 2B | 2B | 2B | 2C | 2C | 3 |
| A/Liaoning-Huanggu/1144/2009 | 03/23/09 | China | H275Y | S31N | Unknown | C2/C1 | 2C | 2C | 2C | 2C | 2C | 2B | 2C | 2C | 4 |
NOTE. NA = neuraminidase;
X = Unknown passage history;
E# = number of passages in embryonated chicken eggs;
C# = number of passages in MDCK cells;
R# = number of passages in RMK cells;
M# = number of passages in Monkey kidney cells;
passage indicated before the/indicate passages from submitting laboratory;
passage indicated after the/indicate passages at CDC;
treated with oseltamivir;
treated with adamantanes: amantadine or rimantadine;
GISAID accession numbers: EPI89455-EPI89457, EPI89861-EPI89863, EPI90085-EPI90087, EPI211257-EPI211259, EPI211263-EPI211265, EPI215523-EPI215525, EPI215535-EPI215536, EPI215538-EPI215540, EPI232853-EPI232855, EPI241608-EPI241610, EPI244128-EPI244130, EPI244149-EPI244157, EPI244243-EPI244245, EPI249557-EPI244560, EPI266810-EP1266935.
Epidemiological investigation of US cases of dual resistance.
Four seasonal influenza A(H1N1) viruses were resistant to both oseltamivir and adamantanes among US isolates from 2008 to 2010 (http://www.cdc.gov/flu/weekly/) (Table 1). Two of these patients with immunocompromising conditions were treated with amantadine prior to the collection of respiratory specimens. The other patients, one pregnant and the other with neurological conditions, did not receive adamantanes. None of the patients reported travel during the 7 days before onset of illness, and none reported illness in a family member or close contact during the week before or after their illness.
Dual-resistant viruses detected globally.
Twenty-one viruses collected in China, including 8 from Hong Kong SAR, as well as 1 virus each from Canada, Kenya, and Vietnam, were dually resistant to adamantanes and oseltamivir (Table 1). Information on exposure to adamantanes or to other antiviral agents was not available.
Full genome phylogenetic analysis of dual-resistant viruses.
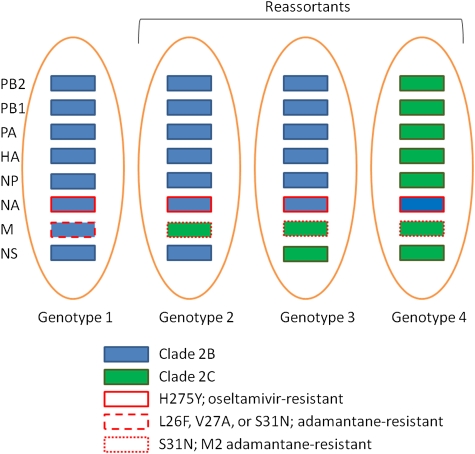
On the basis of full genome sequences, the genome composition of dual-resistant US seasonal influenza A(H1N1) isolates was consistent with genomes of previously characterized viruses bearing a clade 2B hemagglutinin (genotype 1), with the exception of A/Texas/57/2009 (H1N1) (Figure 1, Table 1). The genomes of Canadian and Kenyan dual-resistant viruses also belonged to genotype 1, whereas the majority of dual-resistant viruses from China and Vietnam were reassortants (genotype 2). A/Texas/57/2009 (H1N1) also belonged to genotype 2. Genotype 2 viruses are reassortants that inherited the M gene from clade 2C viruses and all other genes from clade 2B viruses. Two single instances of different genotypes, genotypes 3 and 4, were detected in viruses received from China. A/Guangdong-Zhuangsuyaozuzizhi/51/2009 (H1N1), possessed both the M and NS genes from clade 2C viruses (genotype 3), whereas A/Liaoning-Huanggu/1144/2009 (H1N1) contained a clade 2B NA gene in a clade 2C background (genotype 4).
Figure 1.
Summary of genotypes of dual-resistant seasonal influenza A(H1N1) viruses detected by full genome analysis, 2008–2010. Clade 2B genes are indicated by blue rectangles, and clade 2C genes are indicated by green rectangles. Oseltamivir resistance is indicated by a red solid outline. Adamantane resistance in the clade 2B M gene is indicated by a red dashed outline. Adamantane resistance in the clade 2C M gene is indicated by a red dotted outline. Reassortant genotypes are indicated by the bracket.
DISCUSSION
We characterized 28 seasonal influenza A(H1N1) viruses from 2008 to 2010 that were dually resistant to oseltamivir and adamantanes from 5 countries: the United States, Canada, China, Kenya, and Vietnam. These viruses retained susceptibility to only 1 licensed influenza antiviral agent, inhaled zanamivir. Seven of the dual-resistant viruses were collected during the 2009–2010 influenza season, 21 were from the previous season (2008–2009), and 1 was detected during the 2007–2008 season. Although dual-resistant viruses are still rare, the increase in prevalence among seasonal influenza A(H1N1) viruses was notable during the last 3 seasons, .06% (1 of 1753 tested in 2007–2008), 1.5% (21 of 1426 in 2008–2009), and 28% (7 of 25 in 2009–2010) (χ2; P<.001). Although few seasonal A(H1N1) viruses circulated during 2009-2010 and it is uncertain whether seasonal and pandemic A(H1N1) viruses will cocirculate in future seasons, the detection of dual-resistant seasonal A(H1N1) viruses from 5 countries warrants concern because of the limited treatment options currently available for dual-resistant influenza A viruses.
The acquisition of a mutation in an influenza A virus that confers resistance to an antiviral agent may occur as a result of drug selection, spontaneous mutation, or through genetic reassortment with another drug-resistant influenza A virus. The development of resistance to oseltamivir while on therapy was documented to occur in 1%–18% of patients, including immunocompromised patients, depending on age, treatment regimens, and other differences [11]. The emergence and widespread detection of oseltamivir-resistant seasonal influenza A(H1N1) viruses in the 2008–2009 season is not well understood; however, some evidence suggests that the H275Y mutation in the NA may have occurred spontaneously, without apparent drug pressure or reassortment [12, 13]. In contrast, adamantane resistance has been reported in 30%–80% of isolates from patients treated in clinical studies or during outbreak investigations [3]. In addition, current seasonal influenza A(H1N1) viruses from clade 2C are typically oseltamivir-susceptible and carry the S31N marker of adamantane resistance in the M2 protein, whereas recent clade 2B seasonal influenza A(H1N1) viruses are primarily adamantane-susceptible and carry the oseltamivir resistance-conferring mutation H275Y in the NA gene.
In this study, the dual-resistant viruses belonged to 4 genetic backgrounds on the basis of full genome sequence analysis. Of the US viruses of genotype 1, all genes similar to clade 2B viruses, 2 were identified in severely immunocompromised patients after adamantane treatment. The third US genotype 1 virus was isolated from a patient that did not have a severe immunocompromising condition and received no antiviral agents, suggesting that the virus causing this infection either spontaneously acquired the S31N mutation in the M2 protein or was possibly transmitted from a person treated with adamantane. All 3 of these cases would be consistent with an oseltamivir-resistant clade 2B virus acquiring adamantane resistance through treatment or transmission.
The fourth US case was a genotype 2 virus from a patient with an influenza infection unassociated with adamantane treatment. As evidenced by a 2B backbone and a 2C M gene (genotype 2), adamantane resistance in this virus was likely the result of a reassortment between clade 2B and 2C viruses. An additional 21 dual-resistant viruses in this report were similar reassortants belonging to genotype 2. The predominance of genotype 2 dual-resistant viruses may suggest that the presence of the 2C M gene provides either a fitness advantage over viruses with clade 2B M gene or could be the result of the continued use of adamantanes in some populations. The S31N mutation is also the marker detected in nearly all recent adamantane-resistant seasonal A(H3N2) viruses and 2009 pandemic A(H1N1) viruses (http://www.cdc.gov/h1n1flu/) [3, 14, 15]. However, adamantane resistance in A(H3N2) viruses and 2009 pandemic A(H1N1) viruses were acquired independently (http://www.cdc.gov/h1n1flu/) [16].
Interestingly, 3 of the 5 viruses from North America, including the Canadian virus, A/Alberta/RV2859/2009 (H1N1), contained the less common V27A change in the M2 protein, whereas the other 2 viruses contained the most commonly detected mutation: S31N. Of note, one dual-resistant virus, A/Kenya/1720/2009 (H1N1), also contained another less common adamantane resistance marker: L26F. At this time it is unclear whether these uncommon changes (L26F and V27A) in the M2 protein, all genotype 1 viruses, emerged due to treatment as seen in the 2 US cases, A/Texas/38/2009 (H1N1) and A/Kentucky/08/2009 (H1N1), or if adamantine-resistant viruses with 2B M genes with those mutations circulate regionally.
Genotype 2 and genotype 3 dual-resistant viruses from Asia appear to be genetically similar to previously reported dual-resistant viruses from Hong Kong SAR [8, 9]. The genotype 4 virus, A/Liaoning-Huanggu/1144/2009 (H1N1), was the only dual-resistant virus with a nearly complete 2C genome. Oseltamivir resistance in the A/Liaoning-Huanggu/1144/2009 (H1N1) virus appears to be the result of a reassortment between 2B and 2C viruses, as revealed by the presence of the oseltamivir-resistant clade 2B NA gene. Although the exact mechanisms are unknown, it is likely that the development of dual resistance in reassortant viruses, genotypes 2–4, arose from coinfection with a clade 2B oseltamivir-resistant virus and a clade 2C adamantane-resistant virus. Such intrasubtype reassortment of cocirculating strains has been observed in influenza A viruses [16].
The detection of influenza A(H1N1) viruses that are resistant to both adamantanes and oseltamivir warrants close monitoring. If circulation of viruses with dual resistance to both oseltamivir and adamantanes becomes more widespread among any of the predominant circulating influenza A viruses (eg, 2009 pandemic H1N1, H5N1, etc), treatment options would be extremely limited, especially in young children and for severely ill patients. New antiviral agents and strategies for antiviral therapy are likely to be necessary in the future.
Funding
This work is supported by the Centers for Disease Control and Prevention.
Acknowledgments
We thank our collaborators in the World Health Organization Global Influenza Surveillance Network, including the National Influenza Centers, for the submission of isolates; the Virus Reference Team, Sequencing Activity, and other members of the Influenza Division for their technical assistance and useful discussions.
We would also like to acknowledge Danae Bixler and Dorothy Lockett from the Wetzel County Health Department, the West Virginia Office of Laboratory Services, and Gail Demmler-Harrison and Heather Cook from the Austin/Travis County Health and Human Services Department for their assistance in the epidemiological investigation described.
References
- 1.Hay AJ, Zambon MC, Wolstenholme AJ, Skehel JJ, Smith MH. Molecular basis of resistance of influenza A viruses to amantadine. J Antimicrob Chemother. 1986;18( Suppl B):19–29. doi: 10.1093/jac/18.supplement_b.19. [DOI] [PubMed] [Google Scholar]
- 2.Belshe RB, Smith MH, Hall CB, Betts R, Hay AJ. Genetic Basis of Resistance to Rimantadine Emerging during Treatment of Influenza Virus Infection. J Virol. 1988;62(5):1508–1512. doi: 10.1128/jvi.62.5.1508-1512.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deyde VM, Gubareva LV. Influenza genome analysis using pyrosequencing method: current applications for a moving target. Expert Rev Mol Diagn. 2009;9(5):493–509. doi: 10.1586/erm.09.21. [DOI] [PubMed] [Google Scholar]
- 4.Barr IG, Deng YM, Iannello P, Hurt AC, Komadina N. Adamantane resistance in influenza A(H1) viruses increased in 2007 in South East Asia but decreased in Australia and some other countries. Antivir Res. 2008;80:200–205. doi: 10.1016/j.antiviral.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Sheu TG, Deyde VM, Okomo-Adhiambo M, et al. Surveillance for neuraminidase inhibitor resistance among human influenza A and B viruses circulating worldwide from 2004 to 2008. Antimicrob Agents Chemother. 2008;52:3284–3292. doi: 10.1128/AAC.00555-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lackenby A, Hungnes O, Dudman SG, et al. Emergence of resistance to oseltamivir among influenza A(H1N1) viruses in Europe. Euro Surveill. 2008;13(5):pii 8026. doi: 10.2807/ese.13.05.08026-en. [DOI] [PubMed] [Google Scholar]
- 7.Hurt AC, Ernest J, Deng Y-M, et al. Emergence and spread of oseltamivir-resistant A(H1N1) influenza viruses in Oceania, South East Asia and South Africa. Antivir Res. 2009;83:90–93. doi: 10.1016/j.antiviral.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 8.Cheng PK, Leung TW, Ho EC, et al. Oseltamivir- and amantadine-resistant influenza viruses A(H1N1) Emerg Infect Dis. 2009;15:966–968. doi: 10.3201/eid1506.081357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng PK, To AP, Leung TW, Leung PC, Lee CW, Lim WW. Oseltamivir- and amantadine-resistant influenza virus A(H1N1) Emerg Infec Dis. 2010;16(1):155–156. doi: 10.3201/eid1601.091304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamura K, Dudley J, Nei M, et al. MEGA4: molecular evolutionary genetics analysis (MEGA) software version 4.0. Mol Biol Evol. 2007;24(8):1596–1599. doi: 10.1093/molbev/msm092. [DOI] [PubMed] [Google Scholar]
- 11.Lackenby A, Thompsom CI, Democratis J. The potential impact of neuraminidase inhibitor resistant influenza. Curr Opin Infect Dis. 2008;21:626–638. doi: 10.1097/QCO.0b013e3283199797. [DOI] [PubMed] [Google Scholar]
- 12.Hauge SH, Blix HS, Borgen K, Hungnes O, Dudman SG, Aavitsland P. Sales of oseltamivir in Norway prior to the emergence of oseltamivir resistant influenza A(H1N1) viruses in 2007-08. Virol J. 2009;6:54. doi: 10.1186/1743-422X-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tashiro M, McKimm-Breschkin JL, Saito T, et al. Neuraminidase Inhibitor Susceptibility Network. Surveillance for neuraminidase-inhibitor-resistant influenza viruses in Japan, 1996-2007. Antivir Ther. 2009;14(6):751–761. doi: 10.3851/IMP1194. [DOI] [PubMed] [Google Scholar]
- 14.Barr IG, Hurt AC, Iannello P, Tomasov C, Deed N, Komadina N. Increased adamantane resistance in influenza A(H3) viruses in Australia and neighboring countries in 2005. Antivir Res. 2007;73(2):112–117. doi: 10.1016/j.antiviral.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Zaraket H, Saito R, Sato I, et al. Molecular evolution of human influenza A viruses in a local area during eight influenza epidemics from 2000 to 2007. Arch Virol. 2009;154(2):285–295. doi: 10.1007/s00705-009-0309-9. [DOI] [PubMed] [Google Scholar]
- 16.Nelson MI, Edelman L, Spiro DJ, et al. Molecular epidemiology of A(H3N2) and A(H1N1) influenza virus during a single epidemic season in the United States. PLos Pathog. 2008;4(8):e1000133. doi: 10.1371/journal.ppat.1000133. [DOI] [PMC free article] [PubMed] [Google Scholar]