Abstract
Kristin, a 38-year-old female with breast cancer, was scheduled to begin treatment a week after receiving her diagnosis. Although she was in a four-year-long relationship, she had never thought about having kids. Kristin was told that embryo banking (IVF) was the best option for fertility preservation, and she had to decide immediately if she wanted biological children in order to start an egg-retrieval cycle. Because no other options were provided and she was uncertain about freezing embryos with her current partner, she ended up foregoing fertility preservation prior to the treatments that ultimately left her infertile. Ethan, a 19-year-old male, was in the hospital for four days awaiting surgery to remove a pelvic sarcoma. The surgery required removal of his testes rendering him infertile. During those four days, no one talked to him or his family about sperm banking, even though it could have been accomplished in a matter of minutes.
Introduction
As these scenarios illustrate, cancer patients and their families face a crucible of high-stake decisions during a time of extreme stress. They must cope with the shock and fear that attends a cancer diagnosis and navigate a complex set of treatment options. Then there is the often neglected issue of fertility preservation (FP) for those of reproductive age. Many cancer treatments, including surgery, radiation, and chemotherapy, carry significant risks of irreversibly compromising a patient’s fertility. Patients are often unaware of these risks and in far too many cases, their health-care providers (HCPs) do not adequately inform them of these risks or available fertility preserving or sparing options.
Improving both patient and provider education on the impact of cancer treatments on fertility and the wide range of available fertility options is essential to providing both quality and ethical health care. How can we create a resource that is accessible and effective during the very short and extremely stressful window of time between receiving a cancer diagnosis and commencing treatments that may have permanent and irreversible impacts on fertility? How can we provide the information that patients require to advocate for their needs and make informed decisions when they are already overwhelmed with highly technical medical information concerning their cancer diagnosis, treatment options, side effects, and likely prognosis?
In this chapter, we describe our efforts to address this unique patient education challenge through the design of an innovative web site called MyOncofertility.org. MyOncofertility.org educates health-care providers, patients, and patients’ families about fertility preservation (FP) options when faced with a cancer diagnosis and subsequent treatment. MyOncofertility.org was designed to support patient education and time-critical decision making during periods of extremely high stress and information overload. We begin this chapter by looking at the advantages of the Internet as a tool for patient education in general. Then we focus on the specific challenges associated with patient education for oncofertility. Next, we identify design guidelines and explain how we used them to design the MyOncofertility.org site to address these challenges. Finally, we discuss how the lessons learned from the MyOncofertility.org project can be applied to the wider patient education context.
The Internet as a Powerful Tool for Patient Education
Patient education has become a high priority in various preventative health care and disease management campaigns. Better-educated patients tend to be healthier and more compliant with prescribed treatment and medication regimens [1]. Patient education is a naturally interactive process and the Internet is a well-adapted medium for interactive learning. Furthermore, the advent of widely available Internet access and rich media has created exceptional opportunities for delivering high-quality patient education [2].
Much of the research in patient education has focused on the message content and not the specific affordances of the Internet for message delivery. As a learning tool, the Internet has some unique advantages over other media, including customization of information presented, 24/7 availability, worldwide distribution, a private learning environment, support for decision-making processes, the potential to simulate real-life experiences, easily updated content, and the presentation of rich media including videos and animations. A review of the literature is provided by Lewis [3]. A summary of this literature shows that clinical outcomes are improved, and that patients learn and retain information better when using computer-based media versus traditional instruction [3]. Lewis concludes, “The social integration and sharing of knowledge that occurs through these new connections may increase involvement in learning and expand patients’ understanding of their medical conditions [3].” Another important function of an Internet-based patient education site is that it allows HCPs to refer patients to such resources when appropriate, thereby freeing up time during office visits to focus on critical patient interactions such as diagnosis and discussion of treatment options and specific questions within their areas of expertise.
Fertility Preservation and Patient Education
Fertility preservation in the face of a cancer diagnosis is fraught with challenges that must be thoughtfully considered when designing a suitable patient education resource. News of a cancer diagnosis can be traumatic, overwhelming, and imposes extreme stress and hardship on patients and their families. Yet it is essential that fertility preservation options be addressed prior to cancer treatment in order to provide patients with the greatest number of options and chances for fertility success [4–6].
The data on current practices in FP education and counseling are sobering. Research shows that women who are treated with either radiation or chemotherapy during reproductive years have a 40–80% chance of losing fertility [6]. With male patients, the sterility rate is slightly lower (30–75%), but nevertheless significant enough to merit FP counseling [7]. A study by Quinn et al. states that less than 50% of adult cancer patients of childbearing age “… receive adequate or appropriate education, counseling, and resources about reproductive decisions prior to their cancer treatment and at least 40% of cancer patients of childbearing age who receive treatment are not informed about the potential impact of treatment on fertility [8].” Furthermore, follow-up surveys demonstrate that cancer survivors with treatment induced infertility are at greater risk for emotional distress [8]. While awareness of the importance of FP counseling is improving among HCPs, we know that we still have a long way to go.
Fertility Preservation Communication Barriers and Challenges
Numerous barriers inhibit FP communication among health-care providers, patients, and their families. Given that early intervention is a critical success factor for surviving cancer, patients, patients’ relatives, and HCPs are understandably anxious to start treatment as soon as possible. The urgency for cancer treatment upon diagnosis means that FP discussions are often neglected. Even when fertility options are discussed, the window for considering such options after an initial diagnosis is short and patients must be prepared to make well-informed, potentially life changing decisions within a relatively short time horizon. In aggressive cancer cases, any unreasonable delays to treatment are strongly discouraged. Furthermore, there are significant costs associated with FP, particularly cryopreservation, which may require an out-of-pocket storage fee that can run from hundreds to thousands of dollars annually. Therefore, some HCPs and oncology social workers expressly neglect to discuss FP with cancer patients who clearly cannot afford it, citing ethical dilemmas in offering their patients a service the patient presumably cannot afford. Other patient characteristics, particularly patient age, number of children, and the stage of cancer development also influence HCPs in making unilateral decisions about discussing FP options with patients [9].
Although general guidelines by the American Society of Clinical Oncology (ASCO) have been established concerning FP [10], these guidelines are seldom referred to and not widely disseminated. While information resources concerning FP exist, many HCPs are simply unaware of such resources and do not provide them to patients. Furthermore, many oncologists believe that FP counseling is beyond the scope of their practice, and so they may be reluctant to discuss FP with patients; they may simply assume that other HCPs such as reproductive endocrinologists or obstetrician and gynecological surgeons will attend to this task. Ambiguity regarding the roles and responsibilities of HCPs with respect to FP often results in inadequate FP counseling or in some cases, no counseling [8, 9].
Lastly, the news of a potentially life-threatening cancer diagnosis is traumatic and can significantly impair a patient’s, parents’, or partner’s decision-making abilities [11]. Given the wide range of treatment options and the large volume of medical information on oncology, patients are often overwhelmed with treatment options and unable to process yet another major medical decision such as FP. The urgency, stress, and confusion associated with a cancer diagnosis, the lack of patient education about the impact of cancer treatments on fertility options, and HCPs who often neglect to raise the issue with patients or are not up to date on the full range of FP options all combine to make patient education on FP both difficult and essential. The medical and social science literature are unambiguous about the need for better fertility preservation education for patients of cancer. We now turn to an exploration about how the MyOncofertility.org web site was designed to meet the challenges of designing a patient education resource for oncofertility.
MyOncofertility.org Design Goals
Cancer and oncofertility are serious subjects. Nevertheless, MyOncofertility.org provides a hopeful, human, and inspirational message to users in a way that is both respectful and authoritative. The following are the goals that guided the design of MyOncofertility.org and a discussion of the various methods employed to achieve these goals (Table 26.1).
Table 26.1.
Principal goals for MyOncofertility.org
| Principal goals for MyOncofertility.org |
|---|
|
The Use of Media
MyOncofertility.org makes use of several media, including video, animations, still images, and text. Expert videos and video testimonials of survivors as well as those of relatives, partners, and parents of cancer patients are a prominent feature of the site (see Figs. 26.1 and 26.2). Research in the field of narratology has confirmed that storytelling plays a privileged role in human communication. Postmodern theorist Richard Rorty suggests that the principal role of narrative is that it fosters human solidarity by creating shared experiences [12]. The use of video supports one of the major goals of the site, which is to help users identify with others in similar situations in order to alleviate their feelings of isolation. Video is also particularly useful for children, the elderly, patients with poor literacy, or those with impaired vision.
Fig. 26.1.
MyOncofertility.org videos of survivor experiences
Fig. 26.2.
My Oncofertility.org videos of experts
Studies have shown that video provides patients with “opportunities for enhanced social interaction, diminished feelings of isolation, and improved self-esteem [3].” A study comparing various forms of patient education media found that patients were able to “accomplish learning tasks significantly better when using interactive video [13].” The same study demonstrated that patients with poor literacy can benefit from the customized pace of video instruction and the non-threatening, private learning environment. Another study found that interactive video is preferred to text among patients [14]. Video was critical in achieving the design and usability goals for theMyOncofertility.org web site. While video is more expensive to produce than textual content, we believe the benefits far outweigh the costs.
Narrated animations (see Fig. 26.3) were used to illustrate various fertility preservation procedures and educate users about how cancer treatments affect fertility. Animations were developed to convey complex, multi-step processes using a combination of auditory narrative and animated visuals. Though the processes described by the animations are complex, the animations themselves are purposefully uncomplicated, void of any superfluous visual information, and describe oncofertility processes in concise language that is easy for a lay audience to understand. Analysis of usage data indicates that visitors find these rich media resources among the most valuable on the site (see full discussion below).
Fig. 26.3.
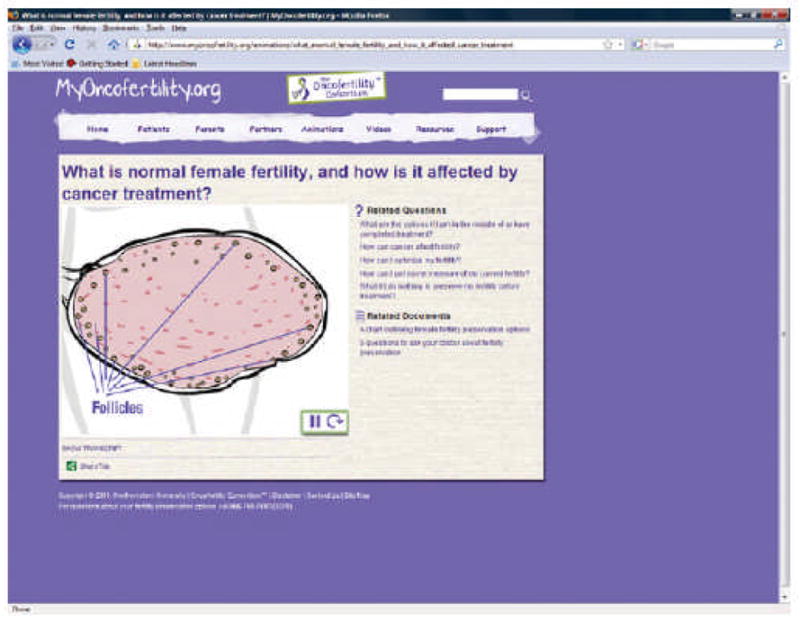
MyOncofertility.org animation of normal female fertility
An Appropriate Design Motif
A key goal of our interface design for the MyOncofertility.org site was to make it feel warm, welcoming, accessible, and non-threatening to our audience. We decided to adopt a scrapbook motif as an informal, yet dynamic approach to achieve this design goal. The scrapbook motif was achieved by employing various scrapbook design elements and frames such as post-it notes, polaroid photos, torn paper, paperclips, and Scotch tape (see Fig. 26.4). In order to soften the interface, the site employs hand-drawn elements and scripted, sans-serif fonts. The animations used within the site were also hand-drawn as opposed to machine rendered. These hand drawn elements create a more human and less threatening interface (see Figs. 26.4 and 26.3). The use of warm pastel colors throughout the site is reminiscent of a pre-school or perhaps a maternity ward and thus provides hope to cancer patients desiring biological children. Among the few exceptions to the pastel theme is the use of a deep blue background for expert videos. The consistent deep blue color conveys authority and consistency of message.
Fig. 26.4.
MyOncofertility.org home page
In designing the look and feel of the site, we chose to include photographs of individuals and families that our audience would relate to and that would emphasize our goals of making the site feel warm, welcoming, and non-threatening. The still images used for the site were carefully selected and vetted by focus groups of cancer patients and their relatives in collaboration with Gilda’s Club of Chicago (see Figs. 26.4, 26.5, and 26.6). For example, it was initially unclear as to whether using an image of a pregnant woman would be offensive to visitors who might be struggling with fertility issues. However, a series of focus group sessions demonstrated that such an image was not only inoffensive but also hopeful to prospective parents. In keeping with the genuine nature of the site, the images used within the site portray a wide range of human emotions without trying to whitewash the realities of cancer and fertility treatments.
Fig. 26.5.
MyOncofertility.org patient timeline for women
Fig. 26.6.
MyOncofertility.org web resources
User Control and Participation
When users first enter the site, they are presented with an intuitive navigation scheme and are invited to self-identify as patients, parents, or partners (see Fig. 26.5). The information presented to them subsequent to this self-identification is filtered to be relevant to their specific needs. A secondary navigation scheme uses a treatment timeline to situate users at various stages – from initial diagnosis to survivorship – further filtering the relevant information presented to them.
Since information overload has been identified as one of the key barriers to FP communication, the site was designed for quick access to layered information which progresses in complexity as users drill down to greater and greater detail. In a similar fashion, the questions posed to users on side- and sub-panels progress from simple to complex.
Throughout the site, a question and answer (Q&A) model was employed based on the expert/novice dyad conversation model. Modeled after the Q&A dialogue that would occur between a doctor and a patient (or between teacher and student), users are presented with questions that, when clicked, link to an answer to that question. After reading or viewing the answer (as text, video, or animation), a number of related follow-up questions or resources are presented. By clicking on a follow-up question, the user mimics the natural question/answer/follow-up question process that occurs in face-to-face dialogues.
User participation is a critical aspect of the site both pre- and post-launch. Focus groups were consulted throughout the design phase and users are invited to participate and contribute to the site as it evolves. The scrapbook motif (see above) supports the site’s dynamic, interactive, and evolving nature. Pink notes prompting users for feedback with captions such as “Suggest a question” or “Share my story!” give users the option to contribute to the site by sharing resources or a personal story of their experience with cancer and FP. Such an approach fosters a sense of solidarity and community and allows us to be responsive to users’ needs for information that may have been initially overlooked. Future plans for the site include creating an online community via message boards and social networking.
Applying Design Principles from MyOncofertility.org to Other Patient Education Web Sites
To facilitate the application of the design of MyOncofertility.org to other patient education web sites, we now examine the key principles that informed the design of the site and the user interaction it supports. Table 26.2 summarizes these principles, which are then discussed in turn.
Table 26.2.
Principles for designing a patient education resource
| Principles for designing a patient education resource |
|---|
|
Users should be in full control of the browsing experience. Among the most important principles for designing a patient education resource is that users should be in full control of the browsing experience. In the case of MyOncofertility.org, this meant providing an intuitive navigation bar either to the left (see Fig. 26.4) or on top of the page (see Fig. 26.5). All the videos and animations used within the site have navigation bars that allow users to stop, play, rewind, pause, or skip to any part as they chose. Furthermore, users are given the opportunity to read the transcripts of both videos and animations. No information is presented without the user initiating a request.
Limit the quantity of information provided at any given time and delimit to a single topic. Information overload is often an issue with patient education, and this was certainly the case with oncofertility. Therefore, limiting the amount of information that users can access at any given time is crucial to providing good user experiences. MyOncofertilty.org invites users to self-identify as patients, parents, or partners. Upon self-identification, the information presented to users is specific to their particular case. Also, a navigational timeline situates users at a particular stage in their journey, further delimiting the information presented to them.
Limit complexity of information to depth that the user requests start simple and allow for drill down. In addition to the design features described above, MyOncofertility.org presents information in layers of complexity. Initial questions and answers are general and non-technical. Follow-up questions become increasingly more specific and technical; only after viewing the answer to a general question are the more detailed questions presented. This means that many of the resources on MyOncofertility.org are intentionally hidden from users until such time as they request them by drilling down, or by navigating to them from menus or timelines.
Utilize a navigation scheme that provides a common and easily recognized framework for your audience. Employ chronology, roles, and user characteristics to develop an intuitive navigation scheme that meets the needs of your audience and does not force them to adopt technical classification schemes more familiar to experts (e.g., disease stages). Whenever relevant, the navigation scheme should be time sensitive and address your audience before, during, and after treatment. Consider roles (patient, parent, and provider) and user characteristics, such as age, gender, phase in treatment, or other treatment-specific criteria as additional navigational structures to help users find the information most relevant to them.
Employ a Q&A model such as the one based on the expert/novice dyad conversation model. The expert/novice dyad conversation model is among the most interactive models for learning and, furthermore, the Internet is particularly well suited to this model. We recommend modeling information access on a site after a question and answer dialogue which might occur between a health-care provider and a patient and then provide branching logic for follow-up questions.
Use video and animations strategically to help make complex concepts, processes, treatment effects, or timelines understandable and accessible. Studies show the effectiveness of animations and videos in conveying complex processes such as those associated with medical treatment. Employing animations and videos throughout a patient education web site will make it more accessible.
Use the power of first-person video stories to improve communication of difficult topics, create emotional connections, and assuage patient feelings of isolation. Studies have demonstrated that video is not only an effective learning tool but also has the additional benefit of alleviating feelings of isolation and anxiety among users. We recommend that patient education web sites make strategic use of both expert videos and survivor/relative testimonials.
Make sure each page of your site can be found directly via search engines by using search engine-friendly HTML. When using video, Flash, or other rich media, provide full text transcriptions that are visible to search engines. Early prototypes of MyOncofertility.org made extensive use of a vector graphics rendering technology called Flash. Though Flash sites are among the most dynamic and interactive on the Internet, there is very little text which can be indexed within Flash sites, and so search engines often have difficulty navigating and indexing such sites as well as the links contained therein. Subsequent iterations of MyOncofertility.org used search engine-friendly HTML. All the videos and animations within MyOncofertility.org were accompanied by text transcriptions visible to search engines making them a simple click away from users (see Fig. 26.3). These transcriptions (see Table 26.2) proved to be extremely useful as they allowed search engines to properly index the content of both video and animations.
Insights from MyOncofertility.org Usage Data
According to data gathered from Google Analytics for the period between October 26, 2008 and October 26, 2009, MyOncofertility.org had 10,754 visitors, of which 80% were new visitors. On average, users visited four pages and spent 3 min viewing the site per visit. A closer examination of usage patterns is also quite revealing. A particularly useful measure in web site analytics is landing page data. A landing page is a web page that is linked directly from other sites, or one that visitors access directly from search engines (rather than arriving from other pages within the site itself). Validating our use of rich media like video and animation on the site, Table 26.3 below shows that the top landing pages – aside from the home page – were either video or animation pages. These data confirm three important observations: (1) third parties appreciate the value of the videos and animations on MyOncofertility.org because they are placing direct links to them on their own web sites; (2) search engines are properly indexing the transcribed text content for videos and animations at MyOncofertility.org so that they can be easily found; and (3) these pages contain among the most highly relevant information for popular search terms sought by our visitors.
Table 26.3.
Top 10 landing pages (data compiled from Google analytics for the period between October 26, 2008 and October 26, 2009)
| Top 10 landing pages | Page visits (annual) |
|---|---|
| Home page | 4,408 |
| Video (expert): what_cost_freezing_eggs_and_embryos | 221 |
| Video (survivor): i_was_diagnosed_stage_2_hodgkins_lymphoma_during_my_engagement | 208 |
| Video (survivor): my_experience_deciding_use_donor_sperm_my_family | 187 |
| Video (expert): what_difference_between_icsi_and_ivf | 155 |
| Animation: what_normal_female_fertility_and_how_it_affected_cancer_treatment | 141 |
| Video (survivor}: my_experience_chemotherapy_and_its_side_effects | 120 |
| Video (expert): pregnancy_safe_after_chemotherapy | 115 |
| Video (survivor): how_i_learned_inject_myself_ivf_process | 106 |
| Video (expert): who_dr_teresa_woodruff | 105 |
Among the greatest strengths of using the Internet over other media is worldwide exposure. Table 26.4 lists the top 10 countries accessing the MyOncofertility.org web site. Not surprisingly, not only English-speaking countries but also countries where English is widely spoken as a second language were well represented among users. Other factors that may have contributed to these data are active oncofertility researcher communities within particular regions, oncofertility events hosted by particular countries, and articles on oncofertility published in journals that are popular in particular regions. An analysis of the country of origin for visitors to the site can indicate which languages would be top priority for any translation of the site.
Table 26.4.
Top 10 user countries (data compiled from Google analytics for the period between October 26, 2008 and October 26, 2009)
| Top 10 user countries | Visits (annual) |
|---|---|
| United States of America | 8,001 |
| United Kingdom | 483 |
| Canada | 390 |
| Australia | 223 |
| India | 214 |
| Netherlands | 177 |
| Philippines | 78 |
| Germany | 55 |
| Poland | 54 |
| Ireland | 53 |
The primary way that a web site is found by potential visitors is through search engines like Google or Yahoo!. Analyzing the search terms used most frequently by visitors arriving to the site from search engines is revealing because such terms indicate preferences and trends among users. These data can then guide the authoring of content for the site in subsequent iterations so that popular search terms appear and thus attract visitors to those pages. The following table shows the top 20 keyword searches for MyOncofertility.org. The keyword phrases that stand out are “Teresa woodruff,” “adriomyacin,” “oncofertility consortium,” “cost of freezing eggs,” “difference between icsi and ivf,” “pregnancy after chemotherapy,” and “fertility hotline.” Teresa Woodruff founded the oncofertility consortium and coined the term oncofertility – thus it makes sense that visitors might use her name or that of the consortium to find the site. The other keyword phrases are technical, reflect user concerns about the costs associated with fertility preservation, or are terms one might use to seek help (Table 26.5).
Table 26.5.
Top 20 keyword search terms (data compiled from Google analytics for the period between October 26, 2008 and October 26, 2009)
| Top 20 keyword search terms | Visits per keyword search term (annual) |
|---|---|
| My oncofertility | 161 |
| Oncofertility | 120 |
| Myoncofertility | 102 |
| Myoncofertility.org | 88 |
| Teresa woodruff | 64 |
| Adriomyacin | 53 |
| Oncofertility consortium | 46 |
| Cost of freezing eggs | 41 |
| Difference between icsi and ivf | 35 |
| Cost of freezing embryos | 34 |
| Stage 2 lymphoma | 33 |
| Wet heat | 33 |
| Difference between ivf and icsi | 30 |
| Pregnancy after chemotherapy | 29 |
| Myoncofertility.com | 28 |
| www.myoncofertility.org | 27 |
| Female procedures | 26 |
| Fertility hotline | 26 |
| Stage 2 hodgkins lymphoma | 26 |
| Embryo banking | 25 |
After search engines, the other way that visitors can find this site is by following links to it posted on other sites they are reading or browsing. These are called referring sites, and there are a total of 563 such sites that currently point to pages on MyOncofertility.org. In addition to directing visitors to a site, having many referring sites – and especially highly ranked ones – are important because this directly impacts how highly search engines rank a site. Being ranked at or near the top of search engine results means that it is much more likely that visitors will find your site when they search for a particular word or phrase (since most of us do not bother scanning past the first page of search results!). The table below lists the top referring sites to MyOncofertility.org. The top referring sites are associated with Northwestern University, a major center for oncofertility research, while others are patient resource sites. Publicity such as a New York Times article has also driven traffic to the site (Table 26.6).
Conclusion
MyOncofertility.org is a patient education resource that addresses an important yet underserved patient community. MyOncofertility.org went through several design iterations as we adapted to feedback and issues in the user community. Furthermore, MyOncofertility.org is a dynamic project that keeps evolving to keep pace with Internet technology and user needs. Our goal in writing this chapter was to share the lessons learned from the MyOncofertility.org development experience with others charged with developing similar patient education resources. We hope that readers will have a much better appreciation for the issues related to patient education, and that the design principles above will serve as useful guidelines for those in a position to design patient education web sites in the future.
Fig. 26.7.
MyOncofertility.org support groups
Acknowledgments
This research was supported by the oncofertility consortium NIH 8UL1DE019587, 5RL1HD058296.
References
- 1.Falvo DR. Effective patient education: a guide to increased compliance. Gaithersburg: Aspen; 1999. [Google Scholar]
- 2.Lewis D. Computer-based patient education: use by diabetes educators. Diabetes Educ. 1996;22(2):140–5. doi: 10.1177/014572179602200207. [DOI] [PubMed] [Google Scholar]
- 3.Lewis D. Computer-based approaches to patient education: a review of the literature. J Am Med Inform Assoc. 1999;6(4):272–82. doi: 10.1136/jamia.1999.0060272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Molloy D, Hall BA, Ilbery M, Irving J, Harrison KL. Oocyte freezing: timely reproductive insurance? Med J Aust. 2009;190(5):247–9. doi: 10.5694/j.1326-5377.2009.tb02385.x. [DOI] [PubMed] [Google Scholar]
- 5.Nakayama K, Ueno NT. American society of clinical oncology recommendations on fertility preservation should be implemented regardless of disease status or previous treatments. J Clin Oncol. 2006;24(33):5334–5. doi: 10.1200/JCO.2006.07.6414. [DOI] [PubMed] [Google Scholar]
- 6.Sonmezer M, Oktay K. Fertility preservation in female patients. Hum Reprod Update. 2004;10(3):251–66. doi: 10.1093/humupd/dmh021. [DOI] [PubMed] [Google Scholar]
- 7.Amory JK. Case 15–2004: cancer therapy and sperm banking. N Engl J Med. 2004;351(5):510. doi: 10.1056/NEJM200407293510521. [DOI] [PubMed] [Google Scholar]
- 8.Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, Wilson C, Munster P. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1(2):146–55. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- 9.Vadaparampil ST, Clayton H, Quinn GP, King LM, Nieder M, Wilson C. Pediatric oncology nurses’ attitudes related to discussing fertility preservation with pediatric cancer patients and their families. J Pediatr Oncol Nurs. 2007;24(5):255–63. doi: 10.1177/1043454207303878. [DOI] [PubMed] [Google Scholar]
- 10.Lee SJ, Schover LR, Partridge AH, Patrizio P,Wallace WH, Hagerty K, Beck LN, Brennan LV, Oktay K. [Accessed October 26, 2009];American Society of Clinical Oncology Recommendations on Fertility Preservation in People Treated for Cancer - ASCO. doi: 10.1200/JCO.2006.06.5888. Available at: http://www.asco.org/guidelines/fertility. [DOI] [PubMed]
- 11.Alpert HR, Emanuel L. Comparing utilization of life-sustaining treatments with patient and public preferences. J Gen Intern Med: official journal of the Society for Research and Education in Primary Care Internal Medicine. 1998;13(3):175. doi: 10.1046/j.1525-1497.1998.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rorty R. Contingency, irony, and solidarity. Cambridge: Cambridge University Press; 1989. [Google Scholar]
- 13.Ogozalek V. The “automated pharmacist”: a comparison of the use of leaflets, text-based computers, and video-based computers to provide medication information to the elderly: a dissertation. Boston: 1991. [Google Scholar]
- 14.Tetzlaff L. Consumer informatics in chronic illness. J Am Med Inform Assoc. 1997;4(4):285–300. doi: 10.1136/jamia.1997.0040285. [DOI] [PMC free article] [PubMed] [Google Scholar]


