Abstract
OBJECTIVE
To prospectively measure the prevalence and effect of symptomatic depression on chronic rhinosinusitis (CRS) patients’ quality of life (QOL), disease-severity, and outcomes of endoscopic sinus surgery (ESS).
STUDY DESIGN
Prospective cohort study
SETTING
Academic, tertiary care center
SUBJECTS AND METHODS
Seventy-six patients with CRS were enrolled prior to ESS and followed post-operatively for a mean of 13.3 months(SD 5.5). Lund-MacKay CT score, Lund-Kennedy endoscopy score, Patient Health Questionnaire-9 (PHQ-9), 2 disease-specific QOL instruments (Rhinosinusitis Disability Index [RSDI] and Chronic Sinusitis Survey [CSS]), and one general QOL instrument (Medical Outcomes Study Short Form-36 [SF-36]) were measured. Differences in outcome scores were analyzed using univariate and multivariate analyses.
RESULTS
Only 7 (9.2%) patients reported a history of depression, but 19 (25.0%) of patients scored in the range of moderate or severe depression on the PHQ-9. Mean (SD) preoperative scores were significantly worse in depressed patients on the RSDI (62.7 [18.2] vs 45.3 [16.3]; p<0.001) and 7 of 8 SF-36 domains (all p ≤ 0.011). Patients with depression significantly improved on both disease-specific QOL instruments (mean change RSDI: 33.5 [24.7], p=0.017; CSS: 25.0 [20.9], p=0.012) and three SF-36 domains (all p≤0.050). Post-operative change scores were not significantly different from patients without depression on the RSDI, CSS, or SF-36. Severity of depression significantly improved postoperatively in depressed patients (preoperative PHQ-9 scores: 13.4 [2.0] vs 6.1 [4.5], p=0.017).
CONCLUSION
CRS patients with depression had worse baseline QOL than other CRS patients, but experienced comparable postoperative improvement in QOL after ESS. Interestingly, depression severity significantly improved after ESS.
Keywords: sinusitis, depression, quality of life, disease-severity, endoscopic sinus surgery, outcomes
INTRODUCTION
Multiple comorbidities have been proposed to modify chronic rhinosinusitis (CRS): one of these is depression.1,2 Major depressive disorder affects 13 to 14 million Americans yearly, is a leading cause of disability in the population between 15 and 44 years old, and is estimated to cost $83 billion annually.3,4 The prevalence of depression has been estimated to be between 5.4% and 8.9% in the general population, but is much more common in patients with chronic disease and has been estimated to be in the range of 14%–36%.5,6 It is a common comorbidity in medical illnesses as diverse as coronary artery disease, congestive heart failure, cerebrovascular disease, diabetes, and cancer.
Depression negatively impacts outcomes of care in chronic disease and has been associated with increased risk of morbidity and mortality.7–10 The data in the CRS literature is much more limited. The prevalence of depression in patients with CRS is estimated to be in the range of 20–25%.11–13 Most studies are limited by self-reported depression status; few use objective screening measures. High levels of depression in patients with CRS have been associated with increased utilization of health care resources including increased antibiotic use, missed workdays, and more physician visits.14
Several authors have reported worse disease-specific quality of life (QOL) in CRS patients with depression, whereas others have reported similar disease-specific symptoms to other patients.1,2,11–13 Some have reported similar outcomes after surgical treatment for depressed and non-depressed patients whereas others report depression as a negative predictor of postoperative QOL outcomes.1,2,11–13 Given the discrepancy between studies, frequent use of self-reported depression in these studies, and intermittent use of prospective data, we set out to examine the role of depression in surgical treatment of patients with CRS in a prospective fashion with objective measures of both depression and outcomes of care.
The specific aims of this study are three-fold. The first aim is to estimate the prevalence of symptomatic depression in patients with CRS presenting for surgery using an objective screening tool for depression and depression disease-severity. The second aim is to compare measures of CRS disease-severity in patients with and without symptomatic depression including computed tomography (CT), endoscopy and QOL. The third aim is to prospectively measure and compare changes in long-term disease-specific and general health-related QOL outcomes after endoscopic sinus surgery (ESS) in patients with and without depression.
MATERIALS AND METHODS
Study Population and Data Collection
All adult (≥18 years) subjects were enrolled prospectively within an academic, tertiary care setting for ambulatory patients presenting with CRS. All subjects met the diagnosis of CRS as defined by the 2007 Adult Sinusitis Guidelines.15 Subjects were enrolled by trained research personnel prior to surgery. Subjects completed standard medical history intake documentation and underwent a physical examination. Demographic data and presence or absence of other clinical characteristics including nasal polyposis, asthma, allergies, aspirin intolerance, and smoking were documented by the physician and confirmed through physical examination when appropriate. Computed tomography and endoscopy findings were recorded. Patients were asked to report a history of depression on the intake form and any anti-depressant medication they were using. Patients also completed the Patient Health Questionnaire-9 (PHQ-9) and QOL surveys at the time of enrollment and all follow-up visits. The Institutional Review Board at Oregon Health & Science University provided approval of study protocol and the informed consent process.
Measurement of Depression
The 9-item Patient Health Questionnaire (PHQ-9) is a validated and reliable self-administered survey which can be used as both a diagnostic tool and measure of depression severity (score range: 0–27).16 The 9 questions are based on criteria from the fourth edition of the Diagnostic and Statistical Manual of Medical Disorders (DSM-IV)17 for major depression. Each question is scored from 0 (not at all) to 3 (nearly every day) and is based on disease severity. A positive test for depression was defined by a PHQ-9 score ≥ 10 in patients; in addition, patients had to report a high score on question 1 or 2 (ie, “little interest or pleasure in doing things” or “feeling down, depressed, or hopeless” more than half the days in the past 2 weeks) and suffer from functional impairment as a consequence of these symptoms. This definition has a sensitivity of 88% and specificity of 88% for major depression.16 Internal reliability is excellent (Cronbach’s alpha 0.86–0.89) while test-retest reliability is also excellent.16 Diagnostic validity of the PHQ-9 was established in 2 studies involving 3,000 patients in two settings and is also sensitive to changes in depression severity over time.18–20 It was administered to each individual at the initial and follow-up visits.
Measurement of CT and Endoscopy
Preoperative CT scans were evaluated and staged in accordance with the Lund-Mackay scoring system (score range, 0–24) where higher scores represented higher severity of disease. 21 Endoscopy exams were scored using the Lund-Kennedy endoscopy scoring system (score range, 0 – 20) where higher scores represented worse disease. 22
Measurement of Disease-Specific and General Health-Related QOL
Subjects were asked to complete 2 brief, validated disease-specific QOL surveys and one general health-related QOL instrument pre- and postoperatively. The Rhinosinusitis Disability Index (RSDI) is a validated disease-specific self-administered survey consisting of 3 domains: physical, functional, emotional (score range, 0 – 120).23 Patients were asked to rate each item on a Likert scale with a higher score representing a higher impact of disease. The RSDI has been found to have high discriminative ability and sufficient reliability (Cronbach’s α = 0.95, r =0.60 – 0.92), is responsive to changes in health status, and predicts rhinitis-specific health outcomes.24,25
The Chronic Sinusitis Survey (CSS) is a validated disease-specific self-administered 6-item monitor of sinus-specific outcomes comprised of 2 subscales: symptom and medication use (score range, 0–100).26 Responses reflect the severity of sinus symptoms and degree of medical therapy for CRS over the previous 8 weeks. Scoring of the CSS involves the use of a transformation such that higher scores represent a lower impact of disease. The CSS is valid, reliable, and responsive (Cronbach’s α = 0.73, r = 0.86).24,26
The Medical Outcome Study Short Form-36 Health Survey (SF-36) is self-administered and used to measure general health-related QOL (score range, 0–100).27 The SF-36 measures patients’ function in eight domains. Scoring involves transformation algorithms with higher scores representing a lower impact of chronic disease. This survey is among the most widely used tools for measuring general health-related QOL; it allows for comparisons between the impact of CRS and other chronic diseases on general health-related QOL. 26,27
Statistical Analyses
All statistical analyses were performed using SPSS v.17.0 statistical software (SPSS Inc., Chicago, IL). Graphical analysis was used to examine normality assumptions and descriptive statistics were calculated for all measures. The proportion of patients who met the criteria for depression was reported. Univariate analyses (t tests, Mann-Whitney U tests) were used to compare mean differences in depressed and non-depressed patients with regard to demographic data, baseline characteristics, CT scores, endoscopy scores, disease-specific and general QOL scores, and change scores based on the underlying distributions of the data. Pearson’s chi-square was used to compare proportions; Fischer’s exact test was used where contingency table cells had less than 5 observations. A multivariate analysis of variance test (Hotelling T) was used to assess global differences in all 8 SF-36 subscale scores between patients with and without depression. A p value ≤ 0.05 was considered statistically significant.
RESULTS
Baseline Characteristics of Study Population
Between August 2007 and December 2008, 76 patients were enrolled in the study. Seventy percent (n=53) were followed for at least 6 months postoperatively, including 8 patients with depression and 45 patients without depression. Mean (SD) follow-up was 13.3 (5.4) months. At enrollment, 7 (9.2%) patients reported a history of depression. However, 19 (25.0%) scored positively for depression using the PHQ-9 criteria. Of patients who scored positively, 5 (26%) were being treated with antidepressant medication. Mean preoperative PHQ scores for patients with depression was 15.1(3.5) and 6.9 (3.7) for patients without depression.
Baseline characteristics of patients with and without PHQ-9-determined depression are reported in Table 1. A smaller proportion of patients with depression had asthma as compared to patients without depression (10.5% vs 42.1%; p=0.013). There was no difference in mean age or the proportion of patients with nasal polyps, allergies, aspirin intolerance, or who smoked.
Table 1.
Baseline Characteristics of Chronic Rhinosinusitis Patients With and Without Depression
| Depressed (n=19) | Not depressed (n=57) | ||||
|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | p value | |
| Age | 46.7 (14.3) | 50.5 (14.3) | 0.232 | ||
| Gender | |||||
| Male | 9 (47.4) | 33 (57.9) | |||
| Female | 10 (52.6) | 24 (42.1) | 0.424 | ||
| Nasal polyps | 7 (36.8) | 30 (52.6) | 0.233 | ||
| Asthma | 2 (10.5) | 24 (42.1) | 0.013* | ||
| Allergy | 4 (21.1) | 14 (24.6) | 0.755 | ||
| Aspirin Intolerance | 2 (10.5) | 8 (14.0) | 0.695 | ||
| Smoking | 1 (5.3) | 4 (7.0) | >0.999 | ||
p≤0.05; SD=standard deviation.
Baseline Disease-Severity as Measured by CT, Endoscopy, and Quality of Life
There was no difference in mean (SD) baseline Lund-Kennedy Endoscopy scores (7.0 [3.1] vs 7.8 [3.9]; p=0.406) or Lund-Mackay CT scores (13.0 [5.6] vs 13.8 [6.5]; p=0.645) in patients with and without depression.
Disease-specific and general health-related QOL scores are reported by depression status in Table 2. Patients with PHQ-9-diagnosed depression scored worse than nondepressed patients on all 3 RSDI subscales and total RSDI score (all p ≤ 0.015). There was no difference between depressed and non-depressed patients for the CSS subscales or total CSS score (p ≥ 0.264). Patients with symptomatic depression scored worse than other patients on 7 of the 8 subscales of the SF-36: bodily pain, mental health, physical function, physical role, emotional role, social function and vitality (all p≤ 0.011). There was no difference in general health scores (p= 0.138).
Table 2.
Preoperative Quality of Life in CRS Patients With and Without Depression
| Depressed | Not depressed | ||
|---|---|---|---|
| Mean (SD) | Mean (SD) | P Value | |
| RSDI Total | 62.7 (18.2) | 45.3 (16.3) | 0.001* |
| Physical Subscale | 24.5 (6.8) | 18.1 (6.8) | 0.002* |
| Functional Subscale | 19.5 (6.7) | 14.9 (6.4) | 0.015* |
| Emotional Subscale | 18.7 (7.6) | 12.3 (6.3) | 0.001* |
| CSS Total | 33.1 (16.2) | 38.3 (19.2) | 0.336 |
| Symptom Subscale | 17.2 (18.8) | 26.9 (26.9) | 0.264 |
| Medication Subscale | 48.9 (24.2) | 49.6 (25.4) | 0.926 |
| SF-36 | |||
| Bodily Pain | 39.3 (20.0) | 61.2 (24.6) | 0.001* |
| Mental Health | 52.3 (16.1) | 69.5 (17.8) | 0.001* |
| Physical Function | 57.0 (21.9) | 73.1 (26.3) | 0.009* |
| Physical Role | 13.3 (22.9) | 41.8 (37.9) | 0.006* |
| Emotional Role | 26.7 (36.1) | 62.1 (39.7) | 0.003* |
| Social Function | 37.5 (17.7) | 62.7 (26.2) | 0.001* |
| General Health | 43.2 (22.2) | 53.9 (24.8) | 0.138 |
| Vitality | 20.7 (14.7) | 38.4 (22.3) | 0.011* |
p≤0.05; SD=standard deviation; RSDI=Rhinosinusitis Disability Index score; CSS=Chronic Sinusitis Survey score; SF-36=Medical Outcomes Study Short Form-36 score.
Post-Operative Change in Depression Severity and QOL
In depressed patients with pre- and postoperative scores, the severity of depression significantly improved from a preoperative PHQ-9 score of 13.4(2.0) to a postoperative PHQ-9 score of 6.1(4.5) (p=0.017).
Postoperative change scores for disease-specific and general-health related QOL are reported in Table 3. Patients with depression experienced significant improvement on the total RSDI and all 3 RSDI subscales (all p≤0.036). Patients with depression experienced significant improvement on the total CSS (p=0.012) and CSS medication subscale (p=0.046) and trended towards improvement on the CSS symptom subscale (p = 0.058). Patients without depression experienced significant improvement across all domains of the RSDI (all p< 0.001) and CSS (all p ≤ 0.003). Mean changes in disease-specific QOL scores in depressed patients were not significantly different from the change scores in non-depressed patients (p ≥ 0.223).
Table 3.
Absolute Change in Disease-Specific and General Health-Related Quality-of-Life After ESS
| Depressed | Not depressed | Between Groups | |||
|---|---|---|---|---|---|
| Mean (SD) | P value | Mean (SD) | P value | P value | |
| RSDI Total | 33.5 (24.7) | 0.017* | 22.0 (17.4) | <0.001* | 0.223 |
| Physical | 13.3 (10.5) | 0.018* | 9.0 (8.4) | <0.001* | 0.311 |
| Functional | 11.4 (7.5) | 0.021* | 7.8 (6.9) | <0.001* | 0.147 |
| Emotional | 8.9 (9.6) | 0.036* | 5.2 (6.2) | <0.001* | 0.389 |
| CSS Total | 25.0 (20.9) | 0.012* | 28.7 (25.0) | <0.001* | 0.493 |
| Symptom | 30.2 (39.3) | 0.058 | 42.2 (35.5) | <0.001* | 0.335 |
| Medication | 19.8 (21.3) | 0.046* | 15.2 (30.8) | 0.003* | 0.610 |
| SF-36 | |||||
| Bodily Pain | 23.3 (26.8) | 0.050* | 11.8 (19.2) | <0.001* | 0.187 |
| Mental Health | 10.9 (14.7) | 0.104 | 6.4 (14.5) | 0.005* | 0.546 |
| Physical Function | 19.4 (39.2) | 0.123 | 8.5 (16.6) | 0.001* | 0.162 |
| Physical Role | 53.1 (36.4) | 0.017* | 26.1 (34.9) | <0.001* | 0.085 |
| Emotional Role | 29.2 (37.5) | 0.068 | 18.2 (28.3) | <0.001* | 0.446 |
| Social Function | 23.4 (23.6) | 0.034* | 16.8 (31.3) | 0.002* | 0.541 |
| General Health | 12.5 (22.1) | 0.205 | 6.6 (17.3) | 0.019* | 0.558 |
| Vitality | 20.7 (41.9) | 0.204 | 13.6 (24.2) | 0.001* | 0.698 |
p≤0.05; SD=standard deviation; RSDI=Rhinosinusitis Disability Index score; CSS=Chronic Sinusitis Survey score; SF-36=Medical Outcomes Study Short Form-36 score.
Depressed patients experienced statistically significant postoperative improvement in 3 SF-36 domains: physical role (53.1 [36.4], p=0.017), social function (23.4 [23.6], p=0.034), and bodily pain (23.3 [26.8], p=0.050). There was a trend towards improvement in the emotional role subscale (29.2 [37.5], p=0.068). Patients without depression experienced statistically significant improvement in all 8 SF-36 domains (all p ≤ 0.019).
Despite these differences, mean change scores in all SF-36 subscales in depressed patients (range, 10.9–53.1) were not significantly different than change scores from patients without depression (range, 6.4–26.1; all p ≥ 0.085). There was no global difference in SF-36 change scores between patients with and without depression (t=0.121; p=0.742).
DISCUSSION
In this prospective cohort study, depression was present in 25% of patients with CRS presenting for surgical treatment. Although preoperative CT and endoscopy scores were not different, patients with depression experienced significantly worse baseline disease-specific and general health-related QOL as measured by the RSDI and SF-36, respectively. Despite these baseline differences, patients with depression reported statistically significant improvement in disease-specific and general health-related QOL. In addition, change scores in disease-specific and general health-related QOL were comparable to patients without depression (ie, patients with depression experienced just as much improvement following ESS).
Depression appears to be a common problem in patients with CRS. While no exact estimates exist based on objective criteria in population-based studies, our findings are consistent with other reports in the CRS literature. Brandsted and Sindwani12 reported a prevalence of 25% in patients with CRS based on self-report and use of antidepressant medications. Davis et al11 also reported an estimated 25% prevalence of depressive disorders based on the PHQ-9. We previously reported a prevalence of 22.5% based on self-report in a different study population. 13 These estimates are greater than the general population and are akin to the prevalence of depression reported in other chronic medical conditions.
Data suggests that depression in patients with CRS negatively impacts patients’ symptom burden, ability to function, and QOL. In our study, patients with depression experienced worse disease-specific and general-health related QOL, even when other measures of disease-severity, including CT and endoscopy, were similar. Others have reported increased pain, increased oropharyngeal and total CRS symptoms, worse energy level, difficulty with daily activities, and occupational impairment.12,14
The role of depression in the outcomes of surgical care for patients with CRS is more controversial. In a retrospective case-control study of 17 depressed and 23 nondepressed patients, Brandsted and Sindwani12 reported that depressed patients did not experience improvement in disease-specific symptoms after surgery as compared to other patients without depression. In a prospective study of 95 patients, Davis et al11 found that patients with elevated psychiatric distress had worse preoperative and postoperative QOL scores but similar change 12 months after surgery. In another prospective study, Smith et al1 found that depression was associated with less improvement in disease-specific QOL after ESS. Of note, these data were adjusted for baseline health-related QOL which is often used to improve efficiency, control confounding, and avoid floor and ceiling effects. However, controlling for baseline health-related QOL may also bias regression coefficient estimates if baseline function and depression are strongly associated. We further examined this issue and reported that baseline adjustment of depression may in fact have overcontrolled the variable of interest.13 When baseline depression was not adjusted for, depressed patients reported worse QOL preoperatively and postoperatively, but experienced similar amounts of change in disease-specific QOL. More recently, we examined depression in a multi-institutional study and found that it did not predict post-operative QOL, but again, this depended on self-report which can under- or overestimate the actual prevalence.2
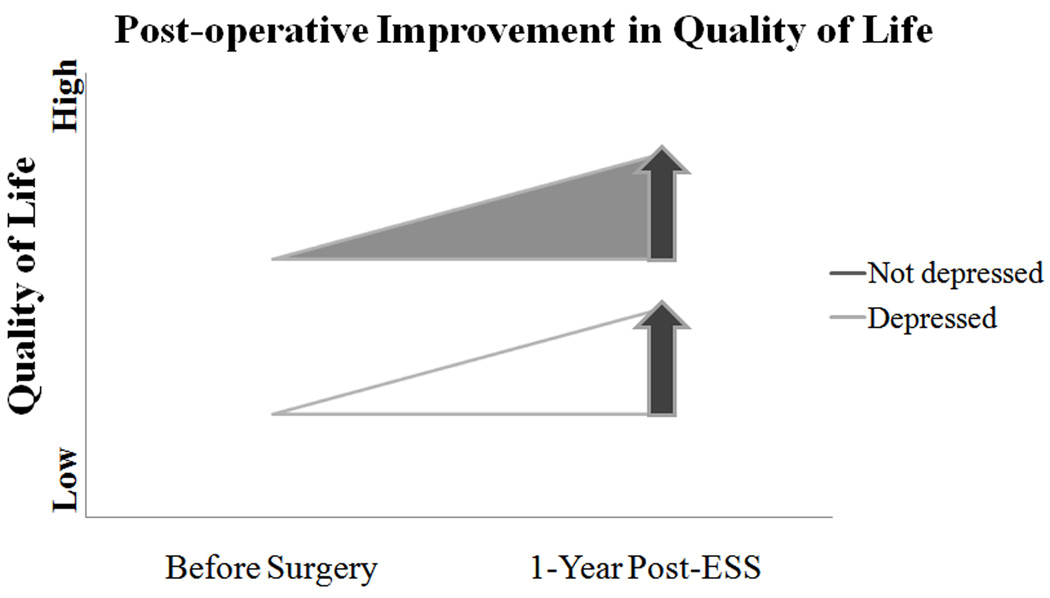
To address the limitations associated with self-reported depression, patients completed screening with an objective depression screening instrument. Patients with depression presented with worse disease-specific and general health-related QOL before surgery but experienced similar degrees of improvement postoperatively. Several of these change scores were statistically significant. Some of these postoperative change scores were not statistically significant, but were clinically significant and comparable to other patients in the cohort; this discrepancy is likely due to the smaller sample size of depressed patients with long-term follow-up. Clinicians can find it frustrating to treat a subgroup of patients with depression that report lower QOL after surgery than others in their practice. In fact, depressed patients improved after surgery and this improvement was comparable to other patients (Figure 1). In a sense, clinicians may need to redefine their internal expectations when treating patients with depression who may be more symptomatic than others but, when asked, still experience significant improvement following treatment.
Figure 1.
Although both patients with and without depression experience similar improvement in QOL after sinus surgery, they do so from different baselines. ESS, endoscopic sinus surgery.
It is important to note that symptomatic depression was determined by an objective screening tool, the PHQ-9, rather than a complete psychiatric evaluation. The PHQ-9 was chosen because it is valid, reliable, sensitive to change and easy to use. It has a high sensitivity and specificity for major depression. It does not replace a comprehensive psychiatric evaluation but serves as a practical tool to use within the limitations of a busy clinical practice. It also provides an element of objectivity to an often self-reported diagnosis in the clinic. Studies that do not use an objective measure of depression are susceptible to misclassification bias. In addition, we were most interested in identifying patients with symptomatic depression. Some patients had a prior diagnosis of clinical depression, had been successfully treated, and acted more like patients without a diagnosis of clinical depression. Conversely, there were patients who screened positively for depression that had not been previously diagnosed or treated for various reasons and yet were symptomatic. To address the issue of most interest to us, we chose to identify patients with symptomatic depression, diagnosed or undiagnosed.
Data was collected at a single institution and a tertiary care referral center; data may not necessarily be generalizable to all patients with sinusitis and depression. However, data from other research suggests that this issue is also pertinent to those practicing in the community.11 Finally, long-term follow up of patients in a prospective fashion can be challenging and expensive, particularly in depressed patients. This questionnaire was presented prior to surgery and each follow up visit after surgery. Patients were lost to follow-up for multiple reasons including moving, changes in insurance, and long distance travel in which case some patients chose to have follow-up closer to home. To address potential biases with follow-up, baseline characteristics in patients with and without long-term follow-up were analyzed; no major differences were noted. To account for the lack of statistically significant improvement in postoperative scores across some domains, prospective studies with larger sample sizes of depressed patients are warranted.
One interesting finding of this study was that the severity of depression as measured by the PHQ-9 lessened after sinus surgery. We do not suggest that surgery improves depression. This may represent an incidental finding in preliminary data, but is worth further investigation as there appears to be a complex interplay between depression and chronic disease in much of the literature.
CONCLUSION
In summary, depression is common and underreported in patients with CRS. Depression significantly impacts patients’ QOL. Depressed patients with CRS report worse disease-specific and general health-related QOL than other CRS patients, but experience comparable postoperative improvement in QOL after ESS. Perhaps with better diagnosis and treatment of depression in this subset of patients, their outcomes of care can be further improved.
Acknowledgments
FUNDING SUPPORT:
Dr. Litvack was supported by a T32 NIH Training Grant at Oregon Health & Science University during this study (T32 DC5945). Partial funding was supported for this project by the American Academy of Otolaryngology-Head & Neck Surgery Foundation Health Service Research Grant, 2008–09. Dr. Smith and Mr. Mace were grant funded by the NIH/NIDCD R01 DC005805 (PI: TL Smith).
Footnotes
PRESENTATION OF DATA: Preliminary analyses of these data were presented orally at the Annual American Academy of Otolaryngology-Head & Neck Surgery Foundation Meeting, San Diego, CA, October 7, 2009. The final results were presented orally at the Annual American Academy of Otolaryngology-Head & Neck Surgery Foundation Meeting, Boston, MA, September 29, 2010.
REFERENCES
- 1.Smith TL, Mendolia-Loffredo S, Loehrl T, et al. Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope. 2005;115:2199–2205. doi: 10.1097/01.mlg.0000182825.82910.80. [DOI] [PubMed] [Google Scholar]
- 2.Smith TL, Litvack JR, Hwang PH, et al. Determinants of outcomes of sinus surgery: A multi-institutional prospective cohort study. Otolaryngol Head Neck Surg. 2010;142:55–63. doi: 10.1016/j.otohns.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Berflund P, Demler O, et al. The epidemiology of major depressive disorder. Results from the national comorbidity replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 4.Greenberg PE, Kessler RC, Birnbaum HG, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 5.Mann JJ. Drug Therapy: The Medical Management of Depression. NEJM. 2005;353(17):1819–1834. doi: 10.1056/NEJMra050730. [DOI] [PubMed] [Google Scholar]
- 6.Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J of Cardiac Failure. 2005;11:455–463. doi: 10.1016/j.cardfail.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 7.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction: Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 8.Frasure-Smith N, Lesperance F, Talajic M. Depression and 18-month prognosis after myocardial infarction. Circulation. 1995;91:999–1005. doi: 10.1161/01.cir.91.4.999. [DOI] [PubMed] [Google Scholar]
- 9.Murberg TA, Bru E, Svebak S, et al. Depressed mood and subjective health symptoms as predictors of mortality in patients with congestive heart failure: A two-year follow-up study. International J Psych Med. 1999;29:311–326. doi: 10.2190/0C1C-A63U-V5XQ-1DAL. [DOI] [PubMed] [Google Scholar]
- 10.May M, McCarron P, Stansfeld S, et al. Does psychological distress predict the risk of ischemic stroke and transient ischemic attack? The Caerphilly Study. Stroke. 2002;33:7–12. doi: 10.1161/hs0102.100529. [DOI] [PubMed] [Google Scholar]
- 11.Davis GE, Yueh B, Walker E, et al. Psychiatric distress amplifies symptoms after surgery for chronic rhinosinusitis. Otolaryngol Head Neck Surg. 2005;132:189–196. doi: 10.1016/j.otohns.2004.09.135. [DOI] [PubMed] [Google Scholar]
- 12.Brandsted R, Sindwani R. Impact of depression on disease-specific symptoms and quality of life in patients with chronic rhinosinusitis. Am J Rhinol. 2007;21:50–54. doi: 10.2500/ajr.2007.21.2987. [DOI] [PubMed] [Google Scholar]
- 13.Mace J, Michael YL, Carlson NE, et al. Effects of depression on quality of life after sinus surgery. Laryngoscope. 2008;118:528–534. doi: 10.1097/MLG.0b013e31815d74bb. [DOI] [PubMed] [Google Scholar]
- 14.Wasan A, Fernandez E, Jamison R, Bhattacharyya N. Association of Anxiety and Depression With Reported Disease Severity in Patients Undergoing Evaluation for Chronic Rhinosinusitis. Ann Otol Rhinol Laryngol. 2007;116(7):491–497. doi: 10.1177/000348940711600703. [DOI] [PubMed] [Google Scholar]
- 15.Rosenfeld RM, Andes D, Bhattacharyya N, et al. Clinical practice guideline: Adult sinusitis. Otolaryngol Head Neck Surg. 2007;137:S1–S31. doi: 10.1016/j.otohns.2007.06.726. [DOI] [PubMed] [Google Scholar]
- 16.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Medical Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 18.Spitzer RL, Kroenke K, Williams JBW Patient Health Questionnaire Study Group. Validation and Utility of Self-report Version of PRIME-MD. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL, Williams JBW, Kroenke K, et al. Validity and utility of the Patient Health Questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 20.Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9) J Affect Dis. 2004;81(1):61–66. doi: 10.1016/S0165-0327(03)00198-8. [DOI] [PubMed] [Google Scholar]
- 21.Lund VJ, Mackay IS. Staging in rhinosinusitis. Rhinology. 1993;107:183–184. [PubMed] [Google Scholar]
- 22.Lund VJ, Kennedy DW. Quantification for staging sinusitis. Ann Otol Rhinol Laryngol. 1995;104:17–21. [PubMed] [Google Scholar]
- 23.Benninger MS, Senior BA. The development of the rhinosinusitis disability index. Arch Otolaryngol Head Neck Surg. 1997;123:1175–1179. doi: 10.1001/archotol.1997.01900110025004. [DOI] [PubMed] [Google Scholar]
- 24.Linder JA, Singer DE, van den Ancker M, Atlas SJ. Measures of Health-related Quality of Life for Adults with Acute Sinusitis: A Systematic Review. J Gen Intern Med. 2003;18:390–401. doi: 10.1046/j.1525-1497.2003.20744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen H, Katz PP, Eisner MD, et al. Health-related quality of life in adult rhinitis: the role of perceived control of disease. J Allergy Clin Immunol. 2004;114(4):845–850. doi: 10.1016/j.jaci.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 26.Gliklich RE, Metson R. The health impact of chronic sinusitis in patients seeking otolaryngologic care. Otolaryngol Head Neck Surg. 1995;113:104–109. doi: 10.1016/S0194-59989570152-4. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]