Abstract
Background
Adolescent idiopathic scoliosis (AIS) is a common disorder in which the spine gradually develops a curvature that is first detected between 11 and 17 years of age. The only accepted treatment methods are bracing and surgery. Whether brace treatment alters the natural history is being questioned, and patient compliance is low. Surgery usually includes a spinal fusion that creates a rigid spine and concentrates stresses at the ends.
Methods
This study focuses on correlating the laboratory results with clinical reports for treating patients with AIS. In the laboratory, scoliosis with vertebral wedging has been created by asymmetric mechanical loading and has been corrected by reversing the loading. In the clinic, bracing and derotational casting have been successful in some reports, but compliance has been a problem with bracing and derotational casts have mainly been used in young children. Operative treatment has been successful, but a nonfusion operation remains elusive.
Findings and Results
In the laboratory, axial loading of growth plates altered growth according to the Hueter-Volkmann law, which states that compression decreases and distraction increases growth. Asymmetric loading of the spine caused asymmetric growth resulting in scoliosis with vertebral wedging. Asymmetric loading of tail vertebrae has created vertebral wedging according to Wolff’s law, which states that bone remodels over time in response to prevailing mechanical demands. In the clinic, studies have shown that bracing may work if patients wore the brace as prescribed. Derotational casting in young children has been shown to prevent progression and even correct the scoliosis in some patients. Convex vertebral stapling has been successful in mild curves, but the results in larger curves have been disappointing. Anterolateral tethering has been successful in mild curves in young patients, but there is limited experience with this technique in patients with large curves.
Conclusions
A brace that applies the appropriate loading and is worn as prescribed may dramatically improve the results of brace treatment. A procedure using external fixation or adjustable anterolateral tethering may achieve a nonfusion correction of AIS.
Keywords: Scoliosis, Growth modulation, Vertebral remodeling, Brace treatment for scoliosis, Operative treatment for scoliosis
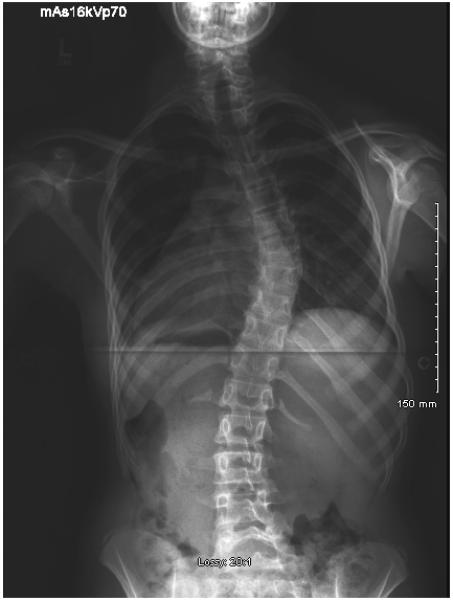
Adolescent idiopathic scoliosis (AIS) is a common disorder of unknown etiology in which the vertebrae and discs gradually develop a curvature that is first detected between 11 and 17 years of age. The deformity is three-dimensional, with a coronal curve measured from radiographs by the Cobb angle, a sagittal curve (usually hypokyphosis) measured by the lateral Cobb angle, and axial rotation measured with the torsion meter developed by René Perdriollle (1). The Cobb angle measurement of scoliosis represents the sum of the angular wedging of each vertebra and disc between the superior and inferior end vertebrae (2). Although a small curve is well tolerated and does not require treatment, a large curve can progress to the point that it is cosmetically unacceptable, interferes with chest wall mechanics, and produces cardiac and pulmonary compromise.
The natural history of AIS apparently includes two stages: the initiation of the curve and its subsequent progression. The factors responsible for the initiation of the curve are unknown, but the subsequent progression of the curve is clearly associated with the adolescent growth spurt (3). The primary risk factors for progression include age at onset and the magnitude of the curve; young patients with large curves are at the highest risk (4). Another risk factor for progression that is currently being investigated is genetic predisposition.
Although numerous treatment methods have been recommended for patients with AIS, the only accepted treatment includes bracing for skeletally immature patients with curves between 25° and 40° and operative correction with spinal fusion for patients with curves greater than 45°. For many teenagers, the cosmetic and social concerns associated with bracing has caused compliance problems with wearing the brace and many patients only wear the brace at home (5). Operative instrumentation and fusion creates a rigid spine, does not completely correct the scoliosis or rib hump, eliminates segmental spinal motion, and concentrates stresses at the ends of the fusion potentially leading to disc degeneration and back pain (Fig. 1). Despite satisfactory short-term results of operative instrumentation and fusion, a minimally invasive technique creating growth modulation and remodeling while preserving vertebral and disc motion and overall growth would be a major improvement. Realizing this goal will be contingent on treating curves early, before they progress to an irreversible deformity, and when there is still enough residual growth and remodeling potential.
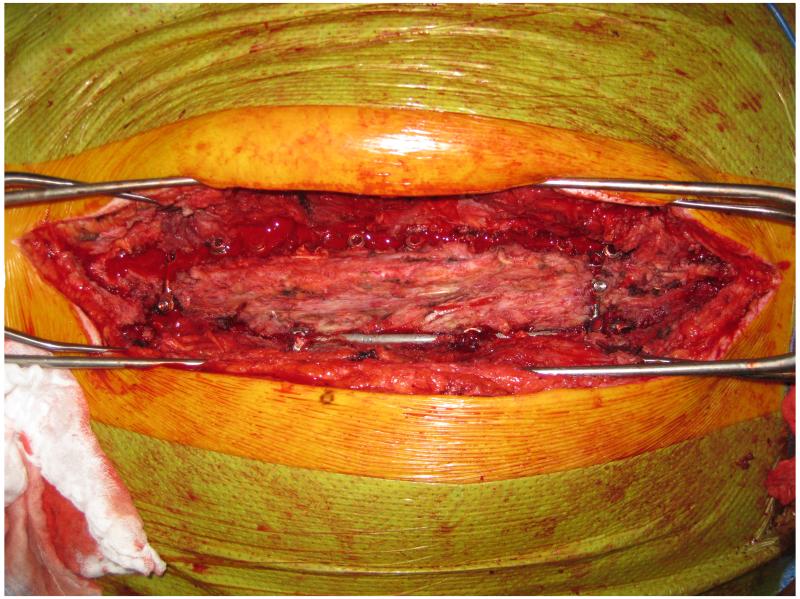
Figure 1.
Operative photograph taken six years after a posterior spinal fusion showing a rigid spine without any segmental motion that transfers stresses to the discs at the ends of the fusion.
The purpose of this study is to review the basic science principles of growth modulation and remodeling and analyze how these principles have been applied in the laboratory to alter spinal growth and correct scoliosis. Several investigators have adopted these principles to treat AIS patients using new techniques designed to achieve motion sparing growth modulation without a spinal fusion. The laboratory reports will be compared with these preliminary clinical reports to determine the status of motion sparing nonfusion growth modulation and remodeling for the treatment for AIS and discuss future innovations.
METHODS
Basic science methods to modulate vertebral growth and remodeling
The rapid progression of scoliosis during the adolescent growth spurt is thought to be secondary to asymmetric growth, with decreased growth on the concave side (6). Vertebral wedging during growth is attributed to the Hueter-Volkmann law of mechanically modulated endochondral growth (7, (8). A spine with scoliosis evidently has greater loading on the concave side and this asymmetric loading with compression on the concave side causes asymmetric growth, creating vertebral wedging, and leading to the “vicious cycle” of scoliosis progression (9, (10). Consequently, if the load asymmetry could be reversed, the “vicious cycle” would be reversed, and the scoliosis curve corrected.
Laboratory studies using several different animal species have applied axial compression and distraction as well as asymmetric compression to mechanically modulate growth according to the principles of the Hueter-Volkmann law. These studies have documented that static compression and distraction stress of 0.1 MPa have a dramatic effect on longitudinal endochondral growth with distraction increasing and compression decreasing growth. There also appears to be a linear dose-response relationship with increased compression or distraction having an increased effect. The key question raised by these reports is what magnitude of loading is required to achieve the desired growth modulation without causing a growth arrest or fracture. To quantify the Hueter-Volkmann effect, growth rates were compared using two different compression and distraction loads in two anatomic locations (tibia and vertebra) in rats, rabbits, and calves at two different ages (11). There was no difference in the growth modulation between species or by age although faster growing tibiae were slightly more sensitive than vertebrae to the same stress. The growth-rate sensitivity to stress averaged 17% per 0.1 MPa. The histological changes in a growth plate subjected to static compression and distraction have been identified as primarily an alteration in the amount of chondrocytic hypertrophy, but the mediators behind these changes are still under investigation.
Although theoretically more physiologic than static loading, the effect of dynamic loading on growth is unclear. One study reported decreased growth with dynamic loading (12), whereas another found no change in animals subjected to different activity levels (13). In a lamb model, 90% of proximal tibia growth occurred during periods of recumbency when the growth plate was not subjected to dynamic loading (14). The growth plate behaves viscoelastically, losing volume under sustained loading, but subsequently recovering its dimensions when unloaded (15). These changes in volume are more concentrated in the proliferative and hypertrophic zones as these zones are three times more permeable than the reserve zone (16) .
Although the progression of AIS during the adolescent growth spurt is thought to be secondary to asymmetric growth, vertebral diaphyseal remodeling governed by Wolff’s law may also contribute to the progression. Wolff’s law states that bone tissue remodels over time in response to prevailing mechanical demands; decreased physical activity leads to osteoporosis and conversely, increased physical activity leads to increased bone density.
Clinical methods to modulate growth and remodeling and treat AIS
Nonoperative treatment includes chiropractic spinal adjustment, osteopathic treatment on trunk morphology, physical therapy, crainosacral therapy, other alternative medicine modalities, and bracing. Although numerous treatment modalities are recommended, bracing is the only method that has been shown to be effective. Despite reports documenting the benefits of bracing, some investigators believe that the evidence supporting bracing is of low quality and question whether bracing alters the natural history of AIS (17) .
Operative treatment is recommended for patients with curves greater than 45°. The procedure includes either an anterior approach, a posterior approach, or combined anterior and posterior approaches with segmental fixation using hooks, wires, and screws anchored to individual vertebrae and attached to longitudinal rods to correct the scoliosis followed by a spinal fusion using bone graft. Anterior thoracoscopic segmental instrumentation and fusion has evolved and advocates of this approach report satisfactory correction of the scoliosis with limited muscular dissection and cosmetically improved scar appearance (18). Posterior segmental instrumentation with fusion has also evolved with the advent of pedicle screw fixation and advocates of this approach report true segmental control and greater correction in the coronal and sagittal planes (19). The risks of pseudarthrosis, instrumentation failure, and surgical revision reported with the anterior approach have caused many surgeons to retain the posterior approach, despite the inherent risks of placing pedicle screws. Following operative correction of the curve, a spinal fusion is performed by decorticating the spine and adding bone graft. Bone graft may come from the iliac crest, locally from the spinous and transverse processes, allograft from the bone bank, and recently some investigators have used bone graft substitutes to avoid the problems associated with harvesting the iliac crest and the potential transmission of disease from allograft bone.
FINDINGS AND RESULTS
Basic science studies on growth modulation and remodeling
The “vicious cycle” hypothesis proposes that asymmetric loading with compression on the concave side causes asymmetric growth, creating vertebral wedging, that results in progression of the curve, aggravating the scoliosis. This hypothesis was tested in a rat tail model with an Ilizarov-type external fixator applied to the tail vertebrae imposing a 30° scoliosis and axial compression. The vertebrae gradually developed a vertebral wedge deformity which was reported to be secondary to asymmetric growth (6). In a follow up report, the reversibility of the vertebral wedge deformity was studied by first creating a scoliosis with vertebral wedging using the same Ilizarov-type fixator and then reversing the loading in one group of animals and removing the loading in a second group (20). The results showed that the vertebral wedging was completely corrected when the loading was reversed and only 36% corrected when the loading was simply removed. These laboratory studies strongly suggest that AIS can be corrected if the appropriate loading can be applied to the growing vertebrae.
The growth modulation created by sustained compression or distraction is directly associated with histological changes in the growth plate (21). Compression loading causes a decrease in the chondrocyte proliferative rate, chondrocyte cell height, and height of zone of hypertrophy, whereas distraction loading causes an increase in these parameters (22). Although these histological changes associated with modulation of growth are well documented, the mechanism that causes these changes remains unknown.
A recent study, including immature and mature animals, evaluated the etiology of vertebral wedging in a rat tail model using an external fixator to impose a 30° scoliosis and compression (23). Serial CT scans and fluorochrome bone labeling measured the contribution of epiphyseal remodeling, asymmetric growth, and diaphyseal remodeling to the vertebral wedging. All of the animals developed scoliosis with vertebral wedging that was caused by a combination of epiphyseal remodeling, asymmetric growth, and diaphyseal remodeling (Fig. 2A). The major contribution to the vertebral wedging was asymmetrical growth in the immature animals and diaphyseal remodeling in the mature animals. The diaphyseal remodeling was accompanied by a corresponding drift of the vertebral cortices toward the concave side with considerable new bone formation of the concave side (Fig. 2B). The diaphyseal new bone formation on the concave side reflected Wolff’s law where the compressed bone responded with remodeling and thickening of the cortex on that side. These results suggest that if appropriate loads can be applied to human vertebrae, scoliosis with vertebral wedging can be corrected without a spinal fusion in both adolescents and adults.
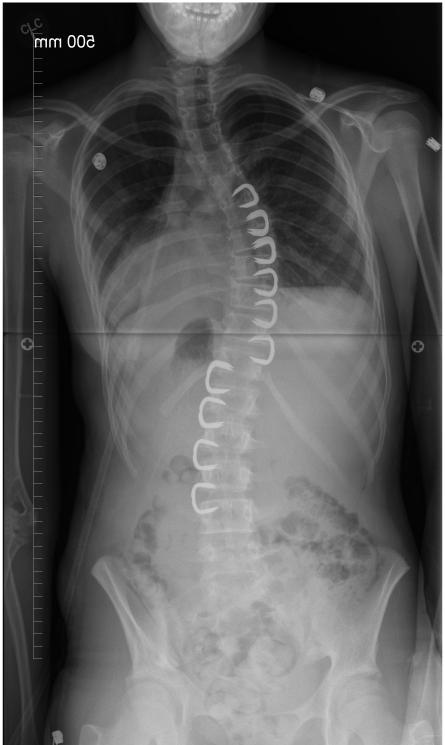
Figure 2.
A, Serial CT scans of a rat tail treated with an external fixator imposing a 30° scoliosis and compression. Weeks 3 and 6 (arrow) show a progressive wedge deformity developing in the apical vertebra. B, Fluorochrome labeling showing increased growth on the convex side (vertical arrow) and diaphyseal remodeling on the concave side with new bone formation (horizontal arrow).
Studies have demonstrated that full-time static loading in compression and distraction modulates growth, with compression decreasing and distraction increasing longitudinal growth. If this is true, what is the effect of part-time loading? Since some investigators believe that the majority of growth occurs at night, would nighttime loading have the same effect as full-time loading? To answer these questions, a rat tail model was used to determine the effect of compression loading on vertebral growth. It was found that full-time loading (24 hours a day) had twice the effect of part-time loading (12 hours a day) (24). Part-time loading had the same effect regardless of whether it was applied during daytime or nighttime hours. The findings of this laboratory study cast serious doubt on the value of part-time compared with full-time bracing for the treatment of AIS.
The concept of placing vertebral staples on the convex side of the scoliosis in an immature patient seemed intriguing as the staples should arrest convex growth while allowing normal concave growth to continue and gradually correct the scoliosis. This technique was used in a pig model to create a thoracic scoliosis (25). The authors reported that the height of the zone of hypertrophy, the chondrocyte cell height, and cell width were all decreased on the stapled side compared to the contralateral side and to control vertebrae. In another study involving goats, the authors created a convex right scoliosis using a posterior asymmetric flexible tether with convex rib resection and concave rib tethering (26). After the scoliosis was created, the tether was removed and the authors treated one group with four convex shape memory alloy staples and the control group had no treatment. The results showed an average scoliosis correction from 56.8° to 43.4° (24%) in the stapled group and from 67° to 59.8° (11%) in the control group. The apical spinal segment wedging showed an average decrease from 22.5° to 20.3° (10%) in the stapled group and an average increase from 22.3° to 25.8° (16%) in the control group.
Similarly, the idea of placing an anterolateral vertebral tether to decrease growth on the anterolateral convex side of the scoliosis seemed interesting because the tether should correct the scoliosis by decreasing growth on the convex side while allowing normal growth on the concave side. In addition, the tether should also correct the hypokyphosis by decreasing anterior growth while allowing normal posterior growth. In a recent study using an anterolateral tether to create scoliosis in a pig model, the authors placed four anterolateral screws into adjacent thoracic vertebrae and connected them by a polyethylene tether (27). After one year, an average scoliosis of 30° was created with associated vertebral wedging. In another study using a goat model, the authors created a scoliosis deformity by a combination of convex rib resection and concave rib tethering followed by tensioning a posterior asymmetric tether (28). The goats were then treated with lateral tethering, shape memory alloy stapling, or no treatment. The authors reported that the mean scoliosis decreased from 73° to 69.9°in the lateral tethering group, but increased from 77.3° to 94.3° in the shape memory alloy stapling group, and increased from 79.5° to 96.8° in the control group. The authors concluded that the lateral tethering corrected scoliosis modestly in the coronal plane, but they did not observe correction in the sagittal or transverse planes.
Clinical nonoperative treatment to modulate vertebral growth and remodeling
Brace treatment of AIS acts passively by directly applying forces to the trunk, and actively by altering trunk muscle activation and hence the reaction forces applied to the spine. The Milwaukee brace was designed to create a constant corrective molding force to the trunk and spine during growth to prevent progression of AIS (29). The early results were encouraging and advocates followed Blount’s advice recommending bracing for 23 hours per day. In reviewing the results of bracing, it became clear that many patients were not wearing the brace 23 hours per day. A prospective study of patients with AIS treated with part-time bracing (16 hours per day) reported that, although the average in-brace correction was less than full-time bracing, only 11% had progression of the curve (5). Another study comparing full-time bracing with part-time bracing reported no significant difference in progression of the AIS (30) .
In contrast to these reports on part-time bracing, a recent prospective study evaluating the efficacy of bracing for AIS patients used a Boston brace equipped with a heat sensor that measured the exact number of hours the brace was worn (31). The authors reported that the total number of hours of brace wear correlated with the lack of curve progression. In other words, the more the brace was worn the better the result. The authors also reported that compliance with prescribed brace wear was 35% in the 16-hour group, and 27% in the 23-hour group. More importantly, curves did not progress in 82% of patients who wore the brace more than twelve hours per day, compared with only 31% of those who wore the brace fewer than seven hours per day.
Even though a brace may prevent curve progression if worn as prescribed, patient acceptance of the brace is a major problem with brace treatment. For this reason, the SpineCor System, a non-rigid orthosis, was developed to apply a dynamic force to the spine while being more comfortable and less hot for the patient (32). Although advocates promote the flexibility of the SpineCor System, a recent study reported that the SpineCor had a higher failure rate than a rigid orthosis (33). Another study reported that patient acceptance and quality of life were similar, with the rigid brace causing more problems with heat, and the SpineCor brace causing more problems with toileting (17) .
Although brace treatment can be successful, the negative psychosocial impact and physical constraints of bracing has caused many patients and families to seek holistic and less harmful approaches in the field of complementary and alternative medicine. Osteopathy, a holistic method, highlights the musculoskeletal system as the origin of health and promotes the integration of body, mind, and spirit. A prospective, randomly, controlled trial girls with AIS reported no evidence to support osteopathy for the treatment of AIS (34) .
Serial derotational casting for progressive early onset scoliosis applies a corrective force to create asymmetric growth and remodeling. A study involving patients with progressive early onset scoliosis treated by serial derotational casting under anesthesia reported that 89% responded to cast correction (35). In children less than 20 months old with curves less than 60° the authors reported that complete correction of the scoliosis was frequently achieved. Thus, serial derotational casting is applying the necessary loading to modulate growth and remodeling in these young children. If further studies confirm these dramatic results, derotational casting may be revisited for patients with AIS.
Clinical operative treatment to modulate vertebral growth and remodeling
Convex anterior and posterior hemiepiphysiodesis in children with progressive congenital scoliosis evolved slowly because of several setbacks. Some surgeons only performed the fusion posteriorly, while others performed it when the patients were mature, and others only included the apex instead of the entire curve. A study involving ten children with progressive congenital scoliosis treated by a combined anterior and posterior hemiepiphysiodesis reported that the scoliosis was halted in all cases and two patients showed evidence of spontaneous improvement (36). A concern with this procedure is that growth on the concave side is decreased by congenital scoliosis.
Expandable spinal implants “growing rods” were developed to control the scoliosis and allow for continued growth until the child reaches the age when a spinal fusion can be performed. The original technique involved the placement of a single subcutaneous Harrington rod without fusion except at the hook sites. The patient wore a postoperative brace and the rod was then periodically distracted. Despite postoperative bracing, complications were frequent including broken rods and hook dislodgement. The surgical technique improved with the implementation of claw and pedicle screw constructs. A recent study reported a mean scoliosis correction of 71% using dual growing rods without an apical fusion that were lengthened every six months (37) .
The Vertical Expandable Prosthetic Titanium Rib (VEPTR) and expansion thoracostomy technique was developed for the treatment of thoracic insufficiency syndrome associated with congenital scoliosis and fused ribs (38). The surgery included opening wedge thoracostomies to separate fused ribs and distraction of the most constricted portion of the chest using rib-to-rib or rib-to-spine devices. The devices are then lengthened approximately every 6 months. The VEPTR results demonstrated increased spinal growth, improvement in scoliosis, decreased ventilator dependence, and increased lung volume and function.
Vertebral staples were designed to span the disc and growth plates of two adjacent vertebrae and to tether growth on the convex side of the scoliosis while allowing normal growth to continue on the concave side. Unfortunately, the early clinical experience with stapling was disappointing with limited correction, broken staples, and staple dislodgement. To address staple dislodgement, Medtronic Sofamor Danek (Memphis, TN) designed a staple using Nitinol, a shape memory alloy, where the prongs are straight when cooled, but clamp down into the bone in a C-shape when subjected to body temperature (Fig. 3). A study evaluating Nitinol staples reported that none of the patients with preoperative curves with Cobb angles less than 30° progressed, whereas 18% of preoperative curves greater than or equal to 30° progressed (39) .
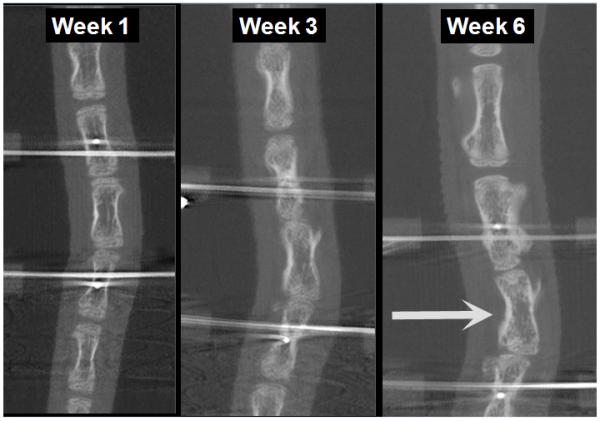
Figure 3.
Postoperative radiograph with Nitinol C-shaped staples placed to produce a convex growth arrest of the right thoracic and left lumbar scoliosis to correct the deformities by growth modulation allowing continued growth on the concave side (Radiograph provided courtesy of John T. Braun, MD).
Anterolateral flexible tethering may have an advantage compared with staples because the continuous tethering may allow for continued correction via vertebral remodeling in addition to asymmetric growth. In a recent case report, a five-year-old boy with juvenile idiopathic scoliosis had a right thoracic curve that progressed from 25° to 40° despite brace treatment. At eight years of age he was treated with an anterolateral flexible tethering procedure (40). Through a mini-thoracotomy vertebral body screws were placed at each level and a polypropylene tether was secured into the screw heads creating an anterior flexible tether without fusion. The postoperative curve was 25° and four years later the curve was 6° (Fig. 4).
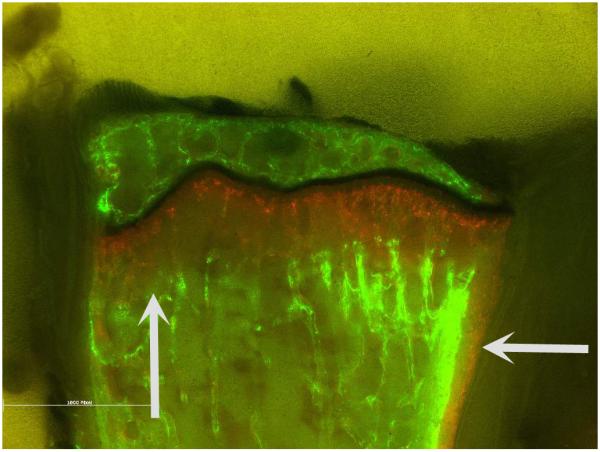
Figure 4.

A, Preoperative posteroanterior radiograph of a 15-year-old girl with adolescent idiopathic scoliosis with a right thoracic curve of 35 degrees. B, Postoperative posteroanterior radiograph showing vertebral body screws creating an anterolateral flexible tether between T5 and T11 with correction of the curve to 20 degrees (Radiographs provided courtesy of John T. Braun, MD).
External fixation to create and correct scoliosis by asymmetric growth and remodeling is well documented in laboratory studies. Although the percutaneous insertion of pedicle screws has been described, there is limited experience with external fixation for the treatment of AIS despite its potential advantages. A preliminary report in a rabbit scoliosis model using an external fixator attached percutaneously to the disc spaces above and below the curve reported satisfactory correction of the scoliosis and vertebral rotation (41). A clinical study of patients with severe scoliosis treated by a two-staged anterior and posterior approach with placement of an external fixator for gradual postoperative correction reported satisfactory results with a follow up of seven years (42). The Russian Ilizarov Scientific Centre “Restorative Traumatology and Orthopaedics” has shown photographs of patients with AIS with dramatic improvement after treatment of their scoliosis with external fixation (Fig. 5).
Figure 5.
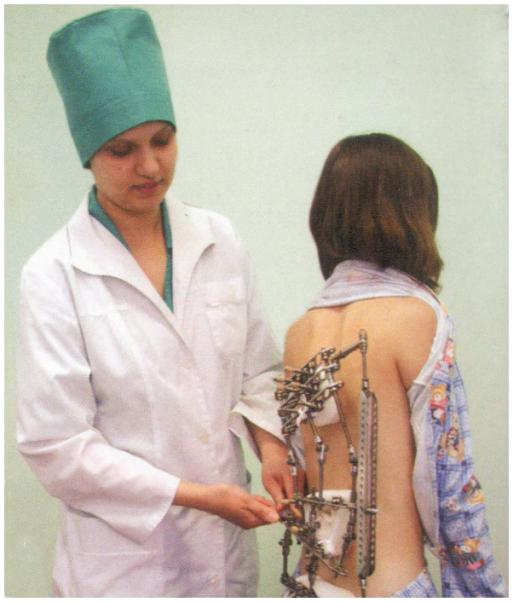

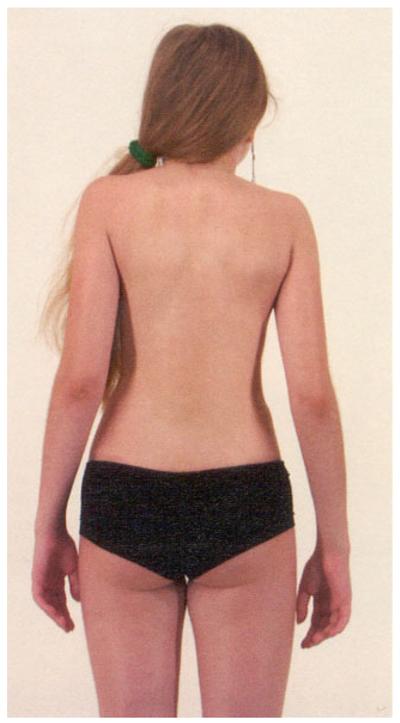
A, Adolescent girl being treated with an external fixator for AIS. B, Preoperative photograph of an adolescent girl with AIS. C, Postoperative photograph after treatment of her scoliosis with an external fixator (Photograph reprinted with permission from The Russian Ilizarov Scientific Centre “Restorative Traumatology and Orthopaedics.”
DISCUSSION
In has been known for centuries that skeletal growth can be modulated by external forces. The custom of binding feet to stunt their growth started in the late 10th century among wealthy Chinese women. The binding resulted in their daughters having feet that were only four inches long. The custom was extremely common, particularly among the upper classes in Northern China, until it was finally outlawed in 1949.
Initially it was believed that scoliosis could only be corrected by the mechanical modulation of growth, so bracing was only recommended for children. The recent animal study creating a 30° scoliosis in older rat tails reported that the vertebral wedge deformity in older animals was caused mainly by diaphyseal remodeling (23). This concept of remodeling in adults has been effective in Orthodontics. Bracing teeth, once considered successful only in children, is now being offered to adults.
To produce asymmetric growth and remodeling in vertebrae by mechanical loading, sufficient forces must be applied for an appropriate period of time. A laboratory study of mechanically modulated growth in rats reported that full-time loading (24 hours/day) created approximately twice the effect of either day-time or night-time loading (12 hours/day) (24). In the clinical study evaluating the efficacy of brace treatment for AIS a logistic regression analyses showed a “dose-response” curve in which the greater number of hours of brace wear correlated with lack of curve progression (31). These reports together support the concept that a spine subjected to sustained mechanical loading will gradually develop corresponding changes in the shape of the vertebrae by a process of asymmetric growth and remodeling. In other words scoliosis can be corrected by applying asymmetric loading to the appropriate vertebrae.
The majority of studies on bracing acknowledge that compliance with brace wear is a major problem. A study on part-time bracing for AIS reported that although the average correction with part-time brace wear was less than that with full-time, compliance was better compared with studies involving full-time bracing (5). Perhaps the improved results of derotational casting compared with bracing, is because the cast cannot be removed so the corrective forces are applied 24 hours per day. If a brace was socially and cosmetically accepted so the patient would were it 24 hours per day, bracing may be a solution for the nonfusion treatment of AIS.
The success of vertebral stapling and anterolateral flexible tethering is thought to be secondary to asymmetric growth created by the instrumentation. A major concern with these procedures is that the stapling or tethering spans the flexible discs, and the immobilized discs may be subject to degeneration. The corrective forces can then be dissipated within the flexible disc, rather than creating the desired effect of modulating vertebral growth and remodeling. Another problem is the concave vertebrae already have decreased growth because of prior loading and the stapling or tethering operation is usually performed only after documented progression of AIS. As a result, these procedures are often performed after closure of the triradiate cartilage (Risser stage I-II), when there is not enough growth remaining to correct the scoliosis by asymmetric growth. The ideal time to use a growth tethering procedure is prior to peak growth velocity, before menses, and before closure of the triradiate cartilage. Unfortunately, patients at this age typically have small curves and the clinician is uncertain whether the scoliosis will progress.
The major advantage of external fixation and anterolateral tethering procedures is that the loading can potentially be adjusted postoperatively. The viscoelastic behavior of the vertebrae and discs combined with the gradual correction of the scoliosis and the presence of continued longitudinal growth over a period of months will require a loading mechanism that is adjustable from outside the patient. With external fixation, the adjustments can be made in the outpatient clinic or possibly at home by the patient or family. With anterolateral tethering, the adjustments could be made with repeat surgery or preferably with a remote controlled device that could adjust forces in the outpatient clinic. Although nonfusion operative correction of AIS is be best suited for young patients with small curves, it may also achieve correction of large curves in older patients via the process of remodeling of the vertebrae and ribs over a longer timeframe.
ACKNOWLEDGMENTS
The authors thank the Scoliosis Research Society Grant #22454 and the National Institutes of Health R01 AR 46543 and R01 AR053132 for their support of this study, and Carole McBride for her substantial contributions to the study.
Supported by the Scoliosis Research Society and the National Institutes of Health, National Institute of Arthritis, Musculoskeletal and Skin Diseases (AR 46543 and AR 053132). None of the authors received any other financial support for this study.
The study was conducted at the University of Vermont College of Medicine, Burlington, VT
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Barsanti CM, deBari A, Covino BM. The torsion meter: a critical review. J Pediatr Orthop. 1990 Jul-Aug;10(4):527–531. [PubMed] [Google Scholar]
- 2.Stokes IA, Aronsson DD. Disc and vertebral wedging in patients with progressive scoliosis. J Spinal Disord. 2001 Aug;14(4):317–322. doi: 10.1097/00002517-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Lonstein J. Idiopathic scoliosis. In: Lonstein RW JE, Bradford DS, Ogilvie JW, editors. Moe’s Textbook of Scoliosis and Other Spinal Deformities. WB Saunders; Philadelphia: 1995. pp. 219–256. [Google Scholar]
- 4.Lonstein JE, Carlson JM. The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am. 1984 Sep;66(7):1061–1071. [PubMed] [Google Scholar]
- 5.Green NE. Part-time bracing of adolescent idiopathic scoliosis. J Bone Joint Surg Am. 1986 Jun;68(5):738–742. [PubMed] [Google Scholar]
- 6.Mente PL, Stokes IA, Spence H, Aronsson DD. Progression of vertebral wedging in an asymmetrically loaded rat tail model. Spine (Phila Pa 1976) 1997 Jun 15;22(12):1292–1296. doi: 10.1097/00007632-199706150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Hueter C. Anatomische studien an den extremitaetengelenken neugeborener und erwachsener. Virchows Arch Pathol Anat Physiol. 1862;25:572–599. [Google Scholar]
- 8.Volkmann R. Verletzungen und krankenheiten der bewegungsorgane. In: Billroth vPa., editor. Handbuch der allgemeinen und speciellen chirurgie Bd II Teil I. Ferdinand Enke; Stuttgart: 1862. [Google Scholar]
- 9.Roaf R. Vertebral growth and its mechanical control. J Bone Joint Surg Br. 1960 Feb;42-B:40–59. doi: 10.1302/0301-620X.42B1.40. [DOI] [PubMed] [Google Scholar]
- 10.Stokes IA, Spence H, Aronsson DD, Kilmer N. Mechanical modulation of vertebral body growth. Implications for scoliosis progression. Spine (Phila Pa 1976) 1996 May 15;21(10):1162–1167. doi: 10.1097/00007632-199605150-00007. [DOI] [PubMed] [Google Scholar]
- 11.Stokes IA, Aronsson DD, Dimock AN, Cortright V, Beck S. Endochondral growth in growth plates of three species at two anatomical locations modulated by mechanical compression and tension. J Orthop Res. 2006 Jun;24(6):1327–1334. doi: 10.1002/jor.20189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Akyuz E, Braun JT, Brown NA, Bachus KN. Static versus dynamic loading in the mechanical modulation of vertebral growth. Spine (Phila Pa 1976) 2006 Dec 1;31(25):E952–958. doi: 10.1097/01.brs.0000248810.77151.22. [DOI] [PubMed] [Google Scholar]
- 13.Niehoff A, Kersting UG, Zaucke F, Morlock MM, Bruggemann GP. Adaptation of mechanical, morphological, and biochemical properties of the rat growth plate to dose-dependent voluntary exercise. Bone. 2004 Oct;35(4):899–908. doi: 10.1016/j.bone.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Noonan KJ, Farnum CE, Leiferman EM, Lampl M, Markel MD, Wilsman NJ. Growing pains: are they due to increased growth during recumbency as documented in a lamb model? J Pediatr Orthop. 2004 Nov-Dec;24(6):726–731. doi: 10.1097/00004694-200411000-00024. [DOI] [PubMed] [Google Scholar]
- 15.Villemure I, Stokes IA. Growth plate mechanics and mechanobiology. A survey of present understanding. J Biomech. 2009 Aug 25;42(12):1793–1803. doi: 10.1016/j.jbiomech.2009.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sergerie K, Lacoursiere MO, Levesque M, Villemure I. Mechanical properties of the porcine growth plate and its three zones from unconfined compression tests. J Biomech. 2009 Mar 11;42(4):510–516. doi: 10.1016/j.jbiomech.2008.11.026. [DOI] [PubMed] [Google Scholar]
- 17.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Spine (Phila Pa 1976) 2010 Jun 1;35(13):1285–1293. doi: 10.1097/BRS.0b013e3181dc48f4. [DOI] [PubMed] [Google Scholar]
- 18.Newton PO, Upasani VV, Lhamby J, Ugrinow VL, Pawelek JB, Bastrom TP. Surgical treatment of main thoracic scoliosis with thoracoscopic anterior instrumentation. Surgical technique. J Bone Joint Surg Am. 2009 Oct 1;91(Suppl 2):233–248. doi: 10.2106/JBJS.I.00368. [DOI] [PubMed] [Google Scholar]
- 19.Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005 Jul 15;30(14):1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 20.Mente PL, Aronsson DD, Stokes IA, Iatridis JC. Mechanical modulation of growth for the correction of vertebral wedge deformities. J Orthop Res. 1999 Jul;17(4):518–524. doi: 10.1002/jor.1100170409. [DOI] [PubMed] [Google Scholar]
- 21.Stokes IA, Mente PL, Iatridis JC, Farnum CE, Aronsson DD. Enlargement of growth plate chondrocytes modulated by sustained mechanical loading. J Bone Joint Surg Am. 2002 Oct;84-A(10):1842–1848. doi: 10.2106/00004623-200210000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Apte SS, Kenwright J. Physeal distraction and cell proliferation in the growth plate. J Bone Joint Surg Br. 1994 Sep;76(5):837–843. [PubMed] [Google Scholar]
- 23.Aronsson DD, Stokes IA, McBride C. The role of remodeling and asymmetric growth in vertebral wedging. Stud Health Technol Inform. 2010;158:11–15. [PubMed] [Google Scholar]
- 24.Stokes IA, Gwadera J, Dimock A, Farnum CE, Aronsson DD. Modulation of vertebral and tibial growth by compression loading: diurnal versus full-time loading. J Orthop Res. 2005 Jan;23(1):188–195. doi: 10.1016/j.orthres.2004.06.012. [DOI] [PubMed] [Google Scholar]
- 25.Bylski-Austrow DI, Wall EJ, Glos DL, Ballard ET, Montgomery A, Crawford AH. Spinal hemiepiphysiodesis decreases the size of vertebral growth plate hypertrophic zone and cells. J Bone Joint Surg Am. 2009 Mar 1;91(3):584–593. doi: 10.2106/JBJS.G.01256. [DOI] [PubMed] [Google Scholar]
- 26.Braun JT, Hoffman M, Akyuz E, Ogilvie JW, Brodke DS, Bachus KN. Mechanical modulation of vertebral growth in the fusionless treatment of progressive scoliosis in an experimental model. Spine (Phila Pa 1976) 2006 May 20;31(12):1314–1320. doi: 10.1097/01.brs.0000218662.78165.b1. [DOI] [PubMed] [Google Scholar]
- 27.Newton PO, Upasani VV, Farnsworth CL, et al. Spinal growth modulation with use of a tether in an immature porcine model. J Bone Joint Surg Am. 2008 Dec;90(12):2695–2706. doi: 10.2106/JBJS.G.01424. [DOI] [PubMed] [Google Scholar]
- 28.Braun JT, Akyuz E, Udall H, Ogilvie JW, Brodke DS, Bachus KN. Three-dimensional analysis of 2 fusionless scoliosis treatments: a flexible ligament tether versus a rigid-shape memory alloy staple. Spine (Phila Pa 1976) 2006 Feb 1;31(3):262–268. doi: 10.1097/01.brs.0000197569.13266.fe. [DOI] [PubMed] [Google Scholar]
- 29.Blount WPMJ. The Milwaukee Brace. Williams and Wilkins; Baltimore: 1973. [Google Scholar]
- 30.Allington NJ, Bowen JR. Adolescent idiopathic scoliosis: treatment with the Wilmington brace. A comparison of full-time and part-time use. J Bone Joint Surg Am. 1996 Jul;78(7):1056–1062. [PubMed] [Google Scholar]
- 31.Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010 Jun;92(6):1343–1352. doi: 10.2106/JBJS.I.01142. [DOI] [PubMed] [Google Scholar]
- 32.Coillard C, Leroux MA, Zabjek KF, Rivard CH. SpineCor--a non-rigid brace for the treatment of idiopathic scoliosis: post-treatment results. Eur Spine J. 2003 Apr;12(2):141–148. doi: 10.1007/s00586-002-0467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wong MS, Cheng JC, Lam TP, et al. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2008 May 20;33(12):1360–1365. doi: 10.1097/BRS.0b013e31817329d9. [DOI] [PubMed] [Google Scholar]
- 34.Hasler CSC, Enggist A, Neuhaus C, Erb T. No effect of osteopathic treatment on trunk morphology and spine flexibility in young women with adolescent idiopathic scoliosis. J Child Orthop. 2010;4:219–226. doi: 10.1007/s11832-010-0258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanders JO, D’Astous J, Fitzgerald M, Khoury JG, Kishan S, Sturm PF. Derotational casting for progressive infantile scoliosis. J Pediatr Orthop. 2009 Sep;29(6):581–587. doi: 10.1097/BPO.0b013e3181b2f8df. [DOI] [PubMed] [Google Scholar]
- 36.Winter RB. Convex anterior and posterior hemiarthrodesis and hemiepiphyseodesis in young children with progressive congenital scoliosis. J Pediatr Orthop. 1981;1(4):361–366. doi: 10.1097/01241398-198112000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Thompson GH, Akbarnia BA, Campbell RM., Jr. Growing rod techniques in early-onset scoliosis. J Pediatr Orthop. 2007 Apr-May;27(3):354–361. doi: 10.1097/BPO.0b013e3180333eea. [DOI] [PubMed] [Google Scholar]
- 38.Campbell RM, Jr., Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. 2004 Aug;86-A(8):1659–1674. doi: 10.2106/00004623-200408000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Betz RR, D’Andrea LP, Mulcahey MJ, Chafetz RS. Vertebral body stapling procedure for the treatment of scoliosis in the growing child. Clin Orthop Relat Res. 2005 May;(434):55–60. doi: 10.1097/01.blo.0000163472.46511.a8. [DOI] [PubMed] [Google Scholar]
- 40.Crawford CH, 3rd, Lenke LG. Growth modulation by means of anterior tethering resulting in progressive correction of juvenile idiopathic scoliosis: a case report. J Bone Joint Surg Am. 2010 Jan;92(1):202–209. doi: 10.2106/JBJS.H.01728. [DOI] [PubMed] [Google Scholar]
- 41.Abe J, Nagata K, Ariyoshi M, Inoue A. Experimental external fixation combined with percutaneous discectomy in the management of scoliosis. Spine (Phila Pa 1976) 1999 Apr 1;24(7):646–653. doi: 10.1097/00007632-199904010-00006. [DOI] [PubMed] [Google Scholar]
- 42.Reyes-Sanchez A, Rosales LM, Miramontes V. External fixation for dynamic correction of severe scoliosis. Spine J. 2005 Jul-Aug;5(4):418–426. doi: 10.1016/j.spinee.2004.11.013. [DOI] [PubMed] [Google Scholar]