Abstract
Background
Despite increasing recognition of the significance of learning from errors, little is known about how learning climate contributes to error reduction.
Objectives
To investigate whether learning climate moderates the relationship between error-producing conditions and medication errors.
Method
A cross-sectional descriptive study was done using data from 279 nursing units in 146 randomly selected hospitals in the United States. Error-producing conditions included work environment factors (work dynamics and nurse mix), team factors (communication with physicians and nurses’ expertise), personal factors (nurses’ education and experience), patient factors (age, health status, and previous hospitalization), and medication-related support services. Poisson models with random effects were used with the nursing unit as the unit of analysis.
Results
A significant negative relationship was found between learning climate and medication errors. It also moderated the relationship between nurse mix and medication errors: When learning climate was negative, having more registered nurses was associated with fewer medication errors, and this relationship trended towards significance. However, no relationship was found between nurse mix and medication errors at either positive or average levels of learning climate. Learning climate did not moderate the relationship between work dynamics and medication errors.
Discussion
The way nurse mix affects medication errors depends on the level of learning climate. Nursing units with fewer registered nurses and frequent medication errors should examine their learning climate. Future research should be focused on the role of learning climate as related to the relationships between nurse mix and medication errors.
Keywords: medication errors, learning climate, nurse mix
Since the Institute of Medicine (IOM) report To Err is Human (Kohn, Corrigan, & Donaldson, 2000), the United States has made significant efforts to improve patient safety. With regard to medication errors, numerous studies have been published identifying the epidemiology and etiology of medication errors, and hospitals, nursing homes, and other health care organizations continue to evaluate evidence-based interventions and to develop safety guidelines and protocols. Despite such progress, the IOM recently estimated that at least one medication error occurs every day for every hospitalized patient, suggesting that medication errors still remain a significant problem (IOM, 2006).
Safety culture has been emphasized as a necessary condition for patient safety, which includes reducing the number of medication errors (Kohn et al., 2000). A positive safety culture exists when group members share perceptions of the importance of safety, communicate with mutual trust, and have confidence in the efficacy of preventive measures (Health and Safety Commission, 1993). The Joint Commission included an annual assessment of safety culture in 2007 patient safety goals, and many healthcare organizations have embarked on efforts to assess safety culture or, on the surface, safety climate.
Although reducing medication errors is an important goal, there is consensus that eliminating them completely is unlikely, particularly when there are high volumes of activity. It has been estimated, for example, that a 600-bed teaching hospital with 99.9% error free drug ordering, dispensing, and administration will still experience 4,000 drug errors a year (Leape, 1994). Therefore, organizations also must improve their strategies in dealing with errors when they do occur. Unfortunately, there has been less emphasis on error management and the central feature, learning climate. The error management approach is focused on how to deal with errors when they occur. It emphasizes creating a positive learning climate, in which learning from errors is fostered in organizations. Although learning climate has been considered similar to, or incorporated into, safety climate, learning climate is focused on errors.
During the past decade, there has been increasing recognition in health care research of the significance of learning from errors (Berta & Baker, 2004; Edmondson, 2004; Rivard, Rosen, & Carroll, 2006). Organizations with a positive learning climate have the competence to draw the appropriate conclusions from their safety information systems and the willingness to implement major reforms where needed (Department of Health, 2000). However, little is known about how learning climate contributes to error management and, ultimately, to error reduction. In fact, the current literature on medication errors tends to be focused primarily on work conditions that are conducive to error occurrence, such as complex work environment or inadequate staffing and resources. Understanding the mechanism of learning climate in error management is therefore of importance for health care organizations to achieve patient safety.
In this study, it was investigated whether learning climate moderated the relationship between work dynamics and nurse mix and medication errors. Specifically, the hypothesis that a positive learning climate would mitigate (and a negative learning climate exacerbate) the negative effects of highly dynamic work conditions and less RNs in the nurse mix on medication errors.
Conceptual Framework
Error management and learning climate
A central premise of the error management approach is that human errors cannot be prevented completely. Therefore, rather than focusing on eliminating errors, this approach emphasizes how to manage errors when they occur and how to learn from them (van Dyck, Frese, Baer, & Sonnentag, 2005). The error management approach targets errors--unintended but failed actions due to a mistakenly faulty plan or a miscue in the execution of the correct plan (Heimbeck, Frese, Sonnentag, & Keith, 2003; Keith & Frese, 2005). Errors are distinguished from their consequences and errors are reported and detected quickly so that negative consequences are handled effectively and minimized, during which learning occurs.
Organizational learning researchers view errors as a natural part of work. Communicating about them should encourage individuals to explore and experiment and finally learn from their errors. Similarly, error management researchers suggest that learning takes place when people are encouraged to learn from errors (Heimbeck et al., 2003), when they think about errors thoroughly (e.g., planning, monitoring, and evaluating actions), and when the negative emotional impact of errors is abated (Keith & Frese, 2005). Error management researchers value organizational practices related to communicating about errors, sharing error knowledge, helping in error situations, and quickly detecting and handling errors (van Dyck et al., 2005), all of which are attributes of learning climate.
A positive learning climate where nurses openly evaluate the potential causes of medication errors will facilitate learning about the errors and, consequently, decrease medication errors over time. When there is a positive learning climate on the unit, nurses are more likely to be aware of errors because they communicate and think about errors frequently. Nurses working in a positive learning climate will be encouraged to engage actively in such error management activities as fixing error-prone work situations or intercepting near misses so that even if an error occurred in a previous stage (i.e., ordering or dispensing), it cannot come through to a subsequent stage of the medication administration process. A negative learning climate, however, not only discourages nurses from acting, but it opens gaps and weaknesses to allow errors to occur, and most importantly, it can allow them to remain uncorrected. In such situations, nurses are not encouraged or allowed to deal proactively with known deficiencies in system defenses and when the holes in the system momentarily line up, an error occurs (Reason, 1990).
Most health care researchers have been interested in the direct relationship between work condition factors and medication errors. However, some have suggested that, depending on an organization’s learning climate, the magnitude of the relationship between work environment and safety outcomes can be either attenuated or intensified (Probst, 2004). Specifically, in a nursing unit in which communication among workers is rare or unidirectional and admitting one’s mistakes is not valued (i.e., negative learning climate), the negative effect of a deficient work environment on error occurrence will be increased and the positive effect of a good work environment will be attenuated. To illustrate, in a nursing unit where work is often delayed due to high volumes of patients and resulting frequent changes of care plans (i.e., highly dynamic work situations) and physical and personnel resources to take care of patients are insufficient (i.e., short staffing), nurses may feel that their primary job priority is to get the work finished as quickly as possible and, therefore, they may be more likely to engage in short-cuts (Tucker, Edmondson, & Spear, 2001). In this circumstance, double checking and documenting may be reduced and actions may be carried out less attentively, resulting in reduced monitoring, sometimes leading to error (Elfering, Semmer, & Grebner, 2006). Further, because the root cause of a problem is neither identified nor remedied, such first-order problem solving can result in future errors.
In contrast, if a nursing unit places patient safety as its priority and encourages nurses to have open channels of communication (i.e., a positive learning climate), the negative impact of the work environment can be mitigated because, in the long run, a positive learning climate fosters the creation of work environments that make it easier for nurses to comply with required safe work practices (DeJoy, Gershon, & Schaffer, 2004). If nursing unit staff members encourage frequent communications and open discussions about errors, nurses will be more likely to be aware of the possibility of committing errors and more cautious in taking care of patients. Such tendencies may be augmented when work is more dynamic because then these nurses, who are aware of the possibility of errors in such a situation, will pay special attention to patient care in order to prevent errors (Zhao & Olivera, 2006). Similarly, when nursing units are staffed with more registered nurses (RNs) in the nurse mix, RNs who anticipate errors, will build heightened levels of redundancy in the surveillance system and be aware of other nurses’ work. Further, other nursing personnel can learn effective error management practices from those RNs. In other words, a positive learning climate can mitigate the negative effect of poor work environment on error occurrence.
Error-producing conditions
A model of antecedents of medication errors was developed based on the conceptualization of error-producing conditions suggested by Dean, Schachter, Vincent, and Barber (2002): work-environment factors, team factors, person factors, medication-related support services, and patient-specific factors (Chang & Mark, 2009). In this previous study, it was examined whether or not medication errors of different severity (severe vs. nonsevere) had different error-producing conditions, and severe and nonsevere medication errors were found to have different antecedents. Contrary to expectations and prior research (Blegen, Goode, & Reed, 1998; McGillis Hall, Doran, & Pink, 2004), no relationship was found between work dynamics and number of RNs in the nurse mix and either type of medication error.
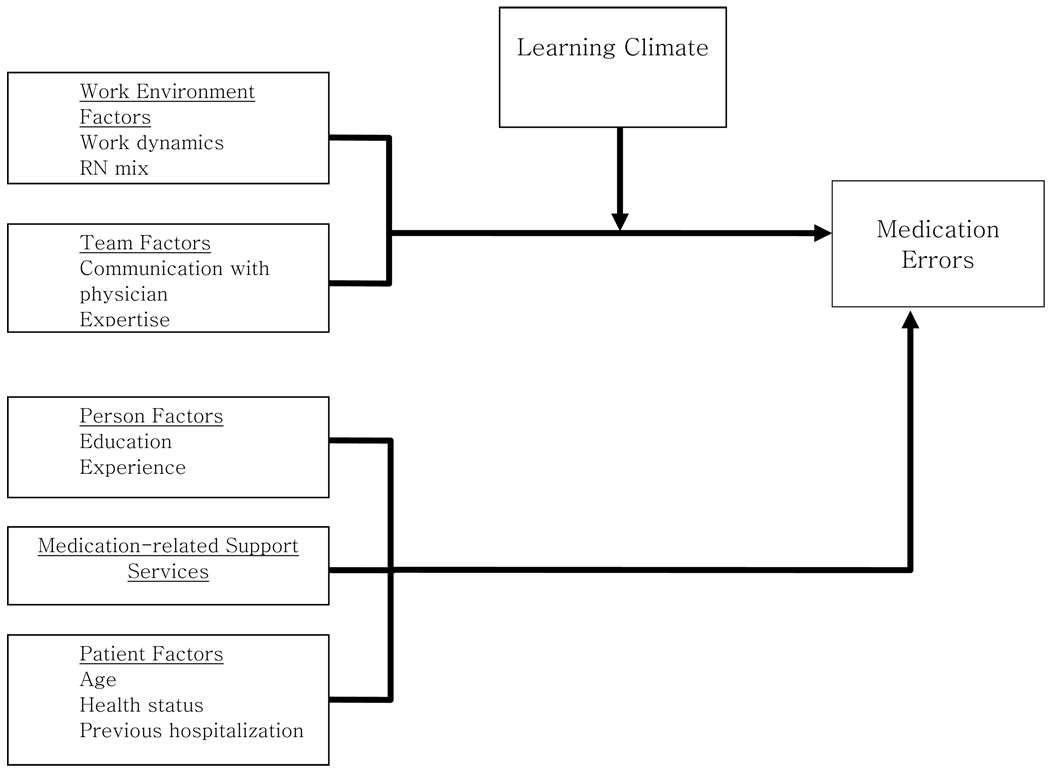
In the current study, these findings were probed further by examining the role of learning climate as a moderator in these relationships. The basic hypothesis was that the direction of the relationship between work environment and safety outcomes can be positive or negative depending on an organization’s learning climate. If learning climate influences these relationships in opposite directions, it might obscure the true relationships and the overall trend may appear to be insignificant. Unlike the previous study, only severe medication errors were investigated, because when incident reports are used as the measurement procedure, the reported numbers of nonsevere errors were likely to reflect nurses’ error-reporting behavior and a tendency to underreport, while incident reports of severe errors are likely to reflect the number of errors more closely. Therefore, learning climate was added to the previous model (Figure 1).
Figure 1.
Theoretical Framework
Work environment factors
Nurses often organize and reorganize priorities simultaneously and manage changing clinical information for multiple patients. Further, nurses constantly shift their attention from patient to patient and often have to carry out several tasks simultaneously, which has great potential to make nurses rush and commit an error. Nurse mix was included because having more RNs in the mix has been shown to be related inversely to medication errors such that higher RN mix has been associated with a decrease in medication errors (Blegen et al., 1998; McGillis Hall et al., 2004), or higher non-RN mix was associated with an increase in failure to rescue from medication error (Seago, Williamson, & Atwood, 2006).
Team factors
Medication administration is a multistage process with involvement of numbers of individuals from multiple disciplines. Therefore, well-coordinated interactions and communication across disciplines in each step are critical for safe medication administration (Manojlovich & DeCicco, 2007). Particularly, inadequate or insufficient communication between nurses and physicians (misinterpretation of orders, oral and written miscommunication, or incorrect interaction) increases medication errors (Kohn et al., 2000; Leape, 1994).
Also examined was nurses’ expertise, or the ability to recognize potentially ominous events early (Minick & Harvey, 2003). The earliest changes in a patient’s condition can be very subtle and difficult to describe, and only nurses who possess clinical expertise can recognize the first indication of a change based on careful monitoring of a patient. Expert nurses are expected to make fewer errors than less expert nurses because they are better at preventing a potential error by checking on a patient’s laboratory data, detecting an adverse effect, and anticipating an adverse reaction related to the patient’s pathophysiology (Eisenhauer, Hurley, & Dolan, 2007).
Personal factors
While researchers have found a linear relationship between education and experience of nurses and medication errors, an asymptotic relationship was found between nurses’ education and medication errors in a recent study: as the percentage of unit BSN-prepared nurses increased, medication errors decreased until the percentage of BSN-prepared nurses reached 54% (Chang & Mark, 2009).
Medication-related support services
While the literature has reported mixed findings in terms of the effectiveness of medication-related support services (Kaushal, Shojania, & Bates, 2003; Oren, Shaffer, & Guglielmo, 2003), these services are expected to minimize the possibility of human error in the medication process. A list of support services were examined, such as computerized physician order entry systems, unit-dose medication systems, automated medication administration systems (i.e., high-tech services), transcribing orders and placing information in patient charts, intravenous (IV) team services, medication and IV fluid delivery services, and pharmacist consultation (i.e., low-tech services).
Patient factors
Patient characteristics examined included patient age, health status, and previous hospitalization to adjust for patient severity. Despite inconclusive findings on the relationship between these factors and medication errors, they are considered as proxy measures of severity, and have been found to be associated with increased risk of adverse drug events (Evans, Lloyd, Stoddard, Nebeker, & Samore, 2005).
Method
Data and Sample
Data were used from a federally funded, multisite organizational study investigating relationships among hospitals’ external and internal environments, staffing adequacy, work conditions, and organizational and patient outcomes (Mark et al., 2007). In the parent study data were collected for 6 months from 146 randomly selected hospitals; these hospitals were nonfederal, not-for-profit, and nonpsychiatric, and had at least 99 licensed beds. Two general medical-surgical or medical-surgical specialty units from each hospital were invited to participate (n = 286). Nurses eligible to participate were RNs employed on their unit for not less than 3 months (n = 4,954). Patients eligible to participate were 18 years or older, able to speak English, hospitalized on the unit for at least 48 hours, and not scheduled for discharge the day the questionnaire was completed (n = 2,744).
Procedures
Study coordinators appointed by each hospital were in charge of distributing questionnaires to staff nurses and obtaining administrative data. Study coordinators participated in 1½ days of training given by the study project team to ensure the fidelity of data collection procedures. Nurses completed three different questionnaires distributed during the 1st, 3rd, and 5th month of data collection. All measures except communication with physicians and learning climate were obtained during the 1st month of data collection. The staff nurse response rates were 75% at the first round, 58% at the second round, and 54% at the third round. Study coordinators selected 10 patients at random from each nursing unit and the patients provided data during the final month of data collection. The patient response rate was 91%.
Measures
Dependent variables
Because incident reports were used as the source of medication error data collection, errors in medication administration were the focus of this study. A medication error was defined as the wrong dose, wrong patient, wrong time, wrong drug, wrong route, or an error of omission. This variable was measured for 6 consecutive months, with values scaled to 1,000 inpatient days. Among all medication errors reported, severe medication errors--defined as those resulting in increased nursing observation, increased technical monitoring, laboratory testing, radiographic testing, medical intervention, or transfer of the patient to another unit--were examined specifically. Previously, different attributes and antecedents were found between nonsevere and severe medication errors and two types of medication errors suggested to have different levels of reporting bias (Chang & Mark, 2009). Knowing that severe medication errors are affected less by reporting bias than nonsevere errors, severe errors were used in this paper to minimize the potential problem caused by reporting bias.
Work environment factors
Work dynamics were measured as the extent to which nursing units were characterized by frequent interruptions or unanticipated events. The scale used consists of seven items with six response options ranging from 1 = strongly disagree to 6 = strongly agree, and higher scores were indicative of greater work dynamics (Salyer, 1996). One factor accounted for 53.8% of variance in work dynamics. The second factor, amount of RNs in the nurse mix, was defined as the percentage of nursing care hours delivered by all RNs among those delivered by all nursing personnel (RNs, LPNs or LVNs, nurse aides).
Team factors
Communication with physicians was measured using a five-point Likert-type scale (Gittell et al., 2000) composed of four communication dimensions (frequency, timeliness, accuracy, and problem-solving) and three relationship dimensions (shared goals, shared knowledge, and mutual respect). Gittell reported Cronbach’s alpha of .85 for the total scale and .72 to .84 for the individual dimensions. This scale consists of two factors representing communication and relationship dimensions and together they explained 65.0% of variance in scores. A total scale score was used, with higher scores indicative of better communication and better relationships among physicians and nurses. Nursing expertise was measured using eight items from the Nursing Expertise and Commitment to Care Scale (Minick, Dilorio, Mitchell, & Dudley, 2000). Nurses were asked to rate the expertise of their nursing workgroup concerning recognizing critical patient problems. A single factor explained 65.2% of the variance in scores. Items were anchored to response options ranging from 1 = strongly disagree to 6 = strongly agree, with higher scores indicative of greater expertise.
Personal factors
Education level was defined as the proportion of nurses on each nursing unit whose highest education level was a bachelor’s degree or higher, and RN experience was defined as the average of each nurse’s experience as a RN in months. A previous study showed curvilinear relationships between these variables and medication errors (Chang & Mark, 2009), thus both linear and squared terms were included.
Medication-related support services
This variable was measured by using a checklist in which nurses rated six medication-related support services as 0 = not available, 1 = inconsistently available, or 2 = consistently available (Mark et al., 2007). Higher scores were indicative of greater availability of these services.
Patient factors
Patient age was defined as the average age of patients who participated in the study. Health status was measured by asking patients to rate their health status in five categories ranging from 1 = very poor to 5 = very good. Previous hospitalization was measured by asking whether the patient had been hospitalized in the past year; yes was coded as 1.
Learning climate
Learning climate was measured using 13 items from the Error Orientation Scale developed by Rybowiak, Garst, Frese, and Batinic (1999). These 13 items represent (a) employees’ willingness to reveal errors, (b) degree of open communication about errors, and (c) extent to which employees actively think about and diagnose the sources of errors. The results of factor analysis confirmed the three-factor structure of this scale. Consistent with past research, the three dimensions showed satisfactory internal consistency reliability ranging from .83 to .92 (Rybowiak et al., 1999; van Dyck et al., 2005). Items on this 5-point Likert-type scale were anchored by response options ranging from 1= strongly disagree to 5 = strongly agree, with higher scores indicative of a positive learning climate.
Because the unit of analysis was nursing units, some variables measured at the individual level (e.g., work dynamics, communication with physicians, nursing expertise, learning climate) were aggregated to the nursing unit level. Justification for data aggregation was based on achieving values equal to .70 or greater for the rwg statistic, which is used to estimate within-group agreement (James, Demaree, & Wolf, 1984; Klein & Kozlowski, 2000). The reliability of the aggregated data was evaluated using the proportion of variance explained by group membership using the intraclass correlation coefficient (ICC[1]) and mean rater reliability using ICC(2). The ICC(2) values of 0.70 or higher indicate acceptable group-level reliability.
Data Analysis
Medication errors were modeled using Poisson regression with random effects. The purpose of including random effects is to account for the clustering of nursing units within the hospitals and overdispersion of the dependent variable. Overdispersion occurs when the observed variance is greater than the mean, which is common in count variables such as medication errors. The number of medication errors was standardized to best reflect actual medication error rates by dividing by patient days. The analyses were performed using SAS version 9.2.
To conduct post hoc tests for the interaction terms, significant interactions were plotted between two continuous variables by using the mean for learning climate and one standard deviation above and below the mean to generate regression lines (Cohen, Cohen, West, & Aiken, 2003). Post hoc tests were used to determine whether the slope of the simple regression lines significantly differed from zero (Aiken & West, 1991).
Results
Descriptive statistics of selected variables along with relevant internal consistency reliability estimates, the ICC1, ICC2, and rwg, where appropriate are presented in Table 1. All except nursing expertise showed satisfactory results. While low reliability statistics may indicate low group membership and provide insufficient justification for aggregation, Klein and Kozlowski (2000) pointed out that researchers usually have concluded that aggregation is justified when the F test for ICC(1) values is significant. Further, low values for ICC(2) may have been caused by small group sizes in the sample because the average number of nurses on nursing units was 17.32, less than 25, the cut-point for a large sample (Bliese, 2000; Klein & Kozlowski, 2000).
Table 1.
Descriptive Statistics
| Mean | SD | Cronbach’s α | ICC(1) | ICC(2) | rwg | |
|---|---|---|---|---|---|---|
| Dependent Variable | ||||||
| Medication errors | 3.71 | 6.05 | NA | |||
| Independent Variables | ||||||
| Work dynamics | 26.84 | 3.50 | 0.85 | 0.17 | 0.78 | 0.80 |
| Percentage of RNs in nurse mix | 62.14 | 13.74 | NA | NA | ||
| Communication with physicians | 25.36 | 2.22 | 0.82 | 0.36 | 0.88 | 0.95 |
| Nursing expertise | 42.44 | 2.09 | 0.92 | 0.09 | 0.62 | 0.96 |
| Education | 36.52 | 19.36 | NA | |||
| RN experience | 138.49 | 45.38 | NA | |||
| Medication-related support services | 8.83 | 1.19 | NA | |||
| Patient Factors | ||||||
| Age (in years) | 56.91 | 7.53 | NA | |||
| Health status | 3.46 | 0.45 | ||||
| Previous hospitalization | 0.53 | 0.21 | ||||
| Learning Climate | 48.04 | 3.94 | 0.92 | 0.23 | 0.80 | 0.95 |
Notes. RN = registered nurse
On average, nursing units had 3.71 medication errors (median = 2, range = 0 to 49) within 6 months. On average, 62% of nursing care hours were provided by RNs. Also, the nursing units employed, on average, a 37% BSN-prepared RN staff and the nurses’ average experience was 138 months. The average age of patients was 57 years, their self-rated health status was moderate to good, and 53% (0 to 100) had experienced hospitalizations in the past year. There was no sign of multicollinearity with overall correlations among the independent variables ranging from −0.41 to 0.27 (results not shown).
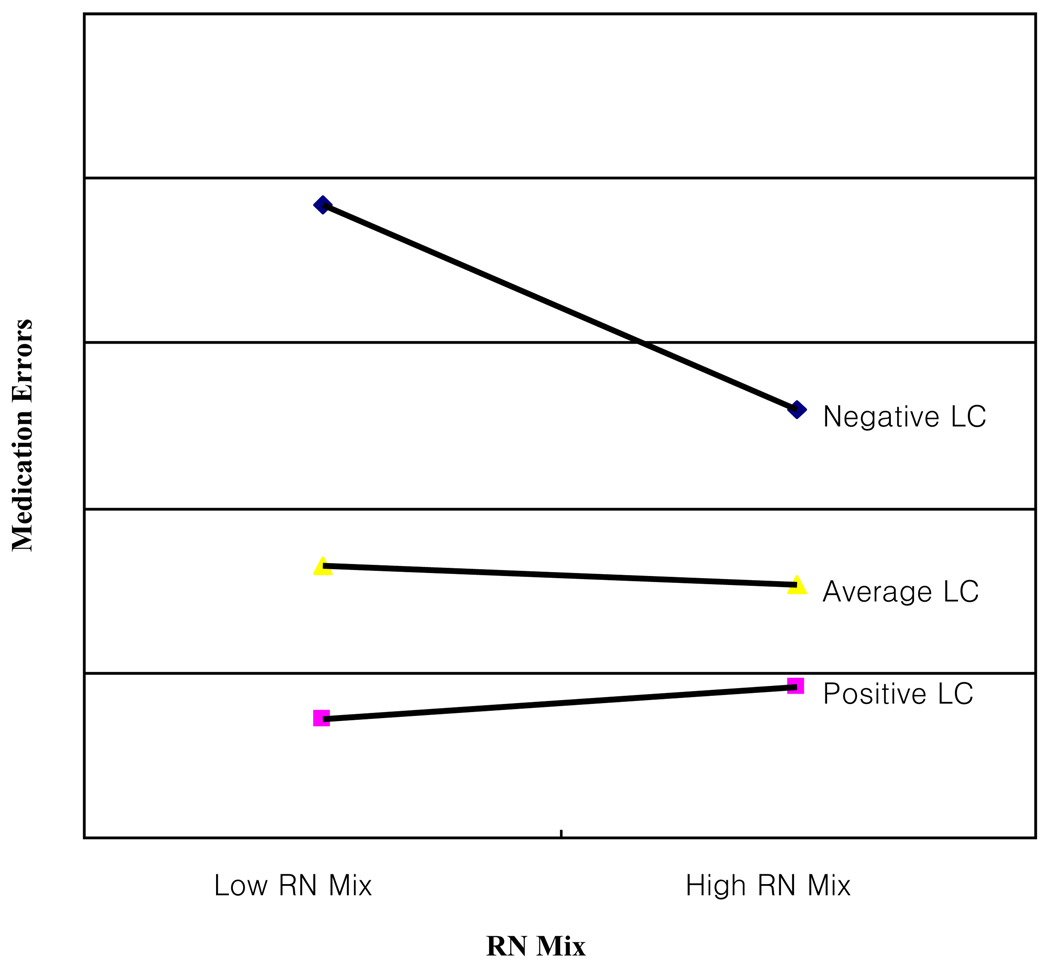
The results of the Poisson regression with random effects model are shown in Table 2. There was a significant negative association between learning climate and medication errors (p < .01), such that the more positive the learning climate, the fewer the medication errors. Further, learning climate moderated the relationship between amount of RNs in the nurse mix and medication error rates (p < .01). To examine this effect more closely, an interaction plot was drawn using the mean for learning climate and one standard deviation above and below the mean to generate regression lines (Cohen et al., 2003). As shown in Figure 2, when learning climate was poor, having a higher amount of RNs was associated with fewer medication errors and this relationship was significant (β = −0.0144, t = −1.95, p < .05). However, no relationship was found between amount and medication errors when learning climate was good (β = .0089, t = 1.16, p = n.s.) or average (β = −0.0027, t = −.43, p = n.s.). In contrast, learning climate did not moderate the relationship between work dynamics and medication errors. Therefore, the moderating effect of learning climate was identified only in the relationship between amount of RNs and medication errors.
Table 2.
The Effects of Error-Producing Conditions on Medication Errors
| Variable | Estimate | Standard Error | t |
|---|---|---|---|
| Intercept | 10.1926 | 6.5491 | 1.56 |
| Work Dynamics | −0.3049 | 0.1702 | −1.79 |
| RN Mix | −0.1447 | 0.0511 | −2.83** |
| Communication with Physician | 0.0478 | 0.0330 | 1.45 |
| Expertise | −0.0229 | 0.0300 | −0.76 |
| Education | −0.0171 | 0.0092 | −1.85 |
| Education2 | 0.0002 | 0.0001 | 2.03* |
| Experience | 0.0086 | 0.0050 | 1.73 |
| Experience2 | −0.00003 | 0.00002 | −1.93 |
| Support Services | −0.1096 | 0.0701 | −1.56 |
| Patient Age | 0.0049 | 0.0064 | 0.77 |
| Health Status | −0.0582 | 0.1209 | −0.48 |
| Previous Hospitalization | 0.1042 | 0.2389 | 0.44 |
| Learning Climate | −0.3572 | 0.1316 | −2.72** |
| Work Dynamics × Learning Climate | 0.0060 | 0.0035 | 1.73 |
| RN Mix × Learning Climate | 0.0030 | 0.0011 | 2.78** |
Notes.
p < .05,
p < .01
Figure 2.
Moderating Effect of Learning Climate on RN Mix and Medication Errors
Nurses’ education had a negative effect on medication error rates with a diminishing marginal effect, and this relationship was significant (p < .05 for education-squared). Specifically, as the level of nurses’ education increased, medication error rates decreased until a nursing unit had 38% of RNs on the unit. After this point, the relationship did not continue, and the shape of the curve was almost flat. In contrast, the effect of nurses’ experience demonstrated the opposite, but this relationship was not significant.
Nurses’ communication with physicians and nurses’ expertise were not associated significantly with medication errors. None of the patient variables was significant, nor was the availability of medication-related support services.
Discussion
Despite the emphasis placed on creating a positive learning climate for patient safety, research evidence has been limited in explicating how and under what mechanisms learning climate plays a role in enhancing patient safety outcomes. The purpose of this study was to examine whether or not learning climate moderated the relationship between work dynamics and amount of RNs in the nurse mix and medication errors. In addition to having a direct negative association with medication errors, learning climate was found to moderate the relationship between nurse mix and medication errors in a way that, when learning climate was poor, nursing units staffed with fewer RNs reported more medication errors than those with more RNs. However, this association did not occur under average or good learning climates.
Learning from errors is the process of creating, retaining, and transferring effective knowledge and practices to reduce the likelihood of similar errors reoccurring in the future (Chuang, Ginsburg, & Berta, 2007). When learning is encouraged, nurses develop mutual understandings of one another’s experiences and perspectives and, through this process, they modify the practices that are perceived collectively to be effective or ineffective. Consequently, practices considered to be effective are likely to be retained and transferred among nurses in the unit (Argote, Ingram, Levine, & Moreland, 2000).
Registered nurses are considered to possess the capability and competence to undertake medication administration correctly. Further, through continuing vigilance and surveillance, they are able to prevent errors or correct near misses to minimize harm to the patient. Under a positive learning climate, RNs may feel responsible for supervising other nursing personnel and sharing clinical expertise. In turn, other nurses may adopt effective practices exemplified by RNs. Over time, RNs’ knowledge and experience with error prevention and management will be shared with and transferred to other nurses on the unit and group learning will take place (Chuang et al., 2007). In such situations, the amount of RNs will be a less important factor in the occurrence of medication errors, because all nurses benefit from group learning. However, when the learning climate is poor, individual learning processes are not shared or transferred among nurses, and only those who possess relevant competency will perform best practices. In this case, amount of RNs matters. This finding is an important addition to existing literature on nurse staffing and patient safety outcomes; not only was an association found between nurse staffing and medication errors, but also identified was the point at which RN mix becomes critical.
Work dynamics failed to have statistically significant associations with medication errors, regardless of learning climate. One explanation for this finding may be related to the unpredictability of work dynamic levels. Heightened levels of error anticipation are likely to yield more error detection because individuals allocate attentional resources to monitor their own work performance in such situations (Zhao & Olivera, 2006). For example, anesthesiologists anticipate errors the most at the beginning of anesthesia because they consider it as the most dangerous phase regardless of anesthesia type. Therefore, they start anesthesia with a heightened awareness of the possibility of committing errors. Unlike anesthesia, however, work dynamics of real world nursing units are likely to be random, and it is hard to predict when the work dynamics will wax and wane. Therefore, when nurses are confronted with highly dynamic work situations, they may be hard at work trying to finish the job at hand and may not have time to think about and get ready for potential errors.
Nurses’ education had a curvilinear relationship with medication errors. This finding suggests that there may be an optimal staffing level of BSN-prepared nurses for patient safety outcomes. Finding adequate levels of BSN-prepared nurses and the best amount of RNs will be important in future nurse staffing research on patient safety.
Limitations
The data for this study were collected in 2003 and 2004, so the results of this study may not reflect the current reality of hospital nursing units. However, medication error rates have not changed much, and more importantly, learning climate, which is rooted in the organization’s value system, is not likely to be altered in a short period of time. Another limitation relates to the use of incident reports. Studies have found that incident reports have low sensitivity and detect only a very small number of errors compared to chart review or observation methods because of a potential reporting bias problem (Flynn, Barker, Pepper, Bates, & Mikeal, 2002; Jha et al., 1998). However, learning climate is likely to be correlated more highly with reporting when errors are not severe than when they are. Given the definition of a severe medication error–one that requires additional attention–reporting bias is less likely to be an issue in the current study. Another limitation relates to the design of this study. Although data were collected in a temporal order (i.e., independent variables were collected prior to dependent variables), the design does not eliminate the possibility of reverse causality, or so called endogeneity problems. For example, it is not clear whether favorable work conditions (i.e., high RN mix, high proportion of BSN-prepared nurses) contribute to fewer medication errors or whether a previous history of frequent medication errors has led a nursing unit to develop error-preventing work conditions. Similarly, it is possible that nurses on units with frequent previous episodes of medication errors decided to engage in creating a positive learning climate. Finally, although the organizational learning model emphasizes the importance of leadership’s strong commitment to patient safety as a key to successfully creating a positive learning climate, the role of leadership was not examined. The inclusion of a measure of leadership in future research would improve the conceptual model used.
Future Research
The circumstances leading to a learning climate in healthcare organizations should be studied. It is well-known that RNs are costly; the national hourly median wage of RNs in 2008 was $30.03 (U.S. Bureau of Labor Statistics, 2008). It may not be feasible for many hospitals to increase their percentages of RNs to reduce medication errors. However, especially for nursing units with fewer RNs in the nurse mix or those experiencing frequent medication errors, it might be worth investigating how improving the learning climate may reduce presumed negative effects of low staffing levels. For example, it will be important to see if a nurse manager’s orientation to error influences the creation of a positive learning climate. Further, support for employee participation and democratization, which opens communication channels, may influence organizational learning. Second, nurse staffing studies have been focused on finding one-to-one associations between various nurse staffing measures and patient outcomes. However, a nurse’s quality that influences patient outcomes is multidimensional and nurse managers need to weigh multiple factors to create the best possible mix of nurses. Therefore, future research should be focused on finding the best combination of skill mix (e.g., percentage of RNs, education level, experience) that yields best patient outcomes.
Acknowledgments
This study was funded by the National Institute for Nursing Research (Grant #5R01 NR003149), the American Nurses Foundation (2006 Southern Nursing Research Society/ANF scholar), and Sigma Theta Tau International, Alpha Alpha Chapter Small Research Grant Program.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
YunKyung Chang, Postdoctoral Fellow, University of North Carolina at Chapel Hill School of Nursing, Chapel Hill, North Carolina.
Barbara Mark, Sarah Russell Frances Distinguished Professor, University of North Carolina at Chapel Hill School of Nursing, Chapel Hill, North Carolina.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Argote L, Ingram P, Levine JM, Moreland RL. Knowledge transfer in organizations: Learning from the experience of others. Organizational Behavior and Human Decision Processes. 2000;82(1):1–8. [Google Scholar]
- Berta WB, Baker R. Factors that impact the transfer and retention of best practices for reducing error in hospitals. Health Care Management Review. 2004;29(2):90–97. doi: 10.1097/00004010-200404000-00002. [DOI] [PubMed] [Google Scholar]
- Blegen MA, Goode CJ, Reed L. Nurse staffing and patient outcomes. Nursing Research. 1998;47(1):43–50. doi: 10.1097/00006199-199801000-00008. [DOI] [PubMed] [Google Scholar]
- Bliese PD. Within-group agreement, non-independence, and reliability: Implications for data aggregation and analysis. In: Klein KJ, Kozlowski SW, editors. Multilevel theory, research, and methods in organizations: Foundations, extensions, and new directions. San Francisco, CA: Jossey-Bass; 2000. pp. 349–381. [Google Scholar]
- Chang YK, Mark BA. Antecedents of severe and nonsevere medication errors. Journal of Nursing Scholarship. 2009;41(1):70–78. doi: 10.1111/j.1547-5069.2009.01253.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chuang YT, Ginsburg L, Berta WB. Learning from preventable adverse events in health care organizations: Development of a multilevel model of learning and propositions. Health Care Management Review. 2007;32(4):330–340. doi: 10.1097/01.HMR.0000296790.39128.20. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied regression/correlation analysis for the behavioral sciences. 3rd ed. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Dean B, Schachter M, Vincent C, Barber N. Causes of prescribing errors in hospital inpatients: A prospective study. Lancet. 2002;359(9315):1373–1378. doi: 10.1016/S0140-6736(02)08350-2. [DOI] [PubMed] [Google Scholar]
- DeJoy DM, Gershon RRM, Schaffer BS. Safety climate: Assessing management and organizational influences on safety. Professional Safety. 2004;49(7):50–57. [Google Scholar]
- Department of Health. An organization with a memory: Report of an expert group on learning from adverse events in the NHS. London, England: The Stationery Office; 2000. [Google Scholar]
- Edmondson AC. Learning from failure in health care: Frequent opportunities, pervasive barriers. Quality & Safety in Health Care. 2004;13 suppl_2:ii3–ii9. doi: 10.1136/qshc.2003.009597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenhauer LA, Hurley AC, Dolan N. Nurses' reported thinking during medication administration. Journal of Nursing Scholarship. 2007;39(1):82–87. doi: 10.1111/j.1547-5069.2007.00148.x. [DOI] [PubMed] [Google Scholar]
- Elfering A, Semmer NK, Grebner S. Work stress and patient safety: Observer-rated work stressors as predictors of characteristics of safety-related events reported by young nurses. Ergonomics. 2006;49(5–6):457–469. doi: 10.1080/00140130600568451. [DOI] [PubMed] [Google Scholar]
- Evans RS, Lloyd JF, Stoddard GJ, Nebeker JR, Samore MH. Risk factors for adverse drug events: A 10-year analysis. The Annals of Pharmacotherapy. 2005;39(7–8):1161–1168. doi: 10.1345/aph.1E642. [DOI] [PubMed] [Google Scholar]
- Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. American Journal of Health-System Pharmacy. 2002;59(5):436–446. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, et al. Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: A nine-hospital study of surgical patients. Medical Care. 2000;38(8):807–819. doi: 10.1097/00005650-200008000-00005. [DOI] [PubMed] [Google Scholar]
- Health and Safety Commission. Organising for safety: Third report of the ACSNI (Advisory Committee on the Safety of Nuclear Installations) study group on human factors. Sudbury, England: HSE Books; 1993. [Google Scholar]
- Heimbeck D, Frese M, Sonnentag S, Keith N. Integrating errors into the training process: the function of error management instructions and the role of goal orientation. Personnel Psychology. 2003;56(2):333–361. [Google Scholar]
- Institute of Medicine. Preventing medication errors. Washington, DC: National Academy Press; 2006. [Google Scholar]
- James LR, Demaree RG, Wolf G. Estimating within-group interrater reliability with and without response bias. Journal of Applied Psychology. 1984;69(1):85–98. [Google Scholar]
- Jha AK, Kuperman GJ, Teich JM, Leape L, Shea B, Rittenberg E, et al. Identifying adverse drug events: Development of a computer-based monitor and comparison with chart review and stimulated voluntary report. Journal of the American Medical Information Association. 1998;5(3):305–314. doi: 10.1136/jamia.1998.0050305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: A systematic review. Archives of Internal Medicine. 2003;163(12):1409–1416. doi: 10.1001/archinte.163.12.1409. [DOI] [PubMed] [Google Scholar]
- Keith N, Frese M. Self-regulation in error management training: emotion control and metacognition as mediators of performance effects. Journal of Applied Psychology. 2005;90(4):677–691. doi: 10.1037/0021-9010.90.4.677. [DOI] [PubMed] [Google Scholar]
- Klein KJ, Kozlowski SWJ. From micro to meso: Critical steps in conceptualizing and conducting multilevel research. Organizational Research Methods. 2000;3(3):211–236. [Google Scholar]
- Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: Building a safer health system. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- Leape LL. Error in medicine. JAMA. 1994;272(23):1851–1857. [PubMed] [Google Scholar]
- Manojlovich M, DeCicco B. Healthy work environments, nurse-physician communication, and patients’ outcomes. American Journal of Critical Care. 2007;16(6):536–543. [PubMed] [Google Scholar]
- March JG. Exploration and exploitation in organizational learning. Organization Science. 1991;2(1):71–87. [Google Scholar]
- Mark BA, Hughes LC, Belyea M, Chang Y, Hofmann D, Jones CB, et al. Does safety climate moderate the influence of staffing adequacy and work conditions on nurse injuries? Journal of Safety Research. 2007;38(4):431–446. doi: 10.1016/j.jsr.2007.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGillis Hall L, Doran D, Pink GH. Nurse staffing models, nursing hours, and patient safety outcomes. The Journal of Nursing Administration. 2004;34(1):41–45. doi: 10.1097/00005110-200401000-00009. [DOI] [PubMed] [Google Scholar]
- Minick P, Dilorio C, Mitchell P, Dudley W. The early recognition of patient problems: Developing an instrument reflecting nursing expertise. 2000. Unpublished manuscript. [Google Scholar]
- Minick P, Harvey S. The early recognition of patient problems among medical-surgical nurses. Medsurg Nursing. 2003;12(5):291–297. [PubMed] [Google Scholar]
- Oren E, Shaffer ER, Guglielmo BJ. Impact of emerging technologies on medication errors and adverse drug events. American Journal of Health-System Pharmacy. 2003;60(14):1447–1458. doi: 10.1093/ajhp/60.14.1447. [DOI] [PubMed] [Google Scholar]
- Probst TM. Safety and insecurity: Exploring the moderating effect of organizational safety climate. Journal of Occupational Health Psychology. 2004;9(1):3–10. doi: 10.1037/1076-8998.9.1.3. [DOI] [PubMed] [Google Scholar]
- Reason JT. Human error. Cambridge, England: Cambridge University Press; 1990. [Google Scholar]
- Rivard PE, Rosen AK, Carroll JS. Enhancing patient safety through organizational learning: Are patient safety indicators a step in the right direction? Health Services Research. 2006;41(4 Pt. 2):1633–1653. doi: 10.1111/j.1475-6773.2006.00569.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rybowiak V, Garst H, Frese M, Batinic B. Error orientation questionnaire (EOQ): Reliability, validity, and different language equivalence. Journal of Organizational Behavior. 1999;20(4):527–547. [Google Scholar]
- Salyer J. Development and psychometric evaluation of an instrument to measure staff nurses’ perception of uncertainty in the hospital environment. Journal of Nursing Measurement. 1996;4(1):33–48. [PubMed] [Google Scholar]
- Seago JA, Williamson A, Atwood C. Longitudinal analyses of nurse staffing and patient outcomes: More about failure to rescue. The Journal of Nursing Administration. 2006;36(1):13–21. doi: 10.1097/00005110-200601000-00005. [DOI] [PubMed] [Google Scholar]
- Tucker AL, Edmondson AC, Spear S. Academy of management proceedings. Birmingham, AL: Author; 2001. Front-line problem solving: The responses of hospital nurses to work system failures; p. C1. [Google Scholar]
- United States Bureau of Labor Statistics. Occupational employment statistics. 2008 Available from http://data.bls.gov/
- van Dyck C, Frese M, Baer M, Sonnentag S. Organizational error management culture and its impact on performance: A two-study replication. Journal of Applied Psychology. 2005;90(6):1228–1240. doi: 10.1037/0021-9010.90.6.1228. [DOI] [PubMed] [Google Scholar]
- Zhao B, Olivera F. Error reporting in organizations. Academy of Management Review. 2006;31(4):1012–1030. [Google Scholar]