Abstract
BACKGROUND
The purpose of this study is to determine the clinical outcomes associated with Alternate Listing Transplantation (ALT) strategies.
METHODS
UNOS provided de-identified patient-level data. Primary analysis focused on patients undergoing heart transplantation between January 1, 1999 to December 31, 2005 (n=13,024). HR criteria included age [gt] 65yo, retransplantation, HepC+, HIV+, CrCI [It] 30 ml/min, DM with PVD, DM with Crcl [It] 40 ml/min. MD criteria included age [gt] 55yo, DM, HIV+, HepC+, EF [It] 45%, and dononrecipient weight [It] 0.7.
RESULTS
Survival in the standard transplant group was better than all other groups (p<0.001). With a median survival of 5.2 years, long-term survival was worst in the alternate listing transplant group (p<0.001). The standard transplant group also had the best transplant hospitalization outcomes, having the lowest incidence of in-hospital infection and dialysis (p<0.001). Alternate listing transplantations had the highest incidence of in-hospital infection (p≤0.001). As expected, LOS for the transplant hospitalization was also shortest for standard list transplants, (p<0.001).
CONCLUSIONS
Pairing high-risk recipients with marginal donors is associated with greater morbidity and resource utilization compared with standard recipients and donors. Nevertheless, this strategy offers 5 years or more of additional survival to patients who otherwise would be expected to live 1 year or less. Therefore, ALT strategies appear to be a reasonable approach to extending the benefits of transplantation in the heart failure population. However, further studies examining the costs and quality of life related to this approach are needed.
INTRODUCTION
There is a critical scarcity of organs available for transplantation. Of an estimated 60,000 potential beneficiaries, fewer than 2,500 undergo cardiac transplantation annually. Given the significant disparities between the supply and demand for transplantable organs, strategies designed to offer transplantation to a greater number of candidates have the potential to provide substantial benefits.
In order to achieve this goal, some centers have advocated for the adoption of Alternate Listing Transplantation (ALT). Under this strategy, high-risk (HR) candidates who fail to meet standard criteria for transplantation are considered for “marginal donor” (MD) organs—these organs do not meet standard donor criteria and would likely otherwise be left unused.
Alternate listing, however, often means matching the highest risk recipients with poor quality donor organs; a phenomenon that may be associated with significant morbidity. A number of small studies have described outcomes using this strategy [1–5]. These studies have largely found that ALT provides good long-term survival compared to that expected from end stage heart failure patients who do not undergo transplantation. However, the studies described experience at only a single center and were limited in size and duration of follow-up. Therefore, it remains unclear whether the reported outcomes support continued endorsement of alternate list strategies.
The purpose of this study is to measure clinical outcomes associated with alternate listing transplantation. This study improves on previous studies by analyzing the national experience with heart transplantation by using the United Network for Organ Sharing (UNOS) database.
METHODS
Data Collection
Use of this data is consistent with the regulations of our university’s Institutional Review Board and the UNOS’ Data Use Agreement. The Standard Transplant Analysis and Research Dataset was provided by UNOS (data source #021606-4) and is de-identified patient-level data. It contains information collected from the UNetsm forms, including the Transplant Candidate Registration form, the Transplant Recipient Registration form, and the Transplant Recipient Follow-up form. These data are the basis of the UNOS Thoracic Registry.
Study Population
All recipients aged 18 years and older undergoing heart transplantation between January 1, 1999 to December 31, 2005 were included in the study population. Follow-up data was provided through February 27, 2006. Patients were followed from the date of transplant until death, re-transplantation (cardiac), or date of last known follow-up which was the last day of follow-up data provided by UNOS. Mean follow-up time was 2.40 ± 1.97 years.
Alternate Listing Criteria
A systematic literature review was conducted of previous studies and professional committee guidelines [6–8] to determine which characteristics and thresholds would be included in the definitions for high-risk recipients and marginal donors. Patients with any of the following conditions were classified as high-risk recipients: advanced age (>65years); retransplantation; hepatitis C+; HIV+; creatinine clearance (CrCI) < 30ml/min; diabetes complicated by peripheral vascular disease (PVD), chronic renal failure (CRF) defined as CrCI < 40ml/min, or history of cerebrovascular accidents (CVA). Marginal donors were those that met at least one of the following characteristics: advanced age (>55years), cocaine or IV drug use, diabetes, hepatitis C seropositivity, ejection fraction < 45%, and a donor/recipient size mismatch (dononrecipient weight ratio < 0.7). Due to the limitations of registry data, which only provides data at limited timepoints, some criteria such as high pressor/inotrope requirements in donors and severe pulmonary hypertension in recipients were not included in the high-risk definitions. Paired recipients and donors were then stratified by recipient and donor characteristics into 4 categories: Standard recipients paired with standard donors (STD), standard recipients paired with marginal donors (SR:MD), high-risk recipients paired with standard donors (HR:SD), and high-risk recipients paired with marginal donors (ALT).
Outcome Measures
The primary outcomes measures were actuarial post-transplant survival as expressed in years and incidence rate of death (IRD) per 100 patient years with 95% confidence intervals. Other outcomes of interest included in-hospital morbidity, as measured by incidence of retransplantation for primary graft failure (PGF), stroke, infection and need for dialysis, as well as length of stay during the transplant hospitalization. Long-term outcomes measures included diabetes mellitus-incidence rate (DM-IR), transplant coronary artery disease-incidence rate (TCAD-IR), and post-transplantation chronic dialysis-incidence rate (CD-IR).
Data Analysis
Continuous variables were reported as means ± standard deviation and compared using the Student’s t-test. To compare categorical variables, the chi-square test was used. The conventional p-value of 0.05 or less was used to determine level of statistical significance. All reported p-values are two-sided. The hazard ratio and 95% confidence interval were reported for each factor. All data was analyzed using a statistical software package, Stata 9 (Stata Corp, College Station, TX).
The primary outcome measure was survival reported as median survival and incidence rate (IR) of death per 100 patient-years with 95% confidence intervals. Kaplan-Meier analysis with log-rank test was used for time to event analysis for actuarial survival, as well as TCAD-IR, CD-IR, and DM-IR. For survival analysis, outcome of interest was death or retransplant, which ever came first. Patients lost to follow-up or alive on February 27, 2006 were censored at the date of last known follow-up. In order to assess the impact of recipient and donor pairing on early and late mortality, the incidence rate of death per 100 patient-years was calculated at multiple time intervals (<30 days, 30dy–1yr, 1–2yrs, 2–5yrs).
RESULTS
Study population
Analysis included 13,024 (Table 1) recipients stratified by recipient and donor characteristics into 4 categories: STD (n=9,642, 74.0%), SR:MD (970, 7.5%), HR: SD (2065, 15.9%), and ALT (347, 2.7%).
Table 1.
Patient Characteristics for all heart transplant recipients aged 18 (1995–2005)
| STD
|
SR:MD
|
HR:SD
|
ALT
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| Heart Transplant Recipients | n | 9642 | 74.0% | 970 | 7.4% | 2065 | 15.9% | 347 | 2.7% |
| Mean Age | years | 50.0 | ±11.6 | 51.8 | ±10.5 | 58.8 | ±11.7 | 60.6 | ±10.7 |
| Male Sex | n | 7249 | 75.18% | 751 | 77.4% | 1598 | 77.4% | 285 | 82.1% |
| Cause of Heart Failure | |||||||||
| Ischemic | n | 4338 | 45.0% | 486 | 50.1% | 1019 | 49.3% | 147 | 42.4% |
| Dilated | n | 4368 | 45.3% | 415 | 42.8% | 528 | 25.6% | 75 | 21.6% |
| Other | n | 936 | 9.7% | 69 | 7.1% | 518 | 25.1% | 125 | 36.0% |
| Status at Transplant | |||||||||
| 1 | n | 6973 | 72.3% | 238 | 24.5% | 536 | 26.0% | 107 | 30.8% |
| 2 | n | 2651 | 27.5% | 236 | 24.3% | 534 | 25.9% | 105 | 30.3% |
| Life Support at Transplant | |||||||||
| Left Ventricular Assist Device | n | 2023 | 21.0% | 207 | 21.3% | 361 | 17.5% | 60 | 17.3% |
| Intra-aortic Balloon Pump | n | 470 | 4.9% | 52 | 5.4% | 158 | 7.7% | 32 | 9.2% |
| Intubated | n | 235 | 2.4% | 46 | 4.7% | 116 | 5.6% | 26 | 7.5% |
SR:SD=standard recipient paired with standard donor, SR:MD=standard recipient paired with marginal donor, HR:SD=high-risk recipient paired with standard donor, HR:MD=high risk recipient paired with marginal donor.
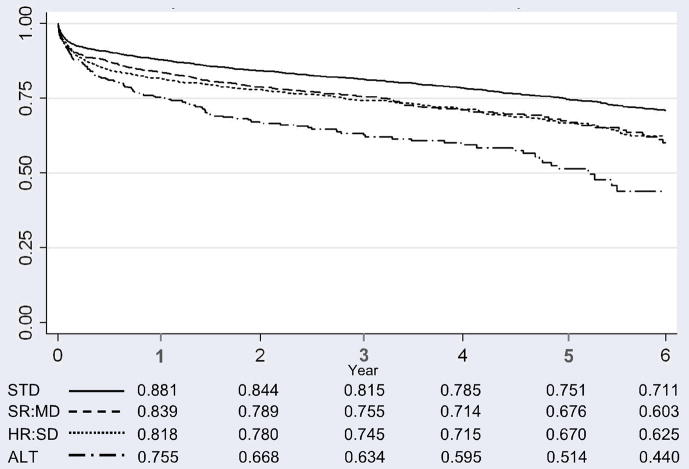
Survival (Figure 1)
Figure 1.
Kaplan Meier Survival Analysis Following Transplantation by Transplant Group
STD=standard recipient paired with standard donor, SR:MD=standard recipient paired with marginal donor, HR:SD=high- risk recipient paired with standard donor, ALT=high risk recipient paired with marginal donor
As expected, survival in the standard transplant group was better than all other groups (p<0.001). Although 30-day survival was similar between all of the non-standard groups (NR:MD, HR:ND, ALT), survival was worst in the ALT group by 1 year (p<0.001). Survival for the STD and ALT groups were, respectively, 95.6% and 92.0% at 30-days and 75.1% and 51.4% at 5 years. Survival was similar between the intermediate risk groups (SR:MD and HR:ND) in both the short and long-term (p=0.80). Survival for the SR:MD and HR:ND groups were, respectively, 92.4% and 93.3% at 30-days and 67.6% and 67.0% at 5 years.
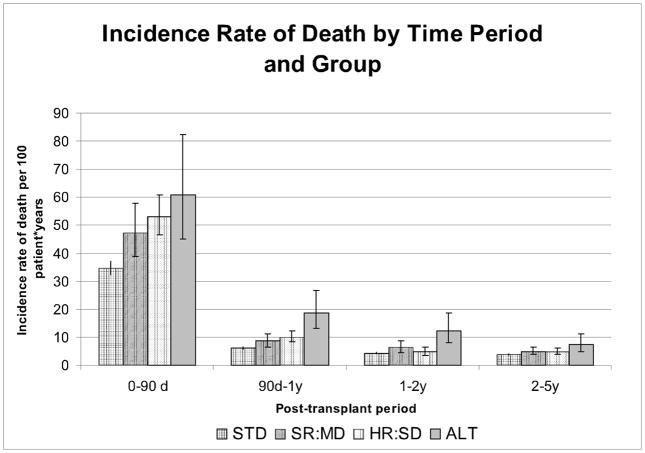
Figure 2 illustrates the IRD during various time periods following transplantation by group. Not surprisingly, in the first 90 days following transplantation the standard group had a significantly lower IRD than the other groups. However, as time passes these differences lessen. In fact, after the first year post transplant, there is no statistical difference between the standard group and the intermediate risk groups, though IRD remains higher in the alternate list group. At years 2–5 there are no differences among these intermediate risk groups and ALT; though ALT remains slightly higher than the standard group
Figure 2.
Incidence rate of death by time period and group
STD=standard recipient paired with standard donor, SR:MD=standard recipient paired with marginal donor, HR:SD=high- risk recipient paired with standard donor, ALT=high risk recipient paired with marginal donor;
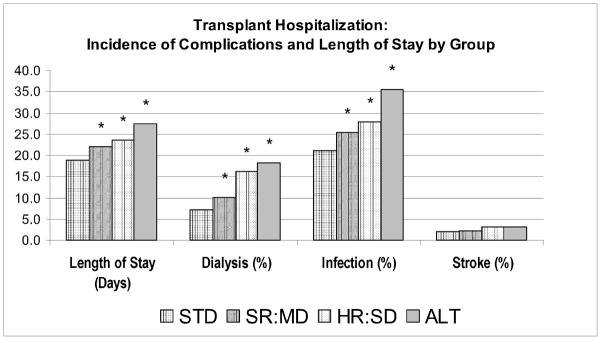
Transplant Hospitalization Adverse Events (Figure 3)
Figure 3.
Transplant hospitalization: length of stay and incidence of complications by group.
*p value<0.05 when compared to the STD group; STD=standard recipient paired with standard donor, SR:MD=standard recipient paired with marginal donor, HR:SD=high-risk recipient paired with standard donor, ALT=high risk recipient paired with marginal donor; Retxp for PGF=retransplantation for primary graft failure.
Standard list transplantations had the lowest incidence of infection (21.1%) and dialysis (7.1%) during the transplant hospitalization (p<0.001). Alternate listing transplantations had the highest incidence of infection, 35.4% (p≤0.001). Although dialysis rates in ALT transplantations were greater than either standard recipient group, they were similar to high-risk recipients who received normal hearts, 16.1% (p=0.27). There were no differences in incidence of stroke between the groups.
Utilization (Figure 3)
Length of stay was used as a proxy for health care resource utilization (Table 2). As expected, length of stay for the transplant hospitalization was the shortest for standard list transplants, 18.8 days (p<0.001). Length of stay for the ALT recipients (27.4 days) was longer then either of the normal recipient transplant groups (p<0.03), however, it was comparable to high-risk recipients who received normal hearts, 23.6 days (p=0.06).
Long-term Complications of Transplantation (Figure 4)
Figure 4.
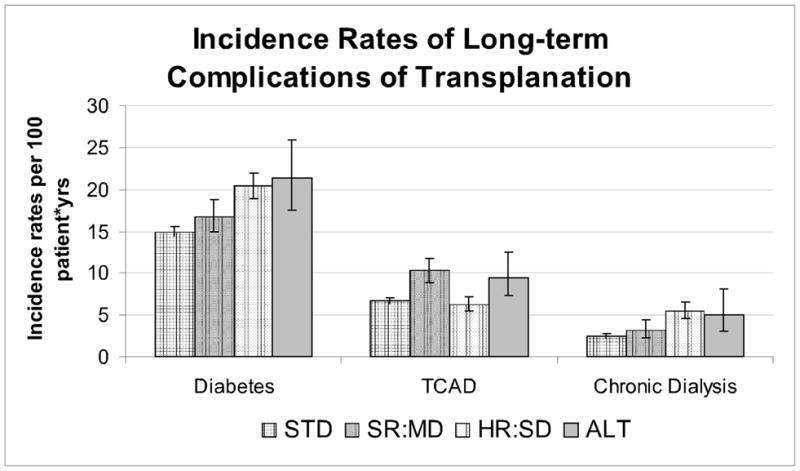
Incidence rates of long-term complications of transplantation.
TCAD=transplant coronary artery disease; STD=standard recipient paired with standard donor, SR:MD=standard recipient paired with marginal donor, HR:SD=high-risk recipient paired with standard donor, ALT=high risk recipient paired with marginal donor
The chronic dialysis incidence rate of the standard group (2.5, 2.2–2.9) was better then both the high risk recipient transplant groups (HR:ND 5.5, 4.5–6.6; ALT 5.0, 3.1–8.0), although no different then NR:MD (3.2, 2.3–4.4). The TCAD incidence rates in the standard population (6.7, 6.3–7.0) was lower then both transplant groups who received marginal donor hearts (NR:MD 10.3., 8.9–11.8; ALT 9.5, 7.3–12.5), but the same as high-risk patients who received a normal donor heart (6.3, 5.5–7.2). The diabetes incidence rate in the standard group (14.9, 14.3–15.5) was lower than both the high-risk recipient groups (HR:ND 20.4, 18.9–22.2; ALT 17.5, 17.5–25.9), but the same as NR:MD (16.7, 14.9–18.7).
COMMENT
The burden related to heart failure continues to grow. Unfortunately, treatment options remain limited. Medical management ameliorates symptoms and prolongs survival in mild to moderate heart failure, however, it does not treat the underlying pathology; therefore, with medical therapy alone, disease remains progressive and typically leads to death [9–10]. Left ventricular assist devices offer a promising alternative, but long-term survival remains limited and adverse events are substantial. Biological therapies for cardiac disease, including gene and stem cell therapies, are in the experimental phases. Heart transplant remains the gold standard in the treatment of end-stage heart failure; however, its use is limited by the critical scarcity of donor organs. Therefore achieving additional benefit from this therapy is predicated on expanding the donor pool.
Alternate waiting list strategies have been promoted as a means to maximize the use of so-called “marginal donor hearts,” and thereby offer the benefit of transplantation to a greater number of candidates. Under this strategy, “high-risk” patients who fail to meet standard criteria for transplantation are considered candidates for organs that would otherwise have been discarded. Paradoxically, as part of this strategy the highest risk recipients are matched with higher-risk donor organs. This poses a number of clinical, ethical, and policy concerns.
Findings here demonstrate that standard recipients paired with standard donors realized the best survival, and high-risk recipients paired with marginal donors had the worst survival. Compared with the standard group, the alternate list group had significantly worse survival. There was a step wise decrease in survival moving from standard to intermediate to alternate list, but survival was similar between the intermediate risk pairs (HR:ND and MR:SD).
Matching high-risk recipients and marginal donors offers a median survival of greater than 5 years to patients. Because this observed survival is significantly less than the median survival of the overall transplant population, it has been argued that it is unethical to offer marginal donor organs for transplantation. However, given a life expectancy of 6 to 12 months among these patients in the absence of heart transplantation [11], matching high-risk recipients with marginal donors should be considered as a treatment option.
When considering survival benefits of standard treatments for other potentially terminal diseases, such as surgical resection for pancreatic or esophageal cancer, where median survival for patients is less than 18 months, alternate listing provides significantly greater survival benefit [12, 13]. Furthermore, in the context of thoracic organ transplantation, providing marginal donor hearts to high-risk recipients offers survival similar to that provided by lung transplantation [14].
Post-transplant morbidity and resource utilization
Additional findings here demonstrate that pairing high-risk recipients with marginal donor hearts is associated with greater morbidity and resource utilization compared with standard recipients and donors. Interestingly, the development of diabetes and the need for chronic dialysis appear to be correlated with high-risk recipient characteristics, while development of transplant coronary artery disease appears to be related to poor donor organ quality.
Given the constraints of our healthcare system, and its finite resources, additional studies examining the cost-effectiveness of this strategy are required to determine the place of this strategy along side other heart failure therapies.
Future studies
These findings suggest that developing a national, standardized mechanism for ALT listing, as has occurred in other organ systems, including liver and kidney, may further maximize the use of potential donor organs and expand the benefit of transplantation. Furthermore, this strategy may provide secondary benefit by risk-adjusting for recipients and transplant centers as we shift to stricter quality oversight and pay for performance, in order to avoid penalizing centers that transplant higher-risk patients.
However, additional studies are needed before a stratified system that pairs recipients and donors by risk can be appropriately employed. First, future studies should determine methods to objectively define high-risk recipient and marginal donor criteria. Second, although the favorable survival described in this analysis supports alternate listing as a clinically effective treatment strategy for patients who might not otherwise be candidates for transplantation, the impact of quality of life and the cost implications of this additional survival still need to be evaluated.
Limitations
This study suffers from a number of limitations. First, UNOS does not formally designate recipients as alternate list candidates. Therefore, outcomes in high-risk patients paired with marginal donors were used as a conservative proxy for alternate list transplantation outcomes. However, considering reports in previous studies that approximately one-quarter of alternate list recipients receive organs from standard donors, this current analysis may underestimate survival under ALT [2].
Second, patient registries often suffer from variability in data entry. However, fields contained within this database were generally well populated with a 95–99% data entry rate for the majority of variables. Though the UNOS reporting system provided definitions for variables in data guidelines, definitions may vary by center.
CONCLUSION AND IMPLICATIONS
In conclusion, alternate listing is associated with greater morbidity, higher resource utilization and diminished survival compared with standard list transplantations. However, end-stage heart failure is a terminal disease; life expectancy among these high-risk candidates is 6 to 12 months in the absence of heart transplantation. Transplantation within the alternate risk group conferred a median survival of more than 5 years.
These findings suggest that developing a national, standardized mechanism for ALT listing, as has occurred in other organ systems, including liver and kidney, may further maximize the use of potential donor organs and expand the benefit of transplantation. However, further studies examining the implications of costs and quality of life related to this approach are needed.
Acknowledgments
We thank UNOS for supplying this data and Katarina Anderson, PhD, for her assistance with our analysis. This work was supported in part by Health Resources and Services Administration contract 231-00-0115. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government. This work was supported in part by NIH Training Grant T32-HL007854-11&12 (Dr. George).
Abbreviations Table
- ALT
Alternate Listing Transplantation
- CVA
Cerebrovascular Accidents
- CrCI
Creatinine Clearance
- DM
Diabetes Mellitus
- EF
Ejection Fraction
- HF
Heart Failure
- HR
High-risk Recipients
- MD
“Marginal” Donor Organs
- PVD
Peripheral Vascular Disease
- UNOS
United Network for Organ Sharing
- STD
Standard Recipients paired with Standard Donors
- SR:MD
Standard Recipients paired with Marginal Donors
- HR:SD
High-risk Recipients paired with Standard Donors
- ALT
High-risk Recipients paired with Marginal Donors
- RF-IR
Chronic Dialysis-Incidence Rate
- DM-IR
Diabetes-Incidence Rate
- TCAD-IR
Transplant Coronary Artery Disease-Incidence Rate
Footnotes
Meeting Presentation
44th Annual Meeting of the Society of Thoracic Surgeons, 2008, Fort Lauderdale, Florida
References
- 1.Felker GM, Milano CA, Yager JE, Hernandez AF, Blue L, Higginbotham MB, Lodge AJ, Russell SD. Outcomes with an alternate list strategy for heart transplantation. J Heart Lung Transplant. 2005 Nov;24(11):1781–6. doi: 10.1016/j.healun.2005.03.014. Epub 2005 Aug 8. [DOI] [PubMed] [Google Scholar]
- 2.Chen JM, Russo MJ, Hammond KM, Mancini DM, Kherani AR, Fal JM, Mazzeo PA, Pinney SP, Edwards NM, Naka Y. Alternate waiting list strategies for heart transplantation maximize donor organ utilization. Ann Thorac Surg. 2005 Jul;80(1):224–8. doi: 10.1016/j.athoracsur.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 3.Laks H, Marelli D, Fonarow GC, Hamilton MA, Ardehali A, Moriguchi JD, Bresson J, Gjertson D, Kobashigawa JA UCLA Heart Tranplant Group. Use of two recipient lists for adults requiring heart transplantation. J Thorac Cardiovasc Surg. 2003 Jan;125(1):49–59. doi: 10.1067/mtc.2003.62. [DOI] [PubMed] [Google Scholar]
- 4.Kobashigawa JA, Laks H, Wu G, Patel J, Moriguchi J, Hamilton M, Fonarow G, Fishbein M, Ardehali A. The University of California at Los Angeles heart transplantation experience. Clin Transpl. 2005:173–85. [PubMed] [Google Scholar]
- 5.Laks H, Scholl FG, Drinkwater DC, Blitz A, Hamilton M, Moriguchi J, Fonarow G, Kobashigawa J. The alternate recipient list for heart transplantation: does it work? J Heart Lung Transplant. 1997 Jul;16(7):735–42. [PubMed] [Google Scholar]
- 6.Zaroff JG, Rosengard BR, Armstrong WF, Babcock WD, D’Alessandro A, Dec GW, Edwards NM, Higgins RS, Jeevanandum V, Kauffman M, Kirklin JK, Large SR, Marelli D, Peterson TS, Ring WS, Robbins RC, Russell SD, Taylor DO, Van Bakel A, Wallwork J, Young JB. Consensus conference report: maximizing use of organs recovered from the cadaver donor: cardiac recommendations, March 28–29, 2001, Crystal City, Va. Circulation. 2002 Aug 13;106(7):836–41. doi: 10.1161/01.cir.0000025587.40373.75. [DOI] [PubMed] [Google Scholar]
- 7.Miller LW. Listing Criteria for Cardiac Translantation: Result of an American Society of Transplant Physicians-National Institutes of Health Conference. Transplantation. 1998 Oct 15;106(7):947–951. doi: 10.1097/00007890-199810150-00032. [DOI] [PubMed] [Google Scholar]
- 8.Mehra MR, Kobashigawa J, Starling R, Russell S, Uber PA, Parameshwar J, Mohacsi P, Augustine S, Aaronson K, Barr M. Listing Criteria for Heart Transplantation: International Society for Heart and Lung Transplantation Guidelines for the Care of Cardiac Transplant Candidates—2006. J Heart Lung Transplant. 2006 Sep;24(9):1024–1042. doi: 10.1016/j.healun.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 9.Greenberg BH. The medical management of chronic congestive heart failure. In: Hosenpud JD, Greenberg BH, editors. Congestive Heart Failure. 2. Lippincott, Williams and Wilkins; Philadelphia: 2000. pp. 673–95. [Google Scholar]
- 10.Cohn JN. The management of heart failure. In: Willerson JT, Cohn JN, editors. Cardiovascular Medicine. Churchill Livingstone; Philadelphia: pp. 1165–83. [Google Scholar]
- 11.Russo MJ, Gelijns A, Renlund D, et al. The cost of medical management in end-stage heart failure: an analysis of the REMATCH trial. American Heart Association; Chicago, IL: 2006. [Google Scholar]
- 12.Cleary SP, Gryfe R, Guindi M, Greig P, Smith L, Mackenzie R, Strasberg S, Hanna S, Taylor B, Langer B, Gallinger S. Prognostic factors in resected pancreatic adenocarcinoma: analysis of actual 5-year survivors. J Am Coll Surg. 2004 May;198(5):722–31. doi: 10.1016/j.jamcollsurg.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Enzinger PC, Mayer RJ. Esophageal cancer. N Engl J Med. 2003;349:2241. doi: 10.1056/NEJMra035010. [DOI] [PubMed] [Google Scholar]
- 14.Russo MJ, Sternberg Dl, Hong KN, Sorabella RA, Moskowitz AJ, Gelijns AC, Wilt JR, D’Ovidio F, Kawut SM, Arcasoy SM, Sonett JR. Postlung transplant survival is equivalent regardless of cytomegalovirus match status. Ann Thorac Surg. 2007 Oct;84(4):1129–34. doi: 10.1016/j.athoracsur.2007.05.037. discussion 1134–5. [DOI] [PubMed] [Google Scholar]