Abstract
Background
Only one-half of Americans have their blood pressure controlled and there continue to be significant racial differences in blood pressure control. The goal of this study was to examine the effectiveness of two patient-directed interventions designed to improve blood pressure control within white and non-white subgroups (49% African Americans).
Methods
Post-hoc analysis of a 2 by 2 randomized trial with two-year follow-up in 2 university-affiliated primary care clinics. Within white and non-white patients (n=634), four groups were examined: 1) usual care; 2) home blood pressure monitoring (three times per week); 3) tailored behavioral self-management intervention administered via telephone by a nurse every other month; or, 4) a combination of the two interventions.
Results
The overall race by time by treatment group effect suggested differential intervention effects on blood pressure over time for whites and non-whites (systolic blood pressure, p=0.08; diastolic blood pressure, p=0.01). Estimated trajectories indicated that among the 308 whites, there was no significant effect on blood pressure at either 12 or 24 months for any intervention compared to control group. At 12 months, the non-whites (n=328) in all three intervention groups had systolic blood pressure decreases of 5.3–5.7 mm hg compared to usual care (p<0.05). At 24 months, in the combined intervention, non-whites had sustained lower systolic blood pressure as compared to usual care (7.5 mm hg; p<0.02). A similar pattern was observed for diastolic blood pressure.
Conclusion
Combined home blood pressure monitoring and a telephone tailored-behavioral intervention appeared to be particularly effective for improving blood pressure in non-white patients.
Keywords: Hypertension, Lifestyle, Clinical Trial, Self-management, Adherence, Disparities
Introduction
Hypertension affects approximately 75 million individuals in the United States and is an important modifiable risk factor for cardiovascular disease, stroke, and renal disease. 1 In spite of effective therapies, only 50% of patients with hypertension achieve their target blood pressure. 2 Hypertension is particularly burdensome among African Americans;3 African Americans have higher average blood pressures than do whites. 1 The racial differences in hypertension and diseases attributed to hypertension account for 15% of the overall difference in mortality between African Americans and whites.4 Cross-sectional analysis of nationally representative samples of black and white adults who participated in the National Health and Nutrition Examination Survey (NHANES) 1999–2002 and NHANES III conducted in 1988–1994 indicated hypertension prevalence increased significantly from 35.8% to 41.4% among blacks and from 24.3% to 28.1% among whites. Disparity in blood pressure control among treated cases increased, with 59.7% of treated whites and 48.9% of treated blacks reaching blood pressure goal in NHANES III (P<.001).5 Race is an independent predictor of uncontrolled blood pressure even after controlling for important comorbidities such as diabetes. 6, 7 The efficacy of lifestyle interventions for lowering blood pressure is at least as great among African Americans as it is among other racial/ethnic groups. 8 While improving the equity of healthcare is one of the key components of quality improvement, 9 it is unclear which components will reduce the significant disparity between African Americans and whites.
We conducted post-hoc analyses among a racially and economically diverse sample of patients who received primary care for hypertension in two diverse primary care sites in a university health system. The main study findings have been previously published. 10 The current study examines the effectiveness of three interventions compared to usual care on systolic and diastolic blood pressure over 24 months within white and non-white patient subgroups: 1) home blood pressure self-monitoring only, 2) nurse-administered tailored behavior self-management intervention only, and 3) a combination of the home blood pressure monitoring and tailored behavioral intervention.
Methods
Setting
Two university-affiliated general internal medicine clinics in Durham, North Carolina.
Patient Eligibility
Potentially eligible study patients were identified through weekly data extractions from the Duke University Health System’s (DUHS) billing and appointment database for the study primary care clinics. Initial inclusion criteria were: 1) having a diagnosis of hypertension at least 12 months prior to the data pull date (ICD9 code of 401.0, 401.1, or 401.9), 2) being enrolled with a primary care physician at the clinic of interest for at least 12 months, 3) having received a hypertensive medication prescription (in the previous year), 4) having a scheduled non-lab primary care physician appointment during the next 30 days, and 5) residing in one of 32 specified zip codes in the areas surrounding Duke University Health System.
Exclusion criteria applied prior to randomization were: 1) having a diagnosis of dementia, Parkinson’s disease, atrial fibrillation, or end stage renal disease; 2) residing in a nursing home or receiving home health care; 4) being hospitalized for a stroke, heart attack, surgery for blocked arteries or being diagnosed with metastatic cancer in the prior 3 months; 3) poor vision or difficulty hearing on the telephone; 6) difficulty understanding English; 4) participating in another blood pressure study; 5) spouse participating in current study; 6) having an arm circumference >17 inches or wrist circumference > 8.5 inches.
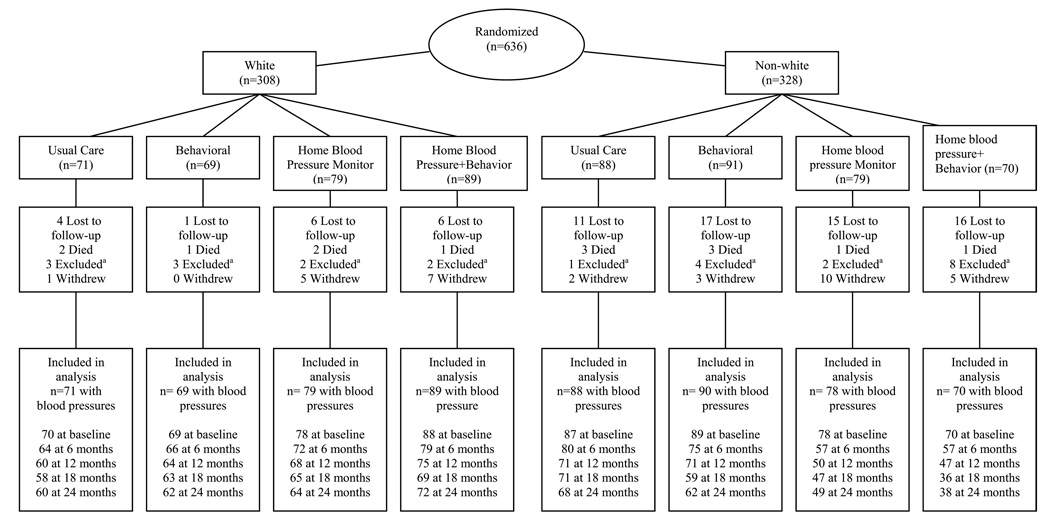
Subjects were considered excluded from the remainder of the study for the following events, and we used their available data up to the point of the following events occurring: 1) no longer receiving most medical care at the Duke clinics; 2) being treated with dialysis in the past 6 months; 3) having received an organ transplant in the past 6 months; 4) residing in a nursing home or receiving home health care; or 5) being diagnosed with pulmonary hypertension in the past 6 months. See Figure 1 for numbers excluded by intervention and race subgroups.
Figure 1.
TCYB Recruitment Flowchart
a No longer receiving care at Duke clinics, receiving dialysis, received organ transplant, residing in nursing home or receiving home health care, no phone, or had pulmonary hypertension
Study members mailed qualifying patients a letter from the patient’s primary care providers providing information about the study and stating that the study team may contact them to participate in the study. Research assistants made weekly screening phone calls to patients from a randomly ordered list of eligible patients with upcoming clinic appointments.
Overall, 2060 letters were mailed to patients inviting them to participate in the study. Research assistants attempted to contact 1728 of potential participants by phone. 656 were enrolled and consented; the remaining 1072 were not consented for the following reasons: had disconnected phones or incorrect phone numbers, were ineligible, declined to participate, and were not included primarily due to scheduling conflicts. Twenty additional patients were excluded at the time of the baseline interview due to arm size (n=18), poor vision (n=1), and not currently taking hypertensive medication (n=1) (see Figure 1 for study flow).
Patient randomization
The remaining 636 eligible patients were randomized to one of four arms: usual care, tailored behavioral phone intervention alone, home blood pressure monitor alone, or both tailored behavioral phone intervention and home blood pressure monitor. Randomization was stratified by enrollment site (two primary care clinics) and literacy status (≥ 9th vs. < 9th grade as determined by the Rapid Estimate of Adult Literacy in Medicine (REALM 11) during the baseline interview. Site and literacy levels were used for stratification purposes because of concerns of potential site differences and prior literature suggesting that literacy may influence self-management interventions. 12, 13 Within each stratum, patients were randomized using consecutively numbered envelopes. Participants were reimbursed $25 for the baseline visit and for each of the four subsequent 6-month blood pressure measurements ($125 total). The study was approved by the Duke Institutional Review Board, and all patients provided written informed consent. There were no study-related adverse events in any intervention group.
Interventions
Tailored Behavior Self-management Intervention
The behavioral intervention was tailored to individuals based on their circumstances and needs. 14 Patient factors targeted in the tailored intervention included perceived risk of hypertension, memory, literacy, social support, patients’ relationships with their health care providers, and side effects of hypertension medication therapy. In addition, the intervention focused on improving adherence to the following five hypertension recommendations: the DASH dietary pattern, 15–18 weight loss in the overweight, 19, 20 reduced sodium intake, 20, 21 regular moderate-intensity physical activity, 22, 23 and moderation of alcohol intake. 24 In the hypertension perceived risk module, African Americans received specific information indicating that as a group, African Americans were almost 2 times more likely to develop high blood pressure than Caucasians; that high blood pressure is generally more severe and occurs 5–10 years earlier in African Americans than other groups; and, that African Americans tend to be more affected by salt intake than other races.
The intervention was delivered by a nurse during bi-monthly telephone calls. All information was presented in an easily understood format with a Flesch-Kincaid readability 25 score of Interventions 003C;9th grade. These encounters included a core group of modules potentially implemented during each call (e.g., medication) plus additional modules activated at specific intervals (e.g., diet, hypertension knowledge).26
The nurse underwent training in aspects of motivational interviewing 27 and in the specific procedures developed for this study. Maintaining or developing motivation and overcoming resistance are key issues for individuals attempting to initiate and change behaviors and these were a focus of the nurse training. To ensure fidelity of the intervention, periodic intervention logs were examined.
Home Blood Pressure Monitoring Intervention
Patients randomized to the home blood pressure monitor interventions received either an Omron HEM 773AC arm monitor (arm circumference 9 –17 inches) or an Omron HEM 637 wrist monitor if arm circumference was > 17 inches and wrist circumference was ≤ 8.5 inches. Patients whose arm and/or wrist sizes did not fit into these categories at baseline were excluded from the study. Research assistants trained patients in proper use of the home blood pressure devices. At each 6-month outcome assessment, patients reviewed their home blood pressure assessment procedures, and were retrained if their procedures were incorrect. Patients were asked to take their blood pressures three times per week, on three separate days at the same time of day, and to record their values in a log. Patients were asked to mail their logs in every 2 months to the study coordinator using study pre-addressed, stamped envelopes.
Combined Intervention
Patients randomized to the combined intervention received a home blood pressure monitor, training on its use, and bi-monthly nurse-administered behavioral self-management intervention. The nurse did not examine home blood pressure values and did not use the home blood pressure values to adjust the intervention.
Usual Care
Patients randomized to usual care received their hypertension care from their primary care provider. They were not provided home blood pressure monitors by the study, nor did they have access to the nurse-administered behavioral intervention.
Study Measures
Baseline
Patient information including age, self-described race, diagnosis of diabetes, and level of education was obtained from patients during a face-to-face baseline interview. Financial status was assessed by asking patients to report whether they had enough money after paying bills for special things; enough to pay the bills, but not purchase extra things; enough money to pay bills by cutting back on things; or difficulty paying bills no matter what is done 28. The latter two categories were categorized as inadequate income. The REALM 29 was used to measure health-related literacy. Health literacy was evaluated as a dichotomous variable with low literacy defined as REALM score 0–60 (<9th grade level) and adequate literacy defined as REALM score 61–66 (≥9th grade level). 30
Study Outcomes – Systolic and Diastolic blood pressure
The primary outcome of the study was systolic blood pressure measured at each time point (baseline, and 6, 12, 18, and 24 months of follow up) over the 24 months. Blood pressure was measured using a digital sphygmanometer (BPTRU Automated Non-invasive blood pressure monitor, Model BPM-100). The readings were taken by a research assistant who was blinded to the patient’s randomization assignment. Two blood pressure readings were taken; the first after patients were seated and had rested in a quiet room separate from the clinical practice site, for at least 5 minutes, and the second 30 seconds after the first. The mean blood pressure reading taken at each of the five visits was used as the outcome. Diastolic blood pressure was a secondary outcome.
Analyses
The primary goal was to compare the effects of the intervention arms to usual care within white and non-white patient subgroups. For both systolic and diastolic blood pressures, general linear models (PROC MIXED in SAS, version 9.2) were used to estimate trajectories over the entire study period by intervention arm and race subgroups. Exploratory analyses indicated that both systolic and diastolic blood pressures had quadratic shapes in which improvements in blood pressures were greatest during the first half of the study. The final model included a common intercept for white patients, a common intercept for non-white patients, and the following interaction terms: intervention arm by time (where time was coded as 0, 6, 12, 18, and 24 months), intervention arm by time-squared, and each of these terms interacted with race to estimate the differential intervention trajectories for white and non-white patients. Estimates and confidence intervals from this model were then used to test for blood pressure differences in the intervention groups relative to usual care at 12 and 24 months within white and non-white subgroups. An unstructured covariance was included to account for patients’ repeated measurements over time.
Patients were analyzed on the basis of initial randomization group (intention to treat); 634 patients were included in the analyses. All available data, including data from participants who subsequently discontinued the study, were used for analyses. Our analysis techniques assumed the probability of dropout may depend on covariates in the model (i.e., race and intervention group) or participants’ previous responses but not on current or future responses 31.
Results
There were 308 white and 328 non-white patients. The vast majority of non-white patients were African American (95%). As shown in Table 1, baseline mean systolic blood pressure was 128.3 mm Hg (SD=19.0) for non-white patients and 121.5 mm Hg (SD=15.6) for white patients; baseline diastolic blood pressure was 73.7 (SD=10.5) for non-white patients and 68.8 (SD=10.6) for white patients. Non-whites were younger, more likely to be female, not married, had lower levels of education and literacy, and less income. In terms of behaviors, non-whites had higher body mass index, and were more likely to report medication non-adherence than their white counterparts.
Table 1.
Take Control of Your Blood Pressure (TCYB) Study Baseline Sample Characteristics, Overall and Stratified by Race
| Baseline Characteristicsa | Total (n=636) |
Non-white (n=328) |
White (n=308) |
P-Valueb |
|---|---|---|---|---|
| Demographics | ||||
| Age (Mean age (SD)) | 61 (12) | 59 (12) | 63 (12) | <0.0001 |
| Non-white Race | -- | |||
| American Indian/Alaskan Native | -- | 1% | -- | |
| Asian | -- | 2% | -- | |
| Black | -- | 95% | -- | |
| Other | -- | 2% | -- | |
| Hispanic | 1% | 2% | 1% | 0.45b |
| Male | 34% | 27% | 41% | 0.0003 |
| Married | 50% | 35% | 67% | <0.0001 |
| Lives alone | 26% | 26% | 25% | 0.79 |
| Completed ≤ 12 years of school | 36% | 50% | 22% | <0.0001 |
| Low literacy level (< 9th grade; REALM Score ≤ 60) | 27% | 45% | 8% | <0.0001 |
| Employed | 39% | 37% | 42% | 0.26 |
| Inadequate incomec | 19% | 28% | 9% | <0.0001 |
| No weekly aerobic exercise lasting ≥ 20 minutes | 23% | 25% | 20% | 0.13 |
| Currently smokes | 16% | 21% | 12% | 0.002 |
| Body mass index (Mean BMI (SD)) | 32.1 (8.2) | 33.7 (8.8) | 30.5 (7.3) | <0.0001 |
| Self-reported Medication | 36% | 49% | 21% | <0.0001 |
| Non-adherenced | ||||
| Insurance | <0.0001 | |||
| Commercial | 39% | 34% | 45% | |
| Medicaid | 17% | 27% | 6% | |
| Medicare | 41% | 35% | 48% | |
| Uninsured | 3% | 5% | 2% | |
| Medical History | ||||
| Started taking blood pressure medication > 5 years ago | 60% | 66% | 54% | 0.001 |
| Parent or sibling has hypertension | 77% | 84% | 70% | 0.001 |
| Diabetic | 36% | 45% | 26% | <0.0001 |
| Blood Pressure e | ||||
| Systolic (Mean mm Hg (SD)) | 125 (18) | 128 (19) | 121 (16) | <0.0001 |
| Diastolic (Mean mm Hg (SD)) | 71 (11) | 74 (10) | 69 (11) | <0.0001 |
| Blood Pressure Control | 80% | 72.5% | 88% | <0.0001 |
All data except blood pressure were patient-reported. When missing values existed, they were included in the calculation of percentages
Cochran-Mantel-Haenszel chi-square p-value for general association between non-whites and whites; for the Hispanic variable, the Fisher’s exact test was used.
Inadequate income defined as reporting difficulty paying bills no matter what was done or having money to pay the bills only because cut back on things
Self-reported adherence was assessed using a four-item measure based on Morisky scale 42. Response options ranged from strongly agree (1) to strongly disagree (4). A summary binary variable was created by coding those who responded strongly agree, agree or “don’t know” to any of the four questions as nonadherent; otherwise, patients were coded as adherent.
When patients had multiple blood pressure readings during their baseline visit, mean systolic and mean diastolic readings were used as the baseline blood pressure values
Intervention effects
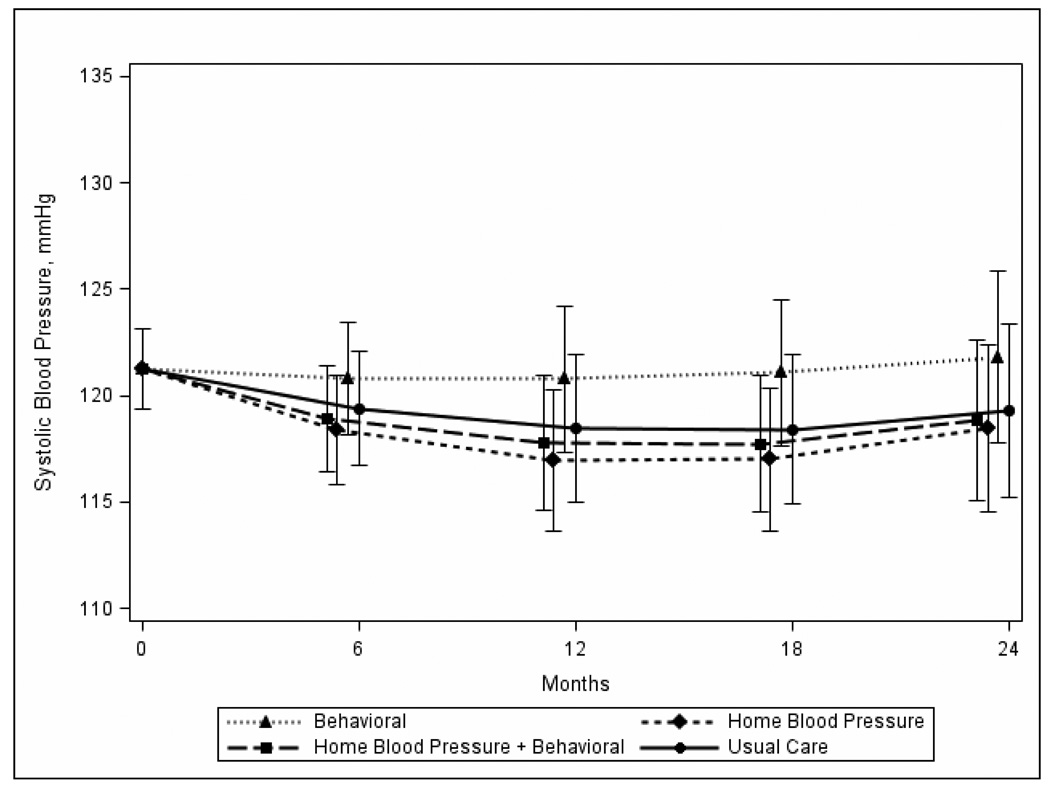
The overall race by time by treatment group effect (6df test) suggested likely differential intervention effects over time for white and non-white patients for both systolic blood pressure (p=0.08) and diastolic blood pressure (p=0.01). Estimated trajectories with confidence intervals are shown in Figures 2a and 2b. The estimated trajectories for white patients (Figure 2b) shows very similar patterns of change between the usual care, home blood pressure monitoring, and combined arms. Among white patients, mean systolic blood pressure was not significantly different at 12 and 24 months for intervention arm patients as compared to usual care patients (see Table 2). A similar pattern was observed for diastolic blood pressure except that white patients in the behavioral only group had a significantly higher mean diastolic blood pressure at 12 months when compared to the usual care group (p=0.03).
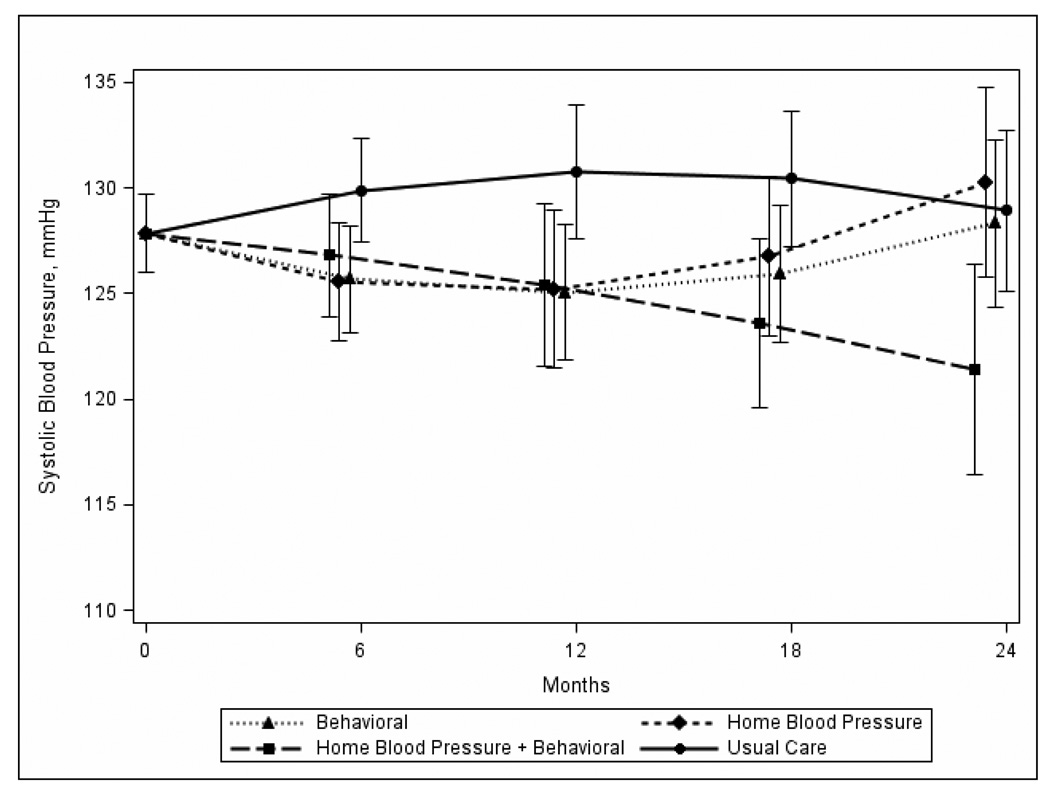
Figure 2.
Figure 2a: Changes in Systolic Blood Pressure from Baseline to 24 Months, by Intervention Group for Non-whites
Figure 2b: Changes in Systolic Blood Pressure from Baseline to 24 Months, by Intervention Group for Whites
Table 2.
Estimated Differences (95% CI) in Blood Pressure Between TCYB Intervention and Usual Care Groups at 12 and 24 Months for Race Subgroups
| Outcome/Subgroup/Time Period |
Behavioral vs. Usual Care |
Home Blood Pressure Monitor vs. Usual Care |
Home Blood Pressure Monitor & Behavioral vs. Usual Care |
|---|---|---|---|
| Systolic Blood Pressure | |||
| White | |||
| 12 months | 2.3 (−2.4, 7.0) | −1.5 (−6.1, 3.2) | −0.7 (−5.2, 3.9) |
| 24 months | 2.5 (−3.1, 8.1) | −0.8 (−6.4, 4.7) | −0.4 (−5.9, 5.0) |
| Non-white | |||
| 12 months | −5.7 (−10.0, −1.4) | −5.5(−10.3, −0.8) | −5.3 (−10.1, −0.5) |
| 24 months | −0.6 (−6.0, 4.8) | 1.3 (−4.4, 7.1) | −7.5 (−13.7, −1.4) |
| Diastolic Blood Pressure | |||
| White | |||
| 12 months | 2.9 (0.4, 5.4) | 0.1 (−2.4, 2.6) | 1.3 (−1.2, 3.7) |
| 24 months | 2.0 (−1.2, 5.1) | 0.1 (−3.0, 3.2) | 0.5 (−2.5, 3.5) |
| Non-white | |||
| 12 months | −3.3 (−5.6, −0.9) | −3.7 (−6.2, −1.1) | −2.7 (−5.3, −0.2) |
| 24 months | 0.6 (−2.4, 3.6) | −0.6 (−3.9, 2.6) | −3.5 (−7.0, −0.1) |
In contrast, several interesting blood pressure patterns occurred among non-white patients. The estimated trajectories for non-white patients (Figure 2a) shows that all intervention improve during the first half of the study, but by the end of the study, only patients in the combined arm continue to show improvement. At 12 months, among non-whites, all intervention groups had significantly lower mean systolic blood pressure (all p<0.05) as compared to the usual care group; estimated differences ranged from −5.3 mm Hg to −5.7 mm Hg. However, at 24 months, only those non-white patients in the combined arm continued to have lower systolic blood pressure as compared to the usual care group (−7.5 mm Hg; 95% CI −13.7, −1.4; p=0.02). A similar pattern was observed for diastolic blood pressure among non-white patients. At 12 months, all intervention groups compared to usual care had significantly lower mean diastolic blood pressure (all p<0.05); estimated differences ranged from −2.7 mm Hg to −3.7 mm Hg. Again, as compared to usual care, only patients in the combined group continued to have lower mean diastolic blood pressure at 24 months (−3.5 mm Hg; 95% CI −7.0, −0.1 mm Hg; p=0.04) (See Table 2).
Discussion
In post-hoc analyses, our data suggest a potential difference in treatment response to a self-management intervention between white and non-white patients. Non-white patients in the nurse behavioral, home blood pressure monitoring, or combined intervention groups had statistically significant systolic blood pressure decreases by 5.3–5.7 mm Hg relative to usual care in the first 12 months, but these improvements were only sustained in the combined behavioral and home monitoring arm (7.5 mm Hg improvement at 24 months) compared to usual care. For whites, we did not observe a significant decrease in blood pressure for any of the intervention groups over the 24 months relative to usual care.
We propose one potential explanation for our findings that the combination of blood pressure monitoring and nurse-administered bi-monthly telephone behavioral intervention was most effective for non-whites and led to clinically and statistically significant improvements. First, consistent with a growing body of literature, lifestyle interventions appear to be as efficacious, if not more among African Americans as compared to whites. 32 There is excellent evidence demonstrating that sodium reduction leads to significant reductions in blood pressure in most patients, but an even greater decrease in both systolic and diastolic blood pressure among African Americans (−8.0 mm Hg and −4.5 mm Hg, respectively) compared with whites (−5.1 mm Hg and −2.2 mm Hg, respectively).33 Additionally, the DASH dietary pattern leads to a reduction in systolic blood pressure and diastolic blood pressure for most patients, but a significantly greater reduction in systolic blood pressure among African Americans with hypertension (−13.2 mm Hg) compared with hypertensive whites (−6.3 mm Hg). 18 In recent “real-life” effectiveness trials, behavioral interventions designed to increase adoption of healthy lifestyles have been effective among African Americans, but generally less so than in whites. 34, 35
This study has several potential limitations. Data were limited to only whites and non-whites seen in two community clinics in one geographic area and therefore may not generalize to other settings. Furthermore, our study was not designed to detect treatment differences in patient subgroups; therefore our ability to provide definitive evidence of a differential treatment response by race was somewhat limited, especially among small subgroups such as whites with poor blood pressure control. In addition, the highest rates of dropout were observed in non-white patients in the combined intervention group. Although our analysis used all available data and is valid under if all predictors of missing data were included in the model (i.e., the missing data assumption of ignorability), the results could be biased if our model was misspecified or if we failed to measure and include other important predictors of dropout. 36 Finally, the comprehensive nature of the self-management intervention makes it difficult to discern which aspects of our intervention were the most beneficial.
The African American population is far from homogeneous, and each African American patient should be treated as an individual. Nonetheless, the rate of cardiovascular disease is 65% higher in African Americans than whites;37 the risk of coronary heart disease is 50% higher38; stroke is 200% higher39; hypertension-related end-stage renal disease is 320% higher40; and congestive heart failure is 2000% higher.41 Thus interventions targeting cardiovascular disease and hypertension that potentially reduce health care barriers and provide improved quality of care among non-whites may directly address one of the most important health disparities in the US today.
Acknowledgement
This research is supported by a NHLBI grant R01 HL070713, and Established Investigator Award from the American Heart Association to the first author. The primary author also received a Pfizer Foundation Health Communication Initiative award, which allowed for increasing the enrollment of individuals with low literacy. No other individuals assisted in manuscript preparation. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No authors have conflicts of interest.
Trial Registration: ClinicalTrials.gov
Registration Number: NCT00123058
Registry URL: http://www.clinicaltrials.gov
References
- 1.American Heart Association. Heart Disease and Stroke Statistics — 2009 Update. American Heart Association, Dallas; [Google Scholar]
- 2.Egan BM, Zhao Y, Axon RN. US Trends in Prevalence, Awareness, Treatment, and Control of Hypertension, 1988–2008. Jama. May 26;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 3.Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008 Nov;52(5):818–827. doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- 4.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002 Nov 14;347(20):1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 5.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005 Oct 10;165(18):2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 6.Fiscella K, Holt K. Racial disparity in hypertension control: tallying the death toll. Ann Fam Med. 2008 Nov–Dec;6(6):497–502. doi: 10.1370/afm.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosworth HB, Powers B, Grubber JM, et al. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med. 2008 May;23(5):692–698. doi: 10.1007/s11606-008-0547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001 Jan 4;344(1):3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 10.Bosworth HB. Hypertension Intervention Nurse Telemedicine Study (HINTS): Testing a multifactorial tailored behavioral/educational and a medication management intervention for blood pressure control. 2009; Paper presented at: National Institute of Health (NIH) Workshop, Future of Telehealth: Essential Tools and Technologies for Clinical Research and Care; Bethesda MD. [Google Scholar]
- 11.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999 Sep;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 12.Fahey T, Schroeder K, Ebrahim S. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2005;(1) doi: 10.1002/14651858.CD005182. CD005182. [DOI] [PubMed] [Google Scholar]
- 13.Powers BJ, Bosworth HB. Revisiting literacy and adherence: future clinical and research directions. J Gen Intern Med. 2006 Dec;21(12):1341–1342. doi: 10.1111/j.1525-1497.2006.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Woolf B. Customer specific marketing. New York: Rand McNally; 1992. [Google Scholar]
- 15.Karanja N, Obarzanek E, Lin PH, McCullough ML, Phillips KM, Swain JF, et al. Descriptive characteristics of the dietary patterns used in the Dietary Approaches to Stop Hypertension Trial. DASH Collaborative Research Group. J Am Diet Assoc. 1999;99:S19–S27. doi: 10.1016/s0002-8223(99)00412-5. [DOI] [PubMed] [Google Scholar]
- 16.Sacks FM, Appel LJ, Moore TJ, et al. A dietary approach to prevent hypertension: a review of the Dietary Approaches to Stop Hypertension (DASH) Study. Clin Cardiol. 1999;22(7) Suppl:III6–III10. doi: 10.1002/clc.4960221503. [DOI] [PubMed] [Google Scholar]
- 17.Svetkey L, Sacks FM, Obarzanek E, et al. for the DASH-Sodium Collaborative Research Group. The DASH diet, sodium intake and blood pressure trial (DASH-sodium): Rationale and Design. Journal of the American Dietetic Association. 1999;99:S96–S104. doi: 10.1016/s0002-8223(99)00423-x. [DOI] [PubMed] [Google Scholar]
- 18.Svetkey L, Simons-Morton D, Vollmer WM, Appel LJ, Conlin PR, Ryan DH, Ard J, Kennedy BM For the DASH research group. Effects of dietary patterns on blood pressure: Subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Archives of Internal Medicine. 1999;159(3):285–293. doi: 10.1001/archinte.159.3.285. [DOI] [PubMed] [Google Scholar]
- 19.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003 Nov;42(5):878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 20.The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. Jama. 1992 Mar 4;267(9):1213–1220. doi: 10.1001/jama.1992.03480090061028. [DOI] [PubMed] [Google Scholar]
- 21.Cutler JA. Randomized clinical trials of weight reduction in nonhypertensive persons. Ann Epidemiol. 1991;1(4):363–370. doi: 10.1016/1047-2797(91)90046-f. [DOI] [PubMed] [Google Scholar]
- 22.Kelley GA, Kelley KS. Progressive resistance exercise and resting blood pressure : A meta-analysis of randomized controlled trials. Hypertension. 2000 Mar;35(3):838–843. doi: 10.1161/01.hyp.35.3.838. [DOI] [PubMed] [Google Scholar]
- 23.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002 Apr 2;136(7):493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 24.Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001 Nov;38(5):1112–1117. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 25.Kincaid J, Fishburne RP, Rogers RL, Chissom BS. Derivation of new readability formulas (Automated Readability Index, Fog Count, and Flesch Reading Ease Formula) for Navy enlisted personnel Research branch report 8–75. In: Tenn, editor. Chief of Naval Training M. 1975. [Google Scholar]
- 26.Bosworth HB, Olsen MK, Neary A, et al. Take Control of Your Blood pressure (TCYB) study: A multifactorial tailored behavioral and educational intervention for achieving blood pressure control. Patient Educ Couns. 2007 Dec 28; doi: 10.1016/j.pec.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller WR, Rollnick S. Motivational Interviewing: Prepapring people to change addictive behaviors. New York: Guilford Press; 1991. [Google Scholar]
- 28.Bosworth HB, Bastian LA, Kuchibhatla MN, et al. Depressive symptoms, menopausal status, and climacteric symptoms in women at midlife. Psychosom Med. 2001 Jul–Aug;63(4):603–608. doi: 10.1097/00006842-200107000-00013. [DOI] [PubMed] [Google Scholar]
- 29.Parker R, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: A new instrument for measuring patients' literacy skills. Journal of General Internal Medicine. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 30.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004 Dec;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York: Springer-Verlag; 2000. [Google Scholar]
- 32.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Jama. 2003;289(19):2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 33.Vollmer WM, Sacks FM, Ard J, et al. Effects of diet and sodium intake on blood pressure: subgroup analysis of the DASH-sodium trial. Ann Intern Med. 2001 Dec 18;135(12):1019–1028. doi: 10.7326/0003-4819-135-12-200112180-00005. [DOI] [PubMed] [Google Scholar]
- 34.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. Jama. 2003 Apr 23–30;289(16):2083–2093. doi: 10.1001/jama.289.16.2083. [DOI] [PubMed] [Google Scholar]
- 35.Svetkey LP, Stevens VJ, Brantley PJ, et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. Jama. 2008 Mar 12;299(10):1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- 36.Gadbury GL, Coffey CS, Allison DB. Modern statistical methods for handling missing repeated measurements in obesity trial data: beyond LOCF. Obes Rev. 2003 Aug;4(3):175–184. doi: 10.1046/j.1467-789x.2003.00109.x. [DOI] [PubMed] [Google Scholar]
- 37.Hozawa A, Folsom AR, Sharrett AR, Chambless LE. Absolute and attributable risks of cardiovascular disease incidence in relation to optimal and borderline risk factors: comparison of African American with white subjects--Atherosclerosis Risk in Communities Study. Arch Intern Med. 2007 Mar 26;167(6):573–579. doi: 10.1001/archinte.167.6.573. [DOI] [PubMed] [Google Scholar]
- 38.Mensah GA. Eliminating disparities in cardiovascular health: six strategic imperatives and a framework for action. Circulation. 2005 Mar 15;111(10):1332–1336. doi: 10.1161/01.CIR.0000158134.24860.91. [DOI] [PubMed] [Google Scholar]
- 39.Rosamond WD, Folsom AR, Chambless LE, et al. Stroke incidence and survival among middle-aged adults: 9-year follow-up of the Atherosclerosis Risk in Communities (ARIC) cohort. Stroke. 1999 Apr;30(4):736–743. doi: 10.1161/01.str.30.4.736. [DOI] [PubMed] [Google Scholar]
- 40.Smith SR, Svetkey LP, Dennis VW. Racial differences in the incidence and progression of renal diseases. Kidney Int. 1991 Nov;40(5):815–822. doi: 10.1038/ki.1991.281. [DOI] [PubMed] [Google Scholar]
- 41.Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. 2009 Mar 19;360(12):1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986 Jan;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]