Abstract
Objectives
Assess population attributable fractions (PAFs) for late postnatal transmission (LPT) of human immunodeficiency virus-1 (HIV-1) in a cohort of HIV-1-exposed infants.
Methods
We used data established from a risk factor analysis of LPT (negative HIV-1 results through the 4-6 week visit, but positive assays thereafter through the 12-month visit) from a perinatal clinical trial conducted in three sub-Saharan countries. PAFs were calculated as the proportions of excess LPTs attributed to identified risk factors.
Results
For the cohort of 1317 infants, 206 (15.6%) had only low maternal CD4+ counts (< 200 cells/mm3), 332 (25.2%) had only high maternal plasma viral loads (VLs) (> 50 000 copies/mL), and 81 (6.2%) had both low CD4+ counts and high VLs. Their PAFs were 26.0% [95% confidence interval (CI), 12.0%-36.0%], 37.0% (95% CI, 22.0%-51.0%) and 16.0% (95% CI, 6.0%-25.0%), respectively.
Conclusions
Our PAF analysis illustrates the public health impact of the substantial proportion of LPTs accounted for by high-risk women with both low CD4+ counts and high VLs. In light of these results, access to and use of antiretroviral therapy (ART) by high-risk HIV-1-infected pregnant women is essential. Additional strategies to reduce LPT for those not meeting criteria for ART should be implemented.
Keywords: Breast feeding, late postnatal transmission, prevention of mother to child transmission/vertical transmission, risk factors, viral load
INTRODUCTION
In resource-limited areas where efficacious interventions to prevent mother-to-child transmission (MTCT) of human immunodeficiency virus type-1 (HIV-1) such as antiretroviral prophylaxis, cesarean section before labor and ruptured membranes, and complete avoidance of breastfeeding are not universally available or feasible, the risk of MTCT of HIV-1 remains high. It is estimated that the rate of MTCT of HIV-1 could be as high as 42.0% in the absence of any intervention to prevent transmission 1 In 2007, an estimated 270,000 children younger than 15 years died of AIDS, and, of those, more than 90.0% were from sub-Saharan Africa 2-3. In those most heavily-affected countries, HIV-1 is the underlying reason for one-third of the deaths among children aged five years or younger 4. Without antiretroviral therapy (ART), HIV disease progression in children is particularly aggressive, with many children dying at a very young age 4-7.
In sub-Saharan Africa, prolonged breastfeeding is customary. Breast milk transmission is one of the most important mechanisms through which MTCT of HIV-1 occurs. In an individual patient data meta-analysis including data from more than 3,000 breastfeeding infants of HIV-1-infected women from sub-Saharan Africa, the cumulative probability of late postnatal transmission (LPT) at 18 months was estimated to be 9.3%, and the overall LPT incidence rate was estimated to be 8.9 per 100 child-years of breastfeeding 1,7.
The HIV Network for Prevention Trials (HIVNET) 024 trial was a randomized clinical trial to assess the efficacy of antibiotics to prevent chorioamnionitis-associated MTCT of HIV-1 and preterm birth in sub-Saharan Africa 8-9. A secondary analysis of risk factors for LPT identified that lower maternal CD4+ counts and higher plasma viral loads at enrollment were significantly associated with higher risk of LPT of HIV-110.
Although lower maternal CD4+ counts and higher maternal plasma viral loads are significant risk factors for LPT, the public health impact of these risk factors by their amelioration (e.g., through effective ART) has rarely been investigated. Toward this end, this analysis aims to evaluate the public health impact, by studying the population attributable fractions (PAFs) of LPTs (breastfeeding transmissions) attributed to low maternal CD4+ counts and/or high maternal plasma viral loads.
Generally speaking, the PAF has been extensively used as an epidemiological parameter to measure the public health impact attributed to being exposed to a risk factor 11-13, although it should be cautiously interpreted in practice 14. For example, a PAF of 15% means that the risk factor would account for 15% of the population disease incidence, and it implies that the population disease incidence would potentially be reduced by 15% if the risk factor were removed from the population. In this analysis, we calculated the PAFs for the identified risk factors of LPTs, to investigate the potential public health implication of amelioration of these risk factors in the HIVNET 024 population. These PAFs, as calculated, are directly related to the sub-Saharan Africa population where the HIVNET 024 study was conducted. Hence, they can be used to assess the impact of low maternal CD4+ counts and high viral loads on breastfeeding transmission (and the potential effect of identifying and treating the high risk group of women with low CD4+ counts and high viral loads).
METHODS
The HIVNET 024 Trial
The HIVNET 024 trial was conducted at four sites in three sub-Saharan African countries: Blantyre and Lilongwe, Malawi; Dar es Salaam, Tanzania; and Lusaka, Zambia. Details regarding the methods and results of this randomized trial have been published 8-9. The protocol, outcome measures and interview details are available at: http://www.hptn.org/research_studies/hivnet024.asp. The study was approved by the institutional review boards at each participating institution, and participants provided written informed consent. All enrolled HIV-1-infected women and their infants were given nevirapine (NVP) according to the HIVNET 012 regimen for prevention of MTCT of HIV-1 16. Infant study visits were conducted at birth (within the first 48 hours), at four to six weeks, and at three, six, nine, and 12 months. Information about breastfeeding and maternal health also was collected at these visits. Each clinical site provided HIV-1 counseling regarding the risks and benefits of breast feeding. However, replacement feeding or other inventions to prevent breastfeeding-related transmission of HIV-1 infection were not provided as part of the trial. ART for mothers and children was not available at the participating clinical sites when the trial was conducted. HIV-1 RNA PCR assays and HIV-1 enzyme immunoassays (EIAs) were used to establish the HIV-1 infection status of infants in the HIVNET 024 study. Laboratory procedures have been described previously 10.
Definitions and Study Population for This Analysis
The study population for this analysis is identical to the one established for the risk factor analysis of LPT of HIV-1 in the HIVNET 024 population 10. Specifically, the study population comprised live born, singleton (or first born if a multiple gestation pregnancy) infants of HIV-1-infected women enrolled in the HIVNET 024 trial, with negative HIV-1 diagnostic assay results at birth and 4-6 weeks of age, who had subsequent HIV-1 diagnostic testing performed, and who continued to breastfeed after six weeks of age. Infants with positive HIV-1 RNA assays at birth were considered to have acquired HIV-1 infection in utero. Those with a first positive assay at the six-week study visits were considered to have acquired HIV-1 infection through perinatal/early postnatal transmission. Infants with negative HIV-1 RNA assay results at birth and at 4-6 weeks of age, but who had positive HIV-1 RNA test results thereafter through the 12-month visit, were considered to have acquired HIV-1 infection during the late postnatal period (HIV-1 acquired through breastfeeding, or LPT). HIV-1-uninfected infants were those with negative EIA results at 12 months of age, or with negative HIV-1 RNA assay results throughout follow-up.
Statistical Analysis
The outcomes of LPT of HIV-1 (through 12 months) were assessed in time-to-event analyses. The event-time of an infected infant was determined by the midpoint between the last negative and the first positive HIV-1 RNA assay results (subsequent to the 6-week visit and at or before the 12-month visit) since an HIV RNA negative result at the 6-week visit, which is the time-zero of this analysis An event-time was considered censored at the date of the last negative HIV-1 RNA test result if the infant did not test positive at or before the 12-month visit. Additional censoring was considered if weaning or death occurred. Discrete-time Cox proportional hazards models 15 stratified by site were used to identify risk factors associated with LPT of HIV-1.
To calculate PAF for a risk factor, E, the PAF was defined by
, where I was the total LPT incidence of HIV-1 during the postnatal period and I0 was the expected LPT incidence for the reference group being unexposed to E 11-13. Unless stated otherwise, PAFs were calculated under the Cox proportional hazards model. Their variances were calculated by the developed methods 13. All statistical calculations and analyses were performed using SAS version 9.1.3 on Sun OS 5.9 platform.
RESULTS
Risk Factors for LPT of HIV-1
Among a total of 2659 women enrolled in the HIVNET 024 trial, 2292 were HIV-1-infected. Of their infants, 1317 had negative HIV-1 diagnostic assay results at six weeks of age, continued to breast-feed after six weeks of age, and had subsequent HIV-1 diagnostic testing performed. For the 1317 infants who were subsequently followed during the late postnatal period up to one year of age, 84 LPTs were observed after 6 weeks but before 12 months of age 10. Analysis based on Kaplan-Meier curves showed that the LPT rates by 6 months and 12 months were 4.1% [95% confidence interval (CI): 5.2%-5.4%] and 6.9% (95% CI: 5.6%-8.5%), respectively. More descriptive results, such as prevalences of the risk factors, can be found in an earlier publication 10.
For multivariate analyses, maternal characteristics at enrollment (age, education, marital status, home electricity use, home running water use, CD4+ count, plasma viral load, cervicovaginal fluid viral load), around the time of delivery (receipt of NVP prophylaxis), and at 4-6 weeks postpartum (mastitis, cracked nipples), and infant characteristics (gestational age at birth, birth weight, gender, receipt of NVP prophylaxis, oral candidiasis at 4-6 weeks of age and infant diarrhea at 4-6 weeks of age) were incorporated 10. In the earlier final multivariate analysis of using a backward stepwise modeling procedure, lower maternal CD4+ counts and higher maternal plasma viral loads at enrollment were the two factors found to be significantly associated with LPT 10. Among the infants who were at risk of LPT in this cohort, 206 (15.6%) had low maternal CD4+ counts (defined as less than 200 cells/mm3 for the current analysis), and 332 (25.2%) had high maternal viral loads (defined as more than 50 000 copies/mL for the current analysis). Furthermore, 29 (14.1%) LPTs were observed among the 206 infants with low maternal CD4+ counts, whereas 49 (5.0%) LPTs were observed among the 975 infants with higher maternal CD4+ counts (defined as 200 cells/mm3 or more for this analysis). Forty-two (12.7%) LPTs were observed among 332 infants with high maternal viral loads, whereas 37 (4.0%) LPTs were observed among 919 infants with lower maternal viral loads (defined as 50 000 copies/mL or less for this analysis).
Population Attributable Fractions
The PAFs were estimated as 26.0% (95% CI, 11%-36.0%) for low CD4+ counts and 37.0% (95% CI, 22.0%-51.0%) for high viral loads: 15.6% of the infants with low maternal CD4+ counts accounted for 26.0% of the total LPTs, and 25.2% of the infants with high maternal viral loads accounted for 37.0% of the total LPTs. From a risk prevention perspective for this cohort of infants, if the 15.6% of infants whose mothers had low CD4 counts were to have an increase in their CD4+ counts to 200 cells/mm3 or more, the overall disease burden of LPTs would be reduced by 26.0%, and if the 25.2% of infants whose mothers had high viral loads were to have a decrease in their plasma viral loads to 50 000 copies/mL or less, the overall disease burden would be reduced by 37.0% (Table 1).
TABLE 1.
Population Attributable Fractions (PAFs) for Maternal CD4+ Counts (CD4s) (cel ls/mm3), Maternal Plasma Viral Loads (VLs) (copies/mL), and Combined Maternal CD4s-V Ls.
| Risk Factor | Late Postnatal Period* |
Total Incidences (I)† |
Expected Incidences (I0)‡ |
PAF § | 95% CI |
|---|---|---|---|---|---|
| VL > 50 000 | 42-182 Days | 48 | 37.3 | 22.0% | |
| 183-365 Days | 30 | 12.3 | 59.0% | ||
| 42-365 Days | 78 | 49.5 | 37.0% | 22.0%, 51.0% | |
| CD4+ < 200 | 42-182 Days | 51 | 34.8 | 32.0% | |
| 183-365 Days | 26 | 22.4 | 14.0% | ||
| 42-365 Days | 77 | 57.2 | 26.0% | 12.0%, 36.0% | |
| CD4+ < 200 and VL > 50 000 | 42-182 Days | 48 | 41.0 | 15.0% | |
| 183-365 Days | 25 | 20.2 | 19.0% | ||
| 42-365 Days | 73 | 61.1 | 16.0% | 6.0%, 25.0% |
CI, Confidence Interval
Number of days after birth
six infants of LPT with unknown maternal plasma viral loads and seven infants of LPT with unknown maternal CD4+ counts
Model-based estimates of expected number of incidences in reference group
PAF = (1-I0/I)×100%
PAFs might fluctuate during the late postnatal period. A person-year analysis showed that point estimates of the LPT incidence rates were likely to be different between the first part of the late postnatal period (six weeks to six months) and the second part of the late postnatal period (six months to 12 months), although a larger sample size may be needed to show whether or not the differences are statistically significant (Table 2). Similarly, the PAFs of low maternal CD4+ counts were 32.0% and 14.0%, and the PAFs of high maternal plasma viral loads were 22.0% and 59.0%, for these two parts of the late postnatal period, respectively (Table 1).
TABLE 2.
Incidences of Late Postnatal Transmission of HIV-1
| Late Postnatal Period* | Infant-Years | Incidences | Incidence Rate† | 95% CI† |
|---|---|---|---|---|
| 42-182 Days | 437.8 | 53 | 11.9% | 8.9%, 15.6% |
| 183-365 Days | 394.8 | 31 | 7.9% | 5.3%, 11.1% |
CI, Confidence Interval
Number of days after birth
Based on person-year analysis
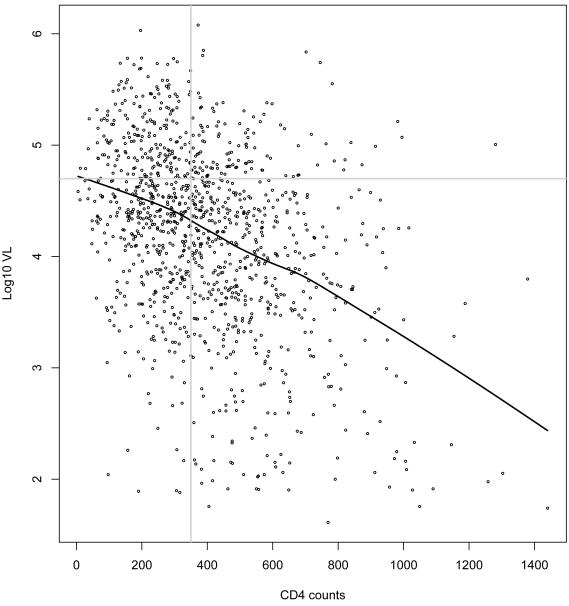
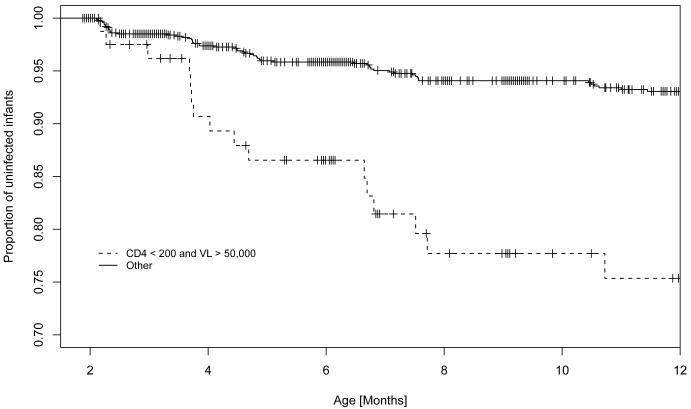
Maternal CD4+ counts and viral loads were negatively correlated, as shown in their scatter plot with a lowess curve (bandwidth = 200) (Figure 1). This negative correlation implies that the maternal CD4+ counts increase as the viral load decreases, and vice versa. A binary CD4-VL factor of combined maternal CD4+ counts and viral loads was formed. In the reference group of 1045 infants with higher maternal CD4+ counts or lower maternal viral loads, 58 (5.5%) LPTs were observed. In the comparison group of 81 infants with low maternal CD4+ counts and high viral loads, 16 (19.7%) LPTs were observed. Kaplan-Meier estimates showed that the comparison group had a greater risk of LPT over time (Figure 2).
Figure 1.
Scatter plot of maternal viral loads (log10 copies/ml) versus maternal CD4+ counts (cells/mm^3)
Figure 2.
Kaplan–Meier Estimates for Proportion of HIV–1 Uninfected Infants During the Late Postnatal Period
In a multivariate regression analysis including all the aforementioned candidate variables and the combined CD4-VL factor, the combined CD4-VL factor became the sole significant variable in the full multivariate Cox model, with a hazards ratio of 4.50 (P < 0.0001). The final Cox model with the only CD4-VL factor showed little change in the hazards ratio.
For the CD4-VL factor, the PAF was calculated as 16.0% (95% CI, 6.0%-25.0%). That is, although only 6.2% of the infants were in the high-risk subgroup, they disproportionally accounted for 16.0% of the total LPTs. From a risk prevention perspective, in this high-risk group, if the 6.2% of mothers had either increased their CD4+ counts to 200 cells/mm3 or more, or decreased their plasma viral loads to 50,000 copies/mL or less, the total LPT disease burden would be reduced by 16.0%. Such a reduction would be 15.0% for the first part of the late postnatal period, and 19.0% for the second part of the late postnatal period (Table 1).
DISCUSSION
In this large cohort of HIV-1-infected women and their infants from three sub-Saharan African countries, low maternal CD4+ counts and high maternal viral loads were found to be significantly associated with the LPT of HIV-1 10. The public health impact of reducing LPTs in sub-Saharan population by effectively ameliorating these risk factors has rarely been investigated. Our PAF assessment showed that, for the high-risk group of infants born to HIV-1-infected mothers with low CD4+ counts and high viral loads in HIVNET 024, if the maternal CD4+ counts increased to 200 cells/mm3 or more, or the viral loads decreased to 50,000 copies/mL or less, the total LPT of HIV-1 would be reduced by 16.0%, although this high-risk group only accounted for 6.2% of the study cohort. In fact, our additional assessment shows similar PAF crude and model-based estimates.
Numerous studies have demonstrated that low maternal CD4+ absolute lymphocyte counts and high maternal plasma viral loads are significantly associated with breast milk transmission of HIV-1 17-23. However, what is less well characterized is the potential impact of these factors on the overall disease burden of LPT (for example, if maternal CD4+ counts were increased or maternal viral loads were decreased with timely and appropriate use of effective ART). Our finding of a potential reduction of 16.0% of the overall LPT burden by increasing maternal CD4+ counts to 200 cells/mm3 or more, or deceasing maternal viral loads to 50 000 copies/mL or less, is similar to what was reported in a prospective cohort study conducted in Thailand 24. In that study, with only maternal viral load being considered, the PAFs were 21.4% for those with maternal viral loads between 31 622 and 100 000 copies/mL, and 16.2% for those with maternal viral loads above 100 000 copies/mL.
A particular strength of our analysis is that maternal CD4+ counts and maternal viral loads were considered jointly by the combined CD4-VL variable. This approach has two advantages. First, even though these two risk factors were both associated with LPT, their negative correlation would usually not allow for one to change while the other is held constant in a particular intervention/prevention strategy. The combined CD4-VL variable captured the significant associations of both risk factors, with a proportion of treatment explained (PTE) of 100% 25. Second, a high-risk group was identified to assess its PAF so that a prevention program might be prioritized to focus on this group. For the HIVNET 024 cohort, for example, PAFs for the combined CD4-VL variable showed that a prevention strategy could efficiently reduce a substantial proportion of total LPTs by focusing on one or more high-risk subgroups, when resources are limited.
There are limitations of our analysis. First, the mothers who agreed to participate in HIVNET 024 might not be representative of the entire population that a potential prevention program would target, since they had to satisfy certain inclusion and exclusion criteria in order to enroll into the trial. For example, social stigma or less awareness of the HIVNET 024 trial might have deterred certain women with low CD4+ counts or high viral loads from participating in the study. Without knowing the prevalence of risk factors in the general population, the PAFs calculated based on HIVNET 024 may not be generalizable. Secondly, the PAF measures a potential reduction of overall LPTs by increasing maternal CD4+ counts or decreasing maternal viral loads. It does not mean such a reduction would always be realized. Also, weaning was considered non-informative censoring in the current analysis. Thus, the assumption was that infants might still be at risk for LPT after weaning, which might inflate the overall LPT risk. Finally, HIVNET 024 trial did not collect information on other factors potentially associated with the risk of LPT, e.g., type of breast feeding (exclusive, predominant, mixed), and there were substantial amounts of missing data for maternal CD4+ counts and viral loads, although post-hoc sensitivity analysis assuming several different scenarios shows little impact on the conclusions. These limitations pose potentially serious challenges to consistent PAF estimates. As a result, PAFs calculated based on HIVNET 024 need to be further validated.
Nevertheless, our PAF calculations have important implications for the prevention of LPT of HIV-1. One important implication is that, when an intervention (such as effective use of ART) is able to increase maternal CD4+ counts or lower maternal viral loads in a high-risk subgroup, the reduction of overall disease burden of LPT of HIV-1 may be substantial, even if this high-risk subgroup only accounts for a small proportion of the total population. The more prevalent the high-risk group, the greater the reduction of LPT incidence that is expected. For example, in a population with a similar high-risk group as in HIVNET 024, the PAF could increase quickly from 47.0%, to 64.0%, and to 72.0%, if the prevalence of the high-risk group in the overall population increased from 25.0%, to 50.0%, and to 75.0%, respectively. Hence, providing access to and encouraging appropriate use of effective ART should greatly reduce the LPT incidence when advanced HIV-1 disease is prevalent (as manifested by lower CD4+ counts and higher plasma viral loads) among pregnant women.
The other important implication is that, if a high-risk subgroup consists of only a small proportion of individuals in a population, only targeting high-risk subgroups with ART (to increase maternal CD4+ counts and/or lower maternal viral loads) may not attain a large reduction of LPTs of HIV-1. For the HIVNET 024 cohort, the PAF was only 16.0%, implying that there were still a large proportion of LPTs contributed by those women with less advanced HIV-1 disease. Therefore, additional interventions are necessary to further lower the risk of LPT among healthier HIV-1-infected women. Such interventions (some of proven efficacy, and others under study) could include antiretroviral prophylaxis to the mother and/or the infant during breastfeeding, chemical or heat treatment of breast milk, and passive or active immunization.
ACKNOWLEDGMENTS
We gratefully acknowledge the contribution of the mothers and children who participated in this study. We are also grateful to the entire study team at each site for their dedication and excellent collaboration. Our thanks are extended to institutions that contributed to the conduct of this study in each country.
The HIVNET 024 Trial was supported by the HIV Network for Prevention Trials (HIVNET) and sponsored by the US National Institute of Allergy and Infectious Diseases (NIAID), National Institutes of Health (NIH), Department of Health and Human Services, through contracts NO1-AI-35173 with Family Health International, NO1-AI-45200 with Fred Hutchinson Cancer Research Center, and subcontract NO1-AI-35173-117/412 with Johns Hopkins University. In addition, the trial was supported by the HIV Prevention Trials Network (HPTN) and sponsored by NIAID, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute on Drug Abuse, the National Institute of Mental Health, and the Office of AIDS Research of the National Institutes of Health, U.S. Department of Health and Human Services, Harvard University (U01-AI-48006), Johns Hopkins University (U01-AI-48005), and the University of Alabama at Birmingham (U01-AI-47972). Nevirapine (Viramune®) for the study was provided by Boehringer Ingelheim Pharmaceuticals, Inc. The conclusions and opinions expressed in this paper are those of the authors and do not necessarily reflect those of the funding agencies and participating institutions.
APPENDIX
The HIVNET 024 Team
Protocol Co-Chairs: Taha E. Taha, MD, PhD (Johns Hopkins University Bloomberg School of Public Health); Robert Goldenberg, MD (University of Alabama at Birmingham);
In-Country Co-Chairs/Investigators of Record: Newton Kumwenda, PhD, George Kafulafula, MBBS, FCOG (Blantyre, Malawi); Francis Martinson, MD, PhD (Lilongwe, Malawi); Gernard Msamanga, MD, ScD (Dare es Salaam, Tanzania); Moses Sinkala, MD, MPH, Jeffrey Stringer, MD (Lusaka, Zambia); US Co-Chairs: Irving Hoffman, PA, MPH (University of North Carolina, Chapel Hill); Wafaie Fawzi, MD, DrPH (Harvard School of Public Health );
In-Country Investigators, Consultants and Key Site Personnel: Robin Broadhead, MBBS, FRCP, George Liomba, MBBS, FRCPath, Johnstone Kumwenda, MBChB, MRCP, Tsedal Mebrahtu, ScM, Pauline Katunda, MHS, Maysoon Dahab, MHS (Blantyre, Malawi); Peter Kazembe, MBChB, David Chilongozi CO, MPH, Charles Chasela CO, MPH, George Joaki, MD, Willard Dzinyemba, Sam Kamanga (Lilongwe, Malawi); Elgius Lyamuya, MD, PhD, Charles Kilewo, MD, MMed, Karim Manji, MD, MMed, Sylvia Kaaya, MD, MS, Said Aboud, MD, MMed, Muhsin Sherrif MD, MPH, Elmar Saathoff, PhD, Priya Satow, MPH, Illuminata Ballonzi, SRN, Gretchen Antelman, ScD, Edgar Basheka, BPharm (Dar es Salaam, Tanzania); Victor Mudenda, MD, Christine Kaseba, MD, Maureen Njobvu, MD, Makungu Kabaso, MD, Muzala Kapina, MD, Anthony Yeta, MD, Seraphine Kaminsa, MD, MPH, Constantine Malama, MD, Dara Potter, MBA, Maclean Ukwimi, RN, Alison Taylor, BSc, Patrick Chipaila, MSc, Bernice Mwale, BPharm (Lusaka, Zambia);
US Investigators, Consultants and Key Site Personnel: Priya Joshi, BS, Ada Cachafeiro, BS, Shermalyn Greene, PhD, Marker Turner, BS, Melissa Kerkau, BS, Paul Alabanza, BS, Amy James, BS, Som Siharath, BS, Tiffany Tribull, MS (UNC-CH); Saidi Kapiga, MD, ScD, George Seage, PhD (HSPH); Sten Vermund, MD, PhD, William Andrews, PhD, MD, Deedee Lyon, BS, MT(ASCP) (UAB);
NIAID Medical Officer: Samuel Adeniyi-Jones, MD;
NICHD Medical Officer: Jennifer S. Read, MD, MS, MPH, DTM&H;
Protocol Pharmacologist: Scharla Estep, RPh, MS;
Protocol Statisticians: Elizabeth R. Brown, ScD, Tom Fleming, PhD, Anthony Mwatha, MS, Lei Wang, PhD, Deborah Donnell, PhD, Ying Q. Chen, PhD;
Protocol Virologist: Susan Fiscus, PhD;
Protocol Operations Coordinator: Lynda Emel, PhD;
Data Coordinators: Debra J. Lands, Ed.M, Ceceilia J. Dominique;
Systems Analyst Programmers: Alice H. Fisher, BA, Martha Doyle;
Protocol Specialist: Megan Valentine, PA-C, MS
REFERENCES
- 1.The Working Group on Mother-to-Child Transmission of HIV Rates of mother-to-child transmission of HIV-1 in Africa, America, and Europe: results from 13 perinatal studies. J Acquir Immune Defic Syndr Hum Retrovirol. 1995;8:506–510. doi: 10.1097/00042560-199504120-00011. [DOI] [PubMed] [Google Scholar]
- 2.The Breastfeeding and HIV International Transmission Study (BHITS) Group Late postnatal transmission of HIV-1 in breastfed children: an individual patient data metaanalysis. J Infect Dis. 2004;189:2154–2166. doi: 10.1086/420834. [DOI] [PubMed] [Google Scholar]
- 3.The Joint United Nations Programme on HIV/AIDS (UNAIDS) UNAIDS; Geneva, Switzerland: 2008. Report on the Global AIDS Epidemic, Ch. 2. Available at: http://data.unaids.org/pub/GlobalReport/2008/jc1510_2008_global_report_pp29_62_en.pdf. [Google Scholar]
- 4.Mason E. Positioning paediatric HIV in the child survival agenda: presentation to UNICEF-WHO consultation. UNICEF; New York: Jan 11-13, 2006. 2006. Available at http://data.unaids.org/pub/GlobalReport/2008/jc1510_2008_global_report_pp325_358_en.pdf. [Google Scholar]
- 5.Taha TE, Kumwenda NI, Hoover DR, et al. Association of HIV-1 load and CD4 lymphocyte count with mortality among untreated African children over one year of age. AIDS. 2000;14:453–459. doi: 10.1097/00002030-200003100-00021. [DOI] [PubMed] [Google Scholar]
- 6.Newell ML, Coovadia H, Cortina-Borja M, et al. Mortality of infected and uninfected infants born to HIV-infected mothers in Africa: a pooled analysis. Lancet. 2006;64:1236–1243. doi: 10.1016/S0140-6736(04)17140-7. [DOI] [PubMed] [Google Scholar]
- 7.Brahmbhatt H, Kigozi G, Wabwire-Mangen F, et al. Mortality in HIV-infected and uninfected children of HIV-infected and uninfected mothers in rural Uganda. J Acquir Immune Defic Synd.r. 2006;41:504–508. doi: 10.1097/01.qai.0000188122.15493.0a. [DOI] [PubMed] [Google Scholar]
- 8.Taha TE, Brown ER, Hoffman IF, et al. A Phase III clinical trial of antibiotics to reduce chorioamnionitis-related perinatal HIV-1 transmission (HPTN 024) AIDS. 2006;20:1313–1321. doi: 10.1097/01.aids.0000232240.05545.08. [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg RL, Mwatha A, Read JS, et al. The HPTN 024 Study: The efficacy of antibiotics to prevent chorioamnionitis and preterm birth. Am J Obs Gyn. 2006;194:650–661. doi: 10.1016/j.ajog.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Chasela C, Chen YQ, Fiscus S, et al. Risk factors for late postnatal transmission of human immunodeficiency virus type 1 in Sub-Saharan Africa. Pedia Infectious Dis J. 2008;27:251–256. doi: 10.1097/INF.0b013e31815b4960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levin ML. The occurrence of lung cancer in man. ACTA Unio Internationalis Contra Cancrum. 1953;9:531–541. [PubMed] [Google Scholar]
- 12.Miettinen OS. Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol. 1974;99:325–332. doi: 10.1093/oxfordjournals.aje.a121617. [DOI] [PubMed] [Google Scholar]
- 13.Chen YQ, Hu CC, Wang Y. Attributable risk function in the proportional hazards model for censored time-to-event. Biostatist. 2006;7:515–529. doi: 10.1093/biostatistics/kxj023. [DOI] [PubMed] [Google Scholar]
- 14.Rockhill B, Newman B, Weinberg B. Use and misuse of population attributable fractions. Amer J Pub Health. 88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Allison P. Discrete-time methods for the analysis of event histories. Social Method. 1982;13:61–98. [Google Scholar]
- 16.Guay LA, Musoke P, Fleming T, et al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother-to-child transmission of HIV-1 in Kampala, Uganda: HIVNET 012 randomised trial. Lancet. 1999;354:795–805. doi: 10.1016/S0140-6736(99)80008-7. [DOI] [PubMed] [Google Scholar]
- 17.Semba RD, Kumwenda N, Hoover DR, et al. Human immunodeficiency virus load in breast milk, mastitis, and mother-to-child transmission of human immunodeficiency virus type 1. J Infect Dis. 1999;180:93–98. doi: 10.1086/314854. [DOI] [PubMed] [Google Scholar]
- 18.Embree JE, Njenga S, Datta P, et al. Risk factors for postnatal mother-child transmission of HIV-1. AIDS. 2000;14:2535–2541. doi: 10.1097/00002030-200011100-00016. [DOI] [PubMed] [Google Scholar]
- 19.Leroy V, Karon JM, Alioum A, et al. Postnatal transmission of HIV-1 after a maternal short-course zidovudine peripartum regimen in West Africa. AIDS. 2003;17:1493–1501. doi: 10.1097/00002030-200307040-00010. [DOI] [PubMed] [Google Scholar]
- 20.Pillay K, Coutsoudis A, York D, et al. Cell-free virus in breast milk of HIV-1-seropositive women. J Acquir Immune Defic Syndr. 2000;24:330–336. doi: 10.1097/00126334-200008010-00006. [DOI] [PubMed] [Google Scholar]
- 21.Contopoulos-Ioannidis DG, Ioannidis JPA. Maternal cell-free viremia in the natural history of perinatal HIV-1 transmission: a meta-analysis. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18:126–133. doi: 10.1097/00042560-199806010-00004. [DOI] [PubMed] [Google Scholar]
- 22.Richardson BA, John-Stewart GC, Hughes JP, et al. Breast-milk infectivity in human immunodeficiency virus type 1-infected mothers. J Infect Dis. 2003;187:736–740. doi: 10.1086/374272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taha TE, Hoover DR, Kumwenda NI, et al. Late postnatal transmission of HIV-1 and associated factors. J Infect Dis. 2007;196:10–14. doi: 10.1086/518511. [DOI] [PubMed] [Google Scholar]
- 24.Mock PA, Shaffer N, Bhadrakom C, et al. Maternal viral load and timing of mother-to-child HIV transmission, Bangkok, Thailand. AIDS. 1999;13:407–414. doi: 10.1097/00002030-199902250-00014. [DOI] [PubMed] [Google Scholar]
- 25.Lin DY, Fleming TR, DeGruttola V. Estimating the proportion of treatment effect explained by a surrogate marker. Statist Med. 1997;16:1515–1527. doi: 10.1002/(sici)1097-0258(19970715)16:13<1515::aid-sim572>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]