Abstract
Objective
The goal of this paper is to identify strategies for connectivity that will optimize point-of-care testing (POCT) organized as small-world networks in disaster settings.
Methods
We evaluated connectivity failures during the 2010 Haiti Earthquake, applied small-world network concepts, and reviewed literature for point-of-care (POC) connectivity systems.
Results
Medical teams responding to the Haiti Earthquake faced connectivity failures that affected patient outcomes. Deploying robust wireless connectivity systems can enhance the efficiency of the disaster response by improving health care delivery, medical documentation, logistics, response coordination, communication, and telemedicine. Virtual POC connectivity education and training programs can enhance readiness of disaster responders.
Conclusions
The admirable humanitarian efforts of more than 4000 organizations substantially impacted the lives of earthquake victims in Haiti. However, the lack of connectivity and small-world network strategies, combined with communication failures, during early stages of the relief effort must be addressed for future disaster preparedness.
Keywords: Bluetooth, field area network, first responder, Haiti, intensive care unit, point-of-care testing, preparedness, response, technology, Wi-Fi, WiMAX, wireless
“The future is already here, it’s just unevenly distributed.”—William Gibson
Medical disaster assistance after the Richter 7.0 scale earthquake on January 12, 2010, in Haiti1 illustrated the use of point-of-care testing (POCT).2,3 However, emergency and disaster care requires connected systems to facilitate bidirectional flow of knowledge and information. Point-of-care (POC) connectivity allows the exchange of diagnostic data between devices and medical personnel for timely evidence-based treatment, disaster response coordination, and wireless patient management. Availability of these functions at the POC can improve disaster relief efforts and patient outcomes. The goals of this article are to assess the immediate connectivity needs of disaster responders, to design innovative networks for emergencies, and to recommend future solutions that use connectivity to optimize the benefits of POCT in disasters.
METHODS
Needs Assessment
We conducted PubMed searches to identify key POC connectivity considerations for emergency and disaster care settings. Internet searches identified the timeline of events after the Haiti earthquake, locations of hospitals in country, and relevant articles regarding POC device use and connectivity. Additionally, medical personnel who responded to the Haiti Earthquake were interviewed at the 2010 Integrated Medical, Public Health, Preparedness and Response Training Summit4 on June 2–6, 2010 and in teleconferences.
Haiti Small-World Network
Google (Google, Mountain View, Calif ) and World Health Organization (Geneva, Switzerland) maps5,6 were used to illustrate the geographical relationship of Haiti’s health care and transportation infrastructures relative to the earthquake epicenter. Names of hospitals damaged or destroyed were collected from searches through internet news media.7–9
POC Disaster Response Testing
Internet searches also identified several POC devices used by or ready to deploy with disaster responders. We identified the strengths and weaknesses of each technology and provide POC connectivity recommendations.
RESULTS
Infrastructure
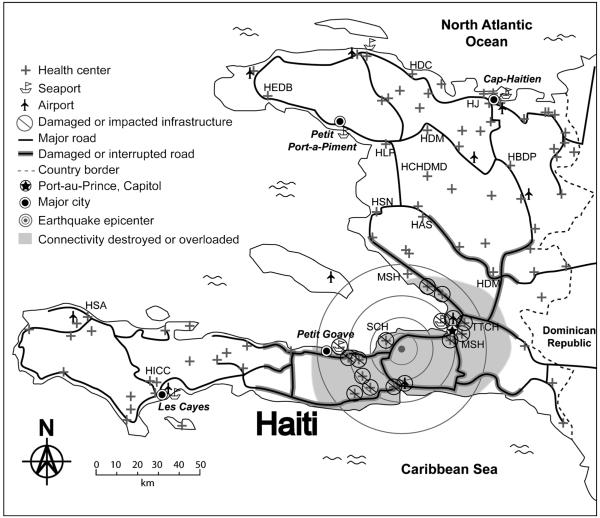
Figure 1 shows Haiti health care infrastructure, transportation systems, and disruptions resulting from the earthquake. Power loss and physical disruption of communication networks after the Haitian earthquake resulted in connectivity failures.4,7,8,10 Cell phone towers and landlines were disabled. Cell phone service was unavailable for at least 17 days in the capital, Port-au-Prince.4
FIGURE 1. High impact of earthquake on health care small-world network in Haiti.
Located on an island in the Caribbean Sea, Haiti borders the Dominican Republic to the East. The SWN relates the earthquake epicenter to health care infrastructure destroyed. Victim rescue routes were interrupted. Disaster responders arrived late and, in some cases, carried POC devices, which they discovered were vulnerable to environmental temperature extremes. Hospitals (“H”) are as follows: HAS, Albert Schweitzer; HBDP, Bienfaisance De Pignon; HCHDMD, Claire Heureuse De Marchand Dessalines; HDC, De Carrefour; HDM, De Marmelade; HEDB, Evangelique De Bombardopolis; HICC, Immaculee Conception des Cayes; HJ, Justinien; HLP, La Providence; HSA, St. Antoine De Jeremie; MSH, Mission Saintard; HSN, St. Nicolas; MSH, Maternité Solidarité; SCH, Sainte Croix; TTCH, Trinite Trauma Center.
Coordination
Experiences described by attendees at the Integrated Training Summit4 revealed an uncoordinated response by multiple non-government organizations (NGOs) after the earthquake. Each NGO group lacked situational awareness of their proximity to other NGOs. Patient referral between NGOs and other health care providers was slow and frustrating. Patient tracking technology often was unavailable. For example, a family brought in a man that needed surgery. He was transported to the United States Navy hospital ship, USNS Comfort, but his family was not allowed to follow. Neither the referring clinic nor the family was able to receive information about the man except that he died on the ship. The family could not locate the body.
Preparedness
Internet searches identified the availability of several POC technologies and platforms. The “Lab-in-a-Backpack”11 developed at RICE University (Houston, Tex) consists of a large backpack that provides basic laboratory testing capabilities at the POC for the disaster responder. Here, we modify the Lab-in-a-Backpack concept by enhancing it with connectivity and POC pathogen detection capabilities (Fig. 2). We recommend small-world network (SWN) connectivity solutions to enhance preparedness in the sections that follow.
FIGURE 2. Field area network for victim information connectivity.
The diagnostic lab-in-a-backpack (A, B) equips first responders with the tools necessary to perform diagnoses in field settings. Field area networks (FANs) use Bluetooth to connect POC devices to handheld computer nodes (eg, iPhone, satellite phone, and smartphone). Field area networks can be modular (eg, FAN1, 2, 3, and 4), allowing addition and multiplexing of POC tests, such as pathogen detection, pulse oximetry, electrocardiograms, and blood pressure monitors, to fit the diagnostic needs of the disaster response. Bridged by 2-way satellite, FANs provide long- and short-range communication and data management for victim identification, position, history, treatment, and triage (C) that spans geographic barriers or disaster-produced obstacles.
VISION, DISCUSSION, AND RECOMMENDATIONS
Disaster POCT
Enhanced disaster connectivity can be achieved with a “field area network” (FAN) for POCT (Fig. 2). Key challenges a successful disaster response must overcome include integrating robust multi-nodal FANs,12 connecting POCT results for documentation and telemedicine,13–16 triaging and tracking patients,17 near-patient testing in connected hubs and portable intensive care units (ICUs), overcoming unpredictable environmental factors,18 incorporating wireless modalities while minimizing security risks, and implementing education and training to improve future preparedness.
Robust Connectivity Infrastructures
Regardless of disaster type, such as a hurricane, earth-quake, tsunami, or terrorist attack, communication infrastructures often are destroyed during the catastrophic event.10,19,20 Even if the destruction is partial, the surviving networks quickly are inundated by the sudden surge of users.10 Therefore, disaster responders need an alternative solution for restoring connectivity.
Patricelli et al12 described a mobile satellite system that quickly restores connectivity to disconnected areas. The satellite connectivity system, called “MOBSAT” (Vizada, Rockville, Md), delivers Wireless-Fidelity (Wi-Fi), Worldwide Interoperability for Microwave Access (WiMAX), and satellite Internet access from a mobile trailer that can be towed by a car or carried by an air vehicle. Through WiMAX, a scalable telecommunication protocol governed by IEEE 802.16 standard,21 a MOBSAT trailer establishes a 1- to 8-km network that provides voice, video, and data services to compatible devices.12 WiMAX can create a mesh network with other WiMAX units nearby to provide a larger area of coverage and prevent single-point connectivity failures.12,21 WiMAX also can provide Internet to a High Altitude Platform,21 a floating infrastructure or air vehicle that can extend the reach of WiMAX.12,21 The use of floating platforms to provide reliable connectivity in disaster settings would be useful in overcoming challenging geographic topologies.21
The Wireless Internet Information System for Medical Response in Disasters (WIISARD) system17 developed at the University of California, San Diego, deploys Calmesh nodes (California Institute for Telecommunications and Information Technology, San Diego, Calif ) to provide disaster connectivity. Each node contains a small, special-purpose Linux computer using multiple wireless modalities, such as Wi-Fi and Global Positioning System, to facilitate connectivity for POC devices. Each Calmesh node is capable of connecting to others to form mesh clusters. In a WIISARD disaster simulation, a Calmesh cluster provided field connectivity diameter of 1.5 km.17,22
POCT, Documentation, and Telemedicine
Connectivity can automate documentation16 to improve accuracy. Compared with manual entry, automated documentation of test results reduces operator errors and ensures proper record keeping.14,17,23,24 Minimizing manual data entry saves valuable time, allowing disaster responders to care for more victims. Current POC connectivity standard, CLSI document POCT1-A2,16 outlines cable and infrared interfaces, which require periodic docking of the POC device for connectivity and lack real-time connectivity provided by a wireless interface.
The number of disaster responders immediately available after a disaster may not be sufficient to handle the surge of patients.7 Disaster responders may encounter patients with unfamiliar illnesses that require consultation with a medical specialist, who is not locally available, or with downloaded visual logistics clues on a handheld computer to speed diagnostics. Telemedicine and POCT could alleviate this surge by connecting POC diagnostic data to resources at a remote site. With connectivity, responders at a disaster site can send POC diagnostic data, in-cluding pictures and video clips, to medical specialists at a remote location for additional consultation.25–28 If available experts are occupied, the connected responder can consult medical databases on the Internet or previously downloaded software for temporary medical solutions.29
A POC system evaluated by Dickson and Pedersen30 illustrates feasibility of using 802.11 g Wi-Fi technology and cellular 3G broadband network to wirelessly stream ultrasound video in real time for telemedicine. A national alerting system, the Autonomous Pathogen Detection System (APDS), developed at the Lawrence Livermore National Laboratory in Livermore, Calif, features connectivity with wired Ethernet, wireless cellular, and Wi-Fi.26 The APDS samples air to detect bio-threat pathogens and can be remotely controlled via a handheld device and command console. The APDS system suggests feasibility of interpreting continuous POC data from remote locations.
Patient Triaging and Tracking
In mass trauma scenarios found in disaster settings, triaging and tracking challenges both victims and responders. Triaged patients must wait for their turn to receive care and may leave or wander off the site without being adequately treated. In the case of a disease outbreak or a biological terrorist attack, patients must be tracked to ensure proper transportation, isolation to prevent an epidemic, and discovery of index cases. Through connectivity, wireless triaging and tracking of patients become feasible and are an improvement over the traditional paper methods.31–34
A next-generation patient monitoring system,33 developed at Johns Hopkins University, features a wireless pulse oximeter and position tracking devices that transmit data wirelessly to the disaster responder. Another system, the Trauma Patient Tracking System35 developed at the Lawrence Berkeley National Laboratory, tracks patient locations using Global Positioning System outdoor and television/radio frequency indoor.
The WIISARD also uses disaster responders with wireless triaging and tracking of patients.17,31 In addition to using wireless pulse oximeter, WIISARD disaster responders carry a handheld computer to tag and triage victims. Victims are tagged with wristlets containing unique identification barcodes. A disaster responder can scan the barcode with a handheld computer to confirm patient identity and retrieve or upload medical records and diagnostic data. Use of barcodes combined with connectivity to an electronic medical record improves speed and accuracy of patient care.17 The WIISARD responders also use tablet personal computers to monitor patients and manage their transportations by coordinating with available ambulances and hospitals.17
Near-Patient Testing in Connected Portable ICUs
Availability of ICUs is essential for rapid treatment of unstable disaster victims. In the event of slow transportation or overcrowded emergency rooms, victims must be treated near the disaster site.36 Point-of-care testing may be used to bring ICU capabilities to the disaster setting. However, these POC devices may not communicate with each other, and a responder must monitor multiple devices to support 1 patient.36 Necessary POC devices include pulse oximeter, electrocardiography, blood pressure monitoring, infusion pumps, automated ventilators, and other critical care instruments.36,37 With availability of FAN connectivity (Fig. 2), a disaster responder can wirelessly monitor multiple POC devices from a single handheld computer node (eg, smartphone, personal digital assistant, laptop).17,38,39
Environmental Factors
Several key differences exist between a hospital setting and a disaster setting. A hospital is a controlled environment with reliable power sources, telecommunication lines, and data networks. Disaster sites are unpredictable and unfamiliar environments. Power generators and batteries replacing wall outlets require periodic maintenance. For example, WIISARD’s Calmesh nodes are mobile wireless access points operating on battery power and can last up to 18 hours of continuous use.17 Mobility allows rapid response but requires daily management, which may be especially hard while facing a surge of victims or shortage of disaster responders.
The unpredictable disaster environment may disrupt recently restored connectivity. In Haiti, at least 59 aftershocks of Richter magnitude 4.5 or greater followed the 7.0-magnitude earthquake.1 Rapidly deployed wireless infrastructures may fail because of recurring disasters. Mesh networking capabilities of wireless infrastructures12,17,21 creates redundant overlapping coverage. However, this redundancy serves as a safety net in case one of the nodes in the network fails.21 In addition to damage caused by the disaster, extreme temperature and humidity may render POC connectivity devices useless.18 Hence, the devices used in a disaster response must be environmentally robust.
Wireless Modalities and Security
For POCT, wireless connectivity offers useful functions for disaster settings. Table 1 lists the advantages and disadvantages of Bluetooth, a wireless modality and IEEE standard 802.15 that operates at 2.4 gigahertz frequency for handheld devices.41 Point-of-care vendors have started to embrace wireless connectivity in their POC devices. Table 2 lists several vendors and devices using Bluetooth connectivity. The Bluetooth core specification 4.0, which contains a dedicated low energy consumption mode, is expected to launch in the summer of 2010.42
TABLE 1.
Advantages and Disadvantages of Bluetooth Connectivity in Disaster Scenarios
| Advantages | Disadvantages |
|---|---|
| Designed to facilitate connections between devices located within a few meters of each other (ie, Smartphone to POC device)16 |
Not designed to replace high-speed connections (ie, Ethernet cable)16 |
| Low power consumption (1–100 mW)41 | Low bandwidth (800 kbps)41 |
| Allows disaster responders access to Internet, hospital networks, patient information, and diagnostic equipment40 |
Vulnerable to unauthorized access of stored patient information40 |
| Easy to use and inexpensive peripheral antennas add Bluetooth functionality to a wide range of devices without the need for additional software or wireless routers40 |
Undocumented “rogue access points” create problems for a network that seems to be secure40 |
| PIN-encrypted connections between devices secure data transmissions40 |
Short PINs easily hijacked and used to gain access to otherwise secure networks40 |
| Several Bluetooth-enabled devices can disable wireless capability when not in use, discouraging unauthorized access40 |
Entire Bluetooth networks may need periodic scans for attached devices use, to ensure security40 |
| Reduces the likelihood of patients accidentally removing wearable POC devices such as pulse oximeters40 |
Uses the same radio frequency as WLAN (2.4 GHz)16 |
PIN indicates personal identification number; and WLAN, wireless local area network.
TABLE 2.
Bluetooth-Capable POC Devices
| Instrument | Manufacturer | Format | Measurements | Time To Result |
Cost ($) |
|---|---|---|---|---|---|
| Alive Pulse Oximeter | Alive Technologies www.alivetec.com |
Fingertip Pulse Oximeter |
%SpO2, heart rate | Continuous | NA |
| Datospir Micro CCE | Siblemed www.sibelmed.es | Portable | Spirometer | Triggered by respiration |
1500–1700 |
| EPOC BloodFDA Analysis system |
Epocal www.epocal.com | Handheld | Measured: pH, pCO2, pO2, Na, K, iCa, Gluc, Hct Calculated: HCO3, TCO2 Base excess, sO2, Hb |
30 seconds | NA |
| GlucoTelCE | BodyTel www.bodytel.com | Handheld | Blood glucose | 10 seconds | ~122 |
| LifeStar BP Pro | LifeWatch Technologies www.instromedix.com |
Portable | Blood pressure | 30 seconds | NA |
| Littmann Model 3200FDA |
3M www.3m.com | Handheld | Electronic stethoscope | Continuous | ~380 |
| Mobil-O-Graph NGFDA |
Numed Holdings Ltd www.numed.co.uk |
Portable | 24 hour blood pressure | Continuous | 2080–2520 |
| MultiscanPVRCE,FDA | Mediwatch Plc www.mediwatch.com |
Portable | Bladder scan | Continuous | NA |
| MyGlucoHealth CE,FDA meter |
Entra Health Systems www.entrahealthsystems.com |
Handheld | Blood glucose | 3 seconds | 90–100 |
| Onyx II 9560CE,FDA | Nonin Medical www.nonin.com | Fingertip Pulse Oximeter |
%SpO2, heart rate | Continuous | ~495 |
| PSA watchCE | Mediwatch Plc www.mediwatch.com |
Handheld | Total prostate specific antigen |
10 minutes | NA |
| Pulse3CE,FDA | evo Medical Solution www.evomedical.com |
Handheld | %SpO2, heart rate | Spot check | NA |
| Wireless ECG SystemFDA |
LIFESync www.lifesynccorp.com |
Transportable | Electrocardiogram | Continuous | ~4000 |
CE indicates CE certification; FDA, FDA approval; NA, not available.
Along with the benefits of wireless technologies comes the security problem. The Health Insurance Portability and Accountability Act of 1996 (HIPAA) was enacted to protect sensitive patient data and personal information. The HIPPA privacy and security rules43 set national standards requiring security of electronic patient information. Wireless networks in disaster settings require verification for access to protected data.44,45
Requiring verification and password protection on both sending and receiving devices ensures protection of sensitive patient data being transmitted over an encrypted wireless network. Solutions to secure access include requiring verification by virtual private network access for both receiving and sending devices, using an access control server, Wired Equivalent Privacy (WEP) security protocol wireless network encryption, and other security requirements used in hospital settings.35,44–47 Wi-Fi Protected Access (WPA and WPA2) encryption also should be considered when deciding how to protect patient data. WPA and WPA2 offer several advantages over WEP.48 The WPA offers stronger encryption algorithms, changes encryption keys constantly, and improves checksum and replay protection, providing a safer network that is harder to access without authorization.48 Implementing WPA encryption requires proper hardware and software that should be accounted for during disaster planning.48 Securing patient data on a wireless network is feasible in a disaster setting.
Preparedness and Education
The success of connectivity systems depends heavily on the proficiency of the operator. Disaster responders tasked with maintaining connectivity must establish or restore complex communication systems in austere operational environments.12 Therefore, emerging connectivity equipment must be operable by unskilled personnel and require minimum field maintenance.
For emerging nations, such as Haiti, a language gap may represent a significant hurdle and basic educational gap when training local personnel to operate connected POC devices. Given current information technology sources, most of the available instructional material is written principally in the English language.49 Instructional “just-in-time” videos or manuals should incorporate visual logistics to minimize laborious text descriptions and bridge educational or language barriers.50,51
With basic educational proficiency, emerging disaster connectivity equipment can have a profound day-to-day impact in low-resource settings where miles of inhospitable or un-navigable terrain may separate health centers. Once operational, these remote connectivity devices can be implemented as rural telemedicine training hubs.52,53
CONCLUSIONS
Use of handheld computers has proven effective at the POC.17,31,32,54,55 The wireless connectivity features of handheld computers (Table 3) offer a connectivity solution that can optimize patient care through enhanced POCT, communication, and patient management.
TABLE 3.
Disaster POC Connectivity: Responder Empowerment
| Handheld Computer Features |
POC Connectivity Applications |
|---|---|
| 802.11× | Connection to a wireless local area network for data transfer, internet access, and voice communications |
| Bluetooth | Pairing with compatible POC devices |
| Camera | Video and photos for multimedia POC connectivity |
| Cellular | Voice communications, SMS, MMS, and internet access |
| Global Positioning System |
Generation of longitude/latitude for user and patient tracking, and situational awareness |
| Universal Serial Bus | Connectivity to personal computers and for battery recharging |
| Web browser | Internet access |
MMS indicates multimedia messaging service; PDA, personal digital assistant; and SMS, short message service (“text message”).
Future POC connectivity and devices must be environmentally robust and disaster ready. Wireless communications can be vulnerable and risk violating HIPAA privacy and security rules. However, some exceptions should be implemented in favor of rapid response for disaster victims. Training and education must follow suit.
The admirable humanitarian efforts of more than 4000 organizations substantially impacted the lives of earthquake victims in Haiti. However, the lack of connectivity and SWN strategies, combined with communication failures, during early stages of the relief effort must be addressed for future disaster preparedness.
ACKNOWLEDGMENTS
This study was supported by the Point-of-Care Testing Center for Teaching and Research and by a National Institute for Biomedical Imaging and Bioengineering (NIBIB) Point-of-Care Technologies Center grant (NIH U54 EB007959 to Dr Kost, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIBIB or the National Institutes of Health. Figures and tables were provided with permission and courtesy of Knowledge Optimization, Davis, CA.
REFERENCES
- 1.USGS [Accessed June 17, 2010];Magnitude 7.0–HAITI REGION. [United States Geological Survey Web site] Available at: http://earthquake.usgs.gov/earthquakes/eqinthenews/2010/us2010rja6/
- 2.Vanholder R, Gibney N, Luyckx VA, et al. Renal disaster relief task force in Haiti earthquake. Lancet. 2010;375:1162–1163. doi: 10.1016/S0140-6736(10)60513-2. [DOI] [PubMed] [Google Scholar]
- 3.Ginzburg E, O’Neill WW, Goldschmidt-Clermont PJ, et al. Rapid medical relief—Project Medishare and the Haitian earthquake. N Engl J Med. 2010;362:e31. doi: 10.1056/NEJMp1002026. [DOI] [PubMed] [Google Scholar]
- 4.2010 Integrated Medical, Public Health, Preparedness and Response Training Summit. Las Vegas, NV: [Accessed June 17, 2010]. Jun 2–6, 2010. Available at: http://www.integratedtrainingsummit.org/ [Google Scholar]
- 5.Google [Accessed June 17, 2010];Satellite Google Maps. Available at: http://maps.google.com/
- 6.WHO [Accessed June 17, 2010];Haiti Earthquake–Health Center Locations (as of 15 Jan 2010) [ReliefWeb Web site] 2010 January 15; Available at: http://www.reliefweb.int/rw/rwb.nsf/db900sid/MNIN-7ZTN8G?OpenDocument&rc=2&emid=EQ-2010-000009-HTI.
- 7. [Accessed June 17, 2010];Haiti Earthquake update [Medecins Sans Frontieres UK Web site] 2010 January 13; Available at: http://www.msf.org.uk/haiti_update_20100113.news.
- 8. [Accessed June 17, 2010];MSF Responding to Devastating Earthquake in Haiti [Medecins Sans Frontieres Web site] 2010 January 12; Available at: http://www.doctorswithoutborders.org/news/article.cfm?id=4147&cat=field-news.
- 9.Talbird J. [Accessed June 17, 2010];Apartments where Chattanoogans often stayed in Haiti are now rubble. 2010 January 15; Available at: http://www.chattanoogan.com/articles/article_166873.asp.
- 10.Corley A. [Accessed June 17, 2010];Why Haiti’s Cellphone Networks Failed [IEEE Spectrum Web site] 2010 February 19; Available at: http://spectrum.ieee.org/telecom/wireless/whyhaitis-cellphone-networks-failed.
- 11.Williams M. [Accessed June 17, 2010];Lab-in-a-Backpack goes to work in Ecuador [RICE University Media Web site] 2010 January 13; Available at: http://www.media.rice.edu/media/NewsBot.asp?MODE=VIEW&ID=13562.
- 12.Patricelli F, Beakley JE, Carnevale A, et al. Disaster management and mitigation: the telecommunications infrastructure. Disasters. 2009;33:23–37. doi: 10.1111/j.1467-7717.2008.01060.x. [DOI] [PubMed] [Google Scholar]
- 13.Kost GJ, Minear M, Siegel PM, et al. Knowledge ⇒ education ⇒ mind connectivity: using telemedicine to achieve a global vision for point-of-care testing. Point of Care. 2008;7:69–71. [Google Scholar]
- 14.Kost GJ. Preventing problems, medical errors, and biohazards in point-of-care testing: using complex adaptive systems to improve outcomes. Point of Care. 2003;2:78–88. [Google Scholar]
- 15.Kost GJ. Connectivity: the millennium challenge for point-of-care testing. Arch Pathol Lab Med. 2000;124:1108–1110. doi: 10.5858/2000-124-1108-C. [DOI] [PubMed] [Google Scholar]
- 16.CLSI . Point-of-Care Connectivity; Approved Standard–Second Edition. CLSI document POCT1-A2. Clinical and Laboratory Standards Institute; Wayne, PA: 2006. p. 289. [Google Scholar]
- 17.Lenert LA, Chan TC, Kirsh D, et al. [Accessed June 17, 2010];Wireless Internet Information System for Medical Response in Disasters. Final Report. 2008 Feb. 12 Available at: http://collab.nlm.nih.gov/webcastsandvideos/siirsv/ucsdsummaryreport.pdf.
- 18.Louie RF, Sumner SL, Belcher S, et al. Thermal stress and point-of-care testing performance: suitability of glucose test strips and blood gas cartridges for disaster response. Disaster Med Public Health Prep. 2009;3:13–17. doi: 10.1097/DMP.0b013e3181979a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kost GJ, Tran NK, Tuntideelert M, et al. Katrina, the tsunami and point-of-care testing: optimizing rapid response diagnosis in disasters. Am J Clin Pathol. 2006;126:513–520. doi: 10.1309/NWU5E6T0L4PFCBD9. [DOI] [PubMed] [Google Scholar]
- 20.Townsend FF. [Accessed June 17, 2010];The Federal Response to Hurricane Katrina: Lessons Learned [The White House Web site] 2006 Feb. 23 Available at: http://georgewbushwhitehouse.archives.gov/reports/katrina-lessons-learned/
- 21.Kuran MS, Tugcu T. A survey on emerging broadband wireless access technologies. Comput Networks. 2007;51(11):3013–3046. [Google Scholar]
- 22.Braunstein B, Trimble T, Mishra R, et al. Feasibility of using distributed wireless mesh networks for medical emergency response. AMIA Annu Symp Proc. 2006;2006:86–90. [PMC free article] [PubMed] [Google Scholar]
- 23.Kost GJ. Controlling economics, preventing errors, and optimizing outcomes in point-of-care testing. In: Kost GJ, editor. Principles and Practice of Point-of-Care Testing. Lippincott Williams & Wilkins; Philadelphia, PA: 2002. pp. 577–600. [Google Scholar]
- 24.Kost GJ. Preventing medical errors in point-of-care testing: security, validation, performance, safeguards, and connectivity. Arch Pathol Lab Med. 2001;125:1307–1315. doi: 10.5858/2001-125-1307-PMEIPO. [DOI] [PubMed] [Google Scholar]
- 25.Bleakley K. Remote systems for responding to occupational pathogens. Telemedicine and e-Health; Abstracts from the American Telemedicine Association Fifteenth Annual International Meeting and Exposition.2010. p. S48. [Google Scholar]
- 26.Hindson BJ, Makarewicz AJ, Setlur US, et al. APDS: the autonomous pathogen detection system. Biosens Bioelectron. 2005;20(10):1925–1931. doi: 10.1016/j.bios.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 27.Sakles JC, Mosier J, Hudson M, et al. Videolaryngoscopic intubation integrated into a telemedicine system: the Tucson Telebation Program. Telemedicine and e-Health; Abstracts from the American Telemedicine Association Fifteenth Annual International Meeting and Exposition.2010. pp. S41–S42. [Google Scholar]
- 28.Siddiqui J, Sandrock C, Bair AE. Disaster preparedness: enhancing surge capacity and partnership effort. Telemedicine and e-Health; Abstracts from the American Telemedicine Association Fifteenth Annual International Meeting and Exposition.2010. pp. S24–S25. [Google Scholar]
- 29.Choi E. Disaster relief informatics: access to KatrinaHealth.org prescription data via OQO ultra mobile PC and cellular wireless connectivity. AMIA Annu Symp Proc. 2006;2006:888. KatrinaHealth.org [PMC free article] [PubMed] [Google Scholar]
- 30.Dickson BW, Pedersen PC. Wireless image streaming in mobile ultrasound. Telemed J E Health. 2010;16:161–166. doi: 10.1089/tmj.2009.0103. [DOI] [PubMed] [Google Scholar]
- 31.Buono CJ, Chan TC, Killeen J, et al. Comparison of the effectiveness of wireless electronic tracking devices versus traditional paper systems to track victims in a large scale disaster. AMIA Annu Symp Proc. 2007;2007:886. [PubMed] [Google Scholar]
- 32.Chan TC, Buono CJ, Killeen JP, et al. Tablet computing for disaster scene managers. AMIA Annu Symp Proc. 2006;2006:875. [PMC free article] [PubMed] [Google Scholar]
- 33.Gao T, Kim MI, White D, et al. Iterative user-centered design of a next generation patient monitoring system for emergency medical response. AMIA Annu Symp Proc. 2006;2006:284–288. [PMC free article] [PubMed] [Google Scholar]
- 34.Killeen JP, Chan TC, Buono C, et al. A wireless first responder handheld device for rapid triage, patient assessment and documentation during mass casualty incidents. AMIA Annu Symp Proc. 2006;2006:429–433. [PMC free article] [PubMed] [Google Scholar]
- 35.Maltz J, Ng TC, Li D, et al. The trauma patient tracking system: implementing a wireless monitoring infrastructure for emergency response. Conf Proc IEEE Eng Med Biol Soc. 2005;3:2441–2446. doi: 10.1109/IEMBS.2005.1616962. [DOI] [PubMed] [Google Scholar]
- 36.Rice DH, Kotti G, Beninati W. Clinical review: critical care transport and austere critical care. Crit Care. 2008;12:207. doi: 10.1186/cc6782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Globe and Mail [Accessed June 17, 2010];Portable ICU for the battlefield [The Globe and Mail Web site] 2010 May 31; Available at: http://www.theglobeandmail.com/report-onbusiness/your-business/grow/your-business-video/portable-icu-for-thebattlefield/article1586457/?cmpid=rss1.
- 38. [Accessed June 17, 2010];MedEx 1000 Portable ICU System [TechFresh Network Web site] 2008 October 14; Available at: http://www.techfresh.net/medex-1000-portable-icu-system/
- 39.Wodajo F. [Accessed June 17, 2010];Turning your iPhone into a Portable ICU Monitor–AirStrip Technologies is Revolutionizing Mobile Health Care [iMedicalApps Web site] 2010 March 10; Available at: http://www.imedicalapps.com/2010/03/airstripremote-patient-monitoring/
- 40.Hernacki B. [Accessed June 17, 2010];Improving Bluetooth security: what IT managers and mobile device users can do. Disaster Recovery Journal. 2006 Available at: http://www.drj.com/articles/win06/1901-13.html. [Google Scholar]
- 41.IEEE [Accessed June 17, 2010];Approves IEEE 802.15.1 standard for wireless personal area networks adapted from the Bluetooth® specification [IEEE Web site] 2002 March 21; Available at: http://standards.ieee.org/announcements/802151app.html.
- 42.Bluetooth [Accessed June 17, 2010];Bluetooth Low Energy Wireless Technology [Bluetooth Web site] 2010 Available at: http://www.bluetooth.com/English/Technology/Works/Pages/Bluetooth_low_energy_technology.aspx.
- 43. [Accessed June 17, 2010];Understanding Health Information Privacy [U.S. Dept. of Health & Human Services Web site] Available at: http://www.hhs.gov/ocr/privacy/hipaa/understanding/index.html.
- 44.Kim DK, Yoo SK, Park JJ, et al. PDA-phone-based instant transmission of radiological images over a CDMA network by combining the PACS screen with a Bluetooth-interfaced local wireless link. J Digit Imaging. 2007;20(2):131–139. doi: 10.1007/s10278-007-9002-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arnold JL, Levine BN, Manmatha R, et al. Information-sharing in out-of-hospital disaster response: the future role of information technology. Prehosp Disaster Med. 2004;19(3):201–207. doi: 10.1017/s1049023x00001783. [DOI] [PubMed] [Google Scholar]
- 46.Zhao X, Rafiq A, Hummel R, et al. Integration of information technology, wireless networks, and personal digital assistants for triage and casualty. Telemed J E Health. 2006;12:466–474. doi: 10.1089/tmj.2006.12.466. [DOI] [PubMed] [Google Scholar]
- 47.Chen D, Soong SJ, Grimes GJ, et al. Wireless local area network in a prehospital environment. BMC Med Inform Decis Mak. 2004;4:12. doi: 10.1186/1472-6947-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Posey BM. [Accessed June 17, 2010];WPA wireless security offers multiple advantages over WEP [TechRepublic Web site] Available at: http://articles.techrepublic.com.com/5100-10878_11-5060773.html.
- 49.Chandrasekhar CP, Ghosh J. Information and communication technologies and health in low income countries: the potential and the constraints. Bull World Health Organ. 2001;79:850–855. [PMC free article] [PubMed] [Google Scholar]
- 50.Mecozzi DM, Brock TK, Tran NK, et al. Evidence-based point-of-care device design for emergency and disaster care. Point of Care. 2010;9:65–69. doi: 10.1097/POC.0b013e3181d9d47a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kools M, van de Wiel MW, Ruiter RA, et al. Pictures and text in instructions for medical devices: effects on recall and actual performance. Patient Educ Couns. 2006;64:104–111. doi: 10.1016/j.pec.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 52.Gul S, Ghaffar H, Mirza S, et al. Multitasking a telemedicine training unit in earthquake disaster response: paraplegic rehabilitation assessment. Telemed J E Health. 2008;14:280–283. doi: 10.1089/tmj.2007.0042. [DOI] [PubMed] [Google Scholar]
- 53.Merrell RC, Cone SW, Rafiq A. Telemedicine in extreme conditions: disasters, war, remote sites. Stud Health Technol Inform. 2008;131:99–116. [PubMed] [Google Scholar]
- 54.Versel N. [Accessed June 17, 2010];Harvard volunteers track Haiti injuries on iPhones [Fierce Mobile Healthcare Web site] 2010 February 2; Available at: http://www.fiercemobilehealthcare.com/story/harvard-volunteers-track-haiti-injuries-iphones/2010-02-02.
- 55.Eplan H. Real time emergency response monitoring and data capture for chemical and radiological incidents. Health Phys. 2005;89(2 Suppl):S40–S41. doi: 10.1097/01.hp.0000165871.80641.8b. [DOI] [PubMed] [Google Scholar]