Abstract
Frameworks are needed to inform diabetes self-care programs for diverse populations. We tested the Information-Motivation-Behavioral Skills (IMB) model among Puerto Ricans with Type 2 diabetes (N=118). Structural equation models evaluated model fit and interrelations among constructs. For diet behavior, information and motivation related to behavioral skills (r=0.19, p<0.05 and r=0.39, p<0.01, respectively); behavioral skills related to behavior (r=0.42, p<0.01 and r=0.32, p<0.05); and behavior was related to glycemic control (r=−0.26, p<0.05). For exercise, personal motivation related to behavioral skills (r=0.53, p<0.001), and behavioral skills related to behavior (r=0.45, p<0.001). The IMB model could inform interventions targeting these behaviors in diabetes.
Keywords: Information, motivation, behavioral skills (IMB) model, glycemic control, Puerto Rican, diabetes, behavior
Diabetes is a chronic debilitating condition worldwide that is associated with increased complications, mortality, and health utilization and cost (Bonow & Gheorghiade, 2004). Puerto Rican Americans have a significantly high rate of diabetes (Melnik et al., 2004; Whitman, Silva, & Shah, 2006); and those with diabetes have low rates of adherence to self-care behaviors (Gollenberg, Pekow, Markenson, Tucker, & Chasan-Taber, 2008), and experience high rates of diabetes-related complications (Lipton et al., 1996) and mortality (Smith & Barnett, 2005). Despite the obvious need for diabetes self-care programs for this population, to our knowledge only a few interventions been developed and published (Cleghorn et al., 2004; Vazquez, Millen, Bissett, Levenson, & Chipkin, 1998). Because self-care behaviors such as diet and exercise are critical for glycemic control, increased efforts are needed to identify what elements should be included in interventions to promote these behaviors in this and other high risk populations.
Several conceptual models of health behavior change describe the factors influencing behavioral performance across disease contexts, with the ultimate goal of informing health promotion interventions (Elder, Ayala, & Harris, 1999). Many models have informed diabetes educational efforts (Whittemore, 2000). However, in a recent review of 185 diabetes education programs, no single conceptual framework to date was comprehensive enough to link attributes of high quality diabetes care to self-care processes and, ultimately, diabetes outcomes (Borgermans et al., 2008). The authors of that review further call on researchers “to develop a standardized framework on high quality diabetes care that is complemented by a practical tool to provide guidance to the design, implementation and evaluation of diabetes care programs.”
In an effort to address this call to action, the current research applies a comprehensive, theoretical model of health behavior change, known as the Information--Motivation--Behavioral Skills (IMB) model (J. D. Fisher & Fisher, 1992), to two critical diabetes self-care behaviors: diet and exercise. Although the basic tenants of the IMB model (J. D. Fisher & Fisher, 1992) have been empirically validated across a number of diverse populations and health promotion behaviors (Amico, Toro-Alfonso, & Fisher, 2005; J. D. Fisher, Amico, Fisher, & Harman, 2008; J. D. Fisher et al., 2004; J. D. Fisher, Fisher, Amico, & Harman, 2006), the model’s application to diabetes has been limited to one study (Osborn & Egede, 2009). In addition, while interventions based on the model have successfully promoted a range of health behaviors (W. A. Fisher, Fisher, & Harman, 2003), to our knowledge, no published diabetes intervention has used the IMB model to inform its design, content, delivery of content, implementation and evaluation of intervention efficacy. More importantly, no study has examined the utility of the model in designing intervention content for ethnic minorities.
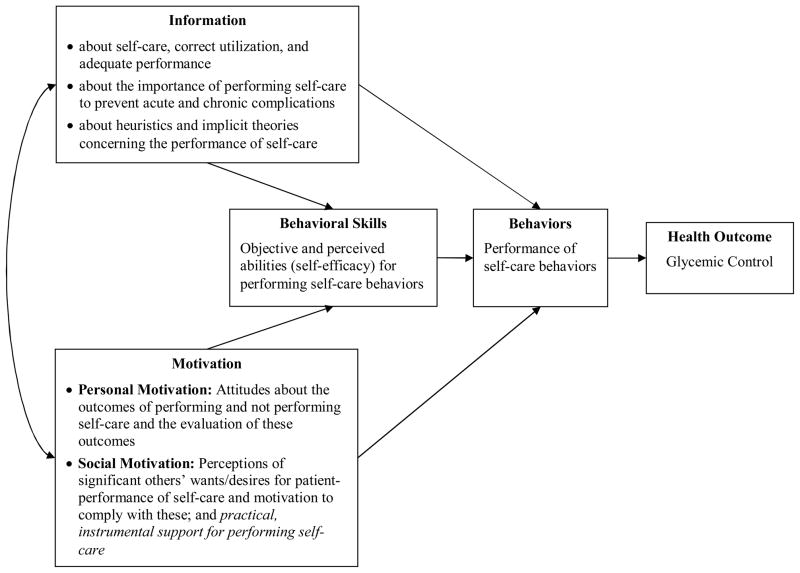
The IMB model identifies three core determinants of the initiation and maintenance of health behaviors: accurate information that can be readily translated into health behavior performance; personal and social motivation to act on such information; and behavioral skills to confidently and effectively implement the health behavior (J. D. Fisher, Fisher, Cornman et al., 2006; S. J. Misovich, Martinez, Fisher, Bryan, & Catapano, 2003; Murray, 2001; Starace et al., 2006). At a general level, the IMB model posits that performing a health behavior is a function of the extent to which someone is well-informed about the behavior, motivated to perform the behavior (e.g., has positive personal beliefs and attitudes towards the behavior or outcome, and social support for the behavior), and has the requisite skills to execute the behavior and confidence in their ability to do so across various situations. For complex behaviors, information and motivation are believed to work largely through the activation of relevant behavioral skills to bring about the initiation and maintenance of the behavior at focus. Information and motivation may also have direct effects on behavior when performance does not require complicated or novel behavioral skills.
According to the IMB model, information relevant to the performance of a behavior is a necessary but insufficient prerequisite to its enactment. Articulated to diabetes self-care behavior, the information construct would arguably include accurate information about specific diabetes self-care behaviors (e.g., exercise is important for managing diabetes). It would also include information concerning any health behavior performance required or recommended (e.g., knowledge of one’s daily recommended carbohydrate intake, and exercise requirements for glycemic control). Finally, it would also include heuristics and implicit theories that house misinformation about the behavior (e.g., “only sweet tasting foods raise blood glucose levels,” or “diet without exercise is enough to manage diabetes”) or heuristic decision rules which are actually accurate (e.g., “foods with carbohydrates raise blood glucose levels,” and “exercise and insulin lower blood glucose levels”).
In addition to behaviorally relevant information, the IMB model specifies that motivation is a critical determinant of whether or not even well-informed individuals will be inclined to enact a specific health behavior. The motivation construct of the IMB model is comprised of two components -- personal and social motivation (Amico et al., 2009; J. D. Fisher & Fisher, 1992; J. D. Fisher, Fisher, Amico et al., 2006). Following Fishbein & Ajzen (1975), personal motivation is a function of beliefs about the consequences of a behavior and evaluations of these consequences. Social motivation involves perceiving that there is normative support for a health behavior (e.g., that significant others, such as family, friends, and health care providers support its performance) and being motivated to comply with these referent others’ wishes (Fishbein & Ajzen, 1975; Pender & Pender, 1986). Articulated to diabetes self-care behavior, personal motivation would include one’s beliefs about the consequences of a diabetes self-care behavior (e.g., believing that monitoring carbohydrate intake and exercising every day would improve glycemic control; or, alternatively, would be intrusive and time consuming), and one’s evaluation of these consequences (e.g., monitoring carbohydrate intake and exercising every day would be a good or a bad thing to do). Social motivation for diabetes self-care would include one’s perceptions of significant others’ support for performing a specific diabetes self-care behavior (e.g., perceiving that important others believe one should monitor carbohydrate intake and exercise every day to manage diabetes), and one’s motivation to comply with these others’ wishes (e.g., “I want to do what my parent/doctor/spouse/friend/co-worker thinks I should do”) (Fishbein & Ajzen, 1975; Pender & Pender, 1986).
Finally, the IMB model identifies behavioral skills as a critical core determinant of complex health behaviors, which influences whether well-informed and well-motivated individuals will be capable of carrying out the health behavior effectively (Bandura, 1986). Behavioral skills include objective and perceived skills for performing the behavior (i.e., being able to enact the potentially complex and novel steps involved in its performance) and a sense of self-efficacy for doing so (i.e., one’s confidence in implementing the behavior in a variety of settings). Articulated to diabetes self-care behavior, behavioral skills may involve the ability to adequately perform a specific diabetes self-care behavior (e.g., one’s ability and confidence in monitoring carbohydrates - by identifying carbohydrate and serving size information on food labels, accurately calculating carbohydrate grams per serving of food, and estimating the appropriate serving size based on this amount; and the ability and confidence in exercising in different commonly occurring challenging situations - when the weather is bad, identifying a convenient time to exercise, after a long break in activity).
The goals of the current research are three-fold: (1) to articulate and validate the IMB model as initially described by Fisher and Fisher (1992) with two diabetes self-care behaviors: diet and exercise; (2) showcase the IMB model’s value across populations by sampling from a high risk, underserved, patient population of Puerto Rican Americans with Type 2 diabetes (T2DM); and (3) discuss the model’s utility in designing and evaluating diabetes self-care programs aimed at improving diet and physical activity in this and other patient populations.
Method
Participants and Procedures
Participants were recruited from an outpatient primary care clinic in Hartford, Connecticut. Eligible patients were of self-reported Puerto Rican ethnicity, 18 years of age or older, and had a clinical diagnosis of T2DM for at least one year. To generate a representative sample of diabetes patients receiving care at the clinic, two bilingual clinic staff members of Puerto Rican heritage generated a list of 260 eligible patients using four distinct sources: (a) physician referrals, (b) approaching patients in waiting rooms, (c) reviewing records of patients who had participated in research two-four years prior to this study, and (d) reviewing records of patients who had either received or were scheduled to receive a group-based diabetes education class. All 260 potential participants were called; 182 were contacted, 28 of these were not interested in participating and 25 were interested but unavailable to participate (11 had no transportation, 8 had no child care, 1 was too ill, and 5 had to work). Of the 129 patients who were scheduled, 118 arrived to participate in the study. All methods were approved by the Institutional Review Boards at the clinic and the University of Connecticut prior to study enrollment.
Clinic staff members scheduled patients to arrive at the clinic to complete informed consent procedures and participate in the study. Self-report measures were presented on laptop computers using computer assisted interview software. Patients read and/or listened to a voiceover recording of all items in English or Spanish (113 of the patients chose Spanish). Immediately following the self-report assessment, a qualified staff member tested patients’ glycated hemoglobin A1C levels. The entire assessment took approximately one hour. All patients received twenty dollars as compensation.
Measures
Demographics
Demographic information included age, gender, education, employment, English proficiency, language spoken most often at home, number of years in the U.S, insurance status, years diagnosed with diabetes, perceived health status, and measures of height and weight to calculate body mass index (BMI).
IMB Measures of Diabetes Self-Care
Information
Given the importance of monitoring carbohydrates for glycemic control (Sheard et al., 2004), information about diet self-care was measured by having respondents demonstrate accurate, stored knowledge of carbohydrate content in foods by correctly reporting whether or not foods familiar to the target group contain carbohydrates. From a list of thirteen different foods (e.g., plantains, papayas, mayonnaise, chicken), participants reported “yes,” “no,” or “I don’t know” to whether or not the food has carbohydrates. Participants were only provided with the name of the food, thus were required to draw from stored, in-memory information about its carbohydrate content. Information about exercise self-care was measured with seven items assessing the degree to which respondents knew the benefits of exercise for blood glucose control and general health. An example item is, “Exercise lowers blood sugar right away.” Likert responses range from 1=strongly disagree to 4=strongly agree. In a previous intervention study that administered the diet and exercise information measures (Osborn, 2006), internal consistency reliability ranged from α = 0.77 – 0.76 (min-max score: 0–13) and from α = 0.64 –0.77 (min-max score: 7–28), respectively. In this study, scores on diet information ranged from 0–13 and scores on exercise information ranged from 9–24. Scores are summed to create scaled composites.
Motivation
Existing valid and reliable IMB model-based motivation measures used in other disease contexts (J. D. Fisher, Fisher, Bryan, & Misovich, 2002;J. D. Fisher, Willcutts, Misovich, & Weinstein, 1998;W. A. Fisher & Fisher, 1993; W. A. Fisher, Fisher, & Rye, 1995; S.J. Misovich, Fisher, & Fisher, 1998) have guided the development of diabetes self-care measures of diet and exercise attitudes and subjective norms. An example two part diet attitudes item is, “During the next 30 days, how good/bad and pleasant/unpleasant would it be for you to monitor your carbohydrate intake at dinner?” An example two part exercise attitudes item is, “During the next 30 days, how good/bad and pleasant/unpleasant would it be to exercise every day.” Likert responses range from 1=very bad to 5=very good, and 1=very pleasant to 5=very unpleasant. An example diet subjective norms item is, “Most people who are important to me think I should keep track of how many carbohydrates I eat for dinner.” An example exercise subjective norms item is, “Most people who are important to me think I should walk everyday.” Likert responses range from 1=very untrue to 6=very true. In a previous intervention study that administered these measures (Osborn, 2006), internal consistency reliability for the diet and exercise attitude measures ranged from α = 0.80 – 0.82 (min-max score: 10–50), and from α = 0.70 – 0.81 (min-max score: 6–30), respectively; and subjective norms measures ranged from α = 0.85 – 0.91 (min-max score: 5–30) and from α = 0.85 – 0.88 (min-max score: 3–18), respectively. In this study, scores on diet and exercise attitudes ranged from 17–50 and 12–30, respectively. Scores on diet and exercise subjective norms ranged from 5–30 and 3–18, respectively. Scores are summed to create scaled composites.
Behavioral skills
Existing valid and reliable IMB model-based behavioral skills measures used in other disease contexts (J. D. Fisher et al., 2002; J. D. Fisher et al., 1998;W. A. Fisher & Fisher, 1993;W. A. Fisher et al., 1995;S.J. Misovich et al., 1998) have guided the development of diabetes self-care measures of diet and exercise behavioral skills. Consistent with other IMB model-based behavioral skills measures, items assess the perceived easiness and the perceived effectiveness of performing diabetes-specific diet and exercise self-care. Example diet behavioral skills items are: “How easy/hard would it be for you to eat breakfast, lunch, and dinner everyday?” and “How effectively/ineffectively could you use a Nutrition Facts label to could carbohydrates?” Example exercise behavioral skills items are, “How easy/hard would it be for you to pick a convenient time of day to exercise?” and “How effectively/ineffectively could you find activities to do when the weather is bad?” Likert responses range from 1=very hard to 4=very easy, and 1=very ineffectively to 4=very effectively. In a previous intervention study that administered these measures (Osborn, 2006), internal consistency reliability for the five-item diet and six-item exercise behavioral skills measures ranged from α = 0.67 - 0.69 (min-max score: 5–20) and from α = 0.70 – 0.77 (min-max score: 6–24), respectively. Because the diet items showed low internal consistency reliability as a full scale, items were separated to distinguish between the perceived easiness of performing self-care (α = 0.74 – 0.77; 3 items; min-max score 3–12) and the perceived effectiveness of performing self-care (α = 0.85 – 0.87; 2 items; min-max score 2–8). In this study, scores on diet easiness and effectiveness ranged from 3-12 and 2-8, respectively. Scores on exercise behavioral skills ranged from 6–24. Scores are summed to create scaled composites.
Diabetes Self-Care Behaviors
Food label reading
Food label reading was measured with a four-item scale that asked, “In the last 30 days, how often did you: look at the serving size information on a food label, look at food labels to look at the total carbohydrate content, count carbohydrates, and select foods that are low in carbohydrates.” Response options ranged from 1=never to 5=always. The mean score represents the frequency of food label reading behavior; and served as one of two indicators of diabetes self-care diet behavior in our analyses. In a previous intervention study that administered this same measure (Osborn, 2006), internal consistency ranged from α = .92–.94.
Diabetes self-care (diet behavior)
The diet subscale of the Summary of Diabetes Self-Care Activities questionnaire (SDSCA) is a standardized measure of diet behavior in diabetes (Toobert, Hampson, & Glasgow, 2000). Response options range from 0–7, corresponding to the number of days in a week. The average score across the four-item scale represents the frequency of adhering to diet recommendations in the past seven days.
Diabetes self-care (exercise behavior)
The exercise subscale of the SDSCA is a standardized measure of physical activity in diabetes (Toobert et al., 2000). Response options range from 0-7, corresponding to the number of days in a week. The average score across the two-item scale represents the frequency of being physically active in the past seven days.
Glycemic Control
Glycated hemoglobin (A1C) is the most widely used measure of glycemic control. Unlike oral glucose tolerance tests and glucometer readings, which measure blood glucose levels at a single point in time and are sensitive to food or drink consumption, A1C tests measure three-month average blood glucose concentrations and are unaffected by food and drink on the day of the test. In our study, a point-of-care immunoassay device that had been certified by the National Glychohemoglobin Standardization Program (NGSP) was used to measure patients’ A1C levels (Kennedy & Herman, 2005).
Analyses
The relationships among the IMB model constructs were estimated using AMOS 17.0, a structural equation modeling program. The estimated models correspond to the IMB model as initially described (J. D. Fisher & Fisher, 1992), and as illustrated in the Appendix. All paths indicated in the IMB model, except for the model’s proposed feedback loop from health outcomes back to information and motivation, were estimated in separate models for diet and exercise, as the two behaviors are not assumed to be necessarily related. All analyses were conducted with the correlation matrix generated by 118 cases. There was no missing data and the sample size was considered to be of adequate power to detect medium effects (Kline, 2004; Loehlin, 1992).
Appendix.
The Information—Motivation--Behavioral Skills model of Diabetes Self-Care (IMB-DSC)
The chi-square (χ2) goodness of fit statistic is a reasonable measure of model fit. However, because sample size and the strength of the correlations between variables may unpredictably influence model fit according to the χ2 test statistic, we relied on the comparative fit index (CFI) and root mean error of approximation (RMSEA) to assess model fit (Ridgon, 1996). Both indices have been recommended for routine use. CFI values that exceed 0.90 and RMSEA values below 0.08 indicate acceptable model fit (Ridgon, 1996); and RMSEA values below 0.05 indicate close fit (Browne & Cudeck, 1993). More recently, values close to 0.06 have been designated as indicative of “good fit” (Hu & Bentler, 1999). The CFI and the RMSEA are both sensitive to model misspecification and are minimally affected by sample size (Ridgon, 1996). Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients.
Results
A total of 118 Puerto Rican men and women completed all instruments noted above, including an A1C test. Participants were, on average, 58 years old, had lived in the U.S. for 25 years, and had been diagnosed with diabetes for 12 years. As indicated in Table 1, the majority were female (68.6%), reported low educational attainment (73.7% < high school or general equivalency diploma), were not working (94.1%) spoke only Spanish at home (84.7%), had health insurance (89%), and/or were morbidly obese (75.5%).
Table 1.
Patient Characteristics (N = 118)
| Variable | M ± SD |
|---|---|
| Age | 57.6 ± 10.4 |
| Female (%) | 68.6 |
| Education (%) | |
| < or = 8th grade | 56.8 |
| some high school | 16.9 |
| high school or GED | 16.9 |
| some college | 6.8 |
| college degree | 2.5 |
| Employed (%) | 5.9 |
| Married (%) | 30.5 |
| English proficiency, 0 = very poor to 5 = very good | 1.6 ± 1.5 |
| Speaks only Spanish at home (%) | 84.7 |
| Years lived in the United States | 24.6 ± 13.4 |
| Health insurance (%) | 89.0 |
| Years diagnosed with diabetes | 12.3 ± 10.3 |
| Perceived health status, 0 = very poor to 5 = very good | 2.5 ± 1.6 |
| Scores 0–1 (%) | 26.3 |
| Scores 2–3 (%) | 48.3 |
| Scores 4–5 (%) | 25.4 |
| Body Mass Index (BMI) | 35.4 ± 7.5 |
| Normal (BMI 18.5–24.9) (%) | 5.9 |
| Overweight (BMI 25 – 29.9) (%) | 18.6 |
| Obese (BMI ≥ 30) (%) | 75.5 |
Note: Data are means ± standard deviations unless otherwise indicated.
Evaluation of the IMB model of Diet Behavior
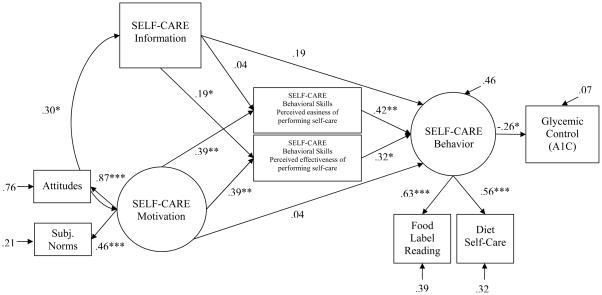
Table 2 presents the group means and standard deviations for each outcome assessment. As can be seen in Table 2, information scores did not appear to cluster towards the maximum possible score, although the overall sample did average towards the higher end of the potential maximum total score value. Skew and kurtosis suggested generally normal distributions. According to the CFI and RMSEA fit statistics, the estimated diet self-care model demonstrated barely adequate fit of the data (see Figure 1), χ2 (14, N = 118) = 25.83, p = 0.03, CFI = 0.90, RMSEA = 0.08 (90% CI: 0.03 – 0.14). Paths from information to behavioral skills (specifically, perceptions of effective implementation of skills), from motivation to behavioral skills, and from behavioral skills to behavior were significant and in the predicted direction. Information and motivation were significantly related to one another; and both were indirectly related to behavior through behavioral skills. The model constructs accounted for 46% of the variability in diet self-care behavior; and behavior was directly related to lower A1C levels (β = −0.26, p < 0.05).
Table 2.
Measurement Outcomes (N = 118)
| Variable | M ± SD |
|---|---|
| Information | |
| Diet (range 0–13) | 4.1 ± 3.0 |
| Exercise (range 7–28) | 17.6 ± 2.6 |
| Motivation | |
| Diet–attitudes (range 10–50) | 39.7 ± 7.4 |
| Exercise–attitudes (range 6–30) | 26.4 ± 4.6 |
| Diet - subjective norms (range 5–30) | 21.9 ± 6.0 |
| Exercise – subjective norms (range 3–18) | 14.5 ± 3.1 |
| Behavioral skills | |
| Diet–perceived easiness of performing self-care (range 3–12) | 8.8 ± 2.1 |
| Diet–perceived effectiveness of performing self-care (range 2–8) | 5.2 ± 1.9 |
| Exercise (range 6–24) | 16.4 ± 3.6 |
| Food label reading (range 1–5) | 2.5 ± 1.4 |
| Diet behavior (range 0–7) | 4.9 ± 2.2 |
| Exercise behavior (range 0–7) | 3.7 ± 2.7 |
| HbA1C | 7.7 ± 1.4 |
Figure 1. IMB model of Diabetes Self-care (Diet Behavior).
Note: Coefficients are standardized path coefficients. For tests of significance of individual paths: * p <. 05, **p < .01, and ***p < .001.
Evaluation of the IMB model of Exercise Behavior
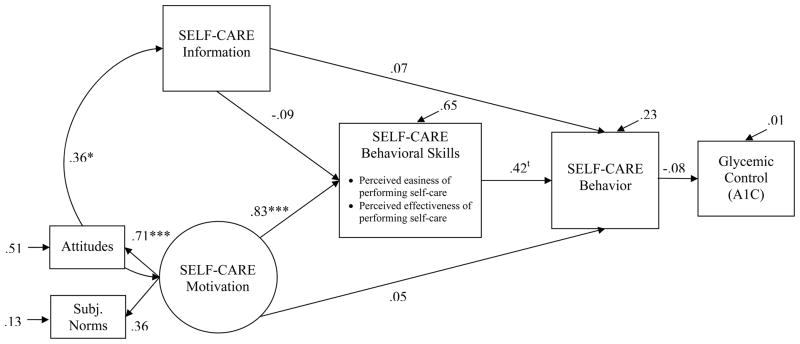
As can be seen in Table 2, across measures for information, motivation, and behavioral skills, the overall sample average suggested generally high funds of these factors relative to exercise behavior. Skew and kurtosis suggested generally normal distributions. As indicated in Figure 2, the estimated model demonstrated adequate/excellent fit of the data, χ2 (6, N = 118) = 2.56, p = 0.86, CFI = 1.00, RMSEA = 0.00 (90% CI: 0.00 – 0.06). The paths from exercise motivation to exercise behavioral skills and from exercise behavioral skills to exercise behavior were significant. The relation between motivation and behavior appeared completely mediated by behavioral skills. While information covaried significantly with motivation, there was no significant direct relationship between information and behavioral skills or information and behavior. The full model accounted for 23% of the variability in behavior, and behavior was not significantly associated with A1C measured concurrently.
Figure 2. IMB model of Diabetes Self-care (Exercise Behavior).
Note: Coefficients are standardized path coefficients. For tests of significance of individual paths, tp = .06, *p < .05, **p < .01 and ***p < .001.
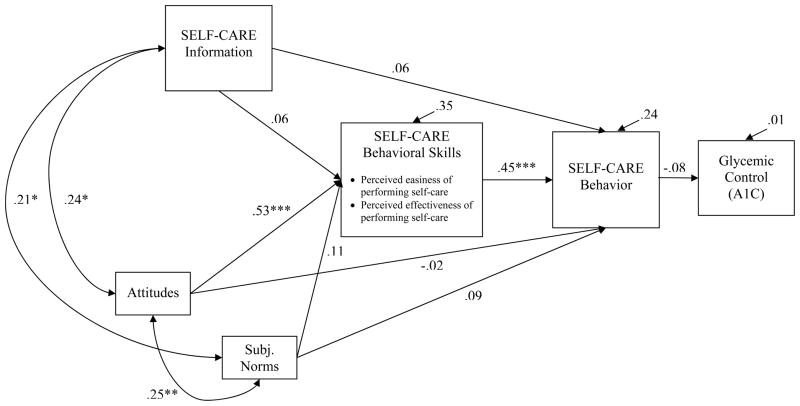
Because social norms demonstrated a low loading on the exercise motivation construct, we ran an additional altered model where exercise attitudes and subjective norms were permitted to covary, but were considered independent representations of diverse aspects of motivation. In this just identified model, the path from exercise attitudes to exercise behavioral skills was significant, as was the path from exercise behavioral skills to exercise behavior (see Figure 3). Exercise information and social norms did not demonstrate significant relations to either exercise behavioral skills or behavior. Similar to the full model, this just identified model accounted for 24% of the variability, and behavior was not related to A1C levels.
Figure 3. Exploratory IMB model of Diabetes Self-care (Exercise Behavior).
Note: Coefficients are standardized path coefficients. Just-identified model (no model fit indices). *p < .05, **p < .01 and ***p < .001.
Discussion
The IMB model of health behavior change (J. D. Fisher & Fisher, 1992; J. D.Fisher, Fisher, Amico et al., 2006;W. A. Fisher & Schachner, in press) was applied to conceptualize the determinants of two critical diabetes self-care behaviors–diet and exercise. These models were evaluated empirically with a sample of Puerto Rican American men and women with T2DM. Results indicated that, overall, the IMB-model based framework for understanding diet behavior was well positioned to explain the sample data. Diet-related information and motivation were associated with diet behavioral skills which were in turn associated with behavior, and finally behavior was linked to A1C levels. This is consistent with the IMB model which proposes that for complex behaviors (e.g., adhering to diet recommendations) information and motivation are insufficient determinants of behavior (Amico et al., 2005;J. D. Fisher et al., 2008; J. D. Fisher et al., 2004;J. D. Fisher, Fisher, Amico et al., 2006). While information and motivation may be important in acquiring skills and confidence, even the best informed and highly motivated individual is anticipated to struggle with adopting a complex health behavior in the absence of solid practical skills to do so. These results support the utility of the IMB model in organizing core determinants of diet behavior and suggest directions for IMB-model based interventions, where information, motivation, and behavioral skills would be formally targeted through behavioral intervention strategies.
For the exercise model, attitudes towards exercise were associated with exercise behavioral skills, which were independently associated with exercise behavior. Social norms for exercise, exercise-related information, and A1C levels were not significantly related to exercise behavior, or behavioral skills. While it is possible that the results do, in fact, accurately reflect a negligible influence of information and social norms on behavioral skills for our sample, we are limited in our conclusions by the nature of the measurements we used. With limited item sets and breadth of coverage of the information and social motivation constructs for exercise, it is possible that our measures lacked sufficient sensitivity.
In this study, social motivation focused on respondents’ perceptions of whether significant others wanted them to perform a behavior rather than actual, but also practical or instrumental support for the behavior (e.g., willingness to engage in the behavior with you, or assist you with performing the behavior) (Coffman, 2008). It is possible that, for exercise behavior particularly, the critical aspect of social motivation may be the extent to which the exercise behavior adopted is positioned as a social activity—where important others actually join the patient in exercise activities or actually facilitate exercising in instrumental ways versus reminders, verbalized desires, or purely social influence. Although our findings clearly highlight the importance of personal motivation (attitudes) towards exercise and exercise behavioral skills, additional research on information and social motivation (specifically instrumental support for a behavior) that can speak to a wider range of definitions of these dynamic and diverse constructs is an exciting area for future research.
Furthermore, the type, duration, and intensity of exercise and how these characteristics of physical activity are measured must be considered when interpreting the relationship between physical activity and glycemic control in research studies. In our study, we used a valid, but less frequently used measure of physical activity and found no association with A1C levels. Cross-sectional studies with type 1 diabetics have also reported non-significant relations between physical activity and glycemic control (Aman et al., 2009; Ligtenberg, Blans, Hoekstra, van der Tweel, & Erkelens, 1999); and prospective studies using pedometers with type 2 diabetics have demonstrated improvements in physical activity without improvements in glycemic control (Araiza, Hewes, Gashetewa, Vella, & Burge, 2006; Tudor-Locke et al., 2004). Other studies using objective measures of physical activity (e.g., accelerometers, cardiorespiratory fitness) have shown an association between improvements in exercise duration and glycemic control and other clinical outcomes (Kirk, Mutrie, MacIntyre, & Fisher, 2003). It is unclear if the failure to find an association between exercise behavior and A1C in the present research may be a function of measurement or of the cross-sectional nature of our research. While we assume that A1C is in fact related to exercise behavior, future tests of the IMB model’s utility in designing exercise interventions for patients with diabetes must establish that changes in exercise behavior as a result of an IMB-model based intervention do in fact produce the desired outcome of improved glycemic control.
Certain limitations of the study must be kept in mind. First, the sample size is small. While a sample size of 118 cases is sufficient (Kline, 2004; Loehlin, 1992) to provide a snap shot of the model’s utility in diabetes, the results should be interpreted with the knowledge that this is the first step in a line of future studies aimed at establishing the IMB model’s utility and relevance to a diverse population of T2DM patients. As such, the current results speak most clearly to the population under study, and should be replicated in different patient groups, and with larger samples. Second, although the IMB model proposes causal relationships between information, motivation, behavioral skills and self-care behavior, the current study measured these constructs cross-sectionally; thus, our results can most appropriately speak to associations between constructs observed at a single point in time, not causality. Future intervention research should be conducted to investigate the longitudinal effects of information, motivation, and behavioral skills constructs on changes in diabetes self-care behaviors. Third, because the SEM analysis presented here was based on self-report measures of the modeled constructs, objective, observable levels of diet and exercise behavioral skills were not assessed. Future work should incorporate ratings of actual performance of diet and exercise behaviors using food labels, portion control techniques, and supervised exercise. Finally, the study was unable to assess all aspects of behavioral skills relevant to diabetes (e.g., medication adherence, self-monitoring of blood glucose). Additional items that operationalize the full range of the constructs depicted in traditional IMB models (Amico et al., 2005;J. D. Fisher et al., 2008;J. D. Fisher, Fisher, Amico et al., 2006; J. D. Fisher, Fisher, Williams, & Malloy, 1994) with proper adaptation to the relevant aspects of diabetes self-care are needed. Items developed in the current study need to be further validated in larger studies in diverse populations.
Interestingly, results did suggest that generally one's diet and exercise behavior were positively correlated, as were funds of positive attitudes, social normative support, and behavioral skills between the two behaviors. Information, however, for diet behavior and for exercise behavior did not correlate significantly. Present results suggest that where improving attitudes, social norms, and skills for diet may positively influence these factors for exercise (and vice versa), information appears to be more unique to the behavior and more relevant to diet behavior, specifically. Information about exercise may have been unrelated to exercise behavior due to the type of information that was assessed, or because information about exercise is really not as influential of its practice compared to attitudes and behavioral skills. Additional studies are needed to identify whether the information construct for exercise or its measurement are problematic.
In conclusion, our findings suggest that, to improve adherence to diet recommendations among Puerto Rican patients with diabetes, interventions will need to include strategies that enhance patients’ diet-related attitudes, perceptions of norms and social support, and diet-related behavioral skills. Such strategies could include fostering positive perceptions of the consequences of diet management (helping individuals to reflect on accomplishments, positive reinforcements of efforts, supporting the development of beliefs about the association between diet choices and better health); decreasing negative beliefs about having to implement diet plans or restrictions (validating negative consequences and then providing reframing); and a strong emphasis on skills building in implementing appropriate diet choices (providing material on steps not only on how to implement the behavior but also on how to continue to reinforce efforts, gain social support, and manage negative affect, beliefs, and consequences).
Similarly, for exercise behavior, results suggest that attitudes and skills should be central targets of intervention efforts. Fostering strong beliefs about the positive consequences of exercise by identifying small goals to reach and celebrate, working from a risk reduction perspective, and providing not only reinforcement for efforts, but also validation of negative consequences of adopting this difficult behavior could assist in providing balanced motivation. Skills for how to implement exercise behaviors across situations and confidence in doing so can be fostered by modeling within exercise groups, exercise partners or buddies, and identification of several kinds of behaviors that could be considered under different challenging conditions. While information about diabetes itself may be of great value to patients on a number of levels, we did not observe this to be linked to the adoption of diet or exercise practices. For these behaviors, efforts to enhance motivation and skills appear more relevant.
Acknowledgments
We thank Demetria N. Cain, Luis Casillas, Andrew Dudley, Matt Dudley, Jill Irvine, Melissa Johnson, Beth La Pierre, Scott McCarthy, Erin Paice, Jane Quale, and Iliri Ibrahimi for their assistance in preparing materials. Special thanks to Carmen Aponte, Chariunis Perez, and Rosemary Perez for study recruitment, and collecting and managing data; Charlene Aponte for delivering the intervention; and Kenneth A. Wallston for his critique of this manuscript.
C.Y.O conducted this research under a National Research Service Award (NIDDK F31 DK067022), and is currently supported by a Diversity Supplement Award (NIDDK P60 DK020593-30S2). The study was supported by an American Psychological Association dissertation award and a pilot grant award from the Center for Health Intervention and Prevention at the University of Connecticut, Storrs, CT.
Footnotes
The authors have no conflict of interest.
References
- Aman J, Skinner TC, de Beaufort CE, Swift PG, Aanstoot HJ, Cameron F. Associations between physical activity, sedentary behavior, and glycemic control in a large cohort of adolescents with type 1 diabetes: the Hvidoere Study Group on Childhood Diabetes. Pediatric Diabetes. 2009;10(4):234–239. doi: 10.1111/j.1399-5448.2008.00495.x. [DOI] [PubMed] [Google Scholar]
- Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, et al. The information-motivation-behavioral skills model of ART adherence in a deep south HIV+ clinic sample. AIDS and Behavior. 2009;13(1):66–75. doi: 10.1007/s10461-007-9311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amico KR, Toro-Alfonso J, Fisher JD. An empirical test of the information, motivation and behavioral skills model of antiretroviral therapy adherence. AIDS Care. 2005;17(6):661–673. doi: 10.1080/09540120500038058. [DOI] [PubMed] [Google Scholar]
- Araiza P, Hewes H, Gashetewa C, Vella CA, Burge MR. Efficacy of a pedometer-based physical activity program on parameters of diabetes control in type 2 diabetes mellitus. Metabolism. 2006;55(10):1382–1387. doi: 10.1016/j.metabol.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Bandura A, editor. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bonow RO, Gheorghiade M. The diabetes epidemic: a national and global crisis. The American Journal of Medicine. 2004;116(Suppl 5A):2S–10S. doi: 10.1016/j.amjmed.2003.10.014. [DOI] [PubMed] [Google Scholar]
- Borgermans LA, Goderis G, Ouwens M, Wens J, Heyrman J, Grol RP. Diversity in diabetes care programmes and views on high quality diabetes care: are we in need of a standardized framework? International Journal of Integrated Care. 2008;8:e07. doi: 10.5334/ijic.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, Cudeck RI. Alternative ways of assessing model fit. In: Bollen K, Long K, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Cleghorn GD, Nguyen M, Roberts B, Duran G, Tellez T, Alecon M. Practice-based interventions to improve health care for Latinos with diabetes. Ethnicity & Disease. 2004;14(3 Suppl 1):S117–121. [PubMed] [Google Scholar]
- Coffman MJ. Effects of tangible social support and depression on diabetes self- efficacy. Journal of Gerontological Nursing. 2008;34(4):32–39. doi: 10.3928/00989134-20080401-02. [DOI] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Harris S. Theories and intervention approaches to health-behavior change in primary care. American Journal of Preventive Medicine. 1999;17(4):275–284. doi: 10.1016/s0749-3797(99)00094-x. [DOI] [PubMed] [Google Scholar]
- Fishbein M, Ajzen I. Belief, attitude, intention and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley; 1975. [Google Scholar]
- Fisher JD, Amico KR, Fisher WA, Harman JJ. The information-motivation-behavioral skills model of antiretroviral adherence and its applications. Current HIV/AIDS Reports. 2008;5(4):193–203. doi: 10.1007/s11904-008-0028-y. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated HIV risk reduction intervention for HIV-positive persons: Formative Research, Acceptability, and Fidelity of the Options Project. Journal of Acquired Immune Deficiency Syndrome. 2004;37(Suppl 2):S78–87. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychological Bulletin. 1992;111(3):455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychology. 2006;25(4):462–473. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Bryan AD, Misovich SJ. Information-motivation-behavioral skills model-based HIV risk behavior change intervention for inner-city high school youth. Health Psychology. 2002;21(2):177–186. [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Acquired Immune Deficiency Syndrome. 2006;41(1):44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA, Williams SS, Malloy TE. Empirical tests of an information-motivation-behavioral skills model of AIDS-preventive behavior with gay men and heterosexual university students. Health Psychology. 1994;13(3):238–250. doi: 10.1037//0278-6133.13.3.238. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Willcutts DLK, Misovich SJ, Weinstein B. Dynamics of sexual risk behavior in HIV-infected men who have sex with men. AIDS and Behavior. 1998;2:101–113. [Google Scholar]
- Fisher WA, Fisher JD. A general social psychological model for changing AIDS risk behavior. In: Pryor J, Reeder G, editors. The Social Psychology of HIV Infection. Hillside, NJ: Erlbaum; 1993. [Google Scholar]
- Fisher WA, Fisher JD, Harman J. The information-motivation-behavioral skills model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social Psychological Foundations of Health and Illness. Malden, MA: Blackwell; 2003. pp. 82–106. [Google Scholar]
- Fisher WA, Fisher JD, Rye BJ. Understanding and promoting AIDS-preventive behavior: Insights from the theory of reasoned action. Health Psychology. 1995;14(3):255–264. doi: 10.1037//0278-6133.14.3.255. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Schachner H. Self-monitoring of blood glucose in diabetic children and adolescents--barriers, behaviors, and the search for solutions. US Endocrinology in press. [Google Scholar]
- Gollenberg A, Pekow P, Markenson G, Tucker KL, Chasan-Taber L. Dietary behaviors, physical activity, and cigarette smoking among pregnant Puerto Rican women. The American Journal of Clinical Nutrition. 2008;87(6):1844–1851. doi: 10.1093/ajcn/87.6.1844. [DOI] [PubMed] [Google Scholar]
- Hu L-t, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Kennedy L, Herman WH. Glycated hemoglobin assessment in clinical practice: comparison of the A1cNow point-of-care device with central laboratory testing (GOAL A1C Study) Diabetes Technology and Therapeutics. 2005;7(6):907–912. doi: 10.1089/dia.2005.7.907. [DOI] [PubMed] [Google Scholar]
- Kirk A, Mutrie N, MacIntyre P, Fisher M. Increasing physical activity in people with type 2 diabetes. Diabetes Care. 2003;26(4):1186–1192. doi: 10.2337/diacare.26.4.1186. [DOI] [PubMed] [Google Scholar]
- Kline R. Principles and practice of structural equation modeling. 2. New York: Guilford; 2004. [Google Scholar]
- Ligtenberg PC, Blans M, Hoekstra JB, van der Tweel I, Erkelens DW. No effect of long-term physical activity on the glycemic control in type 1 diabetes patients: a cross-sectional study. The Netherlands Journal of Medicine. 1999;55(2):59–63. doi: 10.1016/s0300-2977(99)00039-x. [DOI] [PubMed] [Google Scholar]
- Lipton RB, Losey L, Giachello AL, Corral M, Girotti MH, Mendez JJ. Factors affecting diabetes treatment and patient education among Latinos: results of a preliminary study in Chicago. Journal of Medical Systems. 1996;20(5):267–276. doi: 10.1007/BF02257040. [DOI] [PubMed] [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural analysis. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- Melnik TA, Hosler AS, Sekhobo JP, Duffy TP, Tierney EF, Engelgau MM, et al. Diabetes prevalence among Puerto Rican adults in New York City, NY, 2000. American Journal of Public Health. 2004;94(3):434–437. doi: 10.2105/ajph.94.3.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misovich SJ, Fisher WA, Fisher JD. A measure of AIDS prevention information, motivation, behavioral skills, and behavior. In: Davis CM, Yarber WH, Bauserman R, Schreer G, Davis SL, editors. Handbook of Sexuality Related Measures. Sage Publishing; 1998. pp. 328–337. [Google Scholar]
- Misovich SJ, Martinez T, Fisher JD, Bryan A, Catapano N. Predicting breast self-examination: A test of the information-motivation-behavioral skills model. Journal of Applied Social Psychology. 2003;33(4):775–790. [Google Scholar]
- Murray DM. Unpublished Master's Thesis. University of Connecticut; Storrs, CT: 2001. Exploring motorcycle safety gear use: A theoretical approach. [Google Scholar]
- Osborn CY. Using the IMB model of health behavior change to promote self-management behaviors in Puerto Ricans with diabetes. Dissertation Abstracts International Section A: Humanities and Social Sciences. 2006;67(6-A):2064. [Google Scholar]
- Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC) Patient Education and Counseling. 2009 doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pender NJ, Pender AR. Attitudes, subjective norms, and intentions to engage in health behaviors. Nursing Research. 1986;35(1):15–18. [PubMed] [Google Scholar]
- Ridgon E. CFI versus RMSEA: Comparison of two fit indexes for structural equation modeling. Structural Equation Modeling. 1996;3:369–379. [Google Scholar]
- Sheard NF, Clark NG, Brand-Miller JC, Franz MJ, Pi-Sunyer FX, Mayer-Davis E, et al. Dietary carbohydrate (amount and type) in the prevention and management of diabetes: a statement by the american diabetes association. Diabetes Care. 2004;27(9):2266–2271. doi: 10.2337/diacare.27.9.2266. [DOI] [PubMed] [Google Scholar]
- Smith CA, Barnett E. Diabetes-related mortality among Mexican Americans, Puerto Ricans, and Cuban Americans in the United States. Pan American Journal of Public Health. 2005;18(6):381–387. doi: 10.1590/s1020-49892005001000001. [DOI] [PubMed] [Google Scholar]
- Starace F, Wagner TM, Luzi AM, Cafaro L, Gallo P, Rezza G. Knowledge and attitudes regarding preventative HIV vaccine clinical trials in Italy: results of a national survey. AIDS Care. 2006;18(1):66–72. doi: 10.1080/09540120500161777. [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Bell RC, Myers AM, Harris SB, Ecclestone NA, Lauzon N, et al. Controlled outcome evaluation of the First Step Program: a daily physical activity intervention for individuals with type II diabetes. International Journal of Obesity. 2004;28(1):113–119. doi: 10.1038/sj.ijo.0802485. [DOI] [PubMed] [Google Scholar]
- Vazquez IM, Millen B, Bissett L, Levenson SM, Chipkin SR. Buena Alimentacion, Buena Salud: a preventive nutrition intervention in Caribbean Latinos with type 2 diabetes. American Journal of Health Promotion. 1998;13(2):116–119. doi: 10.4278/0890-1171-13.2.116. [DOI] [PubMed] [Google Scholar]
- Whitman S, Silva A, Shah AM. Disproportionate impact of diabetes in a Puerto Rican community of Chicago. Journal of Community Health. 2006;31(6):521–531. doi: 10.1007/s10900-006-9023-7. [DOI] [PubMed] [Google Scholar]
- Whittemore R. Strategies to facilitate lifestyle change associated with diabetes mellitus. Journal of Nursing Scholarship. 2000;32(3):225–232. doi: 10.1111/j.1547-5069.2000.00225.x. [DOI] [PubMed] [Google Scholar]