Abstract
Objective
To determine age-adjusted rates (AAR) of lower urinary tract (LUT) injury and incidence in selected inpatient gynecologic and obstetric procedures.
Study Design
We utilized the National Hospital Discharge Survey, 1979–2006. AAR of non-obstetric bladder and ureteral injuries and incidence of LUT injury for various hysterectomy types and deliveries were calculated for women > 18 years old.
Results
Overall AAR of ureteral injury decreased from 0.06 to 0.03 per 1000 women (1979–2006). AAR of inpatient gynecologic procedures decreased from 24.9 to 11.8 per 1000 women (1979–2006). By hysterectomy type, bladder injury was highest in LAVH (13.8 per 1000) and VH (13.1 per 1000). Ureteral injury recognized during hysterectomy was most common with radical hysterectomy (7.7 per 1000) and least common with LAVH (0 per 1000).
Conclusions
Ureteral injuries at time of inpatient surgical procedures have decreased from 1979–2006. This corresponds with a sharp decrease in inpatient gynecologic procedures.
Keywords: bladder injury, ureteral injury, gynecologic surgery
Introduction
Lower urinary tract (LUT) injury is a potentially devastating complication of gynecologic and obstetric procedures. Bladder and ureteral injury may be associated with significant short-term and long-term morbidity including increased initial operative time, return to the operating room for subsequent procedures, need for prolonged indwelling catheter drainage, urinary tract infection, fistula formation, and loss of renal function.1–6 Urinary tract injury may also lead to socioeconomic sequelae including temporary or permanent loss of employment, anxiety, depression, and deterioration of interpersonal relationships.7 Physicians involved in gynecologic surgery resulting in urinary tract injury may experience significant personal and financial costs related to the high relative risk of litigation.7
The incidence of LUT injury at time of gynecologic surgery and obstetric procedures has been poorly studied. Based on systematic review of benign gynecologic surgery, estimated rates of bladder injury associated with hysterectomy ranged from 0.3 – 6.0 per 1000 surgeries and ureteral injury ranged from 0.2 – 7.3 per 1000 surgeries.8 The estimated rate of bladder injury associated with other gynecologic or urogynecologic surgery was 11.2 per 1000 surgeries and the rate of ureteral injury was 2.2 per 1000 surgeries.8 The data regarding the risk of urinary tract injury at time of obstetric procedures is also limited.9, 10 Case-control data demonstrate an incidence of bladder injury of 0.28% at time of cesarean delivery.11
The primary objective of this study was to determine age-adjusted rates of non-obstetric LUT injury in the United States from 1979–2006. Secondarily, we sought to determine the incidence of LUT injury among women undergoing selected inpatient gynecologic and obstetric procedures. LUT injury associated with various types of hysterectomy was calculated. The incidence of bladder and urethral injury at time of spontaneous vaginal delivery, operative vaginal delivery, and cesarean delivery was determined.
Materials and Methods
The National Hospital Discharge Survey (NHDS) is a federal dataset compiled by the National Center for Health Statistics. This dataset is a national probability sample of non-Federal short-stay hospitals in the US based on approximately 270,000 inpatient records acquired from 466 hospitals annually. The overall dataset error rate for final diagnoses and procedures is 1.0% and 0.7%, respectively.12
University of Pittsburgh Institutional Review Board exempt status was obtained. Using International Classification of Diseases, 9th revision, Clinical Modification (ICD-9-CM) procedure codes, this dataset was used to identify women who sustained bladder injuries (obstetric and non-obstetric) and ureteral injuries. ICD-9-CM procedure codes were also used to estimate the annual number of inpatient gynecologic procedures, 1979–2006.
Women who sustained a bladder and/or ureteral injury at time of hysterectomy were identified using ICD-9-CM procedure codes for non-obstetric bladder and/or ureteral injury (Table 1) and hysterectomy. Hysterectomy types included: subtotal abdominal hysterectomy (SAH; 68.3, 68.39), laparoscopic supracervical hysterectomy (LSH; 68.31), total abdominal hysterectomy (TAH; 68.4), vaginal hysterectomy (VH; 68.5, 68.59), laparoscopic-assisted vaginal hysterectomy (LAVH; 68.51), and radical abdominal hysterectomy (RAH; 68.6).
Table 1.
Variable Names and Associated ICD-9-CM Procedure Codes
| Variable | Procedure Name | ICD-9-CM Procedure Code |
|---|---|---|
| Obstetric bladder and urethral injury | Repair of current obstetric laceration of bladder and urethra | 75.61 |
| Non-obstetric bladder injury | Suture of laceration of bladder | 57.81 |
| Closure of cystotomy | 57.82 | |
| Other repair of bladder | 57.89 | |
| Ureteral injury | Ureteroneocystotomy | 56.74 |
| Transureteroureterostomy | 56.75 | |
| Other anastamosis or bypass of ureter | 56.79 | |
| Suture of laceration of ureter | 56.82 | |
| Closure of ureterostomy | 56.83 | |
| Closure of other fistula of ureter | 56.84 | |
| Ureteropexy | 56.85 | |
| Removal of ligature from ureter | 56.86 | |
| Other repair of ureter | 56.89 |
ICD-9-CM, International Classification of Diseases, 9th Revision, Clinical Modification
Similarly, women who sustained a bladder injury at time of delivery were identified. Deliveries were classified as spontaneous vaginal, operative vaginal (forceps-assisted and vacuum-assisted), or cesarean. Both diagnosis and procedure codes were used to identify deliveries in order to reflect a change in coding practices in the late 1980s which favored the use of procedure codes. Obstetric bladder injuries also include urethral injuries since one ICD-9-CM code exists for this type of injury (Table 1).
To determine disease-classes associated with non-obstetric bladder and ureteral injuries, ICD-9-CM diagnosis codes were used. The NDHS dataset contains up to seven diagnosis codes. Only the primary (first) diagnosis code was considered in this analysis.
Incidence of bladder and ureteral injury and obstetric bladder/urethral injury was calculated for various hysterectomy types and delivery types, respectively. Age-adjusted rates for bladder injuries, ureteral injuries, inpatient gynecologic procedures, and cesarean delivery were calculated using 1990 census data for women > 18 years of age. For accuracy, age-adjustment and frequencies were calculated for each year, 1979 – 2006. Population weighting ratio adjustments were performed according to the NHDS study design.12 Linear regression was used to assess trends in bladder (obstetric and non-obstetric) and ureteral injury rates over the study time period. Statistical analysis was performed using SPSS (version 17.0; SPSS Inc., Chicago, IL). Statistical significance was evaluated at the p <0.05 level.
Results
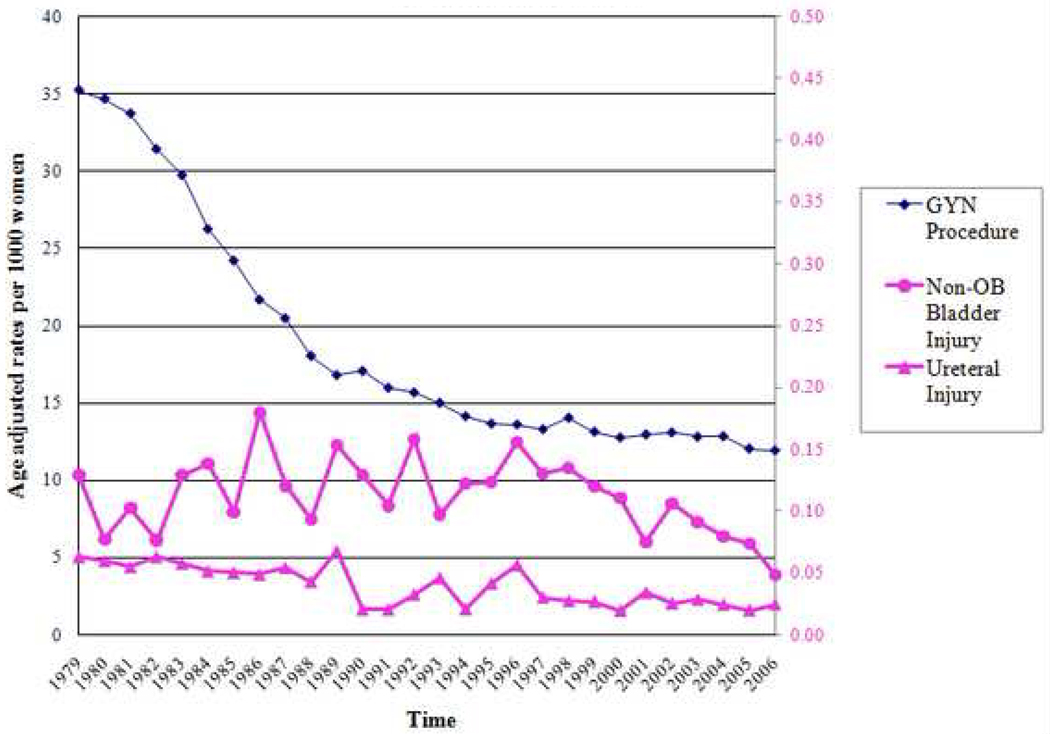
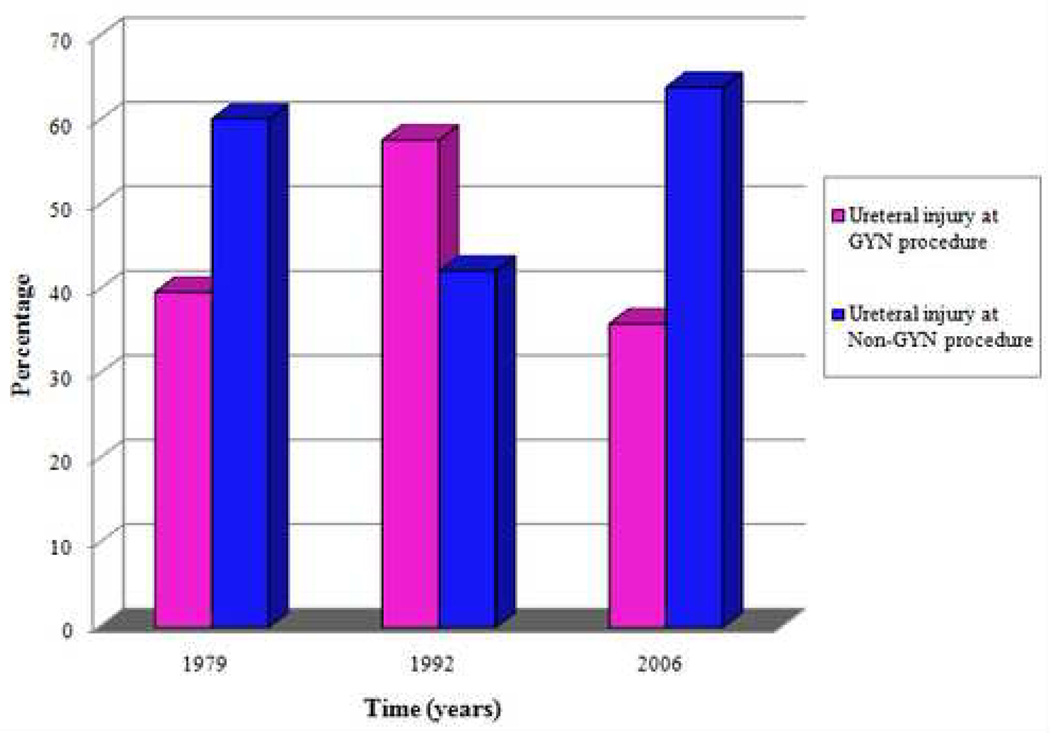
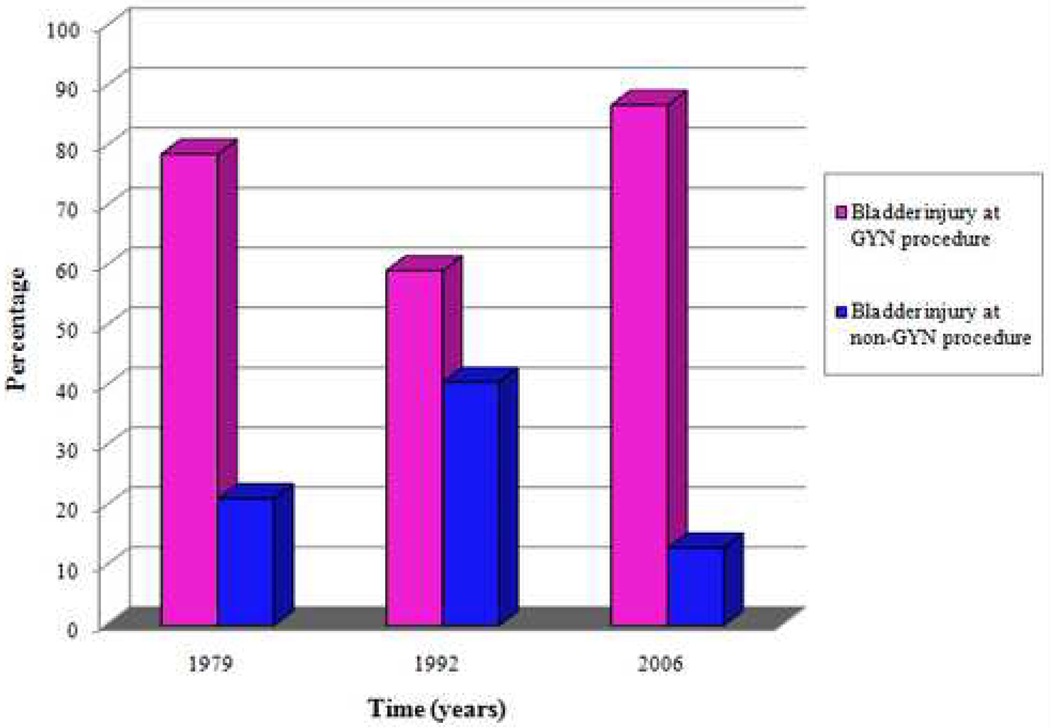
During the study period, AAR of inpatient gynecologic procedures decreased from 35.2 per 1000 women (1979) to 11.9 per 1000 women (2006) (P < 0.001). AAR of ureteral injury per 1000 women decreased from 0.06 (1979) to 0.03 (2006) (P < 0.001). AAR of non-obstetric bladder injury per 1000 women varied from 0.13 (1979) to 0.05 (2006) (P = 0.11) (Figure 1). In 2006, 64% of ureteral injuries recognized at the time of surgery were associated with non-gynecologic procedures (Figure 2). In contrast, 87% of non-obstetric bladder injuries in 2006 recognized at the time of surgery were associated with gynecologic procedures (Figure 3).
Figure 1.
Age-adjusted rates of Inpatient Procedures per 1000 Women from 1979 to 2006 in the United States
Figure 2.
Percentage of Ureteral Injuries at Time of Gynecologic Procedures Versus Non-Gynecologic Procedures
Figure 3.
Percentage of Bladder Injuries at Time of Gynecologic Procedures Versus Non-Gynecologic Procedures
During the study period, 49.8 million gynecologic procedures and 58.6 million non-gynecologic abdominal procedures were performed. Abdominal hysterectomy was performed in 11.7 million women and 4.3 million vaginal hysterectomies were performed. Alternate routes of hysterectomy were utilized less frequently: LAVH (591,069), SAH (327,857), RAH (141,938), and LSH (38,887).
Among women undergoing hysterectomy, the incidence of bladder injury was highest in women undergoing LAVH (13.8 per 1000 women) and VH (13.1 per 1000 women). Lower incidence of bladder injury was observed with TAH (6.9 per 1000 women), SAH (10.3 per 1000 women), RAH (2.2 per 1000 women), and LSH (0 per 1000 women). Ureteral injury recognized at time of hysterectomy was most common with RAH (7.7 per 1000) and TAH (1.2 per 1000) and least common with LAVH (0 per 1000). The incidence of ureteral injury with VH, SAH, and LSH was 0.7, 0.6, and 0.6 per 1000 women, respectively.
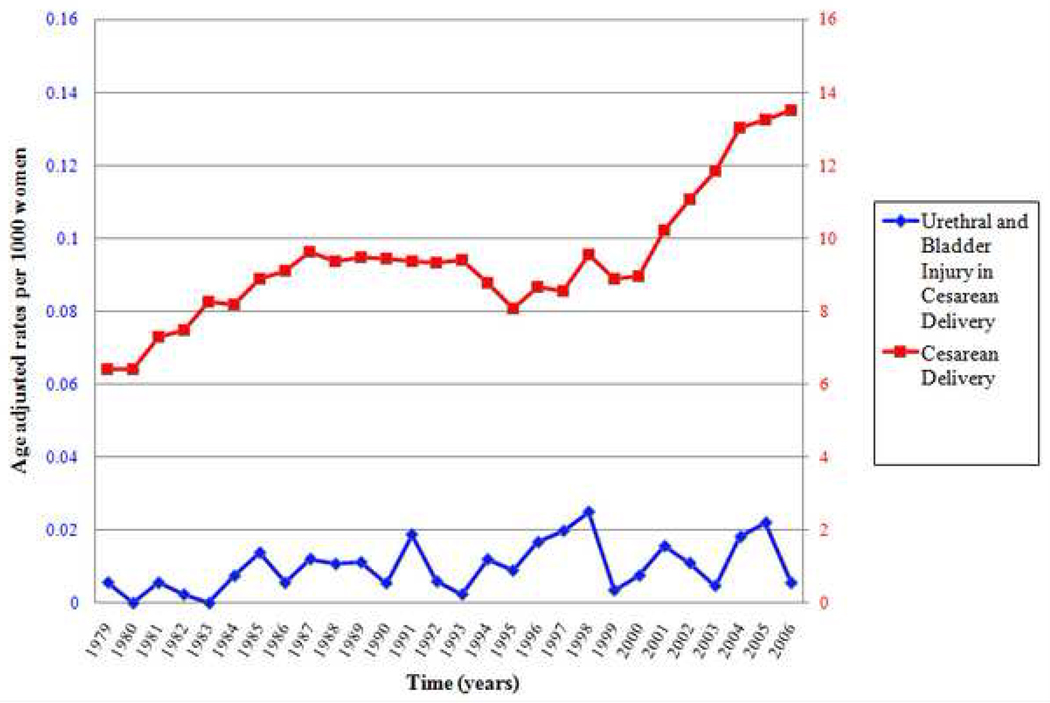
Urethral or bladder injury occurred at the time of SVD in 10.3 per 1000 women and 4.8 per 1000 women with OVD. AAR of cesarean delivery increased significantly from 6.4 per 1000 women (1979) to 13.5 per 1000 women (2006) (P < 0.001). Recognized bladder injury at time of cesarean delivery varied over the study time period from 0.006 per 1000 deliveries (1979) to 0.03 per 100,000 deliveries (1998) to 0.006 per 1000 deliveries (2006) (P = 0.01).
Pelvic organ prolapse and urinary incontinence were the most common primary diagnoses in women with non-obstetric bladder injury. Gynecologic malignancy was the diagnosis most frequently associated with ureteral injury (Table 2).
Table 2.
Primary Diagnoses in Women with Non-Obstetric Bladder and Ureteral Injuries, 1979–2006
| Primary Diagnosis | Non-Obstetric Bladder Injury (N= 315,755) |
Ureteral Injury (N = 109,589) |
|---|---|---|
| Urinary incontinence | 68,690 (21.8%) | 1,251 (1.1%) |
| Pelvic organ prolapse | 56,417 (17.9%) | 4,298 (3.9%) |
| Fibroids | 38,233 (12.1%) | 3,907 (3.6%) |
| Endometriosis | 12,862 (4.1%) | 4,362 (4.0%) |
| Trauma | 9,395 (3.0%) | 267 (0.2%) |
| Gynecologic malignancy, neoplasm, or dysplasia* | 25,556 (8.1%) | 8,218 (7.5%) |
| Non-gynecologic abdominal malignancy, neoplasm, or dysplasia† | 2,350 (0.7%) | 3,523 (3.2%) |
excludes fibroids
excludes urinary tract malignancy or neoplasm
Comment
Gynecologic procedures have traditionally accounted for the majority of iatrogenic lower urinary tract injuries.5 Although we observed a decrease in age-adjusted rates of ureteral injuries corresponding with a sharp decrease in age-adjusted rates of inpatient gynecologic procedures, non-obstetric bladder injuries did not change significantly over the study time period. Although the majority of non-obstetric bladder injuries recognized at the time of surgery appear to be associated with gynecologic procedures, most (64% in 2006) ureteral injuries recognized at the time of surgery appear to occur in association with non-gynecologic procedures. This finding indicates that a greater proportion of ureteral injuries may be associated with non-gynecologic procedures than previously attributed.
The most common major gynecologic procedure is hysterectomy. Approximately 600,000 hysterectomies are performed in the United States each year.13 Although laparoscopy remains the least common approach, patients and surgeons have become increasingly interested in minimally invasive surgical modalities.14 Our data suggest that LAVH poses the highest risk for bladder injury. These findings are consistent with those previously reported which demonstrate a higher incidence of bladder injury related to laparoscopic-assisted hysterectomy as compared to abdominal and vaginal hysterectomy.6
Interestingly, we estimated the incidence of bladder injury at LSH and ureteral injury at LAVH as 0 per 1000 women. These data conflict with previous authors’ data that demonstrate the risk of LUT injury associated with hysterectomy to be highest when a laparoscopic-assisted approach is utilized.6 Because the NHDS dataset is limited to individual cases without linkage data for subsequent or follow-up procedures, only injuries which occur at time of the index procedure are accessible. It is unlikely that coding error accounts for these data given the low overall error rate associated with the NHDS procedure codes (0.7%).12 Rather, we hypothesize that the low frequency of ureteral injury at time of LAVH and bladder injury at LSH may be attributed to lack of intraoperative recognition. Since repair of bladder or ureteral injury recognized at the time of laparoscopic procedure often results in the conversion to an open procedure, it is likely that the low frequency of these injuries is also related to coding practices. A laparoscopic procedure converted to an open procedure is coded as an open procedure.
The value of routine intraoperative cystoscopy for detection of LUT injury is unclear.8, 15 Given the limitations of the NHDS dataset, we are unable to comment regarding the role of cystoscopy at the time of hysterectomy or other inpatient gynecologic procedures. Specifically, we cannot determine whether injuries that occurred during the index surgery were identified using cystoscopy or direct visualization. In the cases utilizing cystoscopy, we are unable to determine whether use was routine or selective. Given the overall low risk of cystoscopy and intravenous indigo carmine administration and the high rate of bladder and ureteral injury associated with hysterectomy, routine cystoscopy at conclusion of a hysterectomy to evaluate for bladder injury and ureteral patency seems a reasonable and prudent option.
Bladder or urethral injury at the time of vaginal delivery occurred twice as frequently with SVD as compared to OVD. We hypothesize that this finding is related to the high frequency of periurethral laceration at SVD and the associated practice of coding this injury using the ICD-9-CM code for obstetric bladder and urethral injury (75.61).
In recent years, increasing attention has been paid to the surgical risks associated with cesarean delivery. Particular concern has been raised regarding these risks in the setting of cesarean delivery on maternal request (CDMR) and women undergoing multiple cesarean deliveries. Data regarding risk of bladder injury at time of cesarean delivery are limited.11 Bladder injury risk is likely related to the number of previous cesarean deliveries, individual patient characteristics including adhesion formation and scarring, and whether the patient is labored or non-labored.. Although we are not able to reliably distinguish between primary or repeat cesarean delivery based on limitations of the ICD-9-CM coding system and the NHDS dataset, despite the sharp increase in cesarean delivery, bladder injury has remained low. We hypothesize that this observation is likely related to a greater proportion of elective repeat cesarean deliveries which may carry a lower risk profile. CDMR may also contribute to the increase in AAR of cesarean deliveries, although recent estimates of CDMR are low, ranging from 0.17–0.82% of total deliveries in the United States (2000–2004).16
The NHDS is one of the most comprehensive, publicly-funded, accessible databases available. Use of this dataset allowed us to examine trends in LUT injury and estimate total gynecologic procedures during a 28 year period. The absence of linkage data in the NHDS dataset prohibits observations regarding LUT injuries identified postoperatively. A patient with a LUT injury not recognized at the time of surgery who is readmitted to the hospital following discharge after the index surgery may not be coded with a gynecologic primary diagnosis code. As a result, our analysis may underestimate the frequency of LUT in women whose primary diagnosis is gynecologic.
ICD-9-CM codes used for hysterectomy reflect current and previous coding practices. Coding for hysterectomy has expanded in order to include specific subtypes of hysterectomy. Prior to the coding expansion, hysterectomy subtypes were coded under the more general hysterectomy code (three-digit codes). As a result, LUT injury associated with subtotal abdominal hysterectomy may be underestimated. Bladder injury with vaginal hysterectomy may be overestimated and ureteral injury may be underestimated.
All surgical procedures carry an inherent risk of injury to adjacent structures. LUT injury has been reported in association with nearly every gynecologic procedure. Disclosure of potential surgical risks is an important component of preoperative counseling and the informed consent process. These data will assist surgeons in the US in accurately counseling patients regarding trends in LUT injuries, rates of gynecologic procedures, and the incidence of various injuries at the time of hysterectomy, vaginal and cesarean delivery.
Figure 4.
Age-adjusted rates of Urethral and Bladder Injury at the Time of Cesarean Delivery per 1000 Women in the United States, 1979–2006
Acknowledgments
Financial acknowledgements: This publication was made possible by Grant Number UL1 RR024153 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on NCRR is available at http://www.ncrr.nih.gov/.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This research was presented at the 30th Annual Meeting of the American Urogynecologic Society, Hollywood, FL, September 24–26, 2009.
References
- 1.Meikle S, Weston N, Orleans M. Complications and recovery from laparoscopy-assisted vaginal hysterectomy compared with abdominal and hysterectomy. Obstet Gynecol. 1997;89:304–311. doi: 10.1016/S0029-7844(96)00315-8. [DOI] [PubMed] [Google Scholar]
- 2.Goodno J, Powers T, Harris V. Ureteral injury in gynecologic surgery: tenyear review in a community hospital. Am J Obstet Gynecol. 1995;172:1817–1813. doi: 10.1016/0002-9378(95)91417-x. [DOI] [PubMed] [Google Scholar]
- 3.Buckspan M, Simha S, Klotz P. Vesicouterine fistula: a rare complication cesarean section. Obstet Gynecol. 1983;62:64s–66s. [PubMed] [Google Scholar]
- 4.Drake M, Noble J. Ureteric trauma in gyencologic surgery. Int Urogynecol. 1998;9:108–117. doi: 10.1007/BF01982219. [DOI] [PubMed] [Google Scholar]
- 5.Symmonds R. Ureteral injuries associated with gynecologic surgery: Prevention and management. Clin Obstet Gynecol. 1976;19:623–643. doi: 10.1097/00003081-197609000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Harkki-Siren P, Sjoberg J, Tiitinen A. Urinary tract injuries after hysterectomy. Obstet Gynecol. 1998;92:113–118. doi: 10.1016/s0029-7844(98)00146-x. [DOI] [PubMed] [Google Scholar]
- 7.Gilmour D, Baskett T. Disability and litigation from urinary tract injuries benign gynecologic surgery in Canada. Obstet Gynecol. 2005;105:109–114. doi: 10.1097/01.AOG.0000144127.78481.8c. [DOI] [PubMed] [Google Scholar]
- 8.Gilmour D, Das S, Flowerdew G. Rates of urinary tract injury from gynecologic surgery and the role of interoperative cystoscopy. Obstet Gynecol. 2006;107:1366–1372. doi: 10.1097/01.AOG.0000220500.83528.6e. [DOI] [PubMed] [Google Scholar]
- 9.Kaskarelis D, Sakkas J, Aravantinos D, Michalas S, Zolotas J. Urinary tract injuries in gynecological and obstetrical procedures. Int Surg. 1975;60:40–43. [PubMed] [Google Scholar]
- 10.Rajasekar D, Hall M. Urinary tract injuries during obstetric intervention. Obstet Gynaecol. 1997;104:731–734. doi: 10.1111/j.1471-0528.1997.tb11986.x. [DOI] [PubMed] [Google Scholar]
- 11.Phipps M, Watabe B, Clemons J, Weitzen S, Myers D. Risk factors for bladder injury during cesarean delivery. Obstet Gynecol. 2005;105:156–160. doi: 10.1097/01.AOG.0000149150.93552.78. [DOI] [PubMed] [Google Scholar]
- 12.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat. 2000;1:1–42. [PubMed] [Google Scholar]
- 13.Keshavarz H, Hillis S, Kieke B, Marchbanks P. Hysterectomy surveillance- United States, 1994–1999. MMWR CDC Surveill Summ. 2002;51:1–8. [PubMed] [Google Scholar]
- 14.Wu J, Wechter MG, E J, Nguyen T, Visco A. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–1095. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 15.Ibeanu O, Chesson R, Echols K, Nieves M, Busangu F, Nolan T. Urinary tract injury during hysterectomy based on universal cystoscopy. Obstet Gynecol. 2009;113:6–10. doi: 10.1097/AOG.0b013e31818f6219. [DOI] [PubMed] [Google Scholar]
- 16.Gossman GL, Joesch JM, Tanfer K. Trends in maternal request cesarean delivery from 1991–2004. Obstet Gynecol. 2006;108:1506–1516. doi: 10.1097/01.AOG.0000242564.79349.b7. [DOI] [PubMed] [Google Scholar]