Abstract
Introduction and Purpose
Abdominal obesity, the central distribution of adipose tissue, is a well established cardiometabolic disease risk factor. The prevalence has steadily increased since 1988, and now more than 50% of adults have abdominal obesity. Psychological distress coupled with increased dietary energy density (ED) may contribute to abdominal obesity. Guided by the stress and coping model, this study examined the relationship between psychological factors (perceived stress and depressive symptoms) and dietary ED in overweight, working adults. The first hypothesis tested if psychological factors explained a significant amount of food and beverage ED variance above that accounted for by demographic factors. The second hypothesis tested if psychological factors explained a significant amount of food and non-alcoholic beverage ED variance above that accounted for by demographic factors. Post hoc analyses compared macronutrient composition and food group pattern between overweight, working adults with and without depressive symptoms.
Methods
This descriptive, cross sectional, correlation study was comprised of 87 overweight, working adults; mean age, 41.3 (SD 10.2) years; mean body mass index (BMI), 32.1 (SD 6.1) kg/m2; 73.6% women; 50.6% African-American. Participants completed the Beck Depression Inventory-II (BDI-II) and Perceived Stress Scale (PSS); weighed three day food record analyzed for caloric intake (kilocalories) and weight (grams) of consumed foods and beverages which were used to calculate ED (kilocalories/gram). Height and weight were measured to calculate BMI. Descriptive statistics, Mann-Whitney U and sequential regression modeling were used for data analysis.
Results
Depressive symptoms were reported by 21.9% of participants, and explained variance in food and beverage ED above that accounted for by African-American race and reporting adequate caloric intake. Depressive symptoms explained variance in food and non-alcoholic beverage ED above that accounted for male gender, African-American race and reporting adequate caloric intake. Perceived stress and depressive symptoms were positively correlated; however, perceived stress was not a significant predictor of food and beverage ED.
Conclusion
Depressive symptoms, potentially modifiable, were four times that found in the general population, and independently predicted increased food and beverage ED. Further research is needed to determine if improvements in depressive symptoms alter dietary ED, potentially reducing cardiometabolic disease risk.
Keywords: Psychological distress, depressive symptoms, dietary energy density, overweight
INTRODUCTION AND PURPOSE
Abdominal obesity, the central distribution of adipose tissue, is a well established risk factor for cardiometabolic disease. Between 1988–2004 the overall age adjusted prevalence has steadily increased from 29.5 to 42.4% in men and 47.0 to 61.3% in women, and now more than 50% of U.S. adults have abdominal obesity.1 Economists estimate a cost in excess of $17 billion per year to American businesses due to lost productivity attributed to obesity and related cardiometabolic risk factors.2 Lack of physical activity and poor dietary quality have been correlated with abdominal obesity, and more recently scientists have investigated the role of chronic psychological distress as an associated factor.3 Scientists hypothesize that psychological distress may alter eating behaviors resulting in the intake of high energy dense diets which may predispose overweight adults to cardiometabolic disease risk. Increased dietary energy density (ED), or diets that are high in calories per gram of food and beverages consumed, represents increased risk due to excess intake of calories, total and saturated fats, and limited intake of micronutrient rich foods.4, 5 Furthermore, the role of beverages in energy regulation and body fat distribution is not well understood; however, caloric soft drinks, fruit juice and punch are correlated with weight gain and linked to other behaviors such as smoking and physical inactivity which increase cardiometabolic disease risk.6
The purpose of this study was to examine the relationship between psychological factors (perceived stress and depressive symptoms) and dietary ED in overweight (Body Mass Index [BMI] ≥ 25 kg/m2), working adults. The first hypothesis tested if psychological factors explained a significant amount of variance in food and beverage energy density above that accounted for by demographic factors. The second hypothesis tested if psychological factors explained a significant amount of variance in food and non-alcoholic beverage energy density above that accounted for by demographic factors. A post hoc analysis compared the macronutrient intake and food group pattern of overweight, working adults with and without depressive symptoms.
BACKGROUND
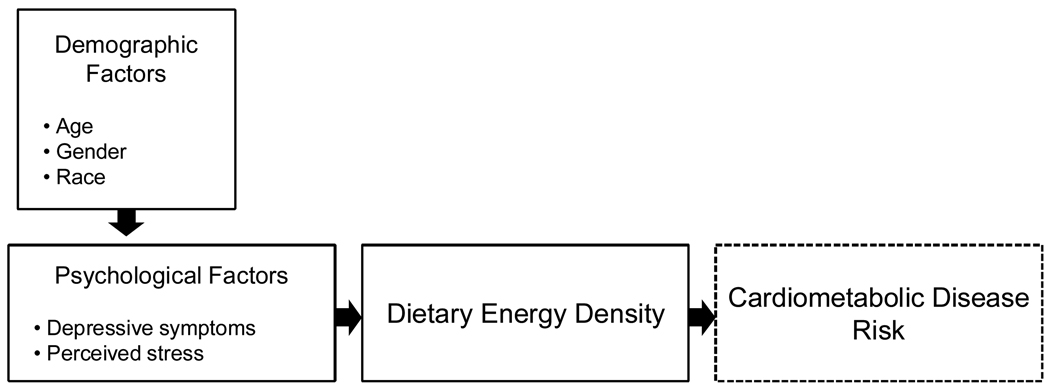
The conceptual model that guided the study is an adaptation of the stress and coping model proposed by Cohen, Kessler and Gordon (1995)7 which asserts that demographic factors and environmental demands may predispose an individual to psychological distress. Depending on the individual’s coping behaviors and available resources, these factors may contribute to psychological distress. Psychological distress, defined as the co-occurrence of perceived stress and depressive symptoms, may be linked to increased cardiometabolic disease risk through the intake of high energy dense diets. Figure 1.
Figure 1.
Proposed associations among demographic factors, psychological factors, dietary energy density and cardiometabolic disease risk. (Source: Author)
Environmental Demands
Over the past twenty years, as the prevalence of overweight has increased so has the pace of daily life. Changes in the family structure including larger numbers of working women and single parent families have implications in terms of financial resources and time constraints.8 Due to time constraints, there are fewer opportunities for physical activity and less time to shop and prepare traditional meals increasing the demand for prepackaged and fast foods. Additionally, portion sizes have increased dramatically contributing to excess caloric intake.9 Furthermore, carbonated soft drink and fruit drink intake has also increased significantly: in comparison to 1977, Americans now consume 83 calories more of added sugar each day, and 54% of this is from carbonated soft drinks and 13% from sugared fruit drinks.10 Cost and access are of concern particularly among low income individuals.11 Low energy dense diets, those high in fruits and vegetables, are more costly than high energy dense diets.12 Furthermore, there is limited access to large supermarkets with well-stocked produce departments in low income neighborhoods.11
Psychological Factors
Adults are more likely to feel stressed when they perceive environmental demands as taxing and see themselves as lacking the resources to cope with these demands.7 Stress can precipitate or exacerbate depressive symptoms and reinforce unhealthy dietary patterns leading to greater psychological distress and potentially chronic illness.13, 14 The relationship between psychological distress may be bidirectional; obesity may contribute to depression due to negative body image and social stigma.15 Overweight individuals report stress and depressive symptoms as psychological factors affecting eating behaviors and food choices.16
Negative emotions such as anger, fear and sadness are associated with irregular eating patterns and eating as a distraction, to relax or feel better.17 Stress is associated with cravings for high fat and high carbohydrate foods particularly among women. Stress related eating is more common in women than men.18, 19 Depressive symptoms are associated with increased appetite, excess food intake, preferences for high fat and carbohydrate foods, excess alcohol intake and higher BMI in women.18, 20 Additionally, severely depressed individuals may be less able to adhere to dietary recommendations.21 Although stress and depressive symptoms may contribute to weight gain in some in individuals, psychological distress can have the opposite effect in others.22 Previous studies has typically focused on psychological factors and food intake in younger, female populations; therefore, little is known about the relationship between psychological distress and food and beverage intake among a diverse population of overweight, working adults.
Dietary Energy Density
Dietary energy density (ED), the ratio of kilocalories per gram of food and beverages consumed, is an important determinant of total daily caloric intake. The ED value of the diet is determined in large part by the amount of water in foods and to a lesser extent, the amount of fat in foods. Foods with high water content, such as vegetables, have a low energy density. Because dietary fats have the highest calorie per gram ratio, high fat foods are energy dense.23 Energy density is also an indicator of nutrient quality. Low energy dense diets, those composed primarily of fruits and vegetables, yield fewer calories, less dietary fat and higher intakes of vitamins A, C, B6, folate, iron, calcium and potassium than high energy dense diets. Additionally, individuals consuming low energy dense diets have been noted to consume fewer caloric beverages.5 On a day to day basis, individuals consume approximately the same volume of food, thus the calories concentrated in that volume are important in determining energy intake and maintaining energy balance. High energy dense foods are palatable and tend to be overconsumed.24 Dietary ED has been associated with lower nutrient quality,4, 5 excess energy intake,25 higher BMI among women and elevated waist circumference in women and men.26
METHODS
This was a prospective, cross-sectional, correlation study approved by the Emory University Institutional Review Board. After IRB approval was obtained, multiple active and passive strategies were used to recruit potential participants. Participants were recruited from community organizations such as neighborhood churches and businesses in the greater metropolitan area of a large southeastern city. Flyers were posted in community settings and participants were recruited from community wellness fairs held within a 20 mile radius of the university. Potential participants were asked to contact the principal investigator by phone. Once contacted, a screening procedure was followed to ensure that participants met the inclusion and exclusion criteria. Potential participants were met according to their preference at their home, work place or a research office at the School of Nursing.
Procedure
During the initial visit, participants were provided with an explanation of the study activities and an opportunity to ask questions, and their understanding of the study activities was elicited by asking for a return explanation. Participants then signed the informed consent and HIPAA documents. The research nurse instructed participants on how to complete the study questionnaires which they completed at home. Using scripted instruction, the research nurse taught participants how to weigh and estimate everything they ate and drank on a loaned Soehnle 67000 digital food scale for three consecutive days including one weekend day. Participants were taught how to record their food intake on a standardized food record. To ensure that participants understood the instruction, they gave a return demonstration to the research nurse. In addition to verbal instructions, participants were given a booklet that included written instructions with illustrations. At the conclusion of the first study visit, anthropometric measurements were obtained using a standardized procedure by the research nurse.
Participants completed study activities at home during the three day study period. On the first study day, the research nurse contacted participants to answer any questions and problem solve any difficulties they encountered. At the conclusion of the three study days, the second study visit was completed. During the second visit, the study questionnaires and food record were collected. A standardized procedure was used to review all data with the participant. Questionnaires were reviewed to ensure completeness and missing items were clarified. Food records were reviewed to ensure completeness including food preparation techniques and accuracy in estimating items such as composite foods or any items that were not weighed. At the conclusion of the second visit, participants received a $25.00 gift card.
Sample
Power Analysis and Sample Size (PASS) software was used to determine sample size a priori based on a multiple regression analysis using a projected R2 of 0.12 accounted for by four predictor variables and an R2 of 0.10 accounted for by four control variables. A sample size of 83 was needed to achieve a power of .80 with an alpha of .05.
Ninety one participants were recruited to allow for 10% attrition in completing the study activities. The inclusion criteria were a BMI ≥ 25.0 kg/m2 and being employed at least 20 hours per week. The focus of this study was to examine the influence of psychological factors on dietary energy density in the context of overweight, and the exclusion criteria were established to minimize the confounding effect on the relationship between psychological factors and dietary energy density. Participants were excluded if they engaged in physical activity for 30 minutes or more, three or more days per week; were pregnant or currently breastfeeding; were currently being treated with steroids, valproic acid, phenothiazines, highly active anti-retroviral therapy (HAART) or antidepressants; or had a history of diabetes, bariatric or other abdominal surgery. Physically active individuals were excluded to control for the effects physical activity may have on mood and food intake. For example, it has been shown that women engaging in moderate physical activity have fewer depressive symptoms than inactive women.27 Furthermore, differences in PA intensity may affect food choices, and this may vary by gender.28, 29 Since pregnant and breastfeeding women have unique dietary fat requirements, and they are in a potential stage of weight gain or loss, they were excluded. Individuals with type 1 or 2 diabetes and those who have undergone bariatric or other abdominal surgeries have unique nutritional needs, and they were excluded. Individuals who were currently being treated with steroids, valproic acid, phenothiazines, HAART or antidepressants were excluded due to the confounding effect of these medications on appetite and food intake.30
Variables and measures
Demographic factors were reported as 1) sex; 2) age; and 3) race categorized as Caucasian or African American. Height and weight were measured using NHANES procedures: body mass index was calculated as weight (kilograms) divided by the square of height (meters).31
Psychological factors measured were depressive symptoms and perceived stress. Depressive symptoms over the prior 2 weeks were measured using the Beck Depression Inventory-II (BDI-II).32 The BDI-II provides a continuous score of depressive symptoms ranging from 0–63, and a score of 14 or higher indicates at least mild symptoms of depression.32 BDI-II questionnaires were reviewed for completeness and scored immediately after the second visit. If the BDI-II score indicated the presence of moderate to severe depressive symptoms, standardized procedures, approved by the IRB, were followed to ensure that participants were referred for mental health services. The Cronbach’s alpha was .91 for the BDI-II demonstrating internal consistency reliability of this instrument in measuring depressive symptoms in this sample.
Perceived stress, or the degree to which an individual feels his/her life has been unpredictable or overwhelming over the past month, was measured using the Perceived Stress Scale (PSS).7 The PSS provides a continuous score of perceived stress ranging from 0 to 40 with higher scores indicating greater perceived stress.7 The Cronbach’s alpha was .89 for the PSS demonstrating internal consistency reliability of this instrument in measuring perceived stress in this sample.
Weighed three day food records were used to assess dietary energy density. The food records were analyzed for total kilocalories and weight in grams of all food and beverages reported. These data were used to calculate energy density values. Food records were analyzed post hoc for macronutrient intake (total and saturated fats, total carbohydrates, total sugars, fiber, and protein) and food group pattern (grain, vegetables, fruit, milk, and meat and beans). All food records were analyzed by the study dietitian using the Food Processor SQL Nutrition Analysis software from ESHA Research, Salem, Oregon.
In order to test the first hypothesis that psychological factors explained a significant amount of variance in food and beverage ED above that accounted for by demographic factors, a mean food and beverage ED value was calculated. Food and beverage ED was calculated by dividing each participant’s reported daily caloric intake (kilocalories) for all foods and beverages consumed by the weight (grams) of all foods and beverages consumed. Food and beverage ED values were calculated for each study day and then averaged to obtain a mean ED value for foods and beverages.
In order to test the second hypothesis that psychological factors explained a significant amount of variance in food and non-alcoholic beverage ED above that accounted for by demographic factors, a mean food and non-alcoholic beverage ED value was calculated. Food and non-alcoholic ED was calculated by dividing each participant’s reported daily caloric intake (kilocalories) for all foods and non-alcoholic beverages consumed by the weight (grams) of all foods and non-alcoholic beverages consumed.50 Food and non-alcoholic beverage ED values were calculated for each study day and then averaged to obtain a mean ED value for foods and non-alcoholic beverages.
In order to account for possible underreporting of food and beverage intake, a continuous variable, reporting adequate caloric intake (RACI), was calculated for each participant and used as a control variable in sequential linear regression modeling. This value was calculated as the ratio of the kilocalories required to maintain one’s current body weight to the mean reported caloric intake (kilocalories). The kilocalories required to maintain one’s current body weight was estimated for each participant using the Harris-Benedict equation which takes age, gender, height, weight and physical activity into account.33 The reported caloric intake was calculated for each study day and then averaged to determine the mean reported caloric intake for the three study days. A RACI value greater than one indicated that the participant underreported his/her caloric intake, and a RACI value equal to or less than one indicated that the participant reported a caloric intake greater than the energy needed to maintain one’s current weight.
Finally, a post hoc analysis was conducted to better understand which dietary factors contributed to differences in dietary ED between those with and without depressive symptoms. For this analysis, the macronutrient composition and food group pattern were examined.
Data Analysis Procedures
All analyses were conducted using SPSS-PC software. Descriptive statistics, t-tests and sequential linear regression were used to explain and predict food and beverage ED and to predict food and non-alcoholic beverage ED. Descriptive analysis included frequency distributions, means, standard deviations, and ranges according to the level of measurement. The t-test was used to assess racial differences in dietary ED, and Mann-Whitney U was used to assess gender differences in dietary ED. Bivariate analyses were used to assess the unadjusted relationships among the variables. To reduce skewness, BDI-II scores were transformed by a square root transformation which resulted in a satisfactory distribution. Sequential linear regression modeling was used to assess the independent association between psychological factors and dietary energy density. Using this approach significant, parsimonious models were developed and are presented here. In each model, variables that trended toward significant (P ≤ .07) or were significant (P ≤ .05) were retained in each step. Post hoc power analyses were conducted and are presented here. Post hoc collinearity diagnostics revealed no multicollinearity between variables in the parsimonious models.
To test the first hypothesis that psychological factors explained a significant amount of variance in food and beverage energy density above that accounted for by demographic factors, sequential linear regression modeling was used to determine the independent association between psychological factors and food and beverage energy density while controlling for age, gender, race, and RACI. In step one, age, gender, race and RACI were entered as a block and regressed against the mean food and beverage ED value. This demonstrated the amount of variance in food and beverage ED explained by these factors. In step two, PSS and BDI-II scores were entered into the model to determine the amount of variance in food and beverage ED explained by psychological factors above that accounted for by age, gender, race and RACI.
To test the second hypothesis that psychological factors explained a significant amount of variance in food and non-alcoholic beverage ED above that accounted for by demographic factors, sequential linear regression was used to determine the independent association between psychological factors and food and non-alcoholic beverage ED while controlling for age, gender, race and RACI. In step one, age, gender, race and RACI were entered as a block and regressed against the mean food and non-alcoholic ED value. This demonstrated the amount of variance in food and non-alcoholic beverage ED explained by these factors. In step two, PSS and BDI-II scores were entered into the model to determine the amount of variance in food and non-alcoholic beverage ED explained by depressive symptoms above that accounted for by age, gender, race and RACI.
RESULTS
Ninety one overweight, working adults consented to participate in the study. Most were self referral (80.2%) and a small number (19.8%) were recruited from community health fairs. Four participants were excluded from data analysis: two participants were unable to complete the study activities, and two participants were considered extreme outliers due to severe underreporting of caloric intake. In total, 87 participants comprised the final study sample.
The sample was comprised primarily of women (73.6%) and African Americans (50.6%) with a mean age of 41.3 (SD 10.2) years and mean BMI of 32.1 (SD 6.1) kg/m2. A small number of participants reported a history of hypertension (20.7%) and high cholesterol (14.9%). No participants reported a history of stroke, heart failure, or cancer. A few participants reported that they had conditions that limited their ability to participate in physical activity (5.7%). The majority (64.6%) reported that they were not currently taking any medications. PSS scores were relatively low with a mean of 16.47 (SD 7.19). The majority reported no or minimal depressive symptoms; however 21.9% reported mild to severe depressive symptoms. Bivariate analysis showed that PSS and BDI-II were moderately correlated (r = .60, P ≤. 01). Table 1 shows characteristics of the participants.
Table 1.
Sample Characteristics (N=87)
| Variable | Mean (SD, range) or N (%) |
|---|---|
| Age | 41.3 (10.2, 20–64) years |
| Gender | 64 (73.6) women |
| Race | 44 (50.6) African-Americans |
| BMI | |
| All | 32.1 (6.1, 24.6–52.0)kg/m2 |
| Women | 32.5 (6.5, 25.1–52.0)kg/m2 |
| Men | 31.0 (4.5, 24.6–43.1)kg/m2 |
| Perceived Stress Scale (PSS) | 16.47 (7.19, 0–33) |
| Beck Depression Inventory-II (BDI-II) | 8.7 (8.34, 0–42) |
Note. BMI = Body Mass Index. PSS = Perceived Stress Scale. BDI-II = Beck Depression Inventory-II.
More than half (n=51; 58.6%) of the participants underreported their caloric intake; the mean RACI value was 1.06 (SD 0.25). Those reporting adequate caloric intake did not differ significantly from those reporting inadequate caloric intake on age, race, BMI, PSS or BDI-II scores.
The mean food and beverage ED value was 0.75 (SD 0.22) kilocalories/gram. African-Americans reported a higher food and beverage energy density than did Caucasians (t = −2.198, P = .03). Table 2. There were no significant gender differences on food and beverage energy density (U = 602.0, P = .31). Younger age was correlated with higher food and beverage ED values (r = −.27, P ≤ .05), and reporting adequate caloric intake was correlated with higher food and beverage ED values (r = −.42, P ≤ .01).
Table 2.
Dietary Energy Density Values by Race
| Dietary Energy Density Values | Mean (SD) | Range |
|---|---|---|
| Food and beverages | ||
| All (N=86) | .75 (.22) | .32–1.31 |
| Caucasians (n=43) | .70 (.19) | .32–1.08 |
| African-Americans (n=43) | .81 (.24) | .41–1.31 |
The majority (n=58, 66.7%) did not report alcohol intake. Among those reporting alcohol intake, the mean alcohol servings per day was 1.04 (SD 0.53) for men (n=7) and 0.92 (SD 0.72) for women. The majority (75.9%) did not exceed the recommendation of two drinks per day for men and one drink per day for women.34 Among individuals reporting alcohol intake, the mean kilocalories of alcohol consumed was 148.15 (SD 154.87).
To test the first hypothesis that psychological factors explained a significant amount of variance in food and beverage energy density while controlling for demographic factors, a sequential linear regression model was developed. A model regressing PSS and BDI-II scores against the mean food and beverage ED value while controlling for demographic factors was tested. In a significant (F = 10.284, P ≤ .01), parsimonious model, demographic factors and depressive symptoms explained 35.3% of the variance in food and beverage ED. Of this variance, depressive symptoms (β = .24, P ≤ .01) explained 5.3% of the variance above that accounted for by younger age (β = −.17, P = .06), male gender (β = −.17, P = .06), African-American race (β = .31, P ≤ .01) and RACI (β = −.52, P ≤ .01). In this model, perceived stress was not a significant predictor. A post hoc power analysis showed 75% power to detect an R2 of .05 attributed to one independent variable and an R2 of .34 attributed to four control variables.
In a previous study, depression was linked to alcoholic beverage consumption;.20 therefore it was important to understand if the variance in food and beverage energy density reported by overweight, working adults with depressive symptoms was related to alcoholic beverage consumption. To test the second hypothesis, a mean food and non-alcoholic beverage energy density value was calculated for each participant, and was evaluated in the sequential linear regression model. The model regressing BDI-II scores against the food and non-alcoholic beverage energy density value while controlling for demographic factors was tested. In a significant (F = 10.957, P ≤ .01), parsimonious model, demographic factors and depressive symptoms explained 36.9% of food and non-alcoholic beverage ED. Of this variance, depressive symptoms (β = .24, P ≤ .01) explained 5.4% of the food and non-alcoholic beverage energy density variance above that accounted for by younger age (β = −.17, P = .07), male gender (β = −.21, P ≤ .05), African-American race (β = .31, P ≤ .01) and RACI (β = −.53, P ≤ .01). In this model, perceived stress was not a significant predictor. A post hoc power analysis showed 76% power to detect an R2 of .05 attributed to one independent variable and an R2 of .35 attributed to four control variables.
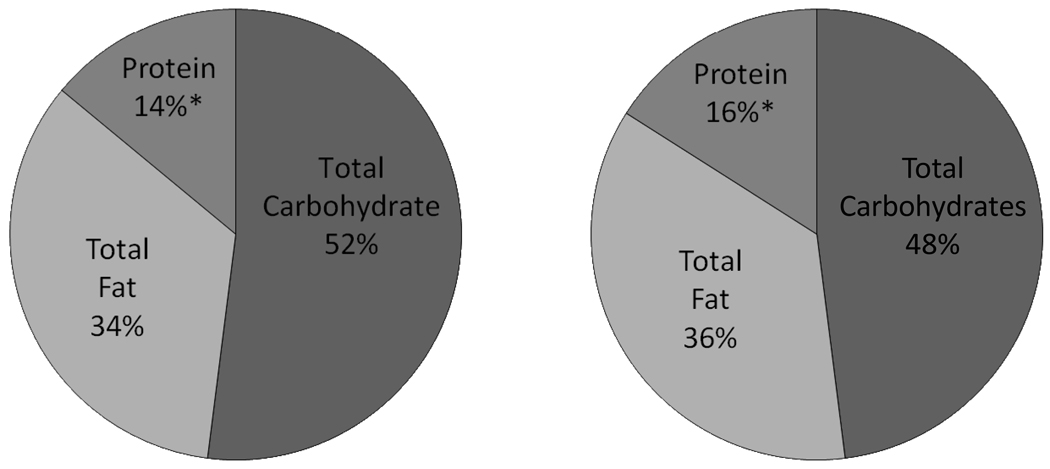
Post hoc analyses compared the macronutrient intake and food group patterns of overweight, working adults with depressive symptoms to those without depressive symptoms. Table 3. Overweight, working adults with depressive symptoms trended toward a significantly lower intake of fiber (U = 469.0, P = .07) and consumed a significantly lower intake of protein (U = 438.0, P = .03) and vegetables (U = 448.5, P = .04). The macronutrient distribution reported by overweight, working adults with depressive symptoms as compared to those without depressive symptoms is depicted in Figure 2.
Table 3.
Dietary Differences between Overweight, Working Adults with and without Depressive Symptoms
| Dietary Factor | No Depressive Symptoms N= 68 Mean (SD) |
With Depressive Symptoms N=19 Mean (SD) |
Mann- Whitney U |
Z Score |
P Value |
|---|---|---|---|---|---|
| Macronutrient Composition | |||||
| Energy (kcal) | 2066.1 (611.9) | 1899.8 (490.9) | 570.0 | −.781 | .44 |
| Total Fat (g) | 81.0 (35.5) | 72.0 (18.9) | 578.0 | −.699 | .49 |
| Saturated Fat (g) | 25.4 (12.0) | 22.8 (7.7) | 589.5 | −.580 | .56 |
| Total carbohydrates (g) | 248.0 (80.0) | 245.4 (105.9) | 625.0 | −.216 | .83 |
| Cholesterol (mg) | 275.9 (151.9) | 217.7 (95.9) | 523.0 | −1.264 | .21 |
| Fiber (g) | 19.7 (9.0) | 15.7 (6.6) | 469.0 | −1.818 | .07 |
| Total sugars (g) | 93.4 (44.5) | 104.5 (59.1) | 587.5 | −.60 | .55 |
| Protein (g) | 81.9 (26.0) | 69.1 (13.8) | 438.0 | −2.137 | .03 |
| Food Group Pattern | |||||
| Grain (oz eq) | 6.8 (3.0) | 6.1 (3.3) | 559.0 | −.894 | .37 |
| Vegetables (cup eq) | 1.9 (1.2) | 1.3 (0.8) | 448.5 | −2.029 | .04 |
| Fruit (cup eq) | 1.0 (1.0) | 0.7 (0.9) | 503.0 | −1.474 | .14 |
| Milk (cup eq) | 1.2 (1.0) | 0.9 (0.7) | 530.0 | −1.192 | .23 |
| Meat & beans (oz eq) | 5.8 (3.9) | 4.9 (1.9) | 550.0 | −.986 | .32 |
Note. Eq=equivalent. G=grams. Kcal=kilocalories. Mg=milligrams. Oz=ounce.
Figure 2.
Macronutrient distribution reported by overweight, working adults with depressive symptoms compared to those without depressive symptoms. * P ≤ .05. (Source: Author)
DISCUSSION
The findings that overweight, working adults who were African-American consumed more energy dense food and beverages, and that men and African-American consumed more energy dense food and non-alcoholic beverages are consistent with those from a large, nationally representative sample.35 Lediwke and others (2005)35 showed that men and non-Hispanic blacks reported consuming higher energy dense foods than women and non-Hispanic whites.35
In this study, perceived stress did not predict food and beverage ED. This is not consistent with other studies of animals and humans which have demonstrated an association between chronic stress and the intake of high fat chow in rats,36 chronic stress and higher caloric intake in subordinate compared to dominant macaques,37 and novel stress with a preference for sweet foods in women.19 This null finding may be due, in part, to participants reporting relatively low levels of stress. The mean PSS score indicated that participants had levels of stress similar to other working adults.38, 39 Furthermore, the majority of participants were well-educated professionals suggesting that they had access to resources, such as health information, that could mitigate the negative effects of stress.7 Although perceived stress did not independently predict food and beverage energy density, participants who reported greater perceived stress also reported increased depressive symptoms. It may be that greater perceived stress exacerbates depressive symptoms, thus contributing indirectly to increased dietary energy density.
Although the majority of participants reported no or minimal depressive symptoms, over 20% of participants reported mild to severe depressive symptoms based on BDI-II scores. The prevalence of depressive symptoms in this sample was four times that found in the general population,40 and is similar to the 20–25% depression prevalence reported in patients undergoing coronary bypass surgery41 and the 20% depression prevalence associated with chronic disease.40 These findings underscore that depressive symptoms are relatively common in overweight, working adults yet are often undetected and untreated.
Increased depressive symptoms independently predicted food and beverage energy density, and explained variance above that explained by younger age, male gender, African-American race and reporting adequate caloric intake. For each gram of food and beverages consumed, individuals with depressive symptoms consumed more kilocalories than individuals without depressive symptoms. This relationship persisted when alcoholic beverages were removed from the equation. Increased depressive symptoms independently predicted food and non-alcoholic beverage energy density, and explained variance above that accounted for by younger age, male gender, African-American race and reporting adequate caloric intake. These findings suggest that those with depressive symptoms consumed a diet with lower nutritional quality than those without depressive symptoms. The post hoc analysis demonstrated 75% power which represents a reasonable degree of protection against a Type II error. In other words, we can be relatively certain important differences that truly exist were detected. 42 Because depressive symptoms are potentially modifiable, early identification of and intervention for depressive symptoms may be an important step toward reducing dietary energy density and cardiometabolic disease risk. Of note, these findings can only be generalized to overweight, working adults with depressive symptoms who are not being treated with antidepressant medications.
In terms of nutrient quality, saturated fat intake was higher than recommended, and fruit, vegetable, and low fat dairy product intake was lower than recommended among all participants.34 In addition, dietary factors differed between those with depressive symptoms compared to those without depressive symptoms. Overweight, working adults with depressive symptoms trended toward significantly lower dietary fiber intake and reported significantly lower protein and vegetable intake than those without depressive symptoms. These differences in nutritional quality may predispose those with depressive symptoms to cardiometabolic disease risk.
Limitations
Limitations of the study include the use of convenience sampling. The study activities required highly motivated participants, and people who chose to enroll may be different from non-participants. The study was biased toward well-educated professionals. In addition, the participants received a modest incentive which may bias study results. Despite the use of a protocol to standardize the level of detail and description of food and beverage intake, the majority reported inadequate caloric intake which has the potential to weaken associations and mask significant findings. Reporting inadequate caloric intake can be attributed to multiple factors including under-recording, underestimating and undereating.43 In addition, weighing and recording all food and beverage intake for three days may have created a recording burden which resulted in underreporting caloric intake.43
Recommendations for Research
This study demonstrated racial differences in dietary energy density with African-American participants reporting a higher energy dense diet than Caucasians. This finding is of great concern because high energy dense diets have been linked to abdominal obesity,26 and the prevalence of abdominal obesity is rising among African American adults.1 Further research is needed to better understand the dietary factors that contribute to these differences as well as other social and environmental factors that may play a role so that culturally appropriate interventions tailored to overweight, working African-American adults can be developed and tested.
A challenge in dietary assessment is the issue of underreporting caloric intake, and novel approaches that minimize underreporting need to be developed and validated. Novel approaches, such as the use of disposable cameras to photograph meals and snacks and hand held electronic devices to record intake, could potentially minimize the error introduced due to underestimating portion sizes and underreporting. Other methods for instance, short instruments that measure dietary ED need to be developed and tested. Statistical methods, such as the RACI variable, that control for the error introduced due to underreporting need to be validated in other populations. Nursing interventions aimed at reducing dietary energy density need to be developed and tested.
Research is needed to better understand how to identify individuals prone to depressive symptoms, and to determine if nursing interventions aimed at reducing depressive symptoms alters dietary energy density. Prospective studies are needed to determine if dietary ED may mediate the relationship between psychological factors and cardiometabolic disease risk. This study examined the relationship between chronic stress and dietary energy density. It may be that a measure of chronic stress does not adequately capture the kind of stress that affects eating behaviors and the intake of high energy dense diets. In future studies it may be important to measure more specific types of stress such as work-related stress, and to understand how intensity and duration of stress may affect eating behaviors and the intake of high energy dense diets.
Recommendations for Clinical Practice
Nurses can play an important role in creating an environment that is sensitive to the needs of overweight adults. Nurses should collaborate with dietitians and other professionals to provide basic instruction and resources to overweight individuals with a focus on decreasing dietary energy density and improving nutrient quality. Basic instruction should include replacing non-nutritious caloric beverages with nutritious beverages and water, consuming low fat milk and dairy products, decreasing saturated fats, consuming lean protein, replacing simple with complex carbohydrates and increasing fruit and vegetable intake.34 These strategies will decrease dietary energy density, improve nutritional quality and potentially decrease cardiometabolic disease risk.44 Nurses can play important roles in assessing readiness and motivation to change dietary patterns as well as tailoring dietary messages to the social and cultural context of overweight adults. Additionally, nurses can assist overweight adults identify emotional states that may trigger unhealthy dietary patterns as well as explore and incorporate healthier dietary patterns into their everyday lives. Advanced practice nurses can perform an initial assessment and use patient-centered counseling to engage patients in setting their own weight loss goals. Lifestyle modifications are the mainstay of weight loss, and a focused assessment of dietary energy density and counseling on reducing dietary energy density may be of benefit. Some overweight adults may benefit from additional treatment options, and nurses should refer to evidence-based practice guidelines related to assessment of and intervention for overweight.45
Nurses need to be aware of the role that depressive symptoms can play in cardiometabolic disease risk. As shown in this study, mild to moderate depressive illnesses are common, and these are often undetected and untreated. In many clinical settings, mood and affect are not assessed or treated until they interfere with activities of daily living; however, early identification of and intervention for those at risk may improve cardiometabolic outcomes.47 Nurses, in primary care, workplaces and other community settings, can play important roles in early identification of individuals experiencing depressive symptoms, referral to qualified mental health professionals, and coordination of the medical and mental health care of these individuals. The Patient Health Questionnaire 2, a two-item questionnaire, is a short tool that can be easily administered by nurses during brief office encounters to screen adults for depression.48 If an individual answers yes to one or both questions, further assessment and follow up is recommended.48
Finally, these findings have implications for worksite interventions. Importantly, working adults with multiple cardiometabolic risk factors missed 179% more work days and spent 147% more days in bed compared to working adults without cardiometabolic risk factors resulting in a cost of more than $17.3 billion in lost productivity to American businesses.2 Worksites offer a venue for nurses to provide educational and behavioral interventions in an environment where working adults typically consume at least one meal per day.49 Education for employees provided by qualified professionals about scientifically sound strategies such as reducing energy density as a healthy, long term weight management strategy could be delivered at the worksite using a variety of formats such as company intranet, at point of purchase for foods in cafeterias and vending machines, at wellness fairs and health screenings, or in face to face instruction.49 In addition, overweight individuals report that although they may receive instruction, they lack the long term guidance and support needed to successfully change their dietary behavior.50 Long term interventions aimed at supporting overweight employees in their attempts to initiate and sustain dietary behavior change could be delivered at worksites by occupational health nurses. Finally, overweight individuals report that interventions that involve their social support networks help them feel accepted and supported in behavior change.50 The social support offered in the worksite may motivate overweight individuals to initiate as well as sustain their efforts to alter their eating behaviors and modify dietary energy density.
In addition to interventions aimed at employees, nurses can work with dietitians to assess the nutritional environment of the worksite to develop strategies aimed at improving the nutritional quality of food and beverages offered.50, 51 Nurses can work with management and human resource personnel to develop policies aimed at creating a work environment that makes low energy dense food choices easy and convenient.50, 51
CONCLUSION
In conclusion, we demonstrated that moderate to severe depressive symptoms were relatively common among overweight, working adults. Increased depressive symptoms predicted food and beverage energy density above that explained by demographic factors. Overweight, working adults with depressive symptoms consumed more kilocalories per gram of food and beverages consumed than those without depressive symptoms. Further research is needed to determine if improvements in depressive symptoms alter dietary energy density, and if lower dietary energy density reduces cardiometabolic disease risk.
SUMMARY.
Depressive symptoms are independent predictors of food and beverage energy density accounting for variance beyond that explained by African-American race and reported adequate caloric intake.
Depressive symptoms are independent predictors of food and non-alcoholic beverage energy density accounting for variance beyond that explained by male gender, African-American race and reported adequate caloric intake.
For each gram of food and beverages consumed, overweight, working adults with depressive symptoms not treated with antidepressants consumed more kilocalories than overweight, working adults without depressive symptoms while controlling for age, gender, race and reporting adequate caloric intake.
Depressive symptoms may be modifiable, and whether a reduction in depressive symptoms alters dietary energy density thus potentially decreasing cardiometabolic disease risk merits further evaluation.
IMPLICATIONS.
Collaborate with dietitians to provide basic patient instruction to overweight, working adults about dietary fats, milk and low fat dairy products, whole grains, lean protein, fruit and vegetable intake.
Assist overweight working adults identify emotional states that may trigger unhealthy dietary patterns and incorporate healthier behaviors.
Screen for depressive symptoms in primary care and community settings.
Develop and test nursing approaches for early recognition and reduction of depressive symptoms.
Develop and test short instruments to assess ED and diet pattern.
-
Develop and test nursing interventions aimed at reducing energy density
-
○
Replace high energy dense foods with high volume foods such as fruits, vegetables, and low fat milk/dairy products.
-
○
Acknowledgments
This work was supported by funding from The National Institutes of Health, National Institute for Nursing Research, National Research Service Award; Nurses Educational Funds, Inc.; American Nurses Foundation; Southern Nurses Research Society; Sigma Theta Tau International, Alpha Epsilon Chapter; National Institutes of Health, National Center for Research Resources, PHS Grant UL1RR025008 Clinical and Translational Science Award program and PHS Grant MO1 RR0039 General Clinical Research Center program.
REFERENCES
- 1.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among U.S. adults. Obesity. 2007;15(1):216–224. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 2.Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Productivity costs associated with cardiometabolic risk factor clusters in the United States. Value Health. 2007;10(6):443–450. doi: 10.1111/j.1524-4733.2007.00199.x. [DOI] [PubMed] [Google Scholar]
- 3.Dallman MF, La Fleur SE, Percoraro NC, Gomez F, Houshyar H, Akana SF. Minireview: Glucocorticoids-food intake, abdominal obesity, and wealthy nations in 2004. Endocrinology. 2004;145(6):2633–2638. doi: 10.1210/en.2004-0037. [DOI] [PubMed] [Google Scholar]
- 4.Cuco G, Arija V, Marti-Henneberg C, Fernandez-Ballart J. Food and nutritional profile of high energy density consumers in an adult Mediterranean population. Eur J Clin Nutr. 2001;55(3):192–199. doi: 10.1038/sj.ejcn.1601144. [DOI] [PubMed] [Google Scholar]
- 5.Ledikwe JH, Blanck HM, Kettel Khan L, et al. Low-energy-density diets are associated with high diet quality in adults in the United States. J Am Diet Assoc. 2006;106(8):1172–1180. doi: 10.1016/j.jada.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Bellisle F, Drewnowski A. Intense sweeteners, energy intake and the control of body weight. Eur J Clin Nutr. 2007 Jun;61(6):691–700. doi: 10.1038/sj.ejcn.1602649. [DOI] [PubMed] [Google Scholar]
- 7.Cohen, Kessler RC, Gordon LU. Measuring Stress: A Guide for Health and Social Scientists. New York: Oxford University Press; 1995. [Google Scholar]
- 8.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: Where do we go from here? Science. 2003;299(5608):853–855. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 9.Nielsen SJ, Popkin BM. Patterns and trends in food portion sizes, 1977–1998. JAMA. 2003;289(4):450–453. doi: 10.1001/jama.289.4.450. [DOI] [PubMed] [Google Scholar]
- 10.Popkin BM, Nielsen SJ. The sweetening of the world's diet. Obes Res. 2003;11(11):1325–1332. doi: 10.1038/oby.2003.179. [DOI] [PubMed] [Google Scholar]
- 11.Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. Why Americans eat what they do: Taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98(10):1118–1126. doi: 10.1016/S0002-8223(98)00260-0. [DOI] [PubMed] [Google Scholar]
- 12.Andrieu E, Darmon N, Drewnowski A. Low-cost diets: More energy, fewer nutrients. Eur J Clin Nutr. 2006 Mar;60:434–436. doi: 10.1038/sj.ejcn.1602331. [DOI] [PubMed] [Google Scholar]
- 13.Bale TL. Stress sensitivity and the development of affective disorders. Horm Beh. 2006;50(4):529–533. doi: 10.1016/j.yhbeh.2006.06.033. [DOI] [PubMed] [Google Scholar]
- 14.McEwen BS. Glucocorticoids, depression, and mood disorders: Structural remodeling in the brain. Metabolism. 2005;54(5 Suppl. 1):20–23. doi: 10.1016/j.metabol.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 15.de Wit LM, van Straten A, van Herten M, Penninx BW, Cujpers P. Depression and body mass index, a u-shaped association. BMC Public Health. 2009;9:14. doi: 10.1186/1471-2458-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chambers JA, Swanson V. A health assessment tool for multiple risk factors for obesity: Results from a pilot study with UK adults. Patient Educ Couns. 2006;62(1):79–88. doi: 10.1016/j.pec.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 17.Macht M, Simons G. Emotions and eating in everyday life. Appetite. 2000;35(1):65–71. doi: 10.1006/appe.2000.0325. [DOI] [PubMed] [Google Scholar]
- 18.Benton D. Carbohydrate ingestion, blood glucose and mood. Neurosci Biobehav Rev. 2002;26(3):293–308. doi: 10.1016/s0149-7634(02)00004-0. [DOI] [PubMed] [Google Scholar]
- 19.Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: A laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26(1):37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- 20.Strine TW, Mokdad AH, Dube SR, et al. The association of depression and anxiety with obesity and unhealthy behaviors among community-dwelling US adults. Gen Hosp Psychiatry. 2008;30(2):127–137. doi: 10.1016/j.genhosppsych.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 21.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25(4):246–252. doi: 10.1016/s0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 22.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: A new view of "comfort food". Proceedings of the National Academy of Sciences of the United States of America. 2003;100:11696–11701. doi: 10.1073/pnas.1934666100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drewnowski A. The role of energy density. Lipids. 2003;38(2):109–115. doi: 10.1007/s11745-003-1039-3. [DOI] [PubMed] [Google Scholar]
- 24.Drewnowski A. Energy density, palatability, and satiety: Implications for weight control. Nutr Rev. 1998;56(12):347–353. doi: 10.1111/j.1753-4887.1998.tb01677.x. [DOI] [PubMed] [Google Scholar]
- 25.Poppitt SD, Prentice AM. Energy density and its role in the control of food intake: Evidence from metabolic and community studies. Appetite. 1996;26(2):153–174. doi: 10.1006/appe.1996.0013. [DOI] [PubMed] [Google Scholar]
- 26.Mendoza JA, Drewnowski A, Christakis DA. Dietary energy density is associated with obesity and the metabolic syndrome in US adults. Diabetes Care. 2007;30(4):974–979. doi: 10.2337/dc06-2188. [DOI] [PubMed] [Google Scholar]
- 27.Augestad LB, Slettemoen RP, Flanders WD. Physical activity and depressive symptoms among Norwegian adults aged 20–50. Public Health Nurs. 2008;25:536–545. doi: 10.1111/j.1525-1446.2008.00740.x. [DOI] [PubMed] [Google Scholar]
- 28.Melzer K, Kayser B, Saris WH, Pichard C. Effects of physical activity on food intake. Clin Nutr. 2005;24(6):885–895. doi: 10.1016/j.clnu.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Duvigneaud N, Wijndaele K, Matton L, et al. Dietary factors associated with obesity indicators and level of sports participation in Flemish adults: a cross-sectional study. Nutr J. 2007;21(6):26. doi: 10.1186/1475-2891-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. [Accessed December 5, 2009];Overweight and obesity: Causes and consequences. http://www.cdc.gov/obesity/causes/index.html.
- 31.National Center for Health Statistics. [Accessed December 5, 2009];National Health and Nutrition Examination Survey: Anthropometry procedures manual. http://www.cdc.gov/nchs/data/nhanes/bm.pdf.
- 32.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory (BDI-II) 2nd ed. San Antonio, TX: The Psychological Association; 1996. [Google Scholar]
- 33.Harris J, Benedict F. A Biometric Study of Basal Metabolism in Man. Washington, D.C.: Carnegie Institute of Washington; 1919. [Google Scholar]
- 34.U. S. Department of Health and Human Services, U.S. Department of Agriculture. Dietary Guidelines for Americans, 2005. Washington, D.C.: U.S. Government Printing Office; 2005. [Google Scholar]
- 35.Ledikwe JH, Blanck HM, Kettel Khan L, Serdula MK, Seymour JD, Tohill BC, Rolls BJ. Dietary energy density determined by eight calculation methods in a nationally representative United States population. J Nutr. 2005;135(2):273–278. doi: 10.1093/jn/135.2.273. [DOI] [PubMed] [Google Scholar]
- 36.La Fleur SE, Akana SF, Manalo SL, Dallman MF. Interaction between corticosterone and insulin in obesity: Regulation of lard intake and fat stores. Endocrinology. 2004;145(5):2174–2185. doi: 10.1210/en.2003-1359. [DOI] [PubMed] [Google Scholar]
- 37.Wilson ME, Fisher J, Fischer A, Lee V, Harris RB, Bartness TJ. Quantifying food intake in socially housed monkeys: Social status effects on caloric consumption. Physiol Beh. 2008;94(4):586–594. doi: 10.1016/j.physbeh.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brunner RL. The Perceived Stress Scale. In: St. Jeor ST, editor. Obesity assessment: Tools, methods, interpretations (a reference case: the RENO diet-heart study) New York: Chapman & Hall; 1997. pp. 471–478. [Google Scholar]
- 39.Rush AJ, Rush JA, First MB, Blacker D. American Psychiatric Association. Handbook of Psychiatric Measures. 2nd ed. Washington, D.C.: American Psychiatric Association; 2008. [Google Scholar]
- 40.Krogh J, Peterssen L, Timmermann M, Saltin B, Nordentoft M. Design paper: The DEMO trial: a randomized, parallel-group, observer-blinded clinical trial of aerobic veersus non-aerobic versus relaxation training for patients with light to moderate depression. Contemp Clin Trials. 2007;28(1):79–89. doi: 10.1016/j.cct.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 41.Parashar S, Vaccarion V. Depression and CHD risk: how should we intervene? Curr Treat Options Cardiovasc Med. 2007;9(4):272–277. doi: 10.1007/s11936-007-0022-5. [DOI] [PubMed] [Google Scholar]
- 42.Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice. 2nd ed. Upper Saddle River, New Jersey: Prentice-Hall, Inc.; 2000. [Google Scholar]
- 43.Gibson RS. Principles of Nutritional Assessment. 2nd ed. New York: Oxford University Press; 2005. [Google Scholar]
- 44.Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc. 2005;105(5 Suppl. 1):S98–S103. doi: 10.1016/j.jada.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 45.National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Bethesda, MD: U.S. Department of Health and Human Services: National Institutes of Health, National Heart Lung and Blood Institute; 1998. pp. 98–4083. 1998. [Google Scholar]
- 46.Klein S, Burke LE, Bray GA, et al. Clinical implications of obesity with specific focus on cardiovascular disease: A statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: Endorsed by the American College of Cardiology. Circulation. 2004;110(18):2952–2967. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 47.Strickland PL, Deakin JFW, Percival C, Dixon J, Gater RA, Goldberg DP. Bio-social origins of depression in the community. Interactions between social adversity, cortisol and serotonin neurotransmission. Br J Psychiatry. 2002;180:168–173. doi: 10.1192/bjp.180.2.168. [DOI] [PubMed] [Google Scholar]
- 48.Whooley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med. 2000;343(26):1942–1950. doi: 10.1056/NEJM200012283432607. [DOI] [PubMed] [Google Scholar]
- 49.Centers for Disease Control and Prevention. [Accessed December 5, 2009];Obesity. Guide to Community Preventive Services. http://www.thecommunityguide.org/obesity/workprograms.html.
- 50.Thomas SL, Hyde J, Karunaratne A, Kausman R, Komesaroff PA. "They all work…when you stick to them": A qualitative investigation of dieting, weight loss, and physical exercise, in obese individuals. Nutr J. 2008;24(7):34. doi: 10.1186/1475-2891-7-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Drewnowski A, Rolls BJ. How to modify the food environment. J Nutr. 2005;135(4):898–899. doi: 10.1093/jn/135.4.898. [DOI] [PubMed] [Google Scholar]