Abstract
The traditional surgical treatment of severe spinal deformities, both in adult and pediatric patients, consisted of a 360° approach. Posterior-based spinal osteotomy has recently been reported as a useful and safe technique in maximizing kyphosis and/or kyphoscoliosis correction. It obviates the deleterious effects of an anterior approach and can increase the magnitude of correction both in the coronal and sagittal plane. There are few reports in the literature focusing on the surgical treatment of severe spinal deformities in large pediatric-only series (age <16 years old) by means of a posterior-based spinal osteotomy, with no consistent results on the use of a single posterior-based thoracic pedicle subtraction osteotomy in the treatment of such challenging group of patients. The purpose of the present study was to review our operative experience with pediatric patients undergoing a single level PSO for the correction of thoracic kyphosis/kyphoscoliosis in the region of the spinal cord (T12 and cephalad), and determine the safety and efficacy of posterior thoracic pedicle subtraction osteotomy (PSO) in the treatment of severe pediatric deformities. A retrospective review was performed on 12 consecutive pediatric patients (6 F, 6 M) treated by means of a posterior thoracic PSO between 2002 and 2006 in a single Institution. Average age at surgery was 12.6 years (range, 9–16), whereas the deformity was due to a severe juvenile idiopathic scoliosis in seven cases (average preoperative main thoracic 113°; 90–135); an infantile idiopathic scoliosis in two cases (preoperative main thoracic of 95° and 105°, respectively); a post-laminectomy kypho-scoliosis of 95° (for a intra-medullar ependimoma); an angular kypho-scoliosis due to a spondylo-epiphisary dysplasia (already operated on four times); and a sharp congenital kypho-scoliosis (already operated on by means of a anterior–posterior in situ fusion). In all patients a pedicle screws instrumentation was used, under continuous intra-operative neuromonitoring (SSEP, NMEP, EMG). At an average follow-up of 2.4 years (range, 2–6) the main thoracic curve showed a mean correction of 61°, or a 62.3% (range, 55–70%), with an average thoracic kyphosis of 38.5° (range, 30°–45°), for an overall correction of 65% (range, 60–72%). Mean estimated intra-operative blood loss accounted 19.3 cc/kg (range, 7.7–27.27). In a single case (a post-laminectomy kypho-scoliosis) a complete loss of NMEP occurred, promptly assessed by loosening of the initial correction, with a final negative wake-up test. No permanent neurologic damage, or instrumentation related complications, were observed. According to our experience, posterior-based thoracic pedicle subtraction osteotomies represent a valuable tool in the surgical treatment of severe pediatric spinal deformities, even in revision cases. A dramatic correction of both the coronal and sagittal profile may be achieved. Mandatory the use of a pedicle screws-only instrumentation and a continuous intra-operative neuromonitoring to obviate catastrophic neurologic complications.
Keywords: Thoracic pedicle subtraction osteotomy, Severe pediatric spinal deformities, Surgical treatment, Posterior-instrumented fusion only, Thoracic pedicle screws
Introduction
The traditional surgical treatment of severe spinal deformities, both in adult and pediatric patients, consisted of a 360° approach. A first stage of anterior release by means of multilevel discectomies and/or corpectomies through an open thoracotomy–thoracophrenolaparotomy was completed by a posterior instrumented fusion [1–5]. A consistent period of pre-operative Halo-traction in single-staged operations, or a long period of Halo-traction between anterior release and posterior instrumentation in two-staged procedures was often guaranteed so as to obtain a certain flexibility of the deformity itself and promote a better respiratory rehabilitation [6–8]. Sometimes, in highly rigid deformities, this combined program was preceded by an additional posterior release [1].
Vertebrectomy was first described in 1922 by MacLennan [9] who described an apical resection from a posterior-only approach with postoperative casting for the treatment of severe scoliosis. Several authors have subsequently reported their experiences with vertebrectomy mostly for congenital scoliosis [9–16], but also used to address oncologic diseases [17]. In late 1980s, a circumferential vertebral column resection (VCR) approach for severe, rigid spinal deformity was first described by Bradford [18]. He was the first to describe the use of a circumferential VCR coupled with concave rib osteotomies, convex thoracoplasty, and segmental spinal instrumentation with fusion in 13 patients with severe, structural deformities. Later on, in 1997, he and Boachie-Adjei [19] further expanded on Bradford’s original case series reporting on 16 patients undergoing the same procedure. Excellent deformity correction and rebalancing of the trunk was reported with few serious complications. The procedure was more extensive than the original vertebrectomy procedure for congenital hemivertebra.
Posterior-based spinal osteotomy has recently been reported as a useful and safe technique in maximizing kyphosis and/or kyphoscoliosis correction [20]. It obviates the deleterious effects of an anterior approach and can increase the magnitude of correction both in the coronal and sagittal plane [21, 22]. The advent of modern segmental spinal instrumentation, in particular pedicle screws fixation, introduced more stable constructs available for the treatment of these challenging, multiplanar, rigid deformities of the spine. Several authors [23–28] reported on their experience with a posterior-only approach, either with concomitant extensive posterior releases, including ligaments and facet joints at multiple levels (Ponte or Smith-Petersen type osteotomies), a posterior-based vertebral decancellation (pedicle subtraction osteotomy or eggshell procedure), or complete corpectomy (posterior hemivertebra excision and circumferential posterior-only VCR approach), as reported by Suk et al. [29] in early 1998.
Lumbar pedicle subtraction osteotomy (PSO) was first described by Thomasen [30] in 1985 for the management of fixed sagittal plane deformities in ankylosing spondylitis and became an increasingly popular method for correcting spinal kyphosis from a number of other etiologies [16, 24]. The technique involves a transpedicular vertebral wedge resection from a dorsal approach and is particularly useful for treating patients who have had a previous anterior fusion of the spine. Nevertheless, it can be used in a wide variety of other settings that result in flatback or kyphotic decompensation syndromes, including congenital anomalies, post-traumatic deformities, metabolic bone disorders, mycotic degeneration, and neoplastic disease [31, 32]. For correction of kypho-scoliotic deformities, an asymmetrical osteotomy can also be performed. By resecting a larger wedge on the convex rather than on the concave side of the vertebral body, coronal plane correction can be achieved during wedge closure. The technique may also be used above the level of the conus, including the cervical and thoracic spine, but more care is required above the cauda equine [33].
To our knowledge, there are few reports in the literature focusing on the surgical treatment of severe spinal deformities in large pediatric-only series (age <16 years old) by means of a posterior-based spinal osteotomy [20, 26], with no consistent results on the use of a single posterior-based thoracic pedicle subtraction osteotomy in the treatment of such challenging group of patients. The purpose of the present study was to review our operative experience with pediatric patients undergoing a single level PSO for the correction of thoracic kyphosis/kyphoscoliosis in the region of the spinal cord (T12 and cephalad), and determine the safety and efficacy of posterior thoracic pedicle subtraction osteotomy (PSO) in the treatment of severe pediatric deformities.
Materials and methods
A retrospective review was performed on 12 consecutive pediatric patients (6 F, 6 M) treated by means of a posterior thoracic PSO (t-PSO) between 2002 and 2006 in a single Institution. An independent spine surgeon reviewed all the medical records and X-rays of the patients considered. Inpatient and outpatient charts were used for collecting demographic data, previous surgical treatment, peri-operative treatment, and annotation of any medical and surgical-related complications [34, 35], including revision surgeries. Radiographic evaluation included standing postero-anterior and lateral films on long-cassettes (90 × 30 cm), before and after surgery and at the latest follow-up. Cobb measurements [36] of the major thoracic curve (MT) were obtained, and the lateral films were evaluated for thoracic kyphosis (T5-T12). Supine preoperative bending films were used to determine flexibility. Supine preoperative radiographs were also performed in a corrective Risser plaster, held for a few hours, to assess the correction rate in the plaster cast. Offset in the coronal plane was determined by measuring (in cm) the distance between the C7 plumb line and the perpendicular line drawn through the center of the S1 vertebral body [center sacral vertical line (CSVL)] (global coronal balance) [37]. MRI of the spine, including cervical, thoracic, and lumbar segments, was performed preoperatively to exclude congenital intra-medullar anomalies, whereas in revision patients, a preoperative 3D CT scan was also included to understand vertebral column anatomo-pathology prior to surgery.
Indication for a t-PSO included a severe, relatively rigid spinal deformity both in the coronal (major scoliosis >90°) and in the sagittal plane (major kyphosis or apical kyphosis >80°). A moderate flexibility (20–40%) on the corrective Risser plaster was considered sufficient so as to avoid an anterior release.
Average age at t-PSO surgery was 12.6 years (range, 9–16), with all patients having a Risser’s sign inferior of 2. A pre-operative conservative treatment by means of a TLSO for an average 4.5 years (range, 2–9) could not prevent a rapid progression of their deformity. The deformity was due to a severe juvenile idiopathic scoliosis in seven cases (average preoperative main thoracic 113°; 90–135); an infantile idiopathic scoliosis in two cases (preoperative main thoracic of 95° and 105°, respectively); a post-laminectomy kypho-scoliosis of 95° (for an intra-medullar ependimoma); an angular kypho-scoliosis of 105° due to a spondylo-epiphisary dysplasia (already operated on four times); and a sharp congenital kypho-scoliosis of 85° (already operated on by means of a anterior–posterior in situ fusion 4 years before).
A preoperative Halo-gravity traction was performed in nine cases (all idiopathic ones) for an average of 3.5 weeks (range, 2–4), following the well-known protocols already described in literature [7, 8]. Traction was maintained generally until a 35–40% of body weight was obtained and a satisfying correction was shown on radiographic evaluation.
Patients underwent a one-level t-PSO at the apex of their main deformity, always performed at T11 or cephalad region of the spinal cord (Table 1). In nine cases, the t-PSO was the first procedure, whereas in three patients the osteotomy represented a revision surgery. The osteotomy was followed by a posterior-based segmental arthrodesis using an all-pedicle screws instrumentation, including poliaxial and/or reduction screws, under continuous intra-operative neuromonitoring (SSEP, NMEP, EMG). In kyphotic deformities, the fusion area included at least three levels above and below the osteotomy, whereas when a kypho-scoliosis had to be addressed the already reported criteria were followed [38].
Table 1.
Osteotomy level and number of patients
| Osteotomy level | Number of patients |
|---|---|
| T7 | 2 |
| T8 | 3 |
| T9 | 2 |
| T10 | 3 |
| T11 | 2 |
Statistical analysis included the t-test (paired and unpaired), the Wilcoxon test for non-parametric paired analysis, and the Mann–Whitney test for non-parametric unpaired analysis, with results expressed as mean (range, min–max).
Results
At an average follow-up of 2.4 years (range, 2–6) we found a mean hospitalization after the t-PSO surgical procedure of 10.4 days (range, 8–13), with all patients encouraged to maintain sitting position as soon as pain permit it. Intensive care unit stay was 1.5 days (range, 1–2) mainly to better address early post-operative pain. A prolonged mechanical ventilation, re-intubation, or thoracic drain insertion was not encountered in any case of the present series. An aggressive post-operative pulmonary rehabilitation program was always initiated as soon as patients returned to ordinary ward, being prescribed for at least 2 months. All patients were discharged with a TLSO for a mean of 3.5 months (range, 2–4) to be worn only day-time.
Mean estimated blood loss during the present series was found up to 19.3 cc/kg (range, 7.7–27.27), whereas in a single case (a post-laminectomy kypho-scoliosis) a complete loss of NMEP occurred, promptly assessed by loosening of the initial correction, with a final negative wake-up test. A total five medical complications [35] (moderate pleural effusion in 3, pneumonia secondary to moderate atelectasis in 1, superior mesenteric artery syndrome in 1) did not necessitate any invasive procedure and healed uneventfully with no adverse effects on final results. Screw misplacement at thoracic level was suspected on postoperative X-rays in three cases (three screws), all considered within a “definite safe zone” at the post-operative Tc control [38]. Screw misplacement did not present evidence of risks and did not cause any symptoms, thus it was decided to leave the misplaced screws in place. At a mean follow-up of 2.4 years (range, 2–6), there were no changes in the X-ray control and no symptoms. No permanent neurologic damage, early superficial to late deep infection, instrumentation-related complications or pseudoarthrosis were observed at latest follow-up.
For what concerned the radiographic evaluation, the preoperative main thoracic curve averaged 103° (range, 85–135), at supine side bending showed a flexibility of only 20% (range, 10–35), which increased up to 32% (range, 20–40) on the corrective Risser plaster. At latest follow-up, we observed a mean correction of 61° (range, 45–75), or a 62.3% (range, 55–70%), with an average thoracic kyphosis of 38.5° (range, 30–45°), for an overall correction of 65% (range, 60–72%) (Table 2). All patients were found to be well compensated for what concerned both overall sagittal contour and global coronal alignment, with no signs of crankshaft phenomenon or progression of a secondary curve not included in the instrumented arthrodesis.
Table 2.
Demographic data and radiologic evaluation
| Mean | Range | Significance | |
|---|---|---|---|
| Age (years) | 12.6 | 9–16 | – |
| Risser | 0.4 | 0–2 | – |
| Follow-up (years) | 2.4 | 2–6 | – |
| Preoperative main thoracic curve | 103° | 85–135 | – |
| Preoperative main thoracic curve bending | 85° | 75–120 | – |
| Flexibility of main thoracic curve | 20.2% | 10–35 | n.s |
| Flexibility of main thoracic curve-risser | 32.3% | 20–40 | n.s |
| Follow-up main thoracic curve | 45° | 38–65 | – |
| Final main thoracic curve correction (Pre-op)-(follow-up) | 61° | 45–75 | 0.0001 |
| Final percent correction main thoracic curve | 62.3% | 55–70 | 0.0000 |
| Post-resection main thoracic curve loss (follow-up-postop) | 2.27° | 0–5 | n.s |
| Preoperative kyphosis (T5-T12) | 62° | 65–105 | – |
| Follow-up kyphosis (T5-T12) | 38.5° | 30–45 | – |
| Overall kyphosis correction (Pre-op)-(follow-up) | 65% | 60–72 | 0.0001 |
| Preoperative global coronal balance (C7-S1) (cm) | 2.17 | 0.2–4 | . |
| Follow-up global coronal balance (C7-S1) (cm) | 0.76 | 0–2.1 | 0.002 |
n.s. not significant
Discussion
Spinal deformity is a three-dimensional pathology. Decompensation both in the coronal and the sagittal plane leads to specific clinical complaints, pain, neurology, progression of deformity, deranged trunk balance, cardiopulmonary compromise, or interference with activities of daily living [18, 19, 39, 40]. A combined anterior release and fusion followed by a posterior spinal fusion and instrumentation was often performed for both large (more than 90°–95°) and stiff (more than 70°–80° at side bending) curves, those with a significant lordotic or hyperkyphotic sagittal thoracic alignment, and in skeletally immature patients to prevent the crankshaft phenomenon [41]. The anterior release and fusion is performed through either an endoscopic or open approach, with similar results reported for each approach [42–45]. Both open anterior and endoscopic approaches have negatively impacted pulmonary function when compared to a posterior-only approach [22, 46].
The correction rate of severe vertebral column deformity with a combined anterior–posterior treatment was 45–47%, using Harrington instrumentation [2] or the multiple hook construct [5], 52% using Zielke instrumentation with Harrington rod [3], and up to 67%, using anterior instrumentation and posterior hybrid construct [1]. The combined anterior and posterior procedure was performed in 1-stage or 2-stage surgery according to different authors with different outcomes: Shuffleburger et al. [5] found decreased hospital stay and operating time, fewer complications, and better correction in the continuous group compared to the staged group; more recently, Shen et al. [47] concluded that there was no significant difference in safety or efficacy between the 1-stage or 2-stage groups.
On the other hand, the role of an all posterior approach using pedicle screws-only instrumentations has been widely reported in the treatment of severe, rigid kypho-scoliosis [38, 48]. Furthermore, two recent studies [1, 21] compared combined treatment (anterior and posterior fusion) versus posterior fusion only in severe AIS: Luhmann and Lenke [21] concluded that patients treated with pedicle screw-only instrumentation presented similar results to patients with combined treatment (60.7 vs. 58.5%), without the negative effects on pulmonary function from anterior release. In highly rigid severe spinal deformities (more than 100°), conventional correction methods, such as posterior only or anterior release and posterior instrumentation, are usually unsatisfactory; therefore, a more aggressive approach is necessary [29].
Recently, Suk et al. reported on a posterior-only approach with a VCR for fixed lumbar spinal deformities [29], as well as for severe, rigid scoliosis [49, 50]. They reported excellent surgical correction with minimal long-term complications for thoracic and lumbar deformities resected around the cauda equina region, with similar results for the thoracic scoliosis patients except for one permanent postoperative paraplegia.
The present series results on twelve consecutive pediatric patients affected by a severe, rigid deformity (Table 2) can be well allocated in the latter type of deformities and surgical treatment reserved for. The accurate pre-operative assessment that routinely includes a corrective Risser plaster was found to be of paramount importance in determining the intermediate flexibility (between 20–40%) shown in the present series. Such flexibility, in particular on the sagittal plane, permitted a less aggressive surgical treatment with respect to vertebral column resection as described by Suk et al. [49, 50], by performing an apical t-PSO [16, 24, 33, 38]. Combined with the wide posterior release performed for the accurate thoracic pedicle screw placement according to the “mini-laminectomy” technique [38], a dramatic correction of both the coronal (62.3%) and sagittal (65%) profile may be achieved even in severe, rigid kypho-scoliosis (average preoperative main thoracic curve of 103°) (Fig. 1).
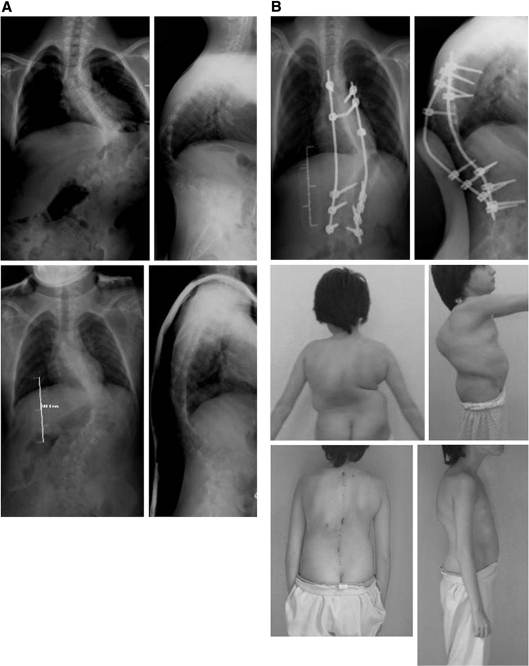
Fig. 1.
An infantile idiopathic scoliosis of 95°. 11 + 8 years; Female. a Satisfying correction on the Risser cast, b Radiographic and clinical result after a t-PSO at T10
Our results combined with those of the recent literature [16, 21, 26, 38, 48–50] permit to create a treatment based “algorithm” for choosing the best type of posterior osteotomy to be performed, taking into account the flexibility of the curve to be addressed:
flexibility > 40%: wide posterior release ± Ponte/Smith-Petersen Osteotomies,
flexibility between 20–40%: PSO (eventually asymmetric),
flexibility < 20%: posterior-only VCR.
It should be noted that only an all-pedicle screw instrumentation can provide a rigid and stable construct that permit such destabilising procedures to be performed [49]. The advent of ultimate generation pedicle screws, including poliaxial/reduction screws placed in strategic positions (apical concave vertebra; proximal and/or distal regions of severe kyphosis or kyphoscoliosis; instrumentation upper and lower limit vertebra) make easier and safer performing substantial multiplanar corrective maneuvers. These corrective maneuvers include a contemporary distraction-traslation, counter clock-wise derotation on convexity-compression, direct vertebral rotation, or “in situ” bending.
Even if technically demanding and potentially prone to catastrophic neurologic complications, performing a t-PSO has been demonstrated to be safe according to the present series results. In a single case (a post-laminectomy kypho-scoliosis), a complete loss of NMEP occurred promptly assessed by loosening of the initial correction, with a final negative wake-up test (Fig. 2). It is in such particular cases that the present authors concur with the strict recommendation made by Cheh and Lenke [20] so as to perform as safely as possible such demanding procedures. It should be anticipated that during the corrective maneuvers, in particular during the osteotomy closure, the mielo-radicular tissues sustain a significant mechanical strain. That is particularly true when an angular kyphosis is addressed, being the latter the only reported to be associated with significant, permanent neurologic injuries [20, 49]. The use of temporary correction rods to be progressively changed may result particularly useful, preventing unintentional osteotomy closures, or dramatic anterior subluxations [16, 20, 50].
Fig. 2.
A post-laminectomy kypho-scoliosis of 95° (intra-medullar ependimoma). 11 + 8 years; Female. a Signs of spinal cord cavitation on MRI; Incomplete paraplegia at presentation. Satisfying correction on the Risser cast, b A complete loss of NMEP occurred during t-PSO at T8 closure, promptly assessed by loosening of the initial correction, with a final negative wake-up test. Complete resolution of pre-operative incomplete paraplegia by post-operative 3rd month
Another crucial point is the continuous, meticulous inspection of neural elements during such corrective maneuvers. A wide laminectomy, usually one level above and one level below the osteotomy, should always be performed with sufficient exposition of the neuroforamen bilaterally.
Once definitive rods have been positioned and locked both spinal cord and corresponding roots should be carefully inspected to assess any osteo-ligamentous impingement or retained bony/disc material during the corrective procedure. In this perspective, it is absolutely imperative to have a continuous intra-operative neuromonitoring (in particular NMEP) to promptly identify and subsequently obviate catastrophic neurological complications. A complete loss of NMEP data, with absolutely normal SSEP registration, has been reported [20] to occur with an incidence up to 21.4% (9 cases in a total of 42 vertebral resection surgeries) some time during the surgical procedure, most commonly during the actual spinal shortening and correction. In their series, Cheh and Lenke [20] have advocated a three step-wise “prompt surgical intervention” once a neurologic incident occurs:
Maintain normo-tensive anesthesia during correction and closure of osteotomy, with mean arterial pressure (MAP) at least 75–80 mm Hg during this time;
Release the correction obtained by loosening the set plugs;
Thereby, lessen the correction and removing the rods if needed.
In all cases, SSEPs were unchanged and NMEPs returned varying from 8 to 20 min after loss, with all patients having a normal wake-up test intra-operatively and a normal neurologic examination after surgery [20].
Finally, as evidenced by prior reports [16, 33], the versatility and safety of single level PSO seems guaranteed. This posterior-only approach, according to the present series, appears a safe but challenging technique to treat severe primary or revision (Fig. 3) pediatric spinal deformity. By resecting a larger wedge on the convex rather than on the concave side of the vertebral body, coronal plane correction can be achieved during wedge closure. It allows for dramatic radiographic and clinical correction of these severely deformed patients both in coronal and the sagittal profile. At a mean follow-up of 2.4 years (range, 2–6), there were no changes in the X-ray control and no symptoms. No permanent neurologic damage, early superficial to late deep infection, instrumentation-related complications or pseudoarthrosis were observed. All patients were found to be well compensated for what concerned both overall sagittal contour and global coronal alignment, with no signs of crankshaft phenomenon or progression of a secondary curve not included in the instrumented arthrodesis.
Fig. 3.
A sharp congenital kypho-scoliosis of 85°. 9 + 6 years; Male. a Patient already operated on by means of a anterior–posterior in situ fusion four years before. Satisfying correction on the Risser cast, mainly on the sagittal profile, b Radiographic and clinical result after a t-PSO at T11
Conclusions
According to our experience, posterior-based thoracic pedicle subtraction osteotomies represent a valuable tool in the surgical treatment of severe pediatric spinal deformities, even in revision cases. A dramatic correction of both the coronal and sagittal profile may be achieved. Mandatory the use of a pedicle screws-only instrumentation and a continuous intra-operative neuromonitoring to obviate catastrophic neurologic complications.
Conflict of interest
None of the authors has any potential conflict of interest.
References
- 1.Bullmann V, Halm HFH, Schulte T, Lerner T, Weber TP, Liljenqvist UR. Combined anterior and posterior instrumentation in severe and rigid idiopathic scoliosis. Eur Spine J. 2006;15:440–448. doi: 10.1007/s00586-005-1016-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Byrd JA, Scoles PV, Winter RB, Bradford DS, Lonstein JE, Moe JH. Adult idiopathic scoliosis treated by anterior and posterior spinal fusion. J Bone Joint Surg Am. 1987;69:843–850. [PubMed] [Google Scholar]
- 3.Korovessis P. Combined VDS and Harrington instrumentation for treatment of idiopathic double major curves. Spine. 1987;12:244–250. doi: 10.1097/00007632-198704000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Savini R, Parisini P et al (1989) The surgical correction of severe vertebral deformities by combined anterior and posterior instrumentation. Prog Spinal Pathol 4:211–221
- 5.Shufflebarger HL, Grimm JO, Bui V, Thomson JD. Anterior and posterior spinal fusion. Staged versus same-day surgery. Spine. 1991;16:930–933. doi: 10.1097/00007632-199108000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Pellin B, Zielke K. Severe scoliosis in adults and older, adolescents. 41 operated cases. Rev Chir Orthop Reparatrice Appar Mot. 1974;60:623–633. [PubMed] [Google Scholar]
- 7.Savini R, Parisini P, Corbascio M, Prosperi L (1977) L’ halo trazione associata alla fisio kinesi terapia nel trattamento correttivo delle scoliosi con gravissimi deficit respiratori. C.O.M vol XLIII fasc. IV.: 353–360 [PubMed]
- 8.Rinella A, Lenke L, Whitaker C, Kim Y, Park SS, Peelle M, Edwards C, 2nd, Bridwell K. Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine. 2005;30:475–482. doi: 10.1097/01.brs.0000153707.80497.a2. [DOI] [PubMed] [Google Scholar]
- 9.Compere EL. Excision of hemivertebrae for correction of congenital scoliosis: report of two cases. J Bone Joint Surg. 1932;14:555–562. [Google Scholar]
- 10.Wiles P. Resection of dorsal vertebrae in congenital scoliosis. J Bone Joint Surg Am. 1951;33:151–154. [PubMed] [Google Scholar]
- 11.Leatherman KD, Dickson RA. Two-stage corrective surgery for congenital deformities of the spine. J Bone Joint Surg Br. 1979;61:324–328. doi: 10.1302/0301-620X.61B3.479255. [DOI] [PubMed] [Google Scholar]
- 12.Floman Y, Penny JN, Micheli LJ, et al. Osteotomy of the fusion mass in scoliosis. J Bone Joint Surg Am. 1982;64:1307–1316. [PubMed] [Google Scholar]
- 13.Luque ER. Vertebral column transposition. Orthop Trans. 1983;7:29. [Google Scholar]
- 14.Tokunaga M, Minami S, Kitahara H, et al. Vertebral decancellation for severe scoliosis. Spine. 2000;25:469–474. doi: 10.1097/00007632-200002150-00013. [DOI] [PubMed] [Google Scholar]
- 15.Deviren V, Berven S, Smith JA, et al. Excision of hemivertebrae in the management of congenital scoliosis involving the thoracic and thoracolumbar spine. J Bone Joint Surg Br. 2001;83:496–500. doi: 10.1302/0301-620X.83B4.11699. [DOI] [PubMed] [Google Scholar]
- 16.Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine. 2006;31(19 Suppl):S171–S178. doi: 10.1097/01.brs.0000231963.72810.38. [DOI] [PubMed] [Google Scholar]
- 17.Tomita K, Kawahara N, et al. Total en bloc spondylectomy for spinal tumors: improvement of the technique and its associated basic background. J Orthop Sci. 2006;11:3–12. doi: 10.1007/s00776-005-0964-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bradford DS. Vertebral column resection. Orthop Trans. 1987;11:502. [Google Scholar]
- 19.Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine. 1997;22:1590–1599. doi: 10.1097/00007632-199707150-00013. [DOI] [PubMed] [Google Scholar]
- 20.Cheh G, Lenke LG, et al. Loss of spinal cord monitoring signals in children during thoracic kyphosis correction with spinal osteotomy. Why does it occur and what should you do? Spine. 2008;33:1093–1099. doi: 10.1097/BRS.0b013e31816f5f73. [DOI] [PubMed] [Google Scholar]
- 21.Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70° and 100°. Is anterior release necessary? Spine. 2005;30:2061–2067. doi: 10.1097/01.brs.0000179299.78791.96. [DOI] [PubMed] [Google Scholar]
- 22.Kim YJ, Lenke LG, Bridwell KH, Kim KL, Steger-May K. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87:1534–1541. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 23.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res. 1969;66:6–9. [PubMed] [Google Scholar]
- 24.Bridwell KH, Lewis SJ, Lenke LG, et al. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. J Bone Joint Surg Am. 2003;85:454–463. doi: 10.2106/00004623-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Shono Y, Abumi K, Kaneda K. One-stage posterior hemivertebra resection and correction using segmental posterior instrumentation. Spine. 2001;26:752–757. doi: 10.1097/00007632-200104010-00011. [DOI] [PubMed] [Google Scholar]
- 26.Ruf M, Harms J. Hemivertebra resection by a posterior approach: innovative operative technique and first results. Spine. 2002;27:1116–1123. doi: 10.1097/00007632-200205150-00020. [DOI] [PubMed] [Google Scholar]
- 27.Kawahara N, Tomita K, Baba H, et al. Closing-opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine. 2001;26:391–402. doi: 10.1097/00007632-200102150-00016. [DOI] [PubMed] [Google Scholar]
- 28.Smith JT, Gollogly S, Dunn HK. Simultaneous anterior-posterior approach through a costotransversectomy for the treatment of congenital kyphosis and acquired kyphoscoliotic deformities. J Bone Joint Surg Am. 2005;87:2281–2289. doi: 10.2106/JBJS.D.01795. [DOI] [PubMed] [Google Scholar]
- 29.Suk SI, Kim JH, Kim WJ et al (1998) Treatment of fixed lumbosacral kyphosis by all posterior vertebral column resection. Presented at: 5th international meeting on advanced spine techniques, Sorrento, Italy
- 30.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142–152. [PubMed] [Google Scholar]
- 31.Buchowski JM, Bridwell KH, Lenke LG, et al. Neurologic complications of lumbar pedicle subtraction osteotomy. A 10-year assessment. Spine. 2007;32:2245–2252. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 32.Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation. Spine. 1997;22:2452–2457. doi: 10.1097/00007632-199710150-00025. [DOI] [PubMed] [Google Scholar]
- 33.Wang MY, Berven SH. Lumbar pedicle subtraction osteotomy. Neurosurgery. 2007;60(2 suppl 1):140–146. doi: 10.1227/01.NEU.0000249240.35731.8F. [DOI] [PubMed] [Google Scholar]
- 34.Asher M et al (2004) Safety and efficacy of Isola instrumentation and arthrodesis for adolescent idiopathic scoliosis. Spine 29:2013–2023 [DOI] [PubMed]
- 35.Tsirikos AI, Chang WN, et al. Comparison of one-stage versus two-stage anteroposterior spinal fusion in pediatric patients with cerebral palsy and neuromuscular scoliosis. Spine. 2003;28:1300–1305. doi: 10.1097/01.BRS.0000065572.10824.AB. [DOI] [PubMed] [Google Scholar]
- 36.Cobb JR. Outline for the study of scoliosis. AAOS Instr Course Lect. 1948;5:261–275. [Google Scholar]
- 37.O’Brien M, Kuklo T et al (2004) Spinal deformity study group. Radiographic Measurement Manual. Edition Medtronic Sofamor Danek
- 38.Di Silvestre M, Bakaloudis G, Lolli F, Vommaro F, Martikos K, Parisini P. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17(10):1336–1349. doi: 10.1007/s00586-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis. An evidence-based review. Spine. 2007;32:S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 40.Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis: a 50-year natural history study. JAMA. 2003;289:559–567. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 41.Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989;9:541–550. doi: 10.1097/01241398-198909010-00008. [DOI] [PubMed] [Google Scholar]
- 42.Graham EJ, Lenke LG, Lowe TG, et al. Prospective pulmonary function evaluation following open thoracotomy for anterior spinal fusion in adolescent idiopathic scoliosis. Spine. 2000;25:2319–2325. doi: 10.1097/00007632-200009150-00009. [DOI] [PubMed] [Google Scholar]
- 43.Anand N, Regan JJ. Video-assisted thoracoscopic surgery for thoracic disc disease: classification and outcome study of 100 consecutive cases with a 2-year minimum follow-up period. Spine. 2002;27:871–879. doi: 10.1097/00007632-200204150-00018. [DOI] [PubMed] [Google Scholar]
- 44.Mack MJ, Regan JJ, McAfee PC, et al. Video-assisted thoracic surgery for the anterior approach to the thoracic spine. Ann Thorac Surg. 1995;59:1100–1106. doi: 10.1016/0003-4975(95)00112-X. [DOI] [PubMed] [Google Scholar]
- 45.Newton PO, Wenger DR, Mubarak SJ, et al. Anterior release and fusion in pediatric spinal deformity. A comparison of early outcome and cost of thoracoscopic and open thoracotomy approaches. Spine. 1997;22:1398–1406. doi: 10.1097/00007632-199706150-00020. [DOI] [PubMed] [Google Scholar]
- 46.Lenke LG, Newton PO, Marks MC, et al. Prospective pulmonary function comparison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine. 2004;29:2055–2060. doi: 10.1097/01.brs.0000138274.09504.38. [DOI] [PubMed] [Google Scholar]
- 47.Shen J, Qiu G, Wang Y, Zhang Z, Zhao Y. Comparison of 1-stage versus 2-stage anterior and posterior spinal fusion for severe and rigid idiopathic scoliosis—A randomized prospective study. Spine. 2006;31:2525–2528. doi: 10.1097/01.brs.0000240704.42264.c4. [DOI] [PubMed] [Google Scholar]
- 48.Dobbs MB, Lenke LG, Kim YJ, Luhmann SJ, Bridwell KH. Anterior/posterior spinal instrumentation versus posterior instrumentation alone for the treatment of adolescent idiopathic scoliotic curves more than 90°. Spine. 2006;31:2386–2391. doi: 10.1097/01.brs.0000238965.81013.c5. [DOI] [PubMed] [Google Scholar]
- 49.Suk SI, Kim JH, Kim WJ, Lee SM, Chung ER, Nah KH. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374–2382. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 50.Suk SI, Chung ER, Kim JH, Kim SS, Lee JS, Choi WK. Posterior vertebral column resection for severe rigid scoliosis. Spine. 2005;30:1682–1687. doi: 10.1097/01.brs.0000170590.21071.c1. [DOI] [PubMed] [Google Scholar]