Abstract
Direct repair of spondylolisthesis can save a functional segment in young patients with slight slipping. Since 1968 many surgeons have proposed different technical solutions to obtain the isthmic repair. Their results changed according to the technique used, the extent of listhesis and the age of the patient. The aim of our study was to perform a retrospective review on the long-term results of the direct repair of spondylolisthesis, according to the different techniques used. We operated 62 patients for isthmic repair, with three different techniques, from 1994 to 2007. We analysed the clinical and radiographic results of 52 cases, with an average follow-up of 9 ± 3 years (range 2–15). Ten patients were lost to the follow-up. The results were different depending on the technique used. Good or excellent clinical outcome by Odom’s criteria were observed in the 83.3% of patients operated with the modified Scott technique. These results are better than those obtained in the group of patients operated with the Scott (62.5%) and the Buck technique (28.5%). Patients with clinical and radiological failure, who then underwent spinal fusion, were 57% with the Buck technique, 12.5% with the Scott technique and 2.7% with the Scott modified technique. The reasons for a new operation were symptomatic pseudarthrosis and progression of slipping. In conclusion, the pars defect repair is a helpful technique in lumbar spondylolisthesis, especially in young patient with slight slipping and painful symptoms resistant to conservative treatment. In our experience, the modified Scott technique seems to provide a better outcome than the Scott and Buck techniques.
Keywords: Direct repair, Spondylolisthesis, Low back pain, Lumbar spine treatment
Introduction
Isthmic repair is an effective surgical procedure in lumbar spondylolysis and spondylolisthesis. It must be performed in young patients with slight slipping and painful symptoms resistant to conservative treatment. The technique avoids fusion, thus saving movement.
Kimura [15] first described direct repair of the defect in 1968. He used bone graft without internal fixation.
In 1970 Buck [5] performed the isthmic repair by iliac bone graft and two trans-isthmic screws. After that other surgeons proposed their technical solution to obtain the isthmic repair. In 1968 Scott performed the fixation with two steel wirings that proceeded anterior to the transverse process and were anchored to the spinous process. This is now widely known as the Scott wiring technique, but his results were not published until 1986 [17]. Morscher et al. [16] described their treatment with bone grafting and direct stabilization by means of a hook and a screw for each side. Tokuhashi and Matsuzaki [26] proposed repairing the deficit by segmental pedicular screws and laminar hook fixation. Subsequently Salib and Pettine [21], Songer and Rovin [24] proposed fixation by pedicular screws, segmental wire and bone grafting. Gillet [11] reported on a rod-screw construct.
The results changed according to the technique used, the extent of listhesis and the age of the patient [1, 6, 13, 14, 16, 17]. However, while the clinical results are good in most cases regardless of the technique used, the radiographic results show significant differences in relation to surgical technique and age of the patient [4, 8, 20, 27].
The aim of our study was to perform a retrospective review on long-term results of the direct repair of spondylolisthesis, according to the different techniques used. We considered some parameters, such as pain, quality of life, capacity to perform the functions of daily life and social relationships. Moreover, we analysed clinical and radiological findings.
Materials and methods
We performed a retrospective study of a consecutive series of 62 patients who were operated with isthmic repair from 1994 to 2007, with Buck, Scott and modified Scott technique. The data were retrieved using the DOVAC computer system.
Inclusion criteria were: spondylolysis and spondylolisthesis with slipping less than 15%, age under 25 years and painful symptoms resistant to conservative treatment. All the patients included in the study were operated at least 2 years before and underwent complete radiographic documentation (X-rays and MRI) and clinical controls directly or by phone.
Disability was measured by the Oswestry disability index (ODI 0 = no disability/ODI 100 = complete disability), whereas the perceived pain was measured by visual analogue scale (VAS 0 = no pain/VAS 10 = worst pain imaginable) by means of a self-completed questionnaire at the control.
Moreover, analysis of the patient’s outcome was done using Odom’s criteria: excellent is absence of symptoms, good is minimal persistence of symptoms, fair is slight improvement of symptoms, and poor when symptoms are unchanged or exacerbated.
Surgical techniques
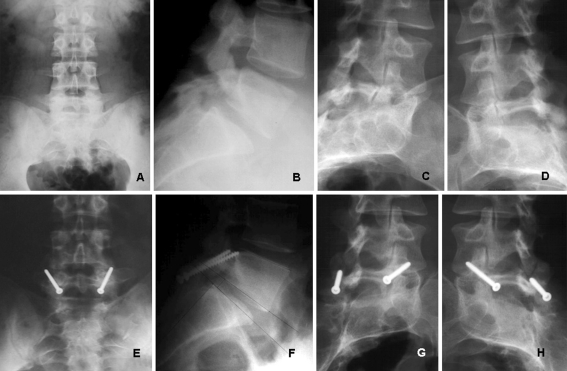
The patient was placed in a prone position, with the spine in a neutral position and the abdomen free of pressure. Through a posterior longitudinal midline incision, the paravertebral muscles were stripped to expose the spinous processes, lamina, and both transverse processes. To avoid stress on the isthmus, the inferior facet joints of the above vertebrae were removed with an osteotome, taking care to remove as little capsular structure as possible. The defect of the pars interarticularis was cleared of any fibrous and cartilagineous tissues; sclerotic bone margins were curetted. At this time, the three surgical techniques proceeded differently. The Buck technique (Fig. 1), performed in the first 7 cases (11.3%), involved a trans-isthmic screw fixation. In all cases the synthesis was performed with two 4.5 mm cortical screws. The isthmic defect was filled in by cancellous bone graft from the iliac crest.
Fig. 1.
16-year-old male—symptomatic spondylolysis. a–d Preoperative X-rays; e–h isthmic repair by Buck technique—follow-up at 10 years
Because of some technical difficulties, over the next 10 cases (16.1%) we performed the Scott technique (Fig. 2), which makes use of a segmental wire fixation from the transverse processes to the spinous process and bone grafting at the lytic defect.
Fig. 2.
20-year-old male—symptomatic spondylolysis. a–d Preoperative X-rays; e–h isthmic repair by Scott technique—follow-up at 10 years
Due to some limitations of the previous technique, we used the modified Scott technique (pedicular screws and wiring) in the next 45 cases (72.6%). The surgical technique involved placement of two pedicular screws in the affected vertebra and the fixation of the loose posterior arch with a wire, taking purchase on the spinous process (Fig. 3). The system realized a dynamic compression. Iliac bone graft was placed in the pars defect before the assembly was tightened.
Fig. 3.
24-year-old male—symptomatic spondylolysis. a–d Preoperative X-rays; e–h isthmic repair by Scott modified technique—follow-up at 5 years
In all patients the wound was closed and a drainage tube was left. The patients were allowed to get up 1 day after surgery. They had to wear a lumbosacral support for the following 2 months.
Results
Patients included in the study were 40 males (64.5%) and 22 females (35.5%). The mean age at the time of operation was 18 ± 4.5 years (range 10–26). The symptoms were: backache in 55 cases (88.7%) and back and radicular pain in 7 cases (11.3%). The defect was in L5 in 59 cases (95.1%) and in L4 in 3 cases (4.9%). The slipping on average was 8 ± 4% (range 0–15%). We did not observe any intra or post-operative complications. The average intra-operative blood loss was 180 ± 83 cc (ranging from 100 to 450).
We analysed the clinical and radiographic results of 52 cases, with an average follow-up of 9 ± 3 years (range 2–15). Ten patients were lost to the follow-up (2 operated with the Scott technique and 8 operated with the Scott modified technique).
The clinical results of seven patients operated with the Buck technique were excellent or good in two cases (28.5%). One case (14.5%) was considered a fair result because backache was present. No change of the slipping, bone graft absorption, adjacent segment degeneration or loosening or breakage of the screws occurred in these patients. The results were poor in four cases (57%) because the patients had worsening pain and X-rays showed increase of the slipping in one case and bone graft absorption in three cases. They were later operated with posterolateral fusion.
The clinical results of eight patients operated with the Scott technique were excellent or good in five cases (62.5%), fair in two cases (25%). In all cases X-rays showed no change of the slipping, adjacent segment degeneration or bone graft absorption. Breakage and loosening of the wirings, but complete repair of defect, was observed in one case and the wires were removed. One case (12.5%) was considered a poor result. The patient had pain, increased slipping and bone graft absorption. He was later operated with posterolateral fusion.
The clinical results of 37 patients operated with the modified Scott technique were excellent or good in 31 cases (83.8%). Fair results were present in five cases (13.5%) because backache and sometimes radicular pain were still present. These patients showed no change of the slipping or adjacent segment degeneration on the X-rays. Breakage and loosening of the fixation were observed in three asymptomatic patients; removal of the implant was performed in one case.
One symptomatic patient (2.7%) was considered as a poor result. The X-rays showed worsening of the slipping and bone graft absorption. He was later operated with posterolateral fusion. The clinical results using Odom’s criteria are summarized in Table 1. The average results were 2.6% ODI score, VAS back 0.4 and VAS leg 0.1 on the last 36 patients who filled it, all operated by Scott modified technique.
Table 1.
Clinical results using Odom’s criteria
| Techniques | No. of patients | Excellent or good results | Fair results | Poor results (failed repair) |
|---|---|---|---|---|
| Buck | 7 | 2 (28.5%) | 1 (14.5%) | 4 (57%) |
| Scott | 8 | 5 (62.5%) | 2 (25%) | 1 (12.5%) |
| Scott modified | 37 | 31 (83.8%) | 5 (3.5%) | 1 (2.7%) |
Discussion
The most frequently used surgical procedure for symptomatic lumbar spondylolysis and spondylolisthesis is fusion, which determines a loss of spinal movement and subsequently an overload of adjacent segments.
A surgical technique that allows an anatomical repair of the isthmus and a functional recovery of the segmental motion could therefore be useful, despite the fact that some authors [22] have related similar clinical and radiological long-term outcomes between the isthmic repair and fusion.
Usually, the indications for isthmic direct repair are spondylolysis and spondylolisthesis with slight slipping in patients with painful symptoms resistant to conservative treatment and younger than 25 years [1, 4, 5, 14, 17, 20, 23]. The best results observed in young patients with mild vertebral slipping, have influenced our choice in surgical indication.
However, some authors [7, 8] have extended the indication for surgery also in adults with spondylolisthesis greater than 20%, sometimes combining a fusion [12].
Szypryt et al. [25] performed a study on the disc morphology with MRI on 40 patients with spondylolysis and spondylolisthesis. They observed no differences compared to normal subjects of the same age and gender in patients younger than 25 years, but there were more frequent degenerative changes in patients with spondylolysis and spondylolisthesis older than 25 years compared to the equivalent control group. This could explain the lower success of the direct repair in these patients [27]. In our opinion, the use of preoperative MRI, with the careful assessment of possible disc degeneration in the affected vertebra, allows a better selection of surgical indications and nowadays we perform it in all cases.
Over the years we have used three different surgical techniques, among those proposed by various authors [5, 11, 16, 19, 21, 23, 24, 26].
In the first seven cases we used the Buck technique that involves the isthmic repair by cancellous bone graft from the iliac crest and two trans-isthmic screw fixations. The accurate placement of screws was the main technical difficulty in achieving a good grip of the screws and adequate compression of the graft into the defect, especially in younger patients. Moreover, the screw itself occupied much of the isthmus and thus sometimes prevented the repair.
Because of this, we decided to use the Scott technique in the subsequent ten cases. This involves a segmental wire fixation from the transverse processes to the spinous process and bone grafting at the lytic defect. The passage of the wire around the base of the transverse process could be difficult, especially when the sacrum is very close to the transverse process of the L5. Sometimes it resulted in a longer surgery time and a greater loss of blood. In addition, it increased the risk of root or vascular damage and the wire could disengage from the transverse process; for this reason, the wires must be pulled very tight. However, the use of the tension band wiring technique gave more stability and a better compression of the bone graft [12].
The need to further improve the biomechanical stability and to reduce the operation time and the risk of neurological or vascular damage, led us to choose another technique, also proposed by other authors in different versions [11, 24, 26]. Our surgical technique was performed on the following 45 patients and involved the placement of screws on the pedicles of the affected vertebra and the fixation of the loose posterior arch with a wire, taking purchase on the spinous process. This synthesis determined a dynamic compression. A bone graft was placed in the pars defect before the synthesis was tightened.
The clinical and radiological results were different depending on the technique used. We had good or excellent clinical outcome in 83.3% of patients operated with the Scott modified technique. They were completely symptom-free and practised sports without problems. These results were better than those obtained in the group of patients operated with the Scott technique (62.5%) and the Buck technique (28.5%).
In contrast, patients who were considered clinical and radiological failures and were then subsequently converted into spinal fusion, were 57% of cases with the Buck technique, 12.5% with the Scott technique and 2.7% of the Scott modified technique. The reasons that led to a new operation were pseudarthrosis and progression of slipping. All patients were symptomatic. We also observed loosening or breakage of the synthesis in five patients (1 Buck, 1 Scott, 3 Scott modified) and it was removed in three cases accusing pain.
The possibility of pseudarthrosis and mobilization of the synthesis is frequently reported [2, 18]. However, a discrepancy was often observed between clinical and radiographic results: persistence of pain in cases of repair of the isthmus radiologically documented and absence of pain in patients with nonunion [3, 20]. In our experience all cases of pseudarthrosis were symptomatic and required a fusion.
A limitation of our study is the lack of a comprehensive assessment of disability measured by the Oswestry disability index and perceived pain measured by visual analogue scale. Both are nowadays extremely important tools that researchers and disability evaluators use to measure a patient’s disability and pain. Even although they have been in use for several years [9], their widespread use is recent [10]. This is the reason why we reported only the post-operative results of the last 36 patients.
Conclusion
Isthmic repair is a helpful and easy surgical procedure in lumbar spondylolysis and spondylolisthesis. The technique avoids fusion, therefore saving the movement. The results are very good especially in young patient with slight slipping. In our experience the modified Scott technique (pedicular screws and wiring) with 83.8% of excellent or good clinical results and only 2.7% of failed surgery, seems to provide a better outcome than the Scott and Buck techniques.
Conflict of interest
None.
References
- 1.Askar Z, Wardlaw D, Koti M. Scott wiring for direct repair of lumbar spondylolysis. Spine. 2003;28(4):354–357. doi: 10.1097/01.BRS.0000048496.55167.22. [DOI] [PubMed] [Google Scholar]
- 2.Beckers L. Buck’s operation for treatment of spondylolysis and spondylolisthesis. Acta Orthop Belg. 1986;52:819–823. [PubMed] [Google Scholar]
- 3.Bonnici AV, Koka SR, Richards DJ. Results of Buck screw fusion in grade I spondylolisthesis. J R Soc Med. 1991;84:270–273. doi: 10.1177/014107689108400509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bradford DS, Iza J. Repair of the defect in spondylolysis or minimal degrees of spondylolisthesis by segmental wire fixation and bone grafting. Spine. 1985;10:673–679. doi: 10.1097/00007632-198509000-00014. [DOI] [PubMed] [Google Scholar]
- 5.Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J. Bone Jt Surg Br. 1970;52:432–437. [PubMed] [Google Scholar]
- 6.Buck JE. Further thoughts on direct repair of the defect in spondylolysis. J Bone Jt Surg Br. 1987;61:123. [Google Scholar]
- 7.David T (1996) Isthmic repair of spondylolisthesis on 80 adult patients with degenerative discs: a retrospective study with 29 months follow up. Abstract Book Eurospine 124–125
- 8.Dreyzin V, Esses SI. A comparative analysis of spondylolysis repair. Spine. 1994;19:1909–1915. doi: 10.1097/00007632-199409000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Fairbank JCT, Couper J, Davies JB. The Oswestry low back pain questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 10.Fairbank JC, Pynsent PB. The Oswestry disability index. Spine. 2000;25(22):2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 11.Gillet P, Petit M. Direct repair of spondylolysis without spondylolisthesis, using a rod–screw construct and bone grafting of the pars defect. Spine. 1999;24:1252–1256. doi: 10.1097/00007632-199906150-00014. [DOI] [PubMed] [Google Scholar]
- 12.Hambly M, Lee CK, Gutteling E, Zimmermann MC, Langrana N, Pyun Y. Tension band wiring-bone grafting for spondylolysis and spondylolisthesis. A clinical and biomechanical study. Spine. 1989;14:455–460. doi: 10.1097/00007632-198904000-00024. [DOI] [PubMed] [Google Scholar]
- 13.Ivanic GM, Pink TP, Achatz W, Ward JC, Homann NC, May M. Direct stabilization of lumbar spondylolysis with a hook screw: mean 11-year follow-up period for 113 patients. Spine. 2003;28(3):255–259. doi: 10.1097/01.BRS.0000042251.62696.A5. [DOI] [PubMed] [Google Scholar]
- 14.Johnson GV, Thompson AG. The Scott wiring technique for direct repair of lumbar spondylolysis. J. Bone Jt Surg (Br) 1992;74:426–430. doi: 10.1302/0301-620X.74B3.1587895. [DOI] [PubMed] [Google Scholar]
- 15.Kimura M. My method of filling the lesion with spongy bone in spondylolysis and spondylolisthesis. Orthop Surg. 1968;19:285–295. [PubMed] [Google Scholar]
- 16.Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolysis by bone grafting and direct stabilization by means of a hook and screw. Arch Orthop Trauma Surg. 1984;103:175–178. doi: 10.1007/BF00435550. [DOI] [PubMed] [Google Scholar]
- 17.Nicol RO, Scott JHS. Lytic spondylolysis repair by wiring. Spine. 1986;11:1027–1030. doi: 10.1097/00007632-198612000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Pedersen AK, Hagen R. Spondylolysis and spondylolisthesis treatment by internal fixation and bone grafting of the defect. J. Bone Jt Surg Am. 1988;70:15–24. [PubMed] [Google Scholar]
- 19.Roca J, Moretta D, Fuster S, Roca A. Direct repair of spondylolysis. Clin. Orthop. 1989;246:86–91. [PubMed] [Google Scholar]
- 20.Roca J, Iborra M, Cavanilles-Walker JM, Albertí G (2005) Direct repair of spondylolysis using a new pedicle screw hook fixation: clinical and CT-assessed study: an analysis of 19 patients. J Spinal Disord Tech Feb 18 Suppl:S82–S89 [DOI] [PubMed]
- 21.Salib RM, Pettine KA. Modified repair of a defect in spondylolysis or minimal spondylolisthesis by pedicle screw, segmental wire fixation, and bone grafting. Spine. 1993;18:440–443. [PubMed] [Google Scholar]
- 22.Schlenzka D, Remes V, Helenius I, Lamberg T, Tervahartiala P, Yrjönen T, Tallroth K, Osterman K, Seitsalo S, Poussa M. Direct repair for treatment of symptomatic spondylolysis and low-grade isthmic spondylolisthesis in young patients: no benefit in comparison to segmental fusion after a mean follow-up of 14.8 years. Eur Spine J. 2006;15(10):1437–1447. doi: 10.1007/s00586-006-0072-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott JHS. The Edinburgh repair of isthmic (Group II) spondylolysis. J Bone Jt Surg Br. 1987;69:491. [Google Scholar]
- 24.Songer MN, Rovin R. Repair of the pars interarticularis defect with a cable-screw construct. A preliminary report. Spine. 1998;23:263–269. doi: 10.1097/00007632-199801150-00023. [DOI] [PubMed] [Google Scholar]
- 25.Szypryt EP, Twining P, Mulholland RC, Worthington BS. The prevalence of disc degeneration associated with neural arch defects of the lumbar spine assessed by magnetic resonance imaging. Spine. 1989;14:977–981. doi: 10.1097/00007632-198909000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Tokuhashi Y, Matsuzaki H. Repair of the defects in spondylolysis by segmental pedicular screw hook fixation. Spine. 1996;21:2041–2045. doi: 10.1097/00007632-199609010-00023. [DOI] [PubMed] [Google Scholar]
- 27.Winter M, Jani L. Results of screw osteosynthesis in spondylolysis and low-grade spondylolisthesis. Arch Orthop Trauma Surg. 1989;108:96–99. doi: 10.1007/BF00932163. [DOI] [PubMed] [Google Scholar]