Abstract
From January 1, 2001 to December 31, 2003, in the Neurosurgery Department of Rome University o “Sapienza,” 167 patients underwent anterior surgery for cervical spondylodiscoarthrosis. The levels treated by the anterior stand-alone technique were: C3–C4 (11%), C4–C5 (19%), C5–C6 (40%), and C6–C7 (30%). All patients underwent left anterior presternocleidomastoid–precarotid approach, microdiscectomy, and interbody fusion using a carbon fiber cage filled with hydroxyapatite. All patients were discharged within 48 h after surgery with cervical orthosis. In one case, a hematoma of the surgical site occurred within 12 h of surgery; for this reason the patient underwent surgical revision and was discharged 4 days later. All patients have worn cervical orthosis for a mean period of 7 weeks and underwent radiological follow-up with cervical RX at 1 and 3 months after surgery. All patients underwent follow-up from 54 to 90 months after surgery, and all of them underwent cervical RX, cervical CT scans for the estimate of fusion, and evaluation of neurological status using VAS and NDI. Of 167 patients, 132 were cooperative for this study, 18 were non-cooperative, and 17 died. The estimation of fusion made by cervical CT scans with sagittal reconstruction showed complete osteointegration of the cage in 115 patients (87.1%), while it showed pseudoarthrosis in 17 patients (12.9%). In 24 patients, we observed adjacent segment degeneration, and 13 of these underwent new surgical procedures in this institute or in another hospital. Clinical evaluation with VAS and NDI showed a good outcome, with poorest benefit in patients over 60 years. The clinical analysis showed a good fusion rate in according with literature, 13% of non-fusion rate without clinical evidence and 20% of ASDegeneration but only 10% had required new surgery. We also observed that patients over 60 years of age had less satisfactory outcome, probably related with the evolution of pathophysiological degeneration of the cervical spine. In the opinion, pseudoarthrosis is caused by malpositioning of the carbon fiber cage.
Keywords: Carbon fiber cage, ACDF, Adjacent segment degeneration, Fusion
Introduction
Intervertebral disc degeneration and cervical spondylosis are the primum movens of the processes that subsequently lead to cervical spondylodiscoarthosis causing biochemical and morphological modifications of cervical spine. Degenerative changes in the cervical spine, resulting in neck pain and/or cervical myelopathy and radiculopathy are commonly observed conditions in neurosurgical practice.
Prior to 1950, cervical spine surgery was primarily performed via a posterior approach. The first ventral cervical spine stabilization with an onlay fusion was performed by Bailey and Bagley [1] in 1952. In 1955, Robinson et al. [2] described their operative technique using an interbody graft. In 1958, Cloward’s [3] modification of the anterior cervical decompression and interbody fusion (ACDF) procedure was published. Initially, ACDF was performed using the patient’s own iliac crest bone or tibia, fibula, and ribs (autograft). However, the use of autologous cancellous bone gave rise to a frequently reported complication, namely acute and chronic pain at the donor site, usually the iliac crest. Graft subsidence was also possible. In fact, graft harvesting complications occurring in traditional fusion procedures favored the ongoing development of cage technology. Carbon Fiber Cages were introduced in the early 1990s. In their study, Brantingan et al. [4, 5] demonstrated that carbon is preferable to titanium, first because it is radiolucent and, second because it also does not induce any kind of bone corrosion or inflammatory reaction.
The study described here is the first one to deal with ACDF employing carbon fiber cages with such a long follow-up (77 months, range 54–90 months) and the only one to evaluate the rate of interbody fusion using CT scan.
The purpose of this study was to demonstrate the high rate of interbody fusion and the low percentile of new adjacent level compression in patients who underwent anterior cervical fusion with carbon fiber cages containing hydroxyapatite.
Materials and methods
Between January 2001 and December 2003, 167 patients were operated in the Department of Neurological and Neurosurgical Sciences of Rome “Sapienza,” for symptomatic cervical spondylosis at one level or a single level disc herniation. We included all the patients who had undergone surgical treatment with anterior cervical discectomy and stand-alone cage interbody fusion in the study. The approach used was the left anterior retropharyngeal one; in all patients, carbon fiber cages containing hydroxyapatite were implanted without anterior plating. The level affected was: C3–C4 (10.78%), C4–C5 (19.16%), C5–C6 (40.12%), and C6–C7 (29.94%) (Table 1). Post-operatively, all patients were discharged within 48 h of operation with the exception of one who presented a hematoma of the surgical cavity 12 h after operation and required a surgical revision; he was discharged in 4 days. All patients were fitted with an orthopedic collar which they wore for 7 weeks. The mean duration of clinical follow-up was 77 months (range 54–90 months). All patients underwent serial cervical X-rays at 1 and 3 month follow-up. Cervical CT scan with sagittal reconstructed images and cervical X-rays were performed 54–90 months after treatment to evaluate complete surgical fusion. Moreover, patients underwent clinical evaluation using the Visual analogue scales (VAS) [6] and the Neck Disability Index (NDI) [7] for arm and neck pain, respectively in order to obtain a clinical picture before and after surgical treatment and at the last follow-up examination.
Table 1.
Vertebral level treated in 167 patients
| Level | No. of cases | % |
|---|---|---|
| C3–C4 | 18 | 10.78 |
| C4–C5 | 32 | 19.16 |
| C5–C6 | 67 | 40.12 |
| C6–C7 | 50 | 29.94 |
Results
Between January 2001 and December 2003, 167 patients (85 males and 82 females, mean age 56 years) underwent cervical anterior discectomy via a left retropharyngeal approach with stand-alone cage fusion. Clinical symptoms were radicular pain in 71 patients (42.5%), myelopathy in 48 patients (29.7%), and both of this in 48 patients (29.7%). During the follow-up period, 35 patients were lost (18 uncollaborative when contacted by phone and 17 deaths). The remaining 132 patients were enrolled in the study and 13 of them required a second operation at another vertebral level.
Radiological results
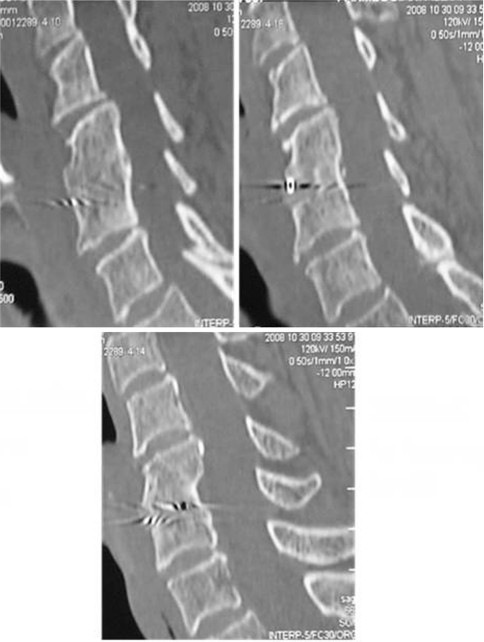
Patients were initially contacted by telephone and then given an out patient appointment, between 54 and 90 months after surgery. They were submitted to cervical X-ray and CT scan to evaluate the rate of interbody fusion (Fig. 1). CT scans demonstrated a rate of fusion of 87% (115 patients): in the remaining 13% (17 patients), it documented clinically asymptomatic pseudoarthrosis. During follow-up, 24 (20%) of the patients included in the study presented Adjacent Segment Degeneration (ASDegeneration) (Fig. 2), and 13 (10%) of these required a new surgical procedure as a result of because of ASDisease. Nine of the 13 patients presented osteophytosis and four of them presented a soft disc herniation that had already been identified prior to the first operation.
Fig. 1.
A 66-year-old woman who complained of radicular and cervical pain before surgery. She underwent C5–C6 ACDF with carbon fiber cage and is now symptom free
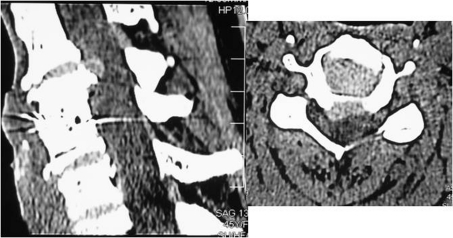
Fig. 2.
CT scan of a 45 year-old woman who underwent C3–C4 ACDF with carbon fiber cage. Before surgery, she presented myeloradiculopathy. Adjacent level degeneration can be observed on the cervical CT images. The patients is now symptom free
Clinical results
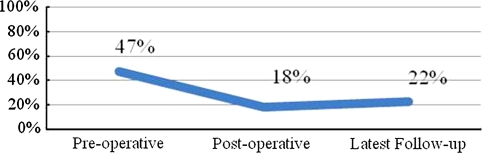
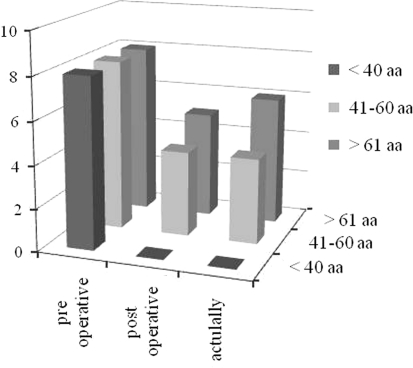
For clinical assessment of patients, two scales were employed: VAS and NDI. The VAS score for neck pain decreased significantly from 8.32 pre-operatively to 3.56 post-operatively and then slightly increased during the follow-up to 4.19 (Fig. 3). There was also a significant improvement of the NDI from 47% pre-operatively to 18% post-operatively and 22% at the latest follow-up (Fig. 4). VAS analysis compared with the age of the patients showed that patients aged over 61 presented a less satisfactory outcome, probably attributable to normal aging of pathophysiological degeneration of the cervical spine (Fig. 5).
Fig. 3.
Neck Disability Index. Evaluation of neck pain and limitation of social life before and after surgery and at latest follow-up in patient treated with ACDF with carbon cages
Fig. 4.
Visual analogue scale to evaluate arm pain
Fig. 5.
Rating of patient satisfaction based on clinical and radiological outcomes. Patients over 61 presented a less satisfactory outcome
Discussion
Anterior cervical discectomy and stand-alone cage fusion is an established surgical procedure for treating cervical disc disease. The use of ACDF for herniated discs or osteophytes was described for the first time at the end of the 1950s by Bailey and Bagdley, favored later by Robinson and Smith and then Cloward. Initially, ACDF was performed using the patient’s own iliac crest harvesting a piece of tricortical bone to replace the removed disc. In their study, Sawin et al. [8] retrospectively compared fusion rates and donor site morbidity in 300 patients submitted to autologous grafting. They found a significantly higher morbidity associated with the use of iliac crest bone, with an overall rate of 25.3%. In these patients, complication included hematoma at the site of the wound, infection, injury to the lateral cutaneous femoral nerve, and chronic pain at the donor site [9]. Moreover, complications at the implantation site are possible, such as displacement, breakage, resorption, or subsidence. In order to avoid co-morbidity from the donor site, other devices became more popular, such as prosthese and cages (titanium, peek, and carbon).
Carbon fiber systems were introduced at the beginning of the 1990s. As shown by Brantingan et al., carbon is preferable to titanium because it is radiolucent (allowing an easier evaluation of bone fusion in the follow-up with X-ray films) and also because it does not induce any kind of bone corrosive or inflammatory reaction at the bone. Moreover, in their retrospective study Frati et al. [10] pointed out the advantages offered by the high elasticity of carbon fiber implants, that redistributes load-sharing to the bone graft inside the implant, thus improving the quality of fusion and reducing stress on the adjacent vertebral level. To increase fusion rates and decrease graft complications, some investigators supplement allograft fusion with an anterior cervical plate, a technique initially described by Bohler and Gaudernak [11] and Caspar [12], for treating cervical trauma. In a meta-analysis of fusion rate’s Fraser et al. [13] observed that for a single disc-level disease, the fusion rates achieved were 84.99% using ACD, 92.1% using ACDF, and 97.1% using ACDF with anterior plating. In the study, an 87% fusion rate was found after ACDF using carbon cages without plating. In the light of these results, the use of anterior plating does not appear to be beneficial when one level is treated, since plating is more costly, requires longer operative times, and may be associated with problems such as breakage or dislocation of the screws and perforation of adjacent structures. Furthermore, other issues, such as how the plate system affects the risk of adjacent segment morbidity, remain unaddressed.
One important and well-documented limit of ACDF is the increased stress exerted on the vertebral adjacent to the level of cervical arthrodesis that leads to more rapid degeneration and altered biomechanics. In a retrospective study of 106 patients with cervical spondylotic myeloradiculopathy at an average of 8.5 years after ACDF, Baba et al. [14] observed that 25% of these patients subsequently developed a new disc herniation above the previously fused segments. Hilibrand et al. [15] performed the most referenced study on adjacent segment disease, in which where they demonstrated that symptomatic adjacent segment disease may affect more than one fourth of all patients up to 10 years after an anterior cervical arthrodesis. They also found a reduced rate of adjacent segment disease in patients submitted to multilevel fusion compared to single level arthrodesis. Very recently, Sugawara et al. [16] have published a retrospective study of 41 patients who underwent ACDF with titanium cages with a 5-year follow-up period. These authors, in the light of the good clinical outcome obtained, support the idea that ADD is the consequence of natural degeneration of the discs. Mccormick [17], in an editorial, emphasizes that the central question regards not only the incidence of adjacent segment disease but also its cause, in an attempt to understand to what degree the occurrence of adjacent segment disease is directly attributable to a previously performed fusion compared with the natural history of cervical disc degeneration. The results of the study have demonstrated that adjacent segment disease is not clinically relevant. The patients were studied by CT scan with sagittal reconstructed images that made possible to evaluate the rate of bone fusion. During follow-up, 24 (20%) of the patients included in the study presented ASDegeneration, and 13 (10%) of these required a new surgical procedure as a result of because of ASDisease. 9 of the 13 patients already presented osteophytosis and four of them presented soft disc herniation prior to the first operation, justifying the assertion that ADdisease is probably a consequence of a natural degeneration of vertebral spine and 11 (45%) of the 24 patients with ASDegeneration already had signs of degeneration on the adjacent levels seen on the pre-operative CT/RMN images. This finding supports the hypothesis of a pathophysiological degeneration of cervical spine by reducing the impact of fusion on adjacent levels in the experience. Moreover, the less satisfactory outcome observed in patients over 61, with development of ASdisease, was probably related to the evolution of pathophysiological degeneration of the cervical spine.
The experience with carbon fiber cages suggests that these devices represent a valid option for restoring the intervertebral disc space and promoting arthrodesis in cervical disc surgery while their elastic properties minimize the risk of kyphosis, subsidence, and adjacent level disease.
Finally, in the 13% of the patients in whom non-fusion was documented by CT scan, this was not correlated to clinical symptoms. In the opinion, pseudoarthrosis is mainly caused by malpositioning of a carbon fiber cage that often rests on the anterior rim of the endplate.
Conclusions
The study demonstrated that the use of carbon fiber cages containing hydroxyapatite is apparently a safe procedure with a favorable clinical and radiological outcome. The simplicity of the technique and its radiolucency is an advantage during follow-up. In this study, a good fusion rate (87%) was achieved in accordance with the literature using carbon fiber cages. The non-fusion rate was 13%. 20% of patients with ASDegeneration did not show clinical evidence and while 10% required a second operation. Patients over 61 had a less satisfactory outcome, probably attributable to ongoing pathophysiological degeneration of the cervical spine.
Acknowledgments
Conflict of interest None.
References
- 1.Bailey RW, Badgeley MD. Stabilization of the cervical spine by anterior fusion. J Bone Joint Surg (Am) 1960;42-A(4):565–594. [PubMed] [Google Scholar]
- 2.Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull Johns Hopkins Hosp. 1995;96:223–224. [Google Scholar]
- 3.Cloward RB. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 4.Brantingan J, Steffee A, Geiger J. A carbon fiber implant to aid interbody fusion. Mechanical testing. Spine. 1991;16(S6):277–282. doi: 10.1097/00007632-199106001-00020. [DOI] [PubMed] [Google Scholar]
- 5.Brantingan J. The use of carbon fiber implant in reconstructing anterior spinal column defects. Orthop Trans. 1992;16:139–140. [Google Scholar]
- 6.Huskisson EC. Measurement of pain. Lancet. 1974;2(7889):1127–1131. doi: 10.1016/S0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 7.Vernon H, Mior S. The Neck disability index: a study of reliability and validity. J Manip Physiol Ther. 1991;14(7):409–415. [PubMed] [Google Scholar]
- 8.Sawin PD, Traynelis VC, Menezes AH. A comparative analysis of fusion rates and donor-site morbidity of autogenic rib and iliac crest bone grafts in posterior cervical fusions. J Neurosurg. 1998;88:255–265. doi: 10.3171/jns.1998.88.2.0255. [DOI] [PubMed] [Google Scholar]
- 9.Younger EM, Chapman MW. Morbidity at bone graft sites. J Orthop Trauma. 1989;3:192–195. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Tancredi A, Agrillo A, Delfini R, Fiume D, Frati A, Rinaldi A. Use of carbon fiber cages for treatment of cervical myeloradiculopathies. Surg Neurol. 2004;61:221–226. doi: 10.1016/j.surneu.2003.07.014. [DOI] [PubMed] [Google Scholar]
- 11.Bohler J, Gaudernak T. Anterior plate stabilization for fracture dislocation of the lower cervical spine. J Trauma. 1980;20:203–205. doi: 10.1097/00005373-198003000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurg. 1989;25:491–502. doi: 10.1227/00006123-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Fraser JF, et al. Anterior approaches to fusion of the cervical spine: a metaanalysis of fusion rates. Neurosurg Spine. 2007;6:298–303. doi: 10.3171/spi.2007.6.4.2. [DOI] [PubMed] [Google Scholar]
- 14.Baba H, Furusawa N, Imura S, et al. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine. 1993;18:2167–2173. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg (Am) 1999;84:519–528. doi: 10.2106/00004623-199904000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Sagawara T, Itoh Y, Hirano Y, Mizoi K. Long term out come and adjacent disc degeneration after anterior cervical discectomy and fusion with titanium cylindrical cages. Acta Neurochir. 2009;151:303–309. doi: 10.1007/s00701-009-0217-5. [DOI] [PubMed] [Google Scholar]
- 17.McCormick PC. The adjacent segment. J Neurosurg Spine. 2007;6:1–4. doi: 10.3171/spi.2007.6.1.1. [DOI] [PubMed] [Google Scholar]