Abstract
Purpose
The aim of this study was to analyze the short-term predictability and reliability of Astra Tech implants according to the demographical distribution of patients and condition of implant sites and location of implants.
Methods
Among patients treated with Astra Tech implant (Astra Tech AB) in the Department of Periodontology at the Dental Hospital of Yonsei University of College of Dentisry and K Dental Clinic from May 2004 to March 2009, 195 implants in 98 patients which had been restored more than 6 months ago were reviewed in this study. Following data were reviewed from patient charts and implants success rate was examined: 1) patient type and implant location, 2) bone status at the implant site, 3) diameter and length of the placed implants, 4) presence or absence of bone augmentation and types of the augmentation.
Results
The results from this study are as follows: 1) most implants were placed in the molar area, especially 1st molar area of maxilla, 2) most implants were placed at D2 and D3 bone type, 3) most implants were placed in areas of B and C bone quantity, 4) autogenous and alloplastic bone graft and artificial membrane were used for placement of 74 implants.
Conclusions
Short-term survival rate of Astra Tech implants was 100%.
Keywords: Dental implantation, Humans, Retrospective studies, Survival rate
INTRODUCTION
In 1981 Albrektsson et al. [1] emphasized the bio-compatibility, morphology, surface treatment, condition of recipient site, surgical technique, and control of loading condition as key factors of successful osseointegration in dental implants. They also reported other factors needed for successful implant therapy such as patient selection, experience of the surgeon, initial stability of the implant, placement timing, esthetics, and responsiveness to the grafting material [2-5]. Clinically, obtaining sufficient initial stability is crucial. This depends on the bone density of the surgical site, the surgical method, and the microscopic surface characteristics and macroscopic morphology of the implants [6].
Among various factors in predicting the success of implant therapy, factors determined by the patient are the volume and density of available bone [7,8]. The atrophy of available bone after extraction limits the length and diameter of the implant. Initial stability is weakened by decreased bone density, which in turn affects implant success. Many previous studies have shown that placement of short implants due to severe bone loss at the implant site resulted in an increased failure rate. Bone density is usually decreased after tooth loss and this also has an effect on implant success [9-12].
Assuming an acceptable level of surgeon's experience and patient's bone quality, reliable implants will result in a more predictable outcome. Therefore, the success rate of implants in the implant system is considered a measure of reliability. Since Schnitman and Shulman [13] proposed success criteria for implants, several criteria have been proposed [14,15], and the report by Albrektsson et al. [16] is most widely used.
However, recent studies have been conducted on implants with immediate placement or early-loading protocols. It is difficult to compare the two types of studies in analyzing their survival or success rates. Carr et al. [17] reviewed 674 1-stage implants with a 78-month follow-up period. In this retrospective study, the implant survival rate was determined by means of Kaplan-Meier survival estimates. No failures were noted 13 months after placement. Penarrocha et al. [18] reported a 1-year survival rate for a single implant with early loading within 6-8 weeks after placement. Buser's survival criteria [15] and the Kaplan-Meier survival estimates were used to compare these results with the survival rates of other implants with early loading. Many studies have considered 1 year after implant placement to be a critical point because the Kaplan-Meier survival curve almost reaches a plateau 1 year after the implant placement. Performance of bone augmentation did not affect the implant success rate or the amount of marginal bone loss [19-21].
Until recently, various implant systems have been introduced to increase the success rate and research on implant design and surface treatment has been actively performed [22,23]. Many studies have revealed that the success rate is higher in rough-surfaced implants by various surface treatments than in smooth-surfaced implants by machining [24,25]. Regarding the morphology of the implants, the initial stability was enhanced by self-tapping implants and the success rate was also increased [26,27].
The Astra Tech implants reviewed in this study have a microthreaded conical neck and TiO blast surface (Fig. 1) [28]. Microthreads on the fixture top prevent concentration of the stress around the alveolar ridge crest and decrease marginal bone loss [29]. The fixture and abutment are strongly connected at an 11.5 degree angle by the conical seal design. The conical design seals off the connection and decreases micro-movement and micro-leakage [30,31]. In 1998 Norton documented a statistically significant decrease in the bone loss around Astra Tech implants after 4 years of radiographic assessment. Palmer et al. [32] found an average 0.39 mm bone loss in a 5-year prospective study in 2000. Shin et al. [33] documented a smaller degree of bone loss in implants with microthreading regardless of bone quality in a 1-year prospective comparative study in 2003. A statistically significant difference was found, especially in the maxilla.
Figure 1.
Astra Tech Implant.
The aim of this study was to analyze the short-term predictability and reliability of Astra Tech implants according to the demographical distribution of patients and condition of implant sites and location of implants.
MATERIALS AND METHODS
Subjects and materials
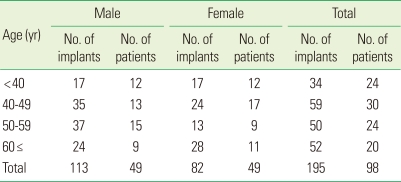
Among patients treated with Astra Tech implants in the Department of Periodontology at the Dental Hospital of Yonsei University of College of Dentisry and K Dental Clinic from May 2004 to March 2009, 195 implants in 98 patients which had been restored more than 6 months earlier were reviewed in this study (Table 1).
Table 1.
Distribution according to patients' age and sex.
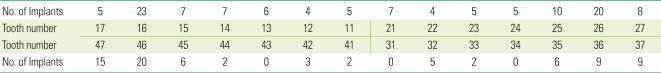
The intraoral locations of the Astra Tech implants are as shown in Table 2.
Table 2.
Implant location distribution.
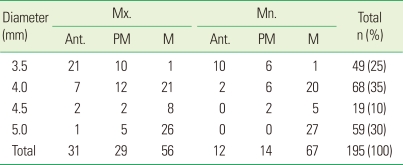
The diameters of Astra Tech implants were 3.5 mm, 4.0 mm, 4.5 mm, and 5.0 mm. The lengths of the implants varied widely, and ranged from 8 mm to 13 mm (Tables 3 and 4).
Table 3.
Distribution of implant length.
Mx: Maxilla, Mn: Mandible, Ant: Anterior, PM: Premolar, M: Molar.
Table 4.
Distribution of implant diameter.
Mx: Maxilla, Mn: Mandible, Ant: Anterior, PM: Premolar, M: Molar.
This study was approved by the Institutional Review Board of Dental Hospital of Yonsei University of College of Dentistry (IRB number 2-2011-0014).
Methods
The following data were reviewed from patient charts: 1) patient type and implant location, 2) bone status at the implant site, 3) diameter and length of the placed implants, 4) presence or absence of bone augmentation and types of the augmentation. The implant success rate was then examined in light of these variables.
Before implant placement, every patient went through oral and radiographic examinations. A medical history was also taken and smoking habits were reviewed. Implants were not placed in patients with an absolute contraindication that could not be controlled. In those patients, the edentulous areas were given an alternative treatment. Patients were also interviewed about the cause and timing of the extraction to determine the types of tooth loss by age and sex.
The bone status at the implant site was documented according to Lekholm and Zarb's classification [11]. Bone quality and bone quantity was evaluated during surgery. The diameter and length of the implants placed were reviewed from the patient charts.
Using the patient charts, the surgical procedures (1-stage or 2-stage implant placement procedure), additional bone augmentation procedures, and graft materials (such as bone or artificial membrane) were reviewed. The time until completion of prosthodontic treatment after implant installation was also investigated. In addition, the follow-up data (including patient interviews and oral and radiographic examinations) older than 6 months after prosthodontic treatment were evaluated.
Assessment method
The survival criteria were based on those proposed by Buser et al. in 1997 and by Cochran et al. in 2002. The criteria includes: 1) the absence of clinical mobility of the implants, 2) the absence of subjective sensitivity or pain, 3) the absence of peri-implantitis, and 4) the absence of persistent radiolucency around the implants.
RESULTS
One hundred and ninety-five implants were evaluated in this study. Regarding implant length, 11 mm was the most common (47%). With respect to the diameter of implants, 4 mm occupied the largest portion (35%), followed by 5.0 mm (30%), 3.5 mm (25%), and 4.5 mm (10%). This is because implant diameter is restricted by the bucco-lingual width of the available bone and the relationship with adjacent teeth [9,34].
Fifty-five implants (28%) were applied using a 1-stage implant placement procedure, and the other 140 implants (72%) using a 2-stage procedure. Also, for 74 implants in surgical sites with poor bone quality or quantity an additional bone augmentation procedure, such as sinus augmentation or the guided bone regeneration procedure, was used. Prosthodontic treatment was completed by 2 to 20 months after implant installation with a mean of 5.9 months.
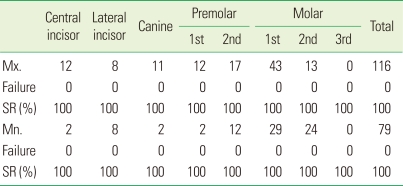
Survival rate according to implant location
Most implants were placed in the molar area, especially the 1st molar area of the maxilla, and there was no difference in the survival rate according to the implant location (Table 5).
Table 5.
Survival rate (SR) of implants according to location.
Mx: Maxilla, Mn: Mandible.
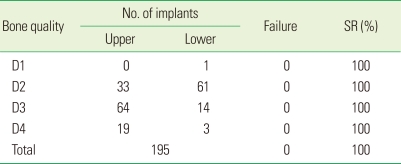
Survival rate according to bone quality
Most implants were placed in D2 and D3 bone types, and there was no difference in survival rate according to bone quality (Table 6).
Table 6.
Survival rate (SR) of implants according to bone quality.
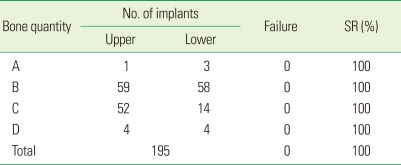
Survival rate according to bone quantity
Most implants were placed in areas of B and C bone quantity, and there was no difference in survival rate according to bone quantity (Table 7).
Table 7.
Survival rate (SR) of implants according to bone quantity.
Survival rate according to the presence or absence of bone augmentation procedure
An autogenous bone graft, allograft, or alloplast with artificial membrane were used for placement of 74 implants. Maxillary sinus elevation procedures were performed for the placement of 33 implants in the maxillary posterior region. Nevertheless, there was no difference in the survival rate (Table 8).
Table 8.
Number of advanced techniques on the recipient site.
SR: Survival rate, GBR: guided bone regeneration.
a)MBCP (Biomatlante, Vigneux de Bretagne, France). b)GTAM (Gore-Tex Augmentation Material membrane; WL Gore, Flagstaff, AZ, USA). c)CollaTape (Zimmer Dental, Carlsbad, CA, USA). d)Osteon (Dentium, Suwon, Korea). e)OraGraft (LifeNet Health Inc., Virginia Beach, VA, USA). f)BioGide (porcine type I and III collagen; Geistlich Biomaterials, Wolhusen, Switzerland).
DISCUSSION
Since the introduction of the concept of osseointegration by Branemark in the early 1960s, implant therapy has been a commonplace for replacing edentulous areas in daily practice. Up to now, implants with various shapes, designs, and surface treatments have been introduced. In the Department of Periodontolgy at the Dental Hospital of Yonsei University of College of Dentisry, 4,500 implants were placed for approximately 10 years from 1992 to 2002, and based on these patient records, basic assessments have been undertaken regarding patient type and distribution of implant location [35]. Among various implant systems, the microthreaded and conical seal design of the Astra Tech implant has shown lower marginal bone loss around implants, as well as less microleakage and micromovement [28-33,36], thus increasing the long term success rate.
In this study, 195 Astra Tech implants were placed in 98 patients in the Department of Periodontolgy at the Dental Hospital of Yonsei University of College of Dentisry and in K Dental Clinic. Based on these data, the short-term survival rate of Astra Tech implants was evaluated by considering bone quality, bone quantity, and bone augmentation procedures.
In 1985, Brånemark et al. [8] classified the bone status around the implant surgery area. This has been used by many clinicians to predict treatment outcomes. In this study, the bone quality and bone quantity were separately evaluated. With respect to bone quality, the predominant bone type was D3 in the maxilla and D2 in the mandible. With regard to bone quantity, type B and C occupied most cases (96%) of the maxilla and type B was predominant in the mandible (73%). We often encounter situations where the bone quantity is deficient in an edentulous area. To place implants with sufficient length and diameter in these areas, a bone graft with autogenous bone or alloplastic material with or without a membrane are required. Additional procedures are also necessary, especially in the maxilla, such as in maxillary sinus elevation. Currently, the development of these procedures has contributed to a high success rate of implants, and implants can be placed in more challenging cases [37].
In 1997, Kemppainen et al. [38] reported that the short-term survival rate of Astra Tech implants is 97.8%, and in 2004, Norton [39] reported that it is 96.4%. In this study, the short-term survival rate was 100% regardless of bone quality, bone quantity, or use of bone augmentation procedures. These high short-term survival rates are due to the distinctive fixture design of the Astra Tech implant, which results in excellent initial bone responses. Therefore, the use of an Astra Tech implant can result in predictably good treatment results even if the bone quality is poor and bone augmentation is necessary because of poor bone quantity.
The patient type, distribution of implant locations, and survival rate of Astra Tech implants were investigated in this study and following was concluded:
1. The short-term survival rate of Astra Tech implants was 100%.
2. Bone quality was in the decreasing order of D3 (55%) >D2 (28%) >D4 (16%) >D1 (0%) for the maxilla and D2 (77%) >D3 (18%) >D4 (4%) >D1 (1%) for the mandible with a 100% survival rate.
3. Bone quantity was in the decreasing order of Type B (51%) >C (49%) >D (3%) >A (1%) for the maxilla and Type B (73%) >C (18%) >D (5%) >A (4%) for the mandible with a 100% survival rate.
4. Bone augmentation was carried out in 38% of implants placed, with 100% survival rate.
Considering the consistent outcomes mentioned above, Astra Tech implants can be reliably used in daily practice. If additional bone augmentation procedures are performed to improve the bone quality and quantity in areas where the bone condition is not optimal, acceptable treatment results can be expected.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Albrektsson T, Brånemark PI, Hansson HA, Lindström J. Osseointegrated titanium implants. Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand. 1981;52:155–170. doi: 10.3109/17453678108991776. [DOI] [PubMed] [Google Scholar]
- 2.Baier RE, Meenaghan MA, Hartman LC, Wirth JE, Flynn HE, Meyer AE, et al. Implant surface characteristics and tissue interaction. J Oral Implantol. 1988;13:594–606. [PubMed] [Google Scholar]
- 3.Smith DC. Future directions for research on materials and design of dental implants. J Dent Educ. 1988;52:815–820. [PubMed] [Google Scholar]
- 4.Chiarenza AR. Retrospective observations on the influence of bone type in determining the nature of bone implant interface. Int J Oral Implantol. 1989;6:43–48. [PubMed] [Google Scholar]
- 5.Tatum OH, Jr, Lebowitz MS. Anatomic considerations for dental implants. J Oral Implantol. 1991;17:16–21. [PubMed] [Google Scholar]
- 6.Martinez H, Davarpanah M, Missika P, Celletti R, Lazzara R. Optimal implant stabilization in low density bone. Clin Oral Implants Res. 2001;12:423–432. doi: 10.1034/j.1600-0501.2001.120501.x. [DOI] [PubMed] [Google Scholar]
- 7.Atwood DA. Postextraction changes in the adult mandible as illustrated by microradiographs of midsagittal sections and serial cephalometric roentgenograms. J Prosthet Dent. 1963;13:810–824. [Google Scholar]
- 8.Brånemark PI, Zarb GA, Albrektsson T. Tissue integrated prostheses: osseointegration in clinical dentistry. Chicago: Quintensence; 1985. pp. 199–209. [Google Scholar]
- 9.Collaert B, De Bruyn H. Comparison of Brånemark fixture integration and short-term survival using one-stage or two-stage surgery in completely and partially edentulous mandibles. Clin Oral Implants Res. 1998;9:131–135. doi: 10.1034/j.1600-0501.1998.090209.x. [DOI] [PubMed] [Google Scholar]
- 10.Cochran DL, Buser D, ten Bruggenkate CM, Weingart D, Taylor TM, Bernard JP, et al. The use of reduced healing times on ITI implants with a sandblasted and acid-etched (SLA) surface: early results from clinical trials on ITI SLA implants. Clin Oral Implants Res. 2002;13:144–153. doi: 10.1034/j.1600-0501.2002.130204.x. [DOI] [PubMed] [Google Scholar]
- 11.Lekholm U, Gröndahl K, Jemt T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin Implant Dent Relat Res. 2006;8:178–186. doi: 10.1111/j.1708-8208.2006.00019.x. [DOI] [PubMed] [Google Scholar]
- 12.Misch CE, Misch-Dietsh F, Silc J, Barboza E, Cianciola LJ, Kazor C. Posterior implant single-tooth replacement and status of adjacent teeth during a 10-year period: a retrospective report. J Periodontol. 2008;79:2378–2382. doi: 10.1902/jop.2008.080188. [DOI] [PubMed] [Google Scholar]
- 13.Schnitman PA, Shulman LB. Recommendations of the consensus development conference on dental implants. J Am Dent Assoc. 1979;98:373–377. doi: 10.14219/jada.archive.1979.0052. [DOI] [PubMed] [Google Scholar]
- 14.Smith DE, Zarb GA. Criteria for success of osseointegrated endosseous implants. J Prosthet Dent. 1989;62:567–572. doi: 10.1016/0022-3913(89)90081-4. [DOI] [PubMed] [Google Scholar]
- 15.Buser D, Weber HP, Lang NP. Tissue integration of non-submerged implants. 1-year results of a prospective study with 100 ITI hollow-cylinder and hollow-screw implants. Clin Oral Implants Res. 1990;1:33–40. doi: 10.1034/j.1600-0501.1990.010105.x. [DOI] [PubMed] [Google Scholar]
- 16.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 17.Carr AB, Choi YG, Eckert SE, Desjardins RP. Retrospective cohort study of the clinical performance of 1-stage dental implants. Int J Oral Maxillofac Implants. 2003;18:399–405. [PubMed] [Google Scholar]
- 18.Penarrocha M, Carrillo C, Boronat A, Martí E. Early loading of 642 Defcon implants: 1-year follow-up. J Oral Maxillofac Surg. 2007;65:2317–2320. doi: 10.1016/j.joms.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 19.Schliephake H, Neukam FW, Wichmann M. Survival analysis of endosseous implants in bone grafts used for the treatment of severe alveolar ridge atrophy. J Oral Maxillofac Surg. 1997;55:1227–1233. doi: 10.1016/s0278-2391(97)90173-7. [DOI] [PubMed] [Google Scholar]
- 20.Becktor JP, Isaksson S, Sennerby L. Survival analysis of endosseous implants in grafted and nongrafted edentulous maxillae. Int J Oral Maxillofac Implants. 2004;19:107–115. [PubMed] [Google Scholar]
- 21.Finne K, Rompen E, Toljanic J. Clinical evaluation of a prospective multicenter study on 1-piece implants. part 1: marginal bone level evaluation after 1 year of follow-up. Int J Oral Maxillofac Implants. 2007;22:226–234. [PubMed] [Google Scholar]
- 22.van Steenberghe D, De Mars G, Quirynen M, Jacobs R, Naert I. A prospective split-mouth comparative study of two screw-shaped self-tapping pure titanium implant systems. Clin Oral Implants Res. 2000;11:202–209. doi: 10.1034/j.1600-0501.2000.011003202.x. [DOI] [PubMed] [Google Scholar]
- 23.Cochran DL. A comparison of endosseous dental implant surfaces. J Periodontol. 1999;70:1523–1539. doi: 10.1902/jop.1999.70.12.1523. [DOI] [PubMed] [Google Scholar]
- 24.Li DH, Liu BL, Zou JC, Xu KW. Improvement of osseointegration of titanium dental implants by a modified sandblasting surface treatment: an in vivo interfacial biomechanics study. Implant Dent. 1999;8:289–294. doi: 10.1097/00008505-199903000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Botticelli D, Berglundh T, Persson LG, Lindhe J. Bone regeneration at implants with turned or rough surfaces in self-contained defects. An experimental study in the dog. J Clin Periodontol. 2005;32:448–455. doi: 10.1111/j.1600-051X.2005.00693.x. [DOI] [PubMed] [Google Scholar]
- 26.Rosenlicht JL. SwissPlus Implant System, part 1: surgical aspects and intersystem comparisons. Implant Dent. 2002;11:144–153. doi: 10.1097/00008505-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 27.Davarpanah M, Martinez H, Etienne D, Zabalegui I, Mattout P, Chiche F, et al. A prospective multicenter evaluation of 1,583 3i implants: 1- to 5-year data. Int J Oral Maxillofac Implants. 2002;17:820–828. [PubMed] [Google Scholar]
- 28.Palmer RM, Smith BJ, Palmer PJ, Floyd PD. A prospective study of Astra single tooth implants. Clin Oral Implants Res. 1997;8:173–179. doi: 10.1034/j.1600-0501.1997.080303.x. [DOI] [PubMed] [Google Scholar]
- 29.Lee DW, Choi YS, Park KH, Kim CS, Moon IS. Effect of microthread on the maintenance of marginal bone level: a 3-year prospective study. Clin Oral Implants Res. 2007;18:465–470. doi: 10.1111/j.1600-0501.2007.01302.x. [DOI] [PubMed] [Google Scholar]
- 30.Norton MR. Assessment of cold welding properties of the internal conical interface of two commercially available implant systems. J Prosthet Dent. 1999;81:159–166. doi: 10.1016/s0022-3913(99)70243-x. [DOI] [PubMed] [Google Scholar]
- 31.Harder S, Dimaczek B, Açil Y, Terheyden H, Freitag-Wolf S, Kern M. Molecular leakage at implant-abutment connection--in vitro investigation of tightness of internal conical implant-abutment connections against endotoxin penetration. Clin Oral Investig. 2010;14:427–432. doi: 10.1007/s00784-009-0317-x. [DOI] [PubMed] [Google Scholar]
- 32.Palmer RM, Palmer PJ, Smith BJ. A 5-year prospective study of Astra single tooth implants. Clin Oral Implants Res. 2000;11:179–182. doi: 10.1111/j.1600-0501.2000.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 33.Shin DH, Cho KS, Park KH, Moon IS. An 1 year prospective comparative study evaluating the effect of microthread on the maintenance of marginal bone level. J Korean Acad Periodontol. 2003;33:349–358. [Google Scholar]
- 34.Yoo HS, So SS, Han DH, Cho KS, Moon IS. The comparison between 2 wide implants and 3 regular implants in mandibular posterior area. J Korean Acad Periodontol. 2002;32:577–588. [Google Scholar]
- 35.Hong SJ, Paik JW, Kim CS, Choi SH, Lee KW, Chai JK, et al. The study of implant patient's type and implant distribution. J Korean Acad Periodontol. 2002;32:539–554. [Google Scholar]
- 36.Hansson S, Norton M. The relation between surface roughness and interfacial shear strength for bone-anchored implants. A mathematical model. J Biomech. 1999;32:829–836. doi: 10.1016/s0021-9290(99)00058-5. [DOI] [PubMed] [Google Scholar]
- 37.Buser D, Brägger U, Lang NP, Nyman S. Regeneration and enlargement of jaw bone using guided tissue regeneration. Clin Oral Implants Res. 1990;1:22–32. doi: 10.1034/j.1600-0501.1990.010104.x. [DOI] [PubMed] [Google Scholar]
- 38.Kemppainen P, Eskola S, Ylipaavalniemi P. A comparative prospective clinical study of two single-tooth implants: a preliminary report of 102 implants. J Prosthet Dent. 1997;77:382–387. doi: 10.1016/s0022-3913(97)70163-x. [DOI] [PubMed] [Google Scholar]
- 39.Norton MR. A short-term clinical evaluation of immediately restored maxillary TiOblast single-tooth implants. Int J Oral Maxillofac Implants. 2004;19:274–281. [PubMed] [Google Scholar]