Abstract
After the surgical procedure of tonsillectomy, hemorrhage ranks among its serious postoperative complications. In this systematic review, we analyze hemorrhage following tonsillectomies performed using the coblation technique. 24 prospective, randomized, and controlled studies were included in the meta-analysis. Data of 796 patients who had undergone coblation tonsillectomy were analyzed. Hemorrhages occurred in 33 patients: 2 classified as primary and 26 as secondary hemorrhages. 5 could not be classified into either group. Overall, the total hemorrhage rate for the coblation procedure was 4.1% with a 95% confidence interval from 2.8 to 5.5%. The overall hemorrhage rate of 4.1% found in this meta-analysis shows that coblation is a safe and effective technique for tonsillectomies with a secondary bleeding rate similar to what is reported for comparable techniques such as bipolar diathermia.
Keywords: Tonsillectomy, Hemorrhage, Coblation, Radiofrequency-based plasma dissection, Complication
Introduction
According to recent statistics presented by German university hospitals, approximately every 25th patient undergoing a tonsillectomy in these hospitals providing maximal medical care must reckon with postoperative hemorrhage (requiring reoperation) (from 1.0 to 9.7%, median 3.8%) [1]. The German Federal Office for Quality Assurance [Bundesgeschäftsstelle für Qualitätssicherung (BQS)] reported a hemorrhage rate of 4.7% for all hospitals in 2003 [2]. Reports of fatal complications go through the press time and again, making both patients and surgeons feel insecure [3]. Also, postoperative pain compromises the patient’s recovery since the adequate intake of food and drink can often not be ensured, especially in children [4, 5]. This situation has led to the development of reportedly “gentler” surgical methods such as that of coblation, also called radiofrequency-based plasma dissection [6]. Contrary to initially publicized euphoria, a Cochrane analysis of morbidity was unable to establish clear positive evidence toward lower peri-operative and postoperative stress on the patient caused by pain and blood loss [7]. In contrast, the focus has recently turned to the frequency of hemorrhages following coblation tonsillectomies. This systematic review will not elaborate on the coblation procedure itself, as comprehensive reports can be found in the literature [8]. Instead, a meta-analysis is to resolve the conflict between the widely differing data on hemorrhage rates in the literature [9]. A reliable assessment of the risk for postoperative hemorrhage would provide valuable support to both patients and surgeons. Even in a systematic review by the National Institute for Health and Clinical Excellence (NICE), contradictory results were found in terms of the incidences of secondary hemorrhages requiring reoperation for the various tonsillectomy procedures [10]. The report expressed a high degree of uncertainty about this assertion due to the low number of secondary hemorrhages at an average of less than 1% of all operations. For coblation, a lower rate was determined in comparison to the bipolar dissection and hemostasis method across all studies examined. The purpose of the analysis described below is to give a solid estimate of the risk of hemorrhage following coblation tonsillectomy based on all prospective, randomized, controlled studies published to date.
Materials and methods
The objective of this systematic review with a meta-analysis was to collect and evaluate data on the hemorrhage rate after tonsillectomies using the coblation procedure. For this purpose, data were gathered from available publications on randomized, controlled, prospective studies: hemorrhages following tonsillectomy were divided into primary hemorrhages, which occurred within 24 h following surgery, and secondary hemorrhages, which appeared after 24 h, but especially between the 5th and 10th day after surgery [9]. The hemorrhage rate was recorded as a total result for the analysis and, if specified, classified as primary or secondary hemorrhage. Studies were taken into consideration only if they reported the hemorrhage rate after tonsillectomy using the coblation method. In order to answer the question posed by the meta-analysis in a systematic manner, an overview of the literature available on this topic was compiled. The criteria and set of topics were defined for conducting the systematic analysis of the question at hand. The search terms were determined with these aspects in mind. The terms were combined with one another, and the identified literature was gathered. The keywords were: electrocoagulation/*methods, tonsillectomy, hemorrhage, coblation, cold ablation, plasma dissection, Arthrocare, tonsillotomy coblation technology, tonsillectomy/*methods, electrosurgery/*methods, electrosurgery, tonsillectomy/instrumentation*, postoperative complications/epidemiology*, tonsillectomy/*instruments (Table 1). Data found concerning the research term “tonsillotomy” was not evaluated as relevant by the reviewers and excluded in this meta-analysis since tonsillotomy has a different indication than tonsillectomy and, thus the hemorrhage rates are not comparable.
Table 1.
Literature quest
| Key words and term combinations for literature search |
|---|
| Tonsillectomy/*methods AND Coblation |
| Tonsillectomy/instrumentation* AND Postoperative Complications/epidemiology* |
| Electrosurgery/*methods AND tonsillectomy/*methods |
| Surgical Instruments/trends* AND tonsillectomy |
| Tonsillectomy/*instruments AND Coblation |
| Electrocoagulation/*methods AND tonsillectomy AND hemorrhage |
| Electrosurgery AND tonsillectomy AND hemorrhage |
| (Coblation OR coblation technology OR coblation laser therapy OR cold ablation OR Arthrocare OR tongue coblation) and (tonsillectomy OR tonsillotomy OR tonsillectomy methods OR adenoidectomy) and (hemorrhage OR haemorrhage OR bleeding OR blood loss OR bleeding frequency OR bleeding rate OR bleeding risk OR hemorrhage frequency) |
| (Coblation OR cold ablation OR Arthrocare) AND (Tonsillectomy OR Tonsillotomy) AND Hemorrhage |
| Coblation AND Tonsillectomy |
| Coblation AND Tonsillectomy AND Hemorrhage |
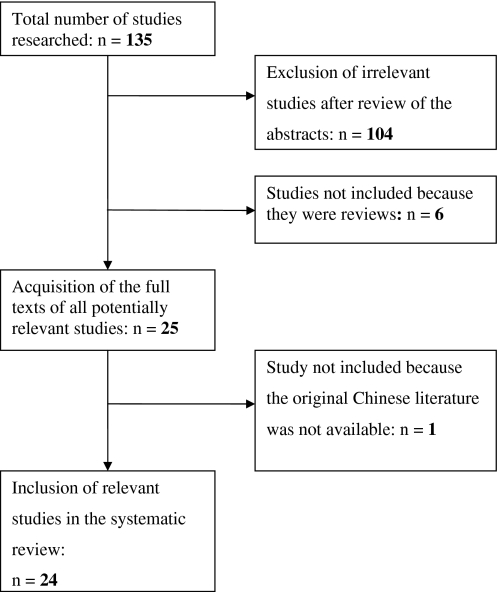
The systematic review of the literature was carried out using the following electronic databases: Medline; Embase; HTA; NHS EED database; NLCM (National Library of Medicine); Scirus; ISI web of Knowledge and Science, and the user interface Pubmed. We also searched for assessments on the following website: NHS Institute for Health and Clinical Excellence (http://guidance.nice.org.uk/). The literature gathered in the search was then evaluated and data were extracted. Three independent reviewers evaluated the abstracts (R.M., S.A., K.A.). Figure 1 shows the inclusion and exclusion of the references during the review process. After two independent reviewers had extracted the data from the included studies, the data were analyzed by means of a statistical procedure.
Fig. 1.
Study inclusions and exclusions during the review process
Statistical methods
For the meta-analysis, the proportions of the individual studies were Freeman–Tukey transformed [35] to enable the application of the common methods for fixed and random effects [6]. The pooled proportion was then calculated by inverse transformation of the weighted averages of the transformed proportions. In the forest plot, the proportions are depicted with 95% confidence intervals according to Clopper and Pearson [36], with the surface of the squares (point estimates) being proportional to the case number of the particular study. Funnel plots were tested for asymmetry [37]. The analysis was conducted in R 2.9.2 [38] (Library meta [39]).
Results
Analysis of the literature
Overall, 24 randomized, prospective and controlled studies were taken into consideration (Table 2). The studies varied in terms of study population. For the analysis, subgroups were therefore formed according to age (adults and children) (Table 3).
Table 2.
Overview studies included in meta-analysis
| References | In- or outpatient | # patients | # TH CTE | # PH CTE | # SH CTE | # “return to theatre” | Study location |
|---|---|---|---|---|---|---|---|
| Temple and Timms [11] | Outpatient | 18 | 0 | 0 | 0 | CTE: 0 | UK |
| Control: 0 | |||||||
| Shah et al. [12] | Outpatient | 17 | 1 | 0 | 1 | CTE: 1 | USA |
| Control: 0 | |||||||
| Timms and Temple [13] | Outpatient | 10 | 0 | 0 | 0 | CTE: 0 | UK |
| Control: 0 | |||||||
| Arya et al. [14] | Unknown | 14 | 0 | 0 | 1 | Unknown | UK |
| Hall et al. [15] | In- and outpatient | 28 | 2 | – | – | CTE: 0 | USA |
| Control: 0 | |||||||
| Stoker et al. [16] | Outpatient | 44 | 4 | 1 | 3 | CTE: 0 | USA |
| Control: 0 | |||||||
| Chan et al. [17] | Outpatient | 27 | 1 | 0 | 1 | CTE: 0 | USA |
| Control: 0 | |||||||
| Chang [18] | In- and outpatient | 52 | 0 | 0 | 0 | CTE: 0 | USA |
| Control: 0 | |||||||
| Philpott et al. [19] | Inpatient | 43 | 11 | 0 | 11 | CTE: 0 | UK |
| Control: 0 | |||||||
| Arya et al. [20] | Inpatient | 19 | 1 | 1 | 0 | CTE: 0 | UK |
| Control: 0 | |||||||
| Littlefield [21] | Outpatient | 17 | 1 | 0 | 1 | CTE: 0 | USA |
| Control: 0 | |||||||
| Parsons et al. [22] | In- and outpatient (mostly outpatients) | 47 | 1 | – | – | CTE: 1 | USA |
| Control 1: 2 | |||||||
| Control 2: 1 | |||||||
| Polites et al. [23] | Inpatient | 19 | 1 | 0 | 1 | CTE: 0 | Australia |
| Control: 1 | |||||||
| Noordzij and Affleck [24] | Unknown | 48 | 1 | 0 | 1 | CTE: 0 | USA |
| Control: 2 | |||||||
| Tan et al. [25] | Inpatient | 29 | 2 | 0 | 2 | CTE: 2 | Singapore |
| Control: 0 | |||||||
| Shapiro and Bhattacharyya [26] | Outpatient | 23 | 1 | 0 | 1 | CTE: 1 | USA |
| Control: 0 | |||||||
| Mitic et al. [27] | Outpatient | 20 | 0 | 0 | 0 | CTE: 0 | Norway |
| Control: 0 | |||||||
| Chang [28] | Unknown | 69 | 1 | 0 | 1 | CTE: 1 | USA |
| Magdy et al. [29] | Outpatient | 60 | 0 | 0 | 0 | CTE: 0 | Egypt |
| Controls: 0 | |||||||
| Hasan et al. [30] | In- and outpatient (mostly outpatients) | 20 | 1 | 0 | 1 | CTE: 1 | Finland |
| Control: 2 | |||||||
| Di Rienzo Businco and Tirelli [31] | Unknown | 21 | 0 | 0 | 0 | CTE: 0 | Italy |
| Control: 0 | |||||||
| Roje et al. [32] | Inpatient | 36 | 0 | 0 | 0 | CTE: 0 | Croatia |
| Control: 0 | |||||||
| Parker et al. [33] | Inpatient | 37 | 2 | – | – | CTE: 0 | UK |
| Control: 0 | |||||||
| D’Eredita and Bozzola [34] | Unknown | 78 | 1 | 0 | 1 | CTE: 0 | Italy |
| Control: 0 |
Table 3.
Overview postoperative hemorrhage rates over all studies
| Age group | Number of studies | Primary hemorrhage | Secondary hemorrhage | Total hemorrhage |
|---|---|---|---|---|
| Adults + children | 24 | 0.9% (n = 21) | 3.6% (n = 21) | 4.1% (n = 24) |
| 95% CI 0.3–1.7 | 95% CI 2.3–5.1 | 95% CI 2.8–5.5 | ||
| Adults | 11 | 0.8% (n = 9) | 6.2% (n = 9) | 5.8% (n = 11) |
| 95% CI 0.08–2.2 | 95% CI 3.6–9.4 | 95% CI 3.6–8.6 | ||
| Children | 13 | 1.0% (n = 12) | 2.3% (n = 12) | 2.9% (n = 13) |
| 95% CI 0.3–2.1 | 95% CI 1.1–4.0 | 95% CI 1.6–4.7 |
Heterogeneity
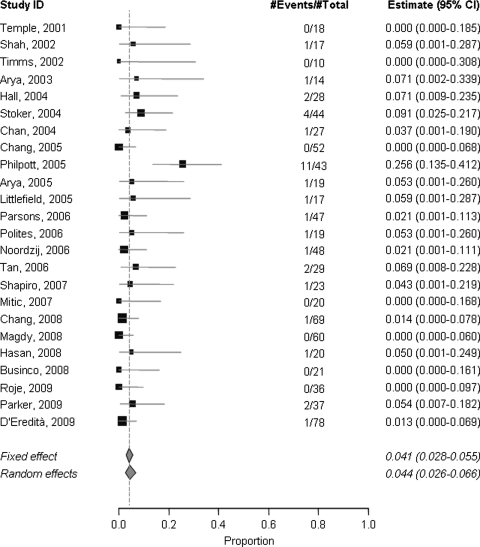
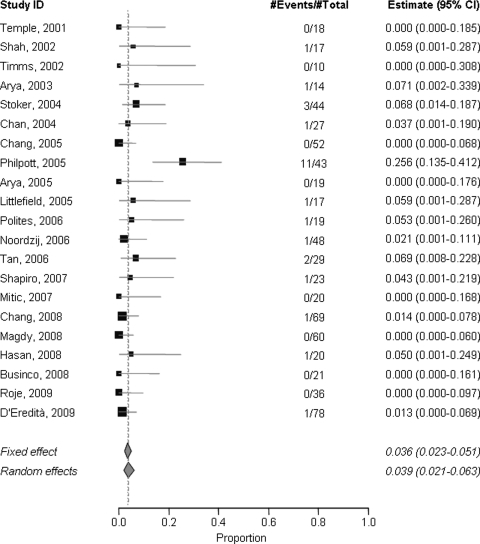
In the subgroup of adult patients the studies showed a moderate degree of heterogeneity in terms of the total hemorrhage rate [I 2 = 61.6% (26; 80.1)] (Fig. 2) and the secondary hemorrhage rate [I 2 = 67.6% (35.1; 84)] (Fig. 4).
Fig. 2.
Total hemorrhage rate, test for heterogeneity: χ 2 = 258.82, df = 37, p < 0.0001, I 2 = 85.7%. Test for overall effect: z = 11.8925, p < 0.0001
Fig. 4.
Secondary hemorrhage rate, test for heterogeneity: χ 2 = 39.61, df = 20, p = 0.0056, I 2 = 49.5%. Test for overall effect: z = 7.1576, p < 0.0001
Publication bias (effects of smaller studies)
Funnel plots and tests for asymmetry yielded no conclusive indications of relevant biases. If they indeed exist, then an overestimation of the pooled proportions, i.e. hemorrhage rates, appears to be plausible (few, upward-tending study results).
Patients
The pooling of all included studies resulted in a total of 796 patients. These could be subdivided into two age groups, one consisting of 461 children and the other of 335 adults. With regard to the child study population, the studies had various age limits. In our analysis, study participants <18 years of age were classified as children. Only patients whose age was certain were assigned to one of the age groups. Only those studies with a clear assignment of patients were included in the subgroup analysis.
Postoperative hemorrhage
Of all tonsillectomies performed using coblation, an overall hemorrhage incidence resulted for 33 patients. Of these, 2 could be classified as primary and 26 as secondary hemorrhages. 5 patients could not be classified into either group. Overall, the hemorrhage rate for the coblation procedure based on the 24 available studies was 4.1% (95% CI 0.028–0.055) when assuming the so-called fixed effect model and 4.4% (95% CI 0.026–0.066) for the random effects model across all studies analyzed (Fig. 2). If only the results of the subgroup children are taken into account, the hemorrhage rate is 2.9% (fixed effect model, 95% CI 0.016–0.047) and 3.0% (random effects model, 95% CI 0.016–0.048). Taking the results of the subgroup adults into consideration, the result is 5.8% (95% CI 0.036–0.086) for the fixed effect model and 6.4% (95% CI 0.027–0.114) for the random effects model.
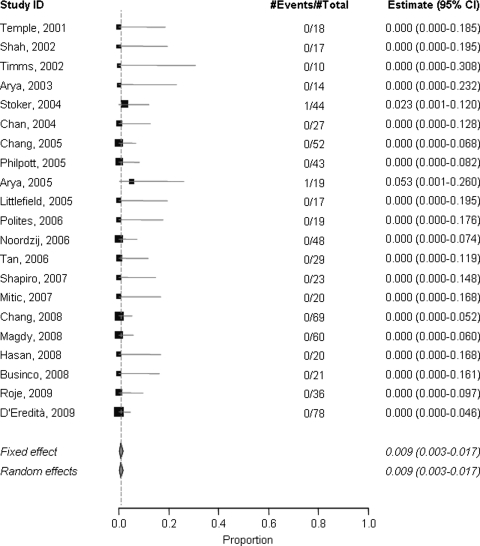
Primary hemorrhage
Of all 21 studies that classified postoperative hemorrhage, the primary hemorrhage rate for the fixed effect model was 0.9% (95% CI 0.003–0.017) and 0.9% (95% CI 0.003–0.017) for the random effects model (Fig. 3). The data analysis of all adult patient data results in a hemorrhage rate of 0.8% for both models (identical 95% CI for both models, 0.0008–0.022). For the children, the use of both models likewise yields hemorrhage rates of 1.0% (with identical 95% CI 0.003–0.021).
Fig. 3.
Primary hemorrhage rate, test for heterogeneity: χ 2 = 5.59, df = 20, p = 0.9993, I 2 = 0%. Test for overall effect: z = 4.9947, p < 0.0001
Secondary hemorrhage
The analysis of all available data on secondary hemorrhage results in a rate of 3.6% for the fixed effect model (95% CI 0.023–0.051) and 3.9% for the random effects model (95% CI 0.021–0.063) (Fig. 4). When differentiating among the age groups, the resulting secondary hemorrhage rate is 6.2% (fixed effect model, 95% CI 0.036–0.094) and 6.8% (random effects model, 95% CI 0.023–0.134) for the adult group. Upon inspection and evaluation of the secondary hemorrhage rates of children, both models likewise yield hemorrhage rates of 2.3% with identical 95% CI for both models (95% CI 0.011–0.040).
Discussion
There is still no generally accepted definition of the term hemorrhage with regard to post-tonsillectomy hemorrhage available. Different authors may use varying definitions of hemorrhage depending on their technique used for assessing hemorrhage, e.g. macroscopic evaluation or by microscope. Some publications focused solely on the need to return to theater, meaning hemorrhage requiring reoperation, whereas other studies recorded all postoperative hemorrhages. The discrepancies in definitions of secondary bleeding led to a big variation in figures stated in various publications. Thus, bleeding rate percentages have to be interpreted carefully. This should also to be taken into account when interpreting the results of this study.
Moreover, in Europe, no consensus concerning the term “inpatient” and “outpatient” with regard to the duration of stay in hospital exists [40]. In Germany and Austria for example, some inpatients stay 5 days postoperatively in hospital, whereas in the UK and Sweden an inpatient mostly stays overnight after surgery. These differing treatment patterns in various countries also have to be taken into account when analyzing bleeding rates (Table 2).
In May 2005 the Royal College of Surgeons of England published the data from the National Prospective Audit of Tonsillectomy (NPTA), which analyzed over 40,514 operation records in England and Northern Ireland [41]. In this report, four different applications of “electrosurgery” were discussed; in particular, the various applications of diathermy such as dissection or hemostasis (bipolar with forceps or scissors/monopolar) and coblation. These were compared with cold steel dissection when used in combination with various hemostasic procedures (hemostasis with ties and/or packs, with bipolar or monopolar diathermy). The two most common surgical techniques observed were cold steel dissection combined with bipolar diathermy for hemostasis (35%), followed by bipolar diathermy forceps (30%). Five percent of all patients underwent an operation using the coblation procedure. In the NPTA final report, focus was placed on postoperative hemorrhage, classifying it into primary and secondary hemorrhage rates. Comparing the two radiofrequency-based techniques for tonsillectomy, overall postoperative hemorrhage rates for bipolar diathermy and coblation were identical (4.6%). The differences between both techniques were mostly reflected by variations in the secondary bleeding rates. While primary bleeding events are often caused by insufficient intraoperative hemostasis, secondary hemorrhage is frequently related to the rejection of the wound surface and fibrinogen degeneration during wound healing determined by the surgical technique used for tonsillectomy [42]. According to the NPTA report, the secondary bleeding rate with coblation was found to be 3.6%, falling between the hemorrhage rates reported for cold steel with bipolar diathermy (2.3%) and bipolar diathermy forceps (4.4%). Regarding reoperation for postoperative hemorrhage, both electrosurgical tonsillectomy techniques required a slightly higher rate of reoperation than following the cold steel method with bipolar diathermy (0.7 as opposed to 0.4%).
Divergent trends pertaining to the use of coblation and bipolar diathermy could be found for different parts of the United Kingdom [43]. The Wales Single-use Instrument Surveillance Programme (SISP), which involved 3,690 patients who underwent tonsillectomy during the period from February 2003 to March 2004, indicates that the electrosurgery techniques were used less frequently than in England and Northern Ireland. In the SISP registry report secondary hemorrhage requiring return to theater after cold steel dissection with bipolar diathermy was found to be 0% (95% CI 0–2.7%). The rate of return to theater concerning bipolar diathermy was 2.2%, with coblation (0.5%) lying between cold steel with bipolar diathermy and bipolar diathermy hemorrhage rates. When taking into account the partially overlapping confidence intervals, it can be assumed that coblation, compared to the classical surgery technique and bipolar diathermy, is a safe method for tonsillectomy.
Another point that deserves to be mentioned is that some authors [44, 45] report about standardized premedication in children, as well as intraoperative pain therapy and postoperative treatment of pain with nonsteroidal anti-inflammatory drugs (NSAIDs). In a meta-analysis, Moiniche et al. [46] observe that under this form of pain therapy, reoperations due to hemorrhage are necessary at an average of more than twice as often (OR = 2.33).
Possible sources of the heterogeneity of the total hemorrhage rates identified in the adult subgroup could lie in the unequal degrees of surgeons’ operative experience, but they could also be due to the varying patient compliance, smoking habits, co-morbidity, condition of the tonsils, or coagulation disorders.
Our data shows a higher hemorrhage rate in the adult subgroup (5.8%) compared to the child subgroup (2.9%). This finding is in line with previous studies [47–53] which also demonstrate an age-dependence for post-tonsillectomy bleeding. This age-dependence is attributed to the fact that older patients have suffered from recurring infections of the tonsils [53] and that patient noncompliance with regard to postoperative management including dietary intake and physical rest increases in the age group between 11 and 40 years [48, 51].
Parental supervision contributes directly to high compliance rates, as children have less freedom of dietary intake after tonsillectomy than adults have. Moreover, it can be assumed that children suffer from less co-morbidity than adults. These assumptions are also consistent with the findings of Myssiorek et al. [50] and Carmody et al. [49] who show that age is a significant risk factor for post-tonsillectomy hemorrhages, since older patients more often have a history of chronic tonsillitis and are allowed more freedom of dietary intake postoperatively. Consequently, this may lead to an increased risk of secondary hemorrhage due to dietary trauma, as suggested by the increased incidence of bleeding between days 5 and 12, a period when eating increases as the odynophagia wanes away.
Very low hemorrhage rates were observed in individual studies. Nevertheless, in one study an even more significantly raised hemorrhage rate was observed. The latter [19] was far beyond the 95% confidence interval of 2.8–5.5% published in the literature, and might possibly have to be interpreted in terms of an autodidactic learning process as previously described in [54]. In light of this analysis, it appears reasonable that as with any other surgical technique, sufficient and proper training is essential. In the hands of trained surgeons, the coblation method does not appear to generate a high hemorrhage rate.
Conclusion
Based on our findings from the meta-analysis, we conclude that coblation is a safe and effective method for tonsillectomy compared to other radiofrequency-based techniques. Nevertheless, every bleeding, regardless of the technique chosen for the tonsillectomy, is a life-threatening event and needs to be treated with utmost care. This analysis clearly showed that there is need for a consistent definition of bleeding after tonsillectomies, as proposed by the Austrian Survey on tonsillectomy.1
Conflict of interest
The authors declare that no conflict of interest exists. The corresponding author R.M. has served as a scientific advisor for Arthrocare Deutschland, GmbH, and presented an honored lecture at a presentation of the manufacturer. The present publication has been prepared under no influence by the manufacturer in the context of a university research project. It was financed with university third-party funds also using an unrestricted research grant provided by the manufacturer Arthrocare Deutschland.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
S. Sarny and W. Habermann (Graz), Presentation of results and data analysis of the Austrian Tonsillectomy Study 2009/2010, 54th Annual Meeting of the Austrian Society of Oto-Rhino-Laryngology, Head and Neck Surgery, Salzburg, 2010.
References
- 1.Tonsillektomie-Nachblutung (2009) Spitzenmedizin der Deutschen Hochschulmedizin—Qualität leben. Verband der Universitätsklinika Deutschlands e.V. VUD, Berlin
- 2.Diagnosen und Prozeduren der vollständigen Patienten und Patientinnen in Krankenhäusern (2008). Statistisches Bundesamt
- 3.Kerst M (2003) Nach Mandelentzündung verbluteten zwei Patienten. Express, 20.10.2003
- 4.Husband AD, Davis A. Pain after tonsillectomy. Clin Otolaryngol Allied Sci. 1996;21(2):99–101. doi: 10.1111/j.1365-2273.1996.tb01310.x. [DOI] [PubMed] [Google Scholar]
- 5.Randall DA, Hoffer ME. Complications of tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg. 1998;118(1):61–68. doi: 10.1016/S0194-5998(98)70376-6. [DOI] [PubMed] [Google Scholar]
- 6.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 7.Burton MJ, Doree C (2007) Coblation versus other surgical techniques for tonsillectomy. Cochrane Database Syst Rev (3):CD004619. doi:10.1002/14651858.CD004619.pub2 [DOI] [PubMed]
- 8.Bortnick DP. Coblation: an emerging technology and new technique for soft-tissue surgery. Plast Reconstr Surg. 2001;107(2):614–615. doi: 10.1097/00006534-200102000-00053. [DOI] [PubMed] [Google Scholar]
- 9.Scheckenbach K, Bier H, Hoffmann TK, Windfuhr JP, Bas M, Laws HJ, Plettenberg C, Wagenmann M. Risk of hemorrhage after adenoidectomy and tonsillectomy. Value of the preoperative determination of partial thromboplastin time, prothrombin time and platelet count. HNO. 2008;56(3):312–320. doi: 10.1007/s00106-007-1585-x. [DOI] [PubMed] [Google Scholar]
- 10.Electrosurgery (diathermy and coblation) for tonsillectomy (2005) Interventional procedure guidance 150. National Institute for Health and Clinical Excellence, London
- 11.Temple RH, Timms MS (2001) Paediatric coblation tonsillectomy. Int J Pediatr Otorhinolaryngol 61 (3):195–198. doi:10.1016/s0165-5876(01)00553-5 [DOI] [PubMed]
- 12.Shah UK, Galinkin J, Chiavacci R, Briggs M (2002) Tonsillectomy by means of plasmamediated ablation: prospective, randomized, blinded comparison with monopolar electrosurgery. Arch Otolaryngol Head Neck Surg 128(6):672–676 [DOI] [PubMed]
- 13.Timms MS, Temple RH (2002) Coblation tonsillectomy: a double blind randomized controlled study. J Laryngol Otol 116(6):450–452. doi:10.1258/0022215021911031 [DOI] [PubMed]
- 14.Arya A, Donne AJ, Nigam A (2003) Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain. Clin Otolaryngol Allied Sci 28(6):503–506. doi:10.1046/j.1365-2273.2003-00750-x [DOI] [PubMed]
- 15.Hall DJ, Littlefield PD, Birkmire-Peters DP, Holtel MR (2004) Radiofrequency ablation versus electrocautery in tonsillectomy. Otolaryngol Head Neck Surg 130(3):300–305. doi:10.1016/j.otohns.2003.09.024 [DOI] [PubMed]
- 16.Stoker KE, Don DM, Kang DR, Haupert MS, Magit A, Madgy DN (2004) Pediatric total tonsillectomy using coblation compared to conventional electrosurgery: a prospective, controlled single-blind study. Otolaryngol Head Neck Surg 130 (6):666–675. doi:10.1016/j.otohns.2004.02.012 [DOI] [PubMed]
- 17.Chan KH, Friedman NR, Allen GC, Yaremchuk K, Wirtschafter A, Bikhazi N, Bernstein JM, Kelley PE, Lee KC (2004) Randomized, controlled, multisite study of intracapsular tonsillectomy using low-temperature plasma excision. Arch Otolaryngol Head Neck Surg 130(11):1303–1307. doi:10.1001/archotol.130.11.1303 [DOI] [PubMed]
- 18.Chang KW (2005) Randomized controlled trial of Coblation versus electrocautery tonsillectomy. Otolaryngol Head Neck Surg 132(2):273–280. doi:10.1016/j.otohns.2004.11.002 [DOI] [PubMed]
- 19.Philpott CM, Wild DC, Mehta D, Daniel M, Banerjee AR. A double-blinded randomized controlled trial of coblation versus conventional dissection tonsillectomy on post-operative symptoms. Clin Otolaryngol. 2005;30(2):143–148. doi: 10.1111/j.1365-2273.2004.00953.x. [DOI] [PubMed] [Google Scholar]
- 20.Arya AK, Donne A, Nigam A (2005) Double-blind randomized controlled study of coblation tonsillotomy versus coblation tonsillectomy on postoperative pain in children. Clin Otolaryngol 30(3):226–229 [DOI] [PubMed]
- 21.Littlefield PD, Hall DJ, Holtel MR (2005) Radiofrequency excision versus monopolar electrosurgical excision for tonsillectomy. Otolaryngol Head Neck Surg 133(1):51–54. doi:10.1016/j.otohns.2005.02.013 [DOI] [PubMed]
- 22.Parsons SP, Cordes SR, Comer B (2006) Comparison of posttonsillectomy pain using the ultrasonic scalpel, coblator, and electrocautery. Otolaryngol Head Neck Surg 134(1):106–113. doi:10.1016/j.otohns.2005.09.027 [DOI] [PubMed]
- 23.Polites N, Joniau S, Wabnitz D, Fassina R, Smythe C, Varley P, Carney AS (2006) Postoperative pain following coblation tonsillectomy: randomized clinical trial. ANZ J Surg 76(4):226–229. doi:10.1111/j.1445-2197.2006.03700.x [DOI] [PubMed]
- 24.Noordzij JP, Affleck BD (2006) Coblation versus unipolar electrocautery tonsillectomy: a prospective, randomized, single-blind study in adult patients. Laryngoscope 116(8):1303–1309. doi:10.1097/01.mlg.0000225944.00189.e9 [DOI] [PubMed]
- 25.Tan AK, Hsu PP, Eng SP, Ng YH, Lu PK, Tan SM, Say JH, Chan YH (2006) Coblation vs electrocautery tonsillectomy: postoperative recovery in adults. Otolaryngol Head Neck Surg 135(5):699–703 doi:10.1016/j.otohns.2006.03.008 [DOI] [PubMed]
- 26.Shapiro NL, Bhattacharyya N (2007) Cold dissection versus coblation-assisted adenotonsillectomy in children. Laryngoscope 117(3):406–410. doi:10.1097/MLG.0b013e31802ffe47 [DOI] [PubMed]
- 27.Mitic S, Tvinnereim M, Lie E, Saltyte BJ (2007) A pilot randomized controlled trial of coblation tonsillectomy versus dissection tonsillectomy with bipolar diathermy haemostasis. Clin Otolaryngol 32(4):261–267. doi:10.1111/j.1365-2273.2007.01468.x [DOI] [PubMed]
- 28.Chang KW (2008) Intracapsular versus subcapsular coblation tonsillectomy. Otolaryngol Head Neck Surg 138(2):153–157. doi:10.1016/j.otohns.2007.11.006 [DOI] [PubMed]
- 29.Magdy EA, Elwany S, el-Daly AS, Abdel-Hadi M, Morshedy MA (2008) Coblation tonsillectomy: a prospective, double-blind, randomised, clinical and histopathological comparison with dissection-ligation, monopolar electrocautery and laser tonsillectomies. J Laryngol Otol 122(3):282–290. doi:10.1017/S002221510700093X [DOI] [PubMed]
- 30.Hasan H, Raitiola H, Chrapek W, Pukander J (2008) Randomized study comparing postoperative pain between coblation and bipolar scissor tonsillectomy. Eur Arch Otorhinolaryngol 265(7):817–820. doi:10.1007/s00405-007-0537-0 [DOI] [PubMed]
- 31.Di Rienzo Businco L, Coen Tirelli G (2008) Paediatric tonsillectomy: radiofrequency-based plasma dissection compared to cold dissection with sutures. Acta Otorhinolaryngol Ital 28(2):67–72 [PMC free article] [PubMed]
- 32.Roje Z, Racic G, Dogas Z, Pisac VP, Timms M (2009) Postoperative morbidity and histopathologic characteristics of tonsillar tissue following coblation tonsillectomy in children: a prospective randomized single-blind study. Coll Antropol 33(1):293–298 [PubMed]
- 33.Parker D, Howe L, Unsworth V, Hilliam R (2009) A randomised controlled trial to compare postoperative pain in children undergoing tonsillectomy using cold steel dissection with bipolar haemostasis versus coblation technique. Clin Otolaryngol 34(3):225–231. doi::10.1111/j.1749-4486.2009.01932.x [DOI] [PubMed]
- 34.D'Eredita R, Bozzola L (2009) Molecular resonance vs. coblation tonsillectomy in children. Laryngoscope 119(10):1897–1901. doi:10.1002/lary.20210 [DOI] [PubMed]
- 35.Mosteller F, Youtz C. Tables of the Freeman–Tukey transformations for the binomial and Poisson distributions. Biometrika. 1961;48(3–4):433–440. [Google Scholar]
- 36.Clopper C, Pearson E. The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika. 1934;26(4):404–413. doi: 10.1093/biomet/26.4.404. [DOI] [Google Scholar]
- 37.Thompson SG, Sharp SJ. Explaining heterogeneity in meta-analysis: a comparison of methods. Stat Med. 1999;18(20):2693–2708. doi: 10.1002/(SICI)1097-0258(19991030)18:20<2693::AID-SIM235>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 38.Team RDC. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2009. [Google Scholar]
- 39.Schwarzer G (2009) meta: Meta-Analysis with R. R package version 1.1-4. http://CRAN.R-project.org/package=meta
- 40.Schmelzer B, Peeters A. Tonsillectomy and adenoidectomy: postoperative management in European countries. Laryngorhinootologie. 1999;78(11):594–595. doi: 10.1055/s-1999-12970. [DOI] [PubMed] [Google Scholar]
- 41.National prospective tonsillectomy audit—final report (2005). Royal College of Surgeons, London
- 42.Schmidt H, Schmiz A, Stasche N, Hormann K. Surgically managed postoperative hemorrhage after tonsillectomy. Laryngorhinootologie. 1996;75(8):447–454. doi: 10.1055/s-2007-997613. [DOI] [PubMed] [Google Scholar]
- 43.Mowatt G, Cook J, Fraser C, Burr J (2005) Systematic review of the safety and efficacy of electrosurgery for tonsillectomy. Review body report submitted to the Interventional Procedures Programme, National Institute for Health and Clinical Excellence
- 44.Windfuhr JP, Deck JC, Krabs C, Sadra R, Remmert S. Coblation tonsillectomy. Results of a pilot study. HNO. 2006;54(3):190–197. doi: 10.1007/s00106-005-1308-0. [DOI] [PubMed] [Google Scholar]
- 45.Schmidt A, Bjorkman S, Akeson J. Preoperative rectal diclofenac versus paracetamol for tonsillectomy: effects on pain and blood loss. Acta Anaesth Scand. 2001;45(1):48–52. doi: 10.1034/j.1399-6576.2001.450108.x. [DOI] [PubMed] [Google Scholar]
- 46.Moiniche S, Romsing J, Dahl JB, Tramer MR. Nonsteroidal antiinflammatory drugs and the risk of operative site bleeding after tonsillectomy: a quantitative systematic review. Anesth Analg. 2003;96(1):68–77. doi: 10.1213/00000539-200301000-00015. [DOI] [PubMed] [Google Scholar]
- 47.Windfuhr JP, Chen YS, Remmert S. Hemorrhage following tonsillectomy and adenoidectomy in 15, 218 patients. Otolaryngol Head Neck Surg. 2005;132(2):281–286. doi: 10.1016/j.otohns.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 48.Roberts C, Jayaramachandran S, Raine CH. A prospective study of factors which may predispose to post-operative tonsillar fossa haemorrhage. Clin Otolaryngol Allied Sci. 1992;17(1):13–17. doi: 10.1111/j.1365-2273.1992.tb00980.x. [DOI] [PubMed] [Google Scholar]
- 49.Carmody D, Vamadevan T, Cooper SM. Post tonsillectomy haemorrhage. J Laryngol Otol. 1982;96(7):635–638. doi: 10.1017/S0022215100092926. [DOI] [PubMed] [Google Scholar]
- 50.Myssiorek D, Alvi A. Post-tonsillectomy hemorrhage: an assessment of risk factors. Int J Pediatr Otorhinolaryngol. 1996;37(1):35–43. doi: 10.1016/0165-5876(96)01364-X. [DOI] [PubMed] [Google Scholar]
- 51.Kristensen S, Tveteras K. Post-tonsillectomy haemorrhage. A retrospective study of 1150 operations. Clin Otolaryngol Allied Sci. 1984;9(6):347–350. doi: 10.1111/j.1365-2273.1984.tb01519.x. [DOI] [PubMed] [Google Scholar]
- 52.Rosenfeld RM, Green RP. Tonsillectomy and adenoidectomy: changing trends. Ann Otol Rhinol Laryngol. 1990;99(31):187–191. [PubMed] [Google Scholar]
- 53.Schrock A, Send T, Heukamp L, Gerstner AO, Bootz F, Jakob M. The role of histology and other risk factors for post-tonsillectomy haemorrhage. Eur Arch Otorhinolaryngol. 2009;266(12):1983–1987. doi: 10.1007/s00405-009-0958-z. [DOI] [PubMed] [Google Scholar]
- 54.Carney AS, Harris PK, MacFarlane PL, Nasser S, Esterman A. The coblation tonsillectomy learning curve. Otolaryngol Head Neck Surg. 2008;138(2):149–152. doi: 10.1016/j.otohns.2007.10.031. [DOI] [PubMed] [Google Scholar]