Abstract
Oral infections caused by yeast of the genus Candida and particularly Candida albicans (oral candidoses) have been recognised throughout recorded history. However, since the 1980s a clear surge of interest and associated research into these infections have occurred. This has largely been due to an increased incidence of oral candidosis over this period, primarily because of the escalation in HIV-infection and the AIDS epidemic. In addition, changes in medical practice leading to a greater use of invasive clinical procedures and a more widespread use of immunosuppressive therapies have also contributed to the problem. Whilst oral candidosis has previously been considered to be a disease mainly of the elderly and very young, its occurrence throughout the general population is now recognised. Candida are true ‘opportunistic pathogens’ and only instigate oral infection when there is an underlying predisposing condition in the host. Treatment of these infections has continued (and in some regards continues) to be problematic because of the potential toxicity of traditional antifungal agents against host cells. The problem has been compounded by the emergence of Candida species other than C. albicans that have inherent resistance against traditional antifungals. The aim of this review is to give the reader a contemporary overview of oral candidosis, the organisms involved, and the management strategies that are currently employed or could be utilised in the future.
Keywords: oral candidosis, Candida
The Candida genus is comprised of over 150 species of asporogenous ‘yeast-like’ fungi. Members of this genus are ubiquitously distributed, persisting as saprophytes in soil and aquatic environments, as well as colonising several animal reservoirs (1–3). The majority of Candida species are unable to grow at 37°C and are, therefore, not normally associated with human colonisation (4). However several species do persist as commensal microorganisms within humans and these can act as opportunistic pathogens in debilitated individuals (Table 1). Candida albicans is the species most frequently associated with normal oral carriage in humans, occurring in the mouths of up to 80% of healthy individuals (13).
Table 1.
Candida species recovered from the human mouth
A change from the harmless commensal existence of Candida to a pathogenic state can occur following alteration of the oral cavity environment to one that favours the growth of Candida. The causes of such changes are the so-called predisposing factors for Candida infection (candidosis) and most often these relate to a weakening of host immune defences (Table 2).
Table 2.
Host-related factors associated with oral candidosis
| Predisposing host factor | Reference |
|---|---|
| Local host factors | |
|
(14) |
| (15, 16) | |
| (17) | |
| (18) | |
| Systemic host factors | |
|
(19) |
| (20) | |
| (21) | |
| (22) | |
| (23) | |
Infections caused by Candida are most frequently superficial, occurring on moist mucosal surfaces in individuals suffering with a mild debilitation. In severely immunocompromised patients, infections can be systemic and are significant because of their associated high mortality. To highlight this, in intensive care unit patients the mortality rate for individuals with systemic candidosis is approximately 30–50% (24).
Recent decades have seen a significant increase in the incidence of all forms of candidosis and this reflects changes in medical practice with a greater use of invasive surgical procedures, a more widespread use of immunosuppressive therapies as well as broad-spectrum antibiotics. Key to the increase in oral candidosis has, however, been the escalation of HIV-infection and AIDs (25).
The most prevalent Candida species involved in human infection is C. albicans. In oral candidosis, C. albicans generally accounts for around 50% of cases (26, 27) and whilst a similar prevalence of C. albicans occurs in systemic candidosis, in recent years higher incidences of non-C. albicans Candida (NCAC) species have been reported (28, 29). The reasons for the increasing incidence of NCAC species in human infection are multifactorial and undoubtedly improved diagnostic methods, changes in medical practices such as the more widespread use of invasive medical procedures (e.g. use of indwelling catheters, organ transplants) and immunosuppressive therapy may all have facilitated increased rates (30).
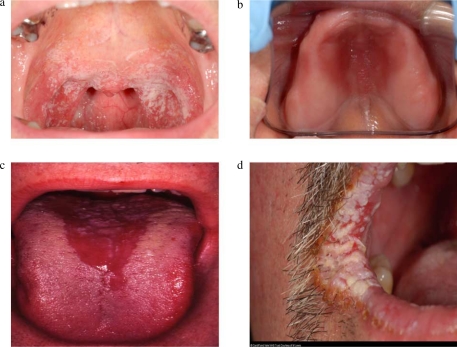
Oral candidosis is not a single infection and generally four primary oral forms are described based on clinical presentation (Fig. 1). Pseudomembranous candidosis (oral thrush) presents as creamy white lesions on the oral mucosa and a diagnostic feature of this infection is that these plaques can be removed by gentle scraping leaving behind an underlying erythematous mucosal surface (31, 32). Histological examination of recovered pseudomembranes reveals desquamated epithelial cells together with yeast and filamentous forms of Candida. The infection has traditionally been regarded as an acute condition often affecting newborn babies where there is an immature immune system. In older individuals, acute pseudomembranous candidosis often occurs when there is a nutritional limitation, local immune suppression (e.g. steroid inhaler administration for the treatment of asthma), or an underlying disease most notably HIV-infection and AIDS (26, 33, 34).
Fig. 1.
Clinical presentation of the primary forms of oral candidosis. (a) acute pseudomembranous candidosis; (b) chronic erythematous candidosis; (c) acute erythematous candidosis; and (d) chronic hyperplastic candidosis.
In the case of AIDS, or other instances where the individual is immunocompromised long-term, chronic pseudomembranous candidosis can develop and whilst antifungal therapy can temporarily resolve the condition, recurrent infection is frequent. Of additional concern with chronic forms of pseudomembranous candidosis is the subsequent progression of infection to oesophageal involvement, which in turn can lead to difficulties in swallowing and chest pains.
In addition to pseudomembranous candidosis, another acute form of Candida infection is acute erythematous candidosis. This form of oral candidosis frequently occurs after receipt of a broad-spectrum antibiotic, which, by lowering the oral bacterial population, facilitates subsequent overgrowth of Candida by alleviating competitive pressures. The infection can occur on the buccal mucosa, but most frequently presents as reddened lesions on the dorsum of the tongue and also the palate (32, 35). Erythematous candidosis is the only form of oral candidosis that is consistently painful. Where antibiotic treatment has been associated with predisposition, cessation of treatment leads to spontaneous resolution of the lesions once the bacterial population of the mouth recovers to pretreatment levels (22).
Chronic forms of erythematous candidosis can also occur and traditionally these infections encompassed the atrophic lesions associated with angular cheilitis and denture stomatitis. However, both infections are also linked to bacterial colonisation and, therefore, these are now often categorised under Candida-associated lesions (see later). Chronic erythematous candidosis is prevalent in HIV-positive individuals and AIDS patients, and depending on the study can represent over a third of the Candida lesions encountered (36).
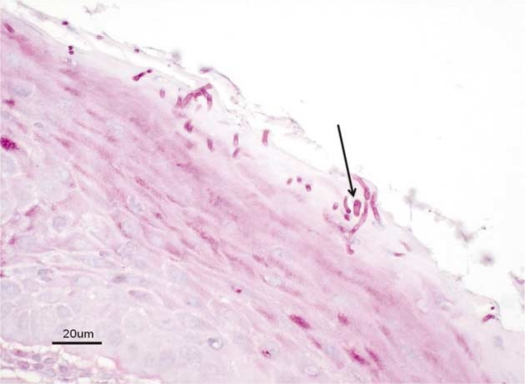
Chronic hyperplastic candidosis (occasionally referred to as candidal leukoplakia) can present on any oral mucosal surface and appears either as smooth (homogenous) or nodular white lesions (37). Unlike the lesions of pseudomembranous candidosis, those of chronic hyperplastic candidosis cannot be removed by gentle scraping. Most frequently, chronic hyperplastic candidosis occurs bilaterally in the commissural regions of the buccal mucosa with highest prevalence in middle-aged men who are smokers (38). A characteristic feature of this form of oral candidosis is the penetration of the oral epithelium by C. albicans hyphae, which are detected in biopsy sections following Periodic Acid-Schiff (PAS) or equivalent staining methods (Fig. 2). Histological examination is indeed the diagnostic tool for this infection and in addition to the presence of Candida hyphae, an inflammatory cell infiltrate is invariably present within the lamina propria together with marked variations in epithelial thickness (39). An important feature of chronic hyperplastic candidosis is its possible association with malignant transformation (40). A confirmed link between Candida and the development of oral cancer remains to be established, although it has been shown in vitro that yeast can generate the carcinogenic nitrosamine, N-nitrosobenzylmethylamine from suitable precursor molecules (41).
Fig. 2.
Periodic Acid Schiff stained biopsy section of chronic hyperplastic candidosis. Typical invading hypha indicated by arrow.
Secondary forms of oral candidosis can also occur and are frequently described as Candida-associated lesions. Angular cheilitis is a condition where lesions manifest at the angles of the mouth and microbiological sampling of these sites frequently reveal the presence of C. albicans, often in combination with the bacterium Staphylococcus aureus (42). The exact role of Candida in this infection remains unclear, but it is worth noting that angular cheilitis often occurs in patients with existing forms of intraoral candidosis and where the Candida load is already high.
Median rhomboid glossitis is a chronic condition that presents as a diamond-shaped lesion at the posterior midline on the dorsum of the tongue (31). High levels of Candida can be recovered from these lesions, which are often associated with individuals who frequently use steroid inhalers or who are tobacco smokers (43).
The most prevalent oral infection involving Candida is Candida-associated denture stomatitis, which occurs in up to 65% of denture wearers, often asymptomatically (44). As this name suggests, denture wearing is the major predisposing factor, particularly in cases where the denture is not adequately cleansed or is retained overnight in the oral cavity. Under these conditions, the stagnant area above the upper fitting surface of the denture provides an ideal environment for the growth of Candida, which is adept at adhering to acrylic used as the base material for the denture (45). Furthermore, the limited flow of saliva at this location means that loosely adherent Candida may not be efficiently removed from the site, as would be the case at other oral locations. In situations where there is an ill-fitting denture, frictional irritation can damage the normally protective mucosal barrier, allowing infiltration of Candida into the tissue thereby promoting infection.
Candida have also been associated with linear gingival erythema, which, whilst rare, is occasionally seen in HIV-infected patients (46, 47). The precise role of Candida in this condition remains to be confirmed, which may in part be due to the frequent use of systemic antifungal agents in HIV patients.
In a discussion on the oral forms of candidosis, mention needs to be made of chronic mucocutaneous candidosis (CMC), characterised by the widespread occurrence of superficial candidosis of the skin, nails, and mucosal membranes (including those of the oral cavity) of infected individuals (48, 49). CMC is primarily associated with disorders resulting in the incorrect functioning of T-lymphocytes (48).
Candida virulence factors
Given the high prevalence of Candida as a harmless commensal in humans, it is not surprising that no single primary virulence factor has been identified with the organism. However, a number of putative virulence factors (Table 3) have been proposed that in the event of host debilitation contribute to tissue damage and persistence of the organism within the host.
Table 3.
Putative virulence factors of Candida albicans
| Virulence factor | Effect |
|---|---|
Adherence
|
Promotes retention in the mouth
|
Evasion of host defences
|
Promotes retention in the mouth
|
Invasion and destruction of host tissue
|
Enhances pathogenicity
|
The ability of Candida to adhere to host surfaces is a prerequisite for both successful commensal carriage as well as persistence during active infection. Within the oral cavity, removal of loosely attached Candida by the physical flushing action of salivary flow or the process of sloughing off of epithelial cells from mucosal surfaces are important factors in host defence against Candida overgrowth. An enhanced ability to overcome these removal mechanisms can therefore be regarded as a virulence attribute.
Adherence of Candida to human epithelial cells is initiated through weak and reversible interactions involving hydrophobic and electrostatic forces (50). The nature of these forces are in part governed by the local environment in the oral cavity; however, studies have shown that strain variation does occur in terms of cell surface hydrophobicity that may give certain isolates greater pathogenic potential (51).
Specific adhesion between Candida and receptors on host tissues results in a stronger covalent attachment. Candida genes of the ALS (agglutinin-like sequence) family (52) and also HWP1 (hyphal wall protein) (53) encodes for cell wall associated glycoproteins that promote adhesion of C. albicans to epithelial surfaces. In addition, specific interaction of Candida with oral bacteria has also been demonstrated that could encourage biofilm formation on dentures and in dental plaque (54).
Biofilms can be defined as microbial communities that are often (but not necessarily) attached to a solid surface; invariably the biofilm microorganisms are encased within an extracellular polysaccharide matrix that has been generated by the organisms themselves. Candida species are adept at forming biofilms (55, 56) and this has been linked to both increased expression of virulence factors (57) as well as reduced susceptibility to antimicrobial agents (58). Candida biofilms in human disease are widely recognised and occur on tissue surfaces as well as the biomaterials of medical devices. Candida biofilms on artificial voice box prostheses have been identified as a major cause of their failure. Urinary tract infections caused by Candida biofilms in catheterised patients are recognised, whilst biofilms at other sites including on prosthetic heart valves, intravascular catheters, and replacement joints have also been linked with infection (59). Candidal biofilms in haemodialysis and peritoneal dialysis catheters are a common occurrence and associated with an infection rate of up to 20% in patients undergoing treatment (55).
In terms of oral candidosis, biofilms on an oral prosthesis, most commonly a denture, are a major predisposing factor to chronic oral candidosis. Candida readily adhere to the polymethylacrylate material of dentures, and also exploit micro fissures and cracks within the material to facilitate retention (60). Biofilm formation on denture surfaces is further promoted by poor oral hygiene and retention of dentures in the mouth whilst sleeping.
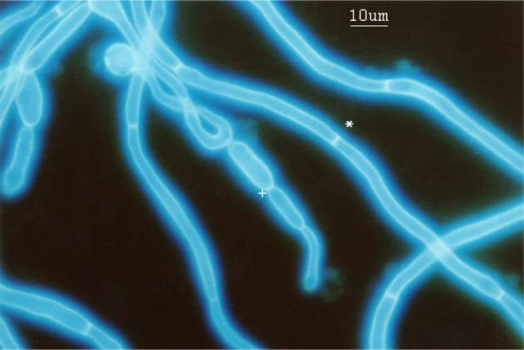
Several Candida species are described as polymorphogenic (61) and whilst in nutrient rich culture media at 37°C, yeast growth would appear to be prevalent, filamentous growth can occur and indeed is frequently seen in clinical situations. Both C. albicans and Candida dubliniensis are species associated with the generation of true hyphae (62). True hyphae are distinct from pseudohyphae (which are effectively elongated yeast cells), as the former lack constriction at yeast/hyphal junctions and also possess septa within the filaments (Fig. 3). The pathogenic significance of being able to produce hyphae could relate to the greater resistance of hyphae to phagocytosis compared with yeast, enhanced adherence to host surfaces, and the ability of hyphae to invade epithelial layers resulting in tissue damage (Fig. 2). Hyphal production is also linked with enhanced expression of several putative virulence genes, some of which are not involved in the morphogenic process itself (63). It should be noted that both filamentous and yeast forms are encountered in the oral cavity of healthy individuals, highlighting the importance of host factors in controlling Candida and the fact that no single predominant virulence factor is associated with the organism (64).
Fig. 3.
Calcofluor white stained Candida albicans showing true hyphae (*) and pseudohyphae (+).
A phenomenon referred to as ‘high frequency phenotypic switching’ is evident in vitro for certain strains of C. albicans when cultured on appropriate agar media. Colonies generated by isolates that are ‘high frequency switchers’ exhibit variation in terms of colour, shape, and translucency. The cause of these colony switch variants relates to cell morphology and differential gene expression by the variants (56, 61). The so-called white-opaque switching is associated with mating in C. albicans as well as the up-regulation of biofilm genes (65, 66). High frequency switching strains have been proposed to have greater virulence, as replication of this property in vivo might aid in evading recognition by adaptive immune responses as well as promoting biofilm formation.
Candida produces several extracellular enzymes that could have a locally damaging effect on host structures (67). Significant attention has been given to the secreted aspartyl proteinases (SAPs) of Candida. C. albicans possesses at least 10 different genes that encode for SAPs, and the resulting proteins are in turn designated SAPs 1–10. SAPs 1–8 are released extracellularly, whilst SAPs 9 and 10 are thought to be membrane bound. SAP enzymes belong to the same class of proteinases as the HIV aspartyl proteinase as well as human pepsin and renin. All Candida SAPs are inhibited by the agent pepstatin A. Candida SAPs have optimal activity at acidic pH (pH 2–7 activity range), although distinct differences in pH optima are evident with SAPs 1–3 being most active at the lower end of the pH scale and SAPs 4–6 at higher pH. This heterogeneity in activity optima of the SAPs could benefit Candida in its survival under different environmental conditions. Of the Candida SAPs, the most widely studied are SAPs 1–6. From research it has been shown that SAP 2 is induced when C. albicans is cultured in media containing proteins as the only nitrogen source (68). SAP 1 and SAP 3 are specifically expressed during switching of C. albicans, whilst SAPs 4–6 are involved in promoting hyphal growth (69). C. albicans proteinases have keratinolytic activity that can both serve to facilitate initial penetration of keratinised cells as well as providing a valuable source of nitrogen during colonisation (70, 71).
In terms of virulence, SAP activity can therefore directly induce damage to host cells, facilitate hyphal growth for invasion of tissue, increase adherence following exposure of receptor sites, and also degrade host immunoglobulins and other defence proteins (55, 72–75).
Another group of hydrolytic enzymes produced by Candida species are the phospholipases (PLs) and seven distinct encoding genes have been identified in C. albicans. These genes have been given the designations PLA, PLB1, PLB2, PLC1, PLC2, PLC3, and PLD1 (76). Through the hydrolysis of ester linkages of phospholipids, PLs can effectively degrade the membrane of host cells leading to cell lysis and death. By this process, both adherence of Candida to receptor sites and its subsequent penetration of damaged tissue can be facilitated.
The role of extracellular lipase and esterase production by Candida in pathogenic processes is less well understood (77). Both lipases and esterases share the ability to hydrolyse the ester bonds in glycerides, although the latter only act on soluble substrate molecules. A total of 10 Candida lipase (LIP1–10) genes have been identified in C. albicans and sequence-related genes found in C. tropicalis, C. parapsilosis, and C. krusei (78). Lipases of C. albicans have recently been shown to exhibit cytotoxic effects on host cells (79) and LIP gene expression detected in oral candidosis (80).
Haemolysins are substances that lyse red blood cells and their production by Candida is considered an important attribute in promoting survival within the host through an increased ability to sequester iron. Luo et al. (81) demonstrated α- and β-haemolysis by clinical isolates of C. albicans, C. dubliniensis, C. kefyr, C. krusei, C. zeylanoides, C. glabrata, C. tropicalis, and C. lusitaniae. Candida haemolysin production positively correlates with glucose concentration and that this could be a predisposing factor in candidosis of poorly controlled diabetics where higher blood and salivary glucose levels occurs (76, 82).
Host response to oral candidosis
Immunocompetent individuals rarely suffer from oral candidosis even when Candida is present in the oral cavity. Prevention of mucosal infection by Candida is mediated primarily by the functions of the innate immune response. In particular, neutrophils and macrophages are key to successful phagocytosis and killing of Candida. Professional phagocytes recognise Candida through pattern recognition receptors (PRRs), which interact with specific molecules (pathogen-associated molecular patterns; PAMPs) exposed on the surface of Candida (83). Following recognition, these cells release cytokines and chemokines to further modulate the immune response. Dendritic cells (DCs) are professional antigen presenting cells that provide a sentinel role in mucosal tissue. Interaction of DCs with Candida leads to DC activation and phagocytosis. Following phagocytosis, DCs migrate to the lymph nodes where the Candida antigen is processed and presented on the surface of the DC to naïve CD4+ T-cells (84–88). Interaction between DCs and T-cells cause the latter to differentiate into mature effective T-cells (89). The type of T-cell generated is thought to be under direction of the DC and examples of effective T-cells include T-helper 1 (Th1), T-helper 2 (Th2), T-helper 17 (Th17), and regulatory T-cells (Tregs). Previously it was generally accepted that a Th1 elicited response was a protective one, whilst Th2 responses were implicated in infection. More recently, evidence suggests that a Th17 response is predominant in protection of mucosal surfaces (90).
Treatment and management of oral candidosis
A priority in the treatment of oral candidosis is the alleviation of any identifiable predisposing factor. Acquiring a thorough medical history is, therefore, an essential component in the management process. An example of this are the recommendations made to patients suffering from chronic erythematous candidosis in order to improve oral hygiene through adequate denture cleansing. Such recommendations would include the regular and frequent use of a denture cleanser with anti-candidal properties such as 1% sodium hypochlorite preparations, together with the removal of dentures overnight. Chlorhexidine (0.2%) should be used if the denture has metal components since hypochlorite will otherwise cause discolouration. However, it should also be noted that discolouration of teeth and mucosal surfaces have been reported with the use of chlorhexidine (91).
Certain predisposing factors are, however, more difficult if not impossible to eradicate such as where there is an underlying disease (e.g. leukaemia or AIDS). In these cases, targeted antifungal therapy, as discussed later, plays an important role in the management strategy.
Both the physical and chemical reduction of Candida load in the oral cavity can be achieved by good oral hygiene practices including tooth brushing and the use of antimicrobial mouthwashes. Manual tooth brushing is limited to accessible oral surfaces, although powered or electrical tooth brushing may be more effective as cavitation within surrounding fluids could disrupt Candida biofilms at otherwise inaccessible sites (92). Several mouthwashes exhibit anti-candidal activity including triclosan, chlorhexidine gluconate, and essential oil formulations. The latter tend to contain natural plant extracts such as thymol, eucalyptol, and bioflavanoids and these can have a direct anti-candidal activity in vitro through cell membrane disruption and enzyme inhibition (93, 94).
When compared with antibacterial agents, the availability of antifungal agents is significantly lower. The reason for this relates to the relatively recent recognition of the significance of human fungal infections and also the fact that fungal organisms are eukaryotic and share many features with mammalian cells making selection of suitable targets for antifungal agents problematic. Classification of antifungal agents is based on the target of activity, and in the treatment of candidosis the two classes most commonly used are the polyenes and the azoles (Table 4).
Table 4.
Antifungals used in the management of candidosis
| Antifungal | Mode of action | Administration | Frequently recommended treatment |
|---|---|---|---|
| Polyenes | Binds to ergosterol and disrupts fungal cell membrane | ||
|
Topical | CEC | |
| Topical | CEC | ||
Azoles
|
Inhibits ergosterol biosynthesis | ||
| Systemic | PMC, AEC, CHC | ||
| Topical | CEC | ||
| Topical/systemic | PMC, AEC, CHC | ||
| Topical | CEC | ||
| Systemic | PMC, AEC, CHC | ||
| Systemic | |||
| Systemic | |||
| 5-flucytosine | Inhibition of DNA/protein synthesis | Systemic, often in combined therapy with amphotericin | |
| Echinocandins | Inhibits ß 1, 3 D-glucan synthesis | Intravenous | |
|
Abbreviations: CEC, chronic erythematous candidosis; PMC, pseudomembranous candidosis; AEC, acute erythematous candidosis; CHC, chronic erythematous candidosis.
Nystatin is used as an ointment or oral suspension.
Amphotericin B is used as a lozenge.
Miconazole is used as an oral gel and cream.
Clotrimazole is used as a cream and pessary.
Other antifungals are available and more frequently used in hospitalised patients.
Polyenes include the drugs amphotericin B and nystatin and their mode of action is through direct binding to the sterol ergosterol found within fungal cell membranes. Polyene binding to ergosterol induces leakage of cytoplasmic contents leading to fungal cell death (95). The equivalent mammalian sterol is cholesterol, which has a lower binding affinity for polyenes and this makes host cells less susceptible to their toxic effects. Nevertheless, at higher therapeutic concentrations polyenes do exhibit a degree of toxicity in humans. The use of polyenes is limited further as they are poorly absorbed through the gut and, therefore, topical application in the form of lozenges and oral suspensions are the principle means of administration in oral infection. Polyenes are frequently used in the treatment of chronic erythematous candidosis, and oral suspension of amphotericin B may be employed in treating refractory oral candidosis frequently seen in HIV-infected and AIDs patients.
Unlike the polyenes, azole antifungals are fungistatic rather than fungicidal (96). The mechanism of action is by inhibiting the enzyme lanosterol demethylase that is a cytochrome P-450 3-A dependent enzyme involved in the synthesis of ergosterol. Subsequent depletion of ergosterol in the fungal cell results in inhibition of fungal growth and impairment of membrane permeability. Since azoles are fungistatic, complete resolution of the infection will be aided by simultaneously addressing predisposing host factors. The two most frequently administered azole antifungals in the treatment of oral candidosis are fluconazole and itraconazole and these drugs have the advantage of being readily absorbed through the gut with the result that oral administration is an effective means of delivery (97). Furthermore, fluconazole is secreted in high levels in saliva making the agent particularly suitable for treating oral infection (98).
Unfortunately, in recent years Candida resistance to azole antifungals has been detected and this can arise through several mechanisms including the over production of the lanosterol demethylase enzyme, an alteration in the demethylase enzyme structure that makes it less susceptible to azole inhibition, the use of multi-drug transporter pumps to remove azoles from the cell, and the incorporation of alternative sterols to ergosterol within the cell membrane (99). Several NCAC species are inherently more resistant to azoles than other species. For example, 35% and 75% of C. glabrata and C. krusei isolates exhibit resistance to fluconazole and this could be a reason why the prevalence of certain NCAC species in human disease has increased in recent years (29, 100).
As the need to expand antifungal options increases, newer azole drugs such as itraconazole have been used in the treatment of oral candidosis, whilst others including voriconazole and pozoconazole are alternatives for invasive infections by Candida. Recently, the echinocandin class of antifungals have emerged as alternatives to the azoles and polyenes (101). Echinocandins act through inhibition of the D-glucan synthase, which is an enzyme required for the synthesis of the fungal cell wall. This enzyme is absent from mammalian cells thereby reducing potential host cell toxicity. Whilst echinocandins such as caspofungin, micafungin, and anidulafungin are fungicidal against Candida, their use is somewhat limited by their large molecular size that dictates the need for intravenous administration. Echinocandins are again primarily used in the treatment of invasive fungal infections.
Successful treatment of candidosis can be hampered where there is an established biofilm. Candida biofilms exhibit significantly higher tolerance to both antimicrobial mouthwashes and also traditional antifungal agents. As a consequence, alternative strategies have been suggested to combat such infections. These have included the modification of biomaterials such as those used in denture prosthesis to inhibit adherence of Candida. Examples include the use of coatings with silanes, chlorhexidine, histatins, antifungals, as well as the incorporation of surface-modifying groups (102–105). Alternative strategies could exploit quorum-sensing agents to promote biofilm disruption with the agent farnesol already having been shown to induce instability in Candida biofilms (106). Other possible strategies could involve the use of probiotics (107), which would induce an added microbiological pressure on Candida within the oral cavity and may also promote local immune function. The potential benefits of probiotics in the management of Candida biofilms have already been reported for indwelling voice box prostheses (108), as well as in lowering the Candida prevalence in the oral cavity (109).
Summary
Whilst Candida species are frequent members of the commensal oral microflora of humans, they are opportunistic pathogens that under conditions of host debilitation can cause a spectrum of oral infection. Oral candidoses have been recognised throughout recorded history, although most attention has been given to the infections in the last few decades when the incidence increased greatly with the advent and escalation of the AIDs epidemic. C. albicans is the species most frequently implicated in oral candidosis, although other species are increasingly being encountered. Putative virulence factors of Candida include the ability to adhere to host surfaces, produce filamentous growth forms, and release hydrolytic enzymes capable of inducing damage to host cells. Effective management of oral candidosis demands correction of any identified predisposing factor together with the administration of appropriate antifungal agents. Given the increasing incidence of NCAC species in oral infection and the development of resistance against some of the traditionally used antifungals, there is a constant need for research into new and effective agents to treat oral candidosis.
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
- 1.Brandão LR, Medeiros AO, Duarte MC, Barbosa AC, Rosa CA. Diversity and antifungal susceptibility of yeasts isolated by multiple-tube fermentation from three freshwater lakes in Brazil. J Water Health. 2010;8:279–89. doi: 10.2166/wh.2009.170. [DOI] [PubMed] [Google Scholar]
- 2.Hsieh CW, Huang LY, Tschen EF, Chang CF, Lee CF. Five novel anamorphic, ascomycetous yeast species associated with mushrooms and soil. FEMS Yeast Res. 2010;10:948–56. doi: 10.1111/j.1567-1364.2010.00652.x. [DOI] [PubMed] [Google Scholar]
- 3.Edelmann A, Krüger M, Schmid J. Genetic relationship between human and animal isolates of Candida albicans . J Clin Microbiol. 2005;43:6164–6. doi: 10.1128/JCM.43.12.6164-6166.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schauer F, Hanschke R. Taxonomy and ecology of the genus Candida . Mycoses. 1999;42:12–21. doi: 10.1111/j.1439-0507.1999.tb04521.x. [DOI] [PubMed] [Google Scholar]
- 5.Martins M, Henriques M, Ribeiro AP, Fernandes R, Gonçalves V, Seabra A, et al. Oral Candida carriage of patients attending a dental clinic in Braga, Portugal. Rev Iberoam Micol. 2010;27:119–24. doi: 10.1016/j.riam.2010.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Meurman JH, Pärnänen P, Seneviratne CJ, Samaranayake LP, Saarinen AM, Kari K. Prevalence and antifungal drug sensitivity of non-albicans Candida in oral rinse samples of self-caring elderly. Gerodontology. 2010 doi: 10.1111/j.1741-2358.2010.00407.x. [DOI] [PubMed] [Google Scholar]
- 7.Vanden Abbeele A, de Meel H, Ahariz M, Perraudin JP, Beyer I, Courtois P. Denture contamination by yeasts in the elderly. Gerodontology. 2008;25:222–8. doi: 10.1111/j.1741-2358.2007.00247.x. [DOI] [PubMed] [Google Scholar]
- 8.Fisher BM, Lamey PJ, Samaranayake LP, MacFarlane TW, Frier BM. Carriage of Candida species in the oral cavity in diabetic patients: relationship to glycaemic control. J Oral Pathol. 1987;16:282–4. doi: 10.1111/j.1600-0714.1987.tb01494.x. [DOI] [PubMed] [Google Scholar]
- 9.Sio JO, Minwalla FK, George RH, Booth IW. Oral candida: is dummy carriage the culprit? Arch Dis Child. 1987;62:406–20. doi: 10.1136/adc.62.4.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luque AG, Biasoli MS, Tosello ME, Binolfi A, Lupo S, Magaró HM. Oral yeast carriage in HIV-infected and non-infected populations in Rosario, Argentina. Mycoses. 2009;52:53–9. doi: 10.1111/j.1439-0507.2008.01542.x. [DOI] [PubMed] [Google Scholar]
- 11.Liguori G, Lucariello A, Colella G, De Luca A, Marinelli P. Rapid identification of Candida species in oral rinse solutions by PCR. J Clin Pathol. 2007;60:1035–9. doi: 10.1136/jcp.2006.040782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Back-Brito GN, Mota AJ, Vasconcellos TC, Querido SM, Jorge AO, Reis AS, et al. Frequency of Candida spp. in the oral cavity of Brazilian HIV-positive patients and correlation with CD4 cell counts and viral load. Mycopathologia. 2009;167:81–7. doi: 10.1007/s11046-008-9153-9. [DOI] [PubMed] [Google Scholar]
- 13.Odds FC. Candida and candidiasis. London: Balliere Tindall; 1988. [Google Scholar]
- 14.Campisi G, Panzarella V, Matranga D, Calvino F, Pizzo G, Lo Muzio L, et al. Risk factors of oral candidosis: a twofold approach of study by fuzzy logic and traditional statistic. Arch Oral Biol. 2008;53:388–97. doi: 10.1016/j.archoralbio.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Fukushima C, Matsuse H, Saeki S, Kawano T, Machida I, Kondo Y, et al. Salivary IgA and oral candidiasis in asthmatic patients treated with inhaled corticosteroid. J Asthma. 2005;42:601–4. doi: 10.1080/02770900500216259. [DOI] [PubMed] [Google Scholar]
- 16.Fukushima C, Matsuse H, Tomari S, Obase Y, Miyazaki Y, Shimoda T, et al. Oral candidiasis associated with inhaled corticosteroid use: comparison of fluticasone and beclomethasone. Ann Allergy Asthma Immunol. 2003;90:646–51. doi: 10.1016/S1081-1206(10)61870-4. [DOI] [PubMed] [Google Scholar]
- 17.Radfar L, Shea Y, Fischer SH, Sankar V, Leakan RA, Baum BJ, et al. Fungal load and candidiasis in Sjogrens syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:283–7. doi: 10.1016/s1079-2104(03)00224-5. [DOI] [PubMed] [Google Scholar]
- 18.Ohman SC, Jontell M. Treatment of angular cheilitis: the significance of microbial analysis, antimicrobial treatment, and interfering factors. Acta Odontol Scand. 1988;46:267–72. doi: 10.3109/00016358809004776. [DOI] [PubMed] [Google Scholar]
- 19.Weerasuriya N, Snape J. Oesophageal candidiasis in elderly patients: risk factors, prevention and management. Drugs Aging. 2008;25:119–30. doi: 10.2165/00002512-200825020-00004. [DOI] [PubMed] [Google Scholar]
- 20.Soysa NS, Samaranayake LP, Ellepola AN. Diabetes mellitus as a contributory factor in oral candidosis. Diabet Med. 2006;23:455–9. doi: 10.1111/j.1464-5491.2005.01701.x. [DOI] [PubMed] [Google Scholar]
- 21.Egusa H, Soysa NS, Ellepola AN, Yatani H, Samaranayake LP. Oral candidosis in HIV-infected patients. Curr HIV Res. 2008;6:485–99. doi: 10.2174/157016208786501445. [DOI] [PubMed] [Google Scholar]
- 22.Soysa NS, Samaranayake LP, Ellepola AN. Antimicrobials as a contributory factor in oral candidosis – a brief overview. Oral Dis. 2008;14:138–43. doi: 10.1111/j.1601-0825.2006.01357.x. [DOI] [PubMed] [Google Scholar]
- 23.Samaranayake LP. Nutritional factors and oral candidosis. J Oral Pathol. 1986;15:61–5. doi: 10.1111/j.1600-0714.1986.tb00578.x. [DOI] [PubMed] [Google Scholar]
- 24.Vazquez JA. Invasive fungal infections in the intensive care unit. Semin Respir Crit Care Med. 2010;31:79–86. doi: 10.1055/s-0029-1246289. [DOI] [PubMed] [Google Scholar]
- 25.de Repentigny L, Lewandowski D, Jolicoeur P. Immunopathogenesis of oropharyngeal candidiasis in human immunodeficiency virus infection. Clin Microbiol Rev. 2004;17:729–59. doi: 10.1128/CMR.17.4.729-759.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson GR, III, Patel PK, Kirkpatrick WR, Westbrook SD, Berg D, Erlandsen J, et al. Oropharyngeal candidiasis in the era of antiretroviral therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:488–95. doi: 10.1016/j.tripleo.2009.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zomorodian K, Haghighi NN, Rajaee N, Pakshir K, Tarazooie B, Vojdani M, et al. Assessment of Candida species colonization and denture-related stomatitis in complete denture wearers. Med Mycol. 2011;49:208–11. doi: 10.3109/13693786.2010.507605. [DOI] [PubMed] [Google Scholar]
- 28.Playford EG, Marriott D, Nguyen Q, Chen S, Ellis D, Slavin M, et al. Candidemia in nonneutropenic critically ill patients: risk factors for non-albicans Candida spp. Crit Care Med. 2008;36:2034–9. doi: 10.1097/CCM.0b013e3181760f42. [DOI] [PubMed] [Google Scholar]
- 29.Krcmery V, Barnes AJ. Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. J Hosp Infect. 2002;50:243–60. doi: 10.1053/jhin.2001.1151. [DOI] [PubMed] [Google Scholar]
- 30.Falagas ME, Roussos N, Vardakas KZ. Relative frequency of albicans and the various non-albicans Candida spp among candidemia isolates from inpatients in various parts of the world: a systematic review. Int J Infect Dis. 2010;14:e954–66. doi: 10.1016/j.ijid.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 31.McCullough MJ, Savage NW. Oral candidosis and the therapeutic use of antifungal agents in dentistry. Aust Dent J. 2005;50:S36–9. doi: 10.1111/j.1834-7819.2005.tb00383.x. [DOI] [PubMed] [Google Scholar]
- 32.Reichart PA, Samaranayake LP, Philipsen HP. Pathology and clinical correlates in oral candidiasis and its variants: a review. Oral Dis. 2000;6:85–91. doi: 10.1111/j.1601-0825.2000.tb00106.x. [DOI] [PubMed] [Google Scholar]
- 33.Thomas MS, Parolia A, Kundabala M, Vikram M. Asthma and oral health: a review. Aust Dent J. 2010;55:128–33. doi: 10.1111/j.1834-7819.2010.01226.x. [DOI] [PubMed] [Google Scholar]
- 34.Reichart PA. Oral manifestations in HIV infection: fungal and bacterial infections, Kaposi's sarcoma. Med Microbiol Immunol. 2003;192:165–9. doi: 10.1007/s00430-002-0175-5. [DOI] [PubMed] [Google Scholar]
- 35.Gabler IG, Barbosa AC, Velela RR, Lyon S, Rosa CA. Incidence and anatomic localization of oral candidiasis in patients with AIDS hospitalized in a public hospital in Belo Horizonte, MG, Brazil. J Appl Oral Sci. 2008;16:247–50. doi: 10.1590/S1678-77572008000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hodgson TA, Rachanis CC. Oral fungal and bacterial infections in HIV-infected individuals: an overview in Africa. Oral Dis. 2002;8:80–7. doi: 10.1034/j.1601-0825.2002.00017.x. [DOI] [PubMed] [Google Scholar]
- 37.Holmstrup P, Besserman M. Clinical, therapeutic and pathogenic aspects of chronic oral multifocal candidiasis. Oral Surg Oral Med Oral Pathol. 1983;56:388–95. doi: 10.1016/0030-4220(83)90349-3. [DOI] [PubMed] [Google Scholar]
- 38.Arendorf TM, Walker DM, Kingdom RJ, Roll JRS, Newcombe RG. Tobacco smoking and denture wearing in oral candidal leukoplakia. Br Dent J. 1983;155:340–3. doi: 10.1038/sj.bdj.4805222. [DOI] [PubMed] [Google Scholar]
- 39.Sitheeque MA, Samaranayake LP. Chronic hyperplastic candidosis/candidiasis (candidal leukoplakia) Crit Rev Oral Biol Med. 2003;14:253–67. doi: 10.1177/154411130301400403. [DOI] [PubMed] [Google Scholar]
- 40.Cawson RA, Binnie WH. Candidal leukoplakia and carcinoma. A possible relationship. In: Mackenzie IA, Dabelsteen E, Squier C, editors. Oral premalignancy. Iowa City: University of Iowa Press; 1980. pp. 59–66. [Google Scholar]
- 41.Krogh P, Hald B, Holmstrup P. Possible mycologic aetiology of oral mucosal cancer: catalytic potential of infecting Candida albicans and other yeasts in production of N-nitrosobenzylmethylamine. Carcinogenesis. 1987;8:1543–8. doi: 10.1093/carcin/8.10.1543. [DOI] [PubMed] [Google Scholar]
- 42.Dias AP, Samaranayake LP. Clinical, microbiological and ultrastructural features of angular cheilitis lesions in Southern Chinese. Oral Dis. 1995;1:43–8. doi: 10.1111/j.1601-0825.1995.tb00156.x. [DOI] [PubMed] [Google Scholar]
- 43.Reamy BV, Derby R, Bunt CW. Common tongue conditions in primary care. Am Fam Physician. 2010;81:627–34. [PubMed] [Google Scholar]
- 44.Webb BC, Thomas CJ, Willcox MD, Harty DW, Knox KW. Candida-associated denture stomatitis. Aetiology and management: a review. Part 2. Oral diseases caused by Candida species. Aust Dent J. 1998;43:160–6. doi: 10.1111/j.1834-7819.1998.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 45.Radford DR, Challacombe SJ, Walter JD. Denture plaque and adherence of Candida albicans to denture-base materials in vivo and in vitro. Crit Rev Oral Biol Med. 1999;10:99–116. doi: 10.1177/10454411990100010501. [DOI] [PubMed] [Google Scholar]
- 46.Grbic JT, Mitchell-Lewis DA, Fine JB, Phelan JA, Bucklan RS, Zambon JJ, et al. The relationship of candidiasis to linear gingival erythema in HIV-infected homosexual men and parenteral drug users. J Periodontol. 1995;66:30–7. doi: 10.1902/jop.1995.66.1.30. [DOI] [PubMed] [Google Scholar]
- 47.Velegraki A, Nicolatou O, Theodoridou M, Mostrou G, Legakis NJ. Paediatric AIDS – related linear gingival erythema: a form of erythematous candidiasis? J Oral Pathol Med. 1999;28:178–82. doi: 10.1111/j.1600-0714.1999.tb02020.x. [DOI] [PubMed] [Google Scholar]
- 48.Eyerich K, Eyerich S, Hiller J, Behrendt H, Traidl-Hoffmann C. Chronic mucocutaneous candidiasis, from bench to bedside. Eur J Dermatol. 2010;20:260–5. doi: 10.1684/ejd.2010.0910. [DOI] [PubMed] [Google Scholar]
- 49.Liu X, Hua H. Oral manifestation of chronic mucocutaneous candidiasis: seven case reports. J Oral Pathol Med. 2007;36:528–32. doi: 10.1111/j.1600-0714.2007.00572.x. [DOI] [PubMed] [Google Scholar]
- 50.Cotter G, Kavanagh K. Adherence mechanisms of Candida albicans . Br J Biomed Sci. 2000;57:241–9. [PubMed] [Google Scholar]
- 51.Hazen KC. Participation of yeast cell surface hydrophobicity in adherence of Candida albicans to human epithelial cells. Infect Immun. 1989;57:1894–900. doi: 10.1128/iai.57.7.1894-1900.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hoyer LL. The ALS gene family of Candida albicans . Trends Microbiol. 2001;9:176–80. doi: 10.1016/s0966-842x(01)01984-9. [DOI] [PubMed] [Google Scholar]
- 53.Staab JF, Bradway SD, Fidel PL, Sundstrom P. Adhesive and mammalian transglutaminase substrate properties of Candida albicans Hwp1. Science. 1999;283:1535–8. doi: 10.1126/science.283.5407.1535. [DOI] [PubMed] [Google Scholar]
- 54.Silverman RJ, Nobbs AH, Vickerman MM, Barbour ME, Jenkinson HF. Interaction of Candida albicans cell-wall Als3 protein with Streptococcus gordonii SspB adhesin promotes development of mixed species communities. Infect Immun. 2010;78:4644–52. doi: 10.1128/IAI.00685-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ramage G, Martínez JP, López-Ribot JL. Candida biofilms on implanted biomaterials: a clinically significant problem. FEMS Yeast Res. 2006;6:979–86. doi: 10.1111/j.1567-1364.2006.00117.x. [DOI] [PubMed] [Google Scholar]
- 56.Silva S, Henriques M, Oliveira R, Williams D, Azeredo J. In vitro biofilm activity of non-Candida albicans Candida species. Curr Microbiol. 2010;61:534–40. doi: 10.1007/s00284-010-9649-7. [DOI] [PubMed] [Google Scholar]
- 57.Rajendran R, Robertson DP, Hodge PJ, Lappin DF, Ramage G. Hydrolytic enzyme production is associated with Candida albicans biofilm formation from patients with type 1 diabetes. Mycopathologia. 2010;170:229–35. doi: 10.1007/s11046-010-9319-0. [DOI] [PubMed] [Google Scholar]
- 58.Nett JE, Sanchez H, Cain MT, Andes DR. Genetic basis of Candida biofilm resistance due to drug-sequestering matrix glucan. J Infect Dis. 2010;202:171–5. doi: 10.1086/651200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Crump JA, Collignon PJ. Intravascular catheter-associated infections. Eur J Clin Microbiol Infect Dis. 2000;19:1–8. doi: 10.1007/s100960050001. [DOI] [PubMed] [Google Scholar]
- 60.Verran J, Maryan CJ. Retention of Candida albicans on acrylic resin and silicone of different surface topography. J Prosthet Dent. 1997;77:535–9. doi: 10.1016/s0022-3913(97)70148-3. [DOI] [PubMed] [Google Scholar]
- 61.Sudbery P, Gow N, Berman J. The distinct morphogenic states of Candida albicans . Trends Microbiol. 2004;12:317–24. doi: 10.1016/j.tim.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 62.Jackson AP, Gamble JA, Yeomans T, Moran GP, Saunders D, Harris D, et al. Comparative genomics of the fungal pathogens Candida dubliniensis and Candida albicans . Genome Res. 2009;19:2231–44. doi: 10.1101/gr.097501.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kumamoto CA, Vinces MD. Contributions of hyphae and hypha-co-regulated genes to Candida albicans virulence. Cell Microbiol. 2005;7:1546–54. doi: 10.1111/j.1462-5822.2005.00616.x. [DOI] [PubMed] [Google Scholar]
- 64.Rindum JL, Stenderup A, Holmstrup P. Identification of Candida albicans types related to healthy and pathological oral mucosa. J Oral Pathol Med. 1994;23:406–12. doi: 10.1111/j.1600-0714.1994.tb00086.x. [DOI] [PubMed] [Google Scholar]
- 65.Morschhäuser J. Regulation of white-opaque switching in Candida albicans . Med Microbiol Immunol. 2010;199:165–72. doi: 10.1007/s00430-010-0147-0. [DOI] [PubMed] [Google Scholar]
- 66.Soll DR. Why does Candida albicans switch? FEMS Yeast Res. 2009;9:973–89. doi: 10.1111/j.1567-1364.2009.00562.x. [DOI] [PubMed] [Google Scholar]
- 67.Naglik J, Albrecht A, Bader O, Hube B. Candida albicans proteinases and host/pathogen interactions. Cell Microbiol. 2004;6:915–26. doi: 10.1111/j.1462-5822.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- 68.Hube B, Sanglard D, Odds FC, Hess D, Monod M, Schafer W, et al. Disruption of each of the secreted aspartyl protease genes SAP1, SAP2, and SAP3 of Candida albicans attenuates virulence. Infect Immun. 1997;65:3529–38. doi: 10.1128/iai.65.9.3529-3538.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chen YC, Wu CC, Chung WL, Lee FJ. Differential secretion of Sap4-6 proteins in Candida albicans during hyphae formation. Microbiology. 2002;148:3743–54. doi: 10.1099/00221287-148-11-3743. [DOI] [PubMed] [Google Scholar]
- 70.Hattori M, Yoshiura K, Negi M, Ogawa H. Keratinolytic proteinase produced by Candida albicans . Sabouraudia. 1984;22:175–83. [PubMed] [Google Scholar]
- 71.Odds FC. Pathogenesis of Candida infections. J Am Acad Dermatol. 1994;31:S2–5. doi: 10.1016/s0190-9622(08)81257-1. [DOI] [PubMed] [Google Scholar]
- 72.Gropp K, Schild L, Schindler S, Hube B, Zipfel PF, Skerka C. The yeast Candida albicans evades human complement attack by secretion of aspartic proteases. Mol Immunol. 2009;47:465–75. doi: 10.1016/j.molimm.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 73.Reinholdt J, Krogh P, Holmstrup P. Degradation of IgA1, IgA2, and S-IgA by Candida and Torulopsis species. Acta Pathol Microbiol Immunol Scand C. 1987;95:265–74. doi: 10.1111/j.1699-0463.1987.tb00040.x. [DOI] [PubMed] [Google Scholar]
- 74.Rüchel R. On the role of proteinases from Candida albicans in the pathogenesis of acronecrosis. Zentralbl Bakteriol Mikrobiol Hyg A. 1983;255:524–36. [PubMed] [Google Scholar]
- 75.Rüchel R. Cleavage of immunoglobulins by pathogenic yeasts of the genus Candida . Microbiol Sci. 1986;3:316–9. [PubMed] [Google Scholar]
- 76.Tsang CSP, Chu FCS, Leung WK, Jin LJ, Samaranayake LP, Siu SC. Phospholipase, proteinase and haemolytic activities of Candida albicans isolated from oral cavities of patients with type 2 diabetes mellitus. J Med Microbiol. 2007;56:1393–8. doi: 10.1099/jmm.0.47303-0. [DOI] [PubMed] [Google Scholar]
- 77.Schaller M, Borelli C, Korting HC, Hube B. Hydrolytic enzymes as virulence factors of Candida albicans . Mycoses. 2005;48:365–77. doi: 10.1111/j.1439-0507.2005.01165.x. [DOI] [PubMed] [Google Scholar]
- 78.Fu Y, Ibrahim AS, Fonzi W, Zhou X, Ramos CF, Ghannoum MA. Cloning and characterization of a gene (LIP1) which encodes a lipase from the pathogenic yeast Candida albicans . Microbiology. 1997;143:331–40. doi: 10.1099/00221287-143-2-331. [DOI] [PubMed] [Google Scholar]
- 79.Paraje MG, Correa SG, Albesa I, Sotomayor CE. Lipase of Candida albicans induces activation of NADPH oxidase and L-arginine pathways on resting and activated macrophages. Bioche Biophys Res Commun. 2009;390:263–8. doi: 10.1016/j.bbrc.2009.09.104. [DOI] [PubMed] [Google Scholar]
- 80.Stehr F, Felk A, Gácser A, Kretschmar M, Mähnss B, Neuber K, et al. Expression analysis of the Candida albicans lipase gene family during experimental infections and in patient samples. FEMS Yeast Res. 2004;4:401–8. doi: 10.1016/S1567-1356(03)00205-8. [DOI] [PubMed] [Google Scholar]
- 81.Luo G, Samaranayake LP, Yau JYY. Candida species exhibit differential in vitro hemolytic activities. J Clin Microbiol. 2001;39:2971–4. doi: 10.1128/JCM.39.8.2971-2974.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Manns JM, Mosser DM, Buckley HR. Production of a hemolytic factor by Candida albicans . Infect Immun. 1994;62:5154–6. doi: 10.1128/iai.62.11.5154-5156.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mukhopadhyay S, Herre J, Brown GD, Gordon S. The potential for Toll-like receptors to collaborate with other innate immune receptors. Immunology. 2004;112:521–30. doi: 10.1111/j.1365-2567.2004.01941.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bonifazi P, Zelante T, D'Angelo C, De Luca A, Moretti S, Bozza S, et al. Balancing inflammation and tolerance in vivo through dendritic cells by the commensal Candida albicans . Mucosal Immunol. 2009;2:362–74. doi: 10.1038/mi.2009.17. [DOI] [PubMed] [Google Scholar]
- 85.Jouault T, Sarazin A, Martinez-Esparza M, Fradin C, Sendid B, Poulain D. Host responses to a versatile commensal: PAMPs and PRRs interplay leading to tolerance or infection by Candida albicans . Cell Microbiol. 2009;11:1007–15. doi: 10.1111/j.1462-5822.2009.01318.x. [DOI] [PubMed] [Google Scholar]
- 86.Gil ML, Gozalbo D. Role of Toll-like receptors in systemic Candida albicans infections. Front Biosci. 2009;14:570–82. doi: 10.2741/3263. [DOI] [PubMed] [Google Scholar]
- 87.Verdijk P, Aarntzen EH, Lesterhuis WJ, Boullart AC, Kok E, van Rossum MM, et al. Limited amounts of dendritic cells migrate into the T-cell area of lymph nodes but have high immune activating potential in melanoma patients. Clin Cancer Res. 2009;15:2531–40. doi: 10.1158/1078-0432.CCR-08-2729. [DOI] [PubMed] [Google Scholar]
- 88.Del Prete A, Vermi W, Dander E, Otero K, Barberis L, Luini W, et al. Defective dendritic cell migration and activation of adaptive immunity in PI3Kgamma-deficient mice. Embo J. 2004;23:3505–15. doi: 10.1038/sj.emboj.7600361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ryan KR, Hong M, Arkwright PD, Gennery AR, Costigan C, Dominguez M, et al. Impaired dendritic cell maturation and cytokine production in patients with chronic mucocutanous candidiasis with or without APECED. Clin Exp Immunol. 2008;154:406–14. doi: 10.1111/j.1365-2249.2008.03778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Conti HR, Gaffen SL. Host responses to Candida albicans: Th17 cells and mucosal candidiasis. Microbes Infect. 2010;12:518–27. doi: 10.1016/j.micinf.2010.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Mohammadi Z, Abbott PV. The properties and applications of chlorhexidine in endodontics. Int Endod J. 2009;42:288–302. doi: 10.1111/j.1365-2591.2008.01540.x. [DOI] [PubMed] [Google Scholar]
- 92.Hope CK, Wilson M. Effects of dynamic fluid activity from an electric toothbrush on in vitro oral biofilms. J Clin Periodontol. 2003;30:624–9. doi: 10.1034/j.1600-051x.2003.00307.x. [DOI] [PubMed] [Google Scholar]
- 93.Filoche SK, Soma K, Sissons CH. Antimicrobial effects of essential oils in combination with chlorhexidine digluconate. Oral Microbiol Immunol. 2005;20:221–5. doi: 10.1111/j.1399-302X.2005.00216.x. [DOI] [PubMed] [Google Scholar]
- 94.Fine DH. Mouth rinses as adjuncts for plaque and gingivitis management. A status report for the American Journal of Dentistry. Am J Dent. 1988;1:259–63. [PubMed] [Google Scholar]
- 95.Sanglard D, Bille J. Current understanding of the modes of action of and resistance mechanisms to conventional and emerging antifungal agents for treatment of Candida infections. In: Calderone RA, editor. Candida and candidiasis. Washington, DC: ASM Press; 2002. pp. 349–83. [Google Scholar]
- 96.Andes D. In vivo pharmacodynamics of antifungal drugs in treatment of candidiasis. Antimicrob Agents Chemother. 2003;47:1179–86. doi: 10.1128/AAC.47.4.1179-1186.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nimmi M, Firth NA, Cannon RD. Antifungal drug resistance of oral fungi. Odontology. 2010;98:15–25. doi: 10.1007/s10266-009-0118-3. [DOI] [PubMed] [Google Scholar]
- 98.Force RW, Nahata MC. Salivary concentrations of ketoconazole and fluconazole: implications for drug efficacy in oropharyngeal and esophageal candidiasis. Ann Pharmacother. 1995;29:10–5. doi: 10.1177/106002809502900102. [DOI] [PubMed] [Google Scholar]
- 99.White TC, Holleman S, Dy F, Mirels LF, Stevens DA. Resistance mechanisms in clinical isolates of Candida albicans . Antimicrob Agents Chemother. 2002;46:1704–13. doi: 10.1128/AAC.46.6.1704-1713.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Redding SW, Kirkpatrick WR, Dib O, Fothergill AW, Rinaldi MG, Patterson TF. The epidemiology of non-albicans Candida in oropharyngeal candidiasis in HIV patients. Spec Care Dentist. 2000;20:178–81. doi: 10.1111/j.1754-4505.2000.tb00015.x. [DOI] [PubMed] [Google Scholar]
- 101.Bal AM. The echinocandins: three useful choices or three too many? Int J Antimicrob Agents. 2010;35:13–8. doi: 10.1016/j.ijantimicag.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 102.Chandra J, Patel JD, Li J, Zhou G, Mukherjee PK, McCormick TS, et al. Modification of surface properties of biomaterials influences the ability of Candida albicans to form biofilms. Appl Environ Microbiol. 2005;71:8795–801. doi: 10.1128/AEM.71.12.8795-8801.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Price CL, Williams DW, Waters MG, Coulthwaite L, Verran J, Taylor RL, et al. Reduced adherence of Candida to silane-treated silicone rubber. J Biomed Mater Res B Appl Biomater. 2005;74:481–7. doi: 10.1002/jbm.b.30226. [DOI] [PubMed] [Google Scholar]
- 104.Pusateri CR, Monaco EA, Edgerton M. Sensitivity of Candida albicans biofilm cells grown on denture acrylic to antifungal proteins and chlorhexidine. Arch Oral Biol. 2009;54:588–94. doi: 10.1016/j.archoralbio.2009.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Redding S, Bhatt B, Rawls HR, Siegel G, Scott K, Lopez-Ribot J. Inhibition of Candida albicans biofilm formation on denture material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:669–72. doi: 10.1016/j.tripleo.2009.01.021. [DOI] [PubMed] [Google Scholar]
- 106.Ramage G, VandeWalle K, Bachmann SP, Wickes BL, Lopez-Ribot JL. In vitro pharmacodynamic properties of three antifungal agents against preformed Candida albicans biofilms determined by time-kill studies. Antimicrob Agents Chemother. 2002;46:3634–6. doi: 10.1128/AAC.46.11.3634-3636.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Meurman JH. Probiotics: do they have a role in oral medicine and dentistry? Eur J Oral Sci. 2005;113:188–96. doi: 10.1111/j.1600-0722.2005.00191.x. [DOI] [PubMed] [Google Scholar]
- 108.Van der Mei HC, Free RH, Elving GJ, Van Weissenbruch R, Albers FW, Busscher HJ. Effect of probiotic bacteria on prevalence of yeasts in oropharyngeal biofilms on silicone rubber voice prostheses in vitro. J Med Microbiol. 2000;49:713–8. doi: 10.1099/0022-1317-49-8-713. [DOI] [PubMed] [Google Scholar]
- 109.Hatakka K, Ahola AJ, Yli-Knuuttila H, Richardson M, Poussa T, Meurman JH, et al. Probiotics reduce the prevalence of oral Candida in the elderly – a randomized controlled trial. J Dent Res. 2007;86:125–30. doi: 10.1177/154405910708600204. [DOI] [PubMed] [Google Scholar]