Abstract
Background:
Supraglottic airway devices (SADs), such as ProSealTM laryngeal mask airway (PLMA), which produce high oropharyngeal seal pressure (OSP) and have the facility for gastric decompression have been used in laparoscopic procedures. i-gel is a new SAD which shares these features with the PLMA. This study was designed to compare the respiratory mechanics of these two devices during positive pressure ventilation in anaesthetised adult patients undergoing laparoscopic cholecystectomy.
Patients & Methods:
The study included 60 ASA I-II adult patients scheduled for laparoscopic cholecystectomy. The patients were randomized to two groups of 30 each, with either PLMA or i-gel as their airway device. Anaesthesia and premedication were standardized for both the groups. In addition to routine monitoring, neuromuscular monitoring with TOF ratio, OSP and respiratory mechanics monitoring (dynamic compliance, resistance, work of breathing, measured minute ventilation and peak airway pressures) were employed. Fibreoptic evaluation of positioning of the devices and adverse events related to them were also compared.
Results:
The OSP (cm H2O) were higher for PLMA (38.9 vs. 35.6, P=0.007). The respiratory mechanics parameters using the two devices were comparable apart from the dynamic compliance, which was significantly higher with i-gel (P < 0.05). Malrotation was higher with i-gel than with PLMA (15 vs. 5, P = 0.006).
Conclusion:
The PLMA formed a better seal while the dynamic compliance was higher with the i-gel. Both devices provided optimal ventilation and oxygenation and the adverse events were also comparable.
Keywords: ProSealTM LMA, I-gel, Equipment, Masks anaesthesia, Respiratory mechanics, Laparoscopy, Ventilation
The record success of the classic laryngeal mask airway (cLMA) in resuscitation and anaesthesia, has led to the introduction of several supraglottic airway devices (SADs) into clinical practice. These devices offer several advantages over the tracheal tube (TT) with regard to ease of insertion, haemodynamic stability, favourable respiratory mechanics and decreased airway morbidity.1–5 The cLMA is the most widely studied SAD while some new products await prospective evaluation. Doubts still remain concerning the use of SADs with positive pressure ventilation (PPV) especially in laparoscopic procedures.6,7 Changes in respiratory mechanics following carboperitoneum may result in increased airway pressures that may exceed the oropharyngeal seal pressure (OSP) of the used device, leading to inadequate ventilation, gastric insufflation and increased risk of regurgitation and subsequent pulmonary aspiration. The ProSealTM laryngeal mask airway (PLMA) (Intavent Orthofix, Maidenhead, UK), and the i-gel airway (Intersurgical Ltd, Wokingham, Berkshire, UK) are two supraglottic devices introduced in 2000 and 2007 respectively. These devices provide higher OSP than the cLMA, have an additional drain tube and have been designed for use with spontaneous as well as PPV.8,9 In a recent cadaveric study, the oesophageal seal of the two devices was compared and it was reported that both devices allowed a fast and complete drainage of oesophageal fluid through the open oesophageal lumen.10 The PLMA has been used as a safe alternative to TT for many laparoscopic procedures while the i-gel is still being evaluated for its use in anaesthesia with PPV.11–13 The aim of this study was to compare the respiratory mechanics using the PLMA / i-gel in adult patients undergoing elective laparoscopic cholecystectomy.
PATIENTS & METHODS
After obtaining approval from the hospital ethics committee and written informed consent from the patients, this prospective randomized comparative study was conducted on 60 adult patients of either sex, of ASA physical status I-II, scheduled to undergo elective laparoscopic cholecystectomy under general anaesthesia. Patients with upper respiratory tract infections, anticipated difficult airway, mouth opening less than 2.5 cm, a body mass index of more than 35kg/m2, hiatus hernia, gastro-oesophageal reflux disease, non-fasting status and lung disease were excluded from the study. The patients were randomly assigned, using computer generated random numbers, to one of the two groups of 30 patients each, to be managed with either PLMA or i-gel as their airway device.
The anaesthesia technique was standardised for both groups. All patients received intravenous ranitidine 50 mg and metoclopramide 10 mg, 30 min prior to surgery and midazolam 1 mg on the operation table. In addition to standard anaesthetic monitoring, neuromuscular monitoring with TOF ratio, OSP and the respiratory mechanics parameters (dynamic compliance, resistance, work of breathing, measured minute ventilation and peak airway pressures) were monitored using the respiratory mechanics module (RESP MECH MODULES M F4RM0777G, GE Medical Systems by Novametrix Medical Systems, Wallingford, USA). Anaesthesia was administered with the patient in the supine position with the head resting on a pillow 7 cm in height. Anaesthesia was induced with fentanyl 1-2 μg kg-1 and propofol 2 mg kg-1 and maintained with propofol l50 μg kg-1 min-1 and 66% nitrous oxide in oxygen. Neuromuscular blockade was achieved with vecuronium 0.08-.1 mg kg-1 and boluses of 0.l mg kg-1were given for maintenance of neuromuscular blockade. After mask ventilation for three minutes, the appropriate sized airway device was inserted by anaesthesiologists who had performed more than 500 PLMA and 50 i-gel insertions.
Effective ventilation with the device was defined as a square wave capnograph trace and bilateral chest movements on manual ventilation. In the event of partial or complete airway obstruction or a significant air leak, the device was removed and reinserted. More than three insertion attempts with either device was considered a failure. An alternative device a tracheal tube, was used in such a situation. Both devices were inserted and fixed according to the manufacturer's instructions. The PLMA cuff was inflated to a pressure of 60 cm H2O using a cuff pressure monitor (Mallinckrodt Medical, Athlone, Ireland) and maintained at this pressure throughout the procedure. The device was connected to the closed circle breathing system (Penlon, Abingdon, made in UK, CE 0473).
After obtaining an effective airway, the OSP was determined by closing the expiratory valve of the circle system at a fixed gas flow of 5 litres mn-1and recording the airway pressure at which equilibrium was reached (maximum pressure allowed was 40 cm H2O). The presence of gas leak at seal pressure was detected as an audible sound escaping from the mouth or by the gel displacement test.8 A flexible fiberoptic scope (OLYMPUS LF-2, made in Japan) was introduced into the airway tube of the two devices, for viewing the laryngeal structures. The fiberoptic view was graded on the following scoring system; 4=vocal cords only; 3 = vocal cords plus posterior epiglottis (PE); 2=vocal cords plus anterior epiglottis (AE); 1=vocal cords not seen.14
The airway tube of the device in both the groups was connected to the respiratory sensor and the respiratory mechanics module. In both groups, the intra-abdominal pressure was held constant at 15 mm Hg by an automatic, high flow insufflation unit (Model OLYMPUS, UHI 3, made in Tokyo, Japan).
The following respiratory data were obtained: dynamic compliance, resistance, work of breathing and measured minute volume at the following time points; a) at insertion of device b) at carboperitoneum c) 10 min after carboperitoneum and d) at release of carboperitoneum. The position of the patient while taking these measurements was supine except at 10 min of carboperitoneum, when it was reverse Trendelenburg. Any regurgitation of fluid through the gastric channel or airway tube was noted.
The patient's lungs were initially ventilated (volume-controlled ventilation) with a tidal volume of 8-10 ml kg-1, a respiratory rate of 12 /minute and an inspiratory: expiratory ratio of 1:2 and fresh gas flow was 2.5 litre min-1. The inspired oxygen concentration and the ventilatory variables were monitored continuously and adjusted to maintain SpO2=95% and EtCO2 <45 mmHg. If oxygenation or ventilation failed during the procedure, the surgeon released the gas from the peritoneal cavity, following which the patient was oxygenated with 100% oxygen and the trachea intubated. After completion of the procedure, anaesthesia was discontinued and residual neuromuscular blockade was reversed with neostigmine methyl sulfate 0.05 mg kg-1 and glycopyrrolate 0.02 mg kg-1. The device was removed when the patient started responding to verbal commands. The patients were transferred to the post anaesthesia care unit where they received oxygen by ventimask and SpO2and other vital parameters were monitored upto two hours. All manipulations of the patient were halted during the measurement of respiratory mechanics. The changes in the compliance in the two groups were our primary outcome measure and the changes in the other respiratory mechanics parameters and adverse events were the secondary outcome measures. Unblinded observers collected intraoperative data and blinded observers collected postoperative data.
The primary variable was the dynamic compliance and the secondary variables were OSP, airway resistance, work of breathing, measured minute ventilation, SpO2, EtCO2, fibreoptic positioning of device and adverse events. Preliminary data from a pilot study showed that 30 patients in each group would give a power of 0.9 at an alpha level of 0.05 (two-tailed test) in order to detect a minimum of 25% difference in dynamic compliance between the i-gel and the PLMA groups. The data were analysed using SPSS software (Version 17.0, Chicago, IL, USA). Continuous variables are presented as mean SD. Categorical variables are expressed as frequencies. Differences between groups were assessed with Chi-square or fisher's exact test for categorical variables. Unpaired t tests were used for comparison of continuous variables between the two groups. A P value less than 0.05 was considered statistically significant.
RESULTS
Complete data was obtained from all patients. The patient characteristics were comparable in both the groups (Table 1). Both PLMA and i-gel could be inserted in all patients with no failures in either group. The gastric tube could be inserted through both the devices in all patients. The mean OSP (cm H2O) was higher for the PLMA Group as compared to the i-gel Group (38.9 vs. 35.6,P= 0.007).
Table 1.
Patient characteristics and periinsufflation data

The dynamic compliance was higher in the i-gel Group measured at all four points of time (Fig. 1Table 2). Throughout the surgery the resistance, work of breathing, peak airway pressures and the minute ventilation were comparable in the two groups (Fig. 2Table 2). The overall mean peak airway pressures (cm H2O) before and after carboperitoneum were (15.96 ± 3.18 vs. 14.96 ± 2.91, P= 0.21) and (21.53 ± 3.22 vs. 20.03 ± 3.71,P= 0.1) for PLMA and i-gel respectively and were comparable in the two groups (Table 1).
Figure 1.
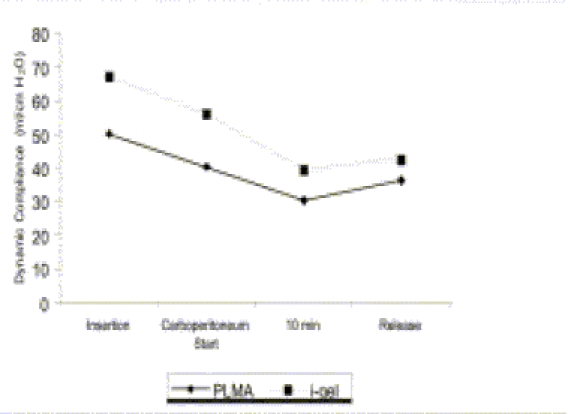
Showing mean dynamic compliance in the two groups at
a) insertion of device
b) carboperitoneum start
c) 10 min after carboperitoneum and
d) at release of carboperitoneum The dynamic compliance was higher in the i-gel Group at all four measured points.
The difference was statistically significant (*P < 0.005)
Table 2.
Comparison of respiratory mechanics and ventilatory parameters between PLMA and i-gel groups at various stages
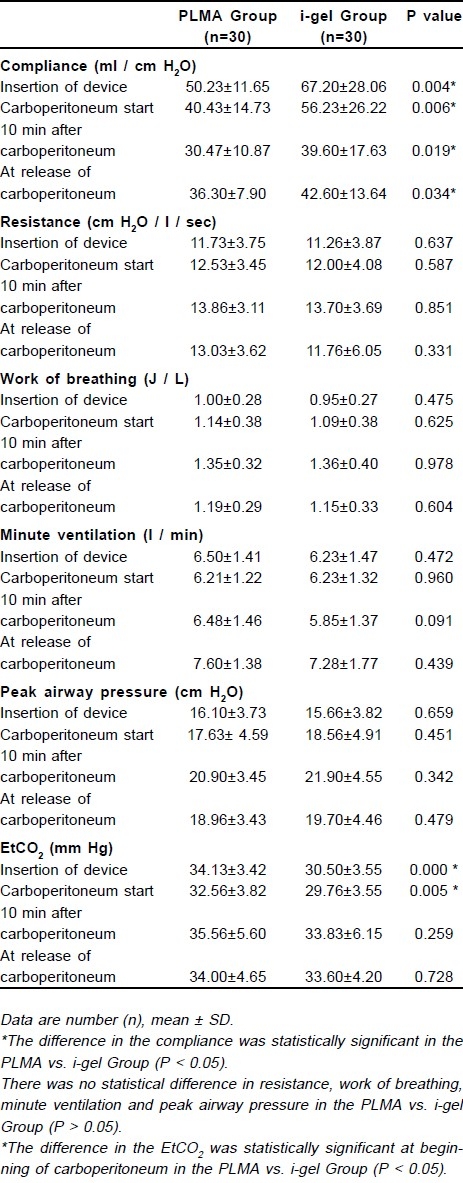
Figure 2.
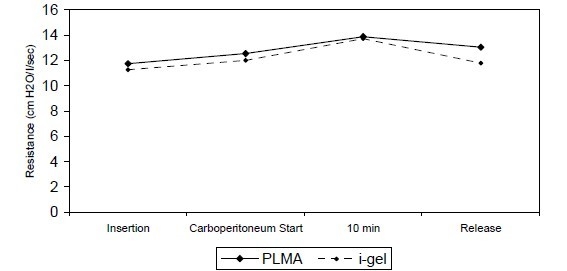
Showing mean resistance(cm H2O / l / sec) in the two groups at a) insertion of device b) carboperitoneum start c)10 min after carboperitoneum and d) at release of carboperitoneum.
The resistance was higher in the PLMA Group but it was not statistically significant (P > 0.05)
The SpO2was comparable in both the groups (Table 1) The end tidal CO2 (Table 2) was within normal limits in both the groups though higher and statistically significant at insertion (P = 0.0) and at carboperitoneum (P = 0.005) in the PLMA Group.
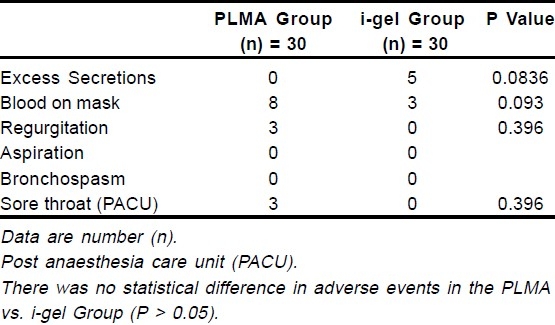
The fibreoptic grading was comparable in the two groups as shown in Table 3. Malrotation was more in i-gel Group than PLMA Group (15 vs. 5,P= 0.006). There was no significant difference in the incidence of adverse events in the two groups as shown in Table 4.
Table 3.
Fiberoptic grading through airway tube of the two devices
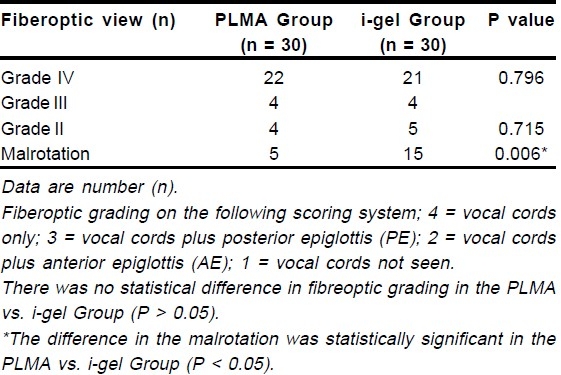
Table 4.
Adverse events
DISCUSSION
Our study demonstrated that the dynamic compliance was significantly higher in the i-gel Group. The oropharyngeal seal pressures were significantly higher for PLMA. The other respiratory mechanics parameters using the two SADs were comparable. Fiberoptic examination of the airway revealed that the incidence of malrotation of the device was higher with the i-gel. The devices were similar with respect to oxygenation and ventilation.
Laparoscopic surgery has been shown to adversely affect intraoperatve pulmonary mechanics, thus providing the most severe test of the efficacy of an airway device.12 Pulmonary compliance is decreased and the resistance is increased leading to high airway pressures.15 Therefore, higher inspiratory pressures are required to provide adequate tidal volume and minute ventilation. Intra-abdominal pressure of 15 - 20 mm Hg is associated with increase in the peak airway pressure of about 50 per cent, decrease in lung compliance by 25 per cent and an increase in PaCO2 by 10 mmHg.15–17 Consistent with these results, we observed that following carboperitoneum, compliance decreased and the peak airway pressure, resistance, work of breathing increased in both groups.
Though the PLMA and the i-gel have a separate channel for gastric tube insertion and are recommended for spontaneous as well as controlled ventilation, there are fundamental design differences between the two devices. The i-gel is cuffless, made of thermoplastic elastomer which is soft, gel-like, and transparent. It has a bigger airway tube and a narrower gastric channel allowing the passage of a smaller sized gastric tube (size 4 allows FG- 12 and size 5 permits FG-14) while the PLMA has a large, wedge shaped inflatable cuff, a narrow airway with reinforced wall tube and a relatively larger drain tube (size 4 allows FG - 16 and size 5 FG - 18 gastric tube). The cuff size and the design affect the ease of insertion and OSP whereas the diameter and the length of a tube has an important bearing on its resistance.8,9,2,18 The size for the gastric channel / drain tube will affect the size of the airway tube indirectly as well as it will have a bearing on the safety against regurgitation and aspiration. Theoretically, the narrower gastric channel of the i-gel would offer more resistance to the regurgitant fluid and increase the chances for pulmonary aspiration. Since the manufacturer's guidelines for selection of the sizes on weight basis differ in the two SADs, this could have an effect on the OSP and the respiratory mechanics.9
SADs which provide higher seal pressure and separate alimentary and respiratory tracts are desirable for laparoscopic surgery, as the seal pressure serves as an index of airway / respiratory mechanics.19 The high oropharyngeal seal pressures are necessary to deliver the required increased peak airway pressures without fear of gastric insufflation and resultant pulmonary aspiration. A study comparing oropharyngeal seal pressure in seven SADs, using cadaveric model of elevated oesophageal pressure concluded that, devices with an additional oesophageal lumen might be superior in patients with an increased risk of aspiration.20 The OSP for i-gel has been reported to be =30 cmH2O.2,13 The mean OSP was higher for PLMA signifying better protection against aspiration and better suitability in patients with low compliance or higher airway resistance. The higher seal pressure for the PLMA is most likely due to the deeper bowl, a bigger cuff with its dorsal and ventral components, the proximal wedge shape of the cuff, the corresponding larger surface area in comparison to i-gel and also due to the inflatable nature of the cuff in comparison to the cuffless i-gel.
Laparoscopic surgery entails raised intra-abdominal pressure, typically 15 mm Hg, which could possibly increase the risk of aspiration.21 There have been several successful reports of the use of the PLMA in laparoscopic cholecystectomy.12,22 The authors have used this device in more than 500 cases of laparoscopic cholecystectomies. However, there have been few reports of the safe use of other SADs in laparoscopic procedures apart from the cLMA which has been used extensively for short gynaecologic surgery.23–25 There is probably no previous report of the use of i-gel in laparoscopic procedures.
In a study comparing the respiratory mechanics of the cLMA and TT, it was observed that due to the larger diameter of the ventilatory tube of the LMA, resistance to flow and work of inspiraton were less with the cLMA as compared to the TT.4 The airway tube of the PLMA is long, narrow and wire-reinforced like that of a flexible LMA and the bowl has no grills. Another study compared the resistive loads of the PLMA with the cLMA and reported that the airway resistance is 20 % greater for the PLMA and is more like that of the flexible LMA.26 Our results are consistent with these findings. The resistance, work of breathing and peak airway pressures were higher for the PLMA Group though not statistically significant, probably because of the higher resistance offered by its comparatively narrow airway tube when compared to the wide bore airway tube of the i-gel. A 30° reverse Trendelenburg position did not have any beneficial effects on respiratory mechanics in any of the patients.
Oxygenation and ventilation were optimal in all patients throughout the surgery as well as in the postoperative period. Our results agree with those of previous work.12,22 The end tidal carbon dioxide levels were comparable in both the groups. During carboperitoneum, minute ventilation was increased mainly by increasing the respiratory rate rather than tidal volume. This was done to eliminate the raised CO2 load and prevent systemic acidosis. In a study of patients undergoing laparoscopic gastroplasty, ventilatory adjustments were performed by increasing the respiratory rate by 25% and minute ventilation by 21% to counteract the increase in CO2 load and prevent intraoperative acidosis.27
The SADs offer greater haemodynamic stability to insertion, during maintenance and at extubation when compared to the TT.19 These changes were comparable between the two groups in our study. Our study has a few limitations. Obese patients and those with restrictive lung disease were not included in the study. The PLMA may prove to be a better device because of its high seal pressure in these patients where higher airway pressures might be required. We did not perform an ABG analysis as most of our patients were healthy. Since the surgical procedures were not prolonged, we did not expect significant arterial-alveolar CO2difference.
Tracheal intubation is considered ideal for airway management in laparoscopic surgery as it provides adequate ventilation and protects against pulmonary aspiration even in the presence of raised airway pressures due to carboperitoneum. However, the device is not foolproof against aspiration and endobronchial intubation is also not uncommon during laparoscopic procedures. Moreover, this definitive airway may fail in a difficult airway scenario. The PLMA and i-gel may overcome some of these problems, even in obese patients and in those who require high airway pressures for adequate ventilation as both the devices are superior to the cLMA in these scenarios.
The higher oropharyngeal seal pressures obtained with the PLMA coupled with its larger drain tube allows the passage of a bigger gastric tube and easy fiberoptic access to the drain tube. The i-gel being disposable, offers the advantage of use in patients with hepatitis B or HIV infections and theortically avoids Prion's disease. Another advantage of the i-gel over the PLMA would be the absence of rise of intracuff pressure in the presence of nitrous oxide anaesthesia since it is cuffless.
In conclusion, though the reduction in dynamic compliance was less with the i-gel, the PLMA's higher seal pressure, lesser incidence of malrotation, a larger drain tube together with adequate and comparable mechanical ventilation and oxygenation with the i-gel may give the PLMA an edge over the i-gel as a ventilatory device in patients undergoing laparoscopic cholecystectomy. More studies with larger numbers of patients need to be carried out to confirm the findings to further widen the scope of these devices in laparoscopic surgery. We suggest that their use should be by experienced anaesthesiologists, who will assess the ventilatory capability and position of these devices carefully before proceeding with the surgery.
Authors disclosure: Authors have no conflict of interest or financial consideration.
Acknowledgments
We thank our General Surgery colleagues for their cooperation and interest.We also thank Mr. Vineet Singh, anaesthesia technician, for his valuable technical assistance during the study period & Mrs. Parul for the statistical help.
REFERENCES
- 1.Dyer RA, Llewellyn RL, James MFM. Total i.v. anaesthesia with propofol and the laryngeal mask for orthopaedic surgery. Br J Anaesth. 1995;74:123–8. doi: 10.1093/bja/74.2.123. [DOI] [PubMed] [Google Scholar]
- 2.Richez B, Saltel L, Banchereau F, Torrielli R. Cros AM A New Single Use Supraglottic Device with a Noninflatable Cuff and an Esophageal Vent: An Observational Study of the i-gel. Anesth Analg. 2008;106:1137–9. doi: 10.1213/ane.0b013e318164f062. [DOI] [PubMed] [Google Scholar]
- 3.Cork RC, Depa RM, Standen JR. Prospective comparison of use of the laryngeal mask and endotracheal tube for ambulatory surgery. Anesth Analg. 1994;79:719–27. doi: 10.1213/00000539-199410000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt SB, Kendall AP, Lin ES, Oh TE. Resistance and additional inspiratory work imposed by the laryngeal mask airway.A comparison with tracheal tubes. Anaesthesia. 1992;47:343–7. doi: 10.1111/j.1365-2044.1992.tb02179.x. [DOI] [PubMed] [Google Scholar]
- 5.Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth. 2002;88:582–4. doi: 10.1093/bja/88.4.582. [DOI] [PubMed] [Google Scholar]
- 6.Sidaras G, Hunter JM. Is it safe to artificially ventilate a paralysed patient through the laryngeal mask?.The jury is still out. Br J Anaesth. 2001;86(6):749–53. doi: 10.1093/bja/86.6.749. [DOI] [PubMed] [Google Scholar]
- 7.Cooper RM. The LMA, laparoscopic surgery and the obese patient can vs.should. Can J Anaesth. 2003;50:5–10. doi: 10.1007/BF03020178. [DOI] [PubMed] [Google Scholar]
- 8.Brain AIJ, Verghese C, Strube PJ. The LMA ‘ProSeal’-a laryngeal mask with an oesophageal vent. Br J Anaesth. 2000;84:650–4. doi: 10.1093/bja/84.5.650. [DOI] [PubMed] [Google Scholar]
- 9.i-gel user guide. 2007. http:/www.i-gel.com. -i-gel instruction manual.
- 10.Schmidbauer W, Bercker S, Volk T, Bogusch G, Mager G, Kerner T. Oesophageal seal of the novel supralaryngeal airway device I-GelTM in comparison with the laryngeal mask airways ClassicTM and ProSealTM using a cadaver model. Br J Anaesth. 2009;102(1):135–9. doi: 10.1093/bja/aen319. [DOI] [PubMed] [Google Scholar]
- 11.Piper SN, Triem JG, Rohm KD, Maleck WH, Schollhorn TA, Boldt J. ProSeal-laryngeal mask versus endotracheal intubation in patients undergoing gynaecologic laparoscopy. Anasthesiol Intensivmed Notfallmed Schmerzther. 2004;39:132–7. doi: 10.1055/s-2004-814331. [DOI] [PubMed] [Google Scholar]
- 12.Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH. The LMA-ProSealTM is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anaesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]
- 13.Uppal V, Fletcher G, Kinsella J. Comparison of the i-gel with the cuffed tracheal tube during pressure-controlled ventilation. Br J Anaesth. 2009;102(2):264–8. doi: 10.1093/bja/aen366. [DOI] [PubMed] [Google Scholar]
- 14.Keller C, Brimacombe J, Puhringer F. A fiberoptic scoring system to assess the position of laryngeal mask devices.Inter-observer variability and a comparison between the standard, flexible and intubating laryngeal mask airway. Anasthesiol Intensivmed Notfallmed Schmerzther. 2000;35:692–4. doi: 10.1055/s-2000-8164. [DOI] [PubMed] [Google Scholar]
- 15.Pelosi P, Foti G, Cereda M, Vicardi P, Gattinoni L. Effects of carbon dioxide insufflation for laparoscopic cholecystectomy on the respiratory system. Anaesthesia. 1996;51:744–9. doi: 10.1111/j.1365-2044.1996.tb07888.x. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham AJ, Brull SJ. Laparoscopic cholecyst-ectomy: anesthetic implications. Anesth Analg. 1993;76:1120–33. doi: 10.1213/00000539-199305000-00035. [DOI] [PubMed] [Google Scholar]
- 17.O'Malley C, Cunningham AJ. Physiologic changes during laparoscopy. Anesthesiol Clin N Am. 2001;19(1):1–19. doi: 10.1016/s0889-8537(05)70208-x. [DOI] [PubMed] [Google Scholar]
- 18.Nunn JF. 3rd edn. London: Butterworths & Co. Publishers; 1987. Applied Respiratory Physiology. [Google Scholar]
- 19.Brimacombe J, Keller C. The ProSeal laryngeal mask airway: a randomized, crossover study with the standard laryngeal mask airway in paralysed, anesthetized patients. Anesthesiology. 2000;93:104–9. doi: 10.1097/00000542-200007000-00019. [DOI] [PubMed] [Google Scholar]
- 20.Bercker S, Schmidbauer W, Volk T, Bogusch G, Bubser HP, Hensel M, Kerner T. A Comparison of seal in seven supraglottic airway devices using a cadaver model of elevated esophageal pressure. Anesth Analg. 2008;106:445–8. doi: 10.1213/ane.0b013e3181602ae1. [DOI] [PubMed] [Google Scholar]
- 21.Versichelen L, Serreyn R, Rolly G, Vanderkerchove D. Physiological changes during anaesthesia adminis-tration for gynaecological laparoscopy. J Reprod Med. 1984;29:697–700. [PubMed] [Google Scholar]
- 22.Lu PP, Brimacombe J, Yang C, Shyr M. ProSeal versus the Classic laryngeal mask airway for positive pressure ventilation during laparoscopic cholecystectomy. Br J Anaesth. 2002;88:824–7. doi: 10.1093/bja/88.6.824. [DOI] [PubMed] [Google Scholar]
- 23.Duffy BL. Regurgitation during pelvic laparoscopy. Br J Anaesth. 1979;51:1089–90. doi: 10.1093/bja/51.11.1089. [DOI] [PubMed] [Google Scholar]
- 24.Maltby JR, Beriault MT, Watson NC, Liepert DJ, Fick GH. LMA-Classic and LMA-ProSeal are effective alternatives to endotracheal intubation for gynecologic laparoscopy. Can J Anaesth. 2003;50:71–7. doi: 10.1007/BF03020191. [DOI] [PubMed] [Google Scholar]
- 25.Verghese C, Brimacombe JR. Survey of laryngeal mask airway usage in 11,910 patients: safety and efficacy for conventional and nonconventional usage. Anesth Analg. 1996;82:129–33. doi: 10.1097/00000539-199601000-00023. [DOI] [PubMed] [Google Scholar]
- 26.Natalini G, Rosano A, Lanza G, Martinelli E, Pletti C, Bernardini A. Resistive load of laryngeal mask airway & ProSeal laryngealmask airway in mechanically ventilated patients. Acta Anaesthesiol Scand. 2003;47(6):761–4. doi: 10.1034/j.1399-6576.2003.00133.x. [DOI] [PubMed] [Google Scholar]
- 27.Dumont L, Mattys M, Mardirosoff C, et al. Changes in pulmonary mechanics during laparoscopic gastroplasty in the morbidly obese patient. Acta Anaesthesiol Scand. 1997;41:408–13. doi: 10.1111/j.1399-6576.1997.tb04707.x. [DOI] [PubMed] [Google Scholar]


