Abstract
Background:
Laryngoscopy and intubation are associated with increase in heart rate and mean blood pressure which are deleterious for patients especially with hypertension, ischaemic heart disease, raised intraocular and intracranial pressure. This study was undertaken with an objective to determine the efficacy of nalbuphine in preventing increase in heart rate and mean arterial pressure in response to laryngoscopy and orotracheal intubation.
Patients & Methods:
A randomized controlled, prospective, double blinded study was undertaken on 60 patients ASA grade I and II posted for elective laparoscopy surgery to receive either saline (group I, control group, n=30) or Nalbuphine 0.2mg kg-1(group II, study group, n=30 ) as a bolus dose, 5 minutes before laryngoscopy. Heart rate and mean arterial pressure were taken 3 minute after study drug (T-1), just after intubation (T-2), then after every minute till 5 min (T3-7) and after 10 min of intubation (T-8). Twenty percent rise in heart rate and mean arterial pressure was considered as significant. Students ‘t’ test was used for the analysis of data by using statistical software Medcal version 11.1.1.0. and P < 0.05 was considered significant.
Results:
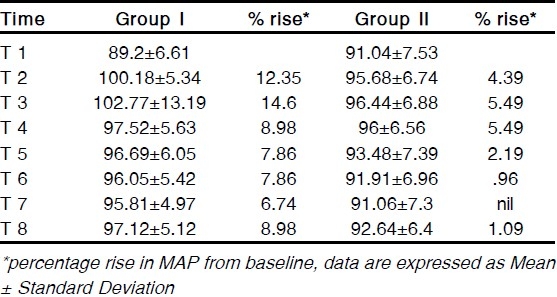
There was significant rise in heart rate(20.4%) in group I after intubation at T-2 compared with baseline at T-1 as compared to group II (16.66%). Mean arterial pressure showed rise of 12.35% in group I and 4.39% in group II at T-2 but was not significant. Heart rate and mean arterial pressure then gradually decreased from T3-8 but remained slightly higher than group II at 8th minute.
Conclusion:
We thus conclude that Nalbuphine 0.2 mg kg -1prevented a marked rise in heart rate and mean arterial pressure associated with laryngoscopy and orotracheal intubation.
Keywords: Nalbuphine, Orotracheal Intubation, Haemodynamic Response
Laryngoscopy and orotracheal intubation is associated with haemodynamic response and a rise in plasma concentrations of catecholamine like noradrenaline, adrenaline and dopamine. Rise in sympathetic hormones during intubation is associated with complications in high risk patients which can increase morbidity as well as mortality in some patients.1–5 Various drugs and induction agents like fentanyl, remifentanyl, buprenorphine, esmolol, lignocaine, thiopentone, propofol, magnesium, vasodilators, etc have been tried to prevent haemodynamic response but each drug has its own limitations.6–12
This drive led to use of nalbuphine, an agonist antagonist opioid acting on μ receptors as antagonist and ê receptor as agonist to study its haemodynamic response to orotracheal intubation. Nalbuphine is an opioid with analgesic potency equal to morphine and its antagonistic potency is approximately 1/4th that of nalorphine. Its cardiovascular stability, longer duration of analgesia, no respiratory depression, less nausea and vomiting and potential safety in overdosage makes it an ideal analgesic for use in balanced anaesthesia.13–15
PATIENTS AND METHODS
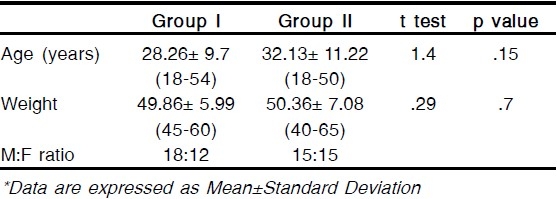
After obtaining ethical committee's approval and informed consent, 60 patients ASA grade I and II undergoing laproscopic surgery like appendicectomy, cholecystectomy and hernia repair were included in the study and were randomly distributed to either group I (saline group, n=30) or group II (study group, n=30). Patient's age, weight, gender, baseline heart rate and mean arterial pressure were similar in both groups under study. Patients with suspected difficult intubation, allergy to opioids, cardiovascular disease, hepatic or renal disease were excluded from study. All the patients were premedicated with glycopyrrolate 4μg kg-1 and midazolam 1mg IV 10 minute prior to induction of anaesthesia. All the patients were monitored for electrocardiography (ECG), HR, MAP, peripheral arterial oxygen saturation (SaO2) and capnography.
Group I received normal saline 5ml and group II received nalbuphine 0.2mg kg-1 diluted to 5 ml with normal saline 5 minutes before intubation. Double blinding was done to prevent observer's bias. Preoxygenation was then done with 100% O2. Baseline HR and MAP were recorded (T-1) 3 minute after giving nalbuphine. Anaesthesia was then induced with thiopentone (5mg kg-1) and succinylcholine (1.5mg kg-1) and orotracheal intubation then performed within 30 seconds.
HR and MAP were measured just after intubation (T-2), then after every 1 minute upto 5 minutes (T3-7) and after 10 minutes of intubation (T-8) and then patients were ventilated to normocapnia with 34% Oxygen with 66%Nitrous oxide with Vecuronium and traces of Isoflorane.
Data were analysed using student's ‘t’ test using statistical software Medcal version 11.1.1.0. and P < 0.05 was considered significant. Twenty percent rise in HR and MAP was considered as significant.
RESULTS
Patient data was almost similar in both the group. (Table 1) There was no significant difference in baseline HR (p=0.15) and baseline MAP (p=0.31) between group I and group II at T-1. Twenty percent increase in HR and MAP was taken as significant. Systolic and diastolic blood pressure reflected similar changes as MAP and so MAP was considered for analysis.
Table 1.
Patients data
HR significantly increased following intubation at T-3 (20.45%) compared with baseline readings in the group I (T-1). (Table 2) Also the rise at T-3 in group I, 20.45% was significant compared to 16.66% increase in group II. HR (T3-8) then gradually decreased in both the groups but remained higher than group II, but the rise was insignificant. In group II, HR increase at any time was also less compared to group I. The MAP also increased after intubation, 12.35% in group I and 4.39% in group II at T-2. (Table 3) But the increase in both groups was insignificant. The increase in group I was higher compared to group II at all times. MAP decreased at T-2 (14.6%) in group I to (6.74%) at T-8, but the increase was higher as compared to (5.49%) at T-2 in group II to baseline at T-8.
Table 2.
Heart rate changes
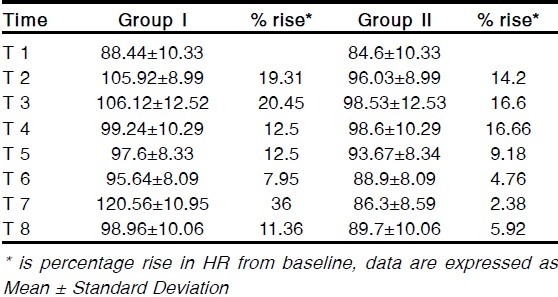
Table 3.
Mean blood pressure changes
None of the patients developed nausea, vomiting, respiratory depression, hypertension, bradycardia or tachycardia after receiving nalbuphine.
DISCUSSION
Various drugs like â blockers, vasodilators, opioids, sedatives have been tried to obtund the pressure response to intubation, but each has its own limitations.6–12 An ideal drug should have a rapid onset of action, be safe and easily administrable with a relatively short duration of action. Nalbuphine is an agonist antagonist opioid acting on μ receptors as antagonist and ê receptor as agonist with analgesic potency equal to morphine and its antagonistic potency is approximately 1/4ththat of naloxone. Nalbuphine has onset of action between 2-3 minutes, duration of action of 3-6 hours, with cardiovascular stability and minimal side effects in the dose of 0.2-0.4mg kg-1.13–15 Nalbuphine in the dose of 0.2mg kg-13-5 minutes before laryngoscopy prevented haemodynamic response associated with laryngoscopy and tracheal intubation while patients in the placebo group exhibited significant increase in HR and MAP after intubation.
Muhammed Ahsan16 has compared nalbuphine 0.2mg kg-1 with placebo. He noticed increases in HR and MAP just after induction which was significant i.e. more than 20% rise from baseline in placebo group. Our result can be compared to this study for HR increase and MBP. Our patients did exhibit rise in MAP (12.35%) in group I but was not significant. This difference can be explained by the adequate sedation effect of the premedication drug given 10 minutes before induction of anaesthesia. Rise in HR and MAP occurs due to elevations in plasma catecholamines levels which occured markedly in group I while lesser increase in HR and MAP occured following intubation in patients receiving nalbuphine.
Khan12 had compared effects of nalbuphine versus fentanyl on haemodynamic response and showed no significant increase in MAP after intubation but HR response after tracheal intubation was significantly higher in the nalbuphine group (25%) as compared to fentanyl group. He observed similar incidence of nausea and vomiting in both groups but early requirement of analgesic in recovery room in fentanyl group as the duration of analgesia was longer in nalbuphine group compared to fentanyl group (62 minutes vs 37 minutes).
Chestnutt17 had also studied effects of nalbuphine, pethidine and placebo and noticed excellent control of haemodynamic response in minor gynaecological surgery in nalbuphine as well as pethidine group, but noticed nausea and vomiting at the end of surgery which was more in pethidine group. We did not notice nausea and vomiting in our patients as the dose used was 0.2 mg kg-1compared to the higher dose used in khan12 and Chestnutt's17 study. We thereby conclude that nalbuphine (0.2mg kg-1) administered 5 minutes before laryngoscopy prevents rise in HR and MAP following laryngoscopy and endotracheal intubation.
Authors disclosure: There is no conflict of interest & financial considerations.
REFERENCES
- 1.Russell WJ, Morris RG, Frewin D B. Changes in plasma catecholamines concentration during endotracheal intubation. Br J Anaesth. 1981;53:837–9. doi: 10.1093/bja/53.8.837. [DOI] [PubMed] [Google Scholar]
- 2.Fox Elizabeth J, Garry S, Hill Constance H, Villanveva Raymond, King Benton D. Complications Related to the Pressor Response to Endotracheal Intubation. Anesthesiology. 1977;44:524–25. doi: 10.1097/00000542-197712000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Lindgren L, Yli Hankala A, Randell T, Kirvela M, Scheinin M, Neuvonen PJ. Haemodynamic and catecholamine responses to induction of anaesthesia and tracheal intubation: comparison between propofol and thiopentone. Br J Anaesth. 1993;70:306–10. doi: 10.1093/bja/70.3.306. [DOI] [PubMed] [Google Scholar]
- 4.Edwards ND, Afford AM, Dobson PMS. Myocardial ischaemia during tracheal intubation and extubation. Br J Anaesth. 1994;73:537–9. doi: 10.1093/bja/73.4.537. [DOI] [PubMed] [Google Scholar]
- 5.Derbyshire DR, Chmielawski A, Fell D, Vater M, Achola K, Smith G. Plasma catecholamine responses to tracheal intubation. Anesth Analg. 1983;55:855–60. doi: 10.1093/bja/55.9.855. [DOI] [PubMed] [Google Scholar]
- 6.Maguire M, Kumar N, Parker JL, Rowbotham DJ, Thompson JP. Comparison of effects of remifentanil and alfentanil on the cardiovascular response to tracheal intubation in hypertensive patients. Br J Anaesth. 2001;86:90–93. doi: 10.1093/bja/86.1.90. [DOI] [PubMed] [Google Scholar]
- 7.Martineau RJ, Tousignant CP, Miller DR. Alfentanil controls the hemodynamic response during rapid sequence induction of anaesthesia. Can J Anaesth. 1990;37:755–61. doi: 10.1007/BF03006534. [DOI] [PubMed] [Google Scholar]
- 8.FA Khan, RS Kamal. Effect of Buprenorphine on the cardiovascular response to tracheal intubation. Anaesthesia. 1989;44:394–97. doi: 10.1111/j.1365-2044.1989.tb11336.x. [DOI] [PubMed] [Google Scholar]
- 9.Jain PN, Divatia JV, Manjshree SS, Chatopadhyay G, Shah SC. Intravenous magnesium inhibits pressure response to nasotracheal intubation. J Anaesth Clin Pharmacol. 1995;11:59–62. [Google Scholar]
- 10.Minal FN, Khan FA. A comparision of morphine and nalbuphine for intraoperative and postoperative analgesia. J Pak Med Assoc. 2003;53:391–6. [PubMed] [Google Scholar]
- 11.Beaver WT, Felse GA. A comparison of the analgesic effect of intramuscular nalbuphine and morphine in patients with postoperative pain. J Pharmacol Exp Ther. 1978;204:486–96. [PubMed] [Google Scholar]
- 12.Khan FA, Hameedullah Comparison of fentanyl and nalbuphine in total intravenous anaesthesia (TIVA) J Pak Med Assoc. 2002;52:459–65. [PubMed] [Google Scholar]
- 13.Fragen RJ, Caldwell N. Acute intravenous premedication with nalbuphine. Anesth Analg. 1977;56:808–12. doi: 10.1213/00000539-197711000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Klepper ID, M Rosen, MD Vickers, Mapleson WW. Respiratory function following nalbuphine and morphine in anaesthetized man. Br J Anaesth. 1986;58:625, 29. doi: 10.1093/bja/58.6.625. [DOI] [PubMed] [Google Scholar]
- 15.Lake CL, Duckworth EN, Difazio CA, Magruder MR. Cardiorespiratory effects of nalbuphine and morphine premedication in adult cardiac surgical patients. Acta Anaesthesiol Scand. 1984;28:305–9. doi: 10.1111/j.1399-6576.1984.tb02066.x. [DOI] [PubMed] [Google Scholar]
- 16.Muhammed Ahsan, Etizaz Haider Kazmim, Zahid Akhtar Rao N. Nalbuphine prevents haemodynamic response to endotracheal intubation. J Coll Physicians Surg Pak. 2005;15:668–70. [PubMed] [Google Scholar]
- 17.Chestnutt WN, Clarke RSJ, Dundee JW. Comparision of nalbuphine, pethidine and placebo as premedication for minor gynaecological surgery. Br J Anaesth. 1987;59:576–80. doi: 10.1093/bja/59.5.576. [DOI] [PubMed] [Google Scholar]


