Abstract
Background:
A double blind randomized prospective study was undertaken to determine the effect of adjuncts like epinephrine 200μg or clonidine 90μg in combination of bupivacaine and lignocaine into the brachial plexus sheath to study the sensory and motor onset, duration of analgesia, hemodynamic changes and adverse effects.
Patients & Methods:
60 patients aged 18-65 years, with ASA grade I and II were randomly divided into group I and group II to receive 10 ml of lignocaine2% and 20 ml of bupivacaine0.5% with 1ml of 200μg epinephrine or 90μg clonidine respectively. Onset of sensory blockade was determined by pinprick method by a three point score and motor blockade by three point scale. Duration of postoperative analgesia, the hemodynamic changes, sedation scores and any adverse effects were observed. Statistical analysis was done by student's “t” test and p<0.05 was considered significant.
Results:
It was found that there was faster onset of sensory and motor blockade, the postoperative analgesia was prolonged and the amount of sedation was profound in group II as compared to group I. All the above findings were statistically significant.
Conclusion:
We thereby conclude that clonidine 90μg is a better option as an additive than epinephrine 200μg for hastening the onset of sensory and motor block with prolonged postoperative analgesia and sedation as the only adverse effect.
Keywords: Supraclavicular brachial plexus block, Clonidine, Epinephrine
Brachial plexus block was first performed by Halsted in 1884.1 The supraclavicular approach of the brachial plexus block has many advantages over other approaches like it provides most complete and reliable anaesthesia for the upper limb surgery and provides excellent anaesthesia for elbow, forearm and hand surgery. Addition of epinephrine appears to be the most widely used additive to local anaesthetic to prolong anaesthesia. Many additives have been tried and this search led us to try an á2 agonist like clonidine in the dose of 90μg as an additive to local anaesthetic comparing it with adrenaline 200 μg. Many theories have been postulated like clonidine may interfere with the vascular resorption of local anaesthetics by producing vasoconstriction2 or clonidine may have a direct action on neural tissues3, especially at spinal level or it may induce analgesia via a systemic mechanism after vascular resorption and secondary distribution to the brainstem4. Direct action of alpha adrenergic agonists on neural tissues i.e. á2 type receptors is suggested as clonidine when injected at peripheral nerve site has obtained earlier onset of analgesia which lasted longer than obtained with epinephrine.3–11
The purpose of this randomized double blind study was to compare additives like epinephrine or clonidine to local anaesthetics for onset of sensory and motor block, duration of analgesia, the hemodynamic changes, level of sedation and complications in brachial plexus block.
PATIENTS AND METHODS
60 ASA physical status I and II, aged 18-65 years of either sex undergoing orthopaedic upper limb surgical procedure were included in this study after approval of local ethical committee and obtaining informed consent. Patients with history of cardiac, respiratory, liver and renal problems, pregnant women, coagulative disorders, drug allergy or sensitivity to drugs, cutaneous infection at the site of injection site were excluded from the study. All the patients were fasted for 6 hours before surgery. 18 G intravenous cannula was inserted on contralateral arm and premedication consisted of Inj. Glycopyrollate 0.2 mg intravenously 15 minutes before giving the block. The patients were randomly alloted to two groups of 30 patients each. Supraclavicular brachial plexus block was then performed by the same experienced anaesthesiologist using classical approach with 10ml 2% lignocaine and 20ml 0.5% bupivacaine. Local anaesthetic was supplemented with 1ml of either 200μg of epinephrine (group I) or 90μg of clonidine (group II). Two anaesthetist were involved to perform a double blind study and prevent observer's bias. Preoperative antianxiety and sedative drugs were avoided to study the sedative effect of the additive drug.
Following criteria were assessed in the operating room
(i) the time to onset of sensory blockade according to a three point score by pinprick method:
Grade-0: Anaesthesia- no sensation felt
Grade-1: Analgesia - dull sensation felt
Grade-2: Sharp pain felt.
Sensory score of 2 was taken as time to onset of sensory block.
(ii) the time to onset of motor blockade according to a three point scale:
Grade - 0: Complete paralysis
Grade - 1: Paresis
Grade - 2: Normal muscle force.
Motor score of 2 was taken as onset time of complete motor block. Onset of block was monitored every one minute for 20 minutes. Heart rate, blood pressure, SpO2 were measured before anaesthesia(baseline), at premedication, in operation theatre T0, at 5 minutes i.e. T5, T10, T15, T20, T25, T30, T45, T60, T75, T90, T105, T120 and postoperatively at 15, 30, 45 and 60min, 2, 3, 5, 8, 12, 15 and18 hours. The quality of analgesia was assessed during surgery and in the postoperative period assessed according to a VAS score. When patient began to experience pain more than 5 on the VAS (0 being no pain and 10 being unbearable pain), it was considered that the analgesic action of the drug has terminated and additional analgesic was given. Hemodynamic changes, level of sedation, any other complications were noted. Sedation score was assessed by using the sedation scale described by Culebras12 for 8 hours postoperatively:
Grade 1 - awake and alert
Grade 2 - sedated, responding to verbal stimulus
Grade 3 - sedated, responding to mild physical stimulus
Grade 4 - sedated, responds to moderate or severe physical stimulus.
Observations recorded were tabulated and were expressed as mean ± standard deviation and compared using student's ‘t’ test by Medcalc software version 11.1.1.0. Significance was assumed if p<0.05.
RESULTS
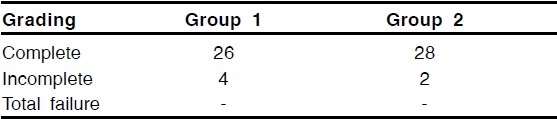
There were no significant differences between the two groups regarding sex, height and weight of the patients and in the duration of surgery (Table- 1). Onset of motor and sensory block were earlier in group II (Table- 2). Also the total duration of analgesia was longer in group II than in group I (760±65.60 vs 829.3±95.08, p<.01) (Table-3). No differences were noted in the hemodynamic parameters during surgery (Table-456) (Fig- 123) however the sedation score was significant (p<.001) between two group after 30 min and remained so for 8 hours postoperatively (Table- 7 (Fig-4). No side effects were noted in either group. 4 patients in group I and 2 patients in group II had inadequate blockade and had to be supplemented with Inj. midazolam and Inj. propofol (Table-8).
Table 1.
Patients Characteristics and Duration of Operation
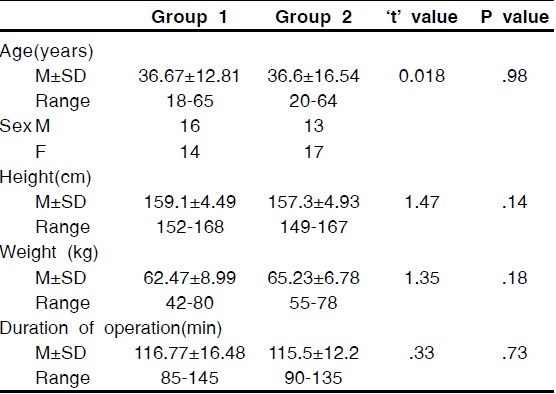
Table 2.
Onset of Sensory Block and Motor Blockade (Seconds)
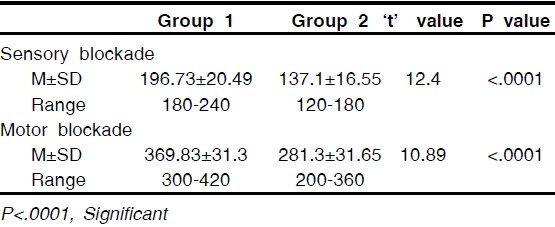
Table 3.
Duration of Analgesia (Minutes)
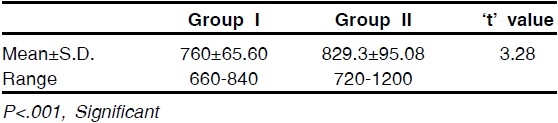
Table 4.
Systolic Blood Pressure Changes
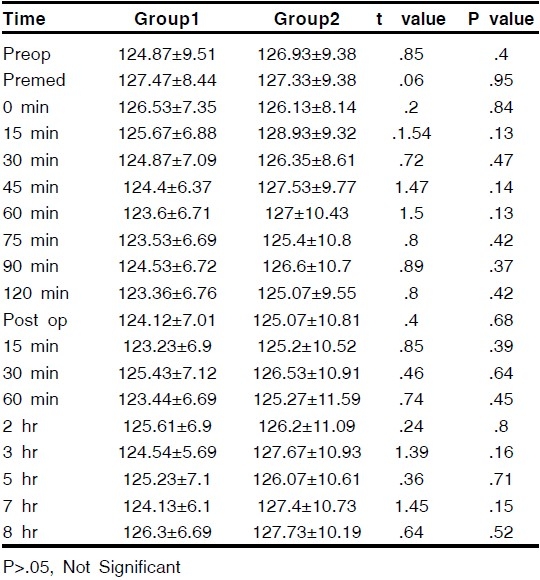
Table 5.
Diastolic Blood Pressure Changes
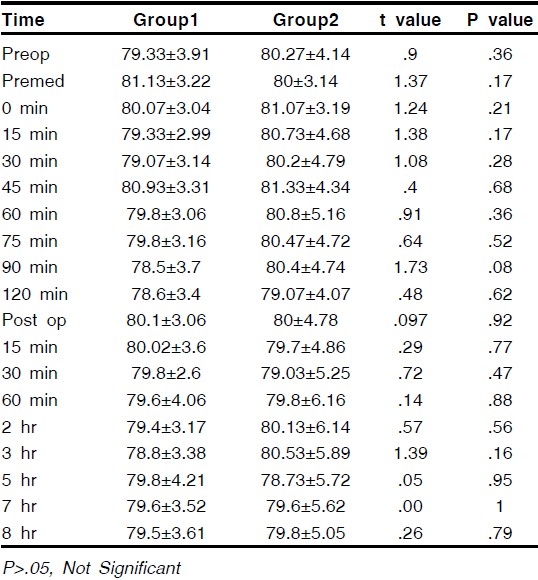
Table 6.
Pulse Rate Changes
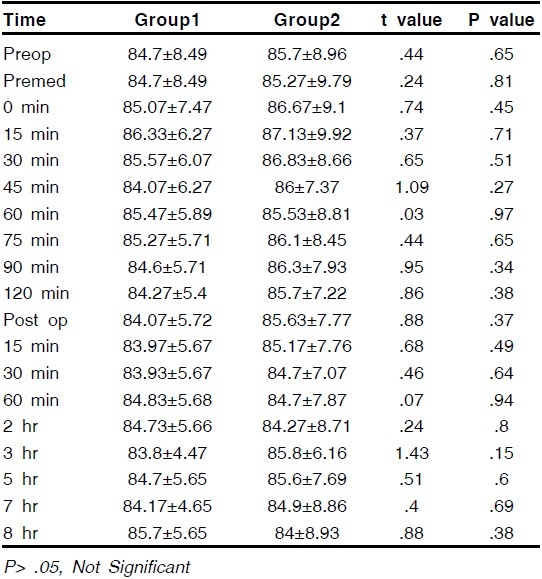
Figure 1.
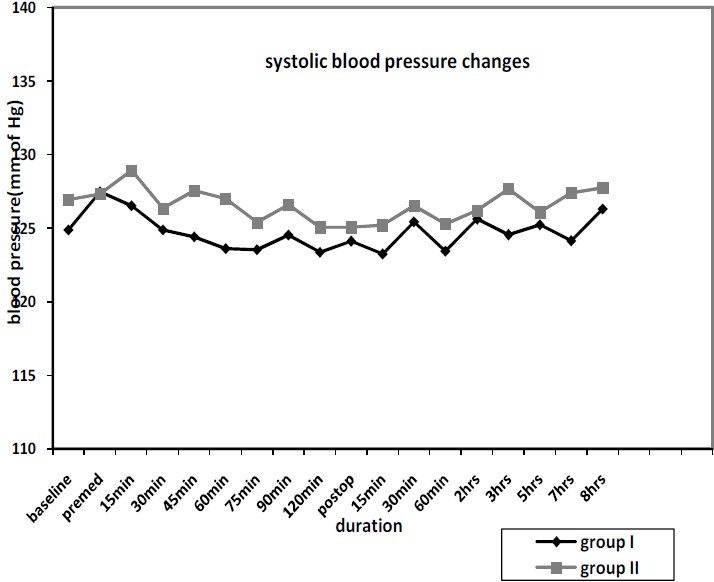
Systolic blood pressure changes
Figure 2.
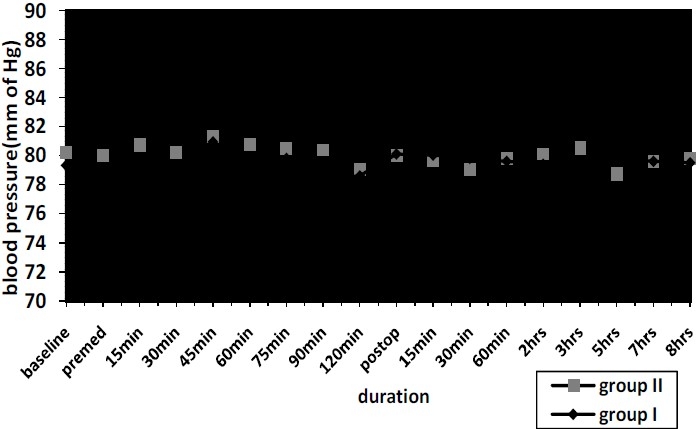
Diastolic blood pressure changes
Figure 3.
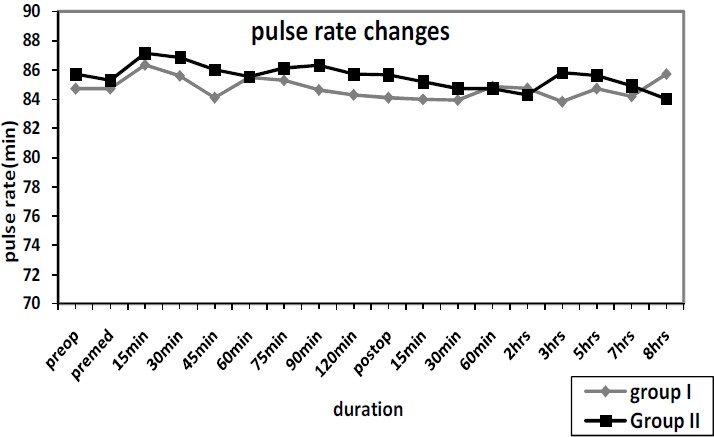
Pulse rate changes
Table 7.
Sedation Score
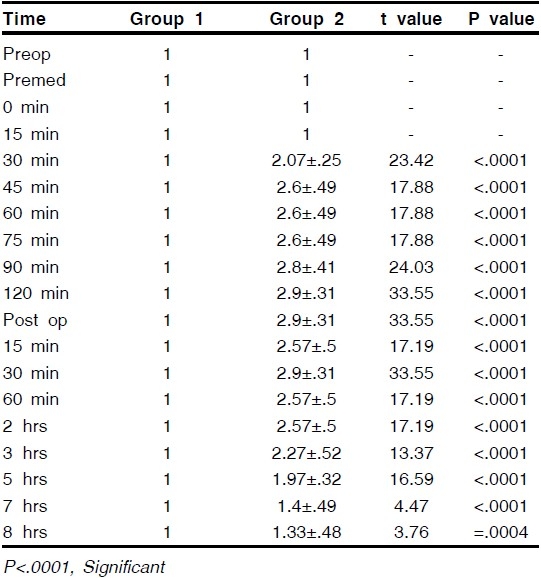
Figure 4.
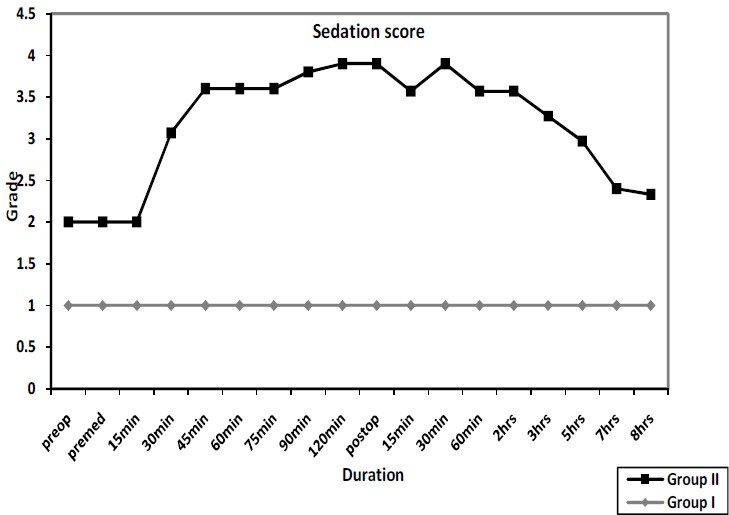
Sedation score
Table 8.
Adequacy of Analgesia
DISCUSSION
This study demonstrates that when clonidine was added to combination of lignocaine and bupivacaine and injected into the brachial plexus sheath, it resulted in earlier sensory and motor onset and longer analgesia than when epinephrine was added. This result is in agreement with Goldfarb G9 and Bernard's13 study where different concentrations of clonidine were used in axillary plexus block with lignocaine. It is difficult to define the duration of analgesia, however we relied on our patient's tolerance to pain to define the end of analgesia which varied markedly among patients. Duration of analgesia suggested prolongation in clonidine group which are in agreement with Jean's14 study using clonidine in brachial plexus block. Their duration in clonidine group was longer than our group which can be explained by the difference in the clonidine dose used i.e.150μg. This is comparable with Bernard's13 study showing dose dependant prolongation of analgesia, reaching a mean of 770 min for 300μg group. Bernard's13 study concluded that the best dose of clonidine to be used clinically is between 30 μg and 90 μg and the side effects of α2 agonist limits itself only to sedation in this dose which is comparable with our study. Though there was profound sedation in some patients, no episode of decrease in SpO2 was noted suggesting 90μg to be advantageous dose as compared to higher doses used. Bernard13 used various concentrations of clonidine and noticed fall in SpO2 levels only in 300 μg group. Clonidine did not produce any significant hemodynamic changes suggesting no side effects with use of clonidine in 90μg. This is in agreement with Jean's14 study with 150 μg clonidine in brachial plexus block. Also Colin's review15 suggested limited side effects at doses of clonidine upto 150μg. Bernard13 observed significant fall in systolic blood pressure, diastolic blood pressure and pulse rate at 300 μg while in smaller doses no hemodynamic changes were noted. 4 patients in clonidine group and 2 in epinephrine group had inadequate block. This can be compared to Bernard's13 study which showed incomplete blocks in saline as well as clonidine groups. Clonidine produces analgesia in animals and humans via a non opiate action on the α2 receptors of the dorsal horn of the spinal cord3. The prolongation of the duration of analgesia by clonidine when injected at a peripheral nerve site is not known. Many theories have been postulated like (1) clonidine may interfere with the vascular resorption of local anaesthetics by producing vasoconstriction but Gaumann16 noticed that peak plasma concentration of lidocaine were higher and occurred earlier than in those treated with epinephrine which indicates the absence of a local vasoconstrictor effect of clonidine. (2) clonidine may have a direct action on neural tissues, especially at spinal level. Hutscala17 observed that duration of action of brachial plexus block got prolonged with addition of clonidine while it did not got prolonged in the group receiving intramuscular clonidine. (3) it may induce analgesia via a systemic mechanism after vascular resorption and secondary distribution to the brainstem18.
To conclude, our study suggests that a small dose of clonidine produced early sensory and motor onset with enhancement of the quality of the peripheral block from local anaesthetics and limits its α2 side effects to sedation. Also the addition of clonidine produced longer duration of analgesia than with epinephrine when injected into the brachial plexus block. Thus clonidine in smaller concentration remains an attractive option to prolong analgesia in the postoperative period under brachial plexus block.
REFERENCES
- 1.Halstead Crile. 7th ed. London: Lioyd Luke; 2003. Great moments in the history of anaesthesiology in a practice of anaesthesia; p. 8. [Google Scholar]
- 2.Cousins MJ, Bridenbaugh PO. Neural blockade in clinical anesthesia and management of pain, Philadel-phia: J B Lippincott. 1987:111–44. [Google Scholar]
- 3.Collins JG, Kitaheta LM, Matsumoto M, Homma E, Suzukawa M. Spinally administered epinephrine sup-presses noxiously evoked activity of wide dynamic range neurons in the dorsal horn. Anesthesiology. 1984;60:269–75. doi: 10.1097/00000542-198404000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Fletwood Walker AM, Mitchell R, Hope P S, Molony V, Igoo A. An alpha 2 receptor mediates the selective inhibition by noradrenaline of nociceptive responses of identified dorsal horn neurons. Brain Res. 1985;334:243–54. doi: 10.1016/0006-8993(85)90216-1. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan A F, Dashwood M R, Dickenson A H. Alpha 2 adrenoceptor modulation of nociception in rat spinal cord: location, effects and interactions with morphine. Eur J Pharmacol. 1987;138:169–77. doi: 10.1016/0014-2999(87)90430-4. [DOI] [PubMed] [Google Scholar]
- 6.Ossipov M H, Suarez L J, Spaulding T C. Antinociceptive interactions between alpha 2 adrener-gic and opiate agonists at the spinal level in rodents. Anesth Analg. 1989;68:194–200. [PubMed] [Google Scholar]
- 7.Luttinger D, Ferrari R, Perrone M H, Haubrich D R. Pharmacological analysis of alpha 2 adrenergic mecha-nisms in nociception and ataxia. J Pharmacol Exp Ther. 1985;68:883–9. [PubMed] [Google Scholar]
- 8.Goldfarb G, Ang E T, Debaene B, Galet C, Jolis P. Duration of analgesia after femoral nerve block with bupivacaine: effect of clonidine added to the anesthetic solution. Anesthesiology. 1989;71:A643. [Google Scholar]
- 9.Goldfarb G, Ang E T, Debaene B, Delefosse D, Jolis P. Duration of analgesia after femoral nerve block with lidocaine: effect of clonidine added to the anesthetic solution. Anesthesiology. 1989;71:A644. [Google Scholar]
- 10.Wing L M H, Reid J L, Hamilton C A, Server P, Davies D S, Dollery C T. Effects of clonidine on biochemical indices of sympathetic function and plasma rnin activity in normotensive man. Clin Sci. 1977;53:45–53. doi: 10.1042/cs0530045. [DOI] [PubMed] [Google Scholar]
- 11.Kunos G, Farsang C, Ramirez-Gonzalez M D. Beta-endorphin:possible involvement in the anti-hyperten-sive effect of central alpha-receptor activation. Science. 1981;211:82–4. doi: 10.1126/science.6108611. [DOI] [PubMed] [Google Scholar]
- 12.Culebras X, Van Gessel E, Hoffmeyer P, Gamulin Z. Clonidine combine with a long acting local hemody-namic changes. Anesth Analg. 2001;92:199–204. doi: 10.1097/00000539-200101000-00038. [DOI] [PubMed] [Google Scholar]
- 13.Bernard Jean Marc, Marcaire, Philippe Dose range effects of clonidine added to lidocaine for brachial plexus block. Anesthesiology. 1997;87:277–84. doi: 10.1097/00000542-199708000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Jean J, Eledjam, Jacques, Deschodt, Viel Eric J, Lubrano Jean F, Chararel Pierre, Francoise Brachial plexus block with bupivacaine : effects of added alpha-adrenergic agonists: comparison between clonidine and epinephrine. Can J Anaesth. 1991;38:870–75. doi: 10.1007/BF03036962. [DOI] [PubMed] [Google Scholar]
- 15.Colin Mc Cartney, Edel Duggan, Emma Apatu. Should we add clonidine to local anaesthesia for peripheral nerve blockade. Reg Anesth Pain Med. 2007;32:330–38. doi: 10.1016/j.rapm.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Gaumann D. Comparison between clonidine and epi-nephrine admixture to lidocaine in brachial plexus block. Anesth Analg. 1992;75:69–74. doi: 10.1213/00000539-199207000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Hutschala D, Mascher H, et al. Clonidine added to bupivacaine enhances and prolongs analgesia after brachial plexus block via a local mechanism in healthy volunteers. Eur J Anaesth. 2004;21:198–204. doi: 10.1017/s0265021504003060. [DOI] [PubMed] [Google Scholar]
- 18.Eisenach James C, De Kock Marc, Klimscha Watter. Alpha sub 2 adrenergic agonists for regional anaes-thesia : A clinical review of clonidine (1984-1995) An-esthesiology. 1996;85:655–74. doi: 10.1097/00000542-199609000-00026. [DOI] [PubMed] [Google Scholar]


