Abstract
Background
In a prospective study of primary care patients with diabetes we determined whether macrovascular or microvascular events or coronary, cerebrovascular or peripheral vascular procedures during follow-up were associated with meeting criteria for major depression at 5-year follow-up.
Design, Patients and Measurements
A total of 2759 patients with diabetes mellitus were followed over a 5-year period. Evidence of macrovascular and microvascular events and coronary, cerebrovascular and peripheral vascular procedures was assembled from automated data using ICD-9 and CPT codes and was verified by chart review. Depression was measured using the Patient Health Questionnaire.
Results
After controlling for baseline severity of depression symptoms and history of depression, having 1 or more coronary procedures during follow-up, and baseline severity of diabetes symptoms were strong predictors of having major depression at 5-year follow-up.
Conclusions
The risk of major depression among persons with diabetes is increased by prior depression history, baseline diabetes symptoms, and cardiovascular procedures.
Introduction
A bidirectional adverse interaction has been hypothesized in patients with comorbid depression and diabetes.1 In patients with diabetes, comorbid depression has been shown to be associated with increased medical symptom burden2, additive functional impairment3, 4, poor self care (i.e. adherence to diet, exercise, disease control medication, and cessation of smoking recommendations)5, increased risk of macrovascular and microvascular complications6, higher medical costs7 and greater mortality8, 9. Incident diabetes complications and resulting functional impairment may also provoke depressive episodes.1 Moreover, macrovascular complications such as stroke and heart attack may raise cytokine levels, thereby, increasing the risk of depressive illness.10
Most studies exploring interactions between diabetes and depression have been cross-sectional6 limiting determinations of causality. Moreover, most studies that are longitudinal have examined the pathway between depression at baseline and complications, disability and mortality8, 9, but not the pathway between complications and subsequent depression. The Pathways Follow-up Study is a 5-year prospective study of a large cohort of patients with diabetes enrolled in a Health Maintenance Organization (HMO).11 For this paper we examined the association of baseline depressive symptoms, initial medical disease severity, subsequent macrovascular and microvascular complications, and coronary, cerebrovascular and peripheral vascular procedures over a 5-year period with depression status at 5 year follow-up in a large cohort of patients with diabetes. We hypothesized that, after controlling for baseline depression and history of depression, subsequent macrovascular and microvascular complications and subsequent coronary, cerebrovascular and peripheral vascular procedures would be associated with meeting DSM-IV criteria for major depression at 5 years.
Methods
Setting
Group Health (GH) is a mixed model prepaid health plan serving about 500,000 members in Washington State. Most GH patients receive medical services within the integrated group practice which includes 30 primary care clinics in Western Washington. The GH enrollment is demographically similar to the area population. Nine GH primary care clinics were selected for the study based on: 1) having the largest number of patients with diabetes; 2) geographical proximity to Seattle; and 3) racial and ethnic diversity. All study procedures were approved by institutional review boards at GH and University of Washington.
Study Cohort Selection
The original cohort for this longitudinal survey (Pathways Epidemiology Study) was sampled from adults 18 years of age or older from the GH diabetes registry who received care at any one of the 9 study clinics between 2000-2002. The diabetes registry database includes all GH members meeting any of the following eligibility criteria in the prior 12 months: filled prescription for insulin or an oral hypoglycemic agent, two fasting glucose levels ≥ 126 mg/dl in a 12 month period, two random plasma glucose levels ≥ 200mg/dl in a 12 month period, two outpatient diagnoses of diabetes, or any inpatient diagnosis of diabetes.12 Beginning in March 2001, surveys were mailed to 9064 potentially eligible patients, but 1222 patients were later found to be ineligible due to death, disenrollment, erroneous diagnosis of diabetes or cognitive impairment. Among 7841 eligible patients, 4839 subjects (61.7% of eligible patients) returned the baseline questionnaire. All surviving patients (N = 4239) who didn't request no further contact (N = 598 deaths, 2 requested no contact) were approached by the GH telephone survey team approximately 5 years after baseline interview.
Assessment of Depression, Clinical Variables, Events, and Procedures
The Patient Health Questionnaire (PHQ-9) was used to screen for depression at both baseline and 5 year follow-up.13, 14 This questionnaire provides both a dichotomous diagnosis of major and minor depression and a continuous severity score. The PHQ-9 diagnosis of major depression has been found to have an adequate sensitivity (73%) and high specificity (98%) in relation to a diagnosis of major depression based on structured interviews.13, 14 A score of ≥ 10 out of a possible 27 points has been recommended as the optimum cutoff for major depression; while a score of 5 to 9 has been the range recommended to define minor depression.14 History of depression was derived from ICD-9 codes for depression in the 18 months prior to screening. A total of 329 patients scoring ≥ 10 on the PHQ were randomized to a depression intervention versus usual care study.15 Analyses reported in this paper controlled for intervention/control group status.
The nine-item version of the Self-Completion Patient Outcome Instrument16 measured the following diabetes symptoms: cold hands and feet, numb hands and feet, polyuria, excessive hunger, abnormal thirst, shakiness, blurred vision, feeling faint and feeling sleepy. Items were rated on a Likert scale from “never” to “every day”. A positive symptom was defined as a symptom that was experienced at least “several days” in the past month. The instrument has been shown to have satisfactory internal consistency, test-retest reliability and responsiveness to change following treatment of diabetes.16 We added one item, pain in hands and feet, based on the perceived importance of these symptoms of neuropathy.
The baseline questionnaire included questions on age, sex, years of education, employment, race/ethnicity, marital status, height and weight. Questions about clinical status and health habits included: age of onset and duration of diabetes, type of treatment at onset of disease, smoking, and usual exercise. Exercise levels were measured using the Summary of Diabetes Self-Care Activities Scale that measured the number of days in the last week that the patient exercised.17 Patients were classified as having type 1 diabetes if onset was prior to 30 years of age and insulin was the first treatment prescribed.
Computerized pharmacy records were used to compute a chronic disease score (Rx Risk), a measure of medical comorbidity based on prescription drug use in the previous 12 months.18 Rx Risk has been shown to predict subsequent hospitalization and mortality rates over the next one-year period.18 A measure using automated data was used to code for 7 types of diabetes complications present at baseline: retinopathy, neuropathy, nephropathy, cerebrovascular, cardiovascular, peripheral vascular and metabolic.19 This diabetes complication measure has been shown to predict mortality and hospitalization rates over the next one year period.19 GH automated data on HbA1c levels were collected for the 18 months before the return date of the mailed screening questionnaire. The HbA1c level closest in time before the return date of the screening questionnaire was used in the analysis. A physician ICD-9 diagnosis of hypertension in the 18 months prior to baseline was identified by review of automated data.
Evidence of macrovascular and microvascular complications and coronary procedures (coronary artery bypass surgery, angioplasty, or stent placement), cerebrovascular procedures (carotid endarterectomy) and peripheral vascular procedures (angioplasty or major vascular surgery of the aorta or peripheral vasculature) were identified both before baseline and during follow-up from automated medical records data using ICD-9 and CPT codes. Macrovascular events including myocardial infarction, stroke, and peripheral vascular disease were verified by chart review. The specific codes and definitions for myocardial infarction, stroke, and coronary procedures were adopted from the Women's Health Initiative study, with the addition of CPT codes that have come into use during the period of follow-up.20, 21 Evidence of microvascular events (retinopathy, nephropathy, amputation), peripheral vascular procedures and cerebrovascular procedures were derived from automated data ICD-9 and CPT codes.22
Statistical Analysis
We first examined differences in those study subjects who completed the 5 year assessment and those who were lost to follow-up and still living at the 5 year assessment date on depression, demographics, baseline clinical severity variables, baseline self-reported health status and risk behaviors. For the continuous variables t-tests were used, and for dichotomous variables Chi-square analyses were employed. Due to the large sample size, many significant differences were found between the groups. These differences in baseline study variables could bias the generalizability of our findings. For this reason, we employed a propensity score methodology to balance the groups on the observed variables. We created a non-response propensity score for each subject who was eligible for the 5-year follow-up. This non-response propensity score is the conditional probability of being a non-respondent at 5-year follow-up based on the multiple variables collected at baseline.23 To create the non-response probability score for each study subject we regressed all significantly different baseline variables upon a dichotomous outcome of responded or not-responded at 5-year follow-up using logistic regression. This model then produced probabilities for each subject conditional on their observed baseline variables. This probability was used as a regression adjustment in all subsequent analyses.23
We next tested for statistical associations between baseline variables and major depression at the 5-year assessment. T-tests and chi-square analyses were used for the unadjusted tests, and logistic regression analyses were used to derive odds ratios for each variable adjusted for the non-response propensity score and baseline PHQ scores. The association of macrovascular and microvascular events after baseline with depression status at the 5-year assessment were also compared using unadjusted (t-test and chi-square) and adjusted (logistic regressions) analyses. In these analyses, adjustment was made for macrovascular and macrovascular events that occurred before baseline and coronary, cerebrovascular and peripheral vascular procedures that occurred before baseline.
Lastly, we created a multivariable logistic regression model estimating the probability of having major depression at the 5-year assessment from the baseline and event variables. All covariates were entered into the logistic model and tested for statistical significance in the presence of the total set of predictors. Individually, the least significant predictor was removed, and the model was refit. This was repeated until we arrived at a statistical model that first included the propensity score, and then only included statistically significant predictors or covariates. Two exceptions were made a priori: 1) if a given event or procedure during follow-up was statistically significant we entered the corresponding baseline variable into the model regardless of statistical significance, and 2) type of diabetes (I or II) was retained in the model. We believe that this approach is conservative, in that it allows the estimation of the odds of depression from a post-baseline event while simultaneously controlling for the other model variables and the baseline status with regard to the event, and increases the generalizability of the model to individuals with either type of diabetes.
Results
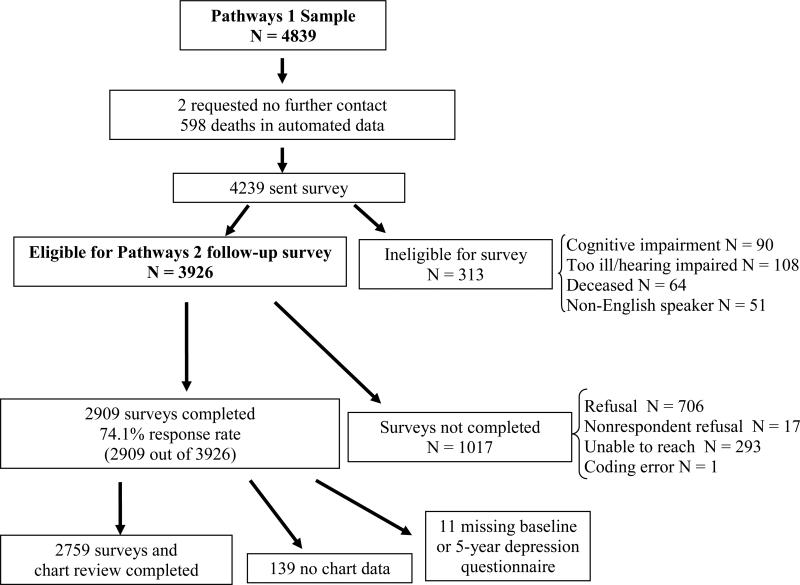
Figure 1 describes the flow of patients from the initial baseline mail survey from The Pathways Epidemiologic Study to the completion of a telephone survey approximately 5 years later (Pathways Follow-up Study). Over the course of 5 years, 662 patients died, 90 became cognitively impaired, 108 were too ill or hearing impaired, and 51 were non-English speakers, such that 3926 were eligible for Pathways-2. A total of 2909 (74.1%) telephone surveys were completed at 5 years. A total of 139 of these patients did not give permission for chart review, and 11 had incomplete baseline or 5-year depression data resulting in a final sample of 2759 (70.3% of those eligible).
Figure 1.
Pathways-Follow-up Study Flow Diagram
Table 1 describes the differences between the final sample of 2759 patients and the 1416 patients who were lost to follow-up who survived the 5-year period. Patients lost to follow-up were significantly less likely to have an ICD-9 of depression in the 18 months prior to the initial survey, were significantly less educated, less likely to be working, more likely to be married or cohabitating, less likely to be Caucasian, less likely to be treated with insulin, less likely to have had a history of one or more macrovascular or microvascular complications before baseline, had lower BMI, were more likely to be smokers and had more days of exercising in the past week. All of these variables with significant differences were included in the propensity analysis and contributed to the 5-year non-response propensity score.
Table 1.
Descriptions of Patients Included and Not Included in the Follow-up Analysis
| Indicators | Used in Study N = 2759 | Lost to Follow-Up & Alive , N = 1416 | t-Test or Chi Square |
|---|---|---|---|
|
Baseline Depression Variables | |||
| Number of depressive symptoms on the PHQ-9, Mean (SD) |
1.6 (2.2) |
1.6 (2.2) |
-0.89 |
| History of depression ICD-9 in the 18 months prior to baseline |
535 (19.3) |
202 (15.9) |
6.61† |
| Major or minor depression at baseline, N (%) | 303 (11.0) | 162 (11.5) | 0.27 |
|
Demographics | |||
| Age > 60, N (%) |
1526 (55.1) |
800 (56.7) |
0.96 |
| Women, N (%) |
1363 (49.2) |
706 (50.1) |
0.25 |
| At least some college, N (%) |
2229 (80.5) |
971 (68.9) |
69.46‡ |
| Employed full or part time, N (%) |
1347 (48.6) |
625 (44.3) |
6.77† |
| Not married or cohabiting, N (%) |
852 (30.8) |
498 (35.3) |
8.68† |
| Non-Caucasian, N (%) |
523 (18.9) |
427 (30.3) |
68.53‡ |
| Intervention subjects, N (%), N = 292 | 0.04 | ||
| Usual care | 108 (49.5) | 35 (47.3) | |
| Case management | 110 (50.5) | 39 (52.7) | |
|
Baseline Clinical Severity Variables | |||
| HbA1c, Mean (SD) |
7.8 (1.5) |
7.7 (1.6) |
0.71 |
| Number of diabetes symptoms, Mean (SD) |
2.6 (2.2) |
2.5 (2.2) |
1.42 |
| Duration of diabetes in years, Mean (SD) |
9.0 (6.0) |
8.6 (8.6) |
1.35 |
| Type I diabetes, N (%) |
134 (4.8) |
64 (4.5) |
0.12 |
| Treatment at baseline with insulin or insulin plus pills, N (%) |
789 (28.5) |
355 (25.2) |
4.97* |
| Rx Risk, Mean (SD) |
2727.5 (2155.2) |
2747.3 (2266.9) |
0.28 |
|
≥ 1 Macrovascular Complications and Procedures before baseline, N (%)
|
484 (17.5) |
116 (8.2) |
64.22‡ |
| MI before baseline |
247 (8.9) |
58 (4.1) |
31.17‡ |
| Stroke before baseline |
109 (3.9) |
39 (2.8) |
3.41 |
| Coronary procedure before baseline |
252 (9.1) |
48 (3.4) |
44.61‡ |
| PVD procedure before baseline |
19 (0.7) |
3 (0.2) |
3.14 |
| Cerebrovascular procedure before baseline |
11 (0.4) |
3 (0.2) |
0.48 |
|
≥ 1 Microvascular Complication before Baseline, N (%)
|
1366 (49.3) |
598 (42.4) |
17.60‡ |
| Nephropathy before baseline |
987 (35.6) |
447 (35.2) |
0.06 |
| Retinopathy before baseline |
707 (25.5) |
306 (24.1) |
0.90 |
| Amputation before baseline | 15 (0.5) | 5 (0.4) | 0.35 |
|
Baseline BMI and Health Risk Behaviors | |||
| BMI, Mean (SD) |
32.2 (7.3) |
30.7 (6.7) |
6.66‡ |
| Current smoking |
217 (7.8) |
151 (10.7) |
9.27† |
| Exercise days in past week | 2.8 (2.1) | 3.0 (2.2) | 2.70† |
p < .05
p < .01
p < .001
Table 2 describes the baseline differences between patients who met criteria for major depression on the PHQ-9 at 5 years and those who did not. In the unadjusted analyses, patients with a history of depression based on an ICD-9 code in the 18 months prior to baseline and those having baseline PHQ-9 scores of 5 to 9 or ≥ 10 were significantly more likely to meet criteria for major depression at 5 years. A total of 158 (5.7%) met DSM-IV criteria for major depression at 5 years. Of these 158 patients, a total of 99 (62.7%) had a PHQ score of ≥10 at baseline, 32 (20.3%) had a PHQ-9 score of 5 to 9 at baseline and only 27 (17.0%) had a PHQ-9 score of <5. Thus, approximately 83% of those with major depression at 5 years had significant depressive symptoms at baseline. Patients meeting criteria for major depression at 5 years also were younger, less likely to be married, had higher HbA1c levels and had a significantly greater number of diabetes symptoms, were more likely to be treated with insulin, and were more likely to have a history of retinopathy. The last column of Table 2 shows the odds ratios for each baseline variable adjusted for baseline PHQ-9 plus propensity scores. After adjustment, only the two depression severity variables, the number of baseline diabetes symptoms, and a baseline history of retinopathy remained statistically significant.
Table 2.
Association of Baseline Characteristics and Events and Procedures Before Baseline with Major Depression at the 5 Year Assessment
| Indicators | No Major Depression N = 2601 | Patients with Major Depression N = 158 | Unadjusted t-Test or Chi Square | Adjusted§ Odds Ratio (95% CI)for Major Depression vs. No Depression |
|---|---|---|---|---|
|
Baseline Depression Assessments | ||||
| History of depression ICD-9 in 18 months before baseline |
467 (17.9) |
67 (42.4) |
55.74‡ |
1.66† 1.16–2.40 |
| PHQ groupings | ||||
| 0– 4 | 1478 (56.8) | 27 (17.1) | 194.5‡ | -- |
| 5– 9 | 656 (25.6) | 32 (20.3) | 2.61‡ (1.55 – 4.40) | |
| 10+ | 458 (17.6) | 99 (62.7) | 11.67‡ (7.52 – 18.12) | |
|
Demographics | ||||
| Age > 60 - N (%) |
1452 (55.7) |
69 (43.7) |
8.26** |
0.85 0.61 – 1.20 |
| Women - N (%) |
1275 (48.9) |
84 (53.2) |
0.91 |
0.88 0.63 – 1.23 |
| At least some college, N (%) |
2099 (80.5) |
126 (79.7) |
0.02 |
0.92 0.57 – 1.49 |
| Employed full or part time, N (%) |
1270 (48.7) |
76 (48.1) |
0.005 |
0.91 0.65 – 1.27 |
| Not married or cohabitating, N (%) |
785 (30.1) |
63 (39.9) |
6.21* |
1.36 0.96 – 1.93 |
| Non-Caucasian, N (%) |
488 (18.7) |
34 (21.5) |
0.59 |
1.23 0.77 – 1.96 |
| Intervention subjects, N (%), N = 292 | 0.00 | 0.98 0.50 – 1.95 |
||
| Usual Care | 87 (49.4) | 21 (50.0) | ||
| Case Management | 89 (50.6) | 21 (50.0) | ||
|
Baseline Clinical Severity Variables | ||||
| HbA1c, Mean (SD) |
7.8 (1.5) |
8.1 (1.7) |
2.47* |
1.06 0.95 – 1.17 |
| Number of diabetes symptoms, Mean (SD) |
2.5 (2.1) |
4.1 (2.5) |
7.96‡ |
1.14† 1.05 – 1.22 |
| Duration of diabetes in years, Mean (SD) |
9.0 (9.0) |
9.2 (8.0) |
0.28 |
1.00 0.98 – 1.02 |
| Type I diabetes, N (%) |
127 (4.9) |
7 (4.4) |
0.004 |
1.10 0.49 – 2.48 |
| Treatment with insulin or insulin plus pills, N (%) |
730 (28.0) |
59 (37.3) |
5.91* |
1.26 0.89 – 1.78 |
| Rx risk – Mean (SD) |
2723.7 (2155.9) |
2779.3 (2168.6) |
0.31 |
1.00 1.00 – 1.00 |
| Hypertension before baseline |
1897 (72.8) |
119 (75.3) |
0.36 |
1.03 0.70 – 1.52 |
|
≥ 1 Macrovascular Complication or Procedure before baseline N (%)
|
448 (17.2) |
36 (22.8) |
2.85 |
1.40 0.88 – 2.24 |
| MI before baseline |
227 (8.7) |
20 (12.7) |
2.39 |
1.37 0.78 – 2.39 |
| Stroke before baseline |
98 (3.8) |
11 (7.0) |
3.23 |
1.63 0.81 – 3.26 |
| Coronary procedure before baseline |
237 (9.1) |
15 (9.5) |
0.001 |
0.89 0.47 – 1.69 |
| PVD procedure before baseline |
19 (0.7) |
0 (0.0) |
0.34 |
-- |
| Cerebrovascular procedure before baseline |
11 (0.4) |
0 (0.0) |
0.03 |
-- |
|
≥ 1 Microvascular Complication, N (%)
|
1613 (61.9) |
107 (67.7) |
1.91 |
1.12 0.79 – 1.60 |
| Nephropathy before baseline |
1242 (47.7) |
79 (50.0) |
0.24 |
0.92 0.66 – 1.29 |
| Retinopathy before baseline |
908 (34.8) |
68 (43.0) |
4.03* |
1.44* 1.03 – 2.03 |
| Amputation before baseline | 15 (0.6) | 0 (0.0) | 0.16 | -- |
|
Baseline Health Risk Behaviors | ||||
| BMI, Mean (SD) |
32.1 (7.3) |
34.4 (8.1) |
3.49‡ |
1.01 0.99 – 1.03 |
| Current smoking |
197 (7.6) |
20 (12.7) |
4.67* |
1.44 0.84 – 2.47 |
| Exercise days in past week | 2.8 (2.1) | 2.0 (1.9) | 4.44‡ | 0.94 0.86 – 1.02 |
adjusted for non-response probability and PHQ depression score groups at baseline assessment
p < .05
p < .01
p < .001
Table 3 shows the association of macrovascular and microvascular events during follow-up with major depression at the 5-year assessment, with each type of event considered in a separate model. Major depression risk was elevated in association with having at least one macrovascular event or procedure, with having a coronary procedure (CABG, angioplasty or stent placement), and with a higher mean number of macrovascular events or procedures during follow-up. These differences remained significant after adjustment for the propensity score and for major depression at baseline. The point estimate was elevated for the association of a stroke event during follow-up with major depression, but this association did not reach statistical significance.
Table 3.
Microvascular and Microvascular Events During Follow up in Relation to Major Depression at 5 year Assessment
| Indicators | No Major Depression N = 2601 | Patients with Major Depression N = 158 | Unadjusted t-test or chi square | Adjusted§Odds Ratio |
|---|---|---|---|---|
| Macrovascular or Microvascular Events During Follow-Up (At least 1), N (%) | ||||
| ≥1 Macrovascular Event or Procedure, N (%) | 317 (12.2) | 31 (19.6) | 6.86‡ | 1.81† 1.18 – 2.80 |
| MI | 100 (3.8) | 6 (3.8) | 0.000 | -- |
| Stroke | 93 (3.6) | 9 (5.7) | 1.35 | 1.75 0.83 – 3.67 |
| Cerebrovascular procedure | 16 (0.6) | 3 (1.9) | 1.97 | -- |
| Coronary procedure | 182 (7.0) | 20 (12.7) | 6.27* | 1.92* 1.14 – 3.25 |
| PVD procedure | 21 (0.8) | 0 (0.0) | 0.44 | -- |
| ≥1 Microvascular Event, N (%) | 823 (31.6) | 47 (29.7) | 0.16 | 0.86 0.30 – 1.24 |
| Amputation | 25 (1.0) | 2 (1.3) | 0.000 | -- |
| Retinopathy∥ | 376 (22.1) | 17 (18.9) | 0.36 | 0.69 0.40 – 1.21 |
| Nephropathy¶ | 517 (37.9) | 33 (41.8) | 0.32 | 1.06 0.65 – 1.71 |
| Total Events (Macrovascular and Microvascular Events & Procedures) | ||||
| Mean (SD) number of macrovascular events or procedures(0-5) | 0.16 (0.46) | 0.24 (0.52) | 2.17* | 1.39* 1.02 – 1.88 |
| Mean (SD) number of microvascular events | 0.35 (0.55) | 0.33 (0.54) | 0.53 | 0.88 0.64 – 1.21 |
adjusted for non response probability and PHQ depression score groups at baseline assessment
development of retinopathy in patients without previous evidence of retinopathy (eligible patients N = 1787)
development of nephropathy in patients without previous evidence of nephropathy (eligible patients N = 1442)
p < .05
p < .01
p < .001
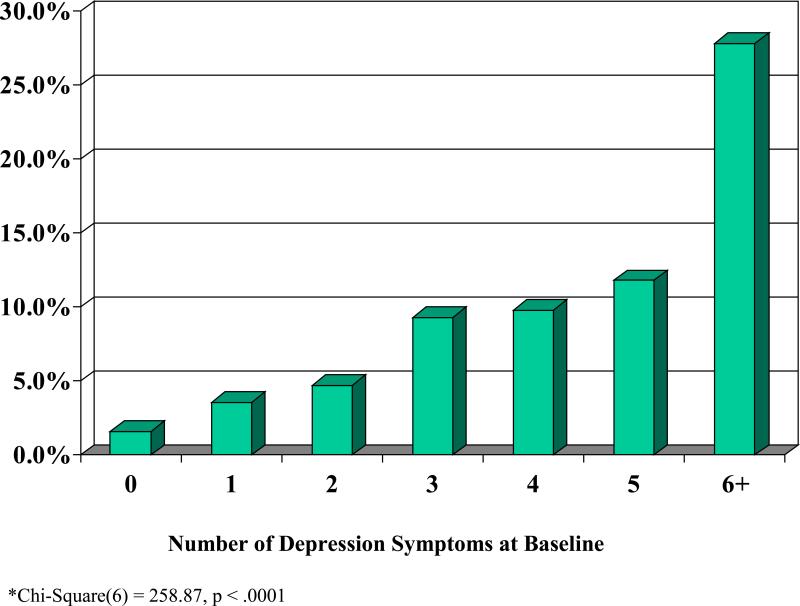
The multivariate logistic regression (Table 4) showed that patients meeting DSM IV criteria for major depression at 5 years were significantly more likely to have baseline scores on the PHQ-9 of 5-9 (corresponding to minor depression) and ≥ 10 (corresponding to major depression) compared with scores of 0-4, and had a significantly higher baseline number of diabetes symptoms. In addition, in the 12 months prior to the baseline survey, they were significantly more likely to have a physician diagnosis of depression. During the 5 year follow-up, those with major depression were also significantly more likely to have had a one or more coronary procedures. Figure 2 shows the significant association between each additional increase in number of depressive symptoms at baseline and the increased risk of major depression at 5-year follow-up.
Table 4.
Multivariable Model for Major Depression at 5-Year Assessment
| Variable |
Beta (SE) |
Wald's Statistic |
Adjusted OR |
95%CI for OR |
|---|---|---|---|---|
| Nonresponse propensity score |
0.21 (0.97) |
0.04 |
0.83 |
0.18–8.31 |
| Baseline PHQ groups | ||||
| 0 – 4 | 1.00 (reference) | |||
| 5 – 9 | 0.81 (0.28) | 8.37† | 2.24 | 1.30 – 3.88 |
| 10+ | 2.04 (0.26) | 61.97‡ | 7.70 | 4.63 – 12.81 |
| History of depression ICD-9 in 18 months before baseline |
0.52 (0.19) |
7.33† |
1.68 |
1.15 – 2.45 |
| Type of diabetes (Type I) |
0.23 (0.42) |
0.31 |
1.26 |
0.56 - 2.85 |
| Number of diabetes symptoms at baseline |
0.12 (0.04) |
9.97† |
1.13 |
1.05 – 1.22 |
| Coronary procedure before baseline |
-0.13 (0.33) |
0.15 |
0.88 |
0.46 – 1.69 |
| Coronary procedure during 5-year follow-up | 0.65 (0.28) | 5.28* | 1.92 | 1.10 - 3.35 |
p < .05
p < .01
p < .001
Figure 2.
Relationship* between Number of Depression Symptoms at Baseline and Major Depression at 5 Year Follow-Up
Discussion
The results of this prospective study show that baseline severity of depressive symptoms, coronary procedures (i.e. coronary artery bypass surgery, angioplasty, and coronary stent placement) during follow-up and baseline severity of diabetes symptoms were each independently associated with risk of major depression at 5 year follow up. The most significant predictor of meeting DSM-IV criteria for major depression was having a PHQ-9 score of ≥10 or greater at baseline which has been the cutoff score on the PHQ-9 that is recommended as having the highest sensitivity and specificity for major depression.14 A PHQ-9 score of 5 to 9 was also associated with an over 2-fold greater risk of major depression at 5 years. Major depression in patients with diabetes has been shown in prior studies to be often a chronic or highly recurrent disorder. The Pathways Clinical Trial which enrolled 329 patients with comorbid major depression and/or dysthymia and diabetes, found that approximately 70% of patients with diabetes and depression described their symptoms as present for two years or more.15 Another long-term follow-up study showed that about 70% of patients with diabetes and major depression relapsed with a mean of approximately 4 episodes over a 5 year period.24 Both dysthymia and having minor depression or residual symptoms after a major depressive episode have been shown in multiple studies to increase the risk of subsequent major depressive episodes25, 26
Our data suggest that coronary procedures but not other microvascular or macrovascular events or procedures during follow-up were associated with higher risk of depression at the 5-year assessment. Because of better prophylactic treatment with statins, antihypertensive medications, aspirin and beta-blockers and early intervention with cardiac procedures like stents, fewer macrovascular complications are being seen in patients with diabetes.27 However, coronary procedures may be stressful to patients and were experienced at an almost two-fold higher rate in those meeting depression criteria at 5 years (12.7% vs. 7.0%) compared to nondepressed patients. High rates of depression after cardiac procedures like coronary artery bypass surgery have been reported by other studies.28
The baseline number of diabetes symptoms was also significantly associated with major depression at 5 years. Each additional diabetes symptom at baseline was associated with a 13% increased risk of meeting criteria for major depression at 5 years. We have shown in a prior study that severity of depression, number of diabetes complications and HbA1c levels are all independently associated with this diabetes symptom score.2 These data suggest that baseline severity of diabetes is associated with major depression at 5-year follow-up.
Limitations of this analysis include that these patients were all from one large HMO in one geographic region of the United States. However, prior epidemiologic research in GH populations with depression and diabetes has consistently been replicated in other large national surveys.29,30 Other limitations include that depression was only measured at baseline and 5 years, and first events but not recurrent events during follow-up were measured. Given the small number of macrovascular and microvascular events and procedures during the 5 year period, and the lack of measurement of repetitive events, we were not able to study time to event and depression outcomes. Also, given the small number of macrovascular procedures, we were unable to examine the risk of subsequent depression with each procedure.
In conclusion, among a large sample of persons with diabetes, by far the strongest variable associated with major depression at 5-year follow-up was the presence of depression (or history of depression) at baseline. In fact, only approximately 17% of persons who met criteria for major depression at follow-up did not manifest either major or minor depression at baseline. Other variables that were associated with depression at follow-up were the number of diabetes symptoms at baseline (which is strongly associated with psychological distress and diabetes complications2) and the occurrence of cardiac procedures in the 5-year interval, whereas macrovascular and microvascular events were not associated with an increased risk of depression at follow-up.
Approximately 70% of patients with comorbid depression and diabetes have been found to have 2 years or more of depressive symptoms.15 The chronicity of depression in this population and the above results point to the importance of testing in future trials interventions that enhance screening and aggressive treatment of depression as well as testing relapse prevention interventions31 in patients with comorbid depression and diabetes.
Acknowledgements
This study was supported by grants from the National Institute of Mental Health to Dr. Katon (K24 MH 067587) and Dr. Von Korff (MH 073686).
Reference
- 1.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–26. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 2.Ludman EJ, Katon W, Russo J, et al. Depression and diabetes symptom burden. Gen Hosp Psychiatry. 2004;26:430–6. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 3.Von Korff M, Katon W, Lin EH, et al. Work disability among individuals with diabetes. Diabetes Care. 2005;28:1326–32. doi: 10.2337/diacare.28.6.1326. [DOI] [PubMed] [Google Scholar]
- 4.Von Korff M, Katon W, Lin EH, et al. Potentially modifiable factors associated with disability among people with diabetes. Psychosom Med. 2005;67:233–40. doi: 10.1097/01.psy.0000155662.82621.50. [DOI] [PubMed] [Google Scholar]
- 5.Lin EH, Katon W, Von Korff M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- 6.de Groot M, Anderson R, Freedland KE, et al. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63:619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Simon G, Katon W, Lin E, et al. Diabetes complications and depression as predictors of health care costs. Gen Hosp Psychiatry. 2005;27:344–51. doi: 10.1016/j.genhosppsych.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 8.Katon WJ, Rutter C, Simon G, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 9.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26:2822–8. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 10.Raison CL, Capuron L, Miller AH. Cytokines sing the blues: inflammation and the pathogenesis of depression. Trends Immunol. 2006;27:24–31. doi: 10.1016/j.it.2005.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914–20. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 12.McCulloch DK, Price MJ, Hindmarsh M, et al. A population-based approach to diabetes management in a primary care setting: early results and lessons learned. Eff Clin Pract. 1998;1:12–22. [PubMed] [Google Scholar]
- 13.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Katon WJ, Von Korff M, Lin EH, et al. The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Arch Gen Psychiatry. 2004;61:1042–9. doi: 10.1001/archpsyc.61.10.1042. [DOI] [PubMed] [Google Scholar]
- 16.Whitty P, Steen N, Eccles M, et al. A new self-completion outcome measure for diabetes: is it responsive to change? Qual Life Res. 1997;6:407–13. doi: 10.1023/a:1018443628933. [DOI] [PubMed] [Google Scholar]
- 17.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 18.Fishman PA, Goodman MJ, Hornbrook MC, et al. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model. Med Care. 2003;41:84–99. doi: 10.1097/00005650-200301000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14:15–23. [PMC free article] [PubMed] [Google Scholar]
- 20.Heckbert SR, Kooperberg C, Safford MM, et al. Comparison of self-report, hospital discharge codes, and adjudication of cardiovascular events in the Women's Health Initiative. Am J Epidemiol. 2004;160:1152–8. doi: 10.1093/aje/kwh314. [DOI] [PubMed] [Google Scholar]
- 21.Curb JD, McTiernan A, Heckbert SR, et al. Outcomes ascertainment and adjudication methods in the Women's Health Initiative. Ann Epidemiol. 2003;13:S122–8. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 22.American Medical Association . Current Procedural Terminology, CPT 2006 Professional Edition. American Medical Association; Chicago, IL: 2005. [Google Scholar]
- 23.Rao RS, Sigurdson AJ, Doody MM, et al. An application of a weighting method to adjust for nonresponse in standardized incidence ratio analysis of cohort studies. Ann Epidemiol. 2005;15:129–36. doi: 10.1016/j.annepidem.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 24.Lustman PJ, Griffith LS, Freedland KE, et al. The course of major depression in diabetes. Gen Hosp Psychiatry. 1997;19:138–43. doi: 10.1016/s0163-8343(96)00170-3. [DOI] [PubMed] [Google Scholar]
- 25.Mueller TI, Leon AC, Keller MB, et al. Recurrence after recovery from major depressive disorder during 15 years of observational follow-up. Am J Psychiatry. 1999;156:1000–6. doi: 10.1176/ajp.156.7.1000. [DOI] [PubMed] [Google Scholar]
- 26.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 27.Fox CS, Coady S, Sorlie PD, et al. Trends in cardiovascular complications of diabetes. JAMA. 2004;292:2495–9. doi: 10.1001/jama.292.20.2495. [DOI] [PubMed] [Google Scholar]
- 28.Oxlad M, Wade TD. Longitudinal risk factors for adverse psychological functioning six months after coronary artery bypass graft surgery. J Health Psychol. 2008;13:79–92. doi: 10.1177/1359105307084314. [DOI] [PubMed] [Google Scholar]
- 29.Egede L, Nietert P, Zheng D. Depresison and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28:1339–45. doi: 10.2337/diacare.28.6.1339. [DOI] [PubMed] [Google Scholar]
- 30.Gilmer T, O'Conner P, Rush W, et al. Predictors of health care costs in adults with diabetes. Diabetes Care. 2005;28:59–64. doi: 10.2337/diacare.28.1.59. [DOI] [PubMed] [Google Scholar]
- 31.Katon W, Rutter C, Ludman E, et al. A randomized trial of relapse prevention of depression in primary care. Arch Gen Psychiatry. 2001;58:241–7. doi: 10.1001/archpsyc.58.3.241. [DOI] [PubMed] [Google Scholar]