Abstract
Objective:
Assessment of the potential efficacy and safety of selective laser trabeculoplasty (SLT) as a primary therapeutic modality for lowering the intraocular pressure (IOP) in high tension open angle glaucoma (OAG) and ocular hypertensive patients (OHT).
Methods:
Twenty five patients (35 eyes) were enrolled in this prospective interventional longitudinal clinical study, undertaken during the period January 2005 to October 2006. All the laser procedures were done in the Oyoon Eye Center in Cairo, Egypt. Informed consent was taken from the patients after explanation of the procedure. Eighteen patients (25 eyes) had mild to moderate high tension open angle glaucoma, and there were 7 ocular hypertensive patients (10 eyes). Participants underwent selective laser trabeculoplasty (SLT) 180 degrees and followed up over a period of 12 months to assess the intraocular pressure lowering effect after SLT. Possible complications of the procedure were reported.
Results:
The intraocular pressure (mean ± standard deviation [StDev]) decreased from baseline pre-operative value of 26.78±3.13 mm Hg to 19.34±1.89 mm Hg 12 months after SLT (p<0.001). The average reduction in intraocular pressure (IOP) was 7.44 mm Hg (95% confidence interval 6.45 – 8.41 mm Hg). By the end of the follow up period (12 months), 62.9% of cases (22 eyes) showed IOP decrease by ≥ 30% from the baseline value, and 77.1% of cases (27 eyes) showed IOP decrease by ≥ 25% of baseline IOP.
Conclusion:
Selective laser trabeculoplasty is an effective IOP lowering modality. It can be used as a primary treatment for open angle glaucoma and ocular hypertensive patients. If the minimal side effects reported are considered, it can be concluded that SLT has a potential safety to be used as primary alternative treatment for open angle glaucoma and ocular hypertensive patients.
Keywords: Glaucoma, Open-Angle; Intraocular Pressure; Laser Surgery; Ocular Hypertension; Trabeculoplasty
Advances in Knowledge
Selective laser trabeculoplasty is a new modality of laser treatment for lowering intraocular pressure both in high tension glaucoma and ocular hypertension.
Selective laser trabeculoplasty has lesser side effects as compared to the other laser therapeutic modalities.
A target intraocular pressure lowering effect of 25–30 % can be reached and maintained over a period of one year in a good percentage of cases (62.9% to 77.1% of cases).
Applications to Patient Care
Selective laser trabeculoplasty is a safe and easy primary therapeutic modality for treatment of open angle glaucoma and ocular hypertensive patients.
Selective laser trabeculoplasty can be used as a safe alternative to argon laser trabeculoplasty and medical treatment of open angle glaucoma and ocular hypertensive patients.
If we consider the relative easiness of Selective laser trabeculoplasty procedure and its safety, the costs of glaucoma patients’ care (antiglaucoma medications) can be minimized and complications of surgical treatment can be avoided or at least delayed.
Intraocular pressure (IOP) is one of the most challenging issues in ophthalmology. For a long time, primary control of IOP in primary open angle glaucoma (POAG) was medical. Laser treatment was indicated in case of a noncompliant patient, or with the aim of cutting down the cost of medications, or to convert the noncompliant patient with multiple topical medications to a compliant one with one topical medication. For these cases, argon laser trabeculoplasty (ALT) was introduced by Wise and Witter as early as 1979.1 Eyes that were treated with ALT tended to have better results, in terms of lower IOP and better functional and morphometric status, than medically treated eyes;2 however, late failure was common. Clinical as well as histological studies of ALT demonstrated that late failure of ALT was due to destruction of the uveoscleral meshwork with surrounding thermal damage which, in addition to membrane formation over the meshwork by migrating endothelial cells, leads to long term loss of effect.3, 4 Other types of laser treatment modalities, including diode laser, were tried, but with limited success.3
In 1998, a new laser trabeculoplasty treating modality was introduced by Marc Latina and his colleagues.4 In this modality of selective laser trabeculoplasty (SLT), a 532 nm, Q switched, frequency doubled, neodymium:yittrium-aluminium-garnet (Nd:YAG) laser is used. SLT selectively targets pigmented TM cells (sparing the non-pigmented cell) producing selective photolysis without causing structural or coagulative damage. Absorption of radiant energy by melanosomes of the pigmented TM cells leads to rupture of these melanosomes and celluar destruction (photolysis). The ruptured melanosomes liberate metalloproteasis and other proteolytic enzymes. These liberated enzymes, as well as other factors, trigger an inflammatory response mediated by macrophages and other phagocytic cells. The phagocytic action in and around the trabecular meshwork is responsible for increased aquous outflow with reduction of IOP.4 Encouraging results, with moderate IOP reduction and minimal side effects had been shown.7, 8 Since there is practically no thermal coagulative damage to the trabecular meshwork, it might be possible to repeat SLT in eyes previously treated with ALT or SLT.
METHODS
The objective of the study was to assess the potential efficacy of selective laser trabeculoplasty (SLT) as a primary therapeutic modality for lowering the intraocular pressure (IOP) in high tension open angle glaucoma (OAG) and ocular hypertensive patients (OHT). Also complications of this procedure are reported. The main outcome measure was the intraocular pressure before and after SLT.
In this prospective clinical study, twenty five patients (35 eyes) were enrolled: 18 patients (25 eyes) with mild to moderate high tension open angle glaucoma, and 7 ocular hypertensive patients (10 eyes). All these patients were treated at the Oyoon Eye Center in Cairo, Egypt, during the period January 2005 to October 2006. Informed consent was taken from each patient after explanation of the procedure
High tension glaucoma patients were defined as those with the following characteristics: 1) intraocular pressure (IOP) ≥ 22 mmHg on at least two measurements, measured on at least two separate occasions; 2) visual field changes (in standard achromatic automated perimetry) that fulfilled the minimal criteria for glaucomatous visual field (VF) damage according to Hodapp, Parrish and Anderson;5 3) optic nerve head and/or retinal nerve fiber layer changes characteristic for glaucoma, based on clinical stereobiomicroscopic slit lamp examination: excavation; notching; focal or diffuse atrophy of neuro-retinal rim area; vertical cup/disc ratio more than 0.6; cup/disc asymmetry between fellow eyes greater than 0.2 and/or localized slit; or wedge defect; or generalized atrophy of the retinal nerve fiber layer as seen with slit lamp biomicroscopy. All patients had open anterior chamber angle.
Ocular hypertensives were defined as those subjects with elevated IOP ≥ 22 mmHg, on at least two measurements, measured on at least two separate occasions. In addition, patients should have no visual field (VF) changes as mentioned in the glaucoma group, and no optic nerve head or retinal nerve fiber layer changes suggestive of glaucoma.
All patients enrolled in the study were subjected to full ophthalmic assessment including visual acuity, IOP measurements, slit lamp biomicrospcopic optic nerve head assessment, and gonioscopy to assure that the anterior chamber was opened, in addition to visual field examination (standard achromatic perimetry).
The surgical procedure was done in all cases with a Coherent Selecta 7000 laser system (Lumenis, Coherent, Inc, CA, USA). This is a frequency doubled, Q-switched Nd:YAG laser wavelength 532 nm, with a fixed pulse duration of 3 ns, and spot size of 400 μm. The laser system is coupled to a slit lamp delivery system with a helium-neon laser (HeNe) aiming beam. For preoperative preparation, the eye was anaesthetised with topical anaesthesia (novesine hydrochloride). No alpha agonist was used as a routine preoperative preparation.
The procedure was as follows: with the patient seated at the slit lamp, a three mirror gonio-lens was placed on the eye, while methylcellulose was used as a coupling medium between the lens and the eye. Then, the laser was focused on the trabecular mesh-work using the HeNe aiming beams. With the 400 μm spot size, the inferior half of the trabecular meshwork was irradiated with laser pulses, starting at the three o’clock position and proceeding till nine o’clock. The laser energy was initially set at 0.8 mJ. If a cavitation bubble appeared (overexposure) the laser energy was reduced by 0.1 mJ steps until no bubble formation was observed and treatment was continued at this energy level. If no cavitation bubble was observed, the pulse energy was increased by of 0.1 mJ steps until bubble formation was observed then decreased again by 0.1 mJ. During whole laser application, bubble formation was monitored with each pulse for the appearance of a bubble; if a bubble appeared, the pulse energy was decreased as described above. Non-overlapping 46–55 laser spots were applied over the entire inferior 180 degrees of the trabecular meshwork. At the end of the laser procedure, a single drop of prednisolone acetate 1% was instilled into the eye.
Postoperatively, the patients were prescribed dexamethasone 0.1% eye drops 4 times a day for 7 days. Then the patients were examined at 1 hour, 1 day, 1 week and followed up at 1, 3, 6, and 12 months intervals. At each visit, patients underwent a full ophthalmic examination, which included visual acuity measurement, slit lamp biomicroscopy. Goldmann applanation tonometry, gonioscopy, and funduscopy were performed at 12 months. Any symptoms of ocular complications were reported.
In case of failure to reach an adequate IOP lowering effect after 3 months, an additional session of SLT was done or medical treatment was resorted to according to the surgeon’s decision.
STATISTICAL ANALYSIS
SPSS 11.01 was used and a paired Student’s t-test was used for comparison between pre- and postoperative intraocular pressure values. A p value of <0.05 was considered statistically significant.
RESULTS
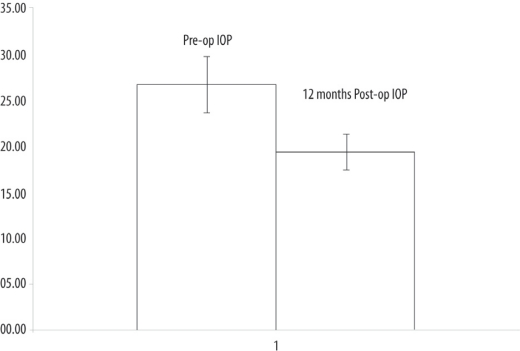
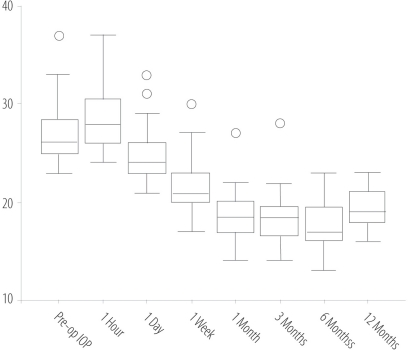
In 35 eyes with high tension OAG and ocular hypertensive patients (25 patients, 14 males and 11 females), SLT was done and the patients followed up over a period of 12 months. The demographic characteristics for these patients are shown in Table 1. After SLT, the IOP (mean ± StDev) decreased from baseline pre-operative value of 26.78±3.13 mm Hg to 19.34±1.89 mm Hg 12 months after SLT (p<0.001) as shown in Figure 1. The mean IOP lowering effect was 7.44 mm Hg (95% confidence interval 6.45 – 8.41 mm Hg). By the end of follow up period (12 months), 62.9% of cases (22 eyes) showed IOP decrease by ≥ 30% from the baseline value, and 77.1% of cases (27 eyes) showed IOP decrease by ≥ 25% of baseline IOP. The mean IOP changes during the follow up period are shown in Figure 2.
Table 1:
Preoperative demographic characteristics and data
| Total number: Patient (Eyes) | 25 (35) |
| Primary open angle glaucoma | 13 (15) |
| Pseudoexpholiation | 3 (6) |
| Pigmentary Glaucoma | 2 (4) |
| Ocular hypertensive | 7 (10) |
| Age: Mean (StDev) | 57.44 (8.99) |
| Sex: Number (Percentage) | |
| Male | 14 (56%) |
| Female | 11 (44%) |
| Vertical Cp/Disc Ratio, Mean (Range) | |
| Primary open angle glaucoma | 0.64 (0.4 – 0.8) |
| Ocular hypertensive | 0.42 (0.2 – 0.6) |
| Pre-Operative Intraocular pressure, Mean (SD) | 26.8 (3.25) |
| Pre-Operative Best corrected visual actuity, Mean (SD) | 0.84 (0.18) |
| VF characteristics for the open angle glaucoma group, Mean (SD) | |
| Mean Defect (MD) | −5.19 (2.69) |
| Pattern Standard Deviation (PSD) | 6.66 (3.65) |
Figure 1:
Mean ± StDev of pre-operative Intraocular pressure and 12 months post-operative after SLT in mmHg
Figure 2:
The mean intraocular pressure changes over time during the follow up period
It has been reported that 5 cases (14.3%) exhibited < 20% reduction of IOP; one of them did not show any decrease in IOP from the baseline measurement. In case of failure to reach 25% reduction of baseline IOP after 3 months (6 eyes 17.1%), the SLT procedure was repeated in the superior 180 degrees. Three cases failed to complete the 12 months follow up period.
Some complications occurred with this procedure. IOP spikes of 4–7mm Hg at 1 hour post-op was detected in 5 cases (14.3%). Mild uveitis was reported with mild AC Flare and cells in 25 cases (71.4%); this was controlled with topical steroid within 24–96 Hours. Ocular discomfort, pain and conjunctival redness were detected in 23 cases (65.7%).
There were no differences in terms of mean Snellen equivalent, best corrected visual acuities, measured cup/disc ratios and average values of mean defects (decibels).
DISCUSSION
In this prospective study, SLT demonstrated an effective IOP lowering effect. It lowers the IOP (mean ± StDev) from baseline pre-operative value of 26.78±3.13 mm Hg to 19.34±1.89 mm Hg 12 months after SLT (p<0.001). The magnitude of IOP lowering effect was 7.44 mm Hg. This is in agreement of the results reported by Melamed et al.6 Their results demonstrated an IOP lowering effect of 7.7 ±3.5 mmHg in a similar mixed group of OAG and OHT patients. Another study published by Nagar et al,7 showed that the IOP lowering effect in 180º SLT treated group was significantly less than in their medically treated group, to whom latanoprost was administered; however, the difference between the 360º treated group and the latanoprost group did not reach a statistical significance level, both of the treatment modalities showing similar results. Also they showed an IOP reduction by >30% from the baseline value in 59% of cases, which is in agreement with our study results. These showed an IOP decrease by ≥ 30% from the baseline value in 62.9% of cases, while 77.1% of cases showed an IOP decrease by ≥ 25% of baseline IOP. McIlraith et al in 2006, reported similar results of a 31% reduction of baseline IOP as compared to 30% reduction with latanoprost.8 Contradictory results were reported in a retrospective study by Song et al.9 They showed a high failure rate in SLT treated patients, as 86% of cases showed <20% IOP reduction. The explanation for this is that the studied group of patients was not treated similarly; some of them underwent 180º while other patients were treated with 90º. Also, most of them had a lower baseline IOP before treatment which was a predictor for failure. Their observation that lower baseline IOP is a predictor for failure is in agreement with our study results, which showed that 5 cases (14.3%) exhibited < 20% reduction of IOP, while one of them did not show any decrease in IOP from the baseline measurement. These cases in our study were those who had lower IOP values and some of them (2 eyes) were patients with pseudoexfoliation glaucoma for whom SLT was repeated. This is in agreement with the study of Gracner, who demonstrated a poor response of patients with capsular glaucoma to SLT.10 In contrast to this, patients with pigmentation of the drainage angle (pigmented races, capsular glaucoma and pigment dispersion syndrome) showed better responses to ALT as compared to SLT.11 This is logical with ALT where coagulative damage is known to occur. However, in SLT the mechanism is suggested to be at a cellular level and debris in the drainage angle in terms of iris pigment and pseudoexfoliation material may prevent adequate laser tissue interaction.
CONCLUSION
In view of the results of our study, which showed that 77.1% of cases showed IOP decrease by ≥ 25% of baseline IOP, we can conclude that SLT is an effective IOP lowering modality. It can be used as a primary treatment for open angle glaucoma and ocular hypertensive patients. If we consider the minimal side effects reported in our study and also in other studies published before, minimal or no coagulative damage is produced, so no subsequent trabecular meshwork fibrosis is produced. It can therefore be concluded that SLT is a safe alternative to ALT and medical treatment of open angle glaucoma and ocular hypertensive patients.
REFERENCES
- 1.Wise JB, Witter SL. Argon laser therapy for open angle glaucoma: a pilot study. Arch Ophthalmol. 1979;97:319–322. doi: 10.1001/archopht.1979.01020010165017. [DOI] [PubMed] [Google Scholar]
- 2.The Glaucoma Laser Trail Research Group The Glaucoma Laser Trail (GLT) and Glaucoma Laser Trial Follow Up Study: 7 results. Am J Ophthalmol. 1995;120:718–731. doi: 10.1016/s0002-9394(14)72725-4. [DOI] [PubMed] [Google Scholar]
- 3.McHugh D, Marshall J, Ffytche TJ, Hamilton PA, Raven A. Diode laser trabeculoplasty (DLT) for primary open angle glaucoma and ocular hypertension. Br J Ophthalmol. 1990;74:743–747. doi: 10.1136/bjo.74.12.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Latina MA, Park C. Selective targeting of trabecular meshwork cells: in vitro studies of pulsed and CW laser interactions. Exp Eye Res. 1995;60:359–371. doi: 10.1016/s0014-4835(05)80093-4. [DOI] [PubMed] [Google Scholar]
- 5.Hodapp E, Parrish RK, Anderson DR. Clinical decisions in glaucoma. St Louis MO: CV Mosby; 1993. [Google Scholar]
- 6.Melamed S, Ben Simon GJ, Levkovitch-Verbin H. Selective laser trabeculoplasty as primary treatment for open-angle glaucoma: a prospective, nonrandomized pilot study. Arch Ophthalmol. 2003;121:957–960. doi: 10.1001/archopht.121.7.957. [DOI] [PubMed] [Google Scholar]
- 7.Nagar M, Ogunyomade A, O’Brart DP, Howes F, Marshall J. A randomised, prospective study comparing selective laser trabeculoplasty with latanoprost for the control of intraocular pressure in ocular hypertension and open angle glaucoma. Br J Ophthalmol. 2005;89:1413–1417. doi: 10.1136/bjo.2004.052795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McIlraith I, Strasfeld M, Colev G, Hutnik CM. Selective laser trabeculoplasty as initial and adjunctive treatment for open-angle glaucoma. J Glaucoma. 2006;15:124–130. doi: 10.1097/00061198-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Song J, Lee PP, Epstein DL, Stinnett SS, Herndon LW, Jr, Asrani SG, et al. High failure rate associated with 180 degrees selective laser trabeculoplasty. J Glaucoma. 2005;14:400–408. doi: 10.1097/01.ijg.0000176939.43681.c2. [DOI] [PubMed] [Google Scholar]
- 10.Gracner T. Intraocular pressure response of capsular glaucoma and primary open-angle glaucoma to selective Nd:YAG laser trabeculoplasty: a prospective, comparative clinical trial. Eur J Ophthalmol. 2002;12:287–292. doi: 10.1177/112067210201200406. [DOI] [PubMed] [Google Scholar]
- 11.Ederer F, Gaasterland DA, Dally LG, Kim J, VanVeldhuisen PC, Blackwell B, et al. The Advanced Glaucoma Intervention Study Group (ASIS): 13. Comparison of treatment outcomes within race: 10-year results. Ophthalmology. 2004;111:651–664. doi: 10.1016/j.ophtha.2003.09.025. [DOI] [PubMed] [Google Scholar]