Abstract
Purpose
To determine the prevalence of refractive error (RE), and the proportion of those with uncorrected refractive error and factors associated with uncorrected RE in Latino adults.
Design
Population-based, cross-sectional study.
Participants
A random sample of 4,509 Latinos ≥40 years from Tucson and Nogales, Arizona with both ophthalmic evaluation and questionnaire were included in these analyses.
Methods
A case of RE was defined as subject wearing prescription glasses for distance vision whose presenting visual acuity (PVA) was 20/25 or better, or subject with PVA worse than 20/25 in at least one eye who improved ≥2 lines after subjective refraction and whose refractive correction met these cutoffs: sphere <−0.5 diopters (D) or >1.0D or cylinder ≥+1.0D. Among those with RE, those who on refraction achieved ≥2 line improvement in at least one eye (definition 1) or in both eyes (definition 2) were classified as uncorrected RE. A questionnaire on access to care, acculturation, perceived barriers, income, and education was asked.
Main Outcome Measures
Prevalence of RE and proportion of uncorrected RE
Results
The overall prevalence of RE in at least one eye was 64%, and in both eyes was 51%. Of participants with RE in at least one eye, 35% have uncorrected RE. Of those with RE in both eyes, 19% have uncorrected RE. As compared to those with corrected RE, those with uncorrected RE in at least one eye were more likely to have lower levels of acculturation (Odds Ratio [OR]=1.2; 95% Confidence Interval [CI]: 1.1–1.4 per unit decrease) and education (OR=1.6 for ≤6 years vs. >12 years; 95% CI: 1.2–2.2). Uncorrected RE was also significantly associated with not having insurance (OR=1.4; 95% CI: 1.1–1.6), a low family income (OR=1.4; 95% CI: 1.1–1.7 < $20,000/year), and time since last health care visit (OR=1.4; 95% CI: 1.1–1.7 for >1 year vs. <6 months).
Conclusions
In our sample of Latinos the overall proportion of uncorrected RE is high, and suggests that one third of those with RE may benefit from a new pair of glasses. Indices of marginalization are associated with uncorrected RE, and could be targeted for future interventions.
Introduction
Uncorrected refractive error (RE) is the leading cause of visual impairment worldwide and in the United States.1–3 It has been associated with decreased quality of life, as well as, limitations in vision-dependent activities.4–6 Uncorrected RE is associated with fewer opportunities for education and employment and reduced productivity.7 The problem of uncorrected RE among the United States (U.S.) Latino population is only now beginning to be examined.
In the U.S., Latinos are one of the fastest growing population groups; it is estimated that almost a quarter of the U.S. population will be Latino by 2050.8 Given the rapid growth and limited access to health care among this population, it is likely that the problem of uncorrected RE will be exacerbated among Latinos. This is particularly troubling as the prevalence of visual impairment among Latinos is higher compared to whites, and is similar to the rates observed among African Americans.1,9 Furthermore, this public health issue is mainly correctable, as almost three quarters of Latinos with visual impairment are likely to have an improvement in vision with refractive correction.9
Despite the treatable nature of uncorrected RE, Latinos, especially those living at the U.S.-Mexico border, face barriers to healthcare including a lack of health insurance and underutilization of preventive services. The 1982–84 Hispanic Health and Nutrition Examination Survey (HHANES) reported that approximately one-third of adult Mexican-Americans had experienced some type of barrier in obtaining health care during their most recent medical visit.10 Furthermore, the uninsured rate for Hispanics according to the 2007 U.S. Census Bureau Population Survey at 32.1% was much higher than that for Blacks (19.5%) and for whites (10.4%).11 Another cross-sectional, population-based survey of mostly Latino women 40 and older living on the U.S.-Mexico border (The Chronic Disease Screening Project) reported that among those living in Douglas, Arizona, only 27%, 16%, and 22% had received vision testing, Pap smears, and mammograms in the past year, respectively, suggesting significant disparities in the provision and utilization of preventive services in this population.12
The goal of our study was to determine the overall prevalence of RE and the proportion of uncorrected RE among those with RE, in a population-based study of adult Latinos living in Arizona. Additionally we aimed to identify associated predictive factors of uncorrected RE among this study population.
Materials and Methods
Study Design and Procedure
Detailed descriptions of the study methods are presented elsewhere13 and summarized here. Proyecto VER (Spanish for “to see”) is a population based survey of ocular disease, visual impairment, and legal blindness among noninstitutionalized Latinos living in southern Arizona. Utilizing the 1990 U.S. Census, block groups from Nogales and Tucson were randomly selected for inclusion in this study with a probability of selection within the strata proportional to the size of the Latino population older than or equal to 40 years in each block group.6,9 Fifty percent of households in the selected block group in Nogales and three-quarters of those in Tucson were randomly selected and contacted to assess eligibility. If at least one self-identified Latino person ≥40 years was a resident, participation of all eligible adults at that residence was sought. Eligibility was defined as noninstitutionalized, self-described Latino or Hispanics aged 40 and older residing at the address for 6 months or longer. Bilingual interviewers clarified details of the project and invited eligible persons to participate. Written informed consent was obtained from each participant, and all procedures and protocols were reviewed and approved by the institutional review boards of the University of Arizona and Johns Hopkins University and adhered to the tenets of the Declaration of Helsinki.
Home Questionnaire
An extensive home questionnaire was administered in either English or Spanish. Eighty percent of the home interviews were conducted in Spanish. The questionnaire consisted of questions regarding education level, socioeconomic status, health status, health and eye care use, past medical history, and history of vision problems and treatment. The interview also included a shortened National Eye Institute Visual Function Questionnaire (NEI-VFQ) and a shortened Cuellar Acculturation Questionnaire using questions on language preference, country of origin, ability to read and write English, and ethnic identification were used to create an index of acculturation of participants to U.S. society.14,15 The acculturation index has range values from 1 to 5, and a value less than 2 was considered to be indicative of low acculturation. Demographic variables analyzed in this study included age, gender, acculturation index, years of education (<6, 6–12, and 12+), and income (less than and greater than $20,000). A second set of access to care variables were also used and included: (1) Difficulty obtaining medical care over the past year (Yes/No); (2) Insured over the past year (Yes/No); (3) Time since last health care visit (<6 months, 6 months to 1 year, and ≥1 year); (4) Visits a particular health center (Yes/No); (5) Regular access to care (Yes/No); (6) Visits a particular physician (Yes/No); (7) Ever examined by an eye doctor (Yes/No). Regular access to care variable was defined as any care provided not in an emergency department or urgent care center where the respondent indicated a usual source of care.
Clinical Examination
Each participant was offered a complete ophthalmic clinical examination at a central site. Transportation, if required, was provided for participants at no cost. Data collection was conducted between April 1997 and September 1999. Details relating to refractive error are provided below.
Visual Acuity Testing
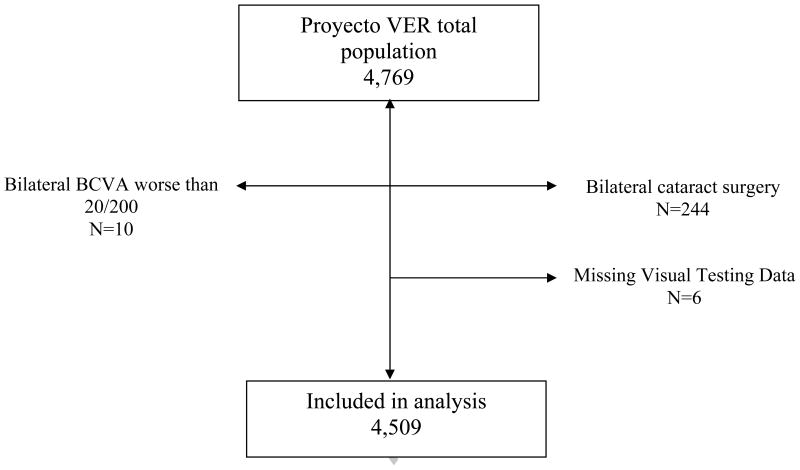
Distance visual acuity was tested monocularly using a modified Early Treatment of Diabetic Retinopathy Study (ETDRS) chart at 3m, illuminated at 130 cd/m2 using a forced choice procedure. Presenting visual acuity (PVA) was measured with the participant’s habitual distance correction. Those that forgot their glasses on the day of exam were treated as if they did not wear glasses. Participants who failed to read the largest letters at 3m were retested at 1.5m, then at 1m. Best-corrected visual acuity (BCVA) was measured for those with PVA worse than 20/25 using subjective refraction, and readings from the autorefractor (Humphrey instruments Inc., San Leandro, CA) were used as a starting point. Visual acuity was scored as the total number of letters read correctly, transformed to logarithm of the minimum angle of resolution (LogMAR) units. Failure to read any letters was assigned an acuity of 1.7 LogMAR units, which is equivalent to an acuity of 20/1000. An E chart was used for participants who were illiterate. Participants with bilateral BCVA worse than 20/200 (n=10) or incomplete visual testing information (n=6) were excluded as it was not possible to fully access visual acuity (Figure 1). Similarly, those who had bilateral cataract surgery (n=244) were excluded as the absence of natural lenses precluded accurate assessment of previous refractive error.
Figure 1.
Study Population Exclusions
BCVA = Best Corrected Visual Acuity
Definitions
Refractive error (RE) for each person was defined as eyes with sphere correction <−0.5 diopters (D) or >1.0D or cylinder ≥+1.0 D. Refraction information was extracted from the glasses prescription for those wearing glasses whose PVA was 20/25 or better, and from the subjective refraction for those who had PVA worse than 20/25. The “no refractive error group” consisted of: eyes without correction with PVA 20/25 or better, eyes without correction with PVA worse than 20/25 but whose acuity failed to improve with subjective refraction, and those with correction that did not meet the above definition (i.e., sphere correction was between −0.5 and +1.0 D correction and/or cylinder correction less than +1.0 D).
Refractive error for a person was examined in two ways: having refractive error in at least one eye or having RE in both eyes.
Uncorrected refractive error for a person was defined first as having an improvement in visual acuity greater or equal to 2 lines in at least one eye (definition 1), and second, as having an improvement in visual acuity greater or equal to 2 lines in both eyes (definition 2).
For the analyses looking at uncorrected refractive error in both eyes, those individuals with only monocular information were classified based on the data from that eye.
Statistical Methods
Contingency table analysis or t-test, as appropriate, was used to examine bivariate associations between uncorrected refractive error and independent demographic variables (age, sex, acculturation, education, annual income). Age adjusted p-values are reported.
Logistic regression analyses were utilized to determine odds ratios (OR) and 95% confidence intervals (CI) for associations between uncorrected refractive error and selected variables. Regression models were optimized using stepwise methods and only contained variables maintaining a p-value of 0.05 or lower when included in the model. First, a regression model including the demographic variables (acculturation index, education, income, and insurance) was created. A second separate model containing the access to care variables resulted in the inclusion of the frequency of care and the health center variables. A final model combining these two models retained acculturation index, education, income, insurance, and frequency of care variables; variables with p-values >0.05 were dropped from the final model. Data was analyzed using SAS (Statistical Analysis System Institute, Cary, NC).
Results
Population Characteristics
From the 4,255 eligible dwelling units, 6,659 eligible subjects were identified. Among the eligible subjects, 4,769 (72%) completed both the home interview and ophthalmic examination including visual acuity assessment. As reported previously9, nonparticipants were more likely to be among either to the youngest age group (40–49 years) or to the oldest age group (80 years or older) and to be male. They were also less likely to report having fair or poor health and less likely to report having problems with their vision. Response rates between the two locations (Nogales and Tucson) did not differ after age-adjustment.9 After all exclusions (Figure 1), our study population was 4,515 participants of whom 6 could not be classified into refractive error categories due to incomplete visual testing information.
Of the 4,509 participants with complete information, the average age was 56 years old (Standard deviation [S.D.] ±11 year), 61% were female, 67% had income less than $20,000 per year, 36% had at least completed high school, 64% had been insured in the past year, and the acculturation index was relatively low with an average of 2.0±0.95.
Prevalence of Refractive and Uncorrected Refractive Error
The prevalence of refractive error in our study population was 63.8% (2,875/4,509) in at least one eye and 51.2% (2,307/4,509) in both eyes. Of those with refractive error, 35.4% (1,018/2,875) were uncorrected in at least one eye, and among those with refractive error in both eyes, 18.6% (430/2,307) were uncorrected in both eyes.
Population Characteristics of those with Refractive Error
Refractive error in (RE) at least one eye (Table 1) was more prevalent in the oldest age groups and ranged from 44.2% in the youngest age group (40–49 years) to 87.7% in the oldest group (70 years or older). After adjusting for age, we also found a significantly higher prevalence of RE in females (67.7%) compared to males (57.6%) (p<.0001).
Table 1.
Prevalence of Refractive Error
| Total Study Population N=4,509 | Refractive Error in at least 1 Eye N (%) 2,875 (63.8%) | Refractive Error in Both Eyes N (%) 2,307 (51.2%) | |
|---|---|---|---|
| Age Group | |||
| 40–49 years | 1590 | 702 (44.2%) | 537 (33.8%) |
| 50–59 years | 1346 | 894 (66.4%) | 699 (51.9%) |
| 60–69 years | 921 | 707 (76.8%) | 590 (64.1%) |
| 70 + years | 652 | 572 (87.7%) | 481 (73.8%) |
| P for trend | <.0001 | <.0001 | |
| Sex | |||
| Female | 2756 | 1865 (67.7%) | 1516 (55.0%) |
| Male | 1753 | 1010 (57.6%) | 791 (45.1%) |
| X2 p value* | <.0001 | <.0001 | |
Age-adjusted p value
In Table 2, we age-stratified our sample as there was evidence of interaction between: (1) acculturation and age and (2) education and age. Stratification revealed that RE in those less than 60 years of age was associated with higher levels of acculturation and education. This relationship, however, was not observed in the older age group (60+ years).
Table 2.
Age Specific Prevalence of Refractive Error by Acculturation and Years of Education
| Total Study Population N=4,509 | Refractive Error in at least 1 Eye N (%) 2,875 (63.8%) | Refractive Error in Both Eyes N (%) 2,307 (51.2%) | ||||
|---|---|---|---|---|---|---|
| <60 years | 60+ years | <60 years | 60+ years | <60 years | 60+ years | |
| Acculturation Index | ||||||
| <2 | 1671 | 943 | 811 (48.5%) | 762 (80.8%) | 587 (35.1%) | 637 (67.6%) |
| 2–3 | 543 | 363 | 336 (61.9%) | 303 (83.5%) | 277 (51.0%) | 252 (69.4%) |
| 3+ | 720 | 267 | 447 (62.1%) | 214 (80.2%) | 371 (51.5%) | 182 (68.2%) |
| P for trend | <.0001 | 0.9 | <.0001 | 0.5 | ||
| Years of Education | ||||||
| <6 | 780 | 749 | 381 (48.9%) | 609 (81.3%) | 279 (35.8%) | 503 (67.2%) |
| 6–12 | 1596 | 702 | 875 (54.8%) | 571 (81.3%) | 680 (42.6%) | 484 (69.0%) |
| 12 + | 558 | 122 | 338 (60.6%) | 99 (81.2%) | 276 (49.5%) | 84 (68.9%) |
| P for trend | <.0001 | 0.5 | <.0001 | 0.1 | ||
Population Characteristics of those with Uncorrected Refractive Error
Uncorrected RE in at least one eye was significantly associated with acculturation (p<.0001), education (p<.0001), and income (p<.0001) (Table 3). These results were also consistent with our both eye analysis. Using both of our definitions of uncorrected RE neither age nor gender demonstrated a significant association with uncorrected RE.
Table 3.
Proportion of Uncorrected Refractive Error (RE) among those with RE: Demographic Variables
| At Least One Eye Analysis | Both Eyes | |||
|---|---|---|---|---|
| Total Participants with RE N=2,875 | Uncorrected RE N (%) 1,018 (35.4%) | Total Participants with RE N=2,307 | Uncorrected RE N (%) 430 (18.6%) | |
| Age Group | ||||
| 40–49 years | 702 | 239 (34.1%) | 537 | 90 (16.8%) |
| 50–59 years | 894 | 326 (36.5%) | 699 | 134 (19.2%) |
| 60–69 years | 707 | 241 (34.1%) | 590 | 117 (19.8%) |
| 70 + years | 572 | 212 (37.1%) | 481 | 89 (18.5%) |
| P for trend | 0.5 | 0.4 | ||
| Sex | ||||
| Female | 1865 | 655 (35.1%) | 1516 | 282 (18.6%) |
| Male | 1010 | 363 (35.9%) | 791 | 148 (18.7%) |
| X2 p value | 0.7 | 0.9 | ||
| Acculturation Index | ||||
| <2 | 1573 | 658 (41.8%) | 1224 | 293 (23.9%) |
| 2–3 | 639 | 182 (28.5%) | 529 | 65 (12.3%) |
| 3+ | 661 | 176 (26.6%) | 553 | 72 (13.0%) |
| P for trend | <.0001 | <.0001 | ||
| Years of Education | ||||
| <6 | 990 | 432 (43.6%) | 782 | 204 (26.1%) |
| 6–12 | 1446 | 481 (33.3%) | 1164 | 188 (16.2%) |
| >12 | 437 | 103 (23.6%) | 360 | 38 (10.6%) |
| P for trend | <.0001 | <.0001 | ||
| Income | ||||
| <$20,000/year | 1886 | 752 (39.9%) | 1496 | 329 (22.0%) |
| > $20,000/year | 911 | 238 (26.1%) | 749 | 87 (11.6%) |
| X2 p value | <.0001 | <.0001 | ||
The proportion of uncorrected RE, using both definitions, is associated with additional markers of marginalization including a lack of insurance, increasing time since last healthcare visit, not having a particular health center or a particular physician, and never being examined by an eye doctor (Table 4). Unlike those with uncorrected RE in at least one eye, difficulty obtaining care over the past year was associated but not statistically significant with uncorrected RE in both eyes (p = 0.1).
Table 4.
Proportion of Uncorrected Refractive Error (RE) in those with RE: Access to Care Variables
| At Least One Eye Analysis | Both Eyes Analysis | |||
|---|---|---|---|---|
| Total Participants with RE N=2,875 | Uncorrected RE N (%) 1,018 (35.4%) | Total Participants with RE N=2,307 | Uncorrected RE N (%) 430 (18.6%) | |
| Difficulty Obtaining Medical Care | ||||
| Over the Past Year | ||||
| Yes | 73 | 37 (50.7%) | 52 | 14 (26.9%) |
| No | 2793 | 976 (34.9%) | 2249 | 414 (18.4%) |
| X2 p value | 0.006 | 0.1 | ||
| Insured Over the Past Year | ||||
| Yes | 1930 | 604 (31.3%) | 1590 | 247 (15.5%) |
| No | 943 | 412 (43.7%) | 716 | 183 (25.6%) |
| X2 p value | <.0001 | <.0001 | ||
| Time Since Last Care Visit | ||||
| < 6 months | 1964 | 650 (33.1%) | 1595 | 264 (16.6%) |
| 6 months to < 1 year | 351 | 131 (37.3%) | 274 | 54 (19.7%) |
| ≥ 1 year | 545 | 231 (42.4%) | 427 | 110 (25.8%) |
| X2 p value | 0.0002 | <.0001 | ||
| Visits a Particular Health Center | ||||
| Yes | 2514 | 856 (34.0%) | 2038 | 355 (17.4%) |
| No | 358 | 159 (44.4%) | 267 | 75 (28.1%) |
| X2 p value | 0.0001 | <.0001 | ||
| Regular access to care | ||||
| Yes | 2483 | 845 (34.0%) | 2012 | 351 (17.5%) |
| No | 28 | 9 (32.1%) | 24 | 3 (12.5%) |
| X2 p value | 0.8 | 0.5 | ||
| Visits a Particular Physician | ||||
| Yes | 2297 | 757 (33.0%) | 1867 | 311 (16.7%) |
| No | 217 | 99 (45.6%) | 171 | 44 (25.7%) |
| X2 p value | 0.0002 | 0.003 | ||
| Ever Examined by an Eye Doctor | ||||
| Yes | 2685 | 862 (32.1%) | 2203 | 366 (16.6%) |
| No | 187 | 153 (81.8%) | 102 | 63 (61.8%) |
| X2 p value | <.0001 | <.0001 | ||
Predictors of Uncorrected Refractive Error
Table 5 shows demographic and access to care factors associated with uncorrected RE using a multivariate approach. Acculturation index score and years of education were inversely related to the odds of uncorrected RE in at least one eye (Table 5). Those without health insurance in the past year and those with an income of less than $20,000 per year were more likely to have uncorrected RE in at least one eye (OR=1.4; 95% CI: 1.1–1.6 and OR=1.4; 95% CI: 1.1–1.7, respectively). Increasing time since last health care visit and uncorrected RE in at least one eye had an inverse relationship. Those with care more than one year ago compared to those with care less than 6 months ago had a significant increase in the odds of uncorrected RE in at least one eye (OR=1.4; 95% CI: 1.1–1.7) (Table 5). Independent contributors were similar for our more restrictive definition requiring uncorrected RE in both eyes (Table 5).
Table 5.
Demographic and Access to Care Predictors of Uncorrected Refractive Error (RE) in the Proyecto VER Study Population Based on Multiple Logistic Regression Models
| Uncorrected RE in at Least 1 Eye N=1,018 | Uncorrected RE in Both Eyes N=430 | |
|---|---|---|
| Variables | OR (95% CI) | OR (95% CI) |
| Acculturation (per unit decrease)¶ | 1.21 (1.09–1.35) | 1.25 (1.08–1.45) |
| Education | ||
| 6 years or less | 1.61 (1.19–2.16) | 1.79 (1.15–2.76) |
| More than 6 years to 12 years | 1.38 (1.06–1.78) | 1.35 (0.91–2.00) |
| More than 12 years | 1 | 1 |
| Lack of Insurance (in past year) | 1.36 (1.14–1.62) | 1.43 (1.13–1.81) |
| Income (</>$20,000)§ | 1.38 (1.14–1.68) | 1.55 (1.18–2.05) |
| Time Since Last Care Visit€ | ||
| Less than 6 months | 1 | 1 |
| 6 months to 1 year | 1.17 (0.91–1.49) | 1.27 (0.91–1.80) |
| More than one year | 1.36 (1.11–1.67) | 1.61 (1.23–2.11) |
CI indicates confidence interval. OR indicates odds ratio. Bolded ORs achieved statistical significance (α<0.05).
Acculturation was measured using the short-form Cuellar Acculturation Scale and has score range 1–5. Index score <2 was considered low acculturation.
Including wages, salary, self-employment, and any other source of income, was the total combined family income during the last 12 months, that is, yours and that of any family members living in this household, more or less than $20,000?
How long has it been since you last saw or talked to a medical doctor or other health professional about your health?
Discussion
Refractive Error
The prevalence of RE among our Latino study population of adults in Arizona was found to be as high as 64% in at least one eye or as low as 51% in both eyes. Analysis of this population revealed that RE was associated with increasing age and female gender. The increase in RE with age is consistent with Hyman’s review of refractive error where she notes increases in RE among adults is accounted by two principle changes: 1) a “hyperopic shift” first seen in the 40–50 age groups and continuing until 60 to 80 years of age; and 2) an increase in myopia at the oldest age groups most likely due to lens opacifications.16 With regards to gender, the research is considerably less clear. Hyman notes that while myopia is generally equally present in males and females, there is variation among different ancestral groups.16 In addition, inconsistent findings have been reported including an increased prevalence of hyperopia among females.16
Stratification by age, those younger than 60 years and those 60 years and older, revealed an interaction between age and education, as well as age and acculturation among those with RE. Previous studies have found that increasing educational levels, intelligence, and socioeconomic status are all associated with myopia.17 This trend may explain the association increase RE and education and acculturation among the younger age group. However, the absence of this association among those 60 years and older may have been a result of our exclusion of subjects with bilateral cataract surgery. As our group previously demonstrated18, Latinos in the U.S. have high rates of both cataract and cataract surgery. We also found increasing access to medical care and use of English as positive predictors of cataract surgery.18 Therefore, as those with cataract surgery are among the older age group, those excluded from our analyses due to this condition may have been more likely to have high levels of education and acculturation. As a result, the relationship between RE and education and acculturation may have been attenuated.
Uncorrected Refractive Error
The problem of uncorrected RE continues to affect a large portion of the world population.19 In a previous study, we reported that uncorrected RE was responsible for the majority of visual impairment (VI) in those with visual acuity worse than 20/40.9 Subsequently, an examination of the U.S. population as part of the National Health and Nutrition Examination Survey (NHANES) demonstrated that 83.3% of those with VI could achieve good visual acuity (VA 20/40 or better in better-seeing eye) with refractive correction.1 This same study also found that the estimated prevalence among NHANES participants with VI due to uncorrected RE was higher among Hispanics than Blacks or Whites.1
In this population-based study of Latinos forty years or older from Arizona, we determined that a high proportion of those with RE were classified as having uncorrected RE (35.4% in at least one eye and 18.6% in both eyes, respectively). With a high response rate of 72% completing both the ophthalmic and home questionnaire the impact of non-participants on our study results is likely to be low.
Our findings suggest that more than a third of Latinos in our study population with RE could benefit from glasses, as they had uncorrected RE in at least one eye. Additionally, nearly 1 out of 5 individuals with RE were classified as having uncorrected RE in both eyes, a more conservative estimate. These findings coupled with our group’s previous research of this same study population examining the effect of uncorrected RE on visual function using a modified NEI-VFQ questionnaire suggest that providing affordable and widespread refractive services to the Latino community may lead to major improvements in visual function.6 However, more research is needed to fully confirm whether provision of corrective lenses to this population especially those with presenting acuity better than 20/40 will actually result in improved visual function and the magnitude of such improvement.
Predictive factors for both definitions of uncorrected RE included lower levels of income, acculturation, and education. Uncorrected RE was also associated with having limited access to health care and a lack of health insurance. These findings suggest that uncorrected RE in this population may be a problem of marginalization, specifically limited financial resources and a lack of health insurance coverage. The rapid growth of the Latino population combined with the high proportion of uncorrected RE observed in this study suggest that this public health issue may continue to increase in magnitude without additional interventions. Furthermore, unlike refractive error, uncorrected RE did not appear to be affected by age or gender. These latter finding suggest that uncorrected RE is more likely to be a societal problem related to marginalization rather than due to an underlying biological process. It is worth noting that despite the differences in definitions used that uncorrected RE was similarly associated with low annual income levels and a lack of health insurance in a similar study of Latinos in southern California, the Los Angeles Latino Eye Study (LALES).20
Interestingly, the Chronic Disease Screening Project, conducted in an Arizona border population demonstrated that vision testing during the previous 12 months among the U.S. subgroup 40–64 years of age was significantly lower among those that were uninsured (18%) compared to those of the same age group that had insurance (36.5%).12 These findings, while inconclusive, suggest that the provision of health insurance may improve vision testing in this Latino population and may help to alleviate the problem of uncorrected RE by increasing their access to eye care services. These results are further supported by association between VI and markers of marginalization (low income, lack of health insurance, and fewer years of education) since a large proportion of VI is due to uncorrected RE.1 These findings coupled with this population’s disadvantaged status imply the need for increased research to determine the impact of providing cost-effective screening, provision of refractive services, and glasses.
To allow for clear comparisons across study populations, there is a need for a standard definition for uncorrected RE. Previous definitions have included VA cutoffs of 20/40 in the better eye,19,20–22 varying cutoffs for line improvements after subjective refraction,22,23,24 and varying differences in classification such as corrected emmetropia.19 While each definition has its own strengths the lack of a standard definition for uncorrected RE has made it difficult to compare results between studies. In addition, although many studies have examined the problem of uncorrected RE among those with VA worse than 20/40, the functional role of uncorrected RE among those with VA between normal VA and 20/40 remains unclear. Our group hypothesizes that regardless of PVA, those with a ≥2 line improvement after subjective refraction are likely to benefit from proper refractive correction.
In this paper, we introduce an alternative approach to uncorrected RE that sets clear definitions for both RE and uncorrected RE at the eye and person level. Using two definitions, one that is more inclusive (requiring RE in at least one eye) and one that is conservative (requiring RE in both eyes) we demonstrate the uncorrected RE is highly dependent on definition. Utilization of these two definitions, however, can be used to give us an estimate of the problems of RE and uncorrected RE in study populations. The use of a proportion approach to estimate the problem of uncorrected RE was selected as it more appropriately identifies the magnitude of the problem of uncorrected RE among those affected (i.e., those subjects with RE). This dual definition approach may provide clinicians and policy makers with a range of estimates when establishing the burden of uncorrected RE. Additionally, research to identify the functional significance of these definitions is needed to further validate this approach.
We were unable directly compare our results to a LALES as a result of differences in the definitions of uncorrected RE. However, an approximate estimate of LALES’s Definition 2 of Unmet Refractive Need was conducted taking those individuals in our study with PVA worse than 20/40 and uncorrected RE and dividing by the total number of individuals with RE in our study to approximate total need (251/2307= 10.9%).20 This is similar to the 9.6% estimated in LALES and thus further strengthens our research findings.20
Ideally we would have checked the PVA for those with glasses without their glasses to ensure that these individuals really benefitted from their correction. As a result, we may have overestimated the number of people with corrected RE. Finally, we would have liked to directly query the perceived barriers to care to determine if other factors were related to having uncorrected RE.
In summary, we report a high proportion of uncorrected RE among those with RE in a Latino population. Associated predictive variables suggest that uncorrected RE is likely a multi-faceted problem affected by the marginalization of the Latino populations. Specifically, limited income and a lack of readily available health care may be contributing to this public health issue. It is possible that provision of affordable visual acuity screening and eye care, as well as provision of low cost corrective lenses could greatly benefit this community. Additional research should be conducted to determine how uncorrected RE can be effectively targeted in this community and should include attitudinal beliefs and functional needs towards spectacle use. We also recognize a need for a standard definition of refractive error and uncorrected RE.
Acknowledgments
Financial Support: a Senior Scientific Investigator award from Research to Prevent Blindness to Dr West; NEI (core grant: EY11283)
Footnotes
Meeting Presentation:
ARVO Annual Meeting, Ft. Lauderdale, FL. 5/6/10
21st Wilmer Research Meeting, Baltimore, MD 4/23/10
Conflict of Interest: No authors have any financial/conflicting interests to disclose
Online Materials: None
Video: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295:2158–63. doi: 10.1001/jama.295.18.2158. [DOI] [PubMed] [Google Scholar]
- 2.Dimitrov PN, Mukesh BN, McCarthy CA, Taylor HR. Five-year incidence of bilateral cause-specific visual impairment in the Melbourne Visual Impairment Project. Invest Ophthalmol Vis Sci. 2003;44:5075–81. doi: 10.1167/iovs.02-0457. [DOI] [PubMed] [Google Scholar]
- 3.Muñoz B, West SK, Rubin GS, et al. SEE Study Team. Causes of blindness and visual impairment in a population of older Americans: the Salisbury Eye Evaluation Study. Arch Ophthalmol. 2000;118:819–25. doi: 10.1001/archopht.118.6.819. [DOI] [PubMed] [Google Scholar]
- 4.Vu HT, Keeffe JE, McCarty CA, Taylor HR. Impact of unilateral and bilateral vision loss on quality of life. Br J Ophthalmol. 2005;89:360–3. doi: 10.1136/bjo.2004.047498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Varma R, Wu J, Chong K, et al. Los Angeles Latino Eye Study Group. Impact of severity and bilaterality of visual impairment on health-related quality of life. Ophthalmology. 2006;113:1846–53. doi: 10.1016/j.ophtha.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 6.Broman AT, Muñoz B, Rodriguez J, et al. The impact of visual impairment and eye disease on vision-related quality of life in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:3393–8. [PubMed] [Google Scholar]
- 7.Vincent JE, Pearce MG, Leasher J, et al. The rationale for shifting from a voluntary clinical approach to a public health approach in addressing refractive errors. Clin Exp Optom. 2007;90:429–33. doi: 10.1111/j.1444-0938.2007.00193.x. [DOI] [PubMed] [Google Scholar]
- 8.Ethnicity and Ancestry Branch, Population Division, U.S. Census Bureau. [Accessed February 28, 2010];Hispanics in the United States. Available at: http://www.census.gov/population/www/socdemo/hispanic/files/Internet_Hispanic_in_US_2006.pdf.
- 9.Muñoz B, West SK, Rodriguez J, et al. Blindness, visual impairment and the problem of uncorrected refractive error in a Mexican-American population: Proyecto VER. Invest Ophthalmol Vis Sci. 2002;43:608–14. [PubMed] [Google Scholar]
- 10.Estrada AL, Treviño FM, Ray LA. Health care utilization barriers among Mexican Americans: evidence from HHANES 1982–84. Am J Public Health. 1990;80(suppl):27–31. doi: 10.2105/ajph.80.suppl.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeNavas-Walt C, Proctor BD, Smith JC U.S. Census Bureau. Current Populations Reports P60-235. Washington, D.C.: U.S. Government Printing Office; 2008. [Accessed September 10, 2010]. Income, Poverty, and Health Insurance Coverage in the United States: 2007; pp. 19–22. Available at: http://www.census.gov/prod/2008pubs/p60-235.pdf. [Google Scholar]
- 12.Hunter JB, de Zapien JG, Denman CA, et al. Healthcare access and utilization among women 40 and older at the U.S. -Mexico border: predictors of a routine check-up. J Community Health. 2003;28:317–33. doi: 10.1023/a:1025440528845. [DOI] [PubMed] [Google Scholar]
- 13.West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care. 2001;24:1204–9. doi: 10.2337/diacare.24.7.1204. [DOI] [PubMed] [Google Scholar]
- 14.Cuellar I, Harris LC, Jasso R. An acculturation scale for Mexican American normal and clinical populations. Hisp J Behav Sci. 1980;2:199–217. [Google Scholar]
- 15.Espino DV, Maldonado D. Hypertension and acculturation in elderly Mexican Americans: results from 1982–84 Hispanic HANES. J Gerontol. 1990;45:M209–13. doi: 10.1093/geronj/45.6.m209. [DOI] [PubMed] [Google Scholar]
- 16.Hyman L. Myopic and hyperopic refractive error in adults: an overview. Ophthalmic Epidemiol. 2007;14:192–7. doi: 10.1080/09286580701535517. [DOI] [PubMed] [Google Scholar]
- 17.Saw SM, Katz JK, Schein OD, et al. Epidemiology of myopia. Epidemiol Rev. 1996;18:175–87. doi: 10.1093/oxfordjournals.epirev.a017924. [DOI] [PubMed] [Google Scholar]
- 18.Broman AT, Hafiz G, Muñoz B, et al. Cataract and barriers to cataract surgery in a US Hispanic population: Proyecto VER. Arch Ophthalmol. 2005;123:1231–6. doi: 10.1001/archopht.123.9.1231. [DOI] [PubMed] [Google Scholar]
- 19.Lamoureux EL, Seang-Mei S, Thumboo J, et al. The impact of corrected and uncorrected refractive error on visual functioning: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci. 2009;50:2614–20. doi: 10.1167/iovs.08-2164. [DOI] [PubMed] [Google Scholar]
- 20.Varma R, Wang MY, Ying-Lai M, et al. Los Angeles Latino Eye Study Group. The prevalence and risk indicators of uncorrected refractive error and unmet refractive need in Latinos: the Los Angeles Study. Invest Ophthalmol Vis Sci. 2008;49:5264–73. doi: 10.1167/iovs.08-1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bourne RR, Dineen BP, Noorul Huq DM, et al. Correction of refractive error in the adult population of Bangladesh: meeting the unmet need. Invest Ophthalmol Vis Sci. 2004;45:410–7. doi: 10.1167/iovs.03-0129. [DOI] [PubMed] [Google Scholar]
- 22.Foran S, Rose K, Wang JJ, Mitchell P. Correctable visual impairment in an older population: the Blue Mountains Eye Study. Am J Ophthalmol. 2002;134:712–9. doi: 10.1016/s0002-9394(02)01673-2. [DOI] [PubMed] [Google Scholar]
- 23.Fotouhi A, Hashemi H, Raissi B, Mohammad K. Uncorrected refractive errors and spectacle utilisation rate in Tehran: the unmet need. Br J Ophthalmol. 2006;90:534–7. doi: 10.1136/bjo.2005.088344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tielsch JM, Sommer A, Witt K, et al. Baltimore Eye Survey Research Group. Blindness and visual impairment in an American urban population: the Baltimore Eye Survey. Arch Ophthalmol. 1990;108:286–90. doi: 10.1001/archopht.1990.01070040138048. [DOI] [PubMed] [Google Scholar]