Abstract
The evolution of the highly pathogenic H5N1 influenza virus produces genetic variations that can lead to changes in antiviral susceptibility and in receptor-binding specificity. In countries where the highly pathogenic H5N1 virus is endemic or causes regular epidemics, the surveillance of these changes is important for assessing the pandemic risk. In Cambodia between 2004 and 2010, there have been 26 outbreaks of highly pathogenic H5N1 influenza virus in poultry and 10 reported human cases, 8 of which were fatal. We have observed naturally occurring mutations in hemagglutinin (HA) and neuraminidase (NA) of Cambodian H5N1 viruses that were predicted to alter sensitivity to neuraminidase inhibitors (NAIs) and/or receptor-binding specificity. We tested H5N1 viruses isolated from poultry and humans between 2004 and 2010 for sensitivity to the NAIs oseltamivir (Tamiflu) and zanamivir (Relenza). All viruses were sensitive to both inhibitors; however, we identified a virus with a mildly decreased sensitivity to zanamivir and have predicted that a V149A mutation is responsible. We also identified a virus with a hemagglutinin A134V mutation, present in a subpopulation amplified directly from a human sample. Using reverse genetics, we verified that this mutation is adaptative for human α2,6-linked sialidase receptors. The importance of an ongoing surveillance of H5N1 antigenic variance and genetic drift that may alter receptor binding and sensitivities of H5N1 viruses to NAIs cannot be underestimated while avian influenza remains a pandemic threat.
INTRODUCTION
Highly pathogenic H5N1 avian influenza virus was first detected in 1997 and has since caused over 500 human infections, with a global fatality rate of around 60% (48). H5N1 virus is now endemic in many countries in Southeast Asia, and sporadic outbreaks in poultry and humans continue to occur. Human-to-human transmission does not occur effectively, and transmission to humans generally occurs via direct contact with infected birds. Highly pathogenic H5N1 viruses could potentially adapt to more effectively transmit between humans and therefore remain a concern as a pandemic threat.
In Cambodia, the H5N1 virus was first detected in wild birds in January 2004 and has since caused 26 outbreaks in poultry and 10 human cases, including 8 fatalities. The 9th and 10th human cases of H5N1 virus infection occurred in December 2009 and April 2010, indicating that the risk of human infection with H5N1 virus remains a concern in Cambodia. Additionally, recent seroprevalence studies in Cambodia have highlighted that asymptomatic H5N1 infections of humans may result in a significant underrepresentation of the H5N1-infected human population (9). As a National Influenza Centre, and in collaboration with the National Veterinary Research Institute in Cambodia (Ministry of Agriculture, Fisheries and Forestry), the Institut Pasteur in Cambodia has isolated and cultured viruses from wild birds, poultry, and humans and conducted genomic analyses. During the last 6 years there has been widespread genetic diversification and an emergence of new clades in the neighboring countries Vietnam, Thailand, and Laos (clade 1, clade 2.3.2, and clade 2.2.4) (5, 39, 42, 44). Cambodian H5N1 strains are thought to have been introduced initially from Thailand and again in subsequent introductions from southern Vietnam (6). Cambodian H5N1 strains are consistently genotype Z, clade 1 viruses, with no other clades being detected to date. Moreover, there is little divergence of these strains over time compared to H5N1 strains in neighboring countries. Cambodian H5N1 strains cluster into 7 sublineages, based on hemagglutinin (HA) sequence analysis (6).
Two classes of influenza virus antiviral drugs are currently commercially available. The adamantanes (amantadine and rimantadine), which target the M2 ion channel protein, have been used extensively worldwide for the treatment and prophylaxis of humans and animals (especially poultry), and resistance to this class of drug emerges rapidly and is now widespread across influenza virus subtypes. All H5N1 clade 1 strains, including Cambodian H5N1 viruses, possess the I26 and N31 substitutions in the M2 protein, which confer resistance to adamantanes (7). Oseltamivir and zanamivir are inhibitors of the neuraminidase enzyme activities of influenza A and B viruses. While few clinical data exist regarding the efficacy of neuraminidase inhibitors (NAIs) for the treatment of H5N1 in humans, there is in vivo evidence of their efficacy in animal models (20, 22, 51). The neuraminidase inhibitors therefore remain the primary control measure for H5N1 influenza virus in the absence of a specific vaccine. Consequently, oseltamivir stockpiling has been a major component of pandemic planning in most countries worldwide.
Resistance to neuraminidase inhibitors can emerge when mutations occur in functional or framework residues that bind the inhibitor (26, 50). Subtype-specific mutations have been extensively documented clinically and in vitro (1, 16, 25, 35). For the N1 subtype, the predominant oseltamivir resistance mutations are H274Y and N294S (N2 numbering) (15). Several other well-described mutations in conserved or semiconserved residues confer resistance or reduced sensitivity to NAIs in N1 subtype viruses, including highly pathogenic H5N1 influenza virus (V116, I117, E119, Q136, K150, D151, D199, and I222) (5, 18, 19, 23). Although resistance normally emerges in response to NAI treatment, several reports described naturally occurring drift mutations, which can alter the susceptibility of H5N1 viruses to neuraminidase inhibitors in the absence of oseltamivir treatment (21, 30, 33, 38). The emergence of widespread oseltamivir resistance in seasonal H1N1 worldwide highlights the potential for the rapid spread of resistance mutations among influenza A virus subtypes (31). Therefore, the surveillance of NAI susceptibility of H5N1 viruses remains a priority.
Another key aspect of influenza virus surveillance is the identification of mutations that alter the HA receptor-binding specificity. Highly pathogenic avian H5N1 influenza viruses have a low affinity for α2,6-linked sialic acid receptors expressed highly in human cells and preferentially bind α2,3-linked receptors (11, 12, 36). Ultimately, a highly pathogenic avian H5N1 virus that can evolve to more efficiently bind human receptors can potentially transmit more easily from human to human and therefore represents a pandemic risk. Several mutations that can alter binding specificity have been identified. In particular, the HA substitutions Q226L and G228S (H3 numbering) are known to influence adaptation to human receptor specificity (37, 43). Additionally, there have been reports of A134V, L129A, and S227N mutations in HA of H5N1 viruses, which also increased the affinity of HA for α2,6-linked receptors (3, 13). The A134V mutation occurred concurrently with an L129A mutation in about 50% of clones generated directly from a virus isolated from a fatal human case (A/Thailand/676/2005) (3).
This study aims to describe the drug sensitivity profile of endemic, highly pathogenic H5N1 viruses isolated in Cambodia during a 6-year period and to identify viruses with potentially increased affinity for human-type α2,6-linked receptors. Indeed, the rigorous surveillance of H5N1 molecular changes and drug sensitivity profiling continue to reveal new information relevant to predicting the pandemic threat of highly pathogenic H5N1 viruses. This is particularly important in countries like Cambodia, where H5N1 is endemic and cocirculating with the 2009 pandemic H1N1 virus.
MATERIALS AND METHODS
Viruses.
Viruses were isolated from poultry and human (bronchoalveolar lavage) clinical specimens at the Institut Pasteur in Cambodia and propagated on MDCK cells or by egg inoculation where specified. An A/H1N1 virus isolated in Cambodia in 2009 (A/CAM/S12007/09) was used as a control human seasonal influenza virus. A/H1N1 viruses used as controls for NA enzyme inhibition tests (A/Mississippi/3/01 wild-type [wt] and H274Y resistant viruses) were kindly provided by Ian Barr and Aeron Hurt at the WHO Reference Centre for Influenza Research, Parkville, Melbourne, Australia. All experiments with highly pathogenic H5N1 virus were conducted in a biosafety level 3 (BSL3) containment facility. Viruses were stored at −80°C.
RNA extraction, RT-PCR, and sequencing.
Viral RNA was extracted from 200 μl of clinical specimen, MDCK supernatant, or egg allantoic fluid using the QIAamp viral RNA kit according to the manufacturer's recommendations (Qiagen, Germany). For the sequencing of the HA and NA genes, reverse transcription (RT)-PCRs were performed with HA5- and NA1-specific primers (see Table S1 in the supplemental material for primer sequences) and the Qiagen One-Step RT-PCR kit (Qiagen, Germany). PCR products were sequenced by using an ABI 3730XL automatic DNA analyzer (Macrogen, South Korea).
Neuraminidase enzyme inhibition assay.
A chemiluminescence-based NA enzyme inhibition assay (NA Star; Applied Biosystems, CA) was used to test cultured viruses for their sensitivities to oseltamivir carboxylate (oseltamivir) and zanamivir, as described previously (8). Briefly, 25 μl of virus diluted in NA Star buffer was dispensed into white CulturPlate 96-well plates in duplicate rows. Serial 5-fold dilutions of zanamivir or oseltamivir carboxylate were prepared in assay buffer, and 25 μl of each dilution was added to wells (final drug concentrations ranging from 6,250 nM to 0.0032 nM). Plates were incubated at 37°C, with shaking for 15 min. Ten microliters of NA Star substrate (100 μM) was added, followed by incubation at 37°C for 15 min. Sixty microliters of Light Emission Accelerator II solution was added, and the plate was read with an Envision multilabel plate reader (Perkin-Elmer). Oseltamivir carboxylate, zanamivir, and 4-amino-4-deoxy-Neu5Ac2en were provided by the Institute of Glycomics, Griffith University, Gold Coast, Australia. Compounds were prepared in distilled water and stored at −20°C until the time of use. The concentration of the drug (average of duplicates) required to inhibit 50% of the NA activity (IC50) was calculated by using the nonlinear curve-fitting function in the Graphpad Prism 4 package (Graphpad, La Jolla, CA). The average IC50 (nM) (± standard deviation) from two independent determinations was calculated for each virus. Outliers of more than 2 standard deviations from the overall mean were tested 6 times.
Generation of recombinant viruses.
Recombinant viruses were generated by using the 8-plasmid reverse genetics (RG) system. The HA and NA genes of H5N1 strains A/Cambodia/408008/05 (GenBank accession numbers HQ664438 for HA and HQ664439 for NA) and A/Chicken/Cambodia/022LC2b/2005 (accession numbers HG664945 for HA and EF473077 for NA) were amplified by using the primers described in Table S1 in the supplemental material, cloned into pCR2.1-TA vectors (Invitrogen, CA), and subcloned into vector pHW2000, as described previously (17, 45). The fidelity of inserts was confirmed by the sequencing of all plasmids. Point mutations were introduced by using a Stratagene site-directed mutagenesis kit (Stratagene, CA) and confirmed by sequencing. HA and NA plasmids were combined with plasmids containing M, PB1, PB2, NS, NP, and PA gene segments from A/WSN/33 H1N1, which were kindly provided by Leo Poon (Department of Microbiology, University of Hong Kong, Hong Kong, SAR, China) and Richard Webby (St. Jude Children's Research Hospital, Memphis, TN). Reverse genetics viruses were generated by transfecting plasmids in cocultured 293T and MDCK cells by using Fugene 6 reagent (Roche) and by expanding recombinant viruses on MDCK cells. Sequencing of the HA and NA RNAs of all recombinant viruses was conducted following RT-PCR in order to verify that no additional sequence changes had occurred.
Viral infectivity and hemagglutination assays.
To compare the infectivities of viruses on MDCK cells or MDCK-SIAT cells, which stably express increased levels of α2,6-linked glycan receptors (29), we determined the dose of virus required to infect 50% of cells (50% tissue culture infective dose [TCID50]). Ninety-six-well plates were seeded with MDCK or MDCK-SIAT1 cells, which were grown to confluence overnight and then infected with quadruplicate 10-fold dilutions of virus. Four days after infection, wells were scored for cytopathic effects, and TCID50 values were calculated according to the method of Reed and Muench (34). Hemagglutination titers were measured by using 0.5% guinea pig red blood cells (RBCs) or, for particular experiments, horse or human (type O) red blood cells. Statistical significance was calculated from an unpaired two-tailed t test with the Graphpad Prism package.
RESULTS
Receptor-binding specificity of Cambodian H5N1 strains.
Between 2004 and 2010, 92 H5N1 strains were detected in humans and animals. Fifty-seven representative viruses were selected and sequenced directly from the original clinical specimen or after propagation on MDCK cells. All Cambodian H5N1 strains retained the amino acids on the HA gene typically associated with avian influenza virus-type receptor specificity (Q226 and S227) (4); however, we detected one virus (A/CAM/408008/05) with an HA mutation (A134V) present in a subpopulation amplified from a specimen from a fatally infected patient. This mutation was previously reported for a subpopulation of strain A/Thailand/676/2005 (GenBank accession number DQ360835), occurring alone or in combination with an L129V substitution, where it was shown to enhance receptor binding to human-type α2,6-linked sialic acid receptors in addition to avian-type α2,3-linked sialic acid receptors (3). We expanded the virus from the patient sample on MDCK cells and embryonated hen eggs and assessed the prevalence of this mutation in the viral populations. The A134V mutation was present in approximately 45% of viruses in the original specimen, 75% of viruses following three passages on MDCK cells, and 60% of viruses after 4 passages on eggs, as assessed by eye from the chromatograms of HA gene sequences (data not shown).
To investigate whether the A134V mutation in A/CAM/408008/05 could change the receptor-binding specificity from an α2,3-linked receptor preference to an α2,6-linked receptor preference, we generated viruses by reverse genetics with the HA wild type (wt) or mutant (A134Vm) from A/CAM/408008/05 and the other gene segments from A/WSN/33 H1N1 (V1 and V2, respectively) (Table 1) or HA (A134Vm) and NA (wt) derived from A/CAM/408008/05 (V3) (Table 1). Additionally, we generated viruses with HA and NA or NA alone both derived from the A/Chicken/Cambodia/022LC2b/05 (A/Ck/CAM/022LC2b/05) field isolate (V4 and V5, respectively) (Table 1).
Table 1.
Reverse genetics viruses generated in this study
| Virus | Segments from A/WSN/33 | H5N1 segment substitution(s) | Donor strain | Additional mutation |
|---|---|---|---|---|
| V1 | NA, PB2, PB1, M, PA, NS, NP | HA | A/CAM/408008/05 | wt |
| V2 | NA, PB2, PB1, M, PA, NS, NP | HA | A/CAM/408008/05 | HA A134Vm |
| V3 | PB2, PB1, M, PA, NS, NP | HA + NA | A/CAM/408008/05 | HA A134Vm |
| V4 | PB2, PB1, M, PA, NS, NP | HA + NA | A/Ck/CAM/022LC2b | wt |
| V5 | HA, PB2, PB1, M, PA, NS, NP | NA | A/Ck/CAM/022LC2b | wt |
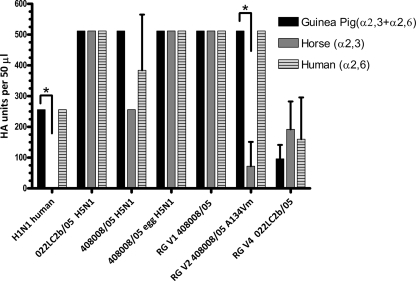
Previous studies have shown that hemagglutination assays with red blood cells (RBCs) from different species or sialidase-treated RBCs can provide interesting information about receptor specificity due to the different receptor contents of the RBCs (3, 24, 40). For example, human H3N2 influenza viruses cannot agglutinate horse RBCs due to their lack of α2,6-linked receptors (24). To investigate the receptor-binding properties of wild-type A/CAM/408008/05 reverse genetics viruses V1 (HA wt) and V2 (HA A134Vm), we conducted hemagglutination assays with horse RBCs, which contain predominantly α2,3-linked receptors; human RBCs, which contain predominantly α2,6-linked receptors; and guinea pig RBCs, which contain both types of receptors (24). Human RBCs, like human lung epithelial cells, express low levels of α2,3-linked receptors; however, horse RBCs contain virtually only α2,3-linked receptors (24, 32). As a control, we tested a human seasonal H1N1 influenza virus strain from Cambodia. This virus could agglutinate the human and guinea pig RBCs to the same degree but had no capacity to agglutinate horse RBCs (Fig. 1), consistent with the absence of α2,6-linked receptors on these RBCs. The wild-type A/CAM/408008/05 virus, which was grown on MDCK cells, had a slightly but not significantly reduced sensitivity to horse blood cells compared to guinea pig blood cells (Fig. 1). The wild-type A/CAM/408008/05 virus grown on eggs could agglutinate all types of RBCs to the same degree. We noted significant differences between the hemagglutination capacities of the reverse genetics viruses V1 (HA wt) and V2 (HA A134Vm) for horse and human RBCs. The reverse genetics virus A/CAM/408008/05 V2 (HA A134Vm) had a 7-fold-reduced hemagglutination titer for horse RBCs in comparison to other RBCs (P ≤ 0.015), suggesting a reduction in affinity toward avian α2,3-linked receptors. Wild-type field isolate A/Ck/CAM/022LC2b H5N1 and the reverse genetics virus with A/Ck/CAM/022LC2b HA (V4) could agglutinate all types of RBCs to the same degree (Fig. 1).
Fig. 1.
Comparative hemagglutination capacities of A/CAM/408008/05 and A/Ck/CAM/022LC2b/05 wild-type and reverse genetics (RG) viruses. Suspensions of guinea pig, horse, and human type O blood (0.75%) were used for hemagglutination assays. Viruses are seasonal human H1N1 virus (A/CAM/S12007/09), wild-type H5N1 strains A/Ck/CAM/022LC2b/05 and A/CAM/408008/05 passaged on MDCK cells, A/CAM/408008/05 virus passaged on eggs, the reverse genetics (RG) virus V1 A/CAM/408008/05 with HA (wt), RG virus V2 A/CAM/408008/05 with HA A134Vm, or RG virus V4 A/Ck/CAM/022LC2b/05 HA (wt). Results represent the averages ± standard deviations (where results were not identical) from two independent experiments, and the asterisks indicate a statistically significant difference (P ≤ 0.015).
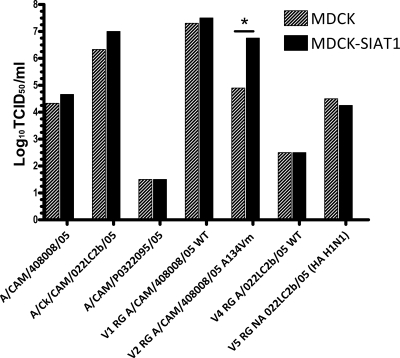
The viral infectivity of cell lines and eggs during the initial phase of the infection is dependent on the compatibility of the virus receptor-binding protein (HA) with the receptors in the cellular or egg growth model. Given the changes in the hemagglutination sensitivity of the V2 RG A/CAM/408008/05 A134Vm virus that we observed, we compared the infectivities of the A/CAM/408008/05 and A/Ck/CAM/022LC2b/05 wild-type and reverse genetics viruses on different cell types. We directly compared the dose of virus required to infect 50% of MDCK cells (TCID50), which contain predominantly α2,3-linked receptors, to that of MDCK-SIAT1 cells, which express higher levels of α2,6-linked receptors (Fig. 2) (29). Wild-type virus A/CAM/408008/05 (containing a mixed population of 134A and 134V) showed similar infectivities with both MDCK-SIAT and MDCK cells, as did A/CAM/P0322095 and A/Ck/CAM/022LC2b/05, which were used for comparison. The V2 RG A/CAM/408008/05 A134Vm virus, which is less efficient at agglutinating horse RBCs, showed a significantly enhanced infectivity on MDCK-SIAT cells (6.75 log10 TCID50/ml compared to 4.9 log10 TCID50/ml on MDCK cells; P ≤ 0.005) (Fig. 2). Similar to the wild-type viruses, RG V1 A/CAM/408008/05 (wt), V4 RG A/Ck/CAM/022LC2b (wt), and V5 RG A/Ck/CAM/022LC2b NA (HA from the WSN33/H1N1 virus) had comparable infectivities in both cell types (Fig. 2).
Fig. 2.
Virus infectivity on MDCK and MDCK-SIAT1 cells. Viruses are wild-type H5N1 strains A/CAM/408008/05, A/Ck/CAM/022LC2b/05, A/CAM/P0322095/05, the reverse genetics (RG) virus V1 A/CAM/408008/05 with HA (wild type), the RG virus V2 A/CAM/408008/05 with HA-A134Vm (mutant), the RG virus V4 A/Ck/CAM/022LC2b/05 with HA (wild type), or the RG virus V5 A/Ck/CAM/022LC2b/05 NA (HA from WSN33/H1N1 virus). Viruses were inoculated onto MDCK or MDCK-SIAT cells in quadruplicate, and TCID50 titers were calculated by using the method of Reed and Muench (34). TCID50 titers (log10 TCID50/ml) are shown as the averages of duplicate experiments. The asterisk shows a statistically significant difference calculated from triplicate experiments (P ≤ 0.005). Minimal interexperimental differences were observed.
Neuraminidase inhibitor sensitivity of Cambodian H5N1 strains.
To address whether naturally occurring mutations can cause changes in sensitivity to neuraminidase inhibitors in the absence of drug treatment and in a relatively homogenous population of H5N1 viruses, we endeavored to phenotypically test all H5N1 strains that were successfully amplified on MDCK cells, excluding those that were genetically identical in the HA and NA genes. Sequence analysis of these viruses revealed no classical resistance mutations or mutations that are associated with a known reduced sensitivity to NAIs (V116, I117, E119, Q136, K150, D151, D199, I223, H275, and N295) (18, 19, 23, 33). However, several other mutations were detected that could eventually modify sensitivity to neuraminidase inhibitors, since they are located within or near the catalytic site. Therefore, we screened 24 highly pathogenic H5N1 viruses isolated between 2004 and 2010 for sensitivity to the neuraminidase inhibitors oseltamivir and zanamivir. The overall average IC50s of these Cambodian clade 1 H5N1 viruses were 0.20 ± 0.14 nM for oseltamivir and 0.40 ± 0.21 nM for zanamivir (Table 2).
Table 2.
Neuraminidase enzyme inhibition assay of Cambodian H5N1 viruses
| Strain | Mean IC50 (nM) ± SDa |
|
|---|---|---|
| Oseltamivir | Zanamivir | |
| A/Gray Herron/CAM/29/04 | 0.07 ± 0.001 | 0.05 ± 0.05 |
| A/Crest Serpent Eagle/CAM/04 | 0.02 ± 0.01 | 0.18 ± 0.05 |
| A/Ck/CAM/022LC2b/05 | 0.33 ± 0.08 | 0.15 ± 0.03 |
| A/CAM/408008/05 | 0.09 ± 0.05 | 0.30 ± 0.03 |
| A/CAM/P0322095/2005 | 0.77 ± 0.07 | 3.35 ± 1.49d |
| A/CAM/Q0321176/06 | 0.30 ± 0.07 | 0.13 ± 0.02 |
| A/Dk/CAM/D5KC167/06 | 0.09 ± 0.01 | 0.34 ± 0.07 |
| A/Dk/CAM/D14AL/06 | 0.15 ± 0.02 | 0.75 ± 0.24 |
| A/CAM/R0405050/07 | 0.29 ± 0.07 | 0.30 ± 0.02 |
| A/Dk/CAM/D8G/07 | 0.13 ± 0.07 | 0.46 ± 0.34 |
| A/Ck/CAM/LC1AL/07 | 0.23 ± 0.05 | 0.15 ± 0.05 |
| A/Dk/CAM/674F/07 | 0.30 ± 0.10 | 0.26 ± 0.10 |
| A/Dk/CAM/671F/07 | 0.27 ± 0.08 | 0.54 ± 0.16 |
| A/CAM/S1211394/08 | 0.13 ± 0.05 | 0.45 ± 0.06 |
| A/Ck/CAM/TLC1/09 | 0.09 ± 0.01 | 0.36 ± 0.06 |
| A/Ck/CAM/TLC2/09 | 0.13 ± 0.01 | 0.37 ± 0.01 |
| CK/CAM/TK/CMB8F/10 | 0.10 ± 0.01 | 0.4 ± 0.08 |
| A/Dk/CAM/TK007D5T/10 | 0.16 ± 0.04 | 0.65 ± 0.19 |
| A/CAM/PV/U0417030/10 | 0.18 ± 0.01 | 0.61 ± 0.07 |
| A/CK/CAM/TK/CMB5F/10 | 0.23 ± 0.08 | 0.56 ± 0.28 |
| A/CK/CAM/TK/CMB1F/10 | 0.25 ± 0.11 | 0.85 ± 0.35 |
| A/Ck/CAM/CMB5T/10 | 0.26 ± 0.03 | 0.56 ± 0.07 |
| A/Ck/CAM/TK/CMB8T/10 | 0.13 ± 0.01 | 0.66 ± 0.14 |
| A/Ck/CAM/PV025LC2/10 | 0.20 ± 0.23 | 0.23 ± 0.07 |
| A/Mississippi/3/01 wild typeb | 0.38 ± 0.18 | 0.58 ± 0.08 |
| A/Mississippi/3/01 mutantb | 137.5 ± 2.47 | 0.99 ± 0.90 |
| Avg Cambodian H5N1c | 0.20 ± 0.14 | 0.40 ± 0.21 |
Results represent means ± standard deviations from two independent determinations.
H1N1 A/Mississippi/3/01 wild-type and H274Y mutant control viruses known to be susceptible and resistant, with known IC50s, were assayed in parallel experiments. Ck, chicken; Dk, duck; CAM, Cambodia.
The average mean IC50s (± standard deviations) for oseltamivir and zanamivir were calculated by excluding outliers.
Outlier.
Strain A/CAM/P0322095/2005 had an approximately 8-fold-reduced sensitivity to zanamivir (IC50 of 3.35 nM) compared to the mean IC50 (0.4 nM). This IC50 remains in the sensitive range; however, we endeavored to examine mutations in the NA of this virus, which could account for the loss in sensitivity. Strain A/CAM/P0322095/2005 has 8 amino acid substitutions in NA (V16I, V34I, T40A, E77K, K78R, V149A, A395T, and V424I) relative to other Cambodian strains that tested sensitive to zanamivir. Visual inspection of the crystal structures of existing influenza virus N1 sialidases and observation of the positions of the above-described mutations relative to the active site suggest that the V149A mutation, which is proximal to the previously identified flexible 150 loop in influenza A virus group 1 neuraminidases (36a), was the most likely mutation to be responsible for the altered sensitivity.
DISCUSSION
Novel mutations associated with resistance or altered sensitivity are continually reported as a result of routine drug sensitivity testing of influenza viruses (5, 30, 33). In a previous study, clade 1 strains isolated in Cambodia in 2005 that were lacking classical resistance mutations were found to have a 6- to 7-fold decrease in sensitivity to oseltamivir compared to viruses isolated in 2004 (average IC50 of 0.41 nM in 2004 compared to 2.88 nM in 2005) (30). That same study determined that clade 2 viruses isolated from Indonesia were 30-fold less sensitive to oseltamivir, suggesting that drift mutations in the absence of oseltamivir treatment can lead to reduced sensitivity over time, which is a cause for concern and vigilant ongoing surveillance. In our study, H5N1 viruses isolated in 2004 were highly sensitive (average IC50s of 0.05 ± 0.04 nM for oseltamivir and 0.12 ± 0.09 nM for zanamivir), and viruses isolated from 2005 onwards had slightly higher IC50s (average IC50s of 0.22 ± 0.14 nM for oseltamivir and 0.43 ± 0.20 nM for zanamivir, excluding one outlier, strain A/CAM/P0322095/2005); however, they were still within the highly sensitive range. Our findings from several outbreak sources during 2005 and subsequent years suggest that there has been no significant decrease in sensitivity to oseltamivir or zanamivir over time. These results suggest that Cambodian clade 1 highly pathogenic H5N1 influenza viruses are fully susceptible to both oseltamivir and zanamivir.
It is noteworthy that the A/CAM/408008/05 virus was previously shown by Rameix-Welti and colleagues to be highly sensitive to oseltamivir, with an IC50 of 0.14 nM (33). That study directly assayed the recombinant purified NA enzyme of A/CAM/408008/05 in a virus-free system and revealed an inhibition constant (Ki) of 0.073 ± 0.006 nM, much lower than those of the other viruses that were tested in the same study, A/Hong Kong/156/97 (Ki of 0.37 ± 0.12 nM) and A/Paris/0650/04 (Ki of 0.31 0.04 nM) (33). The incorporation of the H274Y mutation in A/CAM/408008/05 resulted in an IC50 of 24 ± 2 nM, measured from the recombinant purified NA protein. In comparison to the typical sensitivity changes that have been described for other NA enzymes (between 100 and 1,000 nM), this reduction in sensitivity is less significant and remains within the predicted sensitive range (21), suggesting that a virus with this mutation would remain more sensitive to oseltamivir than other H5 NA enzymes with the H274Y mutation. This prompted us to generate reverse genetics viruses derived from A/CAM/408008/05 and A/Ck/022LC2b/05. Additionally, we attempted to generate several viruses containing point mutations in both HA and NA of A/CAM/408008/05. The NA segment from A/CAM/408008/05 could not be combined with the other 7 gene segments from H1N1 strain A/WSN/33 to yield a viable virus, suggesting an incompatibility with the genetic background of A/WSN/33 H1N1. Moreover, NA of A/CAM/408008/05 was unable to combine with its counterpart HA-A134Vm but would combine with HA (wt) of A/CAM/408008/05 in the background of A/WSN/33 H1N1. This finding suggests that the HA and NA activities are carefully balanced in the A/CAM/408008/05 virus such that NA alone cannot combine with gene segments derived from A/WSN/H1N1, and point mutations can disrupt the balance of HA and NA. We introduced several mutations into NA of the A/CAM/408008/05 virus with the intention to study the effect of these mutations on sensitivity to neuraminidase inhibitors (S246G, S246N, V149A, Q136K, and H274Y); however, we could not successfully generate viruses with these point mutations in NA of A/CAM/408008/05, in combination with either HA of A/WSN/33 or HA of A/CAM/408008/05 (both 134A and 134V variants). The reasons for this are unclear. Although we cannot completely rule out a technical problem, the parallel generation of viruses containing all gene segments from A/WSN/33 H1N1 or containing gene segments from A/Ck/022LC2b/05 successfully produced virus. Comparatively, viruses derived from strain A/Ck/022LC2b/05 were more easily produced, with higher hemagglutination titers, both with NA alone and with HA and NA combined, in the background of A/WSN/33. It is possible that these point mutations reduced the enzymatic activity of A/CAM/408008/05 NA, which was previously shown to have a lower enzymatic activity than other influenza A viruses, such as both A/Hong Kong/156/97 H5N1 and A/Paris/0650/04 H1N1 (33). Point mutations are often associated with a reduction of NA enzyme activity and viral fitness, and certain fitness compromises are deleterious for viral replication. Specifically, the Q136K mutation, which we attempted to introduce in this study, was previously shown to reduce NA activity by 75% in H3N2 reverse genetics viruses (28). This suggests that these mutations would not occur naturally in the A/CAM/408008/05 virus, and it would be useful to try different genetic backgrounds. The incompatibility of several gene combinations and/or point mutations for the generation of reverse genetics viruses have been described frequently (1, 10, 23, 49).
Few studies have explored the association of certain amino acid residues with “hypersensitivity” to neuraminidase inhibitors in order to identify strains less likely to become resistant to these drugs. In A/CAM/408008/05, the active-site residues G248 and H252 are predicted to contribute to the high-affinity interaction of the NA with the substrate, and residue S246 is predicted to stabilize this interaction (33), as this amino acid was previously shown to participate in hydrogen bonding with sialic acids (27). Therefore, it was expected that the S246G mutation present in strain A/Ck/CAM/022LC2b/05 would result in reduced sensitivity to oseltamivir (33). Supporting this theory, an S246N mutation was recently reported for an H5N1 virus from Laos, which caused a 24-fold reduction in sensitivity to oseltamivir (5). In our study the IC50 of A/Ck/CAM/022LC2b/05 was within the average range (Table 2) but marginally reduced only in comparison to “hypersensitive” strain A/CAM/408008/05 (IC50s of 0.33 nM and 0.09 nM, respectively). Likewise, the average IC50 of the RG viruses derived from A/Ck/CAM/022LC2b/05 (V4 and V5) was 0.34 nM (data not shown), suggesting that the S246G mutation does not result in reduced sensitivity to oseltamivir, at least in this genetic background.
We identified one strain (A/CAM/P0322095/2005) with an 8-fold-reduced sensitivity to zanamivir (3.35 ± 1.49 nM). This remains within the predicted sensitive range (21); however, the IC50 thresholds for what can be considered “reduced sensitivity” and “resistance” are poorly defined. Typically, fluorescence-based [2′-(4-methylumbellifenyl)-α-d-N-acetyl-neuramic acid (MUNANA)] and chemiluminescence-based (NA Star) assays have different sensitivities. For example, the NA Star assay used in this study has been frequently reported to be more sensitive and therefore to produce lower IC50s (46). The importance of monitoring IC50 changes, even those not likely to cause in vivo resistance, cannot be underestimated for predicting the ability of NA to evolve the capacity to evade inhibition and can provide useful information for rational drug design. Therefore, we endeavored to predict the mutation responsible for the reduced sensitivity of strain A/CAM/P0322095/2005 to zanamivir, and we propose that the V149A mutation within the 150 loop region is responsible. Although we were unable to verify this by reverse genetics, there are strong molecular data supporting this prediction. The 150 loop in group 1 sialidases is dynamic and flexible, and by altering an amino acid within the loop, such as the V149A substitution, it is likely that the balance between open- and closed-loop forms will be altered (2). In the open form of the 150 loop the main differences (excluding residues involved directly in the loop) are seen in residues Glu119, Asp151, and Arg156. Glu119 and Asp151, both negatively charged residues, are shifted away from what is traditionally known as the C4 pocket of the active site, which is where the positively charged guanidine group of zanamivir binds. The side chain of Arg156 (positively charged) is also shifted so that it would be closer to the guanidine group of bound zanamivir. This suggests that zanamivir would bind less favorably to the open 150 loop form of a group 1 sialidase than to the closed 150 loop form, and any mutations (such as V149A) that favored the open form over the closed form would see a reduction in the affinity for zanamivir.
Amino acid substitutions in the HA gene can additionally contribute to antiviral susceptibility due to the altered viral fitness and infectivity resulting from changes to the balance of HA and NA activities. Cell-based plaque reduction assays can be used to explore these questions; however, they are not always suitable depending on the receptor-binding specificity and plaque-forming properties of the virus to be tested and can provide misleading results (14, 41, 47). For this reason, in vitro NA inhibition assays are considered the most reliable estimation of in vivo neuraminidase inhibitor susceptibility (52). We conducted plaque reduction assays with strain A/CAM/408008/05 to examine whether the 134V mutation could change susceptibility to NAIs; however, this virus produced abnormal plaques, which could not be reliably counted. There is a need for the development of more reliable cell-based assays for addressing these questions.
The increased affinity of HA of highly pathogenic H5N1 viruses for human α2,6-linked receptors, which are expressed in the lower respiratory tract, is considered a prerequisite for a pandemic H5N1 strain. The HA substitution A134V that we detected in our study was previously reported for 50% of sequences from a clinical specimen originating from a fatal H5N1 case, occurring concurrently with an L129V substitution in 45.6% of viruses (3). Auewarakul and colleagues previously produced reverse genetics viruses with L129V/A134V substitutions; however, they could not generate a virus with the A134V substitution alone (3). Using direct binding assay with sialylglycopolymers and hemagglutination assays, those authors predicted that the A134V mutation results in dual specificity for α2,3-linked and α2,6-linked receptors. In our study, we also detected the A134V mutation in approximately half of the viral sequences amplified directly from a specimen derived from a fatal H5N1 case; however, we did not detect the A129V mutation in these viruses. The A134V mutation was selected after passage in both MDCK cells and eggs, which is unexpected given that the 134V mutation should reduce binding to the receptors typically associated with MDCK cells and eggs, suggesting either that this mutation enhances viral infectivity independent of receptor-binding specificity or that a mutation in another viral gene is somehow enhancing the selection of this 134V mutation. We succeeded in generating reverse genetics viruses containing the A134V mutation. Similar to the human H1N1 strain, the reverse genetics virus containing the A134V mutation had a reduced capacity to agglutinate horse blood, compared to those of other H5N1 viruses tested, and enhanced growth on MDCK-SIAT1 cells. These results provide further evidence that the A134V mutation in HA can change the receptor-binding specificity of H5N1 viruses from an avian α2,3-linked to a human α2,6-linked binding preference. Naturally occurring mutations that are markers of pandemic viruses should be monitored vigilantly. The ongoing surveillance of known and novel mutations involved in neuraminidase inhibitor sensitivity and receptor-binding specificity are currently the most informative aspects of pandemic risk assessments.
Supplementary Material
ACKNOWLEDGMENTS
We are very grateful to Ian Barr (WHO Reference Centre, Melbourne, Australia) for providing the reference viruses used for NA Star assays. We thank Rith Sareth and other members of the Virology Unit at the Institut Pasteur in Cambodia for technical assistance. We thank Aeron Hurt (WHO Reference Centre, Melbourne, Australia) for technical advice and Vincent Deubel, Director of the Institut Pasteur in Cambodia, for his valuable comments on the manuscript.
This study was supported by the French Agency for Development (SISEA project) and the Office of the Assistant Secretary for Preparedness and Response within the U.S. Department of Health and Human Services.
Footnotes
Supplemental material for this article may be found at http://aac.asm.org/.
Published ahead of print on 22 February 2011.
REFERENCES
- 1. Abed Y., Baz M., Boivin G. 2006. Impact of neuraminidase mutations conferring influenza resistance to neuraminidase inhibitors in the N1 and N2 genetic backgrounds. Antivir. Ther. 11:971–976 [PubMed] [Google Scholar]
- 2. Amaro R. E., Cheng X., Ivanov I., Xu D., McCammon J. A. 2009. Characterizing loop dynamics and ligand recognition in human- and avian-type influenza neuraminidases via generalized born molecular dynamics and end-point free energy calculations. J. Am. Chem. Soc. 131:4702–4709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Auewarakul P., et al. 2007. An avian influenza H5N1 virus that binds to a human-type receptor. J. Virol. 81:9950–9955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ayora-Talavera G., et al. 2009. Mutations in H5N1 influenza virus hemagglutinin that confer binding to human tracheal airway epithelium. PLoS One 4:e7836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Boltz D. A., et al. 2009. Emergence of H5N1 avian influenza viruses with reduced sensitivity to neuraminidase inhibitors and novel reassortants in Lao People's Democratic Republic. J. Gen. Virol. 91:949–959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Buchy P., et al. 2009. Molecular epidemiology of clade 1 influenza A viruses (H5N1), Southern Indochina Peninsula, 2004-2007. Emerg. Infect. Dis. 15:1641–1644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Buchy P., et al. 2007. Influenza A/H5N1 virus infection in humans in Cambodia. J. Clin. Virol. 39:164–168 [DOI] [PubMed] [Google Scholar]
- 8. Buxton R. C., et al. 2000. Development of a sensitive chemiluminescent neuraminidase assay for the determination of influenza virus susceptibility to zanamivir. Anal. Biochem. 280:291–300 [DOI] [PubMed] [Google Scholar]
- 9. Cavailler P., et al. 2010. Seroprevalence of anti-H5 antibody in rural Cambodia, 2007. J. Clin. Virol. 48:123–126 [DOI] [PubMed] [Google Scholar]
- 10. Chen L. M., Davis C. T., Zhou H., Cox N. J., Donis R. O. 2008. Genetic compatibility and virulence of reassortants derived from contemporary avian H5N1 and human H3N2 influenza A viruses. PLoS Pathog. 4:e1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Connor R. J., Kawaoka Y., Webster R. G., Paulson J. C. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17–23 [DOI] [PubMed] [Google Scholar]
- 12. Couceiro J. N., Paulson J. C., Baum L. G. 1993. Influenza virus strains selectively recognize sialyloligosaccharides on human respiratory epithelium; the role of the host cell in selection of hemagglutinin receptor specificity. Virus Res. 29:155–165 [DOI] [PubMed] [Google Scholar]
- 13. Gambaryan A., et al. 2006. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology 344:432–438 [DOI] [PubMed] [Google Scholar]
- 14. Gubareva L. V., Kaiser L., Matrosovich M. N., Soo-Hoo Y., Hayden F. G. 2001. Selection of influenza virus mutants in experimentally infected volunteers treated with oseltamivir. J. Infect. Dis. 183:523–531 [DOI] [PubMed] [Google Scholar]
- 15. Gubareva L. V., Webster R. G., Hayden F. G. 2002. Detection of influenza virus resistance to neuraminidase inhibitors by an enzyme inhibition assay. Antiviral Res. 53:47–61 [DOI] [PubMed] [Google Scholar]
- 16. Herlocher M. L., et al. 2002. Influenza virus carrying an R292K mutation in the neuraminidase gene is not transmitted in ferrets. Antiviral Res. 54:99–111 [DOI] [PubMed] [Google Scholar]
- 17. Hoffmann E., Neumann G., Kawaoka Y., Hobom G., Webster R. G. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108–6113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hurt A. C., Holien J. K., Barr I. G. 2009. In vitro generation of neuraminidase inhibitor resistance in A(H5N1) influenza viruses. Antimicrob. Agents Chemother. 53:4433–4440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hurt A. C., Holien J. K., Parker M., Kelso A., Barr I. G. 2009. Zanamivir-resistant influenza viruses with a novel neuraminidase mutation. J. Virol. 83:10366–10373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hurt A. C., Lowther S., Middleton D., Barr I. G. 2010. Assessing the development of oseltamivir and zanamivir resistance in A(H5N1) influenza viruses using a ferret model. Antiviral Res. 87:361–366 [DOI] [PubMed] [Google Scholar]
- 21. Hurt A. C., et al. 2007. Susceptibility of highly pathogenic A(H5N1) avian influenza viruses to the neuraminidase inhibitors and adamantanes. Antiviral Res. 73:228–231 [DOI] [PubMed] [Google Scholar]
- 22. Ilyushina N. A., et al. 2008. Oseltamivir-ribavirin combination therapy for highly pathogenic H5N1 influenza virus infection in mice. Antimicrob. Agents Chemother. 52:3889–3897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ilyushina N. A., Seiler J. P., Rehg J. E., Webster R. G., Govorkova E. A. 2010. Effect of neuraminidase inhibitor-resistant mutations on pathogenicity of clade 2.2 A/turkey/15/06 (H5N1) influenza virus in ferrets. PLoS Pathog. 6:e1000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ito T., et al. 1997. Receptor specificity of influenza A viruses correlates with the agglutination of erythrocytes from different animal species. Virology 227:493–499 [DOI] [PubMed] [Google Scholar]
- 25. Jackson D., Barclay W., Zurcher T. 2005. Characterization of recombinant influenza B viruses with key neuraminidase inhibitor resistance mutations. J. Antimicrob. Chemother. 55:162–169 [DOI] [PubMed] [Google Scholar]
- 26. Lackenby A., Thompson C., Democratis J. 2008. The potential impact of neuraminidase inhibitor resistant influenza. Curr. Opin. Infect. Dis. 21:626–638 [DOI] [PubMed] [Google Scholar]
- 27. Landon M. R., et al. 2008. Novel druggable hot spots in avian influenza neuraminidase H5N1 revealed by computational solvent mapping of a reduced and representative receptor ensemble. Chem. Biol. Drug Des. 71:106–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lu B., Zhou H., Ye D., Kemble G., Jin H. 2005. Improvement of influenza A/Fujian/411/02 (H3N2) virus growth in embryonated chicken eggs by balancing the hemagglutinin and neuraminidase activities, using reverse genetics. J. Virol. 79:6763–6771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Matrosovich M., Matrosovich T., Carr J., Roberts N. A., Klenk H. D. 2003. Overexpression of the alpha-2,6-sialyltransferase in MDCK cells increases influenza virus sensitivity to neuraminidase inhibitors. J. Virol. 77:8418–8425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. McKimm-Breschkin J. L., Selleck P. W., Usman T. B., Johnson M. A. 2007. Reduced sensitivity of influenza A (H5N1) to oseltamivir. Emerg. Infect. Dis. 13:1354–1357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Meijer A., et al. 2009. Oseltamivir-resistant influenza virus A (H1N1), Europe, 2007-08 season. Emerg. Infect. Dis. 15:552–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Nicholls J. M., Bourne A. J., Chen H., Guan Y., Peiris J. S. 2007. Sialic acid receptor detection in the human respiratory tract: evidence for widespread distribution of potential binding sites for human and avian influenza viruses. Respir. Res. 8:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rameix-Welti M. A., et al. 2006. Natural variation can significantly alter the sensitivity of influenza A (H5N1) viruses to oseltamivir. Antimicrob. Agents Chemother. 50:3809–3815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reed L. J., Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493–497 [Google Scholar]
- 35. Richard M., et al. 2008. Impact of influenza A virus neuraminidase mutations on the stability, activity, and sensibility of the neuraminidase to neuraminidase inhibitors. J. Clin. Virol. 41:20–24 [DOI] [PubMed] [Google Scholar]
- 36. Rogers G. N., Paulson J. C. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127:361–373 [DOI] [PubMed] [Google Scholar]
- 36a. Russell R. J., et al. 2006. The structure of H5N1 avian influenza neuraminidase suggests new opportunities for drug design. 443:45–49 [DOI] [PubMed] [Google Scholar]
- 37. Stevens J., et al. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J. Mol. Biol. 381:1382–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Stoner T. D., et al. 2010. Antiviral susceptibility of avian and swine influenza of the N1 neuraminidase subtype. J. Virol. 84:9800–9809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Suwannakarn K., et al. 2009. Molecular evolution of H5N1 in Thailand between 2004 and 2008. Infect. Genet. Evol. 9:896–902 [DOI] [PubMed] [Google Scholar]
- 40. Thompson C. I., Barclay W. S., Zambon M. C. 2004. Changes in in vitro susceptibility of influenza A H3N2 viruses to a neuraminidase inhibitor drug during evolution in the human host. J. Antimicrob. Chemother. 53:759–765 [DOI] [PubMed] [Google Scholar]
- 41. Tisdale M. 2000. Monitoring of viral susceptibility: new challenges with the development of influenza NA inhibitors. Rev. Med. Virol. 10:45–55 [DOI] [PubMed] [Google Scholar]
- 42. Uchida Y., et al. 2008. Molecular epidemiological analysis of highly pathogenic avian influenza H5N1 subtype isolated from poultry and wild bird in Thailand. Virus Res. 138:70–80 [DOI] [PubMed] [Google Scholar]
- 43. Vines A., et al. 1998. The role of influenza A virus hemagglutinin residues 226 and 228 in receptor specificity and host range restriction. J. Virol. 72:7626–7631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wan X.-F., et al. 2008. Evolution of highly pathogenic H5N1 avian influenza viruses in Vietnam between 2001 and 2007. PLoS One 3:e3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Webby R. J., et al. 2004. Responsiveness to a pandemic alert: use of reverse genetics for rapid development of influenza vaccines. Lancet 363:1099–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wetherall N. T., et al. 2003. Evaluation of neuraminidase enzyme assays using different substrates to measure susceptibility of influenza virus clinical isolates to neuraminidase inhibitors: report of the neuraminidase inhibitor susceptibility network. J. Clin. Microbiol. 41:742–750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Woods J. M., et al. 1993. 4-Guanidino-2,4-dideoxy-2,3-dehydro-N-acetylneuraminic acid is a highly effective inhibitor both of the sialidase (neuraminidase) and of growth of a wide range of influenza A and B viruses in vitro. Antimicrob. Agents Chemother. 37:1473–1479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. World Health Organization. 2010. Cumulative number of confirmed human cases of avian influenza A/(H5N1) reported to WHO, 18 October 2010. World Health Organization, Geneva, Switzerland: http://www.who.int/csr/disease/avian_influenza/country/cases_table_2010_10_18/en/index.html [Google Scholar]
- 49. Yen H.-L., et al. 2005. Neuraminidase inhibitor-resistant influenza viruses may differ substantially in fitness and transmissibility. Antimicrob. Agents Chemother. 49:4075–4084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Yen H. L., et al. 2006. Importance of neuraminidase active-site residues to the neuraminidase inhibitor resistance of influenza viruses. J. Virol. 80:8787–8795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Yen H. L., Monto A. S., Webster R. G., Govorkova E. A. 2005. Virulence may determine the necessary duration and dosage of oseltamivir treatment for highly pathogenic A/Vietnam/1203/04 influenza virus in mice. J. Infect. Dis. 192:665–672 [DOI] [PubMed] [Google Scholar]
- 52. Zambon M., Hayden F. G. 2001. Position statement: global neuraminidase inhibitor susceptibility network. Antiviral Res. 49:147–156 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.