Abstract
Objective:
This cross-sectional study describes the characteristics of patients with an abnormal Glasgow Coma Scale (GCS) in the prehospital setting.
Methods:
We reviewed existing prehospital care reports (PCRs) in the San Mateo County, California, emergency medical services (EMS) database from January 1 to December 31, 2007. Adults age 18 or greater with a documented GCS fit inclusion criteria. We excluded single and multisystem trauma patients, as well as patients in cardiac arrest, respiratory arrest, or listed as deceased from the study. We classified the remaining patients as a normal GCS of 15 or abnormal (defined as less than 15 at any time during paramedic contact), and then further sub-classified into mild (GCS 13–14), moderate (GCS 9–12) or severe (GCS 3–8).
Results:
Of the 12,235 unique prehospital care record in the database, 9,044 (73.9%) met inclusion criteria, comprised of 2,404 (26.6%) abnormal GCS patients and 6,640 (73.4%) normal GCS patients. In the abnormal GCS category, we classified 1,361 (56.6%) patients as mild, 628 (26.1%) as moderate, and 415 (17.3%) as severe. Where sex was recorded, we identified 1,214 (50.5%) abnormal GCS patients and 2,904 (43.7%) normal GCS patients as male. Mean age was 65.6 years in the abnormal GCS group and 61.4 in the normal GCS group (p<0.0001). Abnormal GCS patients were more likely to have a history of conditions known to be associated, such as alcohol abuse (odds ratio [OR] 2.3, 95% confidence interval [CI]=2.75–3.00), diabetes (OR 1.34, 95% CI=1.17–1.54), substance abuse (OR 1.6, CI=1.09–2.3), stroke/transient ischemic attack (OR 2.0, CI=1.64–2.5), and seizures (OR 3.0, CI=1.64–2.5). Paramedics established intravenous (IV) access on 1,821 (75.7%, OR 1.94, CI=1.74–2.2) abnormal GCS patients and administered medications to 777 (32.3%, OR 1.01, CI=0.92–1.12). Compared to patients with normal GCS, patients with a mildly abnormal GCS were less likely to receive medications (OR 0.61, CI=0.53–0.70) while those with a moderately or severely abnormal GCS were more likely (OR 1.27, CI=1.07–1.50 and OR 2.86, CI=2.34–3.49, respectively). Of the normal GCS patients, 4,097 (61.7%) received an IV and 2,125 (32.0%) received medications by any route.
Conclusion:
Twenty-seven percent of all prehospital patients in our study presented with an abnormal GCS. Prehospital patients with an abnormal GCS are more likely to be male, slightly older, and have higher rates of history of alcohol use or seizure. This group of patients had a higher rate of IV placement. Patients with a mildly abnormal GCS were less likely to receive medications while those with a moderately or severely abnormal GCS were more likely.
INTRODUCTION
Altered level of consciousness (ALOC) is a commonly encountered prehospital syndrome associated with various disorders, and accounts for 4–10% of all presentations to the emergency department (ED). It is one of the most common reasons for hospital admission of patients brought to the ED by emergency medical services (EMS).1,2 Common causes of ALOC include alcohol intoxication, hypoglycemia, illicit drugs, postictal states and trauma.3
Both physicians and paramedics may find evaluation of a patient with ALOC challenging. The reasons include lack of knowledge of a patient’s medical history, baseline mental status, and precipitating events, as well as the range of changes in mental status, from agitation to coma. Paramedics make a presumptive diagnosis, or “field impression,” based on the patient’s clinical presentation and on limited diagnostic tests. Interventions following standard medical protocols are guided by the provider’s judgment. Interventions for patients presenting with ALOC focus on treating the presumed underlying cause and include blood glucose determination, naloxone administration, benzodiazepine administration and airway management as needed. For complicated patient presentations, paramedics may be advised or required to consult a base physician.
The complicated nature of ALOC presentations, coupled with limited understanding of this group of patients and limited diagnostic tools, presents a particular challenge for paramedics. While the history and physical exam are of paramount importance in determining the etiology of ALOC, paramedics lack training in more sophisticated assessment techniques, such as a complete cranial nerve exam or mini-mental status exam that can provide etiologic clues. Additionally, paramedics lack the benefit of imaging, laboratory studies, or invasive diagnostic procedures to determine etiology and hence rely almost entirely on history and physical exam.
Paramedic protocol standards include methods for assessing level of consciousness, such as the Glasgow Coma Scale (GCS).
Given these limitations, we studied whether prehospital patients with an abnormal GCS could provide clues to a likely etiology. We hypothesized that patients with an abnormal GCS would be fundamentally different than patients with a normal GCS in terms of demographics, medical history, and use of advanced life support (ALS) interventions, such as intravenous (IV) lines or medication administration. Further, we predicted that an abnormal GCS would be associated with a known medical condition. We hope that a better understanding of this patient population will lead to prospective studies to elucidate the optimal approach to treatment.
METHODS
San Mateo County is an urban/suburban county with 700,000 people spread over 552 square miles. San Mateo receives approximately 40,000 calls for emergency medical assistance annually. Firefighter paramedics on fire engines and American Medical Response (AMR) ambulances respond to 9-1-1 emergency medical calls. The system is a public/private partnership between AMR, the fire service agencies in San Mateo County, and the County Health Services Department’s EMS office. AMR contracts with a Joint Powers Authority, made up of 17 fire service agencies, to provide paramedic first responder services.4 All ambulances are staffed by at least one emergency medical technician-paramedic, and thus all patients receive ALS level evaluation.
Each patient receiving medical attention generates an electronic prehospital care record (PCR). This record includes data regarding patient demographics, home address, medical history, signs and symptoms, clinical interventions and paramedic field impression. This cross-sectional study examined medical records of the prehospital patients in San Mateo County from January 1, 2007, to December 31, 2007. We recorded these patient encounters in a Structured Query Language searchable database with over 200 data elements per patient encounter.
Inclusion criteria were age 18 years or greater with a documented GCS and documented evaluation by San Mateo County paramedics. Exclusion criteria were cardiac or respiratory arrest, death or trauma (single or multi-system) as the primary paramedic impression. We divided patients into two groups: those with a GCS of less than or equal to 14 at any time during paramedic contact, defined as having an abnormal GCS, and those with a GCS of 15, defined as normal. For purposes of analysis, we further subdivided the abnormal GCS group into mild (GCS 13–14), moderate (GCS 9–12) and severely altered (GCS less than 8) categories to look for associations and trends between severity of ALOC and various predictors. This classification scheme is common to other studies involving abnormal GCS.5
The GCS has three components: eye, verbal and motor responses. The three values are considered separately and summed. The lowest possible GCS is three (deep coma or death), while the highest is 15 (fully alert and oriented). With good interobserver reliability and ease of use, we linked the admission GCS to prognosis prediction for a number of conditions, including risk for aspiration pneumonia, traumatic brain injury, subarachnoid hemorrhage and bacterial meningitis.6–9 Furthermore, prior studies validate paramedic GCS use, demonstrating good inter- and intraobserver reliability, and statistically significant reliability between paramedics and emergency physicians.10
A checkbox format that included 22 medical conditions documents past medical history (PMH). A checked box indicated a known condition in the PMH, while an unchecked box indicated either “none” or “unknown” (no distinction was made). Of the conditions listed, six are known causes of ALOC: stroke/transient ischemic attack (TIA), diabetes (due to episodes of hypoglycemia), alcohol use, psychiatric illness, illicit drug use and seizures.11,12 We excluded trauma patients with ALOC from our analysis. We compared whether the abnormal and normal GCS groups differed statistically in the proportion with a known ALOC etiology or no PMH. The statistical package used for data analysis was SAS 9.1.3, Cary, NC.
RESULTS
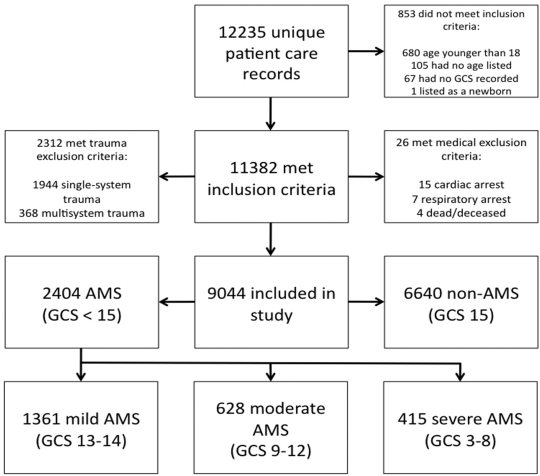
We examined 12,235 unique PCRs, of which 9,044 (73.9%) met inclusion criteria. We excluded only 67 adult patients (0.59%) for having no documented GCS. The normal GCS group contained 6,640 (73.4%) patients and 2,404 (26.6%) abnormals (Figure). The mean age of the abnormal GCS patients was 65.6 years, compared with 61.4 in the normal GCS (Table 1). We associated each ten-year increase in age with an increased likelihood of abnormal GCS (odds ration [OR]=1.1, 95% confidence interval [CI]=1.08–1.12). Abnormal GCS patients were more likely to be male (50.5%) than normal GCS patients (43.7%; OR=1.31, CI=1.19–1.44).
Figure.
Cohort flow diagram.
GCS, Glasgow Coma Scale; AMS, altered mental status
Table 1.
Characteristics of patient by group.
| GCS 15 (n=6640) | GCS 3–14 (n=2404) | |
|---|---|---|
| Mean age (years)* | 61.4 ± 20.8 | 65.6 ± 21.5 |
| Sex (%)* | ||
| Female | 55.1 | 49.0 |
| Male | 43.7 | 50.5 |
| Race (%) | ||
| White | 43.9 | 46.8 |
| Black/African America | 7.6 | 7.2 |
| Hispanic/Latino | 8.1 | 9.2 |
| Native American/Alaskan | <0.1 | 0 |
| Asian/Pacific Islander | 8.1 | 8.8 |
| Other/unknown* | 32.3 | 28.0 |
| History (%) | ||
| Alcohol* | 1.8 | 4.0 |
| Diabetes* | 11.1 | 14.5 |
| Psychiatric | 3.5 | 3.5 |
| Seizure* | 2.4 | 6.9 |
| Stroke/TIA* | 3.4 | 6.6 |
| Substance use* | 1.1 | 1.7 |
Indicates statistically significant result, (p<0.05)
GCS, Glasgow Coma Scale; TIA, transient ischemic attack
In the abnormal GCS group, 415 (17.3%) patients were severe (GCS 8 or less), 628 (26.1%) moderate (GCS 9–12) and 1,361 (56.6%) mild. The mean age in each group was 72.0, 75.0, and 68.0, respectively. There was no statistically significant association between age and severity of abnormal GCS. Male sex was more likely to be associated with a mild abnormal GCS (OR=1.52, CI=1.35–1.71). There was no statistically significant association between male sex and either moderate or severe abnormal GCS. There were no significant differences in race between the two groups (Table 1).
The most common primary paramedic diagnostic impressions in the abnormal GCS group were ALOC (32.3%), postictal state (10.0%), “other” (7.2%), hypoglycemia (6.3%) and syncope/near-syncope (5.9%). In the normal GCS group, they were “other” (14.7%), weakness (13.9%), syncope/near-syncope (9.0%), abdominal pain (8.6%) and non-traumatic body pain (7.3%).
Patients in the abnormal GCS group were more likely to have an IV placed (OR=1.94, CI=1.74–2.2). Although these patients were no more likely to receive medications in the field (OR=1.01, CI=0.92–1.12), patients with a mildly abnormal GCS were less likely to receive medications, while those with a moderately or severely abnormal GCS were more likely (Table 2a). In the abnormal GCS group, patients were no more likely to receive activated charcoal than the normal GCS group, and only twice as likely to receive oral glucose compared with the normal GCS group. The rates of administration for parenteral medications in the abnormal GCS group, compared with the normal GCS group, were dramatically different, with abnormal GCS patients significantly more likely to receive glucagon, midazolam or naloxone (Tables 2a and 2b). The transport rates were similar in both groups (92.5% in the abnormal vs. 90.0% in the normal GCS group).
Table 2a.
Percentage of patients by group receiving intervention
| GCS 15 | GCS 3–14 | |
|---|---|---|
| IV access (%)* | 61.7 | 75.7 |
| Medications administered (%) | 32.0 | 32.3 |
| Activated charcoal | 0.69 | 0.42 |
| Albuterol | 6.3 | 6.8 |
| Glucose, oral* | 1.1 | 2.0 |
| Dextrose, IV* | 0.8 | 9.0 |
| Glucagon* | 0.03 | 1.2 |
| Midazolam* | 0.17 | 2.4 |
| Naloxone* | 0.18 | 5.3 |
| Nitroglycerin* | 9.5 | 2.2 |
Indicates statistically significant result, (p<0.05)
GCS, Glasgow Coma Scale; IV, intravenous
Table 2b.
Odds ratios and 95% confidence intervals for paramedic interventions by GCS group
| Intervention | GCS 13–14 | GCS 9–12 | GCS 3–8 |
|---|---|---|---|
| IV access | 1.57 (1.38–1.78) | 2.25 (1.85–2.73) | 3.60 (2.73–4.75) |
| Medications | 0.61 (0.53–0.70) | 1.27 (1.07–1.50) | 2.86 (2.34–3.49) |
All results were statistically significant (p<0.05)
GCS, Glasgow Coma Scale; IV, intravenous
A known PMH was documented in 43.1% of patients (45.9% of abnormal GCS and 42.1% of normal GCS). The remainder of patients had either no known, or an unknown PMH, though this was not differentiated in the paramedic documentation. The most common PMH for abnormal GCS patients were hypertension (25.2%), diabetes (14.4%), seizures (6.9%), stroke/TIA (6.6%) and non-specific cardiac (5.8%). For normal GCS patients, they were hypertension (25.2%), diabetes (11.1%), non-specific cardiac (5.5%), asthma (5.1%) and congestive heart failure (4.9%).
In comparing known causes of ALOC in the PMH, we found that patients with a PMH of stroke or TIA, diabetes, alcohol use, substance abuse and seizures all were significantly more likely to present in the abnormal GCS group. We found no association, however, between a past psychiatric history and an abnormal GCS (Table 3a). All of the ALOC-associated conditions were positively associated with the male sex and older age. Controlling for age and sex, however, did not significantly affect the results. Additionally, having no known PMH, or an unknown PMH, was negatively associated with an abnormal GCS (OR 0.85, CI=0.78–0.94).
Table 3a.
Odds ratios and 95% confidence intervals for known altered mental status etiologies in past medical history
| Unadjusted odds ratio | Adjusted for age and sex | |
|---|---|---|
| Alcohol* | 2.3 (1.75–3.00) | 2.60 (1.95–3.40) |
| Diabetes* | 1.34 (1.17–1.54) | 1.25 (1.09–1.44) |
| Psychiatric | 1.00 (0.78–1.29) | 1.17 (0.91–1.52) |
| Seizures* | 3.00 (2.40–3.80) | 2.50 (2.80–4.40) |
| Stroke/TIA* | 2.00 (1.64–2.50) | 1.79 (1.45–2.20) |
| Substance use* | 1.60 (1.09–2.30) | 1.86 (1.26–2.70) |
Indicates statistically significant result, (p<0.05)
TIA, transient ischemic attack
We subdivided the abnormal GCS group into mild (GCS 13–14), moderate (GCS 9–12) and severe (GCS 3–8) categories (Table 3b). Patients with alcohol use and seizures in their PMH trended toward higher GCS and patients with diabetes in their PMH trended toward lower GCS. Patients with stroke/TIA or substance use in their PMH had a higher likelihood of presenting in the moderately altered group, with neither group showing a trend toward high or low GCS. Adjusting for age and sex had minimal effects on the results (Table 3c). The only statistically significant change was a new association between mild abnormal GCS and psychiatric illness.
Table 3b.
Unadjusted odds ratios and 95% confidence intervals for known altered level of consciousness etiologies in past medical history by Glasgow Coma Scale (GCS) category.
| GCS 13–14 | GCS 9–12 | GCS 3–8 | |
|---|---|---|---|
| Alcohol | 2.95 (2.18–4.00)* | 2.01 (1.26–3.19)* | 0.67 (0.27–1.66) |
| Diabetes | 1.01 (0.84–1.21) | 1.68 (1.35–2.10)* | 2.04 (1.58–2.62)* |
| Psychiatric | 1.24 (0.92–1.65) | 0.67 (0.39–1.13) | 0.74 (0.40–1.37) |
| Seizure | 3.44 (2.67–4.43)* | 2.48 (1.71–3.59)* | 2.50 (1.61–3.89)* |
| Stroke/TIA | 1.84 (1.42–2.38)* | 2.81 (2.07–3.81)* | 1.45 (0.91–2.32) |
| Substance use | 1.82 (1.17–2.85)* | 1.75 (0.95–3.25) | 0.66 (0.21–2.09) |
Indicates statistically significant result, (p<0.05)
TIA, transient ischemic attack
Table 3c.
Age and sex adjusted odds ratios and 95% confidence intervals for known altered level of consciousness etiologies in past medical history by Glasgow Coma Scale (GCS) category.
| GCS 13–14 | GCS 9–12 | GCS 3–8 | |
|---|---|---|---|
| Alcohol | 3.11 (2.28–4.25)* | 2.55 (1.59–4.08)* | 0.80 (0.32–1.97) |
| Diabetes | 0.95 (0.79–1.14) | 1.53 (1.22–1.91)* | 1.91 (1.48–2.45)* |
| Psychiatric | 1.40 (1.04–1.89)* | 0.84 (0.49–1.43) | 0.88 (0.47–1.63) |
| Seizure | 3.84 (2.96–4.97)* | 3.10 (2.12–4.52)* | 2.95 (1.89–4.61)* |
| Stroke/TIA | 1.67 (1.28–2.18)* | 2.40 (1.76–3.27)* | 1.25 (0.78–2.01) |
| Substance use | 1.99 (1.27–3.13)* | 2.30 (1.23–4.28)* | 0.79 (0.25–2.53) |
Indicates statistically significant result, (p<0.05)
TIA, transient ischemic attack
DISCUSSION
Patients with an abnormal GCS tended to be older and male and increasing age correlated with an increasing likelihood of an abnormal GCS. The higher prevalence of certain ALOC-associated conditions among males (alcoholism and illicit drug use) revealed a potential confounding source, and the association of older age with stroke and diabetes likely demonstrates effect modification.13,14 In our study, all ALOC-associated conditions except psychiatric illness were positively associated with male sex and older age-However, the association between known ALOC etiologies in the PMH and older age tended to become statistically significant only in the oldest quartile of our study group (age 82–104). We found no statistically significant associations between race and abnormal GCS.
An association exists between a known ALOC etiology in PMH and the presentation of an abnormal GCS in the field. Although this finding is not surprising, the number of patients without an unknown PMH or with no known PMH was unexpected. With the advent of binary PMH checkboxes and computerized PCRs, practitioners often miss the distinction between not having a PMH and having an unknown PMH. This is an area of quality control that could be addressed in the future.
In our study population, we identified diabetic patients as among the most common, as well as the most likely to present with a severely abnormal GCS. Although a blood glucose check is standard practice in the patient with an abnormal GCS, given the short and long-term sequelae associated with hypoglycemia, such as increased risk of myocardial infarction, ventricular rhythm disorders, and stroke, perhaps blood glucose monitoring should be given a higher priority in paramedic protocols when treating the severely altered non-trauma patient.15
Another unexpected finding was that while only 38 patients (1.6% of the abnormal GCS group) presented with a persistent seizures or status epilepticus, 2.4% of them received midazolam. San Mateo County paramedic protocols indicate the use of midazolam only for persistent seizures and pre-cardioversion sedation (a relatively rare event). These results likely indicate a significant amount of “off-label” use (e.g., for sedation in agitated patients with base hospital approval). This is in an area where the protocols could be revised to reflect actual field use.
As a group, abnormal GCS patients required more paramedic medical interventions than those with a normal GCS. Patients with an abnormal GCS were more likely to have IV access established by paramedics. Although the rates of medication administration were no different overall between the normal and abnormal GCS groups, mild GCS was associated with lower rates of medication administration than normal GCS, while moderately and severely abnormal GCS were each associated with increasing rates of medication administration. Although existing San Mateo County EMS protocols direct paramedic interventions, routine IV access is not required for ALOC patients.16 Previous studies demonstrated that most paramedics initiated IV lines are not used to provide treatment, such as fluids or medications in the field.17 This seemed to hold true for patients with a mildly abnormal GCS, who were more likely to receive an IV and less likely to receive medications. Patients who were categorized in the moderately and severely abnormal GCS groups, however, had smaller relative odds ratios of receiving an IV compared with receiving medication, indicating that in these groups, IVs were more likely to be medically necessary rather than precautionary.
San Mateo County paramedics carry 18 different medications, but paramedics only used a third of these (activated charcoal, dextrose, glucagon, glucose paste, midazolam and naloxone) in the treatment of known ALOC etiologies. Of the 58 different paramedic diagnostic impressions listed in the database, only a dozen are commonly associated with ALOC (excluding cardiopulmonary arrest). Of these, only hypoglycemia and overdose routinely require medication administration while seizures require medication administration only if the patient is actively seizing. Hypoglycemia, however, was relatively common in the abnormal GCS group (6.3%) while medical conditions in the normal GCS group that routinely required medication administration were relatively rare.
We found five of the six conditions in the PMH known to be associated with ALOC to have an association with an abnormal GCS in our study. Seizures and alcohol use indicate the strongest associations with an abnormal GCS, while associations between an abnormal GCS and stroke/TIA, diabetes and substance abuse were weaker. We did not find the expected association between a history of psychiatric illness and an abnormal GCS. This may be partly attributable to the difficulty of obtaining an accurate psychiatric history from an altered patient. There was, however, a statistically significant negative association between having no listed PMH (“null” category) and an abnormal GCS (OR 0.85, CI=0.78–0.94, p=0.0011). Given the higher prevalence of psychiatric illness among alcoholics and illicit drug users and the difficulty of obtaining a medical history from an altered patient, it is possible that paramedics presumed only a history of alcohol or substance abuse, but not psychiatric illness, in the intoxicated patient.18,19 Thus, psychiatric illness may have been underreported in this group.
LIMITATIONS
A major limitation of this study is that it was conducted in a single county in California. These results would not necessarily generalize to populations in a more rural or more urban setting than San Mateo County. Furthermore, as paramedic interventions are protocol-directed, the rates and types of interventions may differ in counties with more or less aggressive protocols and medical direction.
One limitation of this study is the exclusion of trauma patients from our analysis. This was done for several reasons, including the generally non-episodic nature of trauma, a lack of causality between prior and subsequent trauma, and the often multifactoral etiology of ALOC associated with trauma. Other studies validated the use of the GCS for measuring ALOC in trauma patients.20
Another major limitation of this study is that the “null” category in the PMH could mean either that the patient had none or that the patient’s PMH was unknown. Given the often episodic nature of ALOC, a negative association between having no PMH and ALOC seems reasonable. The degree of that association, however, was likely masked by the number of patients in the “null” category who actually had a PMH causally contributing to their abnormal GCS was not known, and could not be obtained by the paramedics.
The GCS does not distinguish between the various causes of ALOC, and similar GCS does not indicate a similar etiology. The GCS is particularly poor at measuring agitated and sedated states, which have important diagnostic and prognostic value in altered patients.21
The exclusive use of prehospital data limited the scope of our study. Further studies linking prehospital data with ED data would be needed to answer more sophisticated questions on the diagnostic and predictive value of the GCS in non-trauma patients.
CONCLUSION
Patients with an abnormal GCS differ from patients with a normal GCS in terms of age, sex, paramedic field impression, past medical history and prehospital treatment. Patients with an abnormal GCS tend to be older and male, and excluding a history of psychiatric illness, are more likely to have a known ALOC etiology in their PMH. Although the GCS is useful in assessing the level of impairment in arousal, it is of limited usefulness in determining the etiology of ALOC. For these reasons, future prospective studies should focus on subgroups within this diverse patient population, particularly diabetics and the elderly, to help elucidate optimal prehospital management.
Footnotes
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources, and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
REFERENCES
- 1.Kanich W, Brady WJ, Huff JS, et al. Altered mental status: evaluation and etiology in the ED. Am J of Emerg Med. 2002;20(7):613–617. doi: 10.1053/ajem.2002.35464. [DOI] [PubMed] [Google Scholar]
- 2.Richards JR, Ferrall SJ. Triage ability of emergency medical services providers and patient disposition: a prospective study. Prehosp Disaster Med. 1999;14(3):174–9. [PubMed] [Google Scholar]
- 3.Huff JS. Contemporary etiology of coma presenting to academic medical center. Ann Neurol. 1997;42:471. [Google Scholar]
- 4.EMS: Who we are, what we do. County of San Mateo Health System Web site. Available at: http://www.co.sanmateo.ca.us/smc. Accessed January 2, 2009.
- 5.Stryke J, Stålnacke BM, Sojka P, et al. Traumatic brain injuries in a well-defined population: epidemiological aspects and severity. J Neurotrauma. 2007;24:1425–1436. doi: 10.1089/neu.2007.0266. [DOI] [PubMed] [Google Scholar]
- 6.Adnet F, Baud F. Relation between Glasgow Coma Scale and aspiration pneumonia. Lancet. 1996;348(9020):123–4. doi: 10.1016/s0140-6736(05)64630-2. [DOI] [PubMed] [Google Scholar]
- 7.Servadei F, Nasi MT, Cremonini AM, et al. Importance of a reliable admission Glasgow Coma Scale score for determining the need for evacuation of posttraumatic subdural hematomas: a prospective study of 65 patients. J Trauma. 1998;44(5):868–73. doi: 10.1097/00005373-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Qureshi AI, Sung GY, Razumovsky AY, et al. Early identification of patients at risk for symptomatic vasospasm after aneurysmal subarachnoid hemorrhage. Crit Care Med. 2000;28(4):984–90. doi: 10.1097/00003246-200004000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Booth CM, Boone RH, Tomlinson G, et al. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004;291:870. doi: 10.1001/jama.291.7.870. [DOI] [PubMed] [Google Scholar]
- 9.Menegazzi JJ, Paris PM, Sucov AN, et al. Reliability of the Glasgow Coma Scale when used by emergency physicians and paramedics. J Trauma. 1993;34(1):46–8. doi: 10.1097/00005373-199301000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Ferrera PC, Chan L. Initial management of the patient with altered mental status. Am Fam Physician. 1997;55(5):1773–80. [PubMed] [Google Scholar]
- 11.Clinical policy for the initial approach to patients presenting with altered mental status. Ann Emerg Med. 1999;33(2):251–81. doi: 10.1016/s0196-0644(99)70406-3. [DOI] [PubMed] [Google Scholar]
- 12.Van den Bree MB, Johnson EO, Neale MC, et al. Genetic and environmental influences on drug use and abuse/dependence in male and female twins. Drug Alcohol Depend. 1998;52(3):231–41. doi: 10.1016/s0376-8716(98)00101-x. [DOI] [PubMed] [Google Scholar]
- 13.Effective medical treatment of opiate addiction National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction. JAMA. 1998;280(22):1936–43. [PubMed] [Google Scholar]
- 14.Lassman-Vague V. Hypoglycemia in elderly diabetic patients. Diabetes Metab. 2005;31:5S53–5S57. doi: 10.1016/s1262-3636(05)73651-x. [DOI] [PubMed] [Google Scholar]
- 15.EMS Patient care protocols County of San Mateo Health System Web site. Available at: http://www.co.sanmateo.ca.us/smc/department/health/home/0,,1954_8990723_6856909,00.html#introduction. Accessed January 2, 2009.
- 16.Kuzma K, Sporer KA, Michael GE, et al. When are prehospital intravenous catheters used for treatment? J Emerg Med. 2009;36(4):357–62. doi: 10.1016/j.jemermed.2007.11.054. [DOI] [PubMed] [Google Scholar]
- 17.Dawson DA, Grant BF, Stinson FS, et al. Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug Alcohol Depend. 2005;77(2):139–150. doi: 10.1016/j.drugalcdep.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 18.Rounsaville BJ, Weissman MM, Kleber H, et al. Heterogeneity of psychiatric diagnosis in treated opiate addicts. Arch Gen Psychiatry. 1982;39(2):161–8. doi: 10.1001/archpsyc.1982.04290020027006. [DOI] [PubMed] [Google Scholar]
- 19.Menegazzi JJ, Davis EA, et al. Reliability of the Glasgow Coma Scale when used by emergency physicians and paramedics. J Trauma. 1993;34(1):46–8. doi: 10.1097/00005373-199301000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Swift RH, Harrigan EP, Cappelleri JC, et al. Validation of the behavioural activity rating scale (BARS): a novel measure of activity in agitated patients. J Psychiatric Res. 2002;36(2):87–95. doi: 10.1016/s0022-3956(01)00052-8. [DOI] [PubMed] [Google Scholar]