Abstract
Objective:
This study sought to correlate the presence of pleural-based B-lines seen by emergency department ultrasound performed with the linear transducer with B-type natriuretic peptide (BNP) level in patients with suspected congestive heart failure.
Methods:
The study was a prospective convenience sample on adult patients in an academic, urban emergency department with over 100,000 annual patient visits. Adult patients with a BNP level ordered by the treating physician were prospectively enrolled by one of four physicians, blinded to the BNP level. The enrolling physicians included an emergency ultrasound director, two emergency ultrasound fellows, and a senior emergency medicine resident. Bedside ultrasound was performed using a 3–12 MHz linear broadband transducer in four lung fields. The serum BNP level was correlated with bilateral B-lines, defined as three or more comet-tail artifacts arising from the pleural line extending to the far field without a decrease in intensity on the right and left thorax.
Results:
Sixty three patients were consented and enrolled during a four-month period. Fifteen patients had the presence of bilateral B-lines. The median BNP in patients with bilateral B-lines was 1560 pg/mL (95% confidence interval (CI) 1141–3706 pg/mL), compared with 538 pg/mL (95% confidence interval 310–1917 pg/mL) in patients without B-lines. The distributions in the two groups differed significantly (p=0.0006). Based on the threshold level of BNP 500 pg/mL, the sensitivity of finding bilateral B-lines on ultrasound was 33.3% (95% CI: 0.19–0.50), and the specificity was 91.7% (95% CI: 0.73–0.99). In addition, bilateral B-lines were absent in all patients with a BNP<100 pg/mL.
Conclusion:
The presence of bilateral B-lines identified with the linear probe is associated with significantly higher BNP levels than patients without B-lines. In our patient population, the presence of B-lines was specific but not sensitive for BNP>500. Further research may show that it can be applied to quickly assess patients with undifferentiated dyspnea.
INTRODUCTION
In the United States approximately three million people live with congestive heart failure (CHF), and approximately 400,000 new cases are diagnosed each year.1 Prior studies have demonstrated the benefit of early diagnosis and treatment in decompensated CHF.2, 3 However, the clinical diagnosis of CHF may be difficult even for expert physicians.4 The use of serum B-type natriuretic peptide (BNP) coupled with clinical exam significantly improves the diagnostic accuracy in determining acute decompensated CHF. However, the immediate result of this lab test is not generally available.5
Bedside physician-performed ultrasound is increasingly available in academic and community emergency departments (ED). Ultrasound of the thorax may show evidence of extravascular lung water present in patients with CHF.6 Artifacts known as “Lung Rockets,” or “B-lines,” which represent interstitial fluid seen on the periphery of the pleura have been associated with CHF.7 Interstitial pulmonary edema has been reliably detected in multiple studies by chest ultrasound and has been used in the distinction between Chronic Obstructive Pulmonary Disease (COPD) and CHF exacerbation.7–9 However, the sensitivity, specificity, and correlation of “B-lines” with other objective measures of CHF in the ED setting remains incompletely defined. Prior studies have used curvilinear or micro-convex transducers to identify the presence of B-lines. However, no study has yet to evaluate the ability of linear transducers to explore these findings, despite their widespread use to detect pneumothoracies.
The purpose of this study was to correlate the presence of B-lines using emergency physician-performed chest ultrasound with the linear transducer with BNP level in patients with suspected CHF. We hypothesized that the presence of bilateral B-lines would be associated with a significantly elevated serum BNP in patients with suspected CHF.
METHODS
Study Design
The study was a prospective convenience sample of adult patients presenting to the ED in whom the treating physician ordered a BNP level. The study team was composed of a director of emergency ultrasound, two emergency ultrasound fellows and a senior emergency medicine resident. The study team worked non-clinical shifts in the ED during pre-defined four-hour blocks. Generally, enrollment occurred during the weekday morning or afternoon. During the enrollment periods, the study team was not responsible for direct patient care. The study team member would ask the treating physician if a BNP level had been ordered on any patient. The study did not discriminate whether BNP had been ordered for suspicion of heart failure or other reasons.
Prior to enrolling patients, the study team received goal-directed training in thoracic ultrasound. The training included a one-hour lecture with at least 25 thoracic ultrasound exams reviewed by the ultrasound director. Prior to the study, each of the fellows had completed at least 300 bedside ultrasound exams and the emergency medicine resident had completed approximately 100 ultrasound exams. The ultrasound director had completed over 2,000 bedside ultrasound examinations. The study was approved by human subjects committee at the study institution. Each enrolled patient gave written informed consent.
Study Setting and Population
We conducted the study in the adult ED of an urban Level 1 trauma center with an emergency medicine residency and greater than 100,000 patient visits per year. Patients were included if they were at least 18 years old, and a serum BNP was ordered in the ED. We excluded patients if they were non-English speaking, a prisoner or incapable of informed consent without an available representative.
Study Protocol
After informed consent, we collected baseline data on the patient and a bedside ultrasound was performed. The study investigator was blinded to the serum BNP level, other laboratory values and chest radiograph at the time of the ultrasound examination. However, the study team was not blinded to the patient’s appearance, vital signs or other clinical data. Ultrasound was performed with a portable ultrasound scanner (Philips HD-11XE, Andover, MA) using a 3–12 MHz broadband linear transducer in the echocardiography preset with tissue harmonic imaging enabled. Patients were examined lying in the stretcher in the position of comfort. Generally, patients were sitting upright or in a semi-recumbent position. No patient was examined in the full supine position. We investigated four thoracic ultrasound windows: right mid-axillary, right mid-clavicular, left mid-axillary and left mid-clavicular. The probe was placed in a cephalic orientation between the fourth and fifth ribs. The depth settings were adjusted so that the pleural line was placed in the middle of the image. Therefore, the total depth ranged from one patient to another, based on body habitus. All ultrasound examinations were recorded as dynamic images on DVD for later review by the emergency ultrasound director.
Measurements
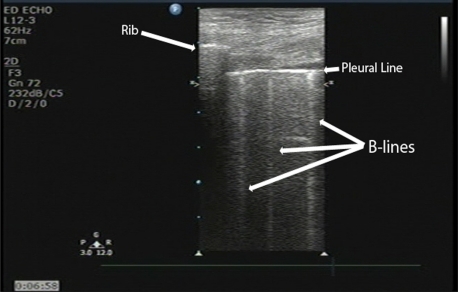
Prior to the enrollment of patients, the study team defined the presence of multiple B-lines as three or more comet tail artifacts originating from the pleural line, extending to the bottom of the ultrasound screen without a decrease in signal intensity as depicted in Figure 1. Bilateral B-lines were defined when multiple B-lines were present on both the left and right. The study investigator immediately recorded the ultrasound findings on a structured data sheet (see Appendix). The emergency ultrasound director later reviewed these findings to confirm the correct interpretation. During the review, the ultrasound director was blinded to the other data. In a subset of patients, a second credentialed physician, who was blinded to the results of the first ultrasound, repeated the ultrasound measurements.
Figure 1.
Sonographic B-lines identified with a linear transducer
Data Analysis
We recorded all data in an Access database (Microsoft Corp., Seattle, WA) and performed statistical analysis using SPSS 15.0 (SPSS Inc., Chicago, IL). We determined the median BNP value for the patients with and without bilateral B-lines and calculated 95% confidence interval (CI) of the difference. Initially, a receiver operating characteristic (ROC) curve was planned to analyze the data, but further evaluation of the data concluded that a Mann-Whitney U test would better delineate the significance of the difference in rank order of BNP in those patients with and without bilateral B-lines. At the study institution, a BNP level was considered positive at the threshold limit of 500 pg/mL.
RESULTS
We consented and enrolled 63 patients during a four-month period. Of the 63 patients, the ultrasound director enrolled three, the ultrasound fellows enrolled 34, and the emergency medicine resident enrolled 28. Of the 63 patients, nine had repeat exams by a second sonologist that showed complete agreement with the presence or absence of multiple bilateral B-lines. The mean age was 70 (range 31–90 years); 51% were male. Fifteen of the 63 (24%) had bilateral B-lines.
Post-hoc analysis revealed that multiple bilateral B-lines were absent in all patients with a BNP<100 pg/mL. Of the 15 patients with B-lines, only two had a BNP level between the indeterminate range of 100–500 pg/mL (306 and 489). Thirteen of the 15 patients with B-lines had a BNP level greater than 500 pg/mL (Table 1).
Table 1.
Presence of thoracic B-lines compared to low, intermediate and high B-type natriuretic peptide (BNP) levels.
| BNP > 500pg/mL | BNP 100–500pg/mL | BNP < 100pg/mL | Total | |
|---|---|---|---|---|
| Bilateral B-lines present | 13 | 2 | 0 | 15 |
| Bilateral B-lines absent | 26 | 9 | 13 | 48 |
| Total | 39 | 11 | 13 | 63 |
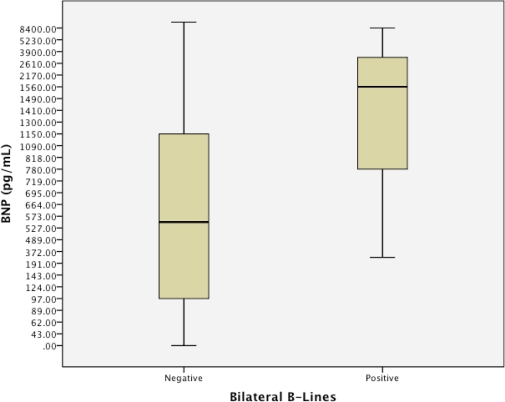
The median BNP in patients with bilateral B-lines was 1560 pg/mL (95% CI 1141–3706 pg/mL), compared with 538 pg/mL (95% CI 310–1917 pg/mL) in patients without B-lines. The distributions in the two groups differed significantly (Mann-Whitney U-statistic = 147.5, p=0.0006, two tailed) [Graph]. Based on the threshold level of BNP 500 pg/mL, the sensitivity of finding bilateral B-lines on ultrasound was 33.3% (95% CI: 0.19–0.50), and the specificity was 91.7% (95% CI: 0.73–0.99). The positive predictive value of bilateral B-lines was 0.87 (95% CI: 0.60–0.98) and the negative predictive value was 0.46 (95% CI: 0.31–0.61) [Table 2].
Graph.
Box-plot of B-type natriuretic peptide (BNP) levels in patients with and without bilateral B-lines. Negative = patients without bilateral B-lines on ultrasound; Positive = patients with the presence of bilateral B-lines on ultrasound.
Table 2.
Presence of B-lines based on B-type natriuretic peptide (BNP) threshold of 500pg/dL.
| Thoracic Ultrasound | BNP level > 500pg/mL | BNP level < 500pg/mL | Total |
|
| |||
| Bilateral B-lines present | 13 | 2 | 15 |
| Bilateral B-lines absent | 26 | 22 | 48 |
| Total | 39 | 24 | 63 |
|
| |||
| Variable | Value | 95% confidence interval | |
|
| |||
| Sensitivity | 0.33 | 0.19 to 0.50 | |
| Specificity | 0.91 | 0.72 to 0.98 | |
| Positive predictive value | 0.86 | 0.59 to 0.98 | |
| Negative predictive value | 0.45 | 0.31 to 0.60 | |
| Likelihood ratio | 4.0 | ||
LIMITATIONS
This pilot study was performed on a convenience sample by a small group of trained investigators. Further work is needed to determine if these findings are broadly applicable. The primary limitation of this study is that it only looked at the correlation between bedside ultrasound and BNP. While BNP has been shown to accurately discriminate between CHF and non-CHF causes of dyspnea at certain levels (>500pg/dl or <100pg/dl), it is an imperfect gold standard. Additionally, the small group of trained investigators may limit this study’s applicability to other hospital settings. The majority of the patients (58.7%) were enrolled by either emergency ultrasound fellows or the ultrasound director. However, the emergency medicine resident with limited prior ultrasound experience enrolled the remainder of the patients. Future studies will be needed to determine whether inexperienced sonologists are capable of repeating these results.
In this study we consistently used the same linear ultrasound probe with the echo preset and tissue harmonic imaging enabled. The authors believe that these settings best emphasize the B-line artifact. However, some machines will not allow the user to apply a cardiac preset on linear probes. Multiple research studies regarding the detection of a pneumothorax with bedside ultrasound have used the linear probe.10, 11 While the evaluation of pneumothorax with bedside ultrasound has been included with the recent American College of Emergency Physician Ultrasound Guidelines, many emergency physicians are not familiar with the evaluation of CHF with bedside ultrasound.12 The evaluation of all types of dyspnea with the linear probe may represent a more natural progression for the average emergency physician.
While the bedside ultrasound was performed within a short amount of time after the serum BNP level was sent to the lab, this study did not specify a cut-off time between the two events, and patients may have been treated in the interim. Prior studies have shown that interstitial edema changes rapidly and dynamically in dialysis patients,13 and the results of this study do not reflect whether the patients had received any prior treatment. Simultaneous phlebotomy and chest ultrasound may alter results. Additionally, this study did not discriminate whether BNP had been ordered for suspicion of heart failure or other reasons. This study was conducted at a teaching institution where residents at various training levels often order labs. The BNP laboratory tests ordered may not necessarily translate to clinical suspicion of CHF. This fact may explain why the majority of ultrasound exams of patients with elevated levels of BNP did not illustrate the presence of multiple bilateral B-lines.
This study, like most studies with B-lines, did not prevent the sonologist from simultaneously seeing the study subject. This clearly introduces a bias to the enrolling physician, as the investigator is not blind to physical findings and ongoing treatments such as Bi-level Positive Airway Pressure, etc. On the other hand, when this test is applied clinically, this bias is also present and in fact integral to the concept of bedside ultrasound. The additional tools and information that bedside ultrasound provides the treating physician are in fact the crux of its value and importance.
Further research will define the role of bedside ultrasound evaluation of the pleural line to improve immediate diagnostic capability of a focused thoracic exam. Future research may also investigate the effect of B-lines on post-test probability of CHF.
DISCUSSION
This is the first published study to show that the presence of B-lines correlates with higher BNP level in patients using physician-performed ultrasound with a linear probe. This brief exam takes under a minute and is easily learned and reproduced.14 While earlier literature has identified similar results with curved probes, no prior studies have extensively used the linear probe for this application.15
“Comet tails” are reverberation artifacts caused by an air fluid interface that result in a hyper-echoic line that extends distally from the visceral pleura. Small, tapering hyper-echoic lines that diminish distally are also known as “Z lines” and are often present in healthy individuals. Their presence has been shown to be helpful in ruling out pneumothorax.16 The more pathologic “B lines” (or “Lung Rockets”), which emanate from the pleural line in the presence of extravascular lung water, create hyper-echoic lines that do not diminish distally.6 While this study showed correlation between B-lines and BNP, B-lines are not entirely specific to CHF and may be present in other conditions, such as acute respiratory distress syndrome, chronic interstitial lung disease, and high altitude pulmonary edema.
Based on pilot evaluation of several patients, the linear probe with a cardiac setting (with a low dynamic range) enhanced the contrast and clarity of the lung-rocket artifact. However, other researchers have used different probes and settings that may affect the identification of B-lines. For instance, an eight-lung window protocol was used in the studies by Liteplo et al,15 Volpicelli et al17 and Lichtensteinet al6 used a six-window protocol. We also chose to focus on four-lung fields to simplify the examination. In fact, the recent study by Liteplo15 suggests that the easier two-zone test may suffice for the evaluation of CHF. It does appear that “B-lines” tend to appear more frequently in the dependent portions of the lung, even in healthy patients.
We are unsure why the majority of patients in this study with elevated BNP levels did not exhibit bilateral B-lines. This study introduces a unique problem for the evaluation of B-lines with bedside ultrasound. Although the specificity of the B-lines is similar to other studies, the sensitivity of the test is significantly lower than other studies. In the future we intend to analyze the contribution of systolic and diastolic cardiac dysfunction and the presence of elevated preload to help differentiate these patients.
CONCLUSION
This study showed that the presence of B-lines in patients correlates with increased BNP level while using a linear transducer. The presence of B-lines is specific for an elevated BNP level but not sensitive. Presence or absence of B-lines can be rapidly determined using bedside emergency ultrasound and may aid in diagnosis of patients with suspected CHF.
Supplementary Material
Footnotes
Reprints available through open access at http://escholarship.org/uc/uciem_westjem
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias.
REFERENCES
- 1.Kannel WB, Belanger AJ. Epidemiology of heart failure. Am Heart J. 1991;121(3 Pt 1):951–7. doi: 10.1016/0002-8703(91)90225-7. [DOI] [PubMed] [Google Scholar]
- 2.Mattu A, Martinez JP, Kelly BS. Modern management of cardiogenic pulmonary edema. Emerg Med Clin North Am. 2005;23(4):1105–25. doi: 10.1016/j.emc.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Peacock WFt, Fonarow GC, Emerman CL, et al. Impact of early initiation of intravenous therapy for acute decompensated heart failure on outcomes in ADHERE. Cardiology. 2007;107(1):44–51. doi: 10.1159/000093612. [DOI] [PubMed] [Google Scholar]
- 4.Remes J, Miettinen H, Reunanen A, et al. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J. 1991;12(3):315–21. doi: 10.1093/oxfordjournals.eurheartj.a059896. [DOI] [PubMed] [Google Scholar]
- 5.McCullough PA, Nowak RM, McCord J, et al. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation. 2002;106(4):416–22. doi: 10.1161/01.cir.0000025242.79963.4c. [DOI] [PubMed] [Google Scholar]
- 6.Lichtenstein D, Meziere G, Biderman P, et al. The comet-tail artifact. An ultrasound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med. 1997;156(5):1640–6. doi: 10.1164/ajrccm.156.5.96-07096. [DOI] [PubMed] [Google Scholar]
- 7.Picano E, Frassi F, Agricola E, et al. Ultrasound lung comets: a clinically useful sign of extravascular lung water. J Am Soc Echocardiogr. 2006;19(3):356–63. doi: 10.1016/j.echo.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 8.Jambrik Z, Monti S, Coppola V, et al. Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung water. Am J Cardiol. 2004;93(10):1265–70. doi: 10.1016/j.amjcard.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Lichtenstein D, Meziere G. A lung ultrasound sign allowing bedside distinction between pulmonary edema and COPD: the comet-tail artifact. Intensive Care Med. 1998;24(12):1331–4. doi: 10.1007/s001340050771. [DOI] [PubMed] [Google Scholar]
- 10.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12(9):844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995;108(5):1345–8. doi: 10.1378/chest.108.5.1345. [DOI] [PubMed] [Google Scholar]
- 12.ACEP Emergency ultrasound guidelines [policy statement] Ann Emerg Med. 2009;53:550–70. doi: 10.1016/j.annemergmed.2008.12.013. [DOI] [PubMed] [Google Scholar]
- 13.Noble VE, Murray AF, Capp R, et al. Ultrasound Assessment for Extravascular Lung Water in Patients Undergoing Hemodialysis: Time Course for Resolution. Chest. 2009 doi: 10.1378/chest.08-1811. [DOI] [PubMed] [Google Scholar]
- 14.Bedetti G, Gargani L, Corbisiero A, et al. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound. 2006;4:34. doi: 10.1186/1476-7120-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liteplo AS, Marill KA, Villen T, et al. Emergency thoracic ultrasound in the differentiation of the etiology of shortness of breath (ETUDES): sonographic B-lines and N-terminal pro-brain-type natriuretic peptide in diagnosing congestive heart failure. Acad Emerg Med. 2009;16(3):201–10. doi: 10.1111/j.1553-2712.2008.00347.x. [DOI] [PubMed] [Google Scholar]
- 16.Lichtenstein D, Meziere G, Biderman P, et al. The comet-tail artifact: an ultrasound sign ruling out pneumothorax. Intensive Care Med. 1999;25(4):383–8. doi: 10.1007/s001340050862. [DOI] [PubMed] [Google Scholar]
- 17.Volpicelli G, Mussa A, Garofalo G, et al. Bedside lung ultrasound in the assessment of alveolar-interstitial syndrome. Am J Emerg Med. 2006;24(6):689–96. doi: 10.1016/j.ajem.2006.02.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.