Abstract
This study examined the impact of childhood activity limitations on family financial burden in the U.S. We used ten complete panels (1996-2006) of the Medical Expenditure Panel Survey (MEPS) to evaluate the burden of out-of-pocket healthcare expenditures for 17,857 families with children aged 0-17 years. Multivariate generalized linear models were used to examine the relationship between childhood activity limitation status and both absolute and relative financial burden. Families of children with limitations had higher absolute out-of-pocket healthcare expenditures than families of children without limitations ($594.36 higher; p<0.05), and were 54% more likely to experience relative burden (p<0.05). Substantial socioeconomic disparities in financial burden were observed. Policies are needed to enable these families to access appropriate and affordable healthcare services.
Keywords: activity limitations, child health, expenditures, financial burden, MEPS
INTRODUCTION
Childhood activity limitations are physical, social, behavioral, and cognitive limitations that alter a child's ability to engage in age-appropriate roles; conditions such as asthma or obesity, for example, may result in activity limitations for children. Over the last several decades, the prevalence of childhood activity limitations has risen dramatically (National Center for Health Statistics 2006; Newacheck et al. 1998; Perrin et al. 2007), leading to increased concern about the physical, mental, and financial health in families of such children. In particular, families of children with ongoing limitations, or activity limitations that are persistent or chronic have been shown to have worse health, mental health, and work outcomes (Witt and DeLeire 2009) than families of children without limitations. Therefore, evaluating ongoing activity limitations, regardless of a child's specific medical condition or diagnosis, may allow us to identify children who are most likely to require additional resources to minimize the negative effects of their condition, such as increased healthcare utilization and subsequent expenditures. Moreover, it is theorized that other family members may be vulnerable to spillover effects of a child's activity limitations on their own health and well-being (Sen and Yurtsever 2007; Silver et al. 1999; Silver et al. 1998; Waddington and Busch-Rossnagel 1992; Witt and DeLeire 2009). The purpose of this study was to examine the deleterious financial and spillover effects of childhood activity limitations and income at both the child and family levels.
Previous studies demonstrate that families of children with activity limitations have higher out-of-pocket (OOP) expenditures (Houtrow et al. 2008; Kuhlthau et al. 2008; Newacheck 2005; Newacheck et al. 2004) than families of children without activity limitations. Increased OOP healthcare expenses for such families can lead to substantial financial burden(Houtrow et al. 2008; Kuhlthau et al. 2005; Newacheck 2005), typically defined as the ratio of total OOP spending for healthcare services to total family income. These and other studies of financial burden examine absolute burden, the total raw dollars spent on OOP expenditures, and/or relative burden, the proportion of OOP expenditures relative to family income. Both measures represent important tools in evaluating financial burden: while some families may have low absolute burden (i.e. spend fewer OOP dollars), their expenditures may be extremely burdensome when evaluated in comparison to their disposable income. Nationally, financial burden has grown across income strata during the last decade, with the largest increases occurring among middle- and higher-income people with private insurance (Cunningham 2010). As such, there is increased concern about the associated psychosocial and economic impacts on children and their families.
Increased expenditures and financial burden due to childhood activity limitations may be compounded by the health and work-related problems that are more prevalent among parents of such children (Baydar et al. 2007; Sharpe and Baker 2007). Recent studies have demonstrated that parents of children with activity limitations are more likely to report poor physical and mental health (Kuhlthau et al. 2008; Witt and DeLeire 2009) and have more yearly sick ambulatory visits (Kuhlthau et al. 2008) than parents of healthy children. Moreover, living with an individual with a chronic illness is associated with an increased probability of incurring personal medical expenditures for other family members (Altman et al. 1999), possibly due to their increased risk for physical and mental health problems.
These work, health, and financial effects are encompassed in the concept of family spillover (Altman et al. 1999; Witt and DeLeire 2009), which describes the within-family impact of caring for a child with an activity limitation. Caring for a child with a limitation may place demands on caregivers' time, above and beyond what is typical for caregivers of children without limitations. This may disrupt family routines or social, leisure or work activities. Further OOP expenses related to the limitation may result in a reduction of available resources for other family members. Therefore, childhood limitations may degrade family resources, both financial and otherwise, and provide a mechanism by which spillover may affect the relationship between child limitation status and resulting family-level financial burden.
Previous research has linked family spillover to physical, psychological, and financial burdens (Gordon et al. 2007; Kuhlthau and Perrin 2001; Leiter et al. 2004; Raina et al. 2005; Thyen et al. 1998; Witt et al. 2003), highlighting the detrimental effects of having a child with activity limitations on family-level outcomes. While most of the existing literature examines the effects of spillover on the primary caregiver, the proposed mechanism of spillover could plausibly result in similar increases in stress and roles changes for all family members. Thus it will be important for future work to consider how spillover affects multiple facets of well-being for the entire family. Furthermore, additional research examining the health status, healthcare utilization, and healthcare-related expenditures of all family members over time is needed to better understand the relationship between caring for a child with a limitation, family-level health status, and associated financial burden.
Theoretical Framework
Substantial theoretical and empirical work supports the concept that childhood chronic health conditions and functional impairments are major life stressors (Moos 1977; Patterson and Garwick 1994; Patterson 1989; Wallander and Varni 1992) and can spillover to impact the health and healthcare utilization patterns of all family members (Witt and DeLeire 2009). The conceptual model for the present research incorporates several established theories that highlight these interrelationships and inform our research questions and hypotheses, including social-ecological systems theory (Bronfenbrenner 1979; Moos 1977; Pless and Pinkerton 1975), role theory (Biddle 1979; Major 2003), stress theory (House 1974; McEwen 1998; Patterson 1989), and the behavioral model of health services (Andersen 1968, 1995).
First, social-ecological systems theory illustrates that children and parents are nested within families, supporting the idea that stress on any person in the family system has a major influence on the health and functioning of all family members. Caring for a child with an activity limitation can have a rippling effect on other areas of family members' lives (i.e. work) and can therefore adversely influence role functioning. As role theory indicates, changes or challenges to family roles can lead to chronic stress if the family does not have the internal or external resources to meet the demands of these new circumstances. Further, stress theory and research have indicated that the long-term effects of chronic stress and psychological distress can negatively impact health outcomes (McEwen and Seeman 1999) and can affect the way in which children and families use healthcare services (Katz et al. 1997; Olfson et al. 2003).
Second, Anderson's “behavioral model” informs this study in how children and their family members may interface with the healthcare system. The model characterizes the determinants of healthcare use as need, enabling, and predisposing factors (Andersen 1968, 1995). Need factors include medically-evaluated and self-perceived health problems and symptomatology; enabling factors refer to resources available to the individual or community, such as health insurance; and predisposing factors include an individual's demographic characteristics and health beliefs (Andersen 1995). For this study, childhood activity limitations are considered a potential need factor in the behavioral model. Additionally, family income (adjusted for family size and composition) is an enabling factor that may moderate the relationship between childhood activity limitations and financial burden.
Contribution to the Literature
While the literature has identified financial burden as an area of concern among families of children with chronic conditions and activity limitations, certain substantive and methodological issues potentially limit the generalizability and accuracy of prior studies. First, most research has examined the financial burden associated with OOP healthcare expenditures specific to the child or the family, but not both (Banthin and Bernard 2006; Galbraith et al. 2005; Houtrow et al. 2008; Hwang et al. 2001; Newacheck 2005; Newacheck et al. 2004; Shattuck and Parish 2008). Given that parents of children with limitations are vulnerable to deleterious spillover effects on their health and mental health (Sen and Yurtsever 2007; Silver et al. 1999; Silver et al. 1998; Waddington and Busch-Rossnagel 1992; Witt and DeLeire 2009), there is potential for increased healthcare use and expenditures not only for the child but also for other family members (Altman et al. 1999). As such, studies that do not account for expenditures on both the child and family-levels have overlooked the important association between childhood limitation and the expenditures of both the affected child and the family as a whole.
Second, while prior studies have examined socioeconomic disparities in financial burden (Galbraith et al. 2005; Newacheck 2005), it remains unclear if, and to what extent, such disparities exist at both the child and family-levels among families caring for children with activity limitations, as compared to those families without such children. To fully understand the direct and indirect effects of childhood activity limitations on the family, studies need to account for interactive effects with socioeconomic status on the child and family level.
Third, prior studies have relied on arbitrary cut-points to define a generalized threshold for financial burden. In the context of individual- and family-level analyses, the experience of financial burden is contingent on a specific set of characteristics that define a family's available resources and the value they assign to these resources. Since many studies do not or cannot take into account how individual families choose to allocate their resources and the scope of their financial obligations, the use of such arbitrary, generalized thresholds make it difficult to capture what is actually burdensome for a specific family. Thus, it will be advantageous to conceptualize financial burden as a continuum to account for the family level variability in the definition of what is burdensome.
Ultimately, the effect of family spillover complicates the distinction between individual-level burden and family-level burden associated with childhood activity limitations. To understand the magnitude of the spillover effect in families of children with activity limitations, there is a need to conduct both individual- and family-level analyses of OOP expenditures, accounting for family size and composition. Also, given that individual and familial resources may exhibit protective effects against family spillover, the presence of a socioeconomic gradient should be assessed in the context of both individual- and family-level burden.
In this nationally-representative population-based study, we addressed these gaps in the literature with several substantive and methodological improvements that make our study unique. First, we examined the relative and absolute financial burden attributable to both child and family expenditures among families with and without a child with an ongoing activity limitation. In addition, we examined the impact of income level on this relationship, and if and to what extent socioeconomic disparities exist in financial burden. Finally, we treat financial burden as a continuum to account for the relative nature of burden.
Based on the empirical and theoretical literature, we hypothesized that children with ongoing limitations would have higher OOP healthcare expenditures and greater financial burden than children without limitations. Similarly, due to theorized spillover effects, we expect that families of children with ongoing limitations would have higher OOP healthcare expenditures and greater financial burden than families of children without limitations. We expect that there will be an interaction between childhood limitation status and income, such that the greatest child- and family-level burden will be observed among those families of children with activity limitations who have the lowest income. Understanding the relationships between child activity limitations and healthcare-related financial burden is essential to identifying families with the greatest need for financial support and to better understand this potential barrier in access to high-quality healthcare.
METHODS
Study Design, Population, and Data Sources
Data are from the Medical Expenditure Panel Survey (MEPS), a nationally representative sample of the civilian non-institutionalized population in the United States. MEPS uses computer-assisted personal interviewing technology to collect data on medical expenditures and utilization at both the person and household level over five different time points (or rounds) throughout a two-year period. Data collection for a new cohort (or panel) of households participating in MEPS begins each calendar year, providing overlapping panels of survey data (at any given time there are two panels of MEPS households being interviewed). Complete data from ten full panels of the 1996-2006 MEPS were pooled through a public-use linkage file prior to analyses. Additional detailed methodology and a description of data available in MEPS are available at: www.meps.ahrq.gov.
Our sample included children 0-17 years of age whose parents were interviewed about their healthcare expenditures in one of ten full panels of MEPS from 1996-2006. Households were eligible for this study if 1) at least one child in the family had an ongoing limitation1, or 2) none of the children in the family had any limitations. All other households were excluded (n=2,546). Among households where only one child had an ongoing limitation, we selected that child to represent the household; otherwise, one child with a limitation was selected at random, using a random number generator. Among households in which no child had a limitation, one child was selected at random. Parents of selected children with incomplete demographic and health information or zero weights were excluded from this study (n=1,482). For households with multiple parents, one parent was chosen at random to be part of this analysis to avoid the correlation of measures among parents of the same children. This resulted in a final sample of 17,857 families with at least one child less than 18 years of age.
Measures
Dependent Variable: Financial Burden
Dependent variables included three levels of financial burden. Specifically, we measured financial burdens based on healthcare expenditures of the index child, other family members, and the whole family separately. Absolute and relative measures of burden were examined. OOP healthcare expenditures were self-reported payments made by the patient or the patient's family for any of the following healthcare services: in-patient, out-patient, office-based, emergency room, dental, home-health, prescription, and other medical expenses. These data collected from household respondents were compared and validated with medical provider records. Expenditures were examined separately for those expenses pertaining to the index child, other family members and for the whole family's collective OOP healthcare expenditures. OOP expenditures reported for MEPS survey years one and two were summed at the child, other family member or whole family level and then annualized. Absolute financial burden was measured in terms of OOP healthcare expenditures. At the child, other family member and whole family level, absolute burden was defined as the sum of OOP expenditures for the child and the sum of OOP expenditures for all family members, respectively. Other family members' absolute burden was defined as the sum of OOP expenditures for all family members except for the index child.
Relative financial burden was measured as the ratio of OOP healthcare expenditures (“numerator”) to adjusted household income (“denominator”). Household income was adjusted for household composition using the Organization for Economic Cooperation and Development (OECD) modified income equivalence scale (Hagenaars et al. 1994). The OECD-modified scale was chosen for this study because it examines both family size and composition (i.e. number of adults and children under 14) and, importantly, assumes moderate economies of scale are achieved by larger families thanks to shared resources.
The OECD-modified scale assigns a value of 1.0 to the head of household, a value of 0.5 to each additional family member 14 years of age or older (a) and a value of 0.3 to each child under 14 years of age (c). The gross annual family-level income was calculated for Year 1 and Year 2 for each MEPS panel and then used to calculate the OECD-adjusted income for both years. To account for any variability in income over the study period, the OECD-adjusted incomes for Year 1 and Year 2 were averaged and this average was used for all future measures of income and financial burden. To account for low or negative incomes (2.4% of our sample), a $1,000 floor was imposed as the gross annual family-level income prior to adjustment and then used in the calculations for adjusted annualized income. A sensitivity analysis revealed that altering the floor to $100 or to $500 did not significantly change our results. All measures of income and expenditures were adjusted for inflation based on 2006 dollars. Panel indicators were included in the analysis and it was determined that the predicted annual expenditures did not substantially change across the MEPS panels; therefore we were confident in concatenating the data from 1996-2006.
Independent Variables
Need factors: Childhood Activity Limitations
In recent decades, the “categorical” or “disease-specific” approach to defining childhood illness has been called into question, as evidence of the compelling commonalities among ill children and their families has emerged (Kohen et al. 2007; Pless and Perrin 1985; Stein et al. 1993). The term activity limitation has become an effective way to refer more generally to the physical, social, behavioral, and cognitive limitations that alter a child's ability to engage in age-appropriate roles, regardless of a child's specific medical condition or diagnosis. In this study, we used a non-categorical (i.e. not disease or diagnosis specific) definition of childhood activity limitation status to identify children who have impairments in their daily living activities (as appropriate for their developmental stage in life).
Children were defined as having activity limitations if they were “limited or prevented in any way in [their] ability to do the things most children of the same age can do” (Agency for Healthcare Research and Quality 2007) due to an impairment or a physical or mental health problem. In the 1996-2000 MEPS, parents of children aged 0-4 reported whether the child was limited in any way, including play activity, because of an impairment or physical or mental health problem. Similarly, parents with children aged 5-17 reported whether the child 1) had an impairment or physical or mental health condition that limited school attendance or required a special school program or 2) was limited in activities other than school because of an impairment or a physical or mental health problem. In the 2001-2006 MEPS, parents of children aged 0-17 reported whether the child: 1) was limited in or prevented from their ability to do the things most children of the same age can do, or 2) needed or received special therapy such as physical, occupational, or speech therapy. If any one of these variables had a “yes” response, the child was considered to have an activity limitation. If the relevant responses were all “no,” then the child was coded as having “no activity limitation.” Data on child limitation status was collected in Rounds 2 and 4 of the MEPS. For analysis, children were categorized into the following groups: 1) no limitations in either round (no limitation); and 2) limitations in both rounds (ongoing limitation). Households with children with a limitation in round 2 only or round 4 only were not included in the analysis. A sensitivity analysis determined that the 1996-2000 results were similar enough to the 2001-2006 results to use data from both time periods in the same analysis despite the question changes.
Predisposing factors: Sociodemographic Characteristics
We examined a number of child, parent, and family sociodemographic characteristics. Child characteristics included: child gender, age (0-3, 4-8, 9-12, and 13+), and race/ethnicity (white non-Hispanic; black non-Hispanic; other non-Hispanic; Hispanic). Parent characteristics included: parent gender, age (18-34, 35-44, 45+ years), race/ethnicity (white non-Hispanic; black non-Hispanic; other non-Hispanic; Hispanic), education level (did not graduate high school, graduated high school, some college, graduated college), and marital status (married versus not married). Family characteristics included: number of children in the household (one, two, or three or more), number of adults in the household (one, two, or three or more), U.S. region of residence (West, Northeast, Midwest, and South), and urbanicity (urban versus rural by Metropolitan Statistical Area (MSA) status).
Enabling factors: Health insurance
Child and parent health insurance status was categorized into four mutually exclusive categories: private (two years of private insurance), public (two years of public insurance or one year of public insurance and one year of private insurance, but continuously insured), partial (intermittent coverage, one year of public or private insurance and one year of no insurance coverage), none. We operationalized income in three ways. First, we present unadjusted family income in the sociodemographic description of our sample. Second, in models of absolute burden we used the unadjusted family income centered at $32,000 (which is the sample mean adjusted for 2006 dollars) (Kraemer and Blasey 2004) as a covariate. Third, in models of relative burden we used log2 of the OECD-adjusted income, centered at log2 $32,000, as a covariate. Note for the regressions that income was expressed in tens of thousands. In addition, indicator variables were created for each independent panel of the MEPS.
Analytic Approach
All analyses were conducted using survey procedures from SAS 9.2 and Stata 11.0 to correct for the complex sample design of the MEPS, using Taylor series expansion to compute variances. All results are based on weighted counts.
We used χ2 analyses to test for differences in OOP healthcare expenditures for the index child and the family by sociodemographic characteristics and children's activity limitation status. If differences were found in the overall χ2 tests, each subgroup was tested for statistical significance, in order to identify which subgroup(s) were influencing the overall group significance. Differences in the unadjusted income and mean parent and child age were tested using the Wilcoxon–Mann–Whitney test.
Absolute and relative financial burden, similar to most cost and utilization data (Diehr et al. 1999), were highly skewed to the right. Generalized linear models (GLM) were therefore used to model absolute and relative burden outcomes. For absolute burden we used a GLM with an identity link and a constant working variance (σ2 = φ). For relative burden we used a GLM with a log link and a working variance function proportional to the square of the mean (σ2 = φ μ2). The Huber/White/sandwich estimate of variance was used to obtain the robust variance estimates while accounting for heteroskedasticity and clustering (Froot 1989).
GLMs were used to determine the relationship among childhood activity limitation status, log base two of the OECD-adjusted income, and financial burden for the child, other family members and whole family, adjusting for demographic factors. For all of the models of absolute burden, we adjusted for the number of children and the number of adults in the household.
| (1) |
For child-level financial burden (Yc), the analyses adjusted for child demographics (including child gender, age, race/ethnicity), parent demographics (including parent education and marital status), child health insurance status, U.S. region of residence, MSA status, and panel indicator. The interaction between child limitation status and log base two of the OECD-adjusted income was also examined.
| (2) |
For other family members' financial burden (Yo), the analyses adjusted for parent demographics (including parent gender, age, race/ethnicity, education, marital status), parent health insurance status, U.S. region of residence, MSA status, and panel indicator. The interaction between child limitation status and log base two of the OECD-adjusted income was also examined.
| (3) |
For whole family financial burden (Yf), the analyses adjusted for parent demographics (including parent gender, age, race/ethnicity, education, marital status), child health insurance status, parent health insurance status, U.S. region of residence, MSA status, and panel indicator. The interaction between child limitation status and log base two of the OECD-adjusted income was also examined.
To ensure that the relationship between our main independent variables (child limitation status and income) and the outcome did not vary by time, we tested for interactions between the panel indicators and child limitation status and income. We applied the Bonferroni correction to adjust for the twelve tests (six outcomes – child-level absolute burden, child-level relative burden, other family members' absolute burden, other family members' relative burden, whole family absolute burden, and whole family relative burden – by two independent variables). None of these interactions was significant and therefore not included in the final models.
RESULTS
Table 1 presents the sociodemographic characteristics of U.S. parents by type of childhood activity limitation (no limitation and ongoing). Overall, 7.2% of families had a child aged 0-17 years with an ongoing limitation over the two-year study period. Children with an ongoing activity limitation were more likely to be male, older, and non-Hispanic. These children were less likely to have private, partial or no insurance and more likely to have public insurance. Compared with parents of children without limitations, parents of children with an ongoing activity limitation were more likely to be older, white (Non-Hispanic), less educated, and have a lower income. These parents were less likely to have private insurance and more likely to have public insurance. Families of children with activity limitations had more children and fewer adults living in the household. Parents of children with activity limitations did not differ from those without by gender, marital status, or urbanicity but did differ overall by U.S. region of residence.
Table 1.
Sociodemographic Characteristics of Families by Childhood Activity Limitation Status
| Child Activity Limitation Status | |||||
|---|---|---|---|---|---|
| TOTAL | No Limitation |
Ongoing Limitationa |
Overall Chi-square P-value |
Chi-square P-valueb |
|
| TOTAL: weighted | 28,533,652 | 26,481,788 | 2,051,864 | ||
| %: weighted | 92.8% | 7.2% | |||
| TOTAL: unweighted | 17,857 | 16,410 | 1,447 | ||
| %: unweighted | 91.9% | 8.1% | |||
| Child Characteristics | |||||
| Gender | *** | ||||
| Male | 49.5% | 63.9% | |||
| Female | 50.5% | 36.1% | |||
| Age (Mean) | 8.4 | 9.4 | *** | ||
| Race/Ethnicity | NS | ||||
| White (Non-Hispanic) | 62.3% | 64.7% | NS | ||
| Black (Non-Hispanic) | 13.9% | 15.3% | NS | ||
| Other (Non-Hispanic) | 6.0% | 5.2% | NS | ||
| Hispanic | 17.9% | 14.8% | ** | ||
| Health Insurance Status | *** | ||||
| Private | 67.8% | 55.8% | *** | ||
| Public | 21.1% | 38.3% | *** | ||
| Partial | 5.0% | 3.2% | ** | ||
| None | 6.2% | 2.8% | *** | ||
| Parent Characteristics | |||||
| Gender | NS | ||||
| Male | 44.3% | 43.2% | |||
| Female | 55.7% | 56.8% | |||
| Age (Mean) | 37.3 | 38.3 | *** | ||
| Race/Ethnicity | *** | ||||
| White (Non-Hispanic) | 66.1% | 72.4% | *** | ||
| Black (Non-Hispanic) | 11.5% | 11.0% | NS | ||
| Other (Non-Hispanic) | 6.1% | 3.4% | ** | ||
| Hispanic | 16.2% | 13.1% | ** | ||
| Marital Status | |||||
| Married | 79.2% | 76.9% | NS | ||
| Not Married | 20.8% | 23.1% | |||
| Education status | * | ||||
| No or some high school | 15.8% | 19.2% | ** | ||
| High school graduate | 33.0% | 33.2% | NS | ||
| Some college | 23.7% | 23.8% | NS | ||
| College or beyond | 27.5% | 23.7% | * | ||
| Health Insurance Status | *** | ||||
| Private | 75.7% | 68.0% | *** | ||
| Public | 8.0% | 15.2% | *** | ||
| Partial | 5.9% | 7.1% | NS | ||
| None | 10.4% | 9.8% | NS | ||
| Family Characteristics | |||||
| Number of children (≤18) | |||||
| 1 | 39.3% | 24.0% | *** | *** | |
| 2 | 40.2% | 41.0% | NS | ||
| 3+ | 20.5% | 35.0% | *** | ||
| Number of adults | ** | ||||
| 1 | 18.5% | 20.7% | NS | ||
| 2 | 67.9% | 68.5% | NS | ||
| 3+ | 13.8% | 10.7% | ** | ||
| Income (Mean, US$) | 32,447 | 26,950 | *** | ||
| Region of US | * | ||||
| Northeast | 18.5% | 21.4% | NS | ||
| Midwest | 23.0% | 25.3% | NS | ||
| South | 35.1% | 32.8% | NS | ||
| West | 23.4% | 20.5% | NS | ||
| MSA Status | NS | ||||
| Urban | 81.6% | 80.9% | |||
| Rural | 18.4% | 19.7% | |||
Abbreviations: NA, not applic able; NS, not significant
Limitation reported in both Rounds 2 and 4.
Statistically significant chi-square test for each category of characteristic.
p <0.05
p <0.01
p<0.001
Data from MEPS 1996-2006
Regression analyses were used to determine the relationship between childhood activity limitation status and absolute financial burden at the child, other family member, and whole family levels, adjusting for covariates (Table 2). At the child level, having an ongoing activity limitation was associated with an increase in absolute burden of $296.18 for families at the mean income (of $32,000). Doubling mean income resulted in an additional $22.19 in absolute burden for children without an activity limitation and an additional $79.05 in absolute burden for children with an activity limitation, indicating a significant interaction between income and childhood activity limitation status. Child characteristics associated with increased child-level absolute burden included age (with older children having greater levels of burden) and the female gender. Being non-white, having public insurance, having less educated parents, having three or more children in the household, residing in the Midwest and residing in a rural area were all associated with a decreased child-level absolute burden.
Table 2.
Generalized Linear Regression Analyses of Absolute Financial Burden among Families with and without Childhood Activity Limitations
| Absolute Out-of-Pocket Expenditures | |||
|---|---|---|---|
| Child Absolute Burden Beta (SE) |
Other Family Members' Absolute Burden Beta (SE) |
Whole Family Absolute Burden Beta (SE) |
|
| Intercept | 208.41 (30.64)*** | −278.29 (86.21)*** | −341.27 (95.73)*** |
| Child Limitation Status | |||
| No Limitation | Reference | Reference | Reference |
| Ongoing Limitation | 296.18 (43.65)*** | 287.77 (54.88)*** | 594.36 (68.98)*** |
| Incomea | 22.19 (6.11)*** | 42.19 (8.70)*** | 60.31 (10.92)*** |
| Child Limitation Status*Income | 56.86 (24.12)* | 29.55 (28.98) | 83.28 (37.98)* |
| Genderb | |||
| Male | Reference | Reference | Reference |
| Female | 41.36 (13.66)** | 45.47 (26.62) | 80.48 (28.12)** |
| Ageb | 22.60 (1.47)*** | 21.63 (2.09)*** | 32.08 (2.14)*** |
| Race/ethnicityb | |||
| White (Non-Hispanic) | Reference | Reference | Reference |
| Black (Non-Hispanic) | −139.21 (18.07)*** | −403.29 (29.53)*** | −551.17 (32.47)*** |
| Other (Non-Hispanic) | −163.74 (20.56)*** | −427.40 (46.74)*** | −582.92 (48.39)*** |
| Hispanic | −85.33 (18.12)*** | −358.44 (31.19)*** | −462.81 (33.57)*** |
| Child Health Insurance Status | |||
| Private | Reference | Reference | |
| Public | −63.37 (20.57)** | −190.69 (39.29)*** | |
| Partial | 8.76 (29.03) | 144.53 (83.86) | |
| None | −30.76 (39.09) | 72.89 (73.01) | |
| Parental Health Insurance Status | |||
| Private | Reference | Reference | |
| Public | −51.66 (34.38) | 20.85 (44.45) | |
| Partial | 65.71 (69.13) | 48.94 (64.57) | |
| None | 58.13 (47.55) | 64.97 (55.69) | |
| Parental Education Status | |||
| No or some high school | −160.79 (25.00)*** | −284.26 (39.96)*** | −372.95 (45.87)*** |
| High school graduate | −112.09 (25.43)*** | −230.47 (37.71)*** | −282.89 (42.75)*** |
| Some college | −81.61 (25.22)*** | −114.68 (43.04)** | −153.75 (45.66)*** |
| College or beyond | Reference | Reference | Reference |
| Parental Marital Status | |||
| Married | Reference | Reference | Reference |
| Not Married | −37.95 (12.64)** | 71.16 (37.41) | 59.32 (38.59) |
| Number of children (≤18) | |||
| 1 | Reference | Reference | Reference |
| 2 | −15.31 (16.30) | 116.06 (29.64)*** | 112.94 (29.02)*** |
| 3+ | −57.22 (15.19)*** | 331.60 (37.39)*** | 304.57 (39.07)*** |
| Number of adults | |||
| 1 | Reference | Reference | Reference |
| 2 | −17.99 (17.97) | 366.37 (40.00)*** | 344.20 (45.56)*** |
| 3+ | −11.21 (23.60) | 732.11 (53.62)*** | 707.64 (58.91)*** |
| MSA Statusc | |||
| Urban | Reference | Reference | Reference |
| Rural | −35.70 (19.46) | 79.76 (34.23)* | 55.52 (38.75) |
Income adjusted using the OECD scale, centered and divided by 10,000
For Child Absolute Burden model, covariates reflect the status of the child.
For Family Absolute Burden model, covariates reflect the status of the parent.
MSA = Metropolitan Statistical Area
p <0.05
p <0.01
p<0.001
Data from MEPS 1996-2006; also controlling for region of the US and panel (cohort) years SE = linearized standard error
For other family members, having a child with an ongoing activity limitation was associated with a $287.77 increase in absolute burden. Doubling the income of families with and without children with activity limitations was associated with an increase in absolute burden of $42.19 and $71.74, respectively. There was not a significant interaction between income and childhood activity limitation status on other family members absolute burden. Increasing parent age, having two or more children in the household, having two or more adults in the household and residing in the South were associated with increased other family member-level absolute burden. Parent characteristics associated with decreased other family member-level absolute burden included being non-white, being less educated and being unmarried.
At the whole family level, having a child with an ongoing activity limitation was associated with a $594.36 increase in absolute burden. Doubling the income of families with and without children with activity limitations was associated with an increase in absolute burden of $60.31and $143.59, respectively. There was a significant interaction between income and childhood activity limitation status on whole family-level absolute burden. Older parent age, female gender, having two or more children in the household, having two or more adults in the household and residing in the South were associated with increased whole family-level absolute burden. Parent characteristics associated with decreased family-level absolute burden included being non-white, the child having public insurance, being less educated and being unmarried.
Similarly, regression analyses were used to determine the relationship between childhood activity limitation status and relative financial burden for child, other family members, and the whole family, adjusting for covariates (Table 3). At the child level, having an ongoing activity limitation was associated with a 2.46-fold increase in relative burden for families at the mean income. Doubling the mean income resulted in a 38% reduction in relative burden for children without an activity limitation and a 51% reduction in relative burden for children with an activity limitation, demonstrating a significant interaction between income and childhood activity limitation status. Child characteristics associated with increased child-level relative burden included age, the female gender and residing in the South. Being non-white, having public insurance and having less educated parents were associated with decreased child-level relative burden.
Table 3.
Generalized Linear Regression Analyses of Relative Financial Burden among Families with and without Childhood Activity Limitations
| Relative Out-of-Pocket Expenditures | |||
|---|---|---|---|
| Child Relative Burden Beta (SE) |
Other Family Members' Relative Burden Beta (SE) |
Whole Family Relative Burden Beta (SE) |
|
| Intercept | −5.44 (0.09)*** | −4.49 (0.09)*** | −4.38 (0.07)*** |
| Child Limitation Status | |||
| No Limitation | Reference | Reference | reference |
| Ongoing Limitation | 0.90 (0.09)*** | 0.31 (0.04)*** | 0.43 (0.04)*** |
| Incomea | −0.47 (0.04)*** | −0.57 (0.02)*** | −0.57 (0.02)*** |
| Child Limitation Status*Income | −0.24 (0.09)** | −0.02 (0.04) | −0.04 (0.04) |
| Genderb | |||
| Male | Reference | Reference | Reference |
| Female | 0.16 (0.05)*** | 0.04 (0.03) | 0.06 (0.02)** |
| Ageb | 0.08 (0.01)*** | 0.03 (0.00)*** | 0.03 (0.00)*** |
| Race/ethnicityb | |||
| White (Non-Hispanic) | Reference | Reference | Reference |
| Black (Non-Hispanic) | −0.74 (0.10)*** | −0.49 (0.05)*** | −0.53 (0.04)*** |
| Other (Non-Hispanic) | −0.55 (0.12)*** | −0.31 (0.06)*** | −0.35 (0.05)*** |
| Hispanic | −0.32 (0.07)*** | −0.33 (0.04)*** | −0.35 (0.03)*** |
| Child Health Insurance Status | |||
| Private | Reference | Reference | |
| Public | −0.73 (0.11)*** | −0.18 (0.04)*** | |
| Partial | 0.09 (0.11) | 0.10 (0.07) | |
| None | −0.08 (0.11) | 0.08 (0.07) | |
| Parental Health Insurance Status | |||
| Private | Reference | Reference | |
| Public | −0.14 (0.06)* | −0.12 (0.06) | |
| Partial | 0.05 (0.06) | 0.01 (0.06) | |
| None | 0.13 (0.05)** | 0.10 (0.05)* | |
| Parental Education Status | |||
| No or some high school | −0.69 (0.09)*** | −0.17 (0.05)*** | −0.20 (0.04)*** |
| High school graduate | −0.32 (0.07)*** | −0.16 (0.03)*** | −0.16 (0.03)*** |
| Some college | −0.16 (0.07)* | −0.10 (0.03)** | −0.09 (0.03)** |
| College or beyond | Reference | Reference | Reference |
| Parental Marital Status | |||
| Married | Reference | Reference | Reference |
| Not Married | −0.08 (0.06) | −0.22 (0.03)*** | −0.16 (0.03)*** |
| MSA Statusc | |||
| Urban | Reference | Reference | Reference |
| Rural | −0.06 (0.07) | 0.13 (0.04)** | 0.10 (0.04)** |
Log base 2 of Income adjusted using the OECD scale and centered
For Child Relative Burden model, covariates reflect the status of the child.
For Family Relative Burden model, covariates reflect the status of the parent.
MSA = Metropolitan Statistical Area
p <0.05
p <0.01
p<0.001
Data from MEPS 1996-2006; also controlling for region of the US and panel (cohort) years SE = linearized standard error
At the other family member level, having a child with an ongoing activity limitation was associated with a 36% increase in relative burden of for families at the mean income. Among families of children without an activity limitation, doubling mean income resulted in 44% reduction in relative burden; families of children with an activity limitation saw a 45% reduction in relative burden with a doubling of income. The interaction between child limitation status and income was not significant on the other family member level for relative burden, however. Older parent age, having no insurance, residing in the South and residing in a rural area were associated with increased other family-level relative burden. Parent characteristics associated with decreased other family-level relative burden included being non-white, having public insurance, being less educated and not married.
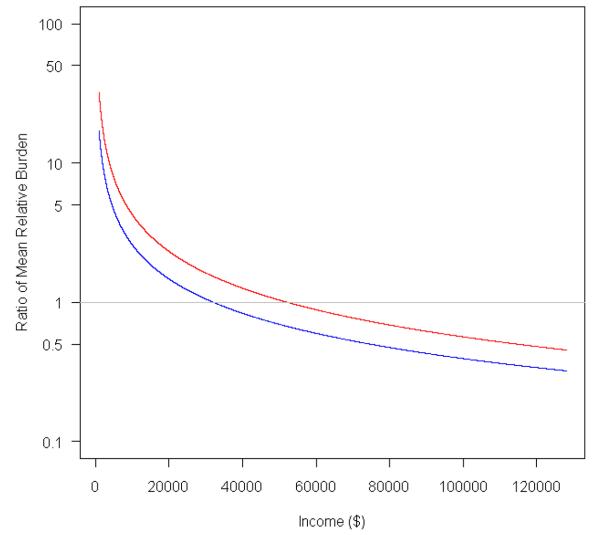
At the whole family level, having a child with an ongoing activity limitation was associated with a 54% increase in relative burden of for families at the mean income. Among families of children without an activity limitation, doubling mean income resulted in 44% reduction in relative burden; families of children with an activity limitation saw a 46% reduction in relative burden with a doubling of income. The interaction between child limitation status and income was not significant on the whole family-level for relative burden, however. Older parent age, female gender, having no insurance, residing in the South and residing in a rural area were associated with increased family-level relative burden. Parent characteristics associated with decreased family-level relative burden included being non-white, the child having public insurance, being less educated and not married.
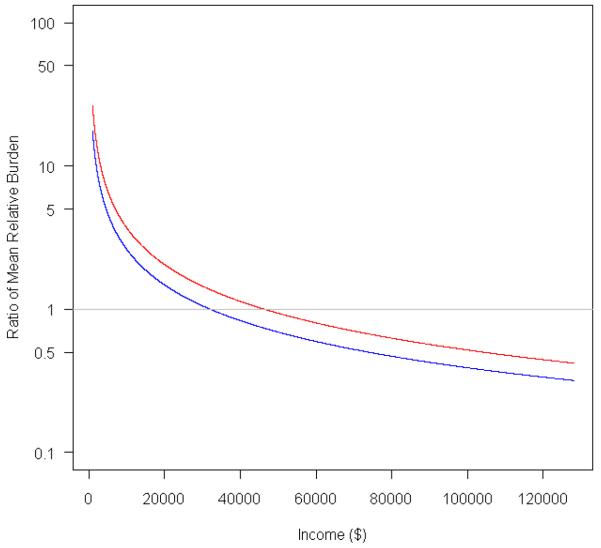
Figure 1 depicts the disparities in absolute and relative financial burden for the child, other family members and the whole family as a function of family OECD-adjusted income. The reference point (gray line) in all six panels is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis in Panels A, B and C represents the mean change in absolute burden in 2006 dollars. For Panels D, E and F, the y axis represents the ratio of the mean change in relative burden presented on a log scale. At the child level, although absolute burden increases with increasing income, relative burden decreases (Panels A and D, respectively). For other family members, absolute burden increases with increasing income, and relative burden remains relatively constant across income (Panels B and E, respectively). At the whole family level, absolute burden increases with increasing income, while relative burden remains relatively constant across income (Panels B and D, respectively).
Figure 1.
Figure 1A – Child-Level Absolute Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1A depicts the disparities in absolute financial burden for the child as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the mean change in absolute burden in 2006 dollars. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
Figure 1B – Other Family Members Absolute Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1B depicts the disparities in absolute financial burden for other family members as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the mean change in absolute burden in 2006 dollars. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
Figure 1C – Whole Family Absolute Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1C depicts the disparities in absolute financial burden for the whole family as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the mean change in absolute burden in 2006 dollars. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
Figure 1D – Child-Level Relative Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1D depicts the disparities in relative financial burden for the child as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the ratio of the mean change in relative burden presented on a log scale. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
Figure 1E – Other Family Members Relative Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1E depicts the disparities in relative financial burden for other family members as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the ratio of the mean change in relative burden presented on a log scale. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
Figure 1F – Whole Family Relative Financial Burden in the US, by Childhood Activity Limitation Status and Income
Figure 1F depicts the disparities in relative financial burden for the whole family as a function of family OECD-adjusted income. The reference point (gray line) is centered at the burden for families of children without an activity limitation with a mean income of $32,000. The y axis represents the ratio of the mean change in relative burden presented on a log scale. The red line indicates children with activity limitations and the blue line represents children without activity limitations.
DISCUSSION
This study on financial burden in families of children with activity limitations contributes new and important findings to the literature and confirms the results of previous studies. Our results are the first to show that families of children with activity limitations are more likely to experience financial burden due to child and family-level OOP expenditures. This demonstrates that the financial impact of caring for a child with an activity limitation is not limited to child-level expenditures, but may spill over to expenditures of other members of the family, further supporting our theoretical framework. As such, attempts to limit financial burden for these families must include provisions that address the family-level consequences of activity limitations.
Furthermore, families of children with activity limitations experience greater financial burden, regardless of income, than those without activity limitations. These families increase their spending with rising income at a faster rate, leading to more substantial absolute burden at higher incomes. Conversely, on the relative scale, disparities in child-level burden are more substantial at lower incomes, but remain steady across the income distribution on the family level. Figure 1 represents these findings visually. Although these outcomes may appear contradictory, this demonstrates how low absolute OOP expenditures for low-income families may represent a much larger proportion of family income and thus characterize significant relative financial burden, a finding consistent with other studies (Francoeur 2002; Houtrow et al. 2008; Lukemeyer et al. 2000; Newacheck 2005; Williams et al. 1991). If increased spending correlates with improved outcomes, the disparities in financial burden between families of children with and without activity limitations may in fact be representative of serious inequities that could contribute to worse health outcomes.
The only modifiable factor that was shown to reduce child and whole family-level burden on both the absolute and relative scale was children's public insurance. This is consistent with other studies, which demonstrated that state-sponsored insurance can reduce both absolute and relative burden among low income families who qualified for State Children's Health Insurance Programs (SCHIP) (Parish et al. 2009). Thus, public health insurance coverage may offer a promising avenue for reducing financial burden. Consistent with the Anderson behavioral model (1995), public insurance – specifically insurance that provides comprehensive coverage and increased eligibility for families of children with activity limitations – may serve as an additional enabling factor that could increase access to valuable health care services for those with the greatest need.
Strikingly, there was no difference in burden for children or families with no or partial insurance compared to private insurance except in the case of family-level relative burden. One possible explanation for the apparent inability of private insurance to provide adequate protection against financial burden associated with OOP medical expenditures is the growing problem of underinsurance. Similarly, the effect of public insurance compared to private insurance may be a reflection of the positive effects due to the generosity of benefits and low-cost sharing associated with public insurance. Although individuals and families may have private coverage, the lack of needed benefits or high level of cost-sharing renders their insurance coverage inefficient at reducing burden and may even contribute to excessive financial burden.
Other factors, such as preferences for or usage patterns of healthcare, may also influence medical expenditures and subsequence financial burden. Those who are non-white, less educated, or unmarried may have less burden, regardless of insurance coverage, because they are not accessing the system. Non-white individuals, for example, have lower levels of healthcare utilization than white individuals (Andersen and Newman 2005), possibly due to patient preferences or attitudes, provider bias, or other pathways (Fiscella et al. 2000). Similar pathways may impact healthcare utilization among those who are less educated. Further, evidence has shown that those who are married are more likely to receive medical checkups (Culica et al. 2002), possibly because they are encouraged to do so by their partner. As such, those who are not accessing the system may be incurring less financial burden not because they are healthier, but because they are delaying or foregoing care.
Our results show that even while accounting for the role of insurance, income disparities in financial burden still exist, indicating that insurance is necessary but not sufficient to alleviate burden. Moreover, such disparities exist across income levels. Expansion of coverage and eligibility and improved generosity of benefits may be one avenue to reduce such disparities. SCHIP was originally established as a public insurance expansion to address the well-noted lack of insurance coverage for families with incomes above the Medicaid threshold (Congressional Budget Office 2007) (Vimo 2007). Aside from the broad federal guidelines for the use of SCHIP funds, states are responsible for administering the program and determining the eligibility requirements (Congressional Budget Office 2007). However, with variation in SCHIP eligibility from state-to-state, there is no guarantee that the families of children with activity limitations will be afforded a reduction in their child, or family-level, financial burden.
Families experiencing greater financial burden may be more likely to delay care or reduce their use of healthcare services in an effort to preserve the funds that would otherwise be spent on medical expenses (Rimsza et al. 2007; Singh and Golden 2006; Wielawski 2000). For those families who are forced to delay or forego necessary treatment, their conditions are more likely to deteriorate and the resulting acute illnesses are often more expensive to treat (Rimsza et al. 2007). Frequently, acute conditions are treated in public hospitals and emergency rooms where, if the patient cannot pay the full cost of treatment, the bill is passed on to others through taxes (public funds supporting local hospitals) or higher insurance premiums (Singh and Golden 2006). Ultimately, financial burden can affect all members of society, regardless of their personal healthcare utilization or insurance coverage.
Since parent's healthcare utilization has been shown to be a strong predictor of children's healthcare use (Hanson 2001), increasing parental access to healthcare may result in better management of children's limitations and appropriate utilization of healthcare services. This has important implications for future policy decisions, both at state and federal levels, regarding the eligibility criteria and expansion of coverage. Ultimately, providing increased access only for children may not be sufficient to improve healthcare utilization or to reduce need and burden on the family.
In Wisconsin, the SCHIP federal funds contribute to BadgerCare, which is a state-run health insurance program that provides comprehensive, affordable coverage not only for uninsured children who meet the SCHIP criteria, but also their parents. All low to moderate-income families, with a child under the age of 19, who do not qualify for Medicaid in Wisconsin are eligible for BadgerCare. It has been estimated that BadgerCare increased the public healthcare coverage of all adults previously receiving cash assistance from Aid to Families with Dependent Children (AFDC) or Temporary Assistance for Needy Families (TANF) by about 17-25% points (Wolfe et al. 2006). Several studies have reported that SCHIP expansion in coverage reduced the likelihood that a parent will report forgoing needed medical care due to cost and an increased utilization of preventative care (Buchmueller et al. 2005; Busch and Duchovny 2005; Guendelman et al. 2006; Yu et al. 2008). Furthermore, the impact of this increase in insurance coverage is expected to manifest in the form of increased healthcare utilization and positive health outcomes.
Other complicating factors may exacerbate financial hardship for these families, including work-related problems, debt, and family functioning. Previous research indicates that parents of children with limitations are less able to maintain employment, reporting reductions in their work attendance or participation (Baydar et al. 2007; Gordon et al. 2007; Kuhlthau et al. 2001; Leiter et al. 2004; Witt et al. 2003). Parents of children with activity limitations, specifically, are more likely to work only part-time or be unemployed (Kuhlthau et al. 2008) and miss more days of work to care for themselves and others (Kuhlthau et al. 2008; Witt and DeLeire 2009). The resulting reduction in income or earning potential can compound the financial burden placed on the family, and has long-term implications for parents', particularly women's, economic well-being as they age (Parish et al. 2004). Lower income may also present a barrier to accessing non-health care goods and services (good child care, developmentally appropriate toys, private programs/services) that affect the extent to which a child's activity limitation is actually disabling.
Medical debts are also a growing issue for many Americans (Seifert and Rukavina 2006), including parents of children with disabilities (Sharpe and Baker 2007). Between 2003 and 2007, the proportion of working age Americans with medical debt rose from 34% to 41% (Doty et al. 2008). Medical debt has been associated with home foreclosures (Pollack and Lynch 2009), poor mental health (Fitch et al. 2009; Jenkins et al. 2008; Reading and Reynolds 2001), and can compound the effect of financial burden on the family thereby leading to worse health and economic outcomes.
In addition to the growing literature on the prevalence and distribution of financial burden related to health care expenses, there is a long history of research on the effects of financial stress on families. This body of work shows unequivocally that financial hardship and stress negatively influences family functioning, parental emotional well-being, parenting behaviors, and in turn, children's socio-emotional functioning and school performance (Coley and Chase-Lansdale 2000; Conger et al. 1992; Gutman and Eccles 1999; Jackson et al. 2000; McLoyd 1998). Caring for a child with activity limitations can also shift family members' roles at different levels of the social environment (Biddle 1979; Major 2003) leading to additional stress and possible additional health problems (House 1974; McEwen 1998; Patterson 1989). Of particular relevance to this study, parents whose emotional well-being has been harmed by financial stress may be less able to effectively manage the child's chronic condition (Bartlett et al. 2001; Fisher and Weihs 2000; Shalowitz et al. 2001).
The disparities we see across the income gradient may be indicative that the support systems currently in place may not adequately address the needs of many families of children with activity limitations. Although public insurance, income transfer, and early intervention programs are in place, families still have substantial out-of-pocket expenditures for healthcare (Kuhlthau et al. 2005). Programs available to low income families and children with disabilities reach only a portion of families of children with activity limitations, while state-level insurance and early intervention programs have varying levels of comprehensiveness (Parish et al. 2009) and may not adequately address the needs of all family members (Davidoff et al. 2004; Department of Health and Human Services Washington DC 1998; Hebbeler et al. 1999). It is clear from these studies and our findings that additional assistance is needed across the income spectrum in order to alleviate extreme financial burden. Furthermore, as indicated by Cunningham (2010), reducing financial burden will also require increases in family income – a shift which may be particularly difficult to achieve among families affected by activity limitations.
More attention should be given to providing comprehensive coverage and expanding eligibility to vulnerable families. However, few studies have examined the intricacies of benefit plan design and thus are not able to determine specifically why insurance is not effective at reducing burden. Given the substantial heterogeneity of the plan benefits and cost-sharing within the private insurance category, this is an avenue of research that merits dedicated investigation. Future studies should seek to identify the characteristics and patterns of insurance that will be most effective at reducing burden and eliminating disparities.
This study has several potential limitations. First, it is possible that our results could have been influenced by unobserved variables that may have biased our parameter estimates. However, it is unclear what magnitude, direction, or the ultimate impact that this could have on our findings.
Second, data on childhood limitation status and OOP expenditures are based solely on household reports. Although parents are often the best source of information about their children, parental reports may be influenced by parents' own health and mental health status. This may be further complicated in households where different parents respond on behalf of themselves, their spouses, and their children in different rounds of the survey. Similarly, respondents may incorrectly report their expenditures; however, the verification process used by the MEPS limits this concern.
Second, this study examined children's activity limitations, as opposed to specific health conditions, and therefore we are not able to discuss potential causes for financial burden among those caring for children with activity limitations. However, using a non-categorical measure of child activity limitation likely reduces the impact of confounders associated with obtaining a medical diagnosis, such as socioeconomic status, race/ethnicity, and health insurance status (Wells and Hogan 2003). Moreover, consideration of activity limitation is perhaps more relevant to policy where functionality, not diagnosis, is the target (Kohen et al. 2007). Additionally, by estimating the burden of child health conditions by only considering children whose illness or disability affects their activity, we are likely underreporting the disparity in burden between healthy children and children with health conditions regardless of activity limitation status (Kohen et al. 2007; Wells and Hogan 2003). While there is a possibility of some genetic spillover (from parent to child), this is likely to contribute a negligible amount to the overall increase in burden that we observed because almost all childhood chronic conditions and activity limitations have strong lifestyle components (Perrin et al. 2007; Van Cleave et al. 2010) and even diseases with known genetic causes have a great deal of variability in penetrance (Van Cleave et al. 2010).
Additionally, we utilized gross annual family-level income prior to adjustment, as opposed to net annual income, eliminating our ability to use take-home income after taxes had been deducted in the analysis. As a result of using gross income, we have larger estimates of family-level income, which may not be an accurate reflection of the liquid income available to these families. However, the use of gross income would suggest that our estimates of relative burden are likely to be conservative, given that the use of net income would increase the ratio of relative burden to adjusted income (after taxes had been deducted).
Finally, our study examined OOP healthcare expenditures and likely does not capture the full range of added costs of caring for a child with an activity limitation. Such additional costs could include special equipment, alterations to the home, travel, and special education. Since we were not able to include these non-medical expenses in our study, our results are likely conservative with regards to the total expenditures incurred as a result of activity limitations.
CONCLUSION
Families of children with activity limitations experience both greater absolute and relative financial burden compared to families of children without activity limitations. Childhood activity limitations are not only responsible for increased expenditures related to the child's healthcare, but also for increased healthcare expenditures by the family as a whole. An increase in family-level expenditures may indicate the rippling effect that an entire family can experience as a result of childhood activity limitations. Furthermore, families of children with activity limitations experience greater financial burden, regardless of income, than those without activity limitations. More policies are needed to assist families in obtaining affordable, comprehensive insurance coverage that will reduce out-of-pocket expenses and enable access to appropriate health care services. To address the disparities in burden and assist those families with the greatest needs, it will be particularly important to re-evaluate SCHIP eligibility requirements and expanded coverage to include the entire family. Future research should investigate the change in burden over time and how insurance type and benefit plan design affects the absolute and relative burden for families of children with activity limitations.
Acknowledgements
This research was supported by a grant from the National Institute of Child Health and Human Development (HD049533, Principal Investigator W.P. Witt) and the Robert Wood Johnson Foundation (MSN106189, Principal Investigator J. Mullahy). We would also like to thank Jing Jian Xiao, Manouchehr Mokhtari, and the anonymous reviewers for their helpful suggestions and comments.
Footnotes
Please note that “ongoing limitations” are defined in the section on ‘Independent variables’ in the Methods of the paper.
Contributor Information
Whitney P. Witt, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison
Kristin Litzelman, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison.
Carmen G. Mandic, Center for Research on Gender & Sexuality, San Francisco State University
Lauren E. Wisk, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison
John M. Hampton, University of Wisconsin Carbone Cancer Center
Paul D. Creswell, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison
Carissa A. Gottlieb, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison
Ronald E. Gangnon, Department of Population Health Sciences, School of Medicine and Public Health, University of Wisconsin-Madison
REFERENCES
- Agency for Healthcare Research and Quality [Retrieved April 13, 2008];MEPS HC-097: 2005 Full Year Consolidated data File. MEPS Data Documentation. 2007 from http://www.meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h97/h97doc.shtml.
- Altman BM, Cooper PF, Cunningham PJ. The case of disability in the family: Impact on health care utilization and expenditures for nondisabled members. Milbank Quarterly. 1999;77(1):39–75, iv. doi: 10.1111/1468-0009.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen R, Newman J. Societal and individual determinants of medical care utilization in the United States. Milbank Quarterly. 2005;83(4):95–124. [PubMed] [Google Scholar]
- Andersen RM. Behavioral model of families' use of health services. Center for Health Administration Studies, University of Chicago; Chicago: 1968. (No. 25). [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36(1):1–10. [PubMed] [Google Scholar]
- Banthin JS, Bernard DM. Changes in financial burdens for health care: National estimates for the population younger than 65 years, 1996 to 2003. Journal of the American Medical Association. 2006;296(22):2712–2719. doi: 10.1001/jama.296.22.2712. [DOI] [PubMed] [Google Scholar]
- Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS. Maternal depressive symptoms and emergency department use among inner-city children with asthma. Archives of Pediatrics and Adolescent Medicine. 2001;155(3):347–353. doi: 10.1001/archpedi.155.3.347. [DOI] [PubMed] [Google Scholar]
- Baydar N, Joesch JM, Kieckhefer G, Kim H, Greek A. Employment behaviors of mothers who have a child with asthma. Journal of Family and Economic Issues. 2007;28(3):337–355. [Google Scholar]
- Biddle B. Role theory: Expectations, identities and behaviors. Academic Press; New York, NY: 1979. [Google Scholar]
- Bronfenbrenner U. The ecology of human development: Experiments by nature and design. Harvard University Press; Cambridge, MA: 1979. [Google Scholar]
- Buchmueller TC, Grumbach K, Kronick R, Kahn JG. The effect of health insurance on medical care utilization and implications for insurance expansion: A review of the literature. Medical Care Research and Review. 2005;62(1):3–30. doi: 10.1177/1077558704271718. [DOI] [PubMed] [Google Scholar]
- Busch SH, Duchovny N. Family coverage expansions: Impact on insurance coverage and health care utilization of parents. Journal of Health Economics. 2005;24(5):876–890. doi: 10.1016/j.jhealeco.2005.03.007. [DOI] [PubMed] [Google Scholar]
- Coley RL, Chase-Lansdale PL. Welfare receipt, financial strain, and African-American adolescent functioning. Social Service Review. 2000;74(3):380–404. [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Jr., Lorenz FO, Simons RL, Whitbeck LB. A family process model of economic hardship and adjustment of early adolescent boys. Child Development. 1992;63(3):526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x. [DOI] [PubMed] [Google Scholar]
- Congressional Budget Office . The state children's health insurance program. Author; Washington, DC: 2007. [Google Scholar]
- Culica D, Rohrer J, Ward M, Hilsenrath P, Pomrehn P. Medical checkups: Who does not get them? American Journal of Public Health. 2002;92(1):88–91. doi: 10.2105/ajph.92.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham P. The growing financial burden of health care: National and state trends, 2001-2006. Health Affairs. 2010;29(5):1037–1038. doi: 10.1377/hlthaff.2009.0493. [DOI] [PubMed] [Google Scholar]
- Davidoff AJ, Yemane A, Hill I. Public Insurance eligibility and enrollment for special health care needs children. Health Care Financing Review. 2004;26(1):119–135. [PMC free article] [PubMed] [Google Scholar]
- Department of Health and Human Services Washington DC. [Retrieved March 15, 2010]; (Guides - Non-Classroom No. ED443795).Healthy People 2010: Conference Edition, Volumes I & II. 1998 :1196. from http://www.health.gov/healthypeople/
- Diehr P, Yanez D, Ash A, Hornbrook M, Lin DY. Methods for analyzing health care utilization and costs. Annual Review of Public Health. 1999;20(1):125–144. doi: 10.1146/annurev.publhealth.20.1.125. [DOI] [PubMed] [Google Scholar]
- Doty MM, Collins SR, Rustgi SD, Kriss JL. Seeing red: The growing burden of medical bills and debt faced by U.S. families. Commonwealth Fund; 2008. pp. 1–12. [PubMed] [Google Scholar]
- Fiscella K, Franks P, Gold M, Clancy C. Inequality in quality: Addressing socioeconomic, racial, and ethnic disparities in health care. Journal of the American Medical Association. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- Fisher L, Weihs KL. Can addressing family relationships improve outcomes in chronic disease? Report of the National Working Group on Family-Based Interventions in Chronic Disease. Journal of Family Practice. 2000;49(6):561–566. [PubMed] [Google Scholar]
- Fitch C, Jenkins R, Hurlston M, Hamilton S, Davey R, Walker F. Debt and mental health: An overview of selected evidence, key challenges, and available tools. Mental Health Today, (September) 2009:26–31. [PubMed] [Google Scholar]
- Francoeur RB. Use of an income-equivalence scale to understand age-related changes in financial strain. Research on Aging. 2002;24(4):445–472. doi: 10.1177/01627502024004003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. Journal of Financial and Quantitative Analysis. 1989;24:333–355. [Google Scholar]
- Galbraith AA, Wong ST, Kim SE, Newacheck PW. Out-of-pocket financial burden for low-income families with children: Socioeconomic disparities and effects of insurance. Health Services Research. 2005;40(6):1722–1736. doi: 10.1111/j.1475-6773.2004.00421.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon M, Rosenman L, Cuskelly M. Constrained labour: Maternal employment when children have disabilities. Journal of Applied Research in Intellectual Disabilities. 2007;20(3):236–246. [Google Scholar]
- Guendelman S, Wier M, Angulo V, Oman D. The effects of child-only insurance coverage and family coverage on health care access and use: Recent findings among low-income children in California. Health Services Research. 2006;41(1):125–147. doi: 10.1111/j.1475-6773.2005.00460.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutman LM, Eccles JS. Financial strain, parenting behaviors, and adolescents' achievement: Testing model equivalence between African American and European American single- and two-parent families. Child Development. 1999;70(6):1464–1476. doi: 10.1111/1467-8624.00106. [DOI] [PubMed] [Google Scholar]
- Hagenaars A, De Vos K, Zaidi M. Poverty statistics in the late 1980s: Research based on micro-data. Office for Official Publications of the European Communities; Luxembourg, Germany: 1994. [Google Scholar]
- Hanson KL. Patterns of insurance coverage within families with children. Health Affairs. 2001;20(1):240–246. doi: 10.1377/hlthaff.20.1.240. [DOI] [PubMed] [Google Scholar]
- Hebbeler K, Spiker D, Wagner M, Cameto R, McKenna P, SRI International Menlo Park CA. [Retrieved February 19, 2010]; (Reports - Research No. ED471879).State-to-State Variations in Early Intervention Systems. National Early Intervention Longitudinal Study (NEILS) 1999 :1–23. from: http://www.sri.com/neils/reports.htmlH159E50001.
- House JS. Occupational stress and coronary heart disease: A review and theoretical integration. Journal of Health and Social Behavior. 1974;15(1):12–27. [PubMed] [Google Scholar]
- Houtrow AJ, Kim SE, Newacheck PW. Health care utilization, access, and expenditures for infants and young children with special health care needs. Infants and Young Children. 2008;21(2):149–159. [Google Scholar]
- Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Affairs. 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- Jackson AP, Brooks-Gunn J, Huang CC, Glassman M. Single mothers in low-wage jobs: Financial strain, parenting, and preschoolers' outcomes. Child Development. 2000;71(5):1409–1423. doi: 10.1111/1467-8624.00236. [DOI] [PubMed] [Google Scholar]
- Jenkins R, Bhugra D, Bebbington P, Brugha T, Farrell M, Coid J, et al. Debt, income and mental disorder in the general population. Psychological Medicine. 2008;38(10):1485–1493. doi: 10.1017/S0033291707002516. [DOI] [PubMed] [Google Scholar]
- Katz SJ, Kessler RC, Frank RG, Leaf P, Lin E, Edlund M. The use of outpatient mental health services in the United States and Ontario: The impact of mental morbidity and perceived need for care. American Journal of Public Health. 1997;87(7):1136–1143. doi: 10.2105/ajph.87.7.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohen DE, Brehaut JC, Garner RE, Miller AR, Lach LM, Klassen AF, et al. Conceptualizing childhood health problems using survey data: A comparison of key indicators. BMC Pediatrics. 2007;7:40–53. doi: 10.1186/1471-2431-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Blasey CM. Centering in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2004;13(3):141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlthau K, Ferris TG, Beal AC, Gortmaker SL, Perrin JM. Who cares for medicaid-enrolled children with chronic conditions? Pediatrics. 2001;108(4):906–912. doi: 10.1542/peds.108.4.906. [DOI] [PubMed] [Google Scholar]
- Kuhlthau K, Hill KS, Yucel R, Perrin JM. Financial burden for families of children with special health care needs. Maternal and Child Health Journal. 2005;9(2):207–218. doi: 10.1007/s10995-005-4870-x. [DOI] [PubMed] [Google Scholar]
- Kuhlthau K, Kahn R, Hill KS, Gnanasekaran S, Ettner SL. The well-being of parental caregivers of children with activity limitations. Maternal and Child Health Journal. 2008;14(2):155–163. doi: 10.1007/s10995-008-0434-1. [DOI] [PubMed] [Google Scholar]
- Kuhlthau KA, Perrin JM. Child health status and parental employment. Archives of Pediatrics and Adolescent Medicine. 2001;155(12):1346–1350. doi: 10.1001/archpedi.155.12.1346. [DOI] [PubMed] [Google Scholar]
- Leiter V, Krauss MW, Anderson B, Wells N. The consequences of caring: Effects of mothering a child with special needs. Journal of Family Issues. 2004;25(3):379–403. [Google Scholar]
- Lukemeyer A, Meyers MK, Smeeding T. Expensive children in poor families: Out of pocket expenditures for the care of disabled and chronically ill children in welfare families. Journal of Marriage and Family. 2000;62(2):399–415. [Google Scholar]
- Major DA. Utilizing role theory to help employed parents cope with children's chronic illness. Health Education Research. 2003;18(1):45–57. doi: 10.1093/her/18.1.45. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53(2):185–204. doi: 10.1037//0003-066x.53.2.185. [DOI] [PubMed] [Google Scholar]
- Moos RH. Coping with Physical Illness. Plenum; New York, NY: 1977. [Google Scholar]
- National Center for Health Statistics . Health, United States, 2006. With chartbook on trends in the health of Americans. Author; Hyattsville, MD: 2006. [PubMed] [Google Scholar]
- Newacheck PW. A national profile of health care utilization and expenditures for children with special health care needs. Archives of Pediatrics and Adolescent Medicine. 2005;159:10–17. doi: 10.1001/archpedi.159.1.10. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114(1):79–85. doi: 10.1542/peds.114.1.79. [DOI] [PubMed] [Google Scholar]
- Newacheck PW, Strickland B, Shonkoff JP, Perrin JM, McPherson M, McManus M, et al. An epidemiologic profile of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):117–123. doi: 10.1542/peds.102.1.117. [DOI] [PubMed] [Google Scholar]
- Olfson M, Marcus SC, Druss B, Alan Pincus H, Weissman MM. Parental depression, child mental health problems, and health care utilization. Medical Care. 2003;41(6):716–721. doi: 10.1097/01.MLR.0000064642.41278.48. [DOI] [PubMed] [Google Scholar]
- Parish S, Seltzer M, Greenberg J, Floyd F. Economic implications of caregiving at midlife: Comparing parents with and without children who have developmental disabilities. Mental Retardation. 2004;42(6):413–426. doi: 10.1352/0047-6765(2004)42<413:EIOCAM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Parish SL, Shattuck PT, Rose RA. Financial burden of raising CSHCN: association with state policy choices. Pediatrics. 2009;124(Supplement 4):S435–442. doi: 10.1542/peds.2009-1255P. [DOI] [PubMed] [Google Scholar]
- Patterson J, Garwick A. Levels of family meanings in family stress theory. Family Process. 1994;33:287–304. doi: 10.1111/j.1545-5300.1994.00287.x. [DOI] [PubMed] [Google Scholar]
- Patterson JM. A family stress model: The family adjustment and adaptation response. In: Ramsey CN Jr., editor. Family systems in medicine. Guilford Press; New York, NY: 1989. pp. 95–118. [Google Scholar]
- Perrin J, Bloom S, Gortmaker S. The Increase of childhood chronic conditions in the United States. Journal of the American Medical Association. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- Pless I, Perrin J. Issues common to a variety of illnesses. In: Hobbs N, Perrin J, editors. Issues in the care of children with chronic illness: A sourcebook on problems, services, and policies. Jossey-Bass; San Francisco, CA: 1985. pp. 41–60. [Google Scholar]
- Pless IB, Pinkerton P. Chronic childhood disorder: Promoting patterns of adjustment. H. Kimpton; London, UK: 1975. [Google Scholar]
- Pollack CE, Lynch J. Health status of people undergoing foreclosure in the Philadelphia region. American Journal of Public Health. 2009;99(10):1833–1839. doi: 10.2105/AJPH.2009.161380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raina P, O'Donnell M, Rosenbaum P, Brehaut J, Walter SD, Russell D, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115(6):E626–E636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- Reading R, Reynolds S. Debt, social disadvantage and maternal depression. Social Science and Medicine. 2001;53(4):441–453. doi: 10.1016/s0277-9536(00)00347-6. [DOI] [PubMed] [Google Scholar]
- Rimsza ME, Butler RJ, Johnson WG. Impact of medicaid disenrollment on health care use and cost. Pediatrics. 2007;119(5):1026–1032. doi: 10.1542/peds.2006-2747. [DOI] [PubMed] [Google Scholar]
- Seifert RW, Rukavina M. Bankruptcy is the tip of a medical-debt iceberg. Health Affairs. 2006;25(2):w89–92. doi: 10.1377/hlthaff.25.w89. [DOI] [PubMed] [Google Scholar]
- Sen E, Yurtsever S. Difficulties experienced by families with disabled children. Journal for Specialists in Pediatric Nursing. 2007;12(4):238–252. doi: 10.1111/j.1744-6155.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- Shalowitz MU, Berry CA, Quinn KA, Wolf RL. The relationship of life stressors and maternal depression to pediatric asthma morbidity in a subspecialty practice. Ambulatory Pediatrics. 2001;1(4):185–193. doi: 10.1367/1539-4409(2001)001<0185:trolsa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Sharpe DL, Baker DL. Financial issues associated with having a child with autism. Journal of Family and Economic Issues. 2007;28(2):247–264. [Google Scholar]
- Shattuck PT, Parish SL. Financial burden in families of children with special health care needs: Variability among states. Pediatrics. 2008;122(1):13–18. doi: 10.1542/peds.2006-3308. [DOI] [PubMed] [Google Scholar]
- Silver EJ, Bauman LJ, Weiss ES. Perceived role restriction and depressive symptoms in mothers of children with chronic health conditions. Journal of Developmental and Behavioral Pediatrics. 1999;20(5):362–369. doi: 10.1097/00004703-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Silver EJ, Westbrook LE, Stein REK. Relationship of parental psychological distress to consequences of chronic health conditions in children. Journal of Pediatric Psychology. 1998;23(1):5–15. doi: 10.1093/jpepsy/23.1.5. [DOI] [PubMed] [Google Scholar]
- Singh B, Golden R. The uninsured patient. American Journal of Medicine. 2006;119:166.e1–5. doi: 10.1016/j.amjmed.2005.08.024. [DOI] [PubMed] [Google Scholar]
- Stein RE, Bauman LJ, Westbrook LE, Coupey SM, Ireys HT. Framework for identifying children who have chronic conditions: The case for a new definition. Journal of Pediatrics. 1993;122(3):342–347. doi: 10.1016/s0022-3476(05)83414-6. [DOI] [PubMed] [Google Scholar]
- Thyen U, Terres NM, Yazdgerdi SR, Perrin JM. Impact of long-term care of children assisted by technology on maternal health. Journal of Developmental and Behavioral Pediatrics. 1998;19(4):273–282. doi: 10.1097/00004703-199808000-00006. [DOI] [PubMed] [Google Scholar]
- Van Cleave J, Gortmaker SL, Perrin JM. Dynamics of obesity and chronic health conditions among children and youth. Journal of the American Medical Association. 2010;303(7):623–630. doi: 10.1001/jama.2010.104. [DOI] [PubMed] [Google Scholar]
- Vimo . The uninsured in America. Vimo Research Group; Mountain View, CA: 2007. [Google Scholar]
- Waddington SR, Busch-Rossnagel NA. The influence of a child's disability on mother's role functioning and psychological well-being. Genetic, Social, and General Psychology Monographs. 1992;118(3):293–311. [PubMed] [Google Scholar]
- Wallander JL, Varni JW. Adjustment in children with chronic physical disorders: Programmatic research on a disability-stress-coping model. In: La Greca AM, Siegel LJ, editors. Stress and coping in child health. Advances in pediatric psychology. The Guilford Press; New York, NY: 1992. pp. 279–298. [Google Scholar]
- Wells T, Hogan D. Developing concise measures of childhood activity limitations. Maternal and Child Health Journal. 2003;7(2):115–126. doi: 10.1023/a:1023868911115. [DOI] [PubMed] [Google Scholar]
- Wielawski I. Gouging the medically uninsured: A tale of two bills. Health Affairs. 2000;19(5):180–185. doi: 10.1377/hlthaff.19.5.180. [DOI] [PubMed] [Google Scholar]
- Williams FL, Hagler A, Martin MA, Pritchard M, Bailey WC. Predictors of out-of-pocket medical expenditures in low-income households. Journal of Family and Economic Issues. 1991;12(1):43–62. [Google Scholar]
- Witt WP, DeLeire T. A family perspective on population health: The case of child health and the family. Wisconsin Medical Journal. 2009;108(5):240–245. [PMC free article] [PubMed] [Google Scholar]
- Witt WP, Riley AW, Coiro MJ. Childhood functional status, family stressors, and psychosocial adjustment among school-aged children with disabilities in the United States. Archives of Pediatric & Adolescent Medicine. 2003;157(7):687–695. doi: 10.1001/archpedi.157.7.687. [DOI] [PubMed] [Google Scholar]
- Wolfe B, Kaplan T, Haveman R, Cho Y. SCHIP expansion and parental coverage: An evaluation of Wisconsin's BadgerCare. Journal of Health Economics. 2006;25(6):1170–1192. doi: 10.1016/j.jhealeco.2005.12.005. [DOI] [PubMed] [Google Scholar]
- Yu H, Dick AW, Szilagyi PG. Does public insurance provide better financial protection against rising health care costs for families of children with special health care needs? Medical Care. 2008;46(10):1064–1070. doi: 10.1097/MLR.0b013e318185cdf2. [DOI] [PubMed] [Google Scholar]