Abstract
Most pancreatic cancer patients present with inoperable disease or develop metastases after surgery. Conventional therapies are usually ineffective in treating metastatic disease. It is evident that novel therapies remain to be developed. Transforming growth factor β (TGF-β) plays a key role in cancer metastasis, signaling through the TGF-β type I/II receptors (TβRI/II). We hypothesized that targeting TβRI/II kinase activity with the novel inhibitor LY2109761 would suppress pancreatic cancer metastatic processes. The effect of LY2109761 has been evaluated on soft agar growth, migration, invasion using a fibroblast coculture model, and detachment-induced apoptosis (anoikis) by Annexin V flow cytometric analysis. The efficacy of LY2109761 on tumor growth, survival, and reduction of spontaneous metastasis have been evaluated in an orthotopic murine model of metastatic pancreatic cancer expressing both luciferase and green fluorescence proteins (L3.6pl/GLT). To determine whether pancreatic cancer cells or the cells in the liver microenvironment were involved in LY2109761-mediated reduction of liver metastasis, we used a model of experimental liver metastasis. LY2109761 significantly inhibited the L3.6pl/GLT soft agar growth, suppressed both basal and TGF-β1–induced cell migration and invasion, and induced anoikis. In vivo, LY2109761, in combination with gemcitabine, significantly reduced the tumor burden, prolonged survival, and reduced spontaneous abdominal metastases. Results from the experimental liver metastasis models indicate an important role for targeting TβRI/II kinase activity on tumor and liver microenvironment cells in suppressing liver metastasis. Targeting TβRI/II kinase activity on pancreatic cancer cells or the cells of the liver microenvironment represents a novel therapeutic approach to prevent pancreatic cancer metastasis.
Introduction
Pancreatic adenocarcinoma is the fourth leading cause of cancer mortality among adults in the United States. For all stages combined, the 5-year survival rate is 5% and the median survival duration after diagnosis is <6 months (1). At the time of diagnosis, two thirds of patients present with locally advanced or metastatic disease. Even when pancreatic cancer is apparently localized to the pancreas and surgically removed, 70% of patients will develop liver metastases (2). Hence, pancreatic cancer poses one of the greatest challenges in cancer research.
Transforming growth factor β (TGF-β) is a family of dimeric polypeptide growth factors that initiate cell signaling by dimerizing the TGF-β type I (TβRI) and type II (TβRII) serine/threonine kinase receptors. This dimerization allows for the constitutively active TβRII kinase to transphosphorylate and activate the TβRI kinase which, in turn, propagates the signal by activating downstream Smad-dependent and Smad-independent pathways (3, 4). The tumor suppressor function of TGF-β signaling is well established. However, TGF-β signaling also plays a key role in the tumor progression and metastasis of many different types of tumor cells, which suggests that TGF-β signaling actually has tumor-promoting effects in advanced disease (5). Some of TGF-β oncogenic activities are linked to its induction of a phenotypic switch known as the epithelial-to-mesenchymal transition, in which cell adhesions are disrupted, the surrounding matrix is degradated, and the tumor cells become more motile and invasive, thereby increasing their metastatic potential (6).
The overexpression of TGF-β ligands has been reported in most tumor types, and elevated levels of these ligands in tumor tissues or in patient serum correlate with more metastatic phenotypes or poorer patient outcome (7). In particular, human pancreatic cancer demonstrating increased levels of TGF-β has been found to be significantly associated with venous invasion, advanced tumor stages, progressive disease, shorter patient survival duration, and liver metastases (8–11). Using a bitransgenic mammary cancer mouse model that expressed the mouse mammary tumor virus promoter-directed Neu oncogene and either the constitutively activated or the dominant-negative form of the TGF-β receptors, Siegel et al. (12) showed that, in mice expressing activated forms of the Neu receptor tyrosine kinase, the activated TβRI increased the latency of mammary tumor formation but also enhanced the frequency of lung metastasis. Conversely, expression of the dominant-negative TβRII decreased the latency of Neu-induced mammary tumor formation while significantly reducing the incidence of extravascular lung metastases. Tian et al. (13) showed that reduced TGF-β receptor function enhanced the tumorigenesis of well-differentiated breast carcinoma cell lines but substantially reduced the formation of lung metastatic lesions in a metastatic breast cell line of common origin.
The effect of TGF-β is not limited to the tumor cells themselves in vivo. A recent study highlighted its paracrine mechanism in the interactions between various cell populations in the tumor microenvironment (14). In particular, TGF-β mediates the transdifferentiation of fibroblasts into myofibroblasts, a cell type that may be responsible for the desmoplastic reaction that surrounds a human pancreatic carcinoma and is able to promote tumorigenesis by secreting growth factors and increasing the metastatic potential of carcinoma cells (14, 15). Moreover, the secretion of TGF-β by pancreatic tumors hampers an effective antitumor immune response by affecting the phenotype and function of dendritic cells in the tumor microenvironment (16).
A series of small molecule inhibitors of TβRI kinase activity have been developed and evaluated in in vivo models of breast cancer (17–20). To investigate whether targeting of TβR activity is an effective therapeutic approach to suppress pancreatic cancer metastasis, we determined the effect of the novel TβRI/II kinase selective inhibitor LY2109761 on the growth, motility, and invasiveness of pancreatic cancer cells in vitro and the metastasis development in vivo by using an orthotopic xenograft model and an experimental model of liver metastasis.
Materials and Methods
Cell Lines, Culture Methods, and Reagents
Human pancreatic cancer cell lines Colo357FG and Colo357L3.6pl were previously described (21). Human pancreatic cancer cell lines C5, C5LM1, and C5LM2 were established as described in Supplementary data.5 The cells were maintained as monolayer cultures in DMEM (Life Technologies) that contained 4.5 g/L glucose, glutamine, and nonessential amino acids and were supplemented with 10% heat-inactivated fetal bovine serum and penicillin (100 IU/mL)–streptomycin (100 μg/mL) in an atmosphere of 5% carbon dioxide and 95% air at 37°C. The immortalized human fibroblasts 041-H were obtained from Dr. Tainsky (Barbara Ann Karmanos Cancer Institute/Wayne State University), and the cells were maintained as previously described in ref. 22.
LY2109761 is an orally active TβRI/II kinase dual inhibitor (I, Ki = 38 nmol/L; II, Ki = 300 nmol/L in vitro kinase assay) generously provided by Eli Lilly Pharmaceuticals. A series of enzymatic and cellular assays was used to characterize the ability of LY2109761 to inhibit TGF-β signaling in vitro. A panel of other ~80 kinases was screened in duplicate at 10 μmol/L with >50% activity against only the following human kinases (% inhibition at 10 μmol/L): Sapk2a (89%), MKK6 (80%), Lck (69%), Yes (64%), Fyn (58%), SapK2b (47%). Initial in vivo time course and dose-response experiments have been conducted in a Calu6 murine model. The pharmacokinetic and pharmacodynamic profiles of LY2109761 indicates that dose of 100 mg/kg/d in a twice daily schedule is necessary to optimally inhibit the target.6 For in vitro assays, LY2109761 was dissolved in 100% DMSO at a stock concentration of 10 mmol/L. The concentration of DMSO did not exceed 0.1% in any assay. For in vivo studies, LY2109761 was dissolved in the SX-1292 oral vehicle (1% sodium carboxymethylcellulose, 0.5% sodium lauryl sulfate, and 0.05% antifoam; Eli Lilly) and given p.o. Gemcitabine (Gemzar, Eli Lilly) was supplied as a lyophilized product, which was then dissolved in sterile saline. TGF-β1 and TGF-β1 ELISA kit were obtained from R&D Systems. The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (Sigma-Aldrich) assay was used to obtain relative variable cell numbers.
For topics on Establishment of Firefly Luciferase–Expressing and Green Fluorescence Protein–Expressing Clone, Soft Agar Colony Formation Assay and Analysis of Combination Index, Western Blot Analysis, and Nude Mouse Orthotopic Xenograft Model, see Supplementary data.5
Cell Invasion Assay
The invasive potential of pancreatic cancer cells was determined using a model based on coculture with fibroblasts (23). See Supplementary data5 for more details.
Treatment of Established Human Pancreatic Carcinoma Tumors Growing in the Pancreas of Athymic Nude Mice
Three days after the orthotopic implantation of 1.0 × 106 L3.6pl/GLT tumor cells in 50 μL of HBSS, when bioluminescence imaging confirmed that tumors were well established, 40 mice were randomly allocated into four groups (n = 10 mice per group) to receive one of the following treatments. (a) Vehicle solution for 50 μL of LY2109761 twice a day p.o. (days 1–5 of each week) and 50 μL of sterile saline daily i.p. (days 2 and 5 of each week; control group). (b) LY2109761 (50 mg/kg) twice a day p.o. (days 1–5 of each week) and 50 μL of sterile saline daily i.p. (days 2 and 5 of each week). (c) Gemcitabine (25 mg/kg) daily i.p. (days 2 and 5 of each week) and p.o. vehicle for 50μL of LY2109761 twice a day (days 1–5 of each week). (d) LY2109761 (50 mg/kg) twice a day (days 1–5 of each week) and gemcitabine (25 mg/kg) daily i.p. (days 2 and 5 of each week). Treatments were continued for 4 wk.
All mice were weighed weekly and observed for tumor growth. Tumor diameter was assessed with a Vernier caliper, and tumor volume (mm3) was calculated as d2 × D/2, wherein d and D represent the shortest and longest diameters, respectively. Bulky disease was considered present when tumor burden was prominent in the mouse abdomen (tumor volume, ≥2,000 mm3).
When at least 6 of 10 mice in a treatment group presented with bulky disease, the median survival duration for that group was considered to be reached. At the median survival duration of the control group, the tumor growth in mice in all groups was evaluated using the bioluminescence emitted by the tumor cells. Bioluminescence imaging was conducted using a cryogenically cooled IVIS 100 imaging system coupled to a data acquisition computer running Living Image software (Xenogen). The mice were sacrificed by carbon dioxide inhalation when evidence of advanced bulky disease was present. The day of sacrifice was considered the day of death for survival evaluation.
Spontaneous In vivo Metastasis Assay
Three days after the orthotopic implantation of L3.6pl/GLT tumor cells, another group of 40 mice was randomly allocated into two groups (n = 20 mice per group) to receive p.o. vehicle for 50 μL of LY2109761 or 50 mg/kg LY2109761 twice a day p.o. (days 1–5 of each week). Treatments were continued for 4 wk. All mice in a group were sacrificed by carbon dioxide inhalation 1 d after at least 11 of the mice in a treatment group presented with bulky disease. At necropsy, the presence of ascites and fluorescent tumor lesions in the pancreas, spleen, lymph nodes (celiac and paraaortic), liver, diaphragm, and other peritoneal organs was confirmed with a Leica MZ16 stereoscopic dissecting fluorescence microscope equipped with a Hamamatsu Orca ER cooled CCD digital camera coupled to a data acquisition computer running the image acquisition software Image-Pro version 6.0.
Experimental In vivo Liver Metastasis Assay
Fifty mice were randomly allocated into five groups (n = 5 mice per group) to receive p.o. vehicle for 50 μL of LY2109761 or 50 mg/kg LY2109761 twice a day p.o. On day 0, mice were anesthetized with 1.5% isofluorane-air mixture, a small left abdominal flank incision was created, and the spleen was carefully exteriorized. L3.6pl/GLT or C5LM2/GLT cells (1.0 × 106 cells/50 μL of HBSS), cultured in the presence of LY2109761 (5 μmol/L) or DMSO from day −5 to day 0, were inoculated into the spleen with a 30-gauge needle. A visible paling of the spleen was the criterion for successful inoculation. After 10 min, the spleen was removed using a high-temperature cautery (Aaron) to avoid the possibility that the ectopic growth of pancreatic tumor cells in the spleen could be a confounding source of hematogenous liver metastatic cells. The abdominal wall was closed in one layer with wound clips. Treatment with 50 mg/kg LY2109761 twice a day p.o. (days 1–5 of each week after inoculation) was continued for one group of untreated mice inoculated with untreated cells.
At days 28 and 91, for mice inoculated with L3.6pl/GLT or C5LM2/GLT cells, respectively, when the median survival duration for the mice in the control group (preinoculation treatment with p.o. vehicle, inoculation with DMSO-cultured cells, and no postinoculation treatment) was reached, the volume of the tumor growing in the liver was evaluated based on the bioluminescence emitted by the tumor cells within the hepatic region using a IVIS 100 imaging system, as we have described. At necropsy, the presence of fluorescent tumor lesions in the liver, diaphragm, and other abdominal organs was confirmed with a Leica MZ16 stereoscopic dissecting fluorescence microscope equipped with a Hamamatsu Orca ER cooled CCD digital camera and a CoolSNAP-Pro cf. 36-bit color digital camera (Media Cybernetics) coupled to a data acquisition computer running the Image-Pro version 6.0 software.
Statistical Analysis
The results of in vitro proliferation and colony formation are expressed as means (95% confidence intervals) for at least three independent experiments done in triplicate, and their statistical significance was determined by two-way ANOVA. The statistical significance of differences in migration and invasion was determined using a two-tailed unpaired Student’s t test. The results of the anoikis assays are expressed as means (95% confidence intervals) for three independent experiments, and the statistical significance of differences in anoikis induction was determined using a two-tailed unpaired Student’s t test. The statistical significance of differences in tumor and experimental liver metastases growth was determined by one-way ANOVA and Dunnett’s multiple comparison posttest, that of differences in survival by a log-rank test, and that of differences in spontaneous metastases by Fisher exact test. All statistical tests were two-sided, and a P value of <0.05 will be used to indicate statistical significance. All of the statistical analyses were done using GraphPad Prism version 4.0c for Macintosh (GraphPad Software).
Results
Targeting TβRI/II Kinase Activity Does Not Influence the In vitro Monolayer Proliferation Rate but Does Inhibit Low-AnchorageTumor Cell Colony Formation
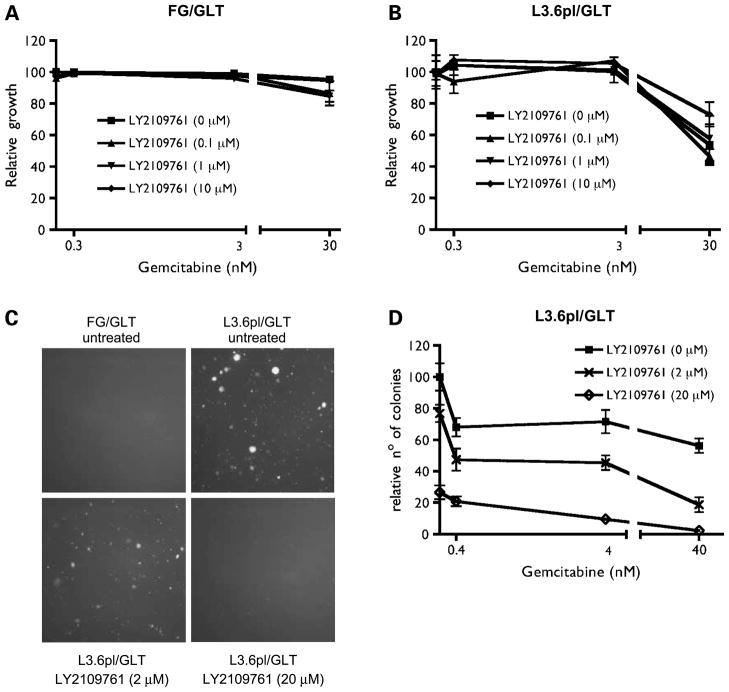
To study the in vitro antiproliferative effects of targeting TβRI/II kinase activity, we determined the expression of TβRI and TβRII on FG/GLT and L3.6pl/GLT, as well as on C5/GLT, C5LM1/GLT, and C5LM2/GLT (Supplementary Fig. S1),5 and we evaluated the growth rate of FG/GLT and L3.6pl/GLT cells treated with escalating doses of LY2109761, alone and with increasing doses of gemcitabine. Whereas gemcitabine had antiproliferative activity (P < 0.0001), particularly in L3.6pl/GLT cells, LY2109761 had no significant antiproliferative effect on either FG/GLT and L3.6pl/GLT cells grown as a monolayer in cell culture dishes (Fig. 1A and B).
Figure 1.
Effect of LY2109761 alone and with gemcitabine on pancreatic cancer cell proliferation and low-anchorage colony formation in vitro. On day 0, FG/GLT nonmetastatic pancreatic carcinoma cells (A) and their highly metastatic subclone L3.6pl/GLT pancreatic carcinoma cells (B) were seeded at a density of 1.0 × 103 per well. On the following day, the cells were treated with increasing doses of LY2109761 (0.1, 1, and 10 μmol/L), gemcitabine (0.3, 3, and 30 nmol/L), and their combinations. On day 2, the medium containing drugs was removed, the cells were washed twice with PBS, and fresh medium was added. After 5 d of incubation, the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide assay was used to obtain relative variable cell numbers. DMSO-treated cells were assigned a value of 100%. Means and 95% confidence intervals of three independent experiments performed in triplicate. C and D, on day 0, FG/GLT and L3.6pl/GLT cells (1.0 × 104 per well) were suspended in 0.6% soft agar. On day 1, L3.6pl/GLT cells were treated with increasing doses of LY2109761 (2 and 20 μmol/L), gemcitabine (0.4, 4, and 40 nmol/L), or both. After 14 d, photographs of fluorescent colonies were taken. L3.6pl/GLT colonies larger than 0.05 mm were automatically counted. The number of colonies that formed from untreated cells was set at 100. Means and 95% confidence intervals of three independent experiments performed in triplicate.
Because low-anchorage growth is a more common characteristic of metastatic cancer cells, we evaluated the ability of FG/GLT and L3.6pl/GLT cells to form colonies in soft agar in the presence or absence of LY2109761. The untreated nonmetastatic FG/GLT cells were not able to form colonies, whereas the untreated metastatic L3.6pl/GLT cells formed numerous colonies (Fig. 1C), thereby demonstrating the latter’s increased potential to survive and grow in low-anchorage conditions. When we treated L3.6pl/GLT soft agar colonies with LY2109761, we observed a significant dose-dependent inhibition of growth (P < 0.0001; Fig. 1C and D), which resulted in ~33% inhibition at 2 μmol/L LY2109761 and 73% inhibition at 20 μmol/L LY2109761. Growth inhibition was enhanced when LY2109761 was combined with increasing doses of gemcitabine (Fig. 1D).
To better evaluate the cooperative effects between LY2109761 and gemcitabine, we did a combination analysis at their equipotent ratio and generated the combination index value. According to this method, combination index values of <1, 1, and >1 indicate synergy, additivity, and antagonism, respectively. The combination index value of 0.36581 showed strong synergistic effects between LY2109761 and gemcitabine on the soft agar growth of L3.6pl/GLT cells.
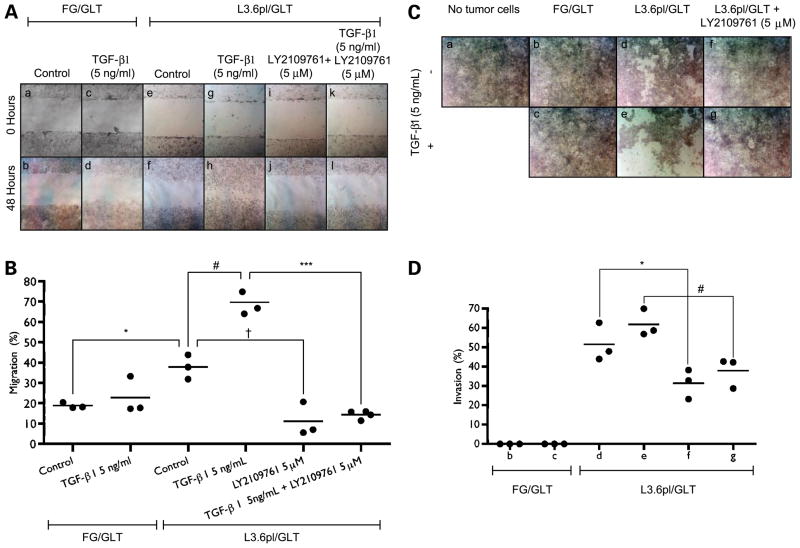
LY2109761 Suppresses In vitro Basal and TGF-β–Stimulated Migration and Invasion of L3.6pl/GLT Cells
To study the role of TGF-β in tumor cell migration, an initial key step in the development of metastasis, we examined its ability to stimulate FG/GLT and L3.6pl/GLT cell migration in a wound-closure assay. Whereas the nonmetastatic FG/GLT cells at 48 h were unable to migrate even if they were stimulated by TGF-β1(P = 0.4955; Fig. 2A, b versus d, and B), their metastatic variant, L3.6pl/GLT cells, had a significantly higher basal migration rate (P = 0.0058) that covered 38% of the distance between the wound edges (Fig. 2A, b versus f, and B). L3.6pl/GLT cell motility was enhanced after stimulation with TGF-β1, increasing up to 70% wound coverage (P = 0.0030; Fig. 2A, f versus h, and B). Targeting TβRI/II kinase activity with LY2109761 (5 μmol/L) almost completely suppressed both the basal (P = 0.0107; Fig. 2A, f versus j, and B) and TGF-β1–stimulated migration of L3.6pl/GLT cells (P < 0.0001; Fig. 2A, h versus l, and B), indicating that the migration of L3.6pl/GLT cells in vitro is effectively driven by endogenous TGF-β.
Figure 2.
Effect of LY2109761 on pancreatic cancer cell basal and TGF-β1–stimulated migration and invasiveness. A, FG/GLT and L3.6pl/GLT cell monolayers were incised with a pipette tip in the central area of the culture. TGF-β1 and LY2109761 were added as indicated. Photographs were taken using phase-contrast microscopy immediately after the incision and after 48 h of treatment. B, results are presented as the percentage of the total distance of the original wound enclosed by cells. Horizontal bars, means of three independent experiments. *, P = 0.0058; #, P = 0.0030; †, P = 0.0107; ***, P < 0.0001 by two-tailed unpaired Student’s t tests. C, 041-H human fibroblasts were seeded up to build a dense cell monolayer. Cells were rinsed with PBS, permeabilized with DMSO, and washed twice with PBS. Subsequently, this layer of fibroblasts was overlaid with FG/GLT or L3.6pl/GLT tumor cells. After 1 h, during which the tumor cells were allowed to adhere to the fibroblast layer, TGF-β1 and LY2109761 were added as indicated. After 8 h, the cells were stained with 0.2% trypan blue/PBS rinsed with PBS and immediately photographed. Because trypan blue stained only the permeabilized fibroblast layer, the dead fibroblasts were easily distinguished from the living carcinoma cells. The areas of unstained cells represent regions where fibroblasts were digested by invasive tumor cells. D, to quantify invasiveness, the stained fibroblasts were lysed and their absorbance measured. Percentage invasion was calculated as [1 − (X/Y)] × 100, wherein X is the absorbance measured in the treated well and Y is the absorbance measured where tumor cells were not seeded. Horizontal bars, means of three independent experiments. *, P = 0.0493; #, P = 0.0176 by two-tailed unpaired Student’s t tests.
We examined the invasiveness of FG/GLT and L3.6pl/GLT cells and their response to TGF-β and LY2109761-mediated TβRI/II inhibition in a more physiologic, cell-based in vitro invasion assay than the commonly used assays with Matrigel. We studied the ability of the cells to invade and digest a monolayer of mesenchymal cells, as previously described for ovarian cancer cells (24). In this assay, FG/GLT cells were unable to invade the fibroblast monolayer, even with TGF-β1 stimulation (Fig. 2C, b and c, and D). In contrast, L3.6pl/GLT cells rapidly invaded the fibroblast monolayer, reaching at 8 hours a mean of 52% invasion when unstimulated and 62% invasion when stimulated with TGF-β1(Fig. 2C, d and e, and D). In this kind of assay, L3.6pl/GLT cells also showed a more aggressive invasive activity than that of several other pancreatic cancer cell lines (data not shown). The invasive ability of L3.6pl/GLT cells was significantly inhibited by treatment with LY2109761 (5 μmol/L), both in unstimulated (P = 0.0493) and TGF-β1–stimulated conditions (P = 0.0176; Fig. 2C, f and g, and D). Thus, their invasive phenotype also seems to be dependent on endogenous TGF-β signaling.
Targeting TβRI/II Kinase Activity Reduces L3.6pl Anoikis Resistance
Because TGF-β is causally involved in tumor cell resistance to anoikis and the reversal of its effect could interfere with tumor cells seeding into secondary sites (25), we determined whether L3.6pl cells have the ability to undergo anoikis and whether they can be sensitized by LY2109761 to trigger this suspension-induced apoptosis. In our experiment, L3.6pl cells strongly resisted anoikis: almost half of the cells still survived after 8 hours of growth in forced suspension (Fig. 3A and B). Targeting the TβRI/II pathway with LY2109761 (5 μmol/L) significantly enhanced the detachment-induced apoptosis, increasing it at 2 hours from 15% to 24% (P = 0.0004), 4 hours from 26% to 44% (P < 0.0001), and 8 hours from 47% to 73% (P = 0.0005; Fig. 3A).
Figure 3.
A, effect of LY2109761 on L3.6pl cell apoptosis induced by the complete loss of adhesion (anoikis). To mimic the condition of complete loss of adhesion present during metastatic hematogenous dissemination, L3.6pl cells (1.0 × 105 per well) pretreated for 24 h with LY2109761 (5 μmol/L) or with DMSO were trypsinized and incubated in suspension in Costar ultra-low attachment plates (Corning) for 2, 4, or 8 h (detached cells) still in the presence of LY2109761 or DMSO or were trypsinized and analyzed immediately (attached cells). The extent of apoptosis was determined by Annexin V and propidium iodide staining and flow cytometric analysis. Means and 95% confidence intervals of three independent experiments. *, P = 0.0004; #, P <0.0001;†, P =0.0005bytwo-tailedunpairedStudent’s t test.B,dotplotsofL3.6plcellsincubatedinsuspensionfor8hinthepresenceofLY2109761. LY2109761. C, effect of LY2109761 on the activation of Smad2-dependent and Smad2-independent intracellular pathways downstream of TGF-β1 types I and II serine/threonine kinase receptors. L3.6pl/GLT cells were cultured for 24 h in serum-free medium and washed in PBS, and the medium was changed to serum-free medium containing LY2109761 or DMSO (as control). After 24 h, 10% fetal bovine serum, 5 ng/mL TGF-β1, or both were added to the medium. Thirty minutes later, L3.6pl/GLT cells were lysed and the whole-cell lysates were subjected to Western blot analysis for examination of the expression of actin, and total and phosphorylated Smad2, extracellular signal-regulated kinase 1/2 (ERK1/2), and c-Jun-NH2-kinase (JNK). Phosphorylated Smad2/Smad2 band density ratios were calculated using the ImageQuant software.
LY2109761 Activity Is Mediated by Suppression of Smad2 Phosphorylation
Because Smad proteins are central mediators of signals from TGF-β receptors, we evaluated the effect of targeting TβRI/II kinase activity on the phosphorylation of Smad2, one of their immediate downstream targets. Confirming the hyperactivation of their TGF-β signaling, L3.6pl/GLT cells showed a constitutive phosphorylated Smad2 because of their active secretion of TGF-β1 (513.31 pg/mL/24 h/1.0 × 106 cells), and the supplement of fetal bovine serum and/or exogenous TGF-β1 for 30 minutes induced a modest but measurable enhancement of the phosphorylation of Smad2. Treatment with LY2109761 (5 μmol/L) completely suppressed TGF-β–induced Smad2 phosphorylation, but the same treatment had only a minimal effect on extracellular signal-regulated kinase 1/2 phosphorylation and no effect at all on the c-Jun-NH2-kinase pathway (Fig. 3C). These results suggest that the Smad-dependent downstream pathway is preferentially inhibited by LY2109761.
LY2109761 Inhibits L3.6pl/GLT Pancreatic Tumor Growth and Spontaneous Metastasis in In vivo Orthotopic Xenografts
To determine the therapeutic potential of LY2109761 and test our in vitro findings in an in vivo setting, we used an orthotopic nude mouse model. Forty mice were orthotopically injected with L3.6pl/GLT metastatic pancreatic cancer cells and received p.o. LY210976 (50 mg/kg), subtherapeutic doses of i.p. gemcitabine, their combination, or the p.o. and i.p. vehicles as control. At the median survival duration of mice in the control group (31.5 days), gemcitabine treatment had a modest effect on tumor volume (Fig. 4A and B) and resulted in the same median survival duration as the control group did (Fig. 4C). LY2109761 greatly reduced the tumor volume and increased the median survival duration of the mice to 45.0 days, but the differences were not significant. Only when the two drugs were combined were significant effects noted on tumor volume (P < 0.05) and median survival duration, which was increased to 77.5 days (P = 0.0018). The activity of LY2109761 on targeting TβRI/II kinase activity was shown by the strong reduction of Smad2 phosphorylation on tumor specimen from treated mice (Fig. 4D). The treatments with LY2109761 and gemcitabine (alone or together) were well tolerated; no weight loss or other signs of acute or delayed toxicity were observed.
Figure 4.
Effect of LY2109761 alone and with gemcitabine (combination) on the tumor growth and survival of athymic mice bearing orthotopic L3.6pl/GLT pancreatic tumors. Forty mice bearing tumors were randomly allocated to be treated with LY2109761, gemcitabine, both, or their p.o. and i.p. vehicles (control), according to the schedule described in Materials and Methods. A, at the median survival duration of the control group (31.5 d), the tumor growth in the mice of all groups was evaluated based on the bioluminescence emitted by the tumor cells. A digital grayscale image of each mouse was acquired, which was followed by the acquisition and overlay of a pseudocolor image representing the spatial distribution of detected photons emerging from active luciferase within the mouse. B, tumor volume was quantified as the sum of all detected photons within the region of the tumor per second. Means and 95% confidence intervals. *, P < 0.05 combination versus control by one-way ANOVA and Dunnett’s multiple comparison posttest. C, mice were sacrificed by carbon dioxide inhalation when evidence of advanced bulky disease was present. The day of sacrifice was considered the day of death for survival evaluation. P = 0.0018 combination versus control, by log-rank test. D, effect of LY2109761 on targeting TGF-β1 types I and II serine/threonine kinase receptor activity on primary tumor. To obtain tumor specimens to study the protein expression, other six mice were randomly allocated into two groups (n = 3 mice per group) to be treated as per control group or group 2. The mice were sacrificed by carbon dioxide inhalation at the end of the 4 wk of treatments, the primary tumors were excised lysed, and the lysates were subjected to Western blot analysis for examination of the expression of total and phosphorylated Smad2. Representative of three independent experiments.
To determine the in vivo antimetastatic effect of targeting TβRI/II kinase activity independently of the effect on primary tumor growth, another group of 40 mice bearing orthotopic L3.6pl/GLT pancreatic tumors was randomly allocated to receive LY2109761 or its p.o. vehicle. The mice in each group were sacrificed at the median survival duration of the group (control, 32 days; treated, 49 days) to reduce the bias due to the effect of the treatment on the primary tumor. The mice in both groups showed a similar primary tumor volume, but the control mice had a diffuse pattern of abdominal metastasis at necropsy (Fig. 5A). The mice treated with LY2109761 developed significantly fewer metastatic lesions and, in some of them, no metastatic lesion, as indicated by the GFP signal, could be identified in the abdomen (Fig. 5B). Compared with control mice, significantly fewer LY2109761-treated mice developed liver (P = 0.0225), spleen (P = 0.0225), and intestinal mesentery (P = 0.0004) nodules and significantly fewer enlarged and positive abdominal lympho nodes (P = 0.0004); in addition, ascites formation was completely suppressed (P < 0.0001; Fig. 5C). Thus, our results indicate that, independently of any activity on the orthotopic primary, targeting TGF-β receptor kinase activity significantly reduces metastasis from pancreatic cancer cells.
Figure 5.
Antimetastatic effect of LY2109761 in an in vivo model of L3.6pl/GLT pancreatic cancer cell spontaneous metastasis. Forty mice bearing orthotopic L3.6pl/GLT pancreatic tumors were randomly allocated to receive the p.o. vehicle for LY2109761 (A) or LY2109761 (B) according to the schedule described in Materials and Methods. The mice in each group were sacrificed at the group’s respective median survival duration (control, 32 d; treated, 49 d) to reduce bias due to the effect of the treatment on the primary tumor. C, at necropsy, the presence of ascites and fluorescent tumor lesions in the spleen, intestinal mesentery, diaphragm, lymph nodes (celiac and paraaortic), liver, and other peritoneal organs was confirmed with a stereoscopic dissecting fluorescence microscope. *, P = 0.0225; **, P = 0.0004; ***, P < 0.0001 by Fisher exact test.
Targeting TβRI/II Kinase Activity on Tumor Cells or the Liver Microenvironment Inhibits Tumor Cells from Developing Secondary Lesions
To understand whether the antimetastatic effect of LY2109761, which was verified in the orthotopic mouse model, was due more to its activity on the tumor cells than to its activity on the microenvironment of the host tissue where metastatic tumor cells colonize to form secondary lesions, we used a model of experimental liver metastasis in which we inoculated untreated or LY2109761-treated L3.6pl/GLT or C5LM2/GLT cells into the spleen of untreated or LY2109761-treated mice and monitored them for the development of liver metastasis. One group of untreated mice inoculated with untreated cells was given additional LY2109761 treatment (group 5). The five treatment groups are summarized in Fig. 6B and Supplementary Fig. S3B.5
Figure 6.
Effect of targeting TβRI/II serine/threonine kinase activity on tumor cells and the liver microenvironment in an in vivo intrasplenic inoculation model of L3.6pl/GLT pancreatic cancer cell experimental liver metastasis. Twenty-five mice were randomly allocated into five treatment groups to be pretreated with LY2109761 or its p.o. vehicle from days −5 to 0. On day 0, L3.6pl/GLT cells (1.0 × 106 per mouse), cultured with LY2109761 (5 μmol/L) or DMSO from days −5 to 0, were inoculated into spleen of each mouse as indicated. Treatment with LY2109761 was continued only for mice in group 5. A, at day 28, the volume of the tumor growing in the liver was evaluated based on the bioluminescence emitted by the tumor cells within the liver region using a IVIS 100 imaging system. Means and 95% confidence intervals. *, P < 0.05 by one-way ANOVA and Dunnett’s multiple comparison posttest. B, at necropsy, the presence of fluorescent tumor lesions in the liver was confirmed with a stereoscopic dissecting fluorescence microscope equipped with a cooled CCD and a color digital camera. For each group, both color and fluorescent pictures of the upper abdominal region of all mice are shown. C, six extra mice were randomly allocated into two groups (n = 3 mice per group) to receive pretreatments as per group 3 (LY2109761, 50 mg/kg twice a day p.o.) or group 1 (vehicle solution for 50 μL of LY2109761 twice a day p.o.) from days −5 to 0. At the end of treatments, the mice were sacrificed by carbon dioxide inhalation, the livers were excised and lysed, and the lysates were subjected to Western blot analysis for examination of the expression of total and phosphorylated Smad2. Representative of three independent experiments.
At the median survival duration for the control group animals, the liver metastases burden of all the mice was quantitatively evaluated (just before sacrifice) by measuring the luciferase signal using an IVIS 100 imaging system. Combinations of ex vivo treatment of L3.6pl/GLT or C5LM2/GLT cells and treatment of mice before and after inoculation with tumor cells were able to substantially reduce liver metastases (Fig. 6A and Supplementary Fig. S3A).5
We then performed necropsy under a fluorescent dissecting microscope to detect every GFP signal from liver metastasis. In the L3.6pl/GLT model, all mice in group 1 (control) developed extensive liver metastatic lesions (Fig. 6B). In contrast, the mice in groups 2 and 3, in which the TGF-β pathway in tumor cells or the host tissue, respectively, was inhibited by LY2109761, only one of five mice developed liver metastasis. Only one of the five mice pretreated with LY2109761 and inoculated with LY2109761-treated tumor cells (group 4), in which both the TGF-β pathway in tumor cells and in the host tissue were inhibited, developed a liver metastasis, and this was substantially smaller than the lesions documented in groups 2 and 3. Complete suppression of liver metastasis was observed in the mice not receiving pretreatment with LY2109761 and inoculated with untreated L3.6pl/GLT cells but posttreated for 4 weeks with LY2109761 starting from the day of the injection. This treatment can be considered as targeting both the pancreatic tumor cells injected and the liver parenchyma for an extended period of time.
In the C5LM2/GLT model, three of five mice in group 1 (control) developed liver metastatic lesions. In contrast, complete suppression of liver metastasis was observed in the mice in groups 2, 3, 4, and 5 (Supplementary Fig. S3B).5 The effective inhibition of any TβRI/II activity on liver microenvironment was shown by the complete suppression of Smad2 phosphorylation on liver protein extracts from mice treated with LY2109761 (as per group 3) compared with the untreated mice (as per group 1; Fig. 6C).
These results suggest that targeting TGF-β signaling by LY2109761 in both pancreatic cancer cells and the hepatic microenvironment contributes to the suppression of pancreatic cancer metastasis.
Discussion
Our study indicates, for the first time, that inhibition of TGF-β signaling cascades by the systemic administration of the novel small molecule–selective TβRI/II kinase inhibitor LY2109761 suppresses liver and other abdominal site metastasis in an in vivo model of human pancreatic cancer.
Current therapies for managing pancreatic cancer patients are not effective. The major causes of morbidity and mortality in pancreatic cancer patients arise from the growth of metastatic lesions and their metabolic effects (26). Tumor metastasis consists of a series of discrete biological processes dependent on both the intrinsic properties of the tumor cells and the unique features of the host tissue microenvironment (27, 28). A primary tumor may contain many different cells, each of which can complete some of the steps in the metastatic process but not all. Only the few cells that can complete all these steps can give rise to a clinically relevant metastasis (29). The paired pancreatic cancer cell lines used in our study, Colo357FG/Colo357L3.6pl (21), and C5/C5LM2, represent an excellent model of this selection process because of the methods of their isolation and allowed us to evaluate the effect of targeting the TGF-β pathway in a human pancreatic cancer cell population and its direct highly metastatic subpopulation, as represented by those cells able to complete the various steps of metastasis formation.
We showed that, although LY2109761 did not have any growth inhibitory or proapoptotic effects on FG/GLT or L3.6pl/GLT cells growing in cell culture as a monolayer, it inhibited the growth of L3.6pl/GLT cells in soft agar and, most important, suppressed both basal and TGF-β–induced L3.6pl/GLT migration and invasion, the steps that initiate the metastatic process. These steps are followed by dissemination through the blood through the lymphatic vessels or across body cavities. TGF-β has been causally involved in tumor cell resistance to anoikis (25), and we showed for the first time that targeting the TGF-β pathway significantly reverts this resistance, thereby reducing the number of viable circulating cells able to give rise to a metastasis.
The intracellular pathways involved in the prometastatic effects of TGF-β and suppressed by targeting TβRI/II kinase activity remain unclear. One of the signature mutations identified in >50% of pancreatic cancer cases is the inactivation of the Smad4 tumor suppressor gene, which is a key transcription factor in TGF-β signaling pathway (30). Recent studies on the in vitro effects of targeting TβRI with small molecule kinase inhibitors in pancreatic cancer cell lines suggested that the inhibition of metastatic processes could be independent of the status of Smad4 (31, 32). Our in vitro and in vivo results in the Smad4-positive L3.6pl/GLT cell line model showed that the dual TβRI/II inhibitor LY2109761 effectively inhibited the phosphorylation of Smad2 and thus suggested that the observed effects of LY2109761 on these cells depend in part on the inhibition of Smad activation.
Studies using TGF-β signaling pathway antagonists in in vivo breast cancer models have presented variable results. Bandyopadhyay et al. (17) showed that treating athymic mice with a TβRI inhibitor effectively reduced the number and size of the lung and bone metastases from human breast cancer cells in both orthotopic xenograft and experimental metastasis models and had no effect on primary tumor growth. Ge et al. (19) showed that treatment with the TβRI inhibitor SD-208 inhibited the number and size of metastases and also affected the primary tumor growth but only in syngeneic R3T or 4T1 mammary tumor-bearing mice models, without any effect in athymic nude mice. In our study, we showed the therapeutic efficacy of treatment with LY2109761 in an in vivo model using athymic nude mice bearing L3.6pl/GLT pancreatic cancer orthotopic xenografts. Treatment with LY2109761 in combination with a suboptimal dose of gemcitabine, the most commonly used cytotoxic drugs for pancreatic cancer (26), significantly reduced L3.6pl/GLT primary tumor growth and prolonged mouse survival. This antitumor activity seems to be contrasted to the lack of in vitro antiproliferative and proapoptotic effects we showed for L3.6pl/GLT cells growing as a monolayer. This discrepancy may be explained by the inhibition of TGF-β signaling by LY2109761 in the tumor microenvironment and the suppression of tumor cell self-seeding (33).
In our study, we showed that LY2109761 significantly reduced abdominal and, especially, liver metastases in a model of spontaneous and experimental pancreatic cancer metastases using athymic nude mice injected with L3.6pl/GLT or C5LM2/GLT cells. In particular, the results obtained by inoculating untreated or LY2109761-pretreated L3.6pl/GLT or C5LM2/GLT cells into the spleen of untreated or LY2109761-pretreated nude mice and examining the frequency of liver metastases suggested that inhibition of the TGF-β pathway in pancreatic cancer cells or in the cells of the liver microenvironment play an important role in suppressing liver metastasis. However, the specific biological mechanisms underlying the suppression of metastasis by LY2109761 in this model remain under active investigation. Hepatic sinusoids are discontinuously lined with endothelial cells and thus are porous to circulating cells (34). For this reason, in the spleen inoculation metastasis model, we believe that LY2109761 is affecting a step that is subsequent to extravasation. One of the rate-limiting steps during metastatic colonization of the liver is the avoidance of cytotoxic immune reactions (28), and pretreatment of the mice with LY2109761 could have blocked the suppressive effect of TGF-β on innate immunity. TGF-β is a potent suppressor of immune function that has pleiotropic effects on several hematopoietic lineages (35). The secretion of TGF-β by tumor cells or cells in the microenvironment can suppress an antitumor immune response and result in tumor promotion. More research on the effect of targeting TβRI/II on the innate immune response against pancreatic cancer cells and on the activities of other important stromal cell populations is warranted.
In conclusion, our results indicate that the targeting of TβRI/II by the selective inhibitor LY2109761 significantly suppresses metastasis of pancreatic cancer in an animal model system and suggest that targeting TβRI/II is a novel therapeutic approach for improving mortality by decreasing liver metastasis in pancreatic cancer patients. Specifically designed clinical trials need to be conducted to evaluate the therapeutic effect of LY2109761 on liver metastasis in patients with locally advanced pancreatic cancer.
Supplementary Material
Acknowledgments
Grant support: U.S. Public Services grants R01CA097159 (P.J. Chiao) and P20-CA101936 (J.L. Abbruzzese), Cancer Center Supporting grant from National Cancer Institute, Lockton Fund for Pancreatic Cancer Research grants (P.J. Chiao), and Topfer Fund for Pancreatic Cancer Research (J.L. Abbruzzese and P.J. Chiao). D. Melisi was recipient of an AIRC-FIRC “Leonino Fontana e Maria Lionello 2005” award and a “Marion D. Edward 2007” award.
We thank Dr. Waun Ki Hong (The University of Texas M. D. Anderson Cancer Center) for his funding support, Helene Pelicano (The University of Texas M. D. Anderson Cancer Center) for FACS analysis, and Elizabeth L. Hess (The University of Texas M. D. Anderson Cancer Center) for editorial assistance.
Footnotes
Supplementary material for this article is available at Molecular Cancer Therapeutics Online (http://mct.aacrjournals.org/).
Jonathan M. Yingling, Eli Lilly, unpublished data.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Varadhachary GR, Tamm EP, Abbruzzese JL, et al. Borderline resectable pancreatic cancer: definitions, management, and role of preoperative therapy. Ann Surg Oncol. 2006;13:1035–46. doi: 10.1245/ASO.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 3.Derynck R, Zhang YE. Smad-dependent and Smad-independent pathways in TGF-β family signalling. Nature. 2003;425:577–84. doi: 10.1038/nature02006. [DOI] [PubMed] [Google Scholar]
- 4.Moustakas A, Heldin CH. Non-Smad TGF-β signals. J Cell Sci. 2005;118:3573–84. doi: 10.1242/jcs.02554. [DOI] [PubMed] [Google Scholar]
- 5.Bierie B, Moses HL. Tumour microenvironment: TGFβ: the molecular Jekyll and Hyde of cancer. Nat Rev Cancer. 2006;6:506–20. doi: 10.1038/nrc1926. [DOI] [PubMed] [Google Scholar]
- 6.Lee JM, Dedhar S, Kalluri R, Thompson EW. The epithelial-mesenchymal transition: new insights in signaling, development, and disease. J Cell Biol. 2006;172:973–81. doi: 10.1083/jcb.200601018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy L, Hill CS. Alterations in components of the TGF-β superfamily signaling pathways in human cancer. Cytokine Growth Factor Rev. 2006;17:41–58. doi: 10.1016/j.cytogfr.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Culhaci N, Sagol O, Karademir S, et al. Expression of transforming growth factor-β-1 and p27Kip1 in pancreatic adenocarcinomas: relation with cell-cycle-associated proteins and clinicopathologic characteristics. BMC Cancer. 2005;5:98. doi: 10.1186/1471-2407-5-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teraoka H, Sawada T, Yamashita Y, et al. TGF-β1 promotes liver metastasis of pancreatic cancer by modulating the capacity of cellular invasion. Int J Oncol. 2001;19:709–15. doi: 10.3892/ijo.19.4.709. [DOI] [PubMed] [Google Scholar]
- 10.Friess H, Yamanaka Y, Buchler M, et al. Enhanced expression of transforming growth factor β isoforms in pancreatic cancer correlates with decreased survival. Gastroenterology. 1993;105:1846–56. doi: 10.1016/0016-5085(93)91084-u. [DOI] [PubMed] [Google Scholar]
- 11.Wagner M, Kleeff J, Friess H, Buchler MW, Korc M. Enhanced expression of the type II transforming growth factor-β receptor is associated with decreased survival in human pancreatic cancer. Pancreas. 1999;19:370–6. doi: 10.1097/00006676-199911000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Siegel PM, Shu W, Cardiff RD, Muller WJ, Massague J. Transforming growth factor β signaling impairs Neu-induced mammary tumorigenesis while promoting pulmonary metastasis. Proc Natl Acad Sci U S A. 2003;100:8430–5. doi: 10.1073/pnas.0932636100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tian F, Byfield SD, Parks WT, et al. Smad-binding defective mutant of transforming growth factor β type I receptor enhances tumorigenesis but suppresses metastasis of breast cancer cell lines. Cancer Res. 2004;64:4523–30. doi: 10.1158/0008-5472.CAN-04-0030. [DOI] [PubMed] [Google Scholar]
- 14.Bierie B, Moses HL. TGF-β and cancer. Cytokine Growth Factor Rev. 2006;17:29–40. doi: 10.1016/j.cytogfr.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Yen TW, Aardal NP, Bronner MP, et al. Myofibroblasts are responsible for the desmoplastic reaction surrounding human pancreatic carcinomas. Surgery. 2002;131:129–34. doi: 10.1067/msy.2002.119192. [DOI] [PubMed] [Google Scholar]
- 16.Bellone G, Carbone A, Smirne C, et al. Cooperative induction of a tolerogenic dendritic cell phenotype by cytokines secreted by pancreatic carcinoma cells. J Immunol. 2006;177:3448–60. doi: 10.4049/jimmunol.177.5.3448. [DOI] [PubMed] [Google Scholar]
- 17.Bandyopadhyay A, Agyin JK, Wang L, et al. Inhibition of pulmonary and skeletal metastasis by a transforming growth factor-β type I receptor kinase inhibitor. Cancer Res. 2006;66:6714–21. doi: 10.1158/0008-5472.CAN-05-3565. [DOI] [PubMed] [Google Scholar]
- 18.Ehata S, Hanyu A, Fujime M, et al. Ki26894, a novel transforming growth factor-β type I receptor kinase inhibitor, inhibits in vitro invasion and in vivo bone metastasis of a human breast cancer cell line. Cancer Sci. 2007;98:127–33. doi: 10.1111/j.1349-7006.2006.00357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ge R, Rajeev V, Ray P, et al. Inhibition of growth and metastasis of mouse mammary carcinoma by selective inhibitor of transforming growth factor-β type I receptor kinase in vivo. Clin Cancer Res. 2006;12:4315–30. doi: 10.1158/1078-0432.CCR-06-0162. [DOI] [PubMed] [Google Scholar]
- 20.Arteaga CL. Inhibition of TGFβ signaling in cancer therapy. Curr Opin Genet Dev. 2006;16:30–7. doi: 10.1016/j.gde.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 21.Bruns CJ, Harbison MT, Kuniyasu H, Eue I, Fidler IJ. In vivo selection and characterization of metastatic variants from human pancreatic adenocarcinoma by using orthotopic implantation in nude mice. Neoplasia. 1999;1:50–62. doi: 10.1038/sj.neo.7900005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malkin D, Li FP, Strong LC, et al. Germ line p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms. Science. 1990;250:1233–8. doi: 10.1126/science.1978757. [DOI] [PubMed] [Google Scholar]
- 23.Trauzold A, Roder C, Sipos B, et al. CD95 and TRAF2 promote invasiveness of pancreatic cancer cells. FASEB J. 2005;19:620–2. doi: 10.1096/fj.04-2984fje. [DOI] [PubMed] [Google Scholar]
- 24.Casey RC, Koch KA, Oegema TR, Jr, et al. Establishment of an in vitro assay to measure the invasion of ovarian carcinoma cells through mesothelial cell monolayers. Clin Exp Metastasis. 2003;20:343–56. doi: 10.1023/a:1024009131191. [DOI] [PubMed] [Google Scholar]
- 25.Rennebeck G, Martelli M, Kyprianou N. Anoikis and survival connections in the tumor microenvironment: is there a role in prostate cancer metastasis? Cancer Res. 2005;65:11230–5. doi: 10.1158/0008-5472.CAN-05-2763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li D, Xie K, Wolff R, Abbruzzese JL. Pancreatic cancer. Lancet. 2004;363:1049–57. doi: 10.1016/S0140-6736(04)15841-8. [DOI] [PubMed] [Google Scholar]
- 27.Steeg PS. Tumor metastasis: mechanistic insights and clinical challenges. Nat Med. 2006;12:895–904. doi: 10.1038/nm1469. [DOI] [PubMed] [Google Scholar]
- 28.Gupta GP, Massague J. Cancer metastasis: building a framework. Cell. 2006;127:679–95. doi: 10.1016/j.cell.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Fidler IJ. The pathogenesis of cancer metastasis: the “seed and soil” hypothesis revisited. Nat Rev Cancer. 2003;3:453–8. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 30.Hahn SA, Schutte M, Hoque AT, et al. DPC4, a candidate tumor suppressor gene at human chromosome 18q21.1. Science. 1996;271:350–3. doi: 10.1126/science.271.5247.350. [DOI] [PubMed] [Google Scholar]
- 31.Halder SK, Beauchamp RD, Datta PK. A specific inhibitor of TGF-β receptor kinase, SB-431542, as a potent antitumor agent for human cancers. Neoplasia. 2005;7:509–21. doi: 10.1593/neo.04640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Subramanian G, Schwarz RE, Higgins L, et al. Targeting endogenous transforming growth factor β receptor signaling in SMAD4-deficient human pancreatic carcinoma cells inhibits their invasive phenotype1. Cancer Res. 2004;64:5200–11. doi: 10.1158/0008-5472.CAN-04-0018. [DOI] [PubMed] [Google Scholar]
- 33.Norton L, Massague J. Is cancer a disease of self-seeding? Nat Med. 2006;12:875–8. doi: 10.1038/nm0806-875. [DOI] [PubMed] [Google Scholar]
- 34.Chambers AF, Groom AC, MacDonald IC. Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer. 2002;2:563–72. doi: 10.1038/nrc865. [DOI] [PubMed] [Google Scholar]
- 35.Letterio JJ, Roberts AB. Regulation of immune responses by TGF-β. Annu Rev Immunol. 1998;16:137–61. doi: 10.1146/annurev.immunol.16.1.137. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.