Abstract
Sarcoidosis is a multisystemic granulomatous disease of unknown etiology. Hepatic involvement was reported in about 11% of patients with sarcoidosis. However, cases of sarcoidosis in which the granuloma is solitary and limited in the liver are very rare. A 51-year-old woman with tumors in the liver underwent extended left lobectomy with caudate lobectomy and bile duct resection. The tumor was located between segment 4 and the hilar region. Some daughter nodules were found in the left lobe, which were regarded as intrahepatic metastasis. Our case displayed clinical and radiologically distinct findings, which are very similar to those of hilar cholangiocarcinoma restricted to the liver. This report demonstrates that sarcoidosis can show solitary hepatic involvement in the absence of thoracic lymphadenopathy. In such a case, it is difficult to distinguish the diagnosis from other malignant neoplasms. In conclusion, the diagnosis of hepatic sarcoidosis has to be made through prudent and comprehensive investigations that include a full clinical history of sarcoidosis in other organs. Despite utilizing several detailed diagnostic modalities, the definitive diagnosis of cases of solitary sarcoidosis may remain difficult. In these cases, surgical treatment including liver resection should be considered in order to avoid missing a suitable opportunity for treatment.
Key Words: Sarcoidosis, Hepatic sarcoidosis, Hepatic granulomas, Hilar cholangiocarcinoma
Introduction
Sarcoidosis is a multisystemic granulomatous disease of unknown etiology characterized by the presence of non-caseating granuloma consisting of epithelioid cells. Sarcoidosis primarily affects the lung and hilar lymph nodes. Heart, spleen, bone marrow and less often eye, skin and salivary glands are common extrapulmonary sites of disease manifestation. The liver has sarcoid nodules on occasions, however these nodules are generally multiple and diffuse [1]. Granulomatous lesions in hepatic sarcoidosis are most often located at the catchment area of Glisson's capsule. In these patients, portal hypertension is the predominant symptom.
The diagnosis of hepatic sarcoidosis might be easy because patients with hepatic sarcoidosis have generally pulmonary lesions or hilar lymph node swelling at the same time. We present a case of hepatic sarcoidosis with a solitary giant nodule in the liver, but with radiological findings typical of hilar cholangiocarcinoma.
Case Report
A 51-year-old female was referred to our institution with abnormal laboratory data of liver function and the biliary system. She had had a light inguinal swelling lymph node for about 6 months. The laboratory data on admission showed slight elevation of alkaline phosphatase (ALP) and gamma-glutamyl transpeptidase (γ-GTP), but a normal level of tumor marker (table 1). She had no symptoms. Her physical condition upon admission was generally good; there was no anemia or jaundice, and the liver was not palpable. A swelling nodule 1.5 cm diameter was palpable at the right groin.
Table 1.
Laboratory data on admission
| WBC | 5.8×103/μl | Alb | 4.2 g/dl | BUN | 11.1 mg/dl |
| RBC | 4.34×106/μl | T.bil | 0.7 mg/dl | Cr | 0.72 mg/dl |
| Hb | 12.8 g/dl | D.bil | 0.1 mg/gl | Na | 143 mEq/l |
| Ht | 40.0% | GOT | 36 IU/l | K | 3.7 mEq/l |
| Plt | 18.2×104/μl | GPT | 33 IU/l | Cl | 105 mEq/l |
| PT | 91% | LDH | 150 IU/l | ACE | 19.7 IU/l |
| aPTT | 33.9 s | ALP | 528 IU/l | HBs-Ag | (−) |
| TT | >100% | γ-GTP | 356 IU/l | HCV-Ab | (−) |
| HPT | 143% | LAP | 84 IU/l | CEA | 1.4 ng/ml |
| FNG | 395 mg/dl | ChE | 4,411 IU/l | CA19-9 | 14.4 U/ml |
| TP | 8.9 g/dl | Amy | 84 IU/l |
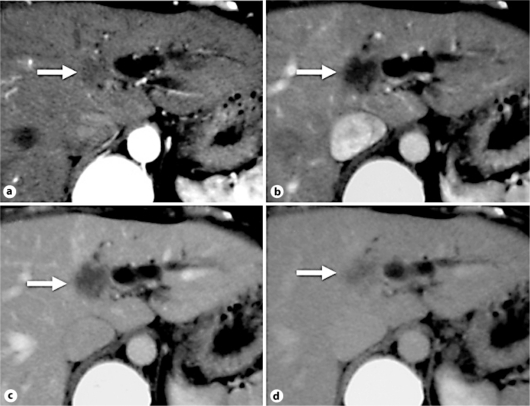
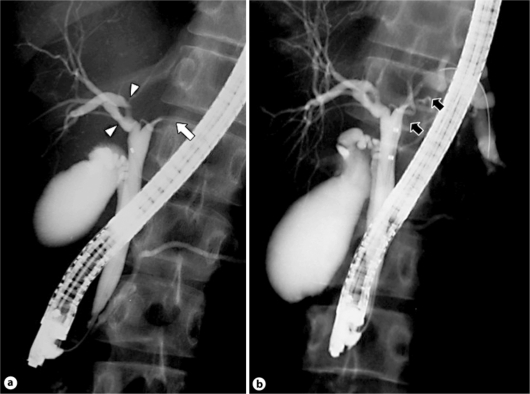
Abdominal ultrasonography showed a low echoic lesion of 37 mm diameter with an unclear margin at segment 4. The intrahepatic bile ducts (IHBDs) of the left lobe were dilated to 6 mm with obstruction by this tumor. A swelling round lymph node of 11 mm diameter was revealed in the hilar region of the liver. Abdominal dynamic computed tomography (CT) revealed a 4.0 cm tumor of low density at segment 4, which partially invaded segments 1, 5, and 8. The tumor had poor enhancement during the early arterial phase (fig. 1a). During the portal in-flow phase, the tumor was detected as a low-density lesion with an irregular shape (fig. 1b). The contrast enhancement of the tumor was slightly intense at the margin of the tumor during the equilibrium phase (fig. 1c) and became more intense during the delayed phase, but the margin became unclear (fig. 1d). Magnetic resonance cholangiopancreatography showed remarkable dilatations of the IHBDs of segment 2 and 3 with an extreme stenosis of the left main hepatic duct. Endoscopic retrograde cholangiopancreatography also revealed conspicuous stenosis at the junction of the left hepatic duct and the common hepatic duct as well as stenosis and rigidity of the anterior and posterior branches of the right hepatic duct. Moreover, the junction of the hepatic duct draining the right caudate lobe had stenosis (fig. 2a). When deep cannulation was performed beyond the stenotic hepatic duct, dilated IHBDs of segment 2, 3 and 4 were detected. The length of the stenotic ducts was about 3 cm (fig. 2b).
Fig. 1.
Abdominal dynamic CT. a Early arterial phase. A 4.0 cm tumor of low density with poor enhancement was detected at segment 4 (arrow). b Portal in-flow phase. The tumor was detected as a low-density lesion with an irregular shape. c Equilibrium phase. Contrast enhancement of the tumor was slightly intense at the margin of the tumor. d Delayed phase. Contrast enhancement became more intense. The margin of the tumor became unclear.
Fig. 2.
a Endoscopic retrograde cholangiopancreatography revealing conspicuous stenosis at the junction of the left hepatic duct and the common hepatic duct (arrow). The right hepatic duct showed another stenosis and rigidity of the anterior and posterior branches (arrowheads). b The length of the stenotic ducts was about 3 cm (arrows).
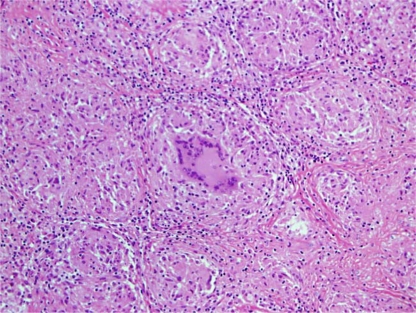
Extended left lobectomy with caudate lobectomy and bile duct resection was performed with a diagnosis of hilar cholangiocarcinoma located predominantly at the left main hepatic duct. The tumor occupied the region between segment 4 and the hilum. Some daughter nodules were found in the left lobe, which were considered to be intrahepatic metastasis. Pathological findings confirmed the presence of non-caseating granuloma with multinucleated giant cells. There were multiple nodules with severe fibrosis in the resected specimen. A lot of small non-caseating granulomas consisting of epithelioid cells were found in the dissected lymph nodes. The final histopathological diagnosis was hepatic sarcoidosis (fig. 3).
Fig. 3.
Histopathological findings show the presence of non-caseating granuloma with multinucleated giant cells, in which the final histopathological diagnosis was determined to be hepatic sarcoidosis.
Discussion
The case reported here is important because of its morphologically distinct characteristics from radiological findings for hepatic sarcoidosis. Sarcoidosis is a systemic disease that primarily affects the lungs and lymphoid tissues of the body. In Japan, sarcoidosis occurs mainly in the age group of 50- to 60-year-olds with a predilection for females [2]. Its prevalence is reported to be 1.01 per 100,000 inhabitants.
Hepatic involvement of sarcoidosis was described in 11.5% of 736 patients in the ACCESS study [3]. Hepatic granulomas due to sarcoidosis were recognized most commonly as multiple and small nodules with less than 1.0 cm diameter. Liver involvement ranges from asymptomatic incidental granulomas to portal hypertension from granulomas in the portal triad, usually with relative preserved liver function [4]. Angiotensin-converting enzyme (ACE) level may be elevated in 70% of patients with sarcoidosis and is elevated in almost all patients with hepatic sarcoidosis. In general, in 20–40% of patients with sarcoidosis, ALP and γ-GTP levels are elevated, but in those with hepatic sarcoidosis the levels are usually much higher [5].
Ultrasonography findings include parenchymal echogenicity, coarsening of the liver parenchyma with or without discrete nodules, and focal calcifications as well as contour irregularity [6]. On CT, hepatic granulomas are visualized as multiple, discrete, low-attenuating, non-contrast-enhancing nodules of variable size. As they increase in size, they tend to become confluent and have to be differentiated from various infectious and neoplasmatic conditions [7]. Magnetic resonance imaging also shows multiple diffuse, densely packed, uniform nodular foci with normal signal intensity with T1- and hypodense with T2-weighted sequence. On dynamic CT imaging, our case was compatible with hepatic sarcoidosis due to a poor enhancement effect on early arterial phase and a slight enhancement from the margin on delayed phase, even though this intrahepatic nodule was huge and solitary.
In most patients with sarcoidosis, the course of hepatic involvement is asymptomatic [8]. In a few patients, chronic intrahepatic cholestasis or portal hypertension can complicate the course of the disease. Portal hypertension could be due to obstruction of portal flow because of granulomas in the portal area, with fibrosis and hyalinization of the portal triad causing presinusoidal block. Another possible mechanism was advocated in which there might be arteriovenous shunts that increase portal blood flow.
Asymptomatic patients with mild elevation in liver function enzymes should not be treated but should be followed with serial blood work. It has been reported that the majority of untreated patients who are clinically asymptomatic have spontaneous improvement in their liver function [5]. Indeed, death from liver failure is rare. Perry and Vuitch reported that the mortality rate of patients with sarcoidosis was 1 of 28 at autopsy and 1 of 18 with portal hypertension [9]. For patients with refractory liver dysfunction, chronic progressive cholestatic disease and portal hypertension that develop more severe liver disease, corticosteroids should be administered. However, corticosteroids cannot prevent disease progression, including development of portal hypertension in patients with early or established cirrhosis [10]. For such cases, when medications are no longer efficacious, liver transplantation is the only option [11].
There are other causes of hepatic granulomas, including bacterial infections such as tuberculosis, brucellosis, viral infections and parasite infections, primary liver disease such as primary biliary cirrhosis, autoimmune cholangiopathy and many other systemic illnesses. As mentioned above, there is a wide differential for granulomas in the liver. In western countries, a large portion is attributed to primary biliary cirrhosis (up to 55%) and sarcoidosis (15–30%), but infective cases, like tuberculosis and brucellosis, should always be kept in mind during initial investigation [12, 13]. Evaluating hepatic granulomas should therefore include a detailed medical and drug history followed by extensive laboratory testing. The majority of cases in which granulomas appear only in the liver are caused by liver disease rather than multisystemic disease. In that case, the differential diagnosis may be frequently difficult compared to other tumor-forming diseases, such as neoplasm in the liver. The diagnostic approach to hepatic sarcoidosis must be made on the histological evidence of non-caseating granulomas in a liver biopsy.
In this report, we describe a rare experience with hepatic sarcoidosis, which we presented with clinical and radiological findings characteristic of hilar cholangiocarcinoma. We could find only two similar cases reported previously [14, 15]. Our experience suggests that the diagnosis of patients with tumors in the liver with atypical radiological findings, who have a case history of sarcoidosis, need to be established by comprehensive and cautious consideration. There should be no hesitation to perform liver biopsy if there is difficulty in making a definitive diagnosis. Despite utilizing several detailed and extensive diagnostic modalities, we may occasionally encounter a patient with a solitary tumor in the liver for whom it is extremely difficult to make a differential diagnosis from the malignant neoplasm, much like our experience. In this case, a surgical treatment including liver resection should be seriously considered, because a patient with hepatic sarcoidosis occasionally had to undergo liver transplantation in the end after a short period of observation without any treatment due to the difficulty of diagnosis like our case.
Disclosure Statement
The authors have no conflict of interest with this report. This study was not supported by any grants.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Baughman RP, Lower EE, du Bois RM. Sarcoidosis. Lancet. 2003;361:1111–1118. doi: 10.1016/S0140-6736(03)12888-7. [DOI] [PubMed] [Google Scholar]
- 2.Morimoto T, Azuma A, Abe S, et al. Epidemiology of sarcoidosis in Japan. Eur Respir J. 2008;31:372–379. doi: 10.1183/09031936.00075307. [DOI] [PubMed] [Google Scholar]
- 3.Baughman RP, Teirstein AS, Judson MA, et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am J Respir Crit Care Med. 2001;164:1885–1889. doi: 10.1164/ajrccm.164.10.2104046. [DOI] [PubMed] [Google Scholar]
- 4.Ebert EC, Kierson M, Hagspiel KD. Gastrointestinal and hepatic manifestations of sarcoidosis. Am J Gastroenterol. 2008;103:3184–3192. doi: 10.1111/j.1572-0241.2008.02202.x. quiz 3193. [DOI] [PubMed] [Google Scholar]
- 5.Judson MA. Hepatic, splenic, and gastrointestinal involvement with sarcoidosis. Semin Respir Crit Care Med. 2002;23:529–541. doi: 10.1055/s-2002-36517. [DOI] [PubMed] [Google Scholar]
- 6.Kessler A, Mitchell DG, Israel HL, Goldberg BB. Hepatic and splenic sarcoidosis: ultrasound and MR imaging. Abdom Imaging. 1993;18:159–163. doi: 10.1007/BF00198055. [DOI] [PubMed] [Google Scholar]
- 7.Warshauer DM, Dumbleton SA, Molina PL, Yankaskas BC, Parker LA, Woosley JT. Abdominal CT findings in sarcoidosis: radiologic and clinical correlation. Radiology. 1994;192:93–98. doi: 10.1148/radiology.192.1.8208972. [DOI] [PubMed] [Google Scholar]
- 8.Valla DC, Benhamou JP. Hepatic granulomas and hepatic sarcoidosis. Clin Liver Dis. 2000;4:269–285. doi: 10.1016/s1089-3261(05)70108-2. ix-x. [DOI] [PubMed] [Google Scholar]
- 9.Perry A, Vuitch F. Causes of death in patients with sarcoidosis. A morphologic study of 38 autopsies with clinicopathologic correlations. Arch Pathol Lab Med. 1995;119:167–172. [PubMed] [Google Scholar]
- 10.Kennedy PT, Zakaria N, Modawi SB, et al. Natural history of hepatic sarcoidosis and its response to treatment. Eur J Gastroenterol Hepatol. 2006;18:721–726. doi: 10.1097/01.meg.0000223911.85739.38. [DOI] [PubMed] [Google Scholar]
- 11.Casavilla FA, Gordon R, Wright HI, Gavaler JS, Starzl TE, Van Thiel DH. Clinical course after liver transplantation in patients with sarcoidosis. Ann Intern Med. 1993;118:865–866. doi: 10.7326/0003-4819-118-11-199306010-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McCluggage WG, Sloan JM. Hepatic granulomas in Northern Ireland: a thirteen year review. Histopathology. 1994;25:219–228. doi: 10.1111/j.1365-2559.1994.tb01321.x. [DOI] [PubMed] [Google Scholar]
- 13.Matheus T, Munoz S. Granulomatous liver disease and cholestasis. Clin Liver Dis. 2004;8:229–246. doi: 10.1016/S1089-3261(03)00137-5. ix. [DOI] [PubMed] [Google Scholar]
- 14.Pungpapong S, Steers JL, Wallace MB, Krishna M, Keaveny AP. Hepatobiliary sarcoidosis mimicking Klatskin's cholangiocarcinoma. Gastrointest Endosc. 2006;64:124–125. doi: 10.1016/j.gie.2006.01.033. [DOI] [PubMed] [Google Scholar]
- 15.Rezeig MA, Fashir BM. Biliary tract obstruction due to sarcoidosis: a case report. Am J Gastroenterol. 1997;92:527–528. [PubMed] [Google Scholar]