Abstract
This study assesses whether California’s minimum nurse staffing legislation affected the amount of uncompensated care provided by California hospitals. Using data from California’s Office of Statewide Health Planning and Development, the American Hospital Association Annual Survey and InterStudy, we divide hospitals into quartiles based on pre-regulation staffing levels. Controlling for other factors, we estimate changes in the growth rate of uncompensated care in the three lowest staffing quartiles relative to the quartile of hospitals with the highest staffing level. Our sample includes short-term general hospitals over the period 1999 to 2006. We find that growth rates in uncompensated care are lower in the first three staffing quartiles as compared to the highest quartile; however, results are statistically significant only for county and for-profit hospitals in quartiles one and three. We conclude that minimum nurse staffing ratios may lead some hospitals to limit uncompensated care, likely due to increased financial pressure.
Keywords: Uncompensated care, nurse staffing, California
INTRODUCTION
Within the U.S. health care system, where under-insurance and lack of insurance are prevalent, uncompensated care has historically granted access to health services for many Americans. Acute care hospitals provided approximately 67 percent of all uncompensated care in 2001 (an estimated $23.6 billion). As much as 12% of these services was financed through hospital operating earnings (Hadley & Holahan, 2003).
In October 1999, California passed legislation that had the potential to threaten hospital operating earnings and therefore the funds available to support uncompensated care. California Assembly Bill (AB) 394 mandated minimum nurse staffing ratios for hospitals. Approximately 30 percent of hospital budgets are dedicated to nursing personnel (Government Accounting Office, 2001), and early estimates of the cost of implementing AB394 ranged from $198,000 to $2.3 million per hospital (Coffman, Seago, and Spetz 2002; Spetz 2004). Recent research indicates that nurse wages rose following implementation, and early cost estimates were likely too low (Mark, Harless, & Spetz, 2009; Spetz et al., 2009). The costs of complying with AB394 appear substantial and raise the question of how hospitals have paid for them.
Although prices to privately insured patients in California have risen since 1999, prices to publicly insured patients have not (Antwi, Gaynor, & Vogt, 2009); therefore, cost reduction and efficiency-improvement strategies may be expected as one response to legislation that essentially imposes a cost increase on many hospitals. Since the amount of care provided to uninsured patients is an elective cost, at least in the short-term, one response to the California legislation may have been a reduction in the amount of uncompensated care.1
The purpose of this study is to investigate the effect of California’s minimum nurse staffing legislation on uncompensated care. More specifically, we test the hypothesis that hospitals reduced the amount of uncompensated care that they provided following the introduction of minimum nurse staffing legislation. Our model allows for differential responses to the legislation based on pre-regulation staffing levels and hospital ownership. Results of this study have important implications for patients, hospital executives, and state and federal health policymakers as they consider minimum nurse staffing legislation and community benefits.
AB394, CALIFORNIA’S MINIMUM NURSE STAFFING LEGISLATION
In October 1999, California became the first state to pass minimum nurse staffing legislation. The legislation was a response to a reported decline in hospitals’ nurse staffing and skill mix induced by pressures from increasing managed care. Many believed that staffing legislation would improve working conditions for nurses, with the expectation that improved working conditions would result in improved quality of care. AB394 directed the California Department of Health Services to establish minimum nurse-to-patient ratios for licensed nurses (Registered Nurses (RNs) and Licensed Vocational Nurses (LVNs)) in all acute care, psychiatric and specialty hospitals in California. Draft regulations were released in January 2002 and implemented in January 2004 after a period of public comment. The regulations specify minimum staffing ratios by type of patient care unit, with some changes over time; the minimum staffing ratio for medical-surgical areas, for example, was set at 1:6 beginning January 1, 2004, and this ratio was scheduled to be enriched to 1:5 on January 1, 2005. The California ratios reflect richer staffing levels than have been found in many hospitals (Aiken, Clarke, Sloane, Sochalski, & Silber, 2002). Although the California Department of Health Services was given limited enforcement power, Medicare and MediCal (California’s Medicaid program) require hospitals to comply with all relevant laws and regulations (Spetz, 2004).
Early evidence on the effects of the legislation showed that RN hours of care per patient day increased 20% on medical-surgical units, and total nursing hours of care per patient day increased by 7.4% in the first two quarters of 2004 in 68 acute care hospitals participating in the California Nursing Outcomes Coalition project (Donaldson et al., 2005). The generality of the findings is not clear, however, because of the size and selection of the sample. More recent research finds that licensed nurse staffing increased 16.2% statewide between 1999 and 2006 (Spetz et al., 2009). These changes suggest that many hospitals had staffing levels below the minimum standards imposed by AB394, as was initially estimated (Coffman et al. 2002; Spetz 2004).
HOSPITAL FINANCIAL PRESSURE AND PROVISION OF UNCOMPENSATED CARE
There is ample evidence to suggest that hospital financial pressure may lead to a reduction in uncompensated care. Hospitals facing high levels of uncompensated care have been shown to be more likely to adopt explicit limits on charity care (Hadley & Feder, 1985). Several studies have found evidence of a positive association between hospital income and uncompensated care (Frank, Salkever, & Mullann, 1990; Rosko, 2004), and more recently between hospital free cash flow and uncompensated care (Kim, McCue, & Thompson, 2009). Similarly, Medicare and Medicaid payment generosity has been found to be positively associated with levels of hospital uncompensated care (Davidoff, LoSasso, Bazzoli, & Zuckerman, 2000; Mann, Melnick, Bamezai, & Zwanziger, 1997), particularly among hospitals defined as core safety net hospitals (Bazzoli, Lindrooth, Kang, & Hasnain-Wynia, 2006). In contrast, having a higher share of patients insured by Medicare and Medicaid is linked to reduced provision of uncompensated care (Hsieh, Clement, & Bazzoli, 2010). Finally, direct state and local subsidies for uncompensated care services have been shown to have a positive effect on state-level per capita uncompensated care provided by hospitals (Lo Sasso & Seamster, 2007).
NEW CONTRIBUTION
While the literature consistently shows that financial pressure negatively affects levels of uncompensated care, there has been no examination of California AB394 as a regulation with the potential to impose a substantial shock to hospital operating expenses. A requirement to implement and maintain a specified level of nurse staffing is significant and unique as compared to many other environmental factors that create financial pressure for hospitals. First, nursing is an integral and pervasive part of hospital operations. As a result, relatively small changes can induce large cost increases and adverse financial effects on the hospital. Second, nursing costs must be funded with internally generated revenue which also is a primary source of funding for uncompensated care (Gray & Schlesinger, 2009). In contrast, many other cost-producing activities such as capital projects or electronic medical records implementation may be eligible for alternative financing, including debt or government grants that would allow hospitals to preserve internally generated funds. Because of the reach of policies like AB394, as well as the potential threat to hospitals’ resources, it is critical to understand the consequences of minimum nurse staffing requirements for uncompensated care. We explore this question, and thus provide knowledge for policymakers and managers to determine whether further policy action or financial supports are needed to maintain access to care.
CONCEPTUAL FRAMEWORK
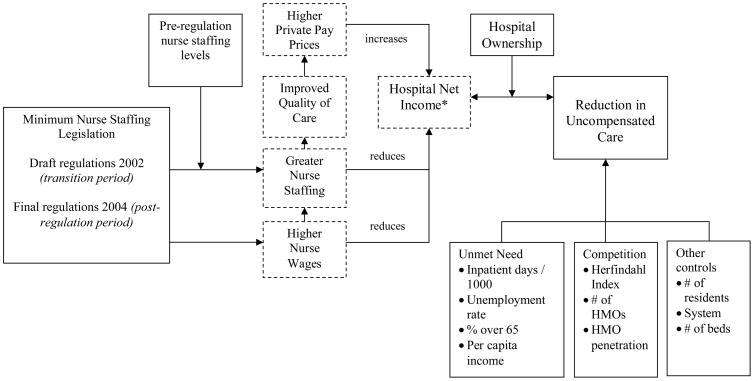
The framework for this study (Figure 1) draws from existing economic models of hospitals’ supply of uncompensated services. These models suggest that, in addition to the amount of unmet need in the community and the amount of uncompensated care provided by competitor hospitals, hospital income is a primary determinant of hospitals’ supply of uncompensated care (Frank & Salkever, 1991). AB394 threatens income for hospitals with pre-regulation nurse staffing levels below the mandated minimum standards by constraining hospitals’ input decisions. First, as hospitals are forced to hire new nurses, operating costs are directly increased through the expansion of the number of employees on the payroll or the substitution of nurses for less expensive labor or equipment (McCue, Mark, & Harless, 2003; Needleman, 2008). Second, as hospitals hire new nurses, wages may rise as the overall demand for nurses in the market is increased. A recent study found that nurse wages in California rose following AB394, suggesting that both mechanisms were working to increase nursing costs for hospitals that were not in compliance with the minimum nurse staffing standards mandated by AB394 (Mark et al., 2009).
Figure 1.
Conceptual Model of the Effect of AB394 on Hospital Uncompensated Care
Notes:
Boxes with dashed lines are not modeled
*Hospital net income would be reduced by increases in nurse staffing and nurse wages. The reduction may be offset by higher private pay prices if higher quality allows hospitals to negotiate better rates. However, we hypothesize that during the study period, the cost increase would not be fully offset by price increases so that the net effect on net income would be a decrease.
In the absence of revenue increases, an increase in labor expense requires a reduction in other operating expenses to maintain a similar level of net income or loss. Theories of hospital behavior posit that hospitals will adjust either the quantity or quality of services provided (Hoerger, 1991; Newhouse, 1970). Evidence suggests that hospitals are unlikely to willingly reduce quality (Newhouse, 1970); this may be particularly true in California hospitals at the time of AB394 since the legislation was enacted in part in response to concerns over hospital quality, and the trend nationally was toward an increased focus on improving hospital quality through both public reporting and financial incentives (e.g., HospitalCompare, Medicare ‘never events’, and value-based purchasing). Thus, the more likely response is to reduce the quantity of services. One option that can be implemented relatively quickly is to reduce the level of uncompensated care.
In addition to affecting hospital income, AB394 may also change the relative cost of providing uncompensated care. Specifically, if improvements in nurse staffing ratios lead to improvements in hospital quality as evidence suggests (Joseph, 2007; Kaestner & Guardado, 2008; Kane, Shamliyan, Mueller, Duval, & Wilt, 2007; Mark & Harless, 2007; Mark, Harless, & Berman, 2007; Mark, Harless, & McCue, 2005; Needleman & Buerhaus, 2003; Needleman, Buerhaus, Mattke, Stewart, & Zelevinsky, 2002; Seago, Spetz, & Mitchell, 2004), hospitals may be able to increase prices to privately insured patients, creating an incentive to treat higher paying patients at the expense of the uninsured in order to cover the increase in labor expense (Needleman, Buerhaus, Stewart, Zelevinsky, & Mattke, 2006; Rothberg, Abraham, Lindenauer, & Rose, 2005).
The extent to which labor cost and private payer price changes influence levels of uncompensated care may depend on ownership, although the specific effect of ownership is not clear. One theory suggests that not-for-profit hospitals behave differently than for-profit hospitals by maintaining specific profit constraints (Hoerger, 1991). The existence of binding profit constraints may make not-for-profit hospitals more likely than for-profit hospitals to respond with reductions in uncompensated care. At the same time, however, for-profit hospitals have an objective to maximize profit for owners and may be more likely to respond to changes in private-pay prices by trading off uncompensated care in favor of more profitable patients (Hoerger, 1991).
While ideally we would estimate a structural model of the effects of AB394 on uncompensated care, data limitations preclude the separation of labor expense and private payer price effects. Moreover, hospital net income and uncompensated care may be endogenous (e.g., hospitals that provide more uncompensated care may have lower net income); therefore, we focus on the reduced form effect of AB394 on uncompensated care controlling for other factors shown to affect uncompensated care. The impact of AB394 is expected to be greatest for hospitals facing the largest pre-regulation nursing shortfalls, thus we test the following hypothesis:
Hospitals reduce the amount of uncompensated care that they provide in response to the passage of AB394, and the degree of response is positively related to the degree of prior nurse staffing shortfall.
Ownership is expected to moderate the response to AB394, thus we allow for varying effects by interacting our policy variables with hospital ownership. Because the effect of ownership is complex, we do not hypothesize a specific relationship. Since draft regulations were released in 2002, but final regulations were not implemented until 2004, we allow for separate effects during the transition and post-regulation periods.
Economic models of uncompensated care provision rely on the assumption that hospitals can control the amount of uncompensated care they provide. Although emergency care must be provided by law, hospital personnel exercise a considerable amount of control over the provision of uncompensated services (Weiner, VanGeest, Abrams, Moswin, & Warnecke, 2008). Moreover, hospital managers often plan and budget for specific levels of uncompensated services when allocating resources in order to balance margin and mission (Gray & Schlesinger, 2009).
METHODS
Data and Study Sample
Data on uncompensated care, total operating expenses, ownership type, and nurse staffing (productive hours and patient days) come from the Annual Hospital Disclosure Reports from the California Office of Statewide Health Planning and Development. Data on system membership, number of residents, aggregate hospital use and competition (as measured by the Herfindahl index calculated using inpatient days) in each hospital’s market area come from the American Hospital Association Annual Survey. Population characteristics include unemployment rate (Bureau of Labor Statistics), percentage of population over 65 (Census Bureau), and per capita income (Bureau of Economic Analysis). InterStudy data are used to measure the number of HMOs and HMO penetration. Data from these files are merged over the period 1999 to 2006. Data on nursing hours from 1999 to 2001 are used to construct baseline measures of nurse staffing. Market areas are defined using Hospital Service Areas (HSAs) (Makuc, Haglund, Ingram, Kleinman, & Feldman, 1991).
The analysis focuses on all short-term, general hospitals in California for which data on nurse staffing and uncompensated care could be obtained. We began with 2,100 cost report observations for general acute care hospitals with an adjusted daily census of at least 20 and with cost reports reflecting at least 360 days. After first-differencing to calculate the yearly growth rate of uncompensated care, there were 1,817 observations. A total of 337 cost report observations were excluded, 97% because they were missing data for charity care, bad debt expense, or both; Kaiser Foundation hospitals, for example, did not report these values at the individual hospital level. Eleven additional observations were excluded because the uncompensated care values were judged to be unbelievable or because there were missing values for regressors. Finally, 28 observations were excluded from three hospitals that had received rural hospital waivers from the staffing regulations. The final study sample consists of 1,451 hospital-year observations from 228 unique hospitals over the period 1999 to 2006.
Empirical Model and Specification
Uncompensated care is defined as the sum of charity care and bad debt. Lack of standardization in the definition or measurement of charity care makes it difficult to differentiate between these two types of uncompensated care (Hellinger 2009; McGregor 2007; Vladeck 2006). Uncompensated care measures reported in the OSHPD Annual Disclosure Reports reflect charges. These measures are deflated to reflect cost using the cost-to-charge ratio as defined by OSHPD. All uncompensated care values are converted to 2006 dollars using the Consumer Price Index. To account for large differences in the level of uncompensated care provided by hospitals of different size and ownership types, the focus of the analysis is on the growth rate of uncompensated care across hospitals (that is, the first-differences of the natural log of charity plus bad debt per day in the hospital’s reporting period).
To assess the extent to which the burden of complying with minimum nurse staffing regulations affected provision of uncompensated care, hospitals were divided into quartiles based on their staffing levels before January 2002 when draft regulations were issued. Controlling for other factors affecting uncompensated care, changes in the growth rate of uncompensated care in the three lowest staffing quartiles relative to the quartile of hospitals with the highest staffing level are estimated. To the extent that hospitals in the highest pre-regulation staffing quartile were also forced to increase staffing to comply with the regulations, the estimates will underestimate the potential impact of the regulations on uncompensated care; evidence is provided on this issue below. An analysis that incorporated data on hospitals from other states that were not affected by the California staffing regulations could potentially address this issue; however, uncompensated care data from other sources such as Medicare cost reports were deemed to be more inconsistent and of inferior quality compared to OSHPD data so that it was preferable to rely on California data alone.
OSHPD data on productive hours of licensed nurses by type of patient care unit are used to construct an index of the burden of minimum staffing regulations. The nurse staffing level on each type of patient care unit to which the legislation applies is measured by nurse hours per patient day (HPPD), where a 1:6 nurse to patient ratio would require at least 4.0 HPPD and a 1:5 nurse to patient ratio would require at least 4.8 HPPD. Under AB394, different ratios applied to different units (e.g., a 1:4 ratio, or a minimum of 6 HPPD, for Pediatric units) and at different points in time, at least for medical-surgical units. Equation (1) shows the measure of the change in staffing level induced by the staffing regulations at hospital i during cost reporting period r.
| (1) |
The “net surplus” reflects the difference between HPPD in cost center c in the pre-regulation period (cost reports with end dates on or prior to December 31, 2001) and the minimum HPPD implied by the staffing regulation during the cost reporting period (τc,r), summed over cost centers subject to the nurse staffing regulations. Where a cost reporting period spanned a period of time with different minimum HPPD, (1) is calculated using a weighted average of the minimum HPPD values, the weights equal to the proportion of days in the cost reporting period for which the particular HPPD value was applicable.
Note that available staffing data on productive hours only indirectly measure compliance with patient to nurse staffing regulations. First, the OSHPD productive hours include all personnel in a job classification, some of whom may not have direct patient care assignments. Second, staffing regulations apply to nursing units on a 24-hour continuous basis, while the OSHPD productive hours reflect an average staffing level in a reporting period. As a simple example, a unit with eight patients and 32 nurse productive hours in a day might appear to be in compliance as 32 hours divided by eight patients equals 4 HPPD. But if the unit had three shifts per day where two nurses worked during one shift while only one nurse worked in the other two shifts, then the unit meets the minimum staffing requirement on average but is out of compliance 16 hours a day. Hence, the net surplus measure in (1) generally underestimates the change in the level of staffing required by the minimum nurse to patient ratios; hospitals with a net surplus of zero or larger should be expected to have to add staffing to come into compliance. The net surplus reflects the change in nurse staffing induced by the regulations, but does not measure it on a ratio scale.
We separate hospitals into staffing level quartiles based on the percentage net surplus equal to the ratio of the mean of net surplus over a hospital’s post-regulation cost reports divided by HPPD in the pre-regulation period, and multiplied by 100. Using the percentage net surplus provides a more appropriate metric for measuring the impact of the regulations on hospitals of different size. A given net surplus expressed as HPPD might represent vastly different total nurse hours for a small versus large hospital. Expressing net surplus in terms of total hours would also be problematic because a given number of total hours might represent a huge burden for a small hospital or a relatively small burden for a larger hospital. The percentage net surplus avoids these problems by scaling the net surplus by HPPD in the pre-regulation period.
To control for differences in uncompensated care provision by hospitals of different ownership types, we include a dummy variable indicating for-profit, county or district ownership (with not-for-profit hospitals the reference group).2 We allow ownership to moderate the effect of AB394 on growth in uncompensated care by interacting ownership with staffing quartile and our policy variable. We also control for hospital and market characteristics likely to influence supply and demand for uncompensated care. We control for the effect of teaching mission by including the number of residents per bed. Hospital size and system membership are controlled for using the natural log of hospital staffed beds and a dummy variable indicating system membership, respectively. We control for market characteristics shown to influence the provision of uncompensated care by including the Herfindahl Index; the number of HMOs in the HSA; and HMO penetration in the HSA.
During the period of our study, the state of California required hospitals to survey their facilities and report on seismic vulnerabilities. By January 2008 or, if an extension was granted, January 2013, hospitals were required to retrofit or stop making use of the buildings most at risk of collapse. Costs of retrofitting or replacing buildings were often substantial and would be expected to impact the provision of uncompensated care; thus we include control variables for differences in seismic risk. As in (Chang & Jacobson, 2008), we based measurement of seismic risk on the peak ground acceleration expected to occur with a 10% probability over a fifty year period.3 Peak ground acceleration at each hospital’s latitude and longitude was calculated using 2002 data from the U.S. Geological Survey (U.S. Geological Survey, 2002). We include dummy variables for the highest and second highest quartile of seismic risk based on the peak ground acceleration values.
To control for population and market characteristics likely to affect demand for uncompensated care, we include variables measuring the overall demand for hospital services in the market and measures of the socioeconomic status of the population. The natural log of inpatient days per 1,000 population in the HSA controls for geographic variation in hospital use. While ideally we would be able to include the rate of uninsured by county to control for demand for uncompensated care, we could not identify a source of complete data on the rate of insurance over the study period. The US Census Bureau’s Small Area Health Insurance Estimates program began providing annual estimates of the percent uninsured by county only in 2005. The California Health Interview Survey program provides estimates on the proportion uninsured in California counties, but the survey is biennial and began only in 2001. As an alternative, we include the natural log of per capita income, the percent of the population older than 65 years, and the unemployment rate to control for the demand for uncompensated care. Finally, variables reflecting each year in the study period are included to control for state or national trends or policies affecting uncompensated care over time for all hospitals in the study sample.
In this analysis the time unit is the hospital cost reporting period rather than calendar year since uncompensated care and nurse staffing levels are measured in these intervals. A consequence is that all variables obtained from sources other than the cost report are matched to a hospital according to the dates of the cost reports, with the value of the variable being a weighted average of the calendar year value with the weight equal to the number of days in the cost report falling in a given calendar year. For example, instead of the usual time dummy variables to control for common time effects, we include quasi-dummy variables taking on values of 0 and 1 for hospitals with cost reports corresponding to calendar years but taking on values equal to the proportion of cost report period days falling in a calendar year for other hospitals.
To test whether there has been a change in the growth rate of uncompensated care that could plausibly be attributed to the impact of staffing regulations, we estimate a difference-indifference model comparing hospitals in the three lowest pre-regulation staffing level quartiles to hospitals in the quartile with highest pre-regulation staffing level (which was least affected by staffing regulations). We include parameters to estimate the differences from the highest staffing level quartile in both the transition to regulatory compliance (from announcement of draft regulations in January 2002 to December 2003) and in the initial years of regulation (2004–2006). Along with the hospital, market, and population characteristics described above, the specification includes a full set of ownership-quartile interactions allowing for differences in the growth rate of uncompensated care for each ownership type (county, district, for-profit, and not-for-profit) in each staffing quartile in the pre-regulation, transition to regulation, and post-regulation periods.
RESULTS
Table 1 provides descriptive statistics for all study variables by staffing quartile. The mean of the ratio of uncompensated care to total operating expenses (the uncompensated care ratio) over the study period was similar across the four staffing quartiles at five to six percent, as was the mean proportional growth rate of uncompensated care. Hospitals in the four staffing quartiles differed significantly in terms of ownership. The lowest staffing quartile was more heavily weighted toward county and for-profit hospitals while the proportion of not-for-profit hospitals was greatest in the highest staffing quartile. In terms of market and population characteristics, the quartiles differed significantly on level of competition, number of HMOs and the percent of the population over age 65. The Herfindahl Index increased from the lowest to highest staffing quartiles while the number of HMOs fell suggesting that hospitals in the highest staffing quartiles were in less competitive markets. Hospitals in the highest staffing quartiles were also located in areas with a greater percentage of the population over age 65.
Table 1.
Descriptive Statistics, by Staffing Quartile
| Variable | Staffing Quartilea |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | F statisticb | |
| UC ratio | 0.06 | 0.08 | 0.06 | 0.05 | 0.05 | 0.06 | 0.05 | 0.04 | 0.53 |
| Proportional growth rate of UC | 0.09 | 0.30 | 0.07 | 0.32 | 0.07 | 0.31 | 0.08 | 0.25 | 0.61 |
| Nurse staffing level | |||||||||
| Nurse HPPD | 6.63 | 1.21 | 7.21 | 1.36 | 7.75 | 1.32 | 8.62 | 1.37 | 43.32*** |
| RN HPPD | 5.94 | 1.30 | 6.52 | 1.48 | 7.09 | 1.49 | 7.85 | 1.57 | 27.58*** |
| Percent Net surplus/shortfall | 2.4 | 12.7 | 17.9 | 3.0 | 27.2 | 2.6 | 40.8 | 6.7 | 277.90*** |
| Hospital characteristics | |||||||||
| County | 0.13 | 0.33 | 0.09 | 0.28 | 0.04 | 0.19 | 0.05 | 0.23 | 1.20 |
| District | 0.05 | 0.22 | 0.09 | 0.29 | 0.12 | 0.33 | 0.06 | 0.24 | 0.75 |
| For-Profit | 0.40 | 0.49 | 0.21 | 0.41 | 0.19 | 0.39 | 0.10 | 0.31 | 5.38** |
| Not For-Profit | 0.42 | 0.49 | 0.61 | 0.49 | 0.65 | 0.48 | 0.78 | 0.41 | 6.08*** |
| Number of residents per bed | 0.08 | 0.22 | 0.06 | 0.14 | 0.08 | 0.25 | 0.10 | 0.19 | 0.64 |
| Number of beds | 192 | 140 | 223 | 180 | 205 | 116 | 215 | 165 | 0.45 |
| System affiliation | 0.69 | 0.44 | 0.72 | 0.44 | 0.77 | 0.41 | 0.77 | 0.41 | 0.57 |
| Highest quartile seismic risk | 0.31 | 0.46 | 0.23 | 0.42 | 0.25 | 0.43 | 0.19 | 0.39 | 0.76 |
| 2nd highest quartile seismic risk | 0.30 | 0.46 | 0.24 | 0.43 | 0.23 | 0.42 | 0.26 | 0.44 | 0.31 |
| Market characteristics | |||||||||
| Herfindahl Index | 0.07 | 0.08 | 0.10 | 0.13 | 0.12 | 0.12 | 0.12 | 0.11 | 3.58* |
| IPDs per 1,000 population | 1,042 | 284 | 999 | 317 | 1,104 | 360 | 1,116 | 392 | 1.44 |
| Number of HMOs | 13.6 | 3.9 | 12.7 | 3.7 | 11.5 | 4.1 | 11.0 | 3.8 | 5.85*** |
| HMO penetration | 48.9 | 9.1 | 48.8 | 11.0 | 47.6 | 15.0 | 48.6 | 14.9 | 0.10 |
| Population characteristics | |||||||||
| Unemployment rate | 6.0 | 1.5 | 6.4 | 2.7 | 5.8 | 1.9 | 5.6 | 1.6 | 1.53 |
| Percent over 65 | 10.6 | 1.8 | 10.5 | 1.6 | 11.3 | 2.1 | 11.3 | 2.0 | 2.71* |
| Per capita income (thousands of 2006 dollars) | 35.0 | 7.3 | 35.7 | 9.7 | 39.1 | 11.5 | 38.6 | 11.4 | 2.57 |
| Number of Hospitals | 57 | 56 | 56 | 58 | |||||
| Number of Observations | 352 | 358 | 359 | 382 | |||||
Staffing quartile 1 contains the hospitals that, relative to the staffing regulations, had the largest percent staffing shortfall or smallest staffing surplus.
F statistic for test if null hypothesis of equality of means across the four staffing quartiles (degrees of freedom 3 and 1,451). F-statistics are calculated allowing for non-independence of observations within hospitals.
indicates the F statistic is significant at the 0.05 level,
significant at the 0.01 level, and
significant at the 0.001 level.
Staffing quartiles are defined using the estimate of percentage net surplus described above; the first quartile reflects the largest change in staffing required to comply with regulations. The minimum and maximum values for quartile 1 are −66.6 percent and 12.8 percent, respectively (i.e., at least one hospital was 66.6% below the staffing hours that would have been required under the minimum staffing regulations and at least one hospital was 12.8% above). The upper and lower limits for the remaining quartiles are as follows: quartile 2: 12.9%, 22.7%; quartile 3: 22.8%, 32.0%; and quartile 4: 32.2%, 58.8%. As discussed previously, however, these estimates likely understate actual hours needed to come into compliance because of the continuous application of the regulations over a 24-hour period. Consistent with previous research, nurse staffing levels differed by ownership with not-for-profit hospitals reporting the highest total nursing and RN hours per patient day and for-profit hospitals reporting the lowest (Mark & Harless, 2007; Spetz et al., 2009) (results not shown).
Table 2 provides descriptive statistics on nurse hours per patient day and uncompensated care by staffing quartile prior to the passage of minimum nurse staffing legislation, during the transition period after passage but before implementation, and post-implementation. Mean nurse hours per patient day and mean RN hours per patient day increased significantly during both the transition and post-regulation periods for hospitals in the lowest three staffing quartiles. RN hours per patient day also increased significantly during the post-regulation period for hospitals in the highest staffing quartile, but the mean increase was only one-third the size of the increase in the other three staffing quartiles. The mean increase in RN hours among hospitals in the lowest staffing quartile was similar to the increase in the second quartile suggesting the hospitals in the lowest quartile may have come into compliance by hiring more LVNs. Hospitals in the third staffing quartile had the highest mean increase in RN hours per patient day in both the transition and post-regulation periods.
Table 2.
Mean and Standard Error of Mean of Nurse Hours Per Patient Day and Uncompensated Care Before, During the Transition to, and After Staffing Regulations, By Staffing Quartile.a
| Staffing Quartileb | Pre-Regulation | Transition | Post-Regulation | ||||
|---|---|---|---|---|---|---|---|
| Mean | S.E. | Mean | S.E. | Mean | S.E. | ||
| Nurse HPPD | 1 | 5.92 | 0.09 | 6.37 | 0.12 | 7.27 | 0.15 |
| 2 | 6.61 | 0.09 | 6.93 | 0.16 | 7.93 | 0.16 | |
| 3 | 7.15 | 0.09 | 7.55 | 0.14 | 8.35 | 0.17 | |
| 4 | 8.58 | 0.13 | 8.35 | 0.15 | 8.82 | 0.19 | |
| Difference from Pre-Regulation Period | 1 | 0.47*** | 0.092 | 1.41*** | 0.113 | ||
| 2 | 0.35** | 0.126 | 1.31*** | 0.141 | |||
| 3 | 0.39*** | 0.103 | 1.18*** | 0.140 | |||
| 4 | −0.25 | 0.133 | 0.22 | 0.194 | |||
| RN HPPD | 1 | 5.35 | 0.11 | 5.69 | 0.14 | 6.48 | 0.18 |
| 2 | 5.96 | 0.12 | 6.27 | 0.18 | 7.17 | 0.18 | |
| 3 | 6.37 | 0.12 | 6.89 | 0.17 | 7.77 | 0.19 | |
| 4 | 7.66 | 0.16 | 7.60 | 0.19 | 8.11 | 0.22 | |
| Difference from Pre-Regulation Period | 1 | 0.38*** | 0.01 | 1.20*** | 0.12 | ||
| 2 | 0.33** | 0.12 | 1.20*** | 0.14 | |||
| 3 | 0.48*** | 0.12 | 1.34*** | 0.15 | |||
| 4 | −0.09 | 0.13 | 0.44* | 0.20 | |||
| UC Ratio | 1 | 0.067 | 0.012 | 0.062 | 0.010 | 0.061 | 0.009 |
| 2 | 0.059 | 0.007 | 0.053 | 0.006 | 0.059 | 0.006 | |
| 3 | 0.047 | 0.007 | 0.050 | 0.008 | 0.049 | 0.007 | |
| 4 | 0.052 | 0.005 | 0.051 | 0.005 | 0.057 | 0.005 | |
| Difference from Pre-Regulation Period | 1 | −0.002 | 0.003 | 0.001 | 0.004 | ||
| 2 | −0.001 | 0.002 | 0.004 | 0.002 | |||
| 3 | 0.003 | 0.002 | 0.005* | 0.002 | |||
| 4 | 0.001 | 0.002 | 0.006** | 0.002 | |||
| UC Growth Rate | 1 | 0.132 | 0.027 | 0.093 | 0.020 | 0.059 | 0.018 |
| 2 | 0.050 | 0.025 | 0.105 | 0.031 | 0.062 | 0.022 | |
| 3 | 0.073 | 0.023 | 0.092 | 0.028 | 0.063 | 0.023 | |
| 4 | 0.051 | 0.017 | 0.103 | 0.020 | 0.099 | 0.017 | |
| Difference from Pre-Regulation Period | 1 | −0.083* | 0.040 | −0.113** | 0.036 | ||
| 2 | 0.016 | 0.047 | − 0.011 | 0.039 | |||
| 3 | −0.009 | 0.047 | −0.018 | 0.039 | |||
| 4 | 0.056 | 0.035 | 0.040 | 0.027 | |||
Statistical significance indicated for differences from pre-regulation period;
significant at the 0.05 level,
significant at the 0.01 level, and
significant at the 0.001 level.
Staffing quartile 1 contains the hospitals that, relative to the staffing regulations, had the largest percent staffing shortfall or smallest staffing surplus.
The mean difference in the uncompensated care ratio from the pre-regulation to the post-regulation period was positive for hospitals in all staffing quartiles; however, the mean difference was much higher in the third and fourth staffing quartiles as compared to the first. In contrast, the mean differences in the growth rate of uncompensated care from the pre-regulation to the transition and post-regulation periods were negative and statistically significant for hospitals in the first staffing quartile. Mean differences in the growth rate of uncompensated care from the pre-regulation to the post-regulation period were also negative for hospitals in the second and third staffing quartiles, but the differences were smaller than for hospitals in the first staffing quartile. Although not statistically significant, the mean differences in the growth rate of uncompensated care during both the transition and post-regulation periods were positive for hospitals in the highest staffing quartile.
Table 3 reports marginal effects of the minimum nurse staffing legislation in the transition and post-regulation periods on the growth rate of uncompensated care by hospital ownership, controlling for hospital, market and population characteristics (results of the complete regression analysis are available upon request to the lead author). During the transition period, the growth rates in uncompensated care were lower for county and for-profit hospitals in the first, second and third staffing quartiles as compared to county and for-profit hospitals with the highest pre-regulation nurse staffing levels, but the estimates were statistically significant only in the first and third staffing quartiles. County hospitals with the lowest pre-regulation staffing levels had growth rates in uncompensated care 14 percentage points lower than that predicted for county hospitals with the highest pre-regulation staffing levels, and those in the third staffing quartile had growth rates 19 percentage points lower. Growth rates among county hospitals in the second staffing quartile were also estimated to be 14 percentage points lower, but the standard error of this estimate was higher. Like county hospitals, growth rates in uncompensated care for for-profit hospitals in the lowest and third staffing quartiles were 16.1 and 22.6 percentage points lower, respectively, than hospitals in the highest staffing quartile.
Table 3.
Estimates of the Change in the Growth Rate of Uncompensated Care in the Transition to and Initial Period of Minimum Nurse Staffing Regulations Relative to Quartile of Hospitals with the Highest Pre-Regulation Nurse Staffing Levelsa,b
| Period | Staffing Quartileb,c | County | District | For-Profit | Not For-Profit |
|---|---|---|---|---|---|
| Transition | 1 | −0.138* (0.060) | 0.028 (0.093) | −0.161* (0.072) | −0.073 (0.089) |
| 2 | −0.136 (0.102) | 0.051 (0.134) | −0.021 (0.182) | 0.021 (0.054) | |
| 3 | −0.192*** (0.053) | 0.147 (0.178) | −0.226* (0.104) | 0.009 (0.065) | |
| Post-Regulation | 1 | −0.022 (0.046) | 0.098 (0.084) | −0.250*** (0.043) | −0.049 (0.064) |
| 2 | −0.060 (0.134) | −0.022 (0.121) | −0.088 (0.110) | −0.023 (0.046) | |
| 3 | −0.158 (0.088) | −0.071 (0.128) | −0.195* (0.089) | −0.015 (0.042) |
These estimates are obtained in a regression which also contains dummy variables for ownership type, a full set of staffing quartile-ownership dummy interactions, pseudo-dummy variables for year, dummy variables for hospitals in the highest and second highest quartile of seismic risk, number of residents per bed, natural log of the number of acute care beds, a dummy variable for system membership, Herfindahl Index, natural log of inpatient days per 1,000 population, number of HMOs, HMO penetration, natural log of per capital income, percentage of population over 65, and the unemployment rate.
Standard errors (in parentheses) beneath the estimates are adjusted for non-independence of observations within hospitals.
Staffing quartile 1 contains the hospitals that, relative to the staffing regulations, had the largest percent staffing shortfall or smallest staffing surplus.
No estimates are reported for the fourth quartile because estimates represent, by ownership type, differences from the quartile of hospitals with the highest pre-regulation nurse staffing levels.
Significant at the 0.05 level.
Significant at the 0.001 level
In the post-regulation period, hospitals in the lower three staffing quartiles had lower rates of growth in uncompensated care than hospitals in the highest staffing quartile for all ownership types except district; however, results were statistically significant only for for-profit hospitals in the first and third staffing quartiles. For-profit hospitals with the lowest pre-regulation nurse staffing levels had growth rates in uncompensated care that were 25 percentage points lower than for-profit hospitals with the highest pre-regulation nurse staffing. Similarly, for-profit hospitals in the third quartile had growth rates 19.5 percentage points lower than for-profit hospitals in the highest staffing quartile.
DISCUSSION
Findings from this study only partially support the hypothesis that hospitals that needed to increase nurse staffing hours the most in order to reach compliance with the minimum nurse staffing regulations reduced the amount of uncompensated care that they provide. As hypothesized, reductions in growth rates of uncompensated care were lower among hospitals that reported the lowest pre-regulation staffing levels; however, reductions in growth rates of uncompensated care were also found for hospitals in the third staffing quartile. Statistically significant results were limited to for-profit hospitals in both the transition and post-regulation periods and county hospitals in the transition period. The lack of statistically significant findings among hospitals in the second staffing quartile may reflect a lack of precision in these estimates due to a different distribution of hospital ownership including smaller numbers of county and for-profit hospitals in this quartile. Alternatively, these results may reflect different strategies for meeting the minimum nurse staffing requirements, for example, alterations to occupational mix to lower the cost of meeting the nurse staffing requirements. Descriptive findings revealed that in the post-regulation period staffing quartiles 1 and 2 had the largest increase in licensed nurse HPPD, but staffing quartile 3 had the largest increase in RN HPPD, thus indicating that staffing quartiles 1 and 2 relied to a greater extent on LVNs to meet the regulatory requirements.
The lack of statistically significant findings for not-for-profit and district hospitals suggests that these hospitals may have found ways of financing increases in nurse staffing costs through reserves, charitable donations, price increases or other reductions in operating costs in order to protect levels of uncompensated care. Increasing focus on not-for-profit hospitals’ accountability for their tax-exemptions may have motivated these hospitals to protect uncompensated care, a publicly visible community benefit activity.
Consistent with an objective to maximize profit for owners, for-profit hospitals in the first and third staffing quartiles displayed the greatest reductions in uncompensated care growth rates both during the transition and post-regulation periods. County hospitals had similar reductions in growth rates in uncompensated care during the transition period; however, these results were not statistically significant in the post-regulation period.
Although limited, findings from this study provide some support for public concerns that financial pressure on hospitals may challenge access to free and reduced price care for indigent patients. Since hospitals have historically used operating earnings to help finance uncompensated care (Hadley & Holahan, 2003), policy actions that threaten hospital profitability may force trade-offs between compliance with regulations and community benefit, especially among for-profit hospitals that must show a return for shareholders and resource-constrained county hospitals that have traditionally served a high number of indigent patients (Conway, Tamara, Zhu, Volpp, & Sochalski, 2008). Although reductions in uncompensated care growth rates did not persist in the post-regulation period for county hospitals, even short-term restrictions on uncompensated services by these safety-net hospitals could have a substantial detrimental effect on access for already vulnerable patients.
The finding of more persistent reductions in uncompensated care growth rates among for-profit hospitals raises the question of whether the reductions reflect declining access to care for vulnerable patients or a transfer of uncompensated care to neighboring hospitals. Data limitations precluded us from answering this question definitively; however, we did examine growth of uncompensated care over the study period in two HSAs with different juxtapositions of for-profit hospitals in the first and fourth staffing quartiles. The closest match included two HSAs, each with two hospitals; the first had a staffing quartile 1 for-profit hospital and a staffing quartile 4 not-for-profit hospital, while the second had a staffing quartile 4 for-profit hospital and a staffing quartile 2 not-for-profit hospital. The HSA-wide level of uncompensated care was similar in 2000, but the growth rates of uncompensated care were drastically different. In 2006, uncompensated care was only 5% higher than in 2000 in the first HSA while it was 130% higher in the second HSA. Hence, this example suggests declining access rather than a transfer of uncompensated care to neighboring hospitals. However, this is just one example using the closest match in our sample based on ownership type, staffing quartiles, and total uncompensated care in 2000. The example ignores all other differences between the two HSAs and thus should be considered cautiously. It is nonetheless suggestive of an approach for future studies that would consider effects on uncompensated care at the market level, including total amounts of care and possible shifting of uncompensated services among hospitals.
Findings from this study are particularly salient at a time when minimum nurse staffing legislation is being considered at both the state and federal levels (Keeler & Cramer, 2007). Such legislation, intended to improve quality of care for patients and quality of life for nurses, may have unintended consequences for uninsured patients. This does not imply that minimum nurse staffing legislation and other quality improvement policies should not be considered. If these policies improve quality, safety and patient outcomes then the costs may be well-spent. The findings suggest, however, that legislators should consider whether there is a need to monitor access to uncompensated services for uninsured patients as hospitals transition to the new requirements. Reporting of uncompensated care may help identify any reductions in access to hospital services, transfers of uninsured patients to alternative settings, or needs for temporary funding mechanisms to support hospitals as they transition to the new requirements. Hospitals need time to strengthen fundraising programs, renegotiate reimbursement contracts, reengineer processes to cut operating costs, and/or reallocate funds to finance cost increases. Temporary funding mechanisms may be particularly important for county hospitals that provide the greatest proportion of uncompensated services, or for hospitals located in markets with substantial nursing shortages regardless of ownership.
This study has several limitations that should be noted. First, data limitations prevented ideal measurement of several important variables. The measure of nurse staffing surplus does not reflect the actual hours required for a hospital to come into compliance with the minimum nurse staffing regulations. The measure of staffing surplus was used to construct quartiles to indicate the extent of burden of staffing regulations on different hospitals; however, it likely understates hospitals’ needs to increase actual direct-care nursing hours. Similarly, the measure of demand for uncompensated care related to insurance status does not reflect the actual proportion of the population in the vicinity of the hospital without health insurance. Although we control for various population characteristics (per capita income, percent over 65, and the unemployment rate), this controls for demand for uncompensated care only to the extent that the measured population characteristics are correlated with insurance status. Lastly, the measure of growth rate in uncompensated care does not reflect the overall amount of uncompensated care provided by hospitals in California nor does it differentiate between the number of patients served and the intensity of services. It is possible lower growth rates in uncompensated care among hospitals in the lower staffing quartiles were partially offset by a redistribution of uncompensated care to hospitals less affected by the legislation. While such a phenomenon would theoretically maintain access, it could create financial pressure for hospitals experiencing growth in uncompensated services, as well as time and travel barriers for patients.
A second limitation is that this study was limited to hospitals in California. There is no control for national trends in uncompensated care. Nevertheless, the significance of findings among hospitals in the lower quartiles of nurse staffing shortfall/surplus combined with the expected negative sign on the majority of coefficients gives us confidence that the results of this study are not spurious.
Third, in addition to the nurse staffing legislation, other changes in California occurred during the study period that could have affected uncompensated care. Most importantly, in late 2005, California begin enacting a series of changes in Medicaid funding that, along with new changes in Medicare funding, would potentially decrease government transfers to safety net hospitals. Time trend variables were included to control for the effects of omitted elements such as reimbursement; however, the effects of omitted variables that could have affected nurse staffing and uncompensated care may not have been fully captured.
Fourth, qualitative research has suggested that some hospitals had sufficient market power to negotiate reimbursement increases from private insurance companies, with the ratio legislation as a justification for higher payment (Spetz et al., 2009). Since there is some descriptive evidence to suggest that hospitals in the top quartile of staffing prior to the legislation may have had greater market power, our findings may reflect the negotiating power of these hospitals.
Although our findings did not show broad reductions in uncompensated care following the implementation of minimum nurse staffing legislation in California, apparent reductions among county and for-profit hospitals suggest the need for caution when considering minimum nurse staffing legislation and other quality improvement policies that directly increase operating expenses, and therefore threaten hospital profitability. Future research should explore the effects of minimum nurse staffing legislation on broader community benefit activities including education and outreach. Qualitative studies are also needed to understand the ways that hospital executives obtain and allocate resources in the face of cost-generating policy mandates.
Footnotes
In the short-term, care to uninsured patients is likely more fungible than service lines or beds making it vulnerable to reductions in hospital resources. Over the longer term, it is less clear that uncompensated care would be the only target for cost-cutting, especially among not-for-profit hospitals that are accountable to their communities and must justify tax-exemption.
District hospitals reflect those under local government control receiving funding from a taxing authority. Although both public, we include separate dummy variables for district and county ownership because data on uncompensated care as a proportion of total operating expenses suggest that hospitals under the two ownership types behave differently. Specifically, the mean ratio of uncompensated care to total operating expenses for county hospitals over the study period is 0.22 versus 0.05 for district hospitals.
For a more detailed explanation, see for example, http://www.consrv.ca.gov/cgs/rghm/psha/Pages/pga.aspx.
Contributor Information
Kristin L. Reiter, Email: reiter@email.unc.edu, Department of Health Policy and Management, The University of North Carolina at Chapel Hill, 1104H McGavran-Greenberg Hall, CB # 7411, Chapel Hill, NC 27599-7411, Phone: (919) 843-8619
David W. Harless, Email: dwharles@vcu.edu, Department of Economics, Virginia Commonwealth University
George H. Pink, Email: gpink@email.unc.edu, Department of Health Policy and Management, The University of North Carolina at Chapel Hill
Joanne Spetz, Email: jojo@thecenter.ucsf.edu, School of Nursing, University of California, San Francisco
Barbara Mark, Email: bmark@email.unc.edu, School of Nursing, The University of North Carolina at Chapel Hill.
References
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout and job dissatisfaction. Journal of the American Medical Association. 2002 Oct 23/30;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Antwi YA, Gaynor M, Vogt WB. NBER Working Paper Series. Cambridge: National Bureau of Economic Research; 2009. A Bargain at Twice the Price? California Hospital Prices in the New Millenium; pp. 1–23. [Google Scholar]
- Bazzoli GJ, Lindrooth RC, Kang R, Hasnain-Wynia R. The influence of health policy and market factors on the hospital safety net. Health Services Research. 2006;41(4 Pt 1):1159–1180. doi: 10.1111/j.1475-6773.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang T, Jacobson M. What is the mission of a not-for-profit hospital? Evidence from California’s seismic retrofit mandate. Mimeo. 2008 November 9; [Google Scholar]
- Conway PH, Tamara R, Zhu J, Volpp K, Sochalski J. Nurse staffing ratios: trends and policy implications for hospitalists and the safety net. Journal of Hospital Medicine. 2008;3(3):193–199. doi: 10.1002/jhm.314. [DOI] [PubMed] [Google Scholar]
- Davidoff AJ, LoSasso AT, Bazzoli GJ, Zuckerman S. The effect of changing state health policy on hospital uncompensated care. Inquiry. 2000;37(3):253–267. [PubMed] [Google Scholar]
- Donaldson N, Bolton LB, Aydin C, Brown D, Elashoff JD, Sandhu M. Impact of California’s licensed nurse-patient ratios on unit-level nurse staffing and patient outcomes. Policy, Politics, & Nursing Practice. 2005;6(3):198–210. doi: 10.1177/1527154405280107. [DOI] [PubMed] [Google Scholar]
- Frank RG, Salkever DS. The supply of charity services by nonprofit hospitals: motives and market structure. Rand Journal of Economics. 1991;22(3):430–445. [PubMed] [Google Scholar]
- Frank RG, Salkever DS, Mullann F. Hospital ownership and the care of uninsured and Medicaid patients: findings from the National Hospital Discharge Survey 1979–1984. Health Policy. 1990;14(1):1–11. doi: 10.1016/0168-8510(90)90294-n. [DOI] [PubMed] [Google Scholar]
- Government Accounting Office. Nursing Workforce: Emerging Shortages Due to Multiple Factors. Washington DC: 2001. [Google Scholar]
- Gray BH, Schlesinger M. Charitable expectations of nonprofit hospitals: lessons from Maryland. Health Affairs (Millwood), Web Exclusive. 2009:w809–w821. doi: 10.1377/hlthaff.28.5.w809. [DOI] [PubMed] [Google Scholar]
- Hadley J, Feder J. Hospital cost shifting and care for the uninsured. Health Affairs (Millwood) 1985;4(3):67–80. doi: 10.1377/hlthaff.4.3.67. [DOI] [PubMed] [Google Scholar]
- Hadley J, Holahan J. How much medical care do the uninsured use, and who pays for it? Health Affairs (Millwood), Supplemental Web Exclusives. 2003:W3-66–81. doi: 10.1377/hlthaff.w3.66. [DOI] [PubMed] [Google Scholar]
- Hoerger TJ. ‘Profit’ variability in for-profit and not-for-profit hospitals. Journal of Health Economics. 1991;10(3):259–289. doi: 10.1016/0167-6296(91)90030-q. [DOI] [PubMed] [Google Scholar]
- Hsieh H, Clement DG, Bazzoli G. Impacts of market and organizational characteristics on hospital efficiency and uncompensated care. Health Care Management Review. 2010;35(1):77–87. doi: 10.1097/HMR.0b013e3181c09956. [DOI] [PubMed] [Google Scholar]
- Joseph AM. The impact of nursing on patient and organizational outcomes. Nursing Economics. 2007;25(1):30–34. 33. [PubMed] [Google Scholar]
- Kaestner R, Guardado J. Medicare reimbursement, nurse staffing, and patient outcomes. Journal of Health Economics. 2008;27(2):339–361. doi: 10.1016/j.jhealeco.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Medical Care. 2007;45(12):1195–1204. doi: 10.1097/MLR.0b013e3181468ca3. [DOI] [PubMed] [Google Scholar]
- Keeler HJ, Cramer ME. A policy analysis of federal registered nurses safe staffing legislation. Journal of Nursing Administration. 2007;37(7–8):350–356. doi: 10.1097/01.nna.0000285117.45442.dd. [DOI] [PubMed] [Google Scholar]
- Kim TH, McCue M, Thompson JM. The relationship of financial and mission factors to the level of uncompensated care provided in California hospitals. Journal of Healthcare Management. 2009;54(6):383–402. [PubMed] [Google Scholar]
- Lo Sasso AT, Seamster DG. How federal and state policies affected hospital uncompensated care provision in the 1990s. Medical Care Research and Review. 2007;64(6):731–744. doi: 10.1177/1077558707305940. [DOI] [PubMed] [Google Scholar]
- Makuc DM, Haglund B, Ingram DD, Kleinman JC, Feldman JJ. Health service areas for the United States. Vital Health Statistics. 1991;2(112):1–102. [PubMed] [Google Scholar]
- Mann JM, Melnick GA, Bamezai A, Zwanziger J. A profile of uncompensated hospital care, 1983–1995. Health Affairs (Millwood) 1997;16(4):223–232. doi: 10.1377/hlthaff.16.4.223. [DOI] [PubMed] [Google Scholar]
- Mark BA, Harless DW. Nurse staffing, mortality, and length of stay in for-profit and not-for-profit hospitals. Inquiry. 2007;44(2):167–186. doi: 10.5034/inquiryjrnl_44.2.167. [DOI] [PubMed] [Google Scholar]
- Mark BA, Harless DW, Berman WF. Nurse staffing and adverse events in hospitalized children. Policy, Politics, & Nursing Practice. 2007;8(2):83–92. doi: 10.1177/1527154407303499. [DOI] [PubMed] [Google Scholar]
- Mark BA, Harless DW, McCue M. The impact of HMO penetration on the relationship between nurse staffing and quality. Health Economics. 2005;14(7):737–753. doi: 10.1002/hec.988. [DOI] [PubMed] [Google Scholar]
- Mark BA, Harless DW, Spetz J. California’s minimum-nurse-staffing legislation and nurses’ wages. Health Affairs (Millwood) 2009;28(2):w326–334. doi: 10.1377/hlthaff.28.2.w326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCue M, Mark BA, Harless DW. Nurse staffing, quality, and financial performance. Journal of Health Care Finance. 2003;29(4):54–76. [PubMed] [Google Scholar]
- Needleman J. Is what’s good for the patient good for the hospital? Aligning incentives and the business case for nursing. Policy, Politics, & Nursing Practice. 2008;9(2):80–87. doi: 10.1177/1527154408320047. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P. Nurse staffing and patient safety: current knowledge and implications for action. International Journal of Quality in Health Care. 2003;15(4):275–277. doi: 10.1093/intqhc/mzg051. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus P, Mattke S, Stewart M, Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002;346(22):1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse staffing in hospitals: is there a business case for quality? Health Affairs (Millwood) 2006;25(1):204–211. doi: 10.1377/hlthaff.25.1.204. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. Toward a Theory of Nonprofit Institutions: An Economic Model of a Hospital. American Economic Review. 1970;60(1):64–74. [Google Scholar]
- Rosko MD. The supply of uncompensated care in Pennsylvania hospitals: motives and financial consequences. Health Care Management Review. 2004;29(3):229–239. doi: 10.1097/00004010-200407000-00008. [DOI] [PubMed] [Google Scholar]
- Rothberg MB, Abraham I, Lindenauer PK, Rose DN. Improving nurse-to-patient staffing ratios as a cost-effective safety intervention. Medical Care. 2005;43(8):785–791. doi: 10.1097/01.mlr.0000170408.35854.fa. [DOI] [PubMed] [Google Scholar]
- Seago JA, Spetz J, Mitchell S. Nurse staffing and hospital ownership in California. Journal of Nursing Administration. 2004;34(5):228–237. doi: 10.1097/00005110-200405000-00006. [DOI] [PubMed] [Google Scholar]
- Spetz J. California’s minimum nurse-to-patient ratios: the first few months. Journal of Nursing Administration. 2004;34(12):571–578. doi: 10.1097/00005110-200412000-00007. [DOI] [PubMed] [Google Scholar]
- Spetz J, Chapman S, Herrera C, Kaiser J, Seago JA, Dower C. Assessing the Impact of California’s Nurse Staffing Ratios on Hospitals and Patient Care. Oakland, CA: California HealthCare Foundation; 2009. [Google Scholar]
- U.S. Geological Survey. 2002 Retrieved May 15, 2010, from http://earthquake.usgs.gov/hazards/products/conterminous/2002/data/
- Weiner SJ, VanGeest J, Abrams RI, Moswin A, Warnecke R. Managing the unmanaged: a case study of intra-institutional determinants of uncompensated care at healthcare institutions with differing ownership models. Medical Care. 2008;46(8):821–828. doi: 10.1097/MLR.0b013e318178eaf7. [DOI] [PubMed] [Google Scholar]