Abstract
Nephrogenic systemic fibrosis (NSF) was first described in 2000 as a scleromyxedema-like illness in patients on chronic hemodialysis. The relationship between NSF and gadolinium contrast during magnetic resonance imaging was postulated in 2006, and subsequently, virtually all published cases of NSF have had documented prior exposure to gadolinium-containing contrast agents. NSF has been reported in patients from a variety of ethnic backgrounds from America, Europe, Asia and Australia. Skin lesions may evolve into poorly demarcated thickened plaques that range from erythematous to hyperpigmented. With time, the skin becomes markedly indurated and tethered to the underlying fascia. Extracutaneous manifestations also occur. The diagnosis of NSF is based on the presence of characteristic clinical features in the setting of chronic kidney disease, and substantiated by skin histology. Differential diagnosis is with scleroderma, scleredema, scleromyxedema, graft-versus-host disease, etc. NSF has a relentlessly progressive course. While there is no consistently successful treatment for NSF, improving renal function seems to slow or arrest the progression of this condition. Because essentially all cases of NSF have developed following exposure to a gadolinium-containing contrast agent, prevention of this devastating condition involves the careful avoidance of administering these agents to individuals at risk.
Keywords: Nephrogenic systemic fibrosis, gadolinium contrast, magnetic resonance imaging
Introduction
Nephrogenic systemic fibrosis (NSF) was first described in 2000 as a scleromyxedema-like illness that presented with cutaneous fibrosis in patients on chronic hemodialysis.[1] NSF has, to date, been reported only in people with renal insufficiency. This condition was formerly known as nephrogenic fibrosing dermopathy as it was initially observed in, and thought to solely affect, the skin. However, it is now known that several organs such as liver, lungs, muscles and heart may be involved, reflecting the systemic nature of the disorder. The relationship between chronic kidney disease (CKD) and gadolinium contrast during MRI was postulated in 2006, and subsequently, virtually all published cases of NSF have had documented prior exposure to gadolinium-containing contrast agents.[2,3] Almost in all reported cases, patients have received hemodialysis, peritoneal dialysis or both, with peritoneal dialysis thought to confer a greater risk of the disorder than hemodialysis.[4–6]
Epidemiology
NSF is a rare condition, with over 335 cases identified in the NSF Registry.[7] NSF affects males and females in approximately equal numbers. Although NSF commonly affects middle-aged individuals, it has been confirmed in children and the elderly. No racial predilection has been observed, and NSF has been reported in patients from a variety of ethnic backgrounds from America, Europe, Asia and Australia.
Pathophysiology
Gadolinium (Gd), an element of the lanthanide series (atomic number, 64), is the chief component of virtually all contrast agents administered for magnetic resonance imaging (MRI). Gd is bound to polyamino-polycarboxylic ligands to exploit its superior imaging qualities, reduce toxicity and facilitate excretion by the kidneys. In patients with normal kidney function, gadolinium-based contrast agents (GBCAs), which include gadodiamide and gadopentetate dimeglumine, are considered safe because the bond between the toxic Gd atom and its ligand molecule is extremely strong, and because the GBCA molecule is excreted rapidly. There is a small risk that Gd atoms could dissociate from their carrier ligands; but if this occurred, it is postulated that Gd (which acts much like calcium atoms in the body) would likely bind to plasma phosphates and form insoluble molecules.[7]
The mechanism of NSF seems to involve Gd-induced activation of circulating fibrocytes and subsequent synthesis of hyaluronan.[8,9] This circulating fibrocyte is thought to leave the circulation and differentiate in the dermis into cells that functionally and histologically resemble normal dermal fibroblasts.[7] Fibroblasts derived from skin affected by nephrogenic systemic fibrosis have been shown to synthesize elevated levels of sulfated glycosaminoglycans, in particular hyaluronan, compared with normal control samples.[10] Following the administration of GBCA to individuals with CKD, Gd may be released from the ligands with which it is chelated. Once free of its chelate in the circulation, Gd then may equilibrate in the extracellular space and migrate into tissue. Within 12 to 24 hours after exposure to free Gd, monocytes and macrophages produce profibrotic cytokines, such as vascular endothelial growth factor and platelet-derived growth factor.[11] Increased transforming growth factor (TGF) b1 mRNA immunostaining has been detected in the involved skin and muscle of patients with NSF.[12] These profibrotic cytokines may then bind to their cognate receptors to stimulate production of collagen and other extracellular matrix proteins, resulting in fibrosis.
Erythropoietin is often administered in CKD to increase the output of red blood cells from the bone marrow. This hormone, through its ability to promote endothelial cell proliferation and augment fibrin-induced wound healing, could play a role in the pathogenesis of NSF.[13] Whether erythropoietin is directly related to the pathogenesis, or severe renal impairment merely sets the stage for NSF, remains unclear.[14]
Increased expression, activation, or concomitant activation and expression of transglutaminases in NSF have been documented, but their exact role in the pathogenesis is not established.[15] Other associations reported include thrombosis or coagulopathy, vascular procedures or vascular injury, and metabolic acidosis.[4,5,16–19]
For patients being considered for MRI, risk factors for NSF include advanced CKD (stages 4 and 5) and acute or chronic inflammatory renal insults. The US Food and Drug Administration (FDA) has updated its public health advisory to include patients with moderate renal insufficiency (CKD stage 3) in the list of those at risk of NSF.[20]
Clinical features
Skin lesions, which may develop over a period of days to several weeks, usually first appear on the distal legs and then extend proximally.[4–6,16,21] Occasionally, skin on the trunk may be involved, but facial skin is never affected. Patients may experience burning, itching or severe sharp pains in areas of involvement.[5,16,21] Early skin lesions may present as a pruritic erythematous rash appearing shortly after exposure to GBCA. This may evolve into poorly demarcated thickened plaques that range from erythematous to hyperpigmented and have an irregular leading edge, which has been termed ameboid.[22] Hypopigmented, flesh-colored or pink superficial macules or papules may develop on the distal upper extremities, which may later coalesce into scaly plaques.[23] With time, the skin becomes markedly indurated and tethered to the underlying fascia, either in focal linear bands or diffusely. The skin becomes shiny with dimpling around hair follicles, giving a peau d’orange texture.[5,21] The skin lesions are commonly symmetrical, with zones between the ankles and thighs most commonly involved, followed by involvement of the upper limbs between the wrist and upper arms.[7] Hand and foot swelling with blister-like lesions has also been reported.[7] Deep induration may develop over the upper arms, back or thighs, creating a “cobblestone”-like uneven texture.[23] Joint contractures secondary to decreased mobility of periarticular skin are a common sequela resulting in limited finger, elbow and knee extension. With relentless progression of the disease, activities of daily living are compromised and the patient becomes bedridden.
Extracutaneous manifestations of NSF also occur. Many patients with NSF have early scleral telangiectasia, followed by yellow scleral plaques nasal and temporal to the iris, which do not typically compromise vision.[4,6,16,19] Visceral fibrosis involving the heart, lungs, skeletal muscle and other organs has been found in patients with NSF.[5,21] Although often asymptomatic, visceral fibrosis may contribute to the development of cardiomyopathy, pulmonary hypertension and skeletal muscle weakness. Rapid, new-onset fluctuating hypertension of unknown cause has been described prior to the onset of the skin lesions.[7] As the disease progresses, patients may develop significant hypotension that can compromise their ability to tolerate hemodialysis.[23] Thromboembolic disease can be a significant complication of NSF.[24]
Diagnosis
The diagnosis of NSF is based on the presence of characteristic clinical features in the setting of CKD, and substantiated by skin histology. The epidermis is usually not affected. Deposition of collagen and mucin is increased in the dermis and interlobular septae. Early lesions show abundant mucin separating thin collagen bundles. With progression of the disease, collagen bundles become thicker. The clefts surrounding collagen bundles are present in all stages, and there is no significant inflammation.[25] The fibrocytes appear as spindle cells with tapered nuclei and indistinct cell membranes. They are distributed between the collagen strands, generally parallel to their predominant direction. In advanced lesions, fibrocytes and elastic fibers are sandwiched between thick collagen bundles.[26] The entire dermis is eventually involved, with increased fibrocytes, collagen, mucin and elastic fibers extending through the subcutaneous tissue along the septae of fatty lobules. The subcutaneous septae are markedly thickened by fibrotic tissue, yielding microlobular architecture. Mucin stains (Alcian blue and colloidal iron), elastic stains (Verhoeff-van Gieson) and trichrome stains may be used to highlight interstitial mucin collections, elastic fibers and collagen, respectively. The fibrocytes have a characteristic immunoprofile, being dually positive for CD34 and procollagen 1. These cells are identified as “circulating fibrocytes” and represent bone marrow-derived mesenchymal cells.[27] Factor XIIIa+ dendritic cells and CD68+ histiocytes (mononuclear and multinucleate) are frequently found in affected tissues. Increased numbers of dendritic cells along with coexpression of CD68 and factor XIIIa have been shown in early lesions of NSF.[28]
Calcification has been described in some cases as a feature of NSF.[29,30] It can be seen in and around thickened collagen or elastic fibers, around basement membrane of vessel walls or occasionally in histiocytes. Extensive fibrosis and calcification in the diaphragm, psoas muscle, myocardial vasculature and in mitral valve, kidneys, lung and testis have been reported.[31,32]
Demonstration of Gd in tissue by inductively coupled plasma mass spectrometry provides further support for the diagnosis of NSF. However, because the amount of Gd deposited in tissue does not correlate with the extent of clinical involvement, the significance of this finding is not fully understood in the context of NSF.[25]
Other laboratory workup which might test positive includes peripheral eosinophilia; antinuclear, anticardiolipin or antiphospholipid antibody; hepatitis B or C serology; and an associated hypercoagulable state.[33] No particular laboratory abnormality is consistently linked to NSF, and the diagnosis basically hinges on good clinicopathological correlation.
Differential diagnosis
Scleroderma is an autoimmune disease that is most often seen in women aged 30 to 50 years and can affect the skin, blood vessels and internal organs. The American College of Rheumatology requires one major criterion or two minor criteria for the diagnosis of scleroderma. The major criterion is symmetric sclerosis proximal to the metacarpophalangeal or metatarsophalangeal joints, and the minor criteria are sclerodactyly, digital pitting scars or loss of substance from the finger pad, and bibasilar pulmonary fibrosis. Cutaneous scleroderma in both the limited and diffuse forms can involve the face in isolation or as a part of the calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia (CREST) syndrome. Facial involvement, telangiectasias, prominent nail fold capillaries and Raynaud's phenomenon are not seen with NSF. Laboratory data in favor of scleroderma include positive tests for antinuclear antibody, antineutrophil cytoplasmic antibody and antitopoisomerase (Scl-70) antibodies.
Scleredema presents as a diffuse hardening of the skin of the upper body due to increased production of mucin and collagen. Unlike in NSF, there is no increase in the number of fibroblasts. Types I and II scleredema are characterized by induration of cervicofacial skin, which can progress to involve the trunk and proximal upper arms.[3] Type I usually follows streptococcal upper respiratory tract infection and resolves spontaneously over a period of months. Type II is idiopathic, slower in onset and resolution, and can be associated with a monoclonal gammopathy.[1,3] Type III (scleredema diabeticorum) results from irreversible glycosylation of collagen fibers that reduces their collagenase-mediated degradation and presents as induration of the skin of the posterior neck and upper back in middle-aged men. All types can have systemic involvement, with dysphagia, dysarthria, serositis and myositis, as well as cardiac and ocular changes.[1,3] Lack of facial involvement in NSF with its characteristic setting and clinical presentation would distinguish it from scleredema.
The terms lichen myxedematosus, papular mucinosis and scleromyxedema are used interchangeably to describe a spectrum of the same disorder. Lichen myxedematosus is a rare skin disorder characterized by fibroblast proliferation and mucin deposition in the dermis. Small monomorphic, indurated, erythematous or hyperpigmented papules occur in a symmetric and commonly linear distribution over the hands, forearms, head, neck, upper trunk, and thighs and are surrounded by shiny, indurated skin.[1,3] Involvement of the forehead produces classic linear furrows, whereas thickening of the skin over the proximal interphalangeal joints produces the “doughnut sign,” a central depression with an elevated, firm rim of skin when these joints are extended.[1,3] Unlike NSF, this condition may be associated with a monoclonal gammopathy.
Longstanding venous insufficiency can induce capillary proliferation, fat necrosis and fibrosis of skin and subcutaneous tissues. A panniculitis follows, which heals with sclerosis and induration of the skin just above the medial malleolus.[5,6] In its acute phase, lipodermatosclerosis presents with pain, warmth, erythema, and induration of the affected areas.[6] As this condition progresses to dermal and subcutaneous sclerosis, a sharply demarcated area of induration develops, with hyperpigmentation due to hemosiderin deposition.[5,6] When the condition is pronounced, the lower legs can resemble an “inverted champagne bottle.”[5] Lipodermatosclerosis is usually not progressive, and the skin changes are restricted to the legs. Although NSF often is mistaken for lipodermatosclerosis or chronic venous stasis change, skin induration and dyspigmentation in these conditions are limited to the leg below the knee, and joint contractures do not occur. Thus the presence of upper extremity involvement and joint contractures is more characteristic of NSF.
Metastatic calcification includes benign nodular calcification and calciphylaxis, both of which are caused by cutaneous precipitation of calcium and phosphate salts, on a background of renal disease. In benign nodular calcification, large deposits accumulate in the skin and subcutis, particularly in periarticular locations.[1] Calciphylaxis is a process of ischemic necrosis of the skin and soft tissues due to increased vascular calcification,[1,7] which manifests clinically as reticulated, violaceous patches, which can progress to exquisite tender lesions with bullae, necrosis and ulceration.[7] Histopathology and clinical setting would help distinguish this condition from NSF.
Eosinophilic fasciitis is an idiopathic, fibrotic disorder with the histopathologic hallmark of fascial fibrosis. It presents as sudden onset of pain, tenderness, edema and erythema in the extremities. The disorder progresses rapidly, and within weeks to months patients develop stiffness and sclerodermatous induration, resulting in characteristic flexion contractures and impaired mobility. In order of decreasing frequency, the forearms, upper arms, lower legs, thighs and trunk are involved. Unlike in NSF, blood count shows eosinophilia (10%-40%) in as many as 80% to 90% of the patients, and there may be associated hypergammaglobulinemia.
Eosinophilia-myalgia syndrome (EMS) is associated with intense myalgias and peripheral blood eosinophilia. The Centers for Disease Control and Prevention (CDCs) defined this syndrome as requiring all of the following criteria: (1) incapacitating myalgias, (2) a blood eosinophil count greater than 1000 cells/µL and (3) no evidence of infection (e.g., trichinosis) or neoplastic conditions that could account for these findings. Cutaneous manifestations develop approximately 3 weeks after the onset of myalgia. Induration of the skin affecting the forearms, arms and legs occurs in approximately one third of the patients, resembling eosinophilic fasciitis or morphea. Digital skin thickening and Raynaud's phenomenon are however rare in EMS.
Porphyria cutanea tarda commonly presents in adults as erosions and bullae, typically on the hands and forearms, and occasionally on the face or feet. It can also present as indurated, waxy, yellowish plaques that resemble lesions of scleroderma, developing on the chest and the back but being most prominent in the preauricular and nuchal areas. These plaques may develop dystrophic calcification. Rarely, the only physical sign of porphyria cutanea tarda is a hyperpigmented sclerodermoid appearance. Urinary porphyrin levels are abnormally high, and RBC enzyme activity assay of the heme synthetic enzyme uroporphyrinogen decarboxylase is deficient.
Dermatofibrosarcoma protuberans (DP) is a cutaneous malignancy that arises from the dermis and invades deeper subcutaneous tissue (e.g., fat, fascia, muscle, bone). It usually presents as a large indurated plaque several centimeters in diameter. DP seldom occurs above the neck (10%-16%).[34] A skin biopsy is essential for definitive diagnosis.
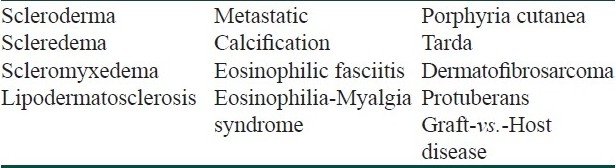
The characteristic anatomic distribution of skin involvement in NSF helps to differentiate it from other fibrosing diseases [Table 1]. Erosive indurated plaques of chronic graft-versus-host disease typically involve the skin of the trunk, and these patients would have received an allograft prior to the onset of their skin changes.
Table 1.
Differential diagnosis of nephrogenic systemic sclerosis
Prognosis
Skin changes in NSF have been reported to improve upon normalization of kidney function following renal transplantation or the resolution of acute renal failure.[23] In most cases, however, NSF progresses relentlessly. NSF has also been reported to develop in patients after implantation of a functioning renal allograft and restoration of normal kidney function.[23] Among patients with stage 5 CKD, those with cutaneous changes of NSF have a threefold risk of dying within 2 years of the diagnosis of NSF.[23] Cardiovascular events are the predominant cause of death in patients with stage 5 CKD, both with and without NSF.[35]
Treatment
While there is no consistently successful treatment for NSF, improving renal function seems to slow or arrest the progression of this condition. Patients who have undergone successful kidney transplantation may show resolution of the lesions.[33] In other cases, kidney transplant has resulted in no obvious improvement of the lesions, even with a fully functioning, successfully transplanted organ.[7] NSF is however not a contraindication for renal transplant.
Prednisone in a dose of 1 mg/kg p.o. daily seems to work in a subset of patients.[7] Worsening of diabetes, possibility of gastrointestinal ulceration and osteoporosis can be unwanted side effects. The response to topical calciprotriene under occlusion has been anecdotal and largely subjective. The combination of occluded calciprotriene and clobetasol with vascular compression stockings has reportedly been of benefit.[7] Three patients suffering from NSF for less than 1 year have been reported to respond with softening of plaques after several courses of extracorporeal photopheresis.[36] Patients suffering from NSF for more than 1 year may not respond to this modality.[7] This treatment is currently under investigation, although no formal trials are yet offered. Plasmapheresis has been reportedly successful in three patients with liver/ kidney transplant. It is however unclear what contribution the improving renal function may have had in the overall clinical improvement.[37] Cutaneous changes have improved in several patients with NSF of recent onset after treatment with oral thalidomide 50-100 mg daily; however, thalidomide has not been effective in patients with longstanding NSF.[23] There have been two reports of development of NSF in patients already taking thalidomide for other medical problems.[7] Ultraviolet therapy (UVA-1) has been reported to be of benefit in a single case report.[38] Psoralen-ultraviolet A (PUVA) in combination with acitretin and prednisone has been anecdotally helpful in two patients.[7] High-dose intravenous immunoglobulin therapy has been reported to improve NSF.[39] Mildly improved skin tightening, range of motion, and/ or functional capacity have been reported with extracorporeal photopheresis (ECP).[40] Of all treatments, ECP seems to be the best, albeit mild and extremely expensive, treatment modality for NSF.[33]
Treatment with oral pentoxifylline (PXF) 1200 mg daily was perceived to slow progression of disease and stabilize NSF.[2] The use of PXF is theoretically justified as it has known antifibrotic activity, thought to be at least partially related to TNF alpha antagonism. In addition, PXF is known to improve red blood cell flexibility and therefore to improve circulation. As thrombosis seems to be an inciting event for many NSF patients, this mechanism could also be partially responsible for the improvements noted clinically.[7]
Imatinib mesylate is a 2-phenylaminopyrimidine compound that selectively inhibits signaling mediated by several cell-surface receptors. It has been shown to inhibit type I collagen and fibronectin synthesis by dermal fibroblasts in vitro and reduce extracellular matrix synthesis and accumulation in bleomycin-induced experimental dermal fibrosis.[41] Treatment of several NSF patients with oral imatinib mesylate 400 mg daily has yielded improvement in objective clinical measures of skin tethering and limited joint mobility and in the histologic appearance of fibrosis.[42] However, its use may be limited by the commonly occurring adverse effects of fluid retention and gastrointestinal upset. There is now an investigator-initiated phase 2, open-label pilot study of imatinib mesylate for the treatment of nephrogenic systemic fibrosis [ClinicalTrials.gov number, NCT00677092 (ClinicalTrials.gov)], supported by a grant from Novartis and by a grant from the National Center for Research Resources to Harvard Clinical and Translational Science Center, in which patients are treated with imatinib mesylate (400 mg daily) for 4 months and then are observed for 2 months after stopping therapy. The primary outcome is the change in the modified Rodnan skin score (a standard outcome measure for skin disease in patients with scleroderma that is calculated by summation of skin thicknesses in 17 body sites) from baseline to 4 months.[22]
Physical therapy (PT), in particular, swimming, may be helpful in slowing the progression of joint contractures.[7] There is no contraindication to PT, and the definite potential upside suggests that PT should be pursued whenever possible.[33]
Prevention
Because essentially all cases of NSF have developed following exposure to a gadolinium-containing contrast agent, prevention of this devastating condition involves the careful avoidance of administering these agents to individuals at risk. Patients with stage 4 or stage 5 CKD (estimated glomerular filtration rate, <30 mL/min per 1.73 m2) should not be administered a gadolinium-containing contrast agent.[23] However, as NSF also occurs in individuals with lesser degrees of renal dysfunction, the threshold level of kidney function above which gadolinium-containing contrast agents may be administered safely is unknown. There is no prophylactic agent that can be administered prior to the gadolinium-containing contrast agent to prevent the development of NSF. Thus the diagnostic benefit of using a gadolinium-containing contrast agent in an imaging study must be weighed very carefully against the significant risk of the patient developing this relentlessly progressive, debilitating condition.
Prognosis
Though spontaneous resolution may occur, typically coincident with improved renal function, NSF is basically a progressive disorder. NSF can be disabling and can restrict the patient's range of motion, resulting in falls and fractures. Many patients report marginal improvement and stabilization after years. Patients need to understand that NSF is not a life-threatening disease but lacks effective treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Cowper SE, Robin HS, Steinberg SM, Su LD, Gupta S, LeBoit PE. Scleromyxoedema-like cutaneous diseases in renal-dialysis patients. Lancet. 2000;356:1000–1. doi: 10.1016/S0140-6736(00)02694-5. [DOI] [PubMed] [Google Scholar]
- 2.Grobner T. Gadolinium—a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis? Nephrol Dial Transplant. 2006;21:1104–8. doi: 10.1093/ndt/gfk062. [DOI] [PubMed] [Google Scholar]
- 3.Marckmann P, Skov L, Rossen K, Dupont A, Damholt MB, Heaf JG, et al. Nephrogenic systemic fibrosis: Suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging. J Am Soc Nephrol. 2006;17:2359–62. doi: 10.1681/ASN.2006060601. [DOI] [PubMed] [Google Scholar]
- 4.Knopp EA, Cowper SE. Nephrogenic systemic fibrosis: Early recognition and treatment. Semin Dial. 2008;21:123–8. doi: 10.1111/j.1525-139X.2007.00399.x. [DOI] [PubMed] [Google Scholar]
- 5.Prasad SR, Jagirdar J. Nephrogenic systemic fibrosis/nephrogenic fibrosing dermopathy: A primer for radiologists. J Comput Assist Tomogr. 2008;32:1–3. doi: 10.1097/RCT.0b013e31805d08ee. [DOI] [PubMed] [Google Scholar]
- 6.Introcaso CE, Hivnor C, Cowper S, Werth VP. Nephrogenic fibrosing dermopathy/ nephrogenic systemic fibrosis: A case series of nine patients and review of the literature. Int J Dermatol. 2007;46:447–52. doi: 10.1111/j.1365-4632.2007.03301.x. [DOI] [PubMed] [Google Scholar]
- 7.Cowper SE. Nephrogenic Fibrosing Dermopathy [ICNSFR Website]. 2001-2009. [last accessed on 2010 Jun 14]. Available from: http://www.icnsfr.org .
- 8.Cowper SE, Kuo PH, Bucala R. Nephrogenic systemic fibrosis and gadolinium exposure: Association and lessons for idiopathic fibrosing disorders. Arthritis Rheum. 2007;56:3173–5. doi: 10.1002/art.22926. [DOI] [PubMed] [Google Scholar]
- 9.Brown H. Gadodiamide, NSF: Direct link identified. Skin Allergy News. 2007;38:37. [Google Scholar]
- 10.Edward M, Fitzgerald L, Thind C, Leman J, Burden AD. Cutaneous mucinosis associated with dermatomyositis and nephrogenic fibrosing dermopathy: Fibroblast hyaluronan synthesis and the effect of patient serum. Br J Dermatol. 2007;156:473–9. doi: 10.1111/j.1365-2133.2006.07652.x. [DOI] [PubMed] [Google Scholar]
- 11.Wermuth PJ, Del Galdo F, Jiménez SA. Induction of the expression of profibrotic cytokines and growth factors in normal human peripheral blood monocytes by gadolinium contrast agents. Arthritis Rheum. 2009;60:1508–18. doi: 10.1002/art.24471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiménez SA, Artlett CM, Sandorfi N, Derk C, Latinis K, Sawaya H, et al. Dialysis-associated systemic fibrosis (nephrogenic fibrosing dermopathy): Study of inflammatory cells and transforming growth factor beta1 expression in affected skin. Arthritis Rheum. 2004;50:2660–6. doi: 10.1002/art.20362. [DOI] [PubMed] [Google Scholar]
- 13.Goveia M, Chan BP, Patel PR. Evaluating the role of recombinant erythropoietin in nephrogenic systemic fibrosis. J Am Acad Dermatol. 2007;57:725–7. doi: 10.1016/j.jaad.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Saab G. Epoetin and nephrogenic systemic fibrosis. J Am Acad Dermatol. 2008;58:174–5. doi: 10.1016/j.jaad.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Parsons AC, Yosipovitch G, Sheehan DJ, Sangüeza OP, Greenberg CS, Sane DC. Transglutaminases: The missing link in nephrogenic systemic fibrosis. Am J Dermatopathol. 2007;29:433–6. doi: 10.1097/DAD.0b013e318156e43f. [DOI] [PubMed] [Google Scholar]
- 16.Weenig RH, Gibson LE, el-Azhary R. The role of the hospital dermatologist in the diagnosis and treatment of calciphylaxis and nephrogenic systemic fibrosis. Semin Cutan Med Surg. 2007;26:163–7. doi: 10.1016/j.sder.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Grobner T, Prischl FC. Patient characteristics and risk factors for nephrogenic systemic fibrosis following gadolinium exposure. Semin Dial. 2008;21:135–9. doi: 10.1111/j.1525-139X.2007.00406.x. [DOI] [PubMed] [Google Scholar]
- 18.Perazella MA. Tissue deposition of gadolinium and development of NSF: A convergence of factors. Semin Dial. 2008;21:150–4. doi: 10.1111/j.1525-139X.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- 19.Scheinfeld N. Nephrogenic fibrosing dermopathy: A comprehensive review for the dermatologist. Am J Clin Dermatol. 2006;7:237–47. doi: 10.2165/00128071-200607040-00005. [DOI] [PubMed] [Google Scholar]
- 20.Saab G, Cheng S. Nephrogenic systemic fibrosis: A nephrologist's perspective. Hemodial Int. 2007;11:S2–6. doi: 10.1111/j.1542-4758.2007.00222.x. [DOI] [PubMed] [Google Scholar]
- 21.Boin F, Hummers LK. Scleroderma-like fibrosing disorders. Rheum Dis Clin North Am. 2008;34:199–220. doi: 10.1016/j.rdc.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroshinsky D, Kay J, Nazarian RM. Case records of the Massachusetts General Hospital. Case 37-2009. A 46-yearold woman with chronic renal failure, leg swelling, and skin changes. N Engl J Med. 2009;361:2166–76. doi: 10.1056/NEJMcpc0907802. [DOI] [PubMed] [Google Scholar]
- 23.Kay J, et al. Nephrogenic systemic fibrosis (Update) In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's Principles of Internal Medicine. [September 2010]. p. 17e. Available from: http://www.lproxy.nymc.edu:60312/updates . [Google Scholar]
- 24.Koreishi AF, Nazarian RM, Saenz AJ, Klepeis VE, McDonald AG, Farris AB, et al. Nephrogenic systemic fibrosis: A pathologic study of autopsy cases. Arch Pathol Lab Med. 2009;133:1943–8. doi: 10.5858/133.12.1943. [DOI] [PubMed] [Google Scholar]
- 25.Thakral C, Abraham JL. Nephrogenic systemic fibrosis: Histology and gadolinium detection. Radiol Clin North Am. 2009;47:841–53. doi: 10.1016/j.rcl.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 26.Cowper SE, Rabach M, Girardi M. Clinical and histological findings in nephrogenic systemic fibrosis. Eur J Radiol. 2008;66:191–9. doi: 10.1016/j.ejrad.2008.01.016. [DOI] [PubMed] [Google Scholar]
- 27.Cowper SE, Bucala R. Nephrogenic fibrosing dermopathy: Suspect identified, motive unclear. Am J Dermatopathol. 2003;25:358. doi: 10.1097/00000372-200308000-00017. [DOI] [PubMed] [Google Scholar]
- 28.Mendoza FA, Artlett CM, Sandorfi N, Latinis K, Piera-Velazquez S, Jimenez SA. Description of 12 cases of nephrogenic fibrosing dermopathy and review of the literature. Semin Arthritis Rheum. 2006;35:238–49. doi: 10.1016/j.semarthrit.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cowper SE, Su LD, Bhawan J, Robin HS, LeBoit PE. Nephrogenic fibrosing dermopathy. Am J Dermatopathol. 2001;23:383–93. doi: 10.1097/00000372-200110000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Edsall LC, English JC, 3rd, Teague MW, Patterson JW. Calciphylaxis and metastatic calcification associated with nephrogenic fibrosing dermopathy. J Cutan Pathol. 2004;31:247–53. doi: 10.1111/j.0303-6987.2004.00169.x. [DOI] [PubMed] [Google Scholar]
- 31.Ting WW, Stone MS, Madison KC, Kurtz K. Nephrogenic fibrosing dermopathy with systemic involvement. Arch Dermatol. 2003;139:903–6. doi: 10.1001/archderm.139.7.903. [DOI] [PubMed] [Google Scholar]
- 32.Daram SR, Cortese CM, Bastani B. Nephrogenic fibrosing dermopathy/nephrogenic systemic fibrosis: Report of a new case with literature review. Am J Kidney Dis. 2005;46:754–9. doi: 10.1053/j.ajkd.2005.06.024. [DOI] [PubMed] [Google Scholar]
- 33.Scheinfeld N, Cowper S. Nephrogenic systemic fibrosis, emedicine (dermatology) Updated. 2009 [Google Scholar]
- 34.Lemm D, Mügge LO, Mentzel T, Höffken K. Current treatment options in dermatofibrosarcoma protuberans. J Cancer Res Clin Oncol. 2009;135:653–65. doi: 10.1007/s00432-009-0550-3. [DOI] [PubMed] [Google Scholar]
- 35.Todd DJ, Kagan A, Chibnik LB, Kay J. Cutaneous changes of nephrogenic systemic fibrosis: Predictor of early mortality and association with gadolinium exposure. Arthritis Rheum. 2007;56:3433–41. doi: 10.1002/art.22925. [DOI] [PubMed] [Google Scholar]
- 36.Mathur K, Morris S, Deighan C, Green R, Douglas KW. Extracorporeal photopheresis improves nephrogenic fibrosing dermopathy/nephrogenic systemic fibrosis: Three case reports and review of literature. J Clin Apher. 2008;23:144–50. doi: 10.1002/jca.20170. [DOI] [PubMed] [Google Scholar]
- 37.Baron PW, Cantos K, Hillebrand DJ, Hu KQ, Ojogho ON, Nehlsen-Cannarella S, et al. Nephrogenic fibrosing dermopathy after liver transplantation successfully treated with plasmapheresis. Am J Dermatopathol. 2003;25:204–9. doi: 10.1097/00000372-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 38.Kreuter A, Gambichler T, Weiner SM, Schieren G. Limited effects of UV-A1 phototherapy in 3 patients with nephrogenic systemic fibrosis. Arch Dermatol. 2008;144:1527–9. doi: 10.1001/archderm.144.11.1527. [DOI] [PubMed] [Google Scholar]
- 39.Chung HJ, Chung KY. Nephrogenic fibrosing dermopathy: Response to high-dose intravenous immunoglobulin. Br J Dermatol. 2004;150:596–7. doi: 10.1111/j.1365-2133.2003.05795.x. [DOI] [PubMed] [Google Scholar]
- 40.Richmond H, Zwerner J, Kim Y, Fiorentino D. Nephrogenic systemic fibrosis: Relationship to gadolinium and response to photopheresis. Arch Dermatol. 2007;143:1025–30. doi: 10.1001/archderm.143.8.1025. [DOI] [PubMed] [Google Scholar]
- 41.Distler JH, Jungel A, Huber LC, Schulze-Horsel U, Zwerina J, Gay RE, et al. Imatinib mesylate reduces production of extracellular matrix and prevents development of experimental dermal fibrosis. Arthritis Rheum. 2007;56:311–22. doi: 10.1002/art.22314. [DOI] [PubMed] [Google Scholar]
- 42.Kay J, High WA. Imatinib mesylate treatment of nephrogenic systemic fibrosis. Arthritis Rheum. 2008;58:2543–8. doi: 10.1002/art.23696. [DOI] [PubMed] [Google Scholar]


