Abstract
Dendritic cells (DCs) play an important role in the clearance of apoptotic cells. The removal of apoptotic cells leads to peripheral tolerance, although their role is still not clear. We show that the uptake of apoptotic thymocytes by DCs converts these cells into tolerogenic DCs resistant to maturation by lipopolysaccharide, modulating the production of interleukin-12 and up-regulating the expression of transforming growth factor-β1 latency associated peptide. We also observed that DCs pulsed with apoptotic cells in the allogeneic context were more efficient in the expansion of regulatory T cells (Tregs), and that this expansion requires contact between DCs and the T cell. The Tregs sorted from in vitro culture suppressed the proliferation of splenocytes in vitro in a specific and non-specific manner. In the in vivo model, the transfer of CD4+ CD25− cells to Nude mice induced autoimmunity, with cell infiltrate found in the stomach, colon, liver and kidneys. The co-transfer of CD4+ CD25− and CD4+ CD25+ prevented the presence of cell infiltrates in several organs and increased the total cell count in lymph nodes. Our data indicate that apoptotic cells have an important role in peripheral tolerance via induction of tolerogenic DCs and CD4+ CD25+ Foxp3+ cells that present regulatory functions.
Keywords: apoptosis, dendritic cells, Foxp3, peripheral tolerance, regulatory T cells
Introduction
Dendritic cells (DCs) are cells specialized in antigen capture, processing and presentation to T lymphocytes, acting as a connection between innate and adaptive immunity. After interaction between DCs, Toll-like receptors and their respective ligands, which are present in microorganisms, these cells undergo maturation.1,2
Depending on the DC activation state, these cells are able to activate T lymphocytes and elicit the immune response. When in the steady state (immature dendritic cells; iDC), they do not activate T lymphocytes in a classical way, which involves clone proliferation and production of pro-inflammatory cytokines. Instead, when presenting antigens to T lymphocytes, an iDC is able to induce the expansion of cells with regulatory properties such as regulatory T cells (Tregs).3
Dendritic cells comprise other mechanisms that contribute to the maintenance of peripheral tolerance. Recent published data indicate that DCs are crucial for the induction and maintenance of tolerance to allogeneic antigens and auto-antigens.4 Moreover, the antigen presentation by DCs, which previously internalized an apoptotic cell, leads to tolerance induction through mechanisms that are not entirely understood. There is evidence that the internalization of apoptotic bodies renders DCs immature, which may explain why apoptotic cells, unlike necrotic cells, are unable to induce immune responses.5–7 This inability to properly activate DCs may be important for establishing peripheral tolerance to auto-antigens.
The Tregs are known as essential for the control and prevention of autoimmune diseases and for the maintenance of self-tolerance. They constitutively express CD4, CD25 [the alpha-chain of the interleukin-2 (IL-2) receptor] and the transcription factor Foxp3.
Mice lacking either CD25 or Foxp3 succumb to a lymphoproliferative, autoimmune disease.8 Several studies have shown that Foxp3 is required for Tregs to exert their suppressive ability and the ectopic expression of this transcription factor by lymphoid and non-lymphoid cells is able to confer suppressive function, so making Foxp3 a critical regulator of Treg function.9–11
The Tregs are anergic to T-cell receptor stimulation in vitro, which means they do not proliferate upon activation.12 On the other hand, in vivo studies show that this anergic state is not observed when these cells are transferred to a lymphopenic host. When CD4+ CD25+ cells are transferred to Nude mice, recombinant activating gene deficient (RAG−/−) mice and severe combined immunodeficient (SCID) mice, they proliferate and populate the lymphoid organs.13,14 This phenomenon is called homeostatic proliferation and it is observed also when effector cells (CD4+ CD25−) are transferred to the same lymphopenic host.
The transfer of effector cells to the lymphopenic host leads to the development of autoimmunity in several organs, including autoimmune gastritis and colitis. Interestingly, the co-transfer of CD4+ CD25− and CD4+ CD25+ is able to prevent the development of organ-specific autoimmunity.14
It is known that the clearance of apoptotic cells is an active process in the induction of peripheral tolerance. One of the methods by which the apoptotic cell is able to promote tolerance is by acting on DCs. There is evidence that apoptotic cells have an immunosuppressive effect on monocytes, leading to the production of IL-10 and decreasing the release of pro-inflammatory cytokines such as tumour necrosis factor-α, IL-1β and IL-12.15
Some other groups showed that the phagocytosis of apoptotic cells is able to modulate the expression of co-stimulatory molecules rendering DCs immature and resistant to maturation by lipopolysaccharide (LPS) and other Toll-like receptor ligands.5–7 Previously, we asked whether the apoptotic cells were able to induce the expansion of cells with regulatory phenotype, which in turn should induce peripheral tolerance. We found that DCs pulsed with either allogeneic or syngeneic apoptotic thymocytes induce cells with regulatory phenotype, the allogeneic context being more efficient in that expansion.16
In this study, we show that DCs pulsed with allogeneic apoptotic cells induce Tregs able to suppress the immune response in vitro and in vivo, and in a specific and non-specific manner.
Materials and methods
Mice
Six- to eight-week-old BALB/c (H-2d), C57BL/6 (H-2b), BALB/c Nude and BALB/c DO11.10 female mice were obtained from the Department of Immunology animal facility at the University of São Paulo and kept in micro-isolator cages under specific pathogen-free conditions. Experiments were performed following the guidelines for animal use and care approved by the Ethics Committee on Animal Research from the Institute of Biomedical Sciences of the University of São Paulo.
Generation of dendritic cells
Immature DCs were derived in vitro from bone marrow cells as described by Inaba et al.,44 with some modifications. Briefly, bone marrow cells were removed from the femurs of BALB/c mice and cultured in Dulbecco's modified Eagle's medium (DMEM) complete medium supplemented with 5% fetal bovine serum (Hyclone, Logan, UT), 10−5m 2-mercaptoethanol (Sigma Chemicals Co, St Louis, MO) 2 mm l-glutamine, 1 mm sodium pyruvate, 0·1 mm non-essential amino acids and 100 μg/ml gentamicin. All of these reagents were purchased from Life Technologies (Grand Island, NY). Cells were cultured for 7 days in a six-well plate (Sarstedt, Newton, NC) at 2 × 106 cells/ml in a total volume of 5 ml/well with 10 ng/ml recombinant murine granulocyte–macrophage colony-stimulating factor (rmGM-CSF). Murine rGM-CSF was renewed on day 4 of culture. For DC maturation, cells were stimulated on day 6 for 24 hr with 1 μg/ml LPS.
Induction of apoptosis in thymocytes
Thymuses were obtained from 3-week-old C57BL/6 and BALB/c female mice. A single cell suspension was prepared and plated in six-well plates at a concentration of 107 cells/ml. Cells were treated with 10−7 m dexamethasone and kept in a 37° 5% CO2 incubator for 4 hr. Cells were washed with DMEM and resuspended in complete culture medium. All centrifugation was performed under 300 g to avoid contamination of the apoptotic bodies with apoptotic blebs. Apoptosis was assessed as in Marguti et al.16
Dendritic cells and lymph node cell co-culture
Immature DCs or mature DCs (mDCs) from BALB/c mice were cultured overnight in complete medium with apoptotic thymocytes from C57BL/6 or BALB/c mice at a 1 : 5 ratio (DCs : apoptotic cells). After the incubation period thymocyte debris was harvested from the culture by washing the cells with DMEM. The DCs were co-cultured in complete medium with syngeneic lymph node cells at a 1 : 5 ratio (DCs : lymph node cells) for 5 days. At the end of the co-culture period, lymph node cells were harvested with DMEM, washed once and characterized by flow cytometry. The same procedure was repeated with the cultures being separated by transwell chambers (Corning, NY).
Flow cytometry
Cells were incubated with anti-CD16/32 (Fc Block) for 30 min at 4° in PBS/3% fetal calf serum/0·01% sodium azide (FACS buffer). Cells were labelled with fluorescent antibodies against CD11c (phycoerythrin-conjugated; PE), MHCII-I-Ad (FITC), CD80 (FITC), CD86 (FITC), CD40 (FITC), CD4 (Cy), CD25 (FITC), CD25 (PE), CD44 (PE), CTLA-4 (PE), CD69 (PE), CD122 (PE), GITR (PE), CD62L (FITC), LAP (biotin) and Streptavidin (PE-Cy5) (0·5 μg/106 cells). All these reagents were purchased from Pharmingen BD (San Diego, CA). Cells were incubated for 30 min at 4°, washed with 1 ml flow cytometry buffer and resuspended in 300 μl of the same buffer used before analysis. For the evaluation of Foxp3 expression, cells were labelled with anti-CD4 (Cy) and anti-CD25 (FITC) antibodies, fixed, permeabilized and labelled with anti-Foxp3 (PE) antibody according to the manufacturer's instructions (‘PE anti-mouse/rat Foxp3 Staining Set’; eBiosciences, San Diego, CA). Cells were analysed by flow cytometry using FACScanto (BD, San Diego, CA) with FlowJo software (Tree Star, Ashland, OR). For intracellular staining, DCs were incubated with medium with or without apoptotic cells in the presence of brefeldin-A (eBiosciences) for 10 hr to avoid cytokine secretion. After treatment, the cells were stained with the surface markers CD11c (allophycocyanin-conjugated) as described above, fixed with Cytofix/Cytoperm (BD Biosciences, Franklin Lakes, NJ) for 30 min, and incubated with polyclonal anti-mouse antibody to IL-12p70 (PE), IL-17A (PE), or IL-10 (PE) (BD Biosciences) for 30 min in Cytoperm buffer (BD, San Diego, CA).
In vitro proliferation assay
The CD4+ CD25+ cells induced in vitro by iDCs pulsed with allogeneic apoptotic cells (4 × 104 for the 1 : 5 ratio, 2 × 104 for the 1 : 10 ratio, 0·8 × 104 for the 1 : 25 ratio, 0·4 × 104 for the 1 : 50 ratio of Tregs : responder cells per well in a U-bottomed 96-well plate) were sorted with FACSvantage and cultured for 72 hr with BALB/c spleen cells (20 × 104 per well) and C57BL/6 irradiated spleen cells (20 × 104 for the 1 : 1 ratio, 40 × 104 for the 1 : 2 and 1 : 4 ratio of responder : target cell).
Sorted CD4+ CD25+ cells (2·5 × 104 for the 1 : 5 ratio, 2 × 104 for the 1 : 10 ratio, 0·8 × 104 for the 1 : 25 ratio of Tregs : responder cells per well in a U-bottomed 96-well plate) expanded in vitro were cultured for 72 hr with BALB/c spleen cells (1·25 × 105 for the 1 : 5 ratio, 2 × 105 for the 1 : 10 and 1 : 25 ratio of Tregs : responder cells per well) and stimulated with αCD3 (0·5 μg/ml) (kindly provided by Prof. João Gustavo Pessini Amarante Mendes from the Immunology Department of the University of São Paulo). The same ratios of Tregs and responder cells were used for the suppression of BALB/c DO11.10 spleen cells stimulated with ovalbumin (50 μg/ml; Sigma Chemicals Co).
The proliferation was measured by the Cell Proliferation Biotrak ELISA (GE Healthcare Life Sciences, Buckinghamshire, UK) and performed as described in the manufacturer's protocol.
In vivo suppression assay
The CD4+ CD25+ (0·2 × 105) and CD4+ CD25− (0·8 × 105) cells expanded in vitro were injected intravenously by the ocular plex into 6-week-old female BALB/c Nude mice. The animals were monitored for 12 weeks for weight loss and then killed for the histological analysis of the stomach, colon, liver and kidneys. Organs were fixed with 10% formalin and processed for haematoxylin & eosin staining. The spleen and lymph nodes were harvested 12 weeks after cell transfer for total cell count.
Statistical analysis
Data were presented as mean values ± SD. Student's t-test or analysis of variance with Tukey's post-test were performed using the GraphPad Prism 5.0 software (San Diego, CA). Data were considered significant for P < 0·05.
Results
Intake of apoptotic cells renders DCs immature and resistant to stimulation by LPS
To investigate the effect of apoptotic cells on DCs, we incubated immature bone marrow DCs with apoptotic thymocytes from syngeneic and allogeneic hosts and evaluated the expression of co-stimulatory molecules. Figure 1 shows that incubation with either syngeneic or allogeneic apoptotic cells did not change the expression pattern of the DCs’ co-stimulatory molecules such as CD80, CD86, CD40 and MHC II. These finding shows that before the co-culture with lymph node cells, DCs pulsed with apoptotic thymocytes were still immature and remained in a tolerogenic condition even when this was followed by stimulation by LPS for 24 hr (Fig. 1).
Figure 1.
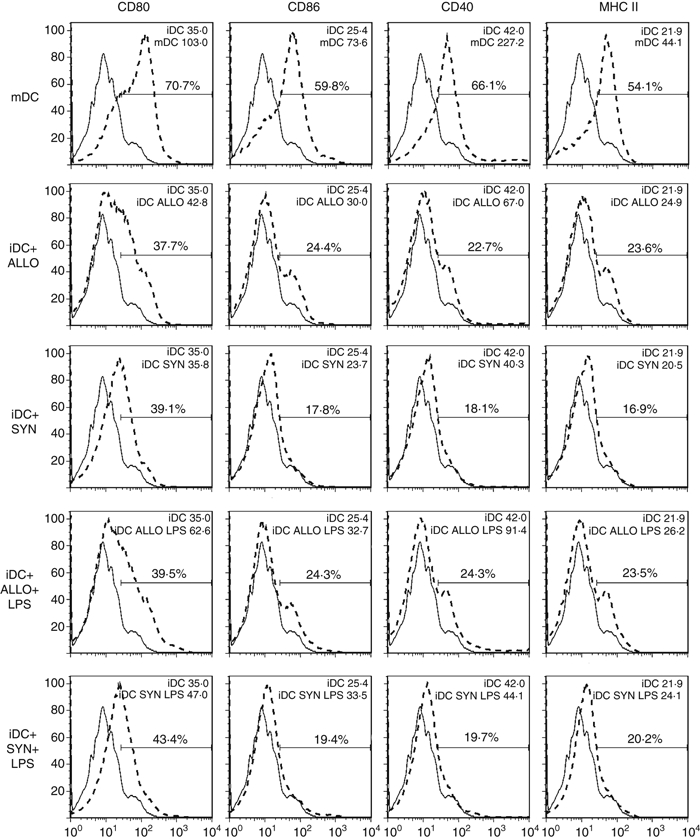
Expression of co-stimulatory molecules on immature (iDCs) or mature (mDCs) dendritic cells incubated with allogeneic (ALLO) or syngeneic (SYN) apoptotic thymocytes. Dendritic cells were generated from bone marrow cells of BALB/c mice with recombinant murine granulocyte?macrophage colony-stimulating factor (rmGM-CSF), as described in the Material and methods. On day 6, cells (mDCs) were stimulated with lipopolysaccharide (LPS) for 24 hr (1 μg/ml). On day 7, iDCs were incubated with allogeneic or syngeneic apoptotic cells overnight and after the incubation iDCs were stimulated with LPS for another 24 hr (1 μg/ml). Cells were collected and evaluated for the expression of CD80, CD86, CD40 and MHC II (gate on CD11c+ cells). Solid line: iDCs and dotted line: sample of DCs. Data are representative of three independent experiments. Numbers inside histograms represent MFI and percentage of gating.
DCs pulsed with allogeneic apoptotic thymocytes expand CD4+ CD25+ Foxp3+ cells
As reported previously by Marguti et al.,16 iDCs pulsed with allogeneic apoptotic cells more efficiently induced CD4+ CD25+ Foxp3+ cells, when compared with iDCs alone or when pulsed with syngeneic apoptotic cells (Fig. 2a). This high efficiency of the alloantigen was observed regardless of the condition of Treg expansion (Fig. 2b). The percentage of CD4+ CD25+ Foxp3+ cells found in the syngeneic expansion was similar to that found in lymph nodes of naive BALB/c mice, in this case used as controls. We also found that when expanded in vitro, Tregs showed an activated phenotype with high expression of activation markers such as CD44, CD69, CD122 and CD62L (see Supplementary material, Fig. S1). The transwell chambers used to isolate the co-culture of DCs and lymph node cells almost abrogated the expression of Foxp3 in CD4+ cells, indicating the requirement for contact between the DCs and lymphocytes to induce the expression of Foxp3 (ALLO TW and SYN TW in Fig. 2a).
Figure 2.
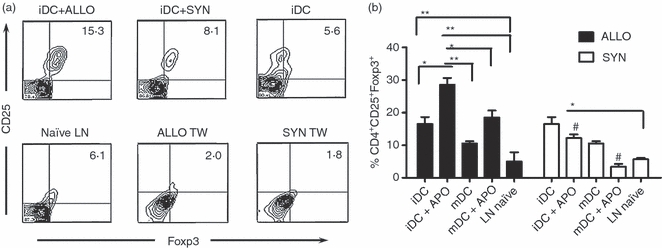
Expansion of CD4+ CD25+ Foxp3+ cells after co-culture of lymph node cells (LNs) from naive mice with dendritic cells (DCs) pulsed with allogeneic or syngeneic apoptotic thymocytes (ALLO or SYN). Immature DCs (iDCs) were incubated with apoptotic thymocytes at a 1 : 5 (DC : apoptotic cell) ratio overnight. The DCs were co-cultured with syngeneic total LN cells for 5 days (1 : 5 DC : lymph node cell ratio). Cells were collected and labelled with fluorescent antibodies for CD4, CD25 and Foxp3. Dot plot (a) and bar chart (b) presentation of CD4+ CD25+ Foxp3+ cells and the same experiment in the presence of transwell chambers separating DCs and T lymphocytes (D) (gate on CD4+ cells). Lymph node cells alone and culture of iDCs with LN cells are presented as controls. Data are presented as mean ± SD and represent six independent experiments. *P < 0·05, **P < 0·005, #P < 0·005 for the comparison of both contexts.
Phagocytosis of apoptotic cells leads to the production of transforming growth factor-β and modulates the production of IL-12
As previously reported by our group,16 the production of IL-2 by iDCs pulsed with the alloantigen was five times higher when compared with iDCs pulsed with syngeneic apoptotic cells. To investigate the differential expansion of Tregs by the syngeneic and allogeneic apoptotic cells, we evaluated the production of cytokines by DCs by intracellular staining. The production of IL-10 was detected, although not significantly altered (IL-10 Fig. 3a). The iDCs pulsed with apoptotic cells up-regulated the expression of transforming growth factor (TGF-β1) -latency associated peptide (LAP) which can infer higher production and secretion of TGF-β (LAP; Fig. 3a,b), which was also detected in the supernatant (see Supplementary material, Fig. S2). We also found that the production of IL-12 by LPS-stimulated DCs was strongly inhibited by the phagocytosis of apoptotic cells in both contexts (IL-12; Fig. 3a,c). Even though reported by some studies, we could not find an IL-17-producing population of DCs after phagocytosis of apoptotic cells (data not shown).
Figure 3.

Cytokine production by immature dendritic cells (iDC) or mature dendritic cells (mDCs) incubated or not with allogeneic or syngeneic apoptotic thymocytes. Surface marker transforming growth factor-latency associated peptide (LAP) and intracell staining for interleukin-10 (IL-10) and IL-12 (a) were performed as described in the Materials and methods. Statistic analysis on mean of fluorescence intensity of LAP (b) and IL-12 production (c) were also performed. Results are presented as mean ± SD and are representative of three independent experiments. *P < 0·05 **P < 0·005.
CD4+ CD25+ cells from in vitro culture are able to suppress the immune response in vitro and in vivo
To assess the suppressive ability of the CD4+ CD25+ cells from the in vitro culture, we sorted CD4+ CD25+ cells from the co-culture of with allogeneic apoptotic cells pulsed iDCs (iDC + ALLO) and lymph node cells, and performed in vitro and in vivo suppression assays. The sorted CD4+ CD25+ cells were able to suppress the proliferation of DO11.10 splenocytes stimulated with ovalbumin (Fig. 4b) and BALB/c splenocytes stimulated with αCD3 (Fig. 4c), at increasing ratios of Tregs : effector cells. However, higher ratios of Tregs : effector cells were unable to suppress the proliferation of the effector cells. We also found that sorted CD4+ CD25+ cells were also able to suppress the proliferation of BALB/c splenocytes stimulated with C57BL/6 irradiated splenocytes at several ratios of Tregs : effector cells, and of effector cells : target cells (Fig. 4a). We observed that the suppression obtained in the different assays did not depend on the production of TGF-β, as no statistical difference was detected (data not shown).
Figure 4.
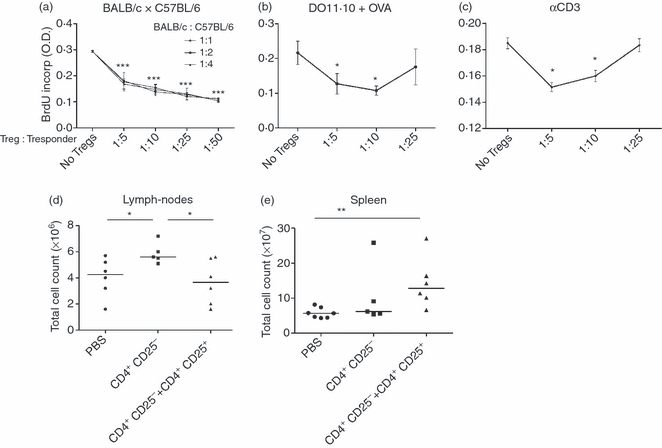
CD4+ CD25+ cells, expanded by iDCs pulsed with allogeneic apoptotic cells(iDC+ALLO) and co-cultured with lymph node cells, were isolated by flow cytometry sorting. (a) The sorted CD4+ CD25+ cells were added at different ratios (Treg: effector cell) to an mixed leukocyte reaction (1 : 5, 1 : 10, 1 : 25 and 1 : 50 ratios) BALB/c spleen cells (20 × 104 per well) and C57BL/6 irradiated spleen cells (1 : 1 ratio, 1 : 2 and 1 : 4 ratios of responder : target cell) for 72 hr. *P = 0·0124, ***P < 0·0001. Sorted Tregs and responder cells were used for the suppression of BALB/c DO11.10 spleen cells stimulated with OVA (50 mg/mL) (b). and BALB/c stimulated with αCD3 (c) (1 : 5, 1 : 10 and 1 : 25 ratios). Total cell count in the lymph nodes (d) and spleen (e) of mice 12 weeks after the transfer of CD4+ CD25+ and/or CD4+ CD25− cells. *P < 0·05, **P < 0·01. Data are representative of 3 independent experiments.
To evaluate the in vivo suppressor capacity of these Tregs, we intravenously inoculated the ocular plexus of Nude mice with sorted CD4+ CD25+ and CD4+ CD25− cells from the in vitro culture. Each group of mice was monitored for the development of wasting disease. Twelve weeks after the cell transfer, we observed that the Nude mice that received only effector cells did not lose body weight, presenting weight gain similar to the control group. The group that received both Tregs and effector cells also gained weight just like the control group (data not shown). Mice transferred with effector cells had more cells in the lymph nodes, but not in the spleen (Fig. 4d,e). In contrast, the group that received effector cells and Tregs had fewer cells in the lymph nodes, but higher cell counts in the spleen. The adoptive transfer of CD4+ CD25− cells induced autoimmunity in several organs of Nude mice. Histological evidence of autoimmune gastritis, colitis and cellular infiltrate in the kidneys and liver was observed (Fig. 5b,e,h,k). However, the group that received effector cells did not lose weight, a typical symptom of colitis. Interestingly, the transfer of CD4+ CD25− and CD4+ CD25+ cells prevented the infiltration of cells in the stomach, liver, kidneys and colon (Fig. 5c,f,i,l).
Figure 5.
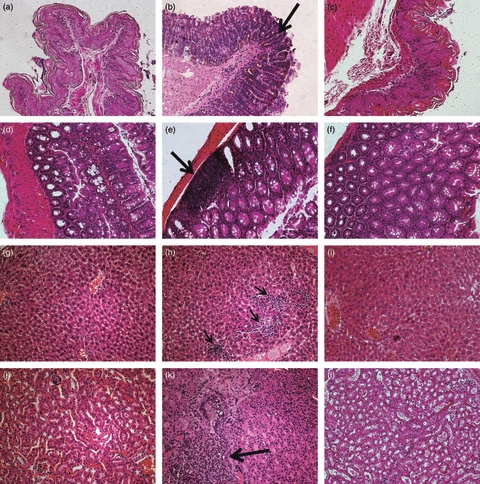
Histological analysis of the stomach, colon, liver and kidneys of Nude mice 12 weeks after the transfer of CD4+ CD25+ and/or CD4+ CD25− expanded in vitro. (a), (b) and (c) show histological analysis of the stomach of mice that received PBS (a), CD4+ CD25− (b) CD4+ CD25− and CD4+ CD25+ (c). (d), (e), and (f) show histological analysis of the colon of mice that received PBS (d), CD4+ CD25− (e) CD4+ CD25− and CD4+ CD25+ (f). (g), (h), and (i) show histological analysis of the liver of mice that received PBS (g), CD4+ CD25− (h) CD4+ CD25− and CD4+ CD25+ (i). (j), (k), and (l) show histological analysis of the kidneys of mice that received PBS (j), CD4+ CD25− (k) CD4+ CD25− and CD4+ CD25+ (l). Original magnification × 200.
Discussion
In our previous study,16 we showed that iDCs pulsed with allogeneic apoptotic cells and co-cultured with lymph node cells were able to expand cells with regulatory phenotype. We also showed that either iDCs or mDCs pulsed with syngeneic apoptotic cells were not as efficient in the expansion of Tregs, when compared with the use of the alloantigen. As discussed previously, the differential expansion of cells with regulatory phenotype by the apoptotic cells might be the result of the production of cytokines involved in the conversion of CD4+ CD25− Foxp3− into CD4+ CD25+ Foxp3+ cells, such as IL-2 and TGF-β.
Recent data showed that mixing contexts between DCs and lymphocytes led to the conversion of CD4+ cells into regulatory T cells without the addition of exogenous cytokines.17 The expansion of Tregs in this case was dependent on IL-2, as with this cytokine neutralized no conversion was observed. In this same study, mDCs and iDCs were equally efficient in the generation of Tregs, which is not consistent with what is presented here. The ability of mDCs in expanding Tregs has been shown in mice,3 and there is evidence that the mDC-induced Treg proliferation requires the addition of exogenous IL-2.18 We also showed that Tregs expanded in vitro have an activated phenotype, with high expression of activation markers such as CD44, CD69, CD122 and CD62L. The typical markers of Tregs CTLA-4 and GITR were also highly expressed by the CD4+ CD25+ cells, which is consistent with the concept that Tregs, even when naive, have the same phenotype of an activated cell.10,12,19,20
The internalization of apoptotic cells was able to confer on DCs resistance to maturation by LPS, a phenomenon that occurs in tolerogenic DCs. Unlike necrotic cells, apoptotic cells are known to be incapable of inducing DC maturation,6,21 although some studies show the opposite effect in which apoptotic blebs, derived from apoptotic cells, induce DC maturation.22 Interleukin-12 is an important cytokine involved in the development of acquired immunity playing a role in inducing the Th1 subtype of lymphocytes.23 As a pro-inflammatory cytokine, high amounts of IL-12 can exacerbate autoimmune processes such as multiple sclerosis in mice24 and its production and secretion can be stimulated by the activation of DCs and macrophages by bacterial compounds such as LPS. Our results show a role of the apoptotic cells in modulating IL-12-producing cells, decreasing their percentage after stimulation with LPS. It has been shown that LPS-stimulated macrophages pulsed with apoptotic cells decrease the production of p35 IL-12 mRNA,25 and here we show that this inhibition is also valid for DCs, even if just for intracellular staining.
In our study, by rendering the DCs immature and resistant to maturation, apoptotic cells are able to induce tolerance by the expansion of cells with regulatory phenotype, such as Tregs expanded in vitro. It has been shown that DCs pulsed with apoptotic DCs are able to expand CD4+ Foxp3+ cells with regulatory properties.26,27 Here we used apoptotic thymocytes instead of apoptotic DCs. The absence of DC maturation upon phagocytosis of apoptotic cells and induction of cells with regulatory properties were also observed. There is evidence that DC interaction with the phosphatidylserine from the apoptotic cells induces the production of TGF-β1,28 and modulates the maturation of human DCs,29 probably increasing the population of CD4+ CD25+ Foxp3+ cells. However, the use of splenocytes as apoptotic cells to feed DCs does not increase the induction of Tregs in vitro. This suggests that not only the phosphatidylserine but also the cell type are responsible for tolerance induction.30 In fact, some studies have shown that the interaction with DCs is not sufficient to induce production of TGF-β1.29–31 In our case, the production of TGF-β alone was not enough to convert Foxp3− into Foxp3+ cells, once the transwell chambers abrogated contact between DCs and T lymphocytes, but allowed the cytokines to pass through the membrane. These results suggest that membrane-bound TGF-β, in LAP+ DCs, could play a crucial role in inducing the expression of Foxp3 and the expansion of regulatory T cells.
The Tregs induced by the alloantigen-pulsed DCs were able to modulate the proliferation of splenocytes in vitro in both specific and non-specific suppression assays. In the specific suppression assay the higher suppression was observed when effector cells highly outnumbered Tregs (1 : 25 and 1 : 50 of Treg : effector cell ratio). This result contrasts with several studies showing that Tregs are more suppressive in the lower ratios of Tregs : effector cells.8,10,32 Here, this was observed when Tregs were added to the polyclonal and DO11.10 suppression assays. In these assays, the proliferation of the splenocytes was restored when the Treg : effector cell ratio was raised. The production of TGF-β does not seem to be the mechanism through which Tregs exert their suppressive effect. As reported, the suppression mechanisms of human and murine Tregs might not be mediated by TGF-β because of the requirement for cell contact and the failure to reverse suppression with neutralizing anti-TGF-β.19,32–35
The inoculation of cells from spleen and lymph node depleted of CD4+ CD25+ into lymphopenic mice is able to induce autoimmunity in several organs, as reported by various authors.12,13 In our model, the CD4+ CD25− cells induced cell infiltrate in several organs and the co-transfer of CD4+ CD25+ cells prevented the induction of autoimmunity in the stomach, colon, liver and kidneys. Protection from inflammatory bowel disease has been a well-known function of Tregs and this effect is dependent on the production of IL-10,8,36 but not on TGF-β.8 Also, the co-transfer of Tregs impaired the proliferation of cells in the lymph nodes of athymic Nude mice, which is consistent with reports of Tregs blocking the homeostatic proliferation of activated cells.37
Nude mice that received CD4+ CD25− cells had a total cell count in the spleen similar to control mice, whereas mice that received both Tregs and effector cells had an increase in total cell count. This phenomenon is consistent with reports of retention of pathogenic T cells in the spleen of mice transferred with Tregs and effector cells,38,39 suggesting that Tregs may act not only by blocking the proliferation of pathogenic T-cell clones but also by keeping these cells inside the lymphoid organs, which impairs their migration to target organs and the development of autoimmune disease. The impaired proliferation in both lymph nodes and spleen might be a mechanism by which the Tregs exert their function in vivo, by preventing the proliferation of potential pathogenic cells both in lymphoid organs and sites of inflammation.
In all mice transferred with either effector cells or Tregs and effector cells, the weight gain was similar. The development of gastritis and colitis in mice that received CD4+ CD25− cells was not capable of changing the weight gain of these animals, the gain being similar to that in control and Treg-treated mice. Itoh et al.12 reported the same results with Nude mice transferred with CD4+ CD25− cells, which showed no difference in body weight gain. In other models of autoimmunity induction using lymphopenic mice such as RAG−/− and SCID mice, the transfer of cells with no apparent regulatory activity led to at least colitis and body weight loss.12,37,40–44
Altogether, the data presented in this work can elucidate some of the mechanisms by which dendritic cells and apoptotic cells are able to induce tolerance and be part of the process of peripheral tolerance. These results may contribute to the development of a new therapeutic approach in transplantation tolerance, and prevention or treatment of autoimmune diseases.
Acknowledgments
This work was supported by grants from the National Council for Scientific and Technologic Development (CNPq) and Fundação de Amparo à Pesquisa do Estado de São Paulo. The authors would like to thank Christina Arslanian Kubo for technical assistance, Paulo Albe for the histology and Dr Luciana Cavalheiro Marti for reviewing the manuscript. The authors would like to state that there were no conflicts of interest on performing the experiments and during the preparation of the manuscript. PNPD #0188085 to Peron JPS and Sardinha LR.
Glossary
Abbreviations
- ALLO
allogeneic apoptotic cell
- APO
apoptotic cell
- DC
dendritic cell
- Foxp3
gene forkhead box P3
- GM-CSF
granulocyte–macrophage colony-stimulating factor
- iDC
immature dendritic cell
- IL-10
interleukin-10
- LAP
TGF-β1-latency associated peptide
- LPS
lipopolysaccharide
- mDC
mature dendritic cell
- RAG
recombination activating gene
- SCID
severe combined immunodeficiency
- SYN
syngeneic apoptotic cell
- TGF-β
transforming growth factor β
- Treg
regulatory T cell
Disclosures
The authors declare no financial or conflict of interest.
Supporting Information
Additional Supporting Information may be found in the online version of this article:
Figure S1. Immature dendritic cells were incubated with allogeneic apoptotic thymocytes at a 1 : 5 (DCs : apoptotic cells) ratio for 18 hr. DCs were co-cultured with syngeneic total lymph node cells for 5 days (1 : 5 DC : lymph-node cell ratio). Cells were collected and labeled with fluorescent antibodies for CD4, CD25, Foxp3 CD122, CD69, CD44, CTLA-4, GITR, and CD62L (gate on CD4+ cells).
Figure S2. Cytokine analysis in the supernatants of immature iDC or mDC and the same cells incubated with allogeneic or syngeneic apoptotic thymocytes. Supernatants were harvested and the production of TGF-β was measured in triplicate of each experimental condition. Results are presented in mean ± SD and are representative of three independent experiments. ***P < 0·0005.
Please note: Wiley-Blackwell are not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than about missing material) should be directed to the corresponding author for the article.
References
- 1.Bach FH, Alter BJ, Schendel DJ, Segall M, Bach ML. Genetic and cellular control of in vitro models of allograft reactivity. Birth Defects Orig Artic Ser. 1975;11:467–76. [PubMed] [Google Scholar]
- 2.Shortman K, Liu YJ. Mouse and human dendritic cell subtypes. Nat Rev Immunol. 2002;2:151–61. doi: 10.1038/nri746. [DOI] [PubMed] [Google Scholar]
- 3.Yamazaki S, Iyoda T, Tarbell K, et al. Direct expansion of functional CD25+ CD4+ regulatory T cells by antigen-processing dendritic cells. J Exp Med. 2003;198:235–47. doi: 10.1084/jem.20030422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang X, Li M, Lian D, et al. Generation of therapeutic dendritic cells and regulatory T cells for preventing allogeneic cardiac graft rejection. Clin Immunol. 2008;127:313–21. doi: 10.1016/j.clim.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Gallucci S, Lolkema M, Matzinger P. Natural adjuvants: endogenous activators of dendritic cells. Nat Med. 1999;5:1249–55. doi: 10.1038/15200. [DOI] [PubMed] [Google Scholar]
- 6.Steinman RM, Turley S, Mellman I, Inaba K. The induction of tolerance by dendritic cells that have captured apoptotic cells. J Exp Med. 2000;191:411–6. doi: 10.1084/jem.191.3.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sauter B, Albert ML, Francisco L, Larsson M, Somersan S, Bhardwaj N. Consequences of cell death: exposure to necrotic tumor cells, but not primary tissue cells or apoptotic cells, induces the maturation of immunostimulatory dendritic cells. J Exp Med. 2000;191:423–34. doi: 10.1084/jem.191.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fontenot JD, Rasmussen JP, Gavin MA, Rudensky AY. A function for interleukin 2 in Foxp3-expressing regulatory T cells. Nat Immunol. 2005;6:1142–51. doi: 10.1038/ni1263. [DOI] [PubMed] [Google Scholar]
- 9.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–61. doi: 10.1126/science.1079490. [DOI] [PubMed] [Google Scholar]
- 10.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+ CD25+ regulatory T cells. Nat Immunol. 2003;4:330–6. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 11.Lipscomb MW, Taylor JL, Goldbach CJ, Watkins SC, Wesa AK, Storkus WJ. DC expressing transgene Foxp3 are regulatory APC. Eur J Immunol. 2010;40:480–93. doi: 10.1002/eji.200939667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Itoh M, Takahashi T, Sakaguchi N, et al. Thymus and autoimmunity: production of CD25+ CD4+ naturally anergic and suppressive T cells as a key function of the thymus in maintaining immunologic self-tolerance. J Immunol. 1999;162:5317–26. [PubMed] [Google Scholar]
- 13.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3+ CD25+ CD4+ regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J Exp Med. 2005;201:723–35. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25) Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–64. [PubMed] [Google Scholar]
- 15.Voll RE, Herrmann M, Roth EA, Stach C, Kalden JR, Girkontaite I. Immunosuppressive effects of apoptotic cells. Nature. 1997;390:350–1. doi: 10.1038/37022. [DOI] [PubMed] [Google Scholar]
- 16.Marguti I, Yamamoto GL, da Costa TB, Rizzo LV, de Moraes LV. Expansion of CD4+ CD25+ Foxp3+ T cells by bone marrow-derived dendritic cells. Immunology. 2009;127:50–61. doi: 10.1111/j.1365-2567.2008.02927.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu C, Wang Q, Liu F, et al. The allogeneic but not syngeneic dendritic cells effectively generated regulatory T cells from total CD4+ population without exogenous cytokines. Scand J Immunol. 2010;71:12–9. doi: 10.1111/j.1365-3083.2009.02334.x. [DOI] [PubMed] [Google Scholar]
- 18.Yamazaki S, Inaba K, Tarbell KV, Steinman RM. Dendritic cells expand antigen-specific Foxp3+ CD25+ CD4+ regulatory T cells including suppressors of alloreactivity. Immunol Rev. 2006;212:314–29. doi: 10.1111/j.0105-2896.2006.00422.x. [DOI] [PubMed] [Google Scholar]
- 19.Takahashi T, Kuniyasu Y, Toda M, et al. Immunologic self-tolerance maintained by CD25+ CD4+ naturally anergic and suppressive T cells: induction of autoimmune disease by breaking their anergic/suppressive state. Int Immunol. 1998;10:1969–80. doi: 10.1093/intimm/10.12.1969. [DOI] [PubMed] [Google Scholar]
- 20.McHugh RS, Whitters MJ, Piccirillo CA, et al. CD4+CD25+ immunoregulatory T cells: gene expression analysis reveals a functional role for the glucocorticoid-induced TNF receptor. Immunity. 2002;16:311–23. doi: 10.1016/s1074-7613(02)00280-7. [DOI] [PubMed] [Google Scholar]
- 21.Peng Y, Martin DA, Kenkel J, Zhang K, Ogden CA, Elkon KB. Innate and adaptive immune response to apoptotic cells. J Autoimmun. 2007;29:303–9. doi: 10.1016/j.jaut.2007.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fransen JH, Hilbrands LB, Ruben J, et al. Mouse dendritic cells matured by ingestion of apoptotic blebs induce T cells to produce interleukin-17. Arthritis Rheum. 2009;60:2304–13. doi: 10.1002/art.24719. [DOI] [PubMed] [Google Scholar]
- 23.Trinchieri G, Wysocka M, D'Andrea A, et al. Natural killer cell stimulatory factor (NKSF) or interleukin-12 is a key regulator of immune response and inflammation. Prog Growth Factor Res. 1992;4:355–68. doi: 10.1016/0955-2235(92)90016-b. [DOI] [PubMed] [Google Scholar]
- 24.Leonard JP, Waldburger KE, Schaub RG, et al. Regulation of the inflammatory response in animal models of multiple sclerosis by interleukin-12. Crit Rev Immunol. 1997;17:545–53. [PubMed] [Google Scholar]
- 25.Kim S, Elkon KB, Ma X. Transcriptional suppression of interleukin-12 gene expression following phagocytosis of apoptotic cells. Immunity. 2004;21:643–53. doi: 10.1016/j.immuni.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 26.Kushwah R, Oliver JR, Zhang J, Siminovitch KA, Hu J. Apoptotic dendritic cells induce tolerance in mice through suppression of dendritic cell maturation and induction of antigen-specific regulatory T cells. J Immunol. 2009;183:7104–18. doi: 10.4049/jimmunol.0900824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kushwah R, Wu J, Oliver JR, et al. Uptake of apoptotic DC converts immature DC into tolerogenic DC that induce differentiation of Foxp3+ Treg. Eur J Immunol. 2010;40:1022–35. doi: 10.1002/eji.200939782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huynh ML, Fadok VA, Henson PM. Phosphatidylserine-dependent ingestion of apoptotic cells promotes TGF-beta1 secretion and the resolution of inflammation. J Clin Invest. 2002;109:41–50. doi: 10.1172/JCI11638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X, Doffek K, Sugg SL, Shilyansky J. Phosphatidylserine regulates the maturation of human dendritic cells. J Immunol. 2004;173:2985–94. doi: 10.4049/jimmunol.173.5.2985. [DOI] [PubMed] [Google Scholar]
- 30.Morelli AE, Larregina AT. Apoptotic cell-based therapies against transplant rejection: role of recipient's dendritic cells. Apoptosis. 2010;15:1083–97. doi: 10.1007/s10495-010-0469-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takahashi M, Kobayashi Y. Cytokine production in association with phagocytosis of apoptotic cells by immature dendritic cells. Cell Immunol. 2003;226:105–15. doi: 10.1016/j.cellimm.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 32.Thornton AM, Shevach EM. Suppressor effector function of CD4+ CD25+ immunoregulatory T cells is antigen nonspecific. J Immunol. 2000;164:183–90. doi: 10.4049/jimmunol.164.1.183. [DOI] [PubMed] [Google Scholar]
- 33.Thornton AM, Shevach EM. CD4+ CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–96. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Read S, Mauze S, Asseman C, Bean A, Coffman R, Powrie F. CD38+ CD45RBlow CD4+ T cells: a population of T cells with immune regulatory activities in vitro. Eur J Immunol. 1998;28:3435–47. doi: 10.1002/(SICI)1521-4141(199811)28:11<3435::AID-IMMU3435>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 35.Stephens GL, McHugh RS, Whitters MJ, et al. Engagement of glucocorticoid-induced TNFR family-related receptor on effector T cells by its ligand mediates resistance to suppression by CD4+ CD25+ T cells. J Immunol. 2004;173:5008–20. doi: 10.4049/jimmunol.173.8.5008. [DOI] [PubMed] [Google Scholar]
- 36.Asseman C, Mauze S, Leach MW, Coffman RL, Powrie F. An essential role for interleukin 10 in the function of regulatory T cells that inhibit intestinal inflammation. J Exp Med. 1999;190:995–1004. doi: 10.1084/jem.190.7.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Levings MK, Sangregorio R, Roncarolo MG. Human CD25+CD4+ T regulatory cells suppress naive and memory T cell proliferation and can be expanded in vitro without loss of function. J Exp Med. 2001;193:1295–302. doi: 10.1084/jem.193.11.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murakami M, Sakamoto A, Bender J, Kappler J, Marrack P. CD25+ CD4+ T cells contribute to the control of memory CD8+ T cells. Proc Natl Acad Sci USA. 2002;99:8832–7. doi: 10.1073/pnas.132254399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matejuk A, Buenafe AC, Dwyer J, et al. Endogenous CD4+ B V8S2– T cells from TG BV8S2+ donors confer complete protection against spontaneous experimental encephalomyelitis (Sp-EAE) in TCR transgenic, RAG-/- mice. J Neurosci Res. 2003;71:89–103. doi: 10.1002/jnr.10450. [DOI] [PubMed] [Google Scholar]
- 40.Powrie F, Leach MW, Mauze S, Caddle LB, Coffman RL. Phenotypically distinct subsets of CD4+ T cells induce or protect from chronic intestinal inflammation in C.B-17 SCID mice. Int Immunol. 1993;5:1461–71. doi: 10.1093/intimm/5.11.1461. [DOI] [PubMed] [Google Scholar]
- 41.Powrie F, Leach MW. Genetic and spontaneous models of inflammatory bowel disease in rodents: evidence for abnormalities in mucosal immune regulation. Ther Immunol. 1995;2:115–23. [PubMed] [Google Scholar]
- 42.Read S, Malmstrom V, Powrie F. Cytotoxic T lymphocyte-associated antigen 4 plays an essential role in the function of CD25+CD4+ regulatory cells that control intestinal inflammation. J Exp Med. 2000;192:295–302. doi: 10.1084/jem.192.2.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Read S, Powrie F. Induction of inflammatory bowel disease in immunodeficient mice by depletion of regulatory T cells. Curr Protoc Immunol. 2001 doi: 10.1002/0471142735.im1513s30. Chapter 15:Unit 15.13. [DOI] [PubMed] [Google Scholar]
- 44.Inaba K, Inaba M, Romani N, et al. Generation of large numbers of dendritic cells from mouse bone marrow cultures supplemented with granulocyte/macrophage colony-stimulating factor. J Exp Med. 1992;176:1693–702. doi: 10.1084/jem.176.6.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


