Abstract
Objective
Millions of adults in the United States travel abruptly across time zones each year. Nevertheless, the impact of traveling over relatively short distances (across 3 or fewer time zones) on diurnal patterning of typical physiological response patterns has yet to be studied in a large, epidemiological sample.
Design
The current research focuses on 764 middle-aged men comparing variations in diurnal cortisol regulation based on number of time zones traveled eastward or westward the day before.
Main Outcome Measure
Participants provided samples of salivary cortisol at waking, 30-min postwaking, 10 a.m., 3 p.m., and bedtime.
Results
Eastward travel was associated with a steeper salivary cortisol awakening response ( p < .01) and lower peak (PEAK) levels of salivary cortisol the next morning ( p < .05). Westward travel was associated with lower peak levels of cortisol the next morning ( p < .05). Effect sizes for these differences ranged from Cohen’s d = .29 to .47. Differences were not present for 2 days in their home environment.
Conclusions
The results provide evidence that traveling across time zones is associated with diurnal cortisol regulation and should be studied further to understand the subsequent impacts on health and well-being in large national samples.
Keywords: jet lag, cortisol diumal rhythms, travel
Millions of people travel across time zones each year for business and pleasure. In 2001, U.S. residents reported an average of nine long distance trips per person per year with a median length of 210 (SE = 3) miles (Department of Transportation [USDOT], 2001). Fatigue, disturbance in sleep, and anxiety have all been associated with traveling long distances (Boulos et al., 1995; Cho, Ennaceur, Cole, & Suh, 2000; Gander, Nguyen, Rosekind, & Connell, 1993; Waterhouse, Reilly, & Atkinson, 1997). These symptoms, commonly referred to as “jet lag,” are attributed to the desynchronization of the circadian rhythm in the body due to changes in the light and dark cycle. Jet lag is associated with lack of alertness, poor sleep, irritability, stress, impaired performance in athletes, and depressed mood (Waterhouse et al., 1997). The degree of jet lag varies by the number of time zones crossed and direction of travel; eastward travel is associated with slower acclimation to the new time zone than westward travel (Boulos et al., 1995; Minors & Waterhouse, 1981). Jet lag has been of interest to those concerned with the productivity and health of frequent business travelers (Striker, Dimberg, & Liese, 2000); frequent travelers have higher rates of insurance claims for psychological problems, infectious diseases, back disorders, and injuries than nontravelers, and the number of claims increases with the number of trips (Liese, Mundt, Dell, Nagy, & Demure, 1997). Several studies have determined that travel across times zones alters hormonal patterns linked to circadian rhythm, such as diurnal rhythms of melatonin and cortisol (Cho, 2001; Cho et al., 2000; Klein & Wegmann, 1974; Lemmer, Kern, Nold, & Lohrer, 2002; Winget, DeRoshia, & Holley, 1985). Of particular interest may be jet-lag effects on the diurnal rhythm of cortisol, a stress hormone and a primary product of the hypothalamic-pituitary-adrenal axis (HPA axis; Kirschbaum & Hellhammer, 1989), as cortisol levels have been associated with individual differences in physical and mental health (for review, see Sapolsky, Romero, & Munck, 2000), and aging (Van Cauter, Leproult, & Kupfer, 1996). Previous studies of jet lag and cortisol have found that cortisol diurnal rhythms have been altered by flights over six or more times zones either westward or eastward (Bullock, Martin, Ross, Rosemond, & Marino, 2007; Klein & Wegmann, 1974; Lemmer et al., 2002; Winget et al., 1985). Other research on jet lag and cortisol has drawn links between repeated long-term flights, elevated cortisol levels after such flights, and later cognitive deficits (Cho, 2001; Cho et al., 2000). In general, results from previous studies provide estimates of 1 day of recovery needed for every one to two time zones crossed for circadian rhythms to adjust (Bullock et al., 2007; Eastman, Gazda, Burgess, Crowley, & Fogg, 2005; Loat & Rhodes, 1989). Although prior studies have demonstrated associations between jet lag and cortisol, most have been conducted on small, selective samples of less than 25 participants. None have examined the associations between cortisol and jet lag within a large national sample of community participants and with control days in their own naturalistic settings. Furthermore, the majority of these studies have examined chronic jet lag (i.e., many trips within a short amount of time) or extreme jet lag (i.e., travel over six or more time zones). Given that only a small minority of long-distance trips cross more than three time zones (Department of Transportation, 2001), prior research may not generalize to the average traveler. The current research focuses on a large sample of middle-aged men, comparing variations in diurnal cortisol regulation based on number of time zones traveled eastward or westward. This study addresses the following questions: (a) Are cortisol diurnal rhythms altered by domestic travel across three or fewer time zones?; (b) does this vary by eastward or westward travel?; and (c) are there potential confounds such as mood, sleep quality and disturbances, and wake time that can account for the dysregulation of the cortisol rhythms?
Method
Participants
The sample for this study included a subset of male monozygotic and dizygotic twins who took part in the Vietnam Era Twin Study of Aging (VETSA). VETSA has been described in detail elsewhere (Kremen et al., 2006). Briefly, VETSA twins were randomly selected for recruitment from a pool of 3,322 twin pairs in the Vietnam Era Twin Registry who served in the U.S. military during the Vietnam era (1965 to 1975) and who took part in a study of psychological health in 1992 (Tsuang, Bar, Harley, & Lyons, 2001). These individuals were not selected as VA patients and most were never in combat (Kremen et al., 2006). There were 1,237 participants in the VETSA. The majority (97.4%) traveled to Boston or San Diego for 1 day of interviews and physical and cognitive assessments. VETSA participants were between the ages of 51 and 60 (M = 55.9, SD = 2.58). Eighty-eight percent of the sample was White, 4.3% African American, 2.9% Hispanic, 0.9% Native American, and 0.4% Pacific Islander. Compared to U.S. Census Data from 2003 for men in their 50s (U.S. Census Bureau, 2003), the VETSA participants are similar to the larger U.S. population of men in this age range based on demographic (age, education, income, marital status, employment) and health data (prevalence of chronic health problems, diabetes, and hypertension). Two years after the VETSA study began, we initiated an additional study to understand the role of hormonal dysregulation as a risk factor for cognitive aging. Approximately one third (N = 442) of VETSA participants had already been studied and were ineligible for the additional cortisol study. Of the remaining 795, 786 (98.9%) participated in the study.
Procedures and Measures
Saliva sampling and diary reports
Participants completed salivary collection at home on 2 nonconsecutive “typical” working days at least 2 to 3 weeks prior to coming to the lab, and then also provided samples on their day of testing in the lab (DOT). For the at-home saliva collection, cortisol kits were mailed via courier and participants received a reminder call to ensure that lab materials were received, to go over procedures, and to answer any questions. On the days at home participants were asked to provide samples at wake up, 30-min postwaking, 10:00 am, 3:00 p.m., and 9:00 p.m. or bedtime. They provided samples by passive drool until they had provided at least 2.25 ml of saliva. If necessary, the participant chewed Trident gum to stimulate saliva and removed the gum prior to providing the sample. Participants stored and refrigerated their saliva samples in an insulated lunch bag included with the cortisol kits. At the end of the 2 days, they sent the saliva samples via overnight mail to the University of California, Davis to be assayed. Participants also provided saliva samples on the DOT. They received their materials the day before the DOT when they arrived at the hotel, and provided saliva samples at wake up, 30-min postwaking, 10 a.m., prior to lunch, following lunch, 3 p.m., and bedtime. The 10 a.m., 3 p.m., and pre- and postlunch collections occurred while participants were in the lab for testing.
Assay procedures
Salivary assays were estimated in duplicate using commercial radioimmunoassasy kits (Siemens Medical Solutions Diagnostics, Los Angeles, CA). Intra- and interassay coefficients of variation are 3.96 and 5.66, respectively. All saliva samples from each individual participant were assayed together in batches containing one to three individuals. Three individuals were excluded due to lost (n = 1) or contaminated (n = 2) samples, resulting in a final sample of N = 783. Of the 13,311 possible samples (17 time points × 783 individuals), 149 (1.0%) of samples were missing due to participant lapses or technical problems, and 22 samples (0.1%) were coded as missing because they had values greater than 50 nanomols per liter (nmol/L; Nicolson, 2008). Cortisol values were positively skewed (skewness range = 1.7 to 20.1) and were log transformed to approximate normality.
Jet-lag data
To participate in the DOT, almost all participants traveled to either Boston or San Diego by plane. Jet lag was calculated as lab time zone minus home time zone, and ranged from −3 (east-to-west travel) to +3 (west-to-east). One participant traveled 8 time zones west and was excluded from the analyses. In addition, jet-lag values were coded as missing for 12 participants who could not travel and were studied in their home towns. Six individuals did not provide at least three cortisol samples on the day of testing and therefore were not included in these analyses. Of the remaining 764 participants, approximately one third (34.4%, n = 263) did not cross time zones for the DOT, 24.7% (n = 189) traveled from west-to-east, and the remaining 312 participants (40.8%) traveled east-to-west.
Covariates
As part of the cortisol collection procedure, participants were asked to record whether they had smoked, eaten, drank alcohol, taken medication, or exercised before each sample. Responses at each time were coded as 0 (no) or 1 (yes). Accordant with prior research (Kirschbaum, Wust, & Strasburger, 1992), smoking prior to the sample was the only variable consistently related to cortisol level. In addition, data were collected on several variables that might be confounded with jet-lag effects, including wake time on the DOT, difference (in hours) between average wake time on the home days and wake time on the DOT, number of hours slept prior to the DOT, sleep quality on the night prior to the DOT, and negative mood during the DOT. Sleep quality was assessed by asking participants how well they slept the night before at the morning cortisol sample. Responses were provided on a 4-point scale ranging from 1 (very well) to 4 (quite poor). Mood was assessed by asking participants to report in a log the extent they felt sleepy, happy, depressed, frustrated, anxious, excited, and angry before each sample. Responses were provided on a 5-point Likert scale ranging from 1 (not at all) to 5 (extremely). Negative mood was created with a standardized composite of average sleepy, depressed, frustrated, and angry responses on the DOT (α = .66). Finally, high levels of depressed mood, as measured by the Center for Epidemiologic Studies Depression Scale (CES–D; score >16; Radloff, 1977), and history of posttraumatic stress disorder (PTSD) were also investigated as possible covariates that might influence cortisol level and/or susceptibility to jet-lag effects.
Data preparation
Cortisol follows a predictable diurnal rhythm with relatively high levels at wake time, followed by an increase of 50 to 60% in the 20 to 40 min after waking, a rapid decline in the subsequent few hours, and a slower decrease throughout the remainder of the day to reach the lowest point near midnight (Pruessner et al., 1997). We simulated this growth curve pattern using the statistical program WinBUGS (Spiegelhalter, Thomas, Best, & Lunn, 2004). WinBUGS uses Markov Chain Monte Carlo, which allowed us to control for the nonindependence of samples introduced when individuals were assayed in batches, and further allowed us to include nicotine use as a time-varying covariate in the analysis. To account for the batch effects, we set the ith assayed value of the jth twin by Yijk, where the subscript k further indicates the batch in which the value was assayed such that assays in the same batch have the same value of k. We used each participant’s log-transformed cortisol values at each time point to model the cortisol slope from wake up to the peak (cortisol awakening response, CAR), the maximum cortisol peak of the day (PEAK), and the exponential decay after the peak until bedtime (DECAY), while also accounting for batch and nicotine use. Models were run for the days at home and DOT separately. Parameter estimates for CAR, PEAK, and DECAY for each participant were then exported for use as the main dependent variables in all analyses.
Statistical analyses
Analyses were conducted using SPSS 15.0. We used a mixed-model approach to account for the correlated observations among participants from the same family, using a repeated-measures analysis of variance (ANOVA) with jet-lag group as the between-participants factor, family as the repeated random effect, and the three cortisol parameters derived from the simulated growth curve analyses (CAR, PEAK, DECAY) as the outcomes of interest. Models were run for the days at home as a preliminary test of between-group differences prior to travel. The statistical significance for all post hoc tests was p < .05. Variables that may be confounded with jet-lag effects (see above) and that differed significantly across jet-lag groups were used as covariates in all analyses.
Results
Preliminary Analyses
Groups traveling 1- (n = 37), 2- (n = 131), or 3- (n = 144) hr westward did not differ significantly from one another. Specifically, CAR for the three westward groups (1 to 3) was 0.567 (SD = .006), 0.568 (SD = .007), and 0.568 (SD = .006), respectively, F(2, 257) = 0.415, p = .661, PEAK was 2.451 (SD = .288), 2.459 (SD = .305), 2.446 (SD = .282), respectively, F(2, 261) = 0.067, p = .935, and DECAY was 0.113 (SD = .034), 0.111 (SD = .031), and 0.113 (SD = .027), respectively, F(2, 249) = 0.103, p = .902.
Similarly, groups traveling 1- (n = 124), 2- (n = 16), or 3- (n = 49) hr eastward did not differ significantly from one another. In the eastward groups (1 to 3) the CAR was 0.570 (SD = .007), 0.572 (SD = .006), and 0.573 (SD = .006), respectively, F(2, 167) = 1.881, p = .156, PEAK was 2.439 (SD = .272), 2.418 (SD = .320), 2.405 (SD = .276), respectively, F(2, 140) = 0.390, p = .678, and DECAY was 0.108 (SD = .027), 0.106 (SD = .028), and 0.102 (SD = .032), respectively, F(2, 161) = 0.765, p = .467. Thus, our primary analysis of jet-lag effects was based on three groups: travel west (TW, n = 312), no time zone difference (0T, n = 263), and travel east (TE, n = 189).
Covariate analyses
Negative mood, sleep quality, depressive symptoms, and PTSD did not vary by jet-lag group, whereas wake time, difference between wake time at home, and wake time on DOT, and hours of sleep did vary significantly by jet-lag group (see Table 1). Thus, wake time, difference in wake time, and hours of sleep were included as covariates in the DOT analyses. CAR and PEAK were associated with hours of sleep (r = −.159, p = .002, r = .081, p = .027). CAR and DECAY were associated with the difference in wake time at home and wake time on DOT (r = −.201, p = .002, r = .087, p = .016).
Table 1.
Means and Standard Deviations and Repeated Analysis of Variance F Statistics for Cortisol Parameters on Day of Testing by Jet Lag
| Jet-lag group | Full sample (minimum, maximum) |
1 hr to 3 hr westwarda |
No time zone crossedb | 1 hr to 3 hr eastwardc | F/χ2(df), p value |
|---|---|---|---|---|---|
| Wake time (Hours postmidnight) |
5:53 a.m. (47 min) (2:30 a.m., 9:25 a.m.) |
5:42 a.m. (49 min) | 5:59 a.m. (38 min) | 6:02 a.m. (51 min) | 9.347 (2, 478) <.001 |
| Wake time difference between test day and days at home (Hours) |
11 min (2 hr, 36 min) (−18 hr, 31 min; 6 hr, 38 min) |
1 hr, 39 min (2 hr, 16 min) | −13 min (1 hr., 54 min.) | −1 hr, 45 min (2 hr., 3 min.) | 154.479 (2, 492) <.001 |
| Hours of Sleep (Hours) |
7 hr, 19 min (1 hr, 32 min) (1 hr 18 min, 13 hr 25 min) |
7 hr, 34 min (1 hr, 26 min) | 7 hr, 8 min (1 hr, 41 min) | 7 hr, 6 min (1 hr, 20 min) | 6.540 (2, 608) .002 |
| Sleep Quality (Range 1 to 4; 1 [high] to 4 [indicating low quality]) |
2.053 (0.752) (1.00, 4.00) |
2.077 (0.772) | 2.023 (0.713) | 2.058 (0.787) | 0.171 (2, 554) .843 |
| Negative mood (Standardized factor score) |
0.000 (1.000) (−1.203, 12.764) |
−0.005 (0.943) | −0.041 (1.025) | 0.024 (0.943) | 0.599 (2, 516) .55 |
| Clinical levels of Depressive symptoms (% of sample) |
14% (34.8%) (0, 1) |
14.6% (35.4%) | 13.9% (34.6%) | 13.2% (33.9%) | 0.193 (2) .908 |
| Posttraumatic stress disorder (% of sample) |
7.5% (26.4%) (0, 1) |
6.3% (24.4%) | 10.5% (30.7%) | 5.3% (22.4%) | 5.349 (2) .069 |
| CAR sloped | 0.569 (0.007) (0.546, 0.593) |
0.568 (0.006) | 0.569 (0.007) | 0.571 (0.007) | 5.373 (2, 626) .0048 |
| PEAK valued | 2.461 (0.291) (1.416, 3.469) |
2.440 (0.291) | 2.509 (0.297) | 2.442 (0.276) | 4.201 (2, 631) .0154 |
| DECAY across the dayd | 0.111 (0.028) (−.034, 0.164) |
0.111 (0.029) | 0.113 (0.025) | 0.107 (0.028) | 2.021 (2, 568) .1135 |
Note. N = 764. Standard deviations are given in parentheses. CAR = cortisol awakening response; PEAK = maximum cortisol peak of the day; DECAY = exponential decay after the peak until bedtime.
n = 312.
n = 263.
n = 189.
Slope and maximum values are estimates from the growth curve analysis of log cortisol (nmol/L) that were batch-and-nicotine-adjusted.
Jet-lag effects on at-home cortisol rhythms
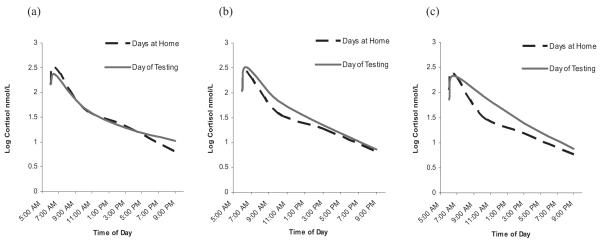
Average, log-transformed cortisol values across the two at-home days are shown by the dashed lines of panels a, b, and c of Figure 1 for the westward, no time zone, and eastward groups, respectively. We ran preliminary mixed model ANOVAs on the CAR, PEAK, and DECAY parameters for the days at home to ensure that there were no a priori differences between the jet-lag groups. As expected, no significant differences were found between the groups on any of the cortisol parameters, CAR: F(2, 552) = 0.541, p = .583, PEAK: F(2, 540) = 1.766, p = .176, DECAY: F(2, 553) = 1.201, p = .302.
Figure 1.
Cortisol rhythms on the days at home and the day of testing for (a) westward travel group, (b) no time zones crossed group, and (c) eastward travel group.
Jet-Lag Effects on DOT Cortisol Rhythms
Average, log-transformed cortisol values across the three jet-lag groups on the DOT are shown by the solid lines in Figure 1. ANOVA revealed a significant main effect of jet-lag group on the CAR, F(2, 626) = 5.373, p = .005, a main effect of jet-lag group for PEAK, F(2, 631) = 4.201, p = .015, and no main effect of jet-lag group on DECAY, F(2, 568) = 2.021, p = .133. Table 2 shows the effect sizes (Cohen’s d) and p values for each of the post hoc comparisons across group for CAR and PEAK. For CAR, those that traveled TE had significantly steeper CAR slopes than all of the other groups (0T: d = .29; TW: d = .47). For PEAK, those that did not cross time zones (0T) had significantly higher peak values than all of the other groups (TW: d = .15; TE: d = .19). See Table 2 for significant contrasts between groups.
Table 2.
Cohen’s d Effect Sizes Between Jet-Lag Groups for Covariate Mixed-Model Analysis of Variance
| Jet-lag group comparison | CAR slope | PEAK value |
|---|---|---|
| Travel westward and no time zones crossed Cohen’s d |
.15 p = .114 |
.15 p = .013 |
| Travel eastward and no time zones crossed Cohen’s d |
.29 p = .009 |
.19 p = .026 |
| Travel eastward and travel westward Cohen’s d |
.47 p = .001 |
.04 p = .950 |
Note. Slope and maximum values are estimates from the growth curve analysis of log cortisol (nmol/L) that were batch-and-nicotine-adjusted. CAR = cortisol awakening response; PEAK = maximum cortisol peak of the day.
Discussion
These results indicate that short-distance domestic travel across three or fewer time zones is associated with deviations in cortisol diurnal rhythms in a large sample of middle-aged men.
Furthermore, associations remained after accounting for possible confounds such as sleep quality and timing, wake times, and mood across the day. Demonstration of these disturbances for travel across relatively short distances is important as previous research has linked chronic long-term disturbances associated with jet lag to stress related outcomes, psychological disturbances and cognitive deficits (Cho, 2001; Cho et al., 2000; Winget, DeRoshia, Markley, & Holley, 1984). Participants who traveled eastward had significantly steeper CAR slopes than participants who did not cross a time zone prior to their day of testing and those who traveled westward. Participants who traveled westward had the flattest CAR; however, they were only significantly different than the eastward travel group. Participants who traveled eastward woke almost 2 hr earlier than they normally did at home and participants traveling westward woke approximately an hour and a half later than they normally did at home. Our results are therefore consistent with prior research demonstrating steeper CAR slopes among early versus late awakeners (Edwards, Evans, Hucklebridge, & Clow, 2001; Kudielka & Kirschbaum, 2003; Williams, Magid, & Steptoe, 2005). However, our analyses included both wake time and difference in wake time between at-home and DOT as covariates, so the increase in CAR among the eastward travel group is due to more than just a shift in normal wake time. We found it interesting that the majority (66%) of the eastward travel group only crossed one time zone; in contrast, 80% of the westward travel group crossed two to three time zones. Yet, the eastward travel group had an effect size that was nearly twice as large as the westward travel group, and was significantly different from the no time zone crossed group. This indicates that an effect size of .29 for the eastward travel group (as compared to the no time zone crossed group) may actually be attenuated and that the true differences may be even larger. These eastward versus westward travel findings from the present study are therefore consistent with prior literature on long distance travel that found that eastward travel was associated with slower acclimation to the new time zone than westward travel (Boulos et al., 1995; Minors & Waterhouse, 1981).
Participants traveling eastward and westward also had lower peak values than those who did not cross a time zone prior to their day of testing. These results suggest that the actual peak of the CAR was missed for both groups. The eastward travel group may have peaked after the sampling and the westward travel group may have peaked prior to the sampling point. The CAR is of particular interest as individual differences in the size of the CAR are substantial, and there is evidence of both genetic and psychosocial contributions to these differences (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Clow, Thorn, Evans, & Hucklebridge, 2004; Fries, Dettenborn, & Kirschbaum, 2009; Shulz, Kirschbaum, Preussner, & Hellhammer, 1998; Wüst, Federenko, Hellhammer, & Kirschbaum, 2000). The results in this study indicated that there is significant variation between groups in their CAR slopes, ranging from small to medium effect sizes that are not otherwise accounted for by other covariates. It has been estimated that short term alterations to diurnal cycles based on changing wake times may be adaptive rather than harmful; however when conceptualized as a form of allostatic load (McEwen, 1998), we hypothesize that long-term or chronic shifts to diurnal patterns associated with frequent business travel might begin to mimic the physiological, psychological, and cognitive deficits that have been associated with extreme long distance travel or chronic travel.
Limitations
Although the present study suggests short-term alterations in diurnal patterning of physiological response due to travel across relatively short distances, we note that we do not have consecutive posttravel days of cortisol sampling and therefore, cannot ascertain whether recovery time and return to normal circadian rhythms are different based on the number of time zones traveled and in which direction. Because the VETSA includes only men from the Vietnam War era, results may not generalize to women or to a younger population. However, 77% of business trips are made by men according to the Department of Transportation’s National Household Travel Survey (2000–2001) so we are able to generalize to a larger population that travels frequently (Department of Transportation, 2001). A final limitation may be that participants were drawn from a study of military veterans. However, the majority of participants did not engage in combat, and the VETSA participants are similar to the larger U.S. population of men in their age range. Moreover, although some of these men (n = 59) had a history of PTSD, this was not significantly associated with jet-lag group membership and thus did not introduce bias into our results. Prior research on jet lag has used small, highly selected samples. To our knowledge this is the first study of a large national sample to demonstrate associations between cortisol diurnal rhythms and circadian disrhythmia as a result of domestic travel. Several interventions have been developed to lessen the effects of jet lag by undergoing “preflight” adjustments such as light exposure treatment (Eastman et al., 2005; Haimov & Arendt, 1999; see Waterhouse, Reilly, & Edwards, 2004, for review). Results of this study should encourage the dissemination of strategies to alleviate jet-lag symptoms to a larger population base that frequently travels across time zones. Furthermore, this study highlights the sensitivity of the HPA-axis to environmental changes and stressors, underscoring the need for continued exploration into short- and long-term consequences of chronic stressors and repeated activation of this system.
Contributor Information
Leah D. Doane, Department of Psychiatry and Behavioral Neuroscience, University of Chicago
William S. Kremen, Department of Psychiatry and Center for Behavioral Genomics, University of California, San Diego and VA San Diego Healthcare System, San Diego, California
Lindon J. Eaves, Virginia Institute for Behavioral and Psychiatric Genetics, Virginia Commonwealth University
Seth A. Eisen, Department of Veterans Affairs, Washington, DC and Departments of Internal Medicine and Psychiatry, Washington University
Richard Hauger, Department of Psychiatry, University of California, San Diego and VA San Diego Healthcare System, San Diego, California.
Dirk Hellhammer, Department of Psychobiology, University of Trier.
Seymour Levine, Department of Psychology, University of California, Davis.
Sonia Lupien, Center for Studies on Human Stress, Centre de recherché Fernand-Séguin, University of Montréal.
Michael J. Lyons, Department of Psychology, Boston University
Sally Mendoza, Department of Psychology, University of California, Davis.
Elizabeth Prom-Wormley, Virginia Institute for Behavioral and Psychiatric Genetics, Virginia Commonwealth University.
Hong Xian, St. Louis VA Medical Center, St. Louis, Missouri and Department of Internal Medicine, Washington University.
Timothy P. York, Virginia Institute for Behavioral and Psychiatric Genetics, Virginia Commonwealth University
Carol E. Franz, Department of Psychiatry, University of California, San Diego
Kristen C. Jacobson, Department of Psychiatry and Behavioral Neuroscience, University of Chicago
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. The Periodicals of the National Academy of Sciences. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulos Z, Campbell S, Lew A, Terman M, Dijk D-J, Eastman CI. Light treatment for sleep disorders: Consensus report. VIII. Jet lag. Journal of Biological Rhythms. 1995;10:167–176. doi: 10.1177/074873049501000209. [DOI] [PubMed] [Google Scholar]
- Bullock N, Martin DT, Ross A, Rosemond D, Marino F. Effects of long haul travel on maximal spring performance and diurnal variations in elite skeleton athletes. British Journal of Sports Medicine. 2007;41:569–573. doi: 10.1136/bjsm.2006.033233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho K. Chronic “jet lag” produces temporal lobe atrophy and spatial cognitive deficits. Nature Neuroscience. 2001;4:567–568. doi: 10.1038/88384. [DOI] [PubMed] [Google Scholar]
- Cho K, Ennaceur A, Cole JC, Suh CH. Chronic jet lag produces cognitive deficits. Journal of Neuroscience. 2000;20:1–5. doi: 10.1523/JNEUROSCI.20-06-j0005.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clow A, Thorn L, Evans P, Hucklebridge F. The awakening cortisol response: Methodological issues and significance. Stress: The International Journal on the Biology of Stress. 2004;7:29–37. doi: 10.1080/10253890410001667205. [DOI] [PubMed] [Google Scholar]
- Department of Transportation (USDOT) Bureau of Transportation Statistics (BTS) Transportation Statistics Annual Report. Vol. 1998. Author; Washington, DC: 1998. [Google Scholar]
- Department of Transportation (USDOT) Research and Innovative Technology Administration, Bureau of Transportation Statistics and USDOT, Federal Highway Administration National household travel survey data. 2001. [CD–ROM]
- Eastman CI, Gazda CJ, Burgess HJ, Crowley SJ, Fogg LF. Advancing circadian rhythms before eastward flight: A strategy to prevent or reduce jet lag. Sleep. 2005;28:33–44. doi: 10.1093/sleep/28.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards S, Evans P, Hucklebridge F, Clow A. Association between time of awakening and diurnal cortisol secretory activity. Psychoneuroendocrinology. 2001;26:613–622. doi: 10.1016/s0306-4530(01)00015-4. [DOI] [PubMed] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): Facts and future directions. International Journal of Psychophysiology. 2009;72:67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Haimov I, Arendt A. The prevention and treatment of jet lag. Sleep Medicine Reviews. 1999;3:229–240. doi: 10.1016/s1087-0792(99)90004-7. [DOI] [PubMed] [Google Scholar]
- Gander P, Nguyen D, Rosekind M, Connell L. Age, circadian rhythms and sleep loss in flight crews. Aviation, Space, and Environmental Medicine. 1993;64:189–195. [PubMed] [Google Scholar]
- Kirschbaum C, Hellhammer DH. Salivary cortisol in psychobiological research: An overview. Neuropsychobiology. 1989;22:150–169. doi: 10.1159/000118611. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Wust S, Strasburger C. Normal” cigarette smoking increases free cortisol in habitual smokers. Life Sciences. 1992;50:435–442. doi: 10.1016/0024-3205(92)90378-3. [DOI] [PubMed] [Google Scholar]
- Klein KE, Wegmann HN. The resynchronization of human circadian rhythms after transmeridian flights as a result of flight direction and mode of activity. In: Sheving LE, Halberg F, Pauly JF, editors. Chronobiology. Igaku Shoin; Tokyo, Japan: 1974. pp. 564–570. [Google Scholar]
- Kremen W, Thompson-Brenner H, Leung Y, Grant M, Franz C, Eisen S, Lyons M. Genes, environment and time: The Vietnam era twin study of aging (VETSA) Twin Research and Human Genetics. 2006;9:1009–1022. doi: 10.1375/183242706779462750. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Kirschbaum C. Awakening cortisol responses are influenced by health status and awakening time but not by menstrual cycle phase. Psyschoneuroendocrinology. 2003;28:35–47. doi: 10.1016/s0306-4530(02)00008-2. [DOI] [PubMed] [Google Scholar]
- Lemmer B, Kern R, Nold G, Lohrer H. Jet lag in athletes after eastward and westward time-zone transition. Chronobiology International. 2002;19:743–764. doi: 10.1081/cbi-120005391. [DOI] [PubMed] [Google Scholar]
- Liese B, Mundt KA, Dell LD, Nagy L, Demure B. Medical insurance claims associated with international business travel. Occupational and Environmental Medicine. 1997;54:499–503. doi: 10.1136/oem.54.7.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loat CE, Rhodes EC. Jet-lag and human performance. Sports Medicine. 1989;8:226–238. doi: 10.2165/00007256-198908040-00003. [DOI] [PubMed] [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Minors D, Waterhouse K. Circadian rhythms and the human. Wright; Bristol, England: 1981. [Google Scholar]
- Nicolson NA. Measurement of cortisol. In: Luecken LJ, Gallo LC, editors. Handbook of physiological research methods in health psychology. Sage; Thousand Oaks, CA: 2008. pp. 37–74. [Google Scholar]
- Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, Kirschbaum C. Free cortisol levels after awakening: A reliable biological marker for the assessment of adrenocortical activity. Life Sciences. 1997;61:2539–2549. doi: 10.1016/s0024-3205(97)01008-4. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES–D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;3:385–401. [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- Schulz P, Kirschbaum C, Pruessner J, Hellhammer D. Increased free cortisol secretion after awakening in chronically stressed individuals due to work overload. Stress Medicine. 1998;14:91–97. [Google Scholar]
- Spiegelhalter D, Thomas A, Best N, Lunn D. WinBUGS user manual. version 2.0 Imperial College and Medical Research Council; London, England: 2004. [Google Scholar]
- Striker J, Dimberg L, Liese BH. Stress and business travel: Individual, managerial, and corporate concerns. Journal of Organizational Excellence. 2000;20:3–8. [Google Scholar]
- Tsuang MT, Bar JL, Harley RM, Lyons MJ. The Harvard twin study of substance abuse: What we have learned. Harvard Review of Psychiatry. 2001;9:267–279. [PubMed] [Google Scholar]
- U.S. Census Bureau [Retrieved January 12, 2009];Population estimates. 2003 from http://www.census.gov/popest/national.
- Van Cauter E, Leproult R, Kupfer DJ. Effects of gender and age on the levels and circadian rhythmicity of plasma cortisol. Journal of Clinical Endocrinology and Metabolism. 1996;81:2468–2473. doi: 10.1210/jcem.81.7.8675562. [DOI] [PubMed] [Google Scholar]
- Waterhouse J, Reilly T, Atkinson G. Jet-lag. Lancet. 1997;350:1611–1615. doi: 10.1016/S0140-6736(97)07569-7. [DOI] [PubMed] [Google Scholar]
- Waterhouse J, Reilly T, Edwards B. The stress of travel. Journal of Sports Sciences. 2004;22:946–966. doi: 10.1080/02640410400000264. [DOI] [PubMed] [Google Scholar]
- Williams E, Magid K, Steptoe A. The impact of time of waking and concurrent subjective stress on the cortisol response to awakening. Psychoneuroendocrinology. 2005;31:312–324. doi: 10.1016/j.psyneuen.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Winget CM, DeRoshia CW, Holley DC. Circadian rhythms and athletic performance. Medicine & Science in Sports & Exercise. 1985;17:498–516. [PubMed] [Google Scholar]
- Winget CM, DeRoshia CW, Markley CL, Holley DC. A review of human physiological and performance changes associated with desynchronosis of biological rhythms. Aviation, Space and Environmental Medicine. 1984;55:1085–1096. [PubMed] [Google Scholar]
- Wüst S, Federenko I, Hellhammer DH, Kirschbaum C. Genetic factors, perceived chronic stress, and the free cortisol response to awakening. Psychoneuroendocrinology. 2000;25:707–720. doi: 10.1016/s0306-4530(00)00021-4. [DOI] [PubMed] [Google Scholar]