Abstract
Korean American women’s breast cancer screening rates are low, and the rates among older Korean American women are even lower. This article describes health beliefs related to older Korean American women’s screening behaviors, comparing them to beliefs of younger Korean American women. The 73 women age 65 and older had significantly different health beliefs than the 114 women between ages 40 and 64. Further, older women’s perceptions of the seriousness of the disease and benefits of and barriers to taking action to prevent the disease predated their screening behaviors. Interventions to change the health beliefs of older Korean American women are suggested.
It is generally known that early detection through screening can improve the survival rate and quality of life of individuals with breast cancer (American Cancer Society, 2007), and this is the main reason the U.S. Preventive Services Task Force (2002) recommends annual mammography screening for women age 40 and older. However, Asian American women, including Korean American women, have the lowest cancer screening rates of all ethnic groups (Kagawa-Singer & Pourat, 2000; Wu, Guthrie, & Bancroft, 2005). The screening rates vary from study to study, but 48% to 78% of Korean American women had ever had a mammogram, and 15% to 50% were estimated to have had a mammogram in the preceding year (Han, Williams, & Harrison, 2000; Juon, Choi, & Kim, 2000; Juon, Kim, Shankar, & Han, 2004; Kim & Sarna, 2004; Kim, Jeong, & Kim, 2004; Lee, Fogg, & Sadler, 2006; Maxwell, Bastani, & Warda, 2000; Sarna, Tae, Kim, Brecht, & Maxwell, 2001; Wismer et al., 1998). The mammography screening rates are even lower among Korean American women age 65 and older: 12% to 69% had ever had a mammogram, and 7% to 35% were estimated to have had a mammogram in the preceding year (Juon et al., 2004; Juon, Seo, & Kim, 2002; Lee et al., 2006).
Although specific breast cancer incidence rates among Korean American women by age group are not available, older Korean American women are believed to be at higher risk for breast cancer than younger Korean American women because in American women in general, the incidence of breast cancer increases with age (American Cancer Society, 2007). According to the National Institutes of Health (2008), in the United States, 1 in 28 women age 60 to 70 and 1 in 24 women age 70 to 80 develops breast cancer, whereas only 1 in 257 women younger than age 40 develops breast cancer. One study estimated that by 2030, two thirds of patients with breast cancer will be older than age 65 (Stewart & Foster, 1989). Therefore, increasing breast cancer incidence rates among older women in the United States and older Korean American women’s low screening rates will most likely put older Korean American women at risk for breast cancer.
LITERATURE REVIEW
Several factors related to breast cancer screening rates among older women in the United States have been identified in the literature. Women who were more educated, married, or had a higher income were more likely to have had screenings than their counterparts (Caplan & Haynes, 1996; Edwards & Jones, 2000; Mayer et al., 1992). In addition, older women who were less disabled, less depressed, more anxious about the test, and had less activity limitation were more likely to obtain a mammogram (Caplan & Haynes, 1996; Edwards & Jones, 2000). Older women who received routine checkups without symptoms or had a regular source of care were more likely to get mammograms (Caplan & Haynes, 1996; Juon et al., 2002; Mayer et al., 1992; Wismer et al., 1998). Fear of discovering a potentially serious condition, such as cancer (Morisky, Fox, Murata, & Stein, 1989), also affected rates of mammography in older women.
Although older Korean American women reported much lower screening rates than younger Korean American women (Juon et al., 2002, 2004), the reason for the lower screening rates is not well described or understood. It is well documented that Korean women’s beliefs and attitudes toward breast cancer screening tests are related to their low participation rate in breast cancer screenings (Im, Park, Lee, & Yun, 2004; Noh, Kim, Yoon, Oh, & Choe, 1998; Ryu, Kyu, Kim, & Koo, 1994). It appears that Korean American women’s health beliefs related to breast cancer and screening are influenced by their culture (Juon et al., 2004; Lee, Tripp-Reimer, Miller, Sadler, & Lee, 2007).
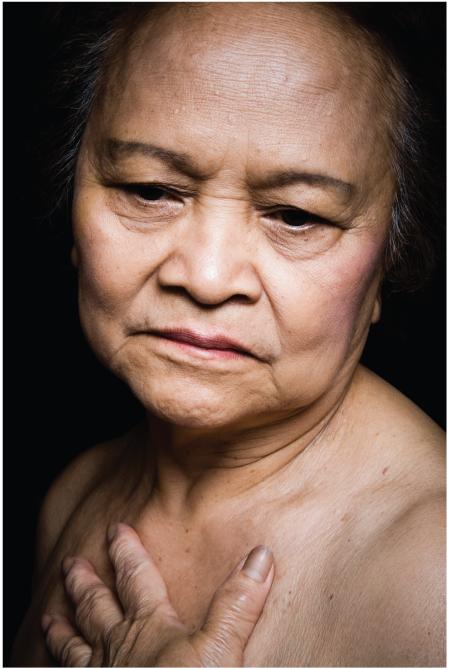 © 2009 iStockPhoto.com/azndc
© 2009 iStockPhoto.com/azndc
This study was guided by the Health Belief Model (HBM). The HBM has been used to explain and predict cancer screening behavior and various other health promotion behaviors (Janz, Champion, & Strecher, 2002). Perceived susceptibility to developing a disease, seriousness of the disease, benefits of taking action to prevent the disease, and barriers to taking action comprise the HBM constructs (Janz et al., 2002). Among those constructs of the HBM, Korean American women who had never had a mammogram reported significantly higher levels of barriers and lower levels of benefits than women who had one (Han et al., 2000).
STUDY PURPOSE
The purpose of this study is two-fold: to identify whether health beliefs differ between older and younger Korean American women, and if they do, to determine how the different health beliefs contribute to the lower breast cancer screening rates in older Korean American women. Nurses in clinical and educational settings play a key role in promoting adherence to screening guidelines. Information obtained from this study will be helpful to nurses in designing and implementing age- and culture-appropriate interventions for improving Korean American women’s breast cancer screening behaviors.
METHOD
This cross-sectional telephone survey was designed to collect information on beliefs and behaviors related to breast cancer screening among 187 Korean American women in Cook County, Illinois, from December 2003 to March 2004.
Sample and Procedures
A search for the most common Korean last names (e.g., Kim, Lee, Park, Jung, Cho, Choi) resulted in more than 2,200 names in the Chicago directory. After human subjects review approval was obtained from the University, telephone calls were made to those with Korean surnames to find out whether any Korean American woman in the household met the inclusion criteria of being age 40 or older and born in Korea. Only 630 of the 2,200 telephone calls were answered. Among the 630 households that answered, many did not contain women who met the inclusion criteria (n = 280, 44%). Among those who were eligible (n = 350), 42% (n = 148) refused to participate in the study, resulting in a 58% response rate, and 15 gave incomplete answers. Finally, a total of 187 Korean American women participated in the study.
Among counties in the United States, Cook County has the fifth largest number of Koreans, with a total of 34,546 (U.S. Census Bureau, 2000). All Korean American women in the sample were immigrants from Korea. In 2000, 78% of Korean Americans in Illinois were foreign born, and 85% of Korean Americans spoke a language other than English at home, most likely Korean (U.S. Census Bureau, 2000). The 22% of non-immigrant Korean Americans are most likely second generation and younger than age 40. In this study, older Korean American women were defined as women age 65 and older, and younger Korean American women were defined as women age 40 to 64.
The project was explained to Korean American women who met the inclusion criteria, and then they were invited to participate in the survey. Verbal agreement to participate in this study on the telephone was considered consent to participate in the study. All of the telephone interviews were conducted in Korean, and each structured interview lasted 20 to 30 minutes. The questionnaire asked for demographic information and about breast cancer screening behaviors, including health care access and beliefs related to breast cancer and screening.
Measures
The dependent variables measured participants’ self-report on the following two questions:
Have you ever had a mammogram?
Have you had a mammogram within the preceding year?
Independent variables of age, marital status, education, employment status, and household income were included in the analysis as sociodemographic characteristics. The variables in this study were post hoc recategorization of data due to a relative small sample and the possibility of using the variables in the logistic regression analysis if any of them were significantly correlated with the outcome variable. An income of $55,000 was chosen as the cut-off for household income because it was the median income.
Age was categorized by two groups: 40 to 64 and 65 and older. Marital status was categorized as married or not married; education was categorized as having completed high school or less or education beyond high school; employment status was categorized as employed or unemployed; household income was categorized as less than $55,000 or equal to or greater than $55,000; and religion was categorized as Protestant or non-Protestant.
Level of acculturation was measured by years of residence in the United States (less than 20 years or 20 years or longer), proportion of life spent in the United States (less than 25% or more than 25%), and English-speaking ability (none/little, some, well/fluent). Health-related questions included health status (poor, fair, good, excellent), coverage by health insurance (yes or no), insurance coverage for mammograms if they had had one (entire cost, some coverage, no coverage, don’t know), usual source of care (i.e., having a regular doctor or place to go for health care) (yes or no), and having routine checkups within the preceding 2 years, even when they were not sick (yes or no).
Health beliefs were measured by the Korean-language HBMS-K, which is a modified version of Champion’s (1993, 1999) Health Belief Model scale (HBMS) to make the HBMS-K culturally appropriate and sensitive. The HBMS-K has four subscales of susceptibility, seriousness, benefits, and barriers, which are composed of 4 items (Cronbach’s alpha coefficient = 0.85), 9 items (Cronbach’s alpha coefficient = 0.79), 5 items (Cronbach’s alpha coefficient = 0.70), and 14 items (Cronbach’s alpha coefficient = 0.69), respectively. The concept of barrier in the barrier subscale includes various domains (e.g., transportation, language, embarrassment), which could result in the relatively lower Cronbach’s alpha coefficient of that subscale.
An item added in the susceptibility subscale was, “As I get older, my chances of getting breast cancer are greater.” Two items added in the HBMS-K seriousness subscale were, “If I had breast cancer, it would interrupt my family harmony,” and “If I don’t think about breast cancer, I will not get it.” One item, “Having a mammogram will give me peace of mind about my health (or will ensure me that I am OK),” was added in the benefit subscale. Six items were added in the barrier subscale, examples of which are “I don’t have a symptom to get a mammogram” and “I don’t think it is necessary for me to receive a mammogram.”
The modified English version of the HBMS was translated and transcribed into Korean by a trained bilingual research assistant. The Korean version was then back-translated into English by another bilingual individual who was unaware of the intent and the concepts underlying the instruments. No significant discrepancies were noted between the different language versions. Scoring for the revised HBMS-K was the same as the original HBMS—using a 5-point scale with response options ranging from 1 (strongly disagree) to 5 (strongly agree). Summed values with higher scores indicate higher levels of belief in susceptibility and seriousness of getting breast cancer and beliefs in benefits of mammography, as well as increases in barriers to getting a mammogram.
Data Analysis
Data were analyzed using SPSS version 15.0 for descriptive statistics, a series of chi-square analyses, bivariate analyses, and independent t tests to compare dependent and independent variables between older and younger Korean American women. Logistic regression analysis was conducted in two phases separately for each age group of women to determine whether different variables predict Korean American women’s screening behaviors by age group. The first phase examined point biserial correlation coefficients between the independent variables (sociodemographics, health-related characteristics, and the four beliefs of the HBM) and outcome variables (have had a mammogram). In the second phase of analysis, the significant bivariate predictors of the outcomes were entered into a multiple logistic regression analysis. Step-wise logistic regression analysis was conducted where the full model had all predictors included. Wald statistics were used to determine what variables significantly predicted the outcome variable of Korean American women having had a mammogram. Statistical differences are reported in this article only when p < 0.05.
For the logistic regression analysis of a relatively small sample of 73 older women, we examined power to detect differences in the sample. Among 187 participants in this study, only 68.5% of older women and 83.3% of the younger women had ever had a mammogram. This is a difference of 14.8% between the two samples. The confidence interval (CI) for a rate of 68.5% using a sample of 93 (a rounded-down estimate of half of 187) is a CI of 59% to 78%, which has an upper bound far below the 83.3% estimate for the younger women in our sample. Thus, this sample was capable of detecting differences in proportions of approximately 10% or more. Most of the significant differences found in this study were near or above 10%. It is likely that more significant differences could be detected if a larger sample were examined, and we suggest this for future research.
In addition, the independent measures of seriousness, susceptibility, benefits, and barriers were all treated as continuous predictors in the logistic regression. The odds ratios (OR) in the tables are based on the standardized regression coefficients of these predictors. Each one-unit change in the standard scores for these predictors resulted in an increase or decrease in the probability of a woman obtaining a mammogram, and those probabilities correspond to the reported OR.
This format for presenting these kinds of results is fairly standard in refereed journals, but many authors argue for a more meaningful method of presenting them. Hosmer and Lemeshow (1989) argued for examining a table of probability changes over a “reasonable” interval. In their discussion, they specifically discussed how changes in age can change the probability of an outcome, and they suggested using a 5-, 10-, or 20-year interval to show such changes. Of course, the choice of any of these intervals could well be considered arbitrary, as Hosmer and Lemeshow (1989) themselves pointed out.
The problem with something like the barriers scale is that there is even less of a reasonable unit to use to demonstrate changes in the likelihood that a woman would obtain a mammogram than in the Hosmer and Lemeshow (1989) example using age. So while we would like to explicate this relationship more clearly, based on the problems associated with such an analysis, we are pessimistic about the prospects of actually being able to do so.
FINDINGS
Sample Characteristics
Detailed descriptions of the overall sample characteristics are described elsewhere (Lee et al., 2006). The total sample of 187 Korean American women consisted of 114 younger women and 73 older women. The mean age of younger women was 50.8 (SD = 7.2 years), and the mean age of older women was 74.8 (SD = 6.8 years).
To understand the differences in mammography utilization patterns between the two age groups, the participants’ sociodemographic and health-related variables were compared using chi-square analysis (Table 1). Significant differences were found in most of the sociodemographic and health-related variables for older and younger Korean American women. Older Korean American women were less likely to be married and employed; they were also less educated and had lower incomes. Caution is required in income reporting because only 65% of young women and 44% of older women responded to the annual household income question. The proportion of life spent in the United States for older Korean American women was significantly less than for their younger counterparts. A significantly higher proportion of older Korean American women reported that they could not speak English at all or only a little (80.8%) compared with younger Korean American women (36%).
TABLE 1. SOCIODEMOGRAPHIC AND HEALTH-RELATED CHARACTERISTICS OF OLDER (n = 73) AND YOUNGER (n = 114) KOREAN AMERICAN WOMEN.
| Characteristic | Age Group | χ 2 | p value | |
|---|---|---|---|---|
| older women n (%) |
younger women n (%) |
|||
| Marital status | 75.87 | 0.000 | ||
| Married | 24 (32.9) | 106 (93) | ||
| Not married | 49 (67.1) | 8 (7) | ||
| Education | 39.76 | 0.000 | ||
| High school diploma or less | 56 (76.7) | 37 (32.5) | ||
| Higher than high school diploma | 11 (15.1) | 70 (61.4) | ||
| Missing data | 6 (8.2) | 7 (6.1) | ||
| Employment | 47.32 | 0.000 | ||
| Unemployed | 71 (97.3) | 56 (49.1) | ||
| Employed | 2 (2.7) | 58 (50.9) | ||
| Household income | 34.34 | 0.000 | ||
| <$55,000 | 26 (35.6) | 15 (13.2) | ||
| ≥ 55,000 | 6 (8.2) | 59 (51.7) | ||
| Missing data | 41 (56.2) | 40 (35.1) | ||
|
Years of residence in United
States |
||||
| <20 | 28 (38.4) | 57 (50) | 2.43 | 0.119 |
| ≥ 20 | 45 (61.6) | 57 (50) | ||
|
Proportion of life spent in United
States |
7.02 | 0.007 | ||
| <25% | 31 (42.5) | 27 (23.7) | ||
| ≥ 25% | 42 (57.5) | 87 (76.3) | ||
| English-speaking ability | 40.57 | 0.000 | ||
| None/little | 59 (80.8) | 41 (36) | ||
| Some | 13 (17.8) | 38 (33.3) | ||
| Well/fluent | 1 (1.4) | 35 (30.7) | ||
| Health status | 12.83 | 0.000 | ||
| Poor/fair | 70 (95.9) | 86 (75.4) | ||
| Good/excellent | 3 (4.1) | 27 (23.7) | ||
| Missing data | 0 (0) | 1 (0.9) | ||
| Health insurance | 20.75 | 0.000 | ||
| Yes | 69 (94.5) | 75 (65.8) | ||
| No | 4 (5.5) | 39 (34.2) | ||
|
Insurance coverage of mammo-
gram a |
20.19 | 0.000 | ||
| Entire cost | 54 (78.3) | 33 (44) | ||
| Some coverage | 12 (17.4) | 25 (33.3) | ||
| No coverage | 0 (0) | 7 (9.3) | ||
| Don’t know | 3 (4.3) | 10 (13.3) | ||
| Usual source of care | 17.12 | 0.002 | ||
| Yes | 65 (89) | 65 (57) | ||
| No | 8 (11) | 49 (43) | ||
|
Routine checkup in preceding 2
years |
2.03 | 0.154 | ||
| Yes | 56 (76.7) | 75 (65.8) | ||
| No | 17 (23.3) | 39 (34.2) | ||
Note. Percentages may not equal 100 due to rounding.
Older women, n = 69; younger women, n = 75.
Almost all older Korean American women reported their health as poor or fair (95.9%) and had health insurance (94.5%). Among those who had health insurance, the insurance was more likely to cover the entire cost of their mammograms than the younger women’s health insurance. Older women (89%) were more likely than younger women (57%) to have a regular doctor or a regular place to go for health care, but there were no significant differences between the two age groups in routine checkups in the preceding 2 years.
Mammography Utilization
Table 2 shows the results of chi-square analyses of the comparisons of mammography utilization and other related variables between the two groups. Older women were significantly less likely to have ever had a mammogram: 68.5% of older women and 83.3% of younger women had had a mammogram. However, there was no difference between the two groups for the rates of having had a mammogram in the preceding year.
TABLE 2. COMPARISON OF MAMMOGRAPHY UTILIZATION AND RELATED CHARACTERISTICS BETWEEN OLDER (n = 73) AND YOUNGER (n = 114) KOREAN AMERICAN WOMEN.
| Age group | χ 2 | p value | ||
|---|---|---|---|---|
| Characteristic | Older Women n (%) | Younger Women n (%) | ||
| Mammogram | 5.63 | 0.018 | ||
| Have had one | 50 (68.5) | 95 (83.3) | ||
| Never had one | 23 (31.5) | 19 (16.7) | ||
| Mammogram in the preceding year a | 0.41 | 0.523 | ||
| Yes | 23 (46) | 49 (51.6) | ||
| No | 27 (54) | 46 (48.4) | ||
Older women, n = 50; younger women, n = 95.
Health Beliefs Related to Breast Cancer and Screening
Health beliefs related to breast cancer and screening measured by the HBMS-K (susceptibility, seriousness, benefits, and barriers subscales) were compared using independent t tests between the two age groups (Table 3). The two groups had significantly different health beliefs about breast cancer and screening on all four HBMS-K subscales. Older women had a significantly lower level of susceptibility and benefits and a higher level of seriousness and barriers compared with the younger women.
TABLE 3. COMPARISON OF HEALTH BELIEFS ABOUT BREAST CANCER AND SCREENING BETWEEN OLDER (n = 73) AND YOUNGER (n = 114) KOREAN AMERICAN WOMEN BY AGE.
| Health Belief | Age Group | Meana (SD) | t test | p value |
|---|---|---|---|---|
| Susceptibility | Older | 2.335 (0.433) | −2.949 | 0.004 |
| Younger | 2.546 (0.535) | |||
| Seriousness | Older | 3.290 (0.432) | 3.026 | 0.003 |
| Younger | 3.089 (0.457) | |||
| Benefits | Older | 3.608 (0.337) | −3.986 | 0.000 |
| Younger | 3.787 (0.274) | |||
| Barriers | Older | 2.305 (0.234) | 6.375 | 0.000 |
| Younger | 2.115 (0.171) |
Mean scores on the Korean-language Health Belief Model scale (Janz, Champion, & Strecher, 2002) range from 1 (strongly disagree) to 5 (strongly agree).
Health beliefs among the older and younger groups of Korean American women who had had a mammogram and those who had never had one were also examined (Table 4). Older women who had had a mammogram had significantly higher levels of perceived seriousness and benefits and a lower level of perceived barriers than women who had never had a mammogram. Among younger women, those who had mammograms had a significantly lower level of perceived barriers than women who never had a mammogram.
TABLE 4. COMPARISON OF HEALTH BELIEFS ABOUT BREAST CANCER AND MAMMOGRAM USE BETWEEN OLDER (n = 73) AND YOUNGER (n = 114) KOREAN AMERICAN WOMEN.
| Health Beliefs | Older Women | Younger Women | ||||
|---|---|---|---|---|---|---|
| Yes (n = 50) | No (n = 23) | t (p value) | Yes (n = 95) | No (n = 19) | t (p value) | |
| Meana (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Susceptibility | 2.325 (0.429) | 2.358 (0.451) | −0.301 (0.765) | 2.539 (0.533) | 2.578 (0.559) | −0.283 (0.780) |
| Seriousness | 3.375 (0.385) | 3.106 (0.479) | 2.565 (0.012) | 3.076 (0.457) | 3.154 (0.460) | −0.654 (0.519) |
| Benefits | 3.704 (0.292) | 3.400 (0.341) | 3.616 (0.001) | 3.793 (0.269) | 3.757 (0.302) | 0.479 (0.636) |
| Barriers | 2.268 (0.145) | 2.534 (0.217) | −6.089 (0.000) | 2.144 (0.152) | 2.371 (0.174) | −5.287 (0.000) |
Mean scores on the Korean-language Health Belief Model scale (Janz, Champion, & Strecher, 2002) range from 1 (strongly disagree) to 5 (strongly agree).
As the first phase of logistic regression analysis, point biserial correlation coefficients were examined by conducting bivariate analyses separately for the two age groups. Among older women, no sociodemographic variables were associated with having had a mammogram, but health-related variables of having a usual source of care, receiving a routine checkup, and all four health beliefs about breast cancer and screening were associated with the outcome variable. Among younger women, education, health insurance, a usual source of care, routine checkups, and all four beliefs about breast cancer and screening variables were associated with having had a mammogram. Therefore, all variables associated with the outcome variable of having had a mammogram were entered into the final model in each group. Due to the small number of older women who had had a mammogram in the preceding year, it was not possible to conduct a logistic regression analysis.
Using forward Wald procedures, the final model for older women included the variables of perceived barriers, seriousness, and benefits as predictors (Table 5). Older women who had a higher level of perceived barriers were significantly less likely to have had a mammogram (OR = 0.07, 95% CI = 0.01 to 0.41). In other words, older women who had lower levels of perceived barriers were 14 times more likely to have had a mammogram than those women who had higher levels of barriers. Those women who had higher levels of seriousness and benefits were more likely to have had a mammogram (OR = 4.59, 4.79, respectively) (Table 5).
TABLE 5. LOGISTIC REGRESSION ANALYSIS: PREDICTORS OF MAMMOGRAMS AMONG OLDER KOREAN AMERICAN WOMEN (n = 73).
| Variable | β | SE | Wald | df | Signifcance | Exp (B) | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Higher | ||||||||
| Barriers | −2.581 | 0.867 | 8.866 | 1 | 0.003 | 0.076 | 0.07 | 0.01 | 0.41 |
| Seriousness | 1.525 | 0.685 | 4.954 | 1 | 0.026 | 4.596 | 4.59 | 1.20 | 17.59 |
| Benefits | 1.568 | 0.746 | 4.414 | 1 | 0.036 | 4.796 | 4.79 | 1.11 | 20.70 |
| Constant | 1.252 | 0.834 | 2.253 | 1 | 0.133 | 3.498 | |||
Note. CI = confdence interval; Exp = exponent; OR = odds ratio; SE = standard error.
Similar to older women, younger women who had higher levels of perceived barriers were significantly less likely to have had a mammogram (OR = 0.15, 95% CI = 0.03 to 0.59) (Table 6) than those who had lower levels of perceived barriers. In other words, younger women who had lower levels of perceived barriers were 6.6 times more likely to have had a mammogram than those women who perceived more barriers. Younger women who had routine checkups in the preceding 2 years were also significantly more likely to have had a mammogram (OR = 4.68, 95% CI = 1.39 to 15.69) compared with those who had not had routine checkups.
TABLE 6. LOGISTIC REGRESSION ANALYSIS: PREDICTORS OF MAMMOGRAMS AMONG YOUNGER KOREAN AMERICAN WOMEN (n = 114).
| Variable | β | SE | Wald | df | Signifcance | Exp (B) | OR | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|
| Lower | Higher | ||||||||
| Barriers | −1.892 | 0.698 | 7.340 | 1 | 0.007 | 0.151 | 0.15 | 0.03 | 0.59 |
| Routine checkups | 1.544 | 0.671 | 6.258 | 1 | 0.012 | 4.682 | 4.68 | 1.39 | 15.69 |
| Constant | 1.994 | 0.677 | 8.679 | 1 | 0.003 | 7.342 | |||
Note. CI = confdence interval; Exp = exponent; OR = odds ratio; SE = standard error.
DISCUSSION
Although annual mammograms can reduce mortality from breast cancer (Shootman, Jeffe, Lian, Aft, & Gillanders, 2008; Weinberger et al., 1991), breast cancer screening rates among Korean American women, especially older Korean American women, remain low. In this study, only 68.5% of older Korean American women and 83.3% of younger Korean American women had ever had a mammogram. Further, only 31.5% of older and 43% of younger Korean American women had a mammogram in the preceding year, similar to findings from a previous study (Juon et al., 2004). The screening rates among Korean American women reported in the literature have increased steadily (Juon et al., 2002, 2004; Wismer et al., 1998). However, the mammography screening rates in the preceding year of Korean American women in this study (43% among the younger women and 31.5% among the older women), are still much lower than women in United States in general. In 2005, 48% of American women in the 40-to-49 age group, 56% in the 50-to-64 age group, and 50% in the 65+ group had had a mammogram in the preceding year (American Cancer Society, 2007). Those rates are still lower than the goal of more than 70% identified in Healthy People 2010 (U.S. Department of Health and Human Services, 2000). Continuous efforts are needed to increase the annual mammography rate for Korean American women. The outcome variable of having had a mammogram was significant between the two age groups, but the outcome variable of having had a mammogram in the preceding year was not different, which could be related to the relatively small sample of women who had had a mammogram in the preceding year. Further research is warranted.
Health beliefs were different between older and younger Korean American women on all of four subscales of the HBMS-K. On three of four subscales (seriousness, benefits, and barriers), there was a difference between older women who had and those who had never had a mammogram, whereas perceived barriers were the only difference between younger women who had had a mammogram and those who had never had one. Further, perceived barriers, benefits, and seriousness predicted older women’s having had a mammogram, whereas for younger women, only barriers predicted their outcome variable, along with the variable of having routine checkups even when they were not sick. Therefore, it is likely that different health beliefs, especially higher levels of perceived barriers and lower levels of perceived seriousness and benefits among older women, could contribute to their lower screening rates.
Perceived barriers have been identified in the literature as one of the strong factors influencing older Korean American women’s breast cancer screening behaviors (Han et al., 2000; Juon et al., 2004; Kim et al., 2004), and in this study, perceived barriers was also the strongest predictor for the outcome variable of having had a mammogram. Perceived barriers were conceptualized in this study as “I am afraid to have a mammogram because I don’t understand what will be done,” “I have other problems more important than getting a mammogram,” and “I am too old to need a routine mammogram,” for example. This study supported previous findings, such as lack of significance (Costanza, 1992) and lack of knowledge (Juon et al., 2004; McCool, 1994), as significant barriers to having a mammogram. For older women, interventions focusing on alleviating their perception of barriers by emphasizing the importance of having a mammogram and the high incidence rates of breast cancer in older age could be effective in improving their screening behaviors.
Interestingly, older Korean American women reported a significantly higher level of seriousness than their younger counterparts, and older women who had higher level of seriousness were almost five times more likely to have had a mammogram than women who had a lower level of seriousness. Older women who believed “If I had breast cancer, my whole life would change” and “If I developed breast cancer, I would not live longer than 5 years” were more likely to have had a mammogram. Therefore, emphasizing the seriousness of breast cancer could be effective in increasing mammography utilization in older Korean American women.
Older women who had a higher level of perceived benefit from mammograms were almost five times more likely to have had a mammogram. In previous studies, lack of belief in the benefits of mammography affected the low rate of cancer screening in general and in Korean women in the United States (Juon et al., 2004; McCool, 1994; Thomas, Fox, Leake, & Roetzheim, 1996). Health beliefs such as “Having a mammogram is the best way for me to find breast cancer” and “Having a mammogram will decrease my chance of dying from breast cancer” were significantly lower in older women. Therefore, interventions for older Korean American women should emphasize the benefit of mammograms (i.e., finding breast cancer early, living longer).
We did not find significant relationships between perceived susceptibility and ever having had a mammogram in older women. In previous studies (Holm, Frank, & Curtin, 1999; Maxwell et al., 1998; Thomas et al., 1996), perceived susceptibility was also not associated with mammography screening. In a study with Korean American women, 38% believed they were at low risk for breast cancer (Juon et al., 2004).
Among younger Korean American women, the perceived barriers (OR = 0.15) and having routine checkups in the preceding 2 years (OR = 4.68) were the predictors. The result of perceived barriers being a significant factor in predicting mammography was the same as in older Korean American women. However, when correlations of each item on the barrier subscale and the outcome variables were examined, time and lack of understanding of the significance of mammography were the most potent barriers for younger Korean American women in this study: “Having a mammogram takes too much time,” “I don’t think it is necessary for me to receive a mammogram,” and “I don’t have any symptoms, so [I] don’t need to get a mammogram.” Therefore, although the perceived barriers were a significant predictor for both older and younger Korean American women, different emphases are required for younger Korean American women—the importance of receiving breast cancer screening even when one does not have symptoms.
Receiving routine checkups in the preceding 2 years was also a predictor in younger women. Routine checkups were a significant factor in increased mammograms for Korean American women in previous studies (Juon et al., 2002; Maxwell et al., 2000; Wismer et al., 1998). In younger Korean American women, lack of preventive orientation, such as perceived barriers of not having symptoms and not having routine checkups in the preceding 2 years, seems to be more prominently related to their screening behaviors compared with perceived seriousness, benefits, and barriers, which are more prominently related to older Korean American women’s screening behaviors.
As might be expected, older Korean American women differed from their younger counterparts on most of the sociodemographic and health-related variables: Older Korean American women were more likely to be unmarried and were less educated, less employed, had less English-speaking ability, and spent less of their lives in the United States. They reported significantly lower income and poorer health status than younger Korean American women. Older women were more likely to have health insurance and a regular place to go for health care. However, none of these variables predicted older Korean American women’s having had a mammogram. Rather, health beliefs of perceived barriers, seriousness, and benefits predicted their screening behaviors. We speculate that most of the older Korean American women in this study were similar in their sociodemographic and health-related characteristics, which could have contributed to the insignificant difference of those characteristics on the outcome variable of having had a mammogram. However, older Korean American women’s health beliefs appear to have greater influence on their breast cancer screening behaviors than their disadvantaged socioeconomic status.
LIMITATIONS
While the results of this study provide a specific picture of breast cancer screening behaviors between older and younger Korean American women, there are several limitations in the study design and sampling. First, the findings of this study may not be generalizable to Korean immigrants living in rural areas of the United States, where resources for health care may be different from those in urban areas. Second, this study was a telephone survey based on last names in online directories, so Korean women who do not have Korean surnames, are married to non-Koreans, or have changed their last names could have different responses to the survey. Koreans who do not have a telephone or have only cell phones were not included in this study, which could also have biased the study results. Third, measurement error in self-reported information about cancer screening might have occurred. Self-reported cancer screening rates tend to over-estimate cancer screening prevalence (Gordon, Hiatt, & Lampert, 1993; McPhee et al., 2002; Suarez, Goldman, & Weiss, 1995). Despite these limitations, information from this study could be used to develop tailored intervention strategies for Korean American women’s breast cancer screening behaviors on the basis of age group.
CONCLUSION
Breast cancer has become a significant public health problem. A variety of research studies and community education programs have been developed to encourage breast cancer screening, particularly for women at great risk, such as older or minority women (Hurdle, 2007). The results of this study provide detailed information about health beliefs related to breast cancer screening in older and younger Korean American women. Nurses should take a proactive role in identifying reasons related to age and culture that prevent Korean American women from following screening recommendations. Interventions for older Korean American women should focus more on changing their health beliefs about the seriousness, benefits, and barriers to mammography, whereas for younger women, more attention should be given to overcoming perceived barriers and encouraging routine checkups even when they do not have symptoms. Information from this study could be used to develop tailored interventions for Korean American women’s breast cancer screening according to age group. Findings of this study suggest that differences (by age) in a specific ethnic/cultural group of women exist, and more detailed interventions should be developed targeting subgroups of women to effectively decrease health disparities in minority women.
KEYPOINTS.
Breast Cancer Screening Beliefs
Eun, Y., Lee, E.E., Kim, M.J., & Fogg, L. (2009). Breast Cancer Screening Beliefs among Older Korean American Women. Journal of Gerontological Nursing, 35(9), 40-50.
Breast cancer screening behaviors among older Korean American women are influenced more by their health beliefs, especially perceived seriousness of the disease, barriers, and benefits of having a mammogram, than their younger counterparts.
For breast cancer screening interventions to be effective for Korean American women, considerations should be given to their health beliefs, which are influenced by their culture and age.
Nurses need to take a proactive role in identifying reasons related to culture and age that prevent Korean American women from following mammography screening recommendations.
Acknowledgments
This study was supported by a National Institute of Nursing Research Mentored Research Scientist Development Award (K01 NR 08096).
Footnotes
The authors disclose that they have no significant financial interests in any product or class of products discussed directly or indirectly in this activity.
REFERENCES
- American Cancer Society Breast cancer facts & figures 2007-2008. 2007 Retrieved June 24, 2009, from http://www.cancer.org/downloads/STT/BCFF-Final.pdf.
- Caplan LS, Haynes SG. Breast cancer screening in older women. Public Health Reviews. 1996;24:193–204. [PubMed] [Google Scholar]
- Champion VL. Instrument refinement for breast cancer screening behaviors. Nursing Research. 1993;42:139–143. [PubMed] [Google Scholar]
- Champion VL. Revised susceptibility, benefits, and barriers scale for mammography screening. Research in Nursing & Health. 1999;22:341–348. doi: 10.1002/(sici)1098-240x(199908)22:4<341::aid-nur8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Costanza ME. Breast cancer screening in older women. Synopsis of a forum. Cancer. 1992;69(7 Suppl.):1925–1931. doi: 10.1002/1097-0142(19920401)69:7+<1925::aid-cncr2820691709>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Edwards NI, Jones DA. Uptake of breast cancer screening in older women. Age and Ageing. 2000;29:131–135. doi: 10.1093/ageing/29.2.131. [DOI] [PubMed] [Google Scholar]
- Gordon NP, Hiatt RA, Lampert DI. Concordance of self-reported data and medical record audit for six cancer screening procedures. Journal of National Cancer Institute. 1993;85:566–570. doi: 10.1093/jnci/85.7.566. [DOI] [PubMed] [Google Scholar]
- Han Y, Williams RD, Harrison RA. Breast cancer screening knowledge, attitudes, and practices among Korean American women. Oncology Nursing Forum. 2000;27:1585–1591. [PubMed] [Google Scholar]
- Holm CJ, Frank DI, Curtin J. Health beliefs, health locus of control, and women’s mammography behavior. Cancer Nursing. 1999;22:149–156. doi: 10.1097/00002820-199904000-00007. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. Wiley and Sons; New York: 1989. [Google Scholar]
- Hurdle DE. Breast cancer prevention with older women: A gender-focused intervention study. Health Care for Women International. 2007;28:872–887. doi: 10.1080/07399330701615291. [DOI] [PubMed] [Google Scholar]
- Im EO, Park YS, Lee EO, Yun SN. Korean women’s attitudes toward breast cancer screening tests. International Journal of Nursing Studies. 2004;41:583–589. doi: 10.1016/j.ijnurstu.2004.01.004. [DOI] [PubMed] [Google Scholar]
- Janz NK, Champion VL, Strecher VJ. The health belief model. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education: Theory, research, and practice. 3rd ed. Jossey-Bass; San Francisco: 2002. pp. 45–66. [Google Scholar]
- Juon HS, Choi Y, Kim MT. Cancer screening behaviors among Korean-American women. Cancer Detection and Prevention. 2000;24:589–601. [PubMed] [Google Scholar]
- Juon HS, Kim M, Shankar S, Han W. Predictors of adherence to screening mammography among Korean American women. Preventive Medicine. 2004;39:474–481. doi: 10.1016/j.ypmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Juon HS, Seo YJ, Kim MT. Breast and cervical screening among Korean American elderly women. European Journal of Oncology Nursing. 2002;6:228–235. doi: 10.1054/ejon.2002.0213. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast and cervical carcinoma screening rates and Healthy People 2000 objectives. Cancer. 2000;89:695–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Kim SH, Jeong IS, Kim JS. Breast cancer screening and repeat screening. Journal of Korean Academy of Nursing. 2004;34:791–800. doi: 10.4040/jkan.2004.34.5.791. [DOI] [PubMed] [Google Scholar]
- Kim YH, Sarna L. An intervention to increase mammography use by Korean American women. Oncology Nursing Forum. 2004;31:105–110. doi: 10.1188/04.ONF.105-110. [DOI] [PubMed] [Google Scholar]
- Lee EE, Fogg LF, Sadler GR. Factors of breast cancer screening among Korean immigrants in the United States. Journal of Immigrant and Minority Health. 2006;8:223–233. doi: 10.1007/s10903-006-9326-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee EE, Tripp-Reimer T, Miller AM, Sadler GR, Lee SY. Korean American women’s beliefs about breast and cervical cancer and associated symbolic meanings. Oncology Nursing Forum. 2007;34:713–720. doi: 10.1188/07.ONF.713-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Mammography utilization and related attitudes among Korean-American women. Women and Health. 1998;27:89–107. doi: 10.1300/J013v27n03_07. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. American Journal of Preventive Medicine. 2000;18:62–68. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- Mayer JA, Slymen DJ, Drew JA, Wright BL, Elder JP, Williams SJ. Breast and cervical cancer screening in older women: The San Diego Medicare Preventive Health Project. Preventive Medicine. 1992;21:395–404. doi: 10.1016/0091-7435(92)90049-n. [DOI] [PubMed] [Google Scholar]
- McCool WF. Barriers to breast cancer screening in older women. A review. Journal of Nurse-Midwifery. 1994;39:283–299. doi: 10.1016/0091-2182(94)90129-5. [DOI] [PubMed] [Google Scholar]
- McPhee SJ, Nguyen TT, Shema SJ, Nguyen B, Somkin C, Vo P, et al. Validation of recall of breast and cervical cancer screening women in an ethnically diverse population. Preventive Medicine. 2002;35:463–473. doi: 10.1006/pmed.2002.1096. [DOI] [PubMed] [Google Scholar]
- Morisky DE, Fox SA, Murata PJ, Stein JA. The role of needs assessment in designing a community-based mammography education program for urban women. Health Education Research. 1989;4:469–478. [Google Scholar]
- National Institutes of Health NIH senior health: Breast cancer: Causes and risk factors. 2008 Retrieved June 24, 2009, from http://nihseniorhealth.gov/breastcancer/causesandriskfactors/03.html.
- Noh DY, Kim JS, Yoon YK, Oh SK, Choe KJ. Clinical manifestations of breast cancer and current trends of treatment. Journal of Korean Academy of Surgery. 1998;54:464–473. [Google Scholar]
- Ryu KW, Kyu JW, Kim JS, Koo BH. Symptoms of breast disease in Korea. The Korea Surgical Society. 1994;46(1):44–55. [Google Scholar]
- Sarna L, Tae YS, Kim YH, Brecht ML, Maxwell AE. Cancer screening among Korean Americans. Cancer Practice. 2001;9(3):134–140. doi: 10.1046/j.1523-5394.2001.009003134.x. [DOI] [PubMed] [Google Scholar]
- Shootman M, Jeffe DB, Lian M, Aft R, Gillanders WE. Surveillance mammography and the risk of death among elderly breast cancer patients. Breast Cancer Research and Treatment. 2008;111 doi: 10.1007/s10549-007-9795-1. Retrieved May 19, 2008, from http://www.springerlink.com/content/u2x90w3087474q81/fulltext.pdf. [DOI] [PubMed] [Google Scholar]
- Stewart JA, Foster RS., Jr. Breast cancer and aging. Seminars in Oncology. 1989;16:41–50. [PubMed] [Google Scholar]
- Suarez L, Goldman DA, Weiss NS. Validity of Pap smear and mammogram self-reports in a low-income Hispanic population. American Journal of Preventive Medicine. 1995;11:94–98. [PubMed] [Google Scholar]
- Thomas LR, Fox SA, Leake BG, Roetzheim RG. The effects of health beliefs on screening mammography utilization among a diverse sample of older women. Women & Health. 1996;24:77–94. doi: 10.1300/j013v24n03_05. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau Census 2000 demographic profile highlights: Illinois. Selected population group: Korean alone. 2000 Retrieved January 3, 2009, http://factfinder.census.gov/servlet/SAFFIteratedFacts?_event=&geo_id=04000US17&_geoContext=01000US%7C04000US17&_street=&_county=&_cityTown=&_state=04000US17&_zip=&_lang=en&_sse=on&ActiveGeoDiv=&_useEV=&pctxt=fph&pgsl=040&_submenuId=factsheet_2&ds_name=DEC_2000_SAFF&_ci_nbr=023&qr_name=DEC_2000_SAFF_R1040®=DEC_2000_SAFF_R1040%3A023&_keyword=&_industry=
- U.S. Department of Health and Human Services . Healthy people 2010. 2nd ed. Vol. 1. 2000. Cancer: Healthy people 2010 objectives; pp. 3-26–3-27. Retrieved December 22, 2008, from http://www.healthypeople.gov/Document/pdf/Volume1/03Cancer.pdf. [Google Scholar]
- U.S. Preventive Services Task Force Screening for breast cancer. 2002 Retrieved June 24, 2009, from http://www.ahrq.gov/clinic/USpstf/uspsbrca.htm.
- Weinberger M, Saunders AF, Samsa GP, Bearon LB, Gold DT, Brown JT, et al. Breast cancer screening in older women: Practices and barriers reported by primary care physicians. Journal of the American Geriatrics Society. 1991;39:22–29. doi: 10.1111/j.1532-5415.1991.tb05901.x. [DOI] [PubMed] [Google Scholar]
- Wismer BA, Moskowitz JM, Chen AM, Kang SH, Novotny TE, Min K, et al. Mammography and clinical breast examination among Korean American women in two California counties. Preventive Medicine. 1998;27:144–151. doi: 10.1006/pmed.1997.0259. [DOI] [PubMed] [Google Scholar]
- Wu TY, Guthrie BJ, Bancroft JM. An integrative review of breast cancer screening practice and correlates among Chinese, Korean, Filipino, and Asian Indian American women. Health Care for Women International. 2005;26:225–246. doi: 10.1080/07399330590917780. [DOI] [PubMed] [Google Scholar]


