Abstract
OBJECTIVES:
Volunteering is associated with lower mortality in the elderly. Driving is associated with health and well-being and driving cessation has been associated with decreased out-of-home activity levels including volunteering. We evaluated how accounting for driving status altered the relationship between volunteering and mortality in US retirees.
DESIGN:
Observational prospective cohort
SETTING and PARTICIPANTS:
Nationally representative sample of retirees over age 65 from the Health and Retirement Study in 2000 and 2002, followed to 2006 (n=6408).
MEASUREMENTS:
Participants self-reported their volunteering, driving status, age, gender and race/ethnicity, presence of chronic conditions, geriatrics syndromes, socioeconomic factors, functional limitations and psychosocial factors. Death by December 31, 2006 was the outcome.
RESULTS:
For drivers, the mortality rates between volunteers (9%) and non-volunteers (12%) were similar; for limited or non-drivers, the mortality rate for volunteers (15%) was markedly lower compared to non-volunteers (32%). Our adjusted results showed that for drivers, the volunteering-mortality Odds Ratio (OR) was 0.90 (95%CI: 0.66–1.22), whereas for limited or non-drivers, the OR was 0.62 (95%CI: 0.49–0.78), (interaction p=0.05). The impact of driving status was greater for rural participants, with greater differences between rural drivers versus rural limited or non-drivers (interaction p=0.02) compared to urban drivers versus urban limited or non-drivers (interaction p=0.81).
CONCLUSION:
The influence of volunteering in decreasing mortality seems to be stronger among rural retirees who are limited or non-drivers. This may be because rural or non-driving retirees are more likely to be socially isolated and thus receive more benefit from the increased social integration from volunteering.
Keywords: mortality, volunteerism, driving
INTRODUCTION
Among older Americans, volunteering is common and strongly associated with good health outcomes including better function and lower mortality. [1-9] Volunteering may be particularly appealing to older adults, with 24% of Americans over 65 reporting some volunteer work in 2009. [10] Thus, volunteering may be a widely acceptable way to engage retirees to be more physically, mentally and socially active. [1, 11] Because volunteering appears to benefit both older adults who volunteer and the charitable organizations that receive the volunteers’ efforts, there has been increasing research [1, 8, 12] and government support for volunteering with 2 recently enacted federal laws. In 2006, the Older American’s Act was reauthorized, charging the Department of Health and Human Services’ Administration on Aging to support and enhance older Americans’ volunteer opportunities. [13] In April 2009, the Serve America Act was signed into law, expanding volunteer opportunities for Americans age 55 or older. [14] A fuller understanding of the association between volunteering and mortality could guide the design of future volunteer opportunities and help insure access to those most likely to benefit. [15]
Driving status may be an important factor to consider when examining the volunteering-mortality relationship for two reasons. First, driving remains the primary mode of transportation for older adults [16] and the cessation of driving leads to decreased out-of-home activity, including decreased volunteering. [17] Since driving status is also strongly associated with mortality, [18] accounting for driving status may help explain the volunteering-mortality relationship. [19] Second, driving cessation leads to decreased social integration and social ties. [20] Since one proposed mechanism for the health benefits of volunteering is through increased social integration, [4, 5, 7, 8] driving status may also alter the volunteering-mortality relationship through its effect on social integration. Despite these relationships, previous studies on the relationship between volunteering and mortality have not accounted for driving status.
Thus, our objective was to examine the effect of driving status on the relationship between volunteering and mortality in a national, population-based sample of US retirees over 65. We accounted for a wide range of factors which may confound this relationship, including demographic variables, chronic conditions, health behaviors, function, geriatric syndromes, socioeconomic status and psychosocial factors. Finally, the importance of driving may vary between elders in rural and urban settings due to differences in the availability of alternate means of transportation.[21, 22] Thus, we evaluated whether relationships between volunteering, driving, and mortality differed among elders in rural versus urban settings.
METHODS
Participants
We studied community-dwelling participants interviewed in the 2000 and 2002 waves of the Health and Retirement Study (HRS), a nationally representative sample of all persons in the contiguous US. Data were collected primarily through telephone interviews, with an overall response rate of 81%. [23]
A total of 8017 participants over age 65 were interviewed in 2000 and 2002 for the HRS. We excluded participants who reported not being completely retired (1600), or if critical data needed for the analysis were missing such as 2002 volunteer activity (4) or 2006 vital status (5). Our final analytic sample consisted of 6408 retirees with 1423 individuals (22%) dying by 2006.
Analytic Strategy
Factors such as depression and physical function may both confound and modify the relationship between volunteering and mortality. For example, elders who are depressed may be less likely to volunteer and more likely to die, suggesting that depression confounds the volunteering-mortality relationship and thus should be adjusted for. However, volunteering may lead to lower mortality in part by improving depression; [24, 25] if this is the case, adjusting for depression would lead to over-adjustment (inappropriately minimizing the role of volunteering by adjusting for factors on the causal pathway).
To adjust for possible confounding factors while decreasing the chances of over-adjustment, we utilized the longitudinal design of the HRS and used 2002 primary predictor data (volunteering, driving status and urban/rural designation) but used 2000 data for possible confounding factors. By adjusting for factors that precede the primary predictors, we decreased the chances of adjusting for factors on the causal pathway since a 2000 factor cannot directly mediate a relationship between a 2002 predictor and 2006 outcome. Although some predictors were similar between 2000 and 2002, this analytic strategy has been used successfully in previous volunteering studies [5, 26, 27] and is more likely to yield unbiased results than using predictor and confounding factor data from a single year.
Measures: Outcome
The primary outcome was death by December 31, 2006. We assessed mortality using the HRS follow-up procedures, which entailed cross-referencing HRS information with the National Death Index. [23]
Measures: Primary Predictors
Volunteer activity and driving status were ascertained by self-report in 2002. To determine volunteer activity, subjects were asked, “Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations?” To determine driving status, subjects were asked, “Are you able to drive?” and “Do you limit your driving to nearby places, or do you also drive on longer trips?” Because non-drivers and drivers who limited their driving had very similar results, our primary analysis combines limited and non-drivers into a single group. We used retirees’ county of residence in 2002 and the Beale rural-urban continuum codes to determine whether each retiree lived in an urban (county within metropolitan area with greater than 1 million population) or rural setting (all other counties). [28]
Measures: Possible Confounding Factors
Factors that may confound the relationship between volunteering and mortality were ascertained by self-report in 2000. For demographics, participants were asked about their age, gender, race and ethnicity and marital status. For chronic conditions, participants were asked, “Have you ever had, or has a doctor told you, that you have/had X?” with follow-up questions to gauge the severity of disease. We examined a total of 7 conditions with up to 3 levels of severity: hypertension, diabetes mellitus, cancer, chronic lung disease, heart disease, congestive heart failure and stroke. For smoking, participants were asked, “Have you ever smoked cigarettes?” and “Do you smoke cigarettes now?” Participants were asked about their weight and height, which allowed us to calculate body mass index (BMI).
For geriatric syndromes, participants or their proxy were asked about memory, falls, incontinence, pain, eyesight and hearing in 2000 with follow up questions to gauge the severity of the geriatric syndrome. For functional limitations, participants were asked “Because of a health or memory problem, do you have any difficulty with X?” in 2000. Difficulties in 5 activities of daily living (ADL: bathing, dressing, eating, transferring and toileting); 5 instrumental activities of daily living (IADL: shopping, preparing meals, using the telephone, managing medications and managing finances) and walking were determined.
For socioeconomic status (SES) in 2000, participants were asked about the highest educational degree that they obtained, their annual income and net wealth. [29] Because of the positively skewed nature of these variables, we categorized wealth and income into quintiles for analysis. For psychosocial factors in 2000, we assessed depressive symptoms using a modified 8-item Center for Epidemiologic Studies-Depression (CES-D) Scale. [30, 31] Participants were asked “Did you feel depressed much of time during the past week?” Similar questions explored other depressive symptoms including restless sleep, feelings of loneliness and sadness, decreased energy and enjoying life. We also asked participants, “Would you say your health is Excellent, Very Good, Good, Fair or Poor?”
In our bivariate analysis of these potential confounding factors, we found that falls, incontinence, pain, visual impairment, ADLs and income were not associated with mortality at the p<0.2 level. These factors were not included in the final model. Missing data for confounders were rare, with all variables more than 98.7% complete.
Statistical Analysis
Using multivariate logistic regression, we determined the relationship between volunteering and 4-year mortality. We conducted analyses stratified by driving status to obtain point estimates of the relationship between volunteering and mortality in drivers versus volunteering and mortality in limited or non-drivers. To determine an unadjusted measure of association between volunteering and 4-year mortality, our initial multivariate models only accounted for demographic factors. Our fully adjusted models also accounted for chronic condition and health behaviors, geriatric syndromes, function, socioeconomic status (SES) and psychosocial factors that were associated with our mortality outcome at the p<0.2 level in our bivariate analysis. To test the statistical significance of differences between these estimates, we ran a single model using driving and the driving-volunteering interaction term as covariates. Because we hypothesized that the ability to drive may have a stronger effect in rural settings with fewer alternate transportation options, we also performed analyses stratified by urban/rural status.
Because of our concerns about residual confounding, we augmented our primary analyses with a propensity score analysis. [32, 33] We determined the propensity of each subject of being a volunteer through logistic regression using the covariates from our primary analysis. We divided subjects into quintiles of propensity [34, 35] and found that in the lowest propensity quintile, there were very few volunteers (n=57) compared to non-volunteers (n=1225). We omitted the lowest propensity quintile from further analysis [32, 33] and compared volunteers to non-volunteers (stratified by driving status) adjusting for propensity of volunteering along with our other covariates. As a sensitivity analysis, we performed our propensity score analysis including the lowest propensity quintile and found that our results were similar to our lowest quintile excluded propensity analysis. Thus, we present our propensity score analysis with the lowest quintile of propensity score subjects excluded.
All statistics were performed using Stata MP software (version 10.0; Stata Corporation, College Station, TX). The Committee on Human Research of the University of California, San Francisco and the San Francisco Veterans Affairs Research and Development committee approved this study.
RESULTS
Characteristics of the Participants
Volunteers had a more favorable risk factor profile than non-volunteers across virtually every measure examined. (Table 1) For example, compared to non-volunteers, volunteers were less likely to smoke, to have diabetes mellitus and to have poor memory. Volunteers were more likely to have earned a college degree and have higher wealth. Volunteers also were more likely to report excellent or very good overall health and no depressive symptoms. Volunteers were less likely to report being a limited or non-driver at 44% compared to 71% of non-volunteers who reported being a limited or non-driver.
Table 1. Selected Characteristics of Participants.
| Limited or Non-Drivers (n=4073) |
Drivers (n=2335) |
|||
|---|---|---|---|---|
| Characteristics | Volunteers (n=779) |
Non- Volunteers (n=3294) |
Volunteers (n=992) |
Non- Volunteers (n=1343) |
| Demographics | ||||
| Age, mean (± SD) | 78 (6) | 79 (7) | 75 (5) | 75 (5) |
| Women, % | 79 | 69 | 49 | 37 |
| Married/Coupled, % | 47 | 42 | 74 | 73 |
| Race/Ethnicity, % | ||||
| White, non-hispanic | 80 | 71 | 92 | 90 |
| Black, non-hispanic | 14 | 16 | 6 | 5 |
| Other, non-hispanic | 2 | 2 | 1 | 1 |
| Hispanic | 5 | 11 | 1 | 4 |
| Health Behaviors, % | ||||
| Currently Smoking | 7 | 11 | 4 | 10 |
| Highest Quintile BMI (>29.7) |
19 | 20 | 17 | 19 |
| Chronic Conditions, % | ||||
| Diabetes Mellitus | 14 | 19 | 12 | 15 |
| Cancer | 14 | 14 | 16 | 15 |
| Heart Disease | 27 | 33 | 25 | 27 |
| Previous Stroke | 8 | 14 | 5 | 6 |
| Geriatric Syndromes | ||||
| Falls | 28 | 32 | 23 | 19 |
| Incontinence | 24 | 24 | 19 | 16 |
| Pain | 27 | 36 | 21 | 22 |
| Visual Impairment | 7 | 12 | 1 | 3 |
| Hearing Impairment | 5 | 8 | 3 | 6 |
| Poor memory (<3/10 words, immediate recall) |
9 | 23 | 6 | 13 |
| Function, % | ||||
| No difficulty in ADLs | 84 | 72 | 93 | 93 |
| No difficulty in Instrumental ADLs |
89 | 74 | 97 | 95 |
| No difficulty walking several blocks |
64 | 50 | 82 | 78 |
| Socioeconomic Status, % | ||||
| College Degree or Higher | 19 | 10 | 33 | 22 |
| $450+ in Wealth (× $1000) |
18 | 11 | 38 | 29 |
| Psychosocial Factors | ||||
| Religion Very Important | 81 | 66 | 76 | 51 |
| Self-Rated Health Very Good or Excellent |
40 | 24 | 57 | 49 |
| No depression symptoms (CES-D = 0) |
35 | 24 | 54 | 41 |
| Lives in Urban setting, % | 45 | 44 | 39 | 42 |
SD is standard deviation
BMI is Body Mass Index
CES-D is Center for Epidemiologic Studies-Depression
ADL is activity of daily living
Percentages may not sum to 100% due to rounding
Compared to limited or non-drivers, drivers were more likely to be male, married and white. Drivers were less likely to report pain or visual impairment and more likely to report no functional difficulties. Drivers were also more likely to have earned a college degree, more likely to report no depressive symptoms and live in a rural setting.
Demographic Factor Adjusted Volunteering-Mortality Relationship, Stratified by Driving Status
When we examined the volunteering-mortality relationship stratified by driving status, among limited or non-drivers, volunteers had a markedly lower mortality rate of 15% compared to 32% for non-volunteers (p<0.001). (Figure 1) However, among drivers who reported no limitations, volunteers had only a slightly lower mortality rate of 9% compared to 12% for non-volunteers (p=0.01).
Figure 1.
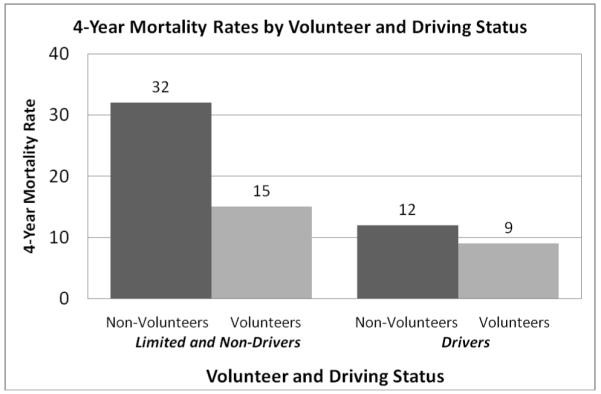
4-Year Mortality Rates by Volunteer and Driving Status
Multivariable Adjusted Volunteering-Mortality Relationship, Stratified by Driving Status
Next, we examined the effect of accounting for other factors on the volunteering-mortality relationship and how this association may differ between older adults who drive versus those who limit their driving or do not drive altogether. We first just adjusted for demographic factors (age, gender, race and ethnicity, marital status), we found that in all subjects, volunteering was strongly associated with lower mortality, with an OR of 0.45 (95% CI: 0.38 – 0.53). (Table 2) However, when we stratified by driving status, we found that the volunteering-mortality relationship differed dramatically between drivers and limited or non-drivers. In limited or non-drivers, volunteering remained strongly protective, with an OR of 0.44 (95% CI: 0.36 – 0.55) but in drivers, volunteering was not significantly protective, with an OR of 0.81 (95% CI: 0.61 – 1.08). The p-value to assess the relationship between driving and volunteering was determined through an interaction term (driving x volunteering) and was highly significant at 0.002.
Table 2.
Odds Ratio of 4-Year Mortality for Volunteers, Stratified by Driving Status
| Adjusted for | All Subjects, OR (95% CI) |
Drivers, OR (95% CI) |
Limited or Non- Drivers, OR (95% CI) |
P Value for interaction by driving status |
|---|---|---|---|---|
| Demographic variables |
0.45 (0.38 – 0.53) |
0.81 (0.61- 1.08) |
0.44 (0.36 – 0.55) |
0.002 |
| Fully adjusted | 0.65 (0.54 – 0.78) |
0.90 (0.66 – 1.22) |
0.62 (0.49 – 0.78) |
0.05 |
| Fully adjusted with Propensity adjustment |
0.69 (0.57 – 0.83) |
0.89 (0.64 – 1.23) |
0.68 (0.53 – 0.86) |
0.16 |
Demographic variables include age, gender, race/ethnicity and marital status
Fully adjusted model accounted for demographic variables as well as chronic conditions, health behaviors, geriatric syndromes, function, socioeconomic status and psychosocial factors.
OR is odds ratio
CI is confidence interval
When we accounted for other factors beyond demographic variables, the differences between drivers versus limited or non-drivers persisted. (Table 2) Thus, we found that among drivers, volunteering was not protective when accounting for all other factors with an OR for mortality of 0.90 (95% CI: 0.66 – 1.22). In contrast, among limited or non-drivers, volunteering remained strongly protective even after accounting for all other factors with an OR for mortality of 0.62 (95% CI: 0.49 – 0.78). For the fully adjusted model, the p-value for interaction approached significance at 0.05. Propensity adjustment did not alter our results substantially, with volunteering continuing to be more protective in limited or non-drivers (OR 0.68, 95% CI: 0.53 – 0.86) than drivers (OR 0.89, 95% CI: 0.64 – 1.23).
We then examined whether the differences in the volunteering-mortality relationship between drivers versus limited or non-drivers were affected when stratified further by urban/rural status. (Table 3) We found that driving was more important to consider for rural subjects than urban subjects with greater differences between drivers and limited or non-drivers. In urban subjects, after full multivariable adjustment, there was no significant difference in the association between volunteering and mortality for drivers versus limited or non-drivers (p-value for interaction 0.81), suggesting that in urban subjects, the volunteering-mortality relationship was similar in drivers and limited or non-drivers. In contrast, in rural subjects, there were significant differences in the association between volunteering and mortality between drivers versus limited or non-drivers (p-value for interaction 0.02), suggesting that in rural subjects, volunteering was more protective in limited or non-drivers.
Table 3.
Fully Adjusted Odds Ratios for the Association Between Volunteering and Mortality Stratified By Driving and Urban/Rural Status
| Urban/Rural Status |
All Retirees, OR (95% CI) |
Drivers, OR (95% CI) |
Limited or Non- Drivers, OR (95% CI) |
P value |
|---|---|---|---|---|
| All | 0.65 (0.54 – 0.78) |
0.9 (0.66 – 1.22) |
0.62 (0.49 – 0.78) |
0.05 |
| Urban | 0.67 (0.51 – 0.88) |
0.84 (0.51 – 1.38) |
0.7 (0.50 – 0.99) |
0.81 |
| Rural | 0.73 (0.59 – 0.90) |
0.95 (0.61 – 1.48) |
0.54 (0.39 – 0.74) |
0.02 |
All Odds Ratios are adjusted for demographics, chronic conditions, behaviors, geriatric syndromes, function, socioeconomic status and psychosocial factors.
P values test whether the 2 categories of drivers are significantly different from each other
DISCUSSION
In a population-based sample of US retirees over age 65, we found that volunteering was strongly associated with lower mortality in limited or non-drivers, with an adjusted OR for mortality of 0.62 (95% CI: 0.49 – 0.78). In contrast, volunteering was not associated with lower mortality in drivers, with an adjusted OR for mortality of 0.90 (95% CI: 0.66 – 1.22). These findings suggest that the decreased mortality seen in volunteers are concentrated in US retirees who limit their driving or are unable to drive altogether. When we examined these relationships in urban and rural settings, we found that the differences in the volunteering-mortality relationship between drivers versus limited or non-drivers were more pronounced in rural retirees (p-value for interaction of 0.02) than in urban retirees (p-value for interaction of 0.81). Our results suggest that any future expansion of national and community service should include older adults who have limited access to volunteer opportunities due to their inability to drive.
One possible explanation for our findings is that limited or non-drivers are more likely to be socially isolated, with volunteer activity in these retirees leading to relatively large improvements in social integration, ultimately resulting in decreased mortality. Conversely, for drivers, because they are able to drive to maintain social relationships with family and friends, their level of social integration even without volunteering may be sufficient, leading to minimal decreases in mortality from the additional social integration from volunteering. Previous studies on the effects of social integration on health outcomes have suggested a threshold effect, where additional integration below a threshold was beneficial but further social integration beyond that threshold did not lead to further improved outcomes. [4, 7, 8, 36] Even without volunteering, retirees who are able to drive may be above this threshold of social integration, so that the additional social integration from volunteering does not lead to substantial decreases in mortality.
Our urban/rural results provide further evidence for social integration as an important factor in the volunteering-mortality relationship. Driving is often required for an active social life, especially in rural areas where there are fewer alternative transportation options. [21, 37] Thus, we hypothesized that driving would be more important to consider in rural areas compared to urban areas. Our results showing that the differences between limited or non-drivers versus drivers were greater in rural subjects compared to urban subjects confirmed our hypothesis and suggest that social integration is an important factor in the volunteering-mortality relationship. This is of particular policy importance give that rural areas generally have a higher proportion of older residents than urban areas. [38]
Given the many differences in risk factors between volunteers and non-volunteers, it is likely that some of the observed association between volunteering and mortality is due to residual confounding. However, we accounted for a wide range of possible confounding factors, including subjective factors such as overall self-rated health which have been previously shown to be strongly associated with our primary predictors and outcomes, [39-41] making it less likely that our results are entirely due to residual confounding. Second, if volunteering and driving status are simply measures of the same underlying factor such as overall health, it is unlikely that the volunteering-mortality relationship would differ by driving status since both volunteering and driving status would identify the same subjects with marginal overall health.
Our results have several practical implications. First, organizations with older volunteers should ensure that volunteer opportunities are available to all older Americans, regardless of their ability to drive. For example, volunteer organizations could partner with elder mobility services or provide ride sharing opportunities to make it easier for non-driving retirees to volunteer, ensuring that volunteering opportunities are available to those retirees most likely to benefit from volunteering. Supporting volunteer activity among non-driving retirees who may be at highest risk for social isolation will minimize the chances that an expansion of volunteering opportunities will exacerbate existing disparities. [42] Second, our results support continued investment in mass transportation, as well as the zoning and development of mixed use neighborhoods that would allow elders to remain socially integrated without driving. [43] Naturally Occurring Retirement Communities [44, 45] and Beacon Hill Village [46] are specific models of senior living where the physical environment and services are tailored to allow non-driving elders to maintain an active social life that includes volunteering. Third, our results suggest that rural retirees may be especially vulnerable to isolation and adverse outcomes if they are unable to drive. Rural communities should consider increasing access to volunteering opportunities as they address the broader zoning and transportation challenges posed by an increasing number of older people with limited ability to drive themselves.
Our study has several limitations. First, like almost all studies on volunteering, most of our information was obtained through self-report. For some factors such as pain, depressive symptoms and overall self-rated health, self-report is the gold standard. For other factors such as chronic conditions and function, previous studies have suggested that self-report is a valid and reliable way to measure these risk factors. [47, 48] Second, we were unable to directly measure social integration; thus, we were unable to test whether social isolation is a critical mediating factor between driving status and mortality. However, previous studies have shown strong associations between driving, social integration and mortality. [4, 17-20] Furthermore, driving status may be easier to measure than social integration and mobility services provide a possible remedy to driving cessation, facilitating the translation of research findings such as ours into policy recommendations. Third, our decision to use 2000 and 2002 data required us to only include retirees who were alive and participating in the HRS study in both years, enriching our cohort with survivors. Because the use of 2000 and 2002 data allowed us to minimize the chances of over-adjustment, we believe the advantages of our approach outweigh the disadvantages. Fourth, since we were unable to account for access to healthcare and previous studies have suggested that healthcare access may be more problematic in rural areas, [49, 50] our urban/rural results may be due in part to differences in healthcare access between urban and rural retirees. Future studies should explicitly account for healthcare access as a possible mechanism of the volunteering-mortality relationship. Finally, our observational study design precludes conclusions regarding causality. Thus, although our study provides supporting evidence for the beneficial effects of volunteering, questions regarding a causal relationship between volunteering and mortality must await an ongoing randomized trial. [1, 11]
We found that volunteering was associated with lower 4-year mortality in US retirees who are limited or non-drivers and that this association was most pronounced among rural retirees. Our results suggest that the expansion of volunteer opportunities could lead to improved health and quality of life for American retirees, especially if recruitment and retention efforts supported access for rural, non-driving elders. The next federal transportation funding bill and the anticipated reauthorization of the Older Americans’ Act in 2011 provide an important opportunity to increase access to volunteer opportunities, along with other opportunities for social integration, for older Americans who are limited drivers or do not drive.
ACKNOWLEDGMENTS
Conflict of Interest
Dr. Lee was supported by the Hartford Geriatric Health Outcomes Research Scholars Award, Hellman Family Foundation Award for Young Faculty Scholars at UCSF and KL2RR024130 from the National Center for Research Resources, a component of the NIH. Dr. Steinman was supported by a Beeson Career Development Award from the National Institute of Aging and the American Federation for Aging Research (K23 AG030999). Dr. Tan was supported by the NIA Johns Hopkins Older Americans Independence Center (contract P30-AG02133) and the John A. Hartford Foundation.
(This manuscript represents work done while Dr. Tan was at the Division of Geriatric Medicine and Gerontology, Johns Hopkins. The opinions expressed in this article are those of the authors and do not represent the official position of the Corporation for National and Community Service.)
Sponsor’s Role: The funding sources had no role in the design or conduct of the study, data management or analysis, or manuscript preparation
Footnotes
Previous Presentations:
This work was presented at the Society of General Internal Medicine Annual National Meeting in Miami, Florida in May 2009 and the American Geriatrics Society Annual National Meeting in Chicago, Illinois in May 2009.
REFERENCES
- 1.Fried LP, Carlson MC, Freedman M, et al. A social model for health promotion for an aging population: initial evidence on the Experience Corps model. J Urban Health. 2004;81:64–78. doi: 10.1093/jurban/jth094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glass TA, de Leon CM, Marottoli RA, et al. Population based study of social and productive activities as predictors of survival among elderly Americans. BMJ. 1999;319:478–483. doi: 10.1136/bmj.319.7208.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris AHS, Thoresen CE. Volunteering is associated with delayed mortality in older people: Analysis of the Longitudinal Study of Aging. J Health Psychol. 2005;10:739–52. doi: 10.1177/1359105305057310. [DOI] [PubMed] [Google Scholar]
- 4.House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241:540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- 5.Luoh MC, Herzog AR. Individual consequences of volunteer and paid work in old age: health and mortality. J Health Soc Behav. 2002;43:490–509. [PubMed] [Google Scholar]
- 6.Musick MA, Herzog AR, House JS. Volunteering and mortality among older adults: findings from a national sample. J Gerontol B Psychol Sci Soc Sci. 1999;54:S173–180. doi: 10.1093/geronb/54b.3.s173. [DOI] [PubMed] [Google Scholar]
- 7.Oman D, Thoresen CE, McMahon K. Volunteerism and Mortality Among Community-Dwelling Elderly. J Health Psychology. 1999;4:301–316. doi: 10.1177/135910539900400301. [DOI] [PubMed] [Google Scholar]
- 8.Piliavin JA, Siegl E. Health benefits of volunteering in the Wisconsin longitudinal study. J Health Soc Behav. 2007;48:450–464. doi: 10.1177/002214650704800408. [DOI] [PubMed] [Google Scholar]
- 9.Seeman TE. Social ties and health: The benefits of social integration. Ann Epidemiol. 1996;6:442–451. doi: 10.1016/s1047-2797(96)00095-6. [DOI] [PubMed] [Google Scholar]
- 10. [Accessed Jan 26, 2010];Volunteering in the United States--2009. 2010 Available at: http://www.bls.gov/news.release/pdf/volun.pdf.
- 11.Tan EJ, Tanner EK, Seeman TE, et al. Marketing Public health through older adult volunteering: Experience corps as a social marketing intervention. Am J Public Health. 2010;100:727–734. doi: 10.2105/AJPH.2009.169151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang F, Choi E, Morrow-Howell N. Organizational support and volunteering benefits for older adults. Gerontologist. 2010;50:603–612. doi: 10.1093/geront/gnq020. [DOI] [PubMed] [Google Scholar]
- 13. [Accessed Mar 5, 2010];Civic Engagement Initiative. 2009 12/4/09. Available at: http://www.aoa.gov/aoaroot/aoa_programs/special_projects/civic_engagement/index.aspx.
- 14.Edward M. [Accessed Jan 26, 2010];Kennedy Serve America Act of 2009. 2010 Available at: http://www.nationalservice.gov/about/serveamerica/index.asp.
- 15.Morrow-Howell N. Volunteering in later life: Research frontiers. J Gerontol B Psychol Sci Soc Sci. 2010;65:461–469. doi: 10.1093/geronb/gbq024. [DOI] [PubMed] [Google Scholar]
- 16.Jette AM, Branch LG. A ten-year follow-up of driving patterns among community-dwelling elderly. Hum Factors. 1992;34:25–31. doi: 10.1177/001872089203400104. [DOI] [PubMed] [Google Scholar]
- 17.Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci. 2000;55:S334–340. doi: 10.1093/geronb/55.6.s334. [DOI] [PubMed] [Google Scholar]
- 18.Edwards JD, Perkins M, Ross LA, et al. Driving status and three-year mortality among community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2009;64:300–305. doi: 10.1093/gerona/gln019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards JD, Lunsman M, Perkins M, et al. Driving cessation and health trajectories in older adults. J Gerontol A Biol Sci Med Sci. 2009;64:1290–1295. doi: 10.1093/gerona/glp114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mezuk B, Rebok GW. Social integration and social support among older adults following driving cessation. J Gerontol B Psychol Sci Soc Sci. 2008;63:S298–303. doi: 10.1093/geronb/63.5.s298. [DOI] [PubMed] [Google Scholar]
- 21.Johnson JE. Older rural adults and the decision to stop driving: The influence of family and friends. J Community Health Nurs. 1998;15:205–216. doi: 10.1207/s15327655jchn1504_2. [DOI] [PubMed] [Google Scholar]
- 22.Johnson JE. Urban older adults and the forfeiture of a driver’s license. J Gerontol Nurs. 1999;25:12–18. doi: 10.3928/0098-9134-19991201-11. [DOI] [PubMed] [Google Scholar]
- 23. [Accessed Nov 16, 2009];Sample Sizes and Response Rates (2002 and beyond). Fall 2008 [on-line] Available at: http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf.
- 24.Li Y, Ferraro KF. Volunteering and depression in later life: Social benefit or selection processes? J Health Soc Behav. 2005;46:68–84. doi: 10.1177/002214650504600106. [DOI] [PubMed] [Google Scholar]
- 25.Musick MA, Wilson J. Volunteering and depression: The role of psychological and social resources in different age groups. Soc Sci Med. 2003;56:259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- 26.Thoits PA, Hewitt LN. Volunteer work and well-being. J Health Soc Behav. 2001;42:115–131. [PubMed] [Google Scholar]
- 27.Van Willigen M. Differential benefits of volunteering across the life course. J Gerontol B Psychol Sci Soc Sci. 2000;55:S308–318. doi: 10.1093/geronb/55.5.s308. [DOI] [PubMed] [Google Scholar]
- 28.Parker T. [Accessed Nov 17, 2009];Measuring Rurality: Rural-Urban Continuum Codes. 2004 Apr 24; 2004. Available at: http://www.ers.usda.gov/briefing/rurality/RuralUrbCon/
- 29.St Clair P, Bugliari D, Chien S, et al. RAND HRS Data Documentation, Version D. RAND Center for the Study of Aging; Apr, 2004. p. 981. [Google Scholar]
- 30.Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr. 1999;11:139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- 31.Weissman MM, Sholomskas D, Pottenger M, et al. Assessing depressive symptoms in five psychiatric populations: A validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- 32.D’Agostino RB., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17:2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 33.Rosenbaum P, Rubin DB. The Central Role of the Propensity Score in Observational Studies for Causal Effects. Biometrika. 1983;70:44–55. [Google Scholar]
- 34.Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984;79:516–524. [Google Scholar]
- 35.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 36.Krause N. Assessing stress-buffering effects: A cautionary note. Psychol Aging. 1995;10:518–526. doi: 10.1037//0882-7974.10.4.518. [DOI] [PubMed] [Google Scholar]
- 37.Johnson JE. Informal social support networks and the maintenance of voluntary driving cessation by older rural women. J Community Health Nurs. 2008;25:65–72. doi: 10.1080/07370010802017034. [DOI] [PubMed] [Google Scholar]
- 38.Rogers CC. The Older Population in 21st Century Rural America. Rural Am. 2002;17:2–10. [Google Scholar]
- 39.Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 40.Morrow-Howell N, Hinterlong J, Rozario PA, et al. Effects of volunteering on the well-being of older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58:S137–145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- 41.Sims RV, Ahmed A, Sawyer P, et al. Self-reported health and driving cessation in community-dwelling older drivers. J Gerontol A Biol Sci Med Sci. 2007;62:789–793. doi: 10.1093/gerona/62.7.789. [DOI] [PubMed] [Google Scholar]
- 42.Adler NE. Community preventive services. Do we know what we need to know to improve health and reduce disparities? Am J Prev Med. 2003;24:10–11. doi: 10.1016/s0749-3797(02)00649-9. [DOI] [PubMed] [Google Scholar]
- 43.Dannenberg AL, Jackson RJ, Frumkin H, et al. The impact of community design and land-use choices on public health: A scientific research agenda. Am J Public Health. 2003;93:1500–1508. doi: 10.2105/ajph.93.9.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Masotti PJ, Fick R, Johnson-Masotti A, et al. Healthy naturally occurring retirement communities: A low-cost approach to facilitating healthy aging. Am J Public Health. 2006;96:1164–1170. doi: 10.2105/AJPH.2005.068262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ormond BA, Black KJ, Tilly J, et al. [Accessed Mar 5, 2010];Supportive Services Programs in Naturally Occurring Retirement Communities. 2004 Nov; Available at: http://aspe.hhs.gov/daltcp/Reports/NORCssp.htm#concept.
- 46.Gross J. Aging at Home: For a Lucky Few, a Wish Come True. New York Times. New York City. 2006 Feb 6; [Google Scholar]
- 47.Covinsky KE, Palmer RM, Counsell SR, et al. Functional status before hospitalization in acutely ill older adults: Validity and clinical importance of retrospective reports. J Am Geriatr Soc. 2000;48:164–169. doi: 10.1111/j.1532-5415.2000.tb03907.x. [DOI] [PubMed] [Google Scholar]
- 48.Katz JN, Chang LC, Sangha O, et al. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 49.Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22:140–146. doi: 10.1111/j.1748-0361.2006.00022.x. [DOI] [PubMed] [Google Scholar]
- 50.Pathman DE, Ricketts TC, 3rd, Konrad TR. How adults’ access to outpatient physician services relates to the local supply of primary care physicians in the rural southeast. Health Serv Res. 2006;41:79–102. doi: 10.1111/j.1475-6773.2005.00454.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


