Abstract
Psychiatric disorders are now the most common reason for long-term sickness absence. The associated loss in productivity and the payment of disability benefits places a substantial burden on the economies of many developed countries. The occupational dysfunction associated with psychiatric disorders can also lead to poverty and social isolation. As a result the area of work and psychiatric disorders is a high priority for policymakers.
There are two main agendas: for many researchers and clinicians the focus is on the need to overcome stigma and ensure people with severe psychiatric disorders have meaningful work; however the public health agenda predominantly relates to the more common disorders such as depression and anxiety, which contribute a greater burden of disability benefits and pensions. In this review we attempt to address this second agenda.
The relatively sparse evidence available reveals a complex field with significant interplay between medical, psychological social and cultural factors. Sick leave can be a ‘process’ as well as an ‘event’. In this review we propose a staged model where different risk and protective factors contribute to the onset of psychiatric disorders in the working population, the onset of short-term sickness absence, and the transition from short- to long-term absence. We also examine strategies to manage psychiatric disorder in the workforce with a view towards returning the employee to work.
Our aim in this review is to highlight the complexity of the area, to stimulate debate and to identify important gaps in knowledge where further research might benefit both patients and wider society.
Introduction
One of the most powerful ways in which psychiatric disorders lead to social exclusion is via their impact on occupational function.1 Psychiatric disorders account for one-third of all disability benefits across the OECD member countries2 and significantly reduce the ability of people with other disorders to work.3,4 While low rates of employment among patients with severe psychiatric disorders remains a major concern,5 this review will focus on the increasing number of individuals on disability benefits whose long-term absence is attributed to common psychiatric disorders, such as anxiety and depression.
The literature on occupation and psychiatric disorders often focuses on work as a potentially harmful ‘exposure’.6 We suggest that, while such risk factors are important, for most people, most of the time, good work is beneficial for mental health.7 Being in work is associated with lower prevalence of depression and lower incidence of suicide,8,9 while longstanding worklessness carries its own risks.10
In this review we examine the relationship between work and common psychiatric disorders across the process of becoming ill at work, going off sick, staying off sick and returning to work. We also examine the evidence for interventions to assist individuals to either remain in or return to work.
Stages of symptom development
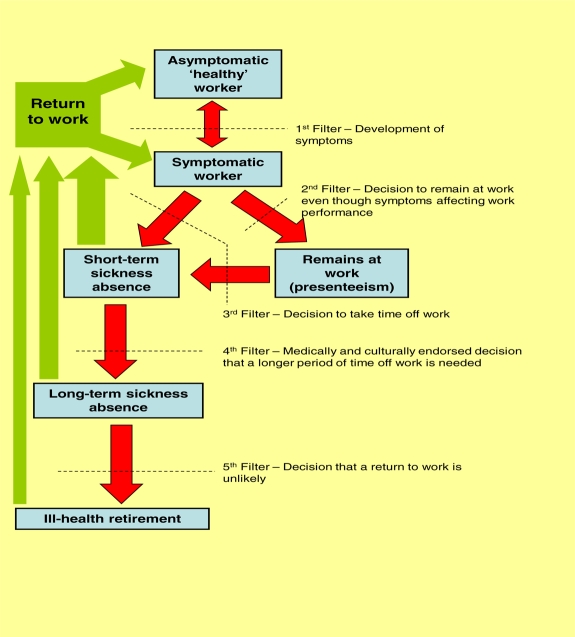
Going off work sick and returning to work are complex behaviours in which individual perceptions, beliefs and decisions are crucial. We suggest it is helpful to divide this process into stages, in a model akin to Goldberg and Huxley's model of levels of psychiatric care.11 They described the pathway from being symptomatic; seeking help; having a psychiatric disorder recognized in primary care; being referred to secondary care; and finally, inpatient treatment. Between each level ‘filters’ operate, and the chance of passing through these filters is influenced by different sets of risk factors. We propose a similar model for the progress of employees from the development of symptoms at work and through any sickness absence (Figure 1). On rare occasions, some employees may ‘skip’ stages, for example if an individual is involved in a accident and is injured to the point that they pass straight from being a healthy worker to a having medically and culturally endorsed period of long-term sickness absence (fourth filter). However, such instances are unusual and for most workers on long-term sickness absence, their progression towards increasing occupational incapacity has occurred in stages, each of which has a unique set of contributing factors.
Figure 1.
Proposed model of the ‘journey’ from symptom development to ill health retirement, highlighting the key stages, barriers and decisions involved (in colour online)
The development of symptoms: the job
Using UK Office for National Statistics data, Stansfeld found higher rates of psychiatric disorders among teachers, sales staff and managers in government organizations, and lower rates in plant operatives and health-associated professions.12 Other sources of routinely collected data have shown similar results – nurses, teachers, welfare officers and policemen had higher levels of psychiatric disorders while construction workers had low rates of illness.13 Similar studies from Norway identified farmers at particular risk for anxiety and depression.14 Although a wide range of ‘good’ and ‘bad’ jobs have been identified there is no obvious common ‘toxic’ link. Furthermore the direction of causation is unclear. Certain people are drawn to certain jobs and the observed effect may be due to self-selection.
The development of symptoms: the individual and his background
Most research into work and psychiatric disorder has focused on the nature of the work or the nature of the disorder.15 Relatively little interest has been shown on the link between the two – the individual. Individual factors must play a role in the development of symptoms and any decision to take time off work. Not all employees in a ‘toxic’ workplace go off sick, and, in the UK, there are about 3 million ‘disabled’ people in work,16 more than claim Incapacity Benefit. Karasek,17 Marmot18 and Stansfeld19 have all alluded to the role of individual perceptions as the mediator between external factors and occupational dysfunction but what might influence such perceptions is difficult to study.
One mechanism to investigate this area involves examining potential early life risk factors. Henderson used data from the Aberdeen Children of the 1950s study to show an association between teachers' ratings of temperament in childhood and being permanently sick or disabled 40 years later.20
The development of symptoms: psychosocial work environment
Two major models have emerged to describe the broader ‘psychosocial work environment’. In the ‘Job Strain’ model, described by Karasek and Theorell, the ‘demands’ of work are contrasted with the level of control over that work.17 ‘Job strain’ is said to occur when high demands are associated with low decision latitude and is an independent predictor of psychiatric morbidity.21 The ‘effort–reward imbalance’ model was proposed by Siegrist. Stress responses occur when effort expended at work is not matched by rewards in terms of pay, self-esteem and sense of achievement.22 This too has been shown to be associated with psychiatric disorder.21
While the study of the psychosocial work environment has deepened our understanding of the nature of the relationship between the individual and his work, the models have limitations. Mostly they rely on self-reported data thus incorporating beliefs, perceptions and attitudes to work. When supervisors report, rather than self-reported assessments, of work demands were included in one analysis of Whitehall II data the association between the psychosocial work environment and psychological morbidity disappeared.23 There have been two methodologically stronger studies more recently that have used objective measures of the psychosocial work environment. In Virtanen's study24 overcrowding in hospital wards was used as a proxy for the psychosocial work environment of the doctors and nurses working there. On this objective measure greater overcrowding was associated with an increased consumption of antidepressant medication. Occupational function, e.g. sick leave, was not assessed. While an important study, it is not clear whether ‘overcrowding’ is a ‘demand’ or ‘control’ issue. The question as to why some staff on overcrowded wards became depressed and some did not remains unanswered. Iennaco studied a cohort of workers in heavy industrial settings.25 Job demand and job control were rated externally by a safety and hygiene manager. Externally rated control was not associated with subsequent depression. Externally rated job demands were associated with depression in multivariable analyses although this association was lost following adjustment for location. The conflicting results of these two studies highlight the need for further research in this area.
Presenteeism
Presenteeism describes a situation where an employee is symptomatic and under-performing, but remains at work.26 Many employees come to work with symptoms suggestive of physical disease, but being less productive due to ill health (presenteeism) is most strongly associated with psychiatric disorders.27 Those whose psychiatric disorder has developed insidiously may not realize how ill they are. There may be a belief that taking time off with psychological symptoms will invite scorn from colleagues and discrimination from managers. The Sainsbury Centre for Mental Health suggested that up to 20% of workers experience psychological symptoms in any one day and that 60% of the costs of psychiatric disorder at work arise from reduced productivity.28 Other studies confirm that depression, of all conditions, has the greatest negative impact on time management and productivity and is equivalent to rheumatoid arthritis in its impact on physical tasks.29
What is it about psychiatric disorder that impairs occupational function? Fatigue might be one of the occupationally toxic elements of depression.30–33 More studies, though, have concentrated on cognitive dysfunction.34 There is relatively little association between the objective level of psychiatric severity and occupational function. One study found that only half of the impairment reported by those who were out of the workforce could be explained by mental and physical symptoms or illnesses.35 More work is needed on identifying which aspects of psychiatric illness are associated with occupational dysfunction.
Short-term sickness absence
Short-term absences are by far the most common type of absence episode and the ‘causes’ appear to be different to longer-term sick leave. The Whitehall II study found respiratory and gastrointestinal disorders were the most common causes of short-term absences,36 although it is likely the role played by psychiatric disorders is underestimated. Psychiatric disorders may present as physical symptoms and those assessing may not recognize or be confident to diagnose a psychiatric illness or may see labelling the patient's difficulty as ‘physical’ as being in their best interest.37
Long-term sickness absence
There is no agreed demarcation between short- and long-term sickness absence,38 complicating comparisons between studies and countries.39 Although long-term absence makes up only a small proportion of absences, it accounts for up to one-third of days off and 75% of absence costs.40–42
Compared to the literature on risk factors for sickness absence, the literature on its outcomes is very sparse.43 A recent systematic review of long-term sickness absence identified five cohort studies investigating 77 risk factors. All 16 significant risk factors were predisposing rather than perpetuating factors, and the level of evidence for these was weak at best. The authors concluded that there are no published studies on perpetuating factors for long-term sickness absence.44 We suggest that distinguishing precipitating and perpetuating factors may be an essential step prior to developing interventions. Perpetuating factors may include a wide range of social operants (receipt of disability payments, fulfilment of the sick role, family support, and so on) all of which potentially reduce the chance that the individual will return to work.
Ill health retirement
Less work still has been done on ill health retirement. As with sickness absence, the most common ‘causes’ are psychiatric disorders and musculoskeletal problems. Again, the true impact of psychiatric symptoms may be underestimated. A large prospective study found that anxiety and depression were strong predictors of ill health retirement even for non-psychiatric attributions.45–47 The same was found for insomnia, which only in rare cases is denoted as a cause for disability pensions.48
The health impact of ill health retirement is unclear – some studies show an improvement over time.49 However, this apparent improvement might instead be a return to normal after a temporarily increased level of symptoms around the time of being awarded the disability pension.50 Given the potential harmful social and individual effects, it is surprising that many of those awarded ill health retirement for psychiatric illness report having received minimal treatment51 often without a trial of more than one antidepressant.52,53 Nonetheless several studies, most notably of health service employees and teachers in the UK, identify that a high proportion of ill health retired employees (up to 36%) are back in work a year later.54,55
Returning to work
A successful return to work is the desired outcome for most episodes of sick leave. There has been little research on ways to secure this. The longer someone is off sick the less likely he or she is to return to work. This relates partly to factors surrounding the decision to take time off, but also to obstacles implementing a return to work. Fear-avoidant and catastrophizing coping strategies56 impact on the decision to leave work and are also likely to play a role in decisions on returning to work. Particularly in workers who believe that their work has either caused their health problem or made it worse,57 there may be a fear that symptoms will be made worse by going back to work. Other concerns will include how to re-establish relationships with both colleagues and managers after a period away.
A commonly used technique to overcome some of these problems is a phased return to work. The employee starts back to work initially part-time and gradually builds up the hours and/or days over several weeks. While apparently sensible, there is little evidence to support its use. There is also no standard way in which an individual moves through the ‘stages’ or ‘phases’. Recovery from psychiatric disorders is difficult to predict and might not fit into a rigid protocol. However, adjusting time at work based on symptom levels may exacerbate avoidant coping.
Decisions about when to return to work are made more difficult by issues of timing. In depression improvements in functional or occupational ability lag behind standard markers of clinical improvement.58 As such, even though an employee may have been passed fit to return to work, he or she is unlikely to be able rapidly to attain previous levels of productivity. Such situations can produce conflict and difficulty between managers and employees. The person returning to work may realize he is not able to perform effectively, and may become vigilant for any symptoms which might confirm his belief that he is starting to become ill again. The attitudes of the individual's co-workers might also play a role, positive or negative, in making the return to work a success.59
Health and occupational function
Physical symptoms and mental symptoms
Psychiatric disorders are often co-morbid with physical illness.60 While it might be apparent from the outside that it is the psychiatric disorder that has ‘tipped the scales’ and led to sick leave being taken, this may not be so obvious to the individual who might not seek help for the psychiatric disorder. This then persists and acts as a barrier to recovery and return to work.3 Attributing sickness absence to a single ‘cause’ ignores the multiple factors that contribute to the process and the fact that both physical and mental functioning exist on a continuum rather that discrete categories.61 The propensity for those with psychiatric disorders to have periods of absence, ‘… not necessarily the type diagnosed as nervous’ has been recognized for at least 80 years.62 The significant effect of co-morbidity has been demonstrated both ways round4 – a study of women with psychiatric disorders showed elevated levels of sickness absence labelled as ‘musculoskeletal’ and ‘gastrointestinal’63 while a large study of those off work with musculoskeletal disorders found that 20% had a co-morbid psychiatric diagnosis.64
What can be done?
The public health impact of psychiatric symptoms on occupational outcomes is substantial but it is unclear how governments, insurers, employers, and health services should respond and there is a paucity of high quality studies to guide them.65 There is an urgent need to provide appropriate services, including reducing potential workplace exposures, improving detection and developing treatments for workers with psychiatric disorders. Care must be taken though as campaigns which screen for psychiatric symptoms, attempt to reduce stigma and raise awareness may lead many individuals with otherwise transient minor symptoms having their distress medicalized. An analogy is provided by Coggon who in a review of interventions for back pain66 suggested that the back pain epidemic of the 1970s and 1980s was partly a result of the very interventions which aimed to make workers aware of the risk of harm to their backs.
Prevention
While there have been some examples of simple changes in the workplace leading to lower levels of distress,67 a recent systematic review concluded there was insufficient evidence to judge the effectiveness of any specific organizational programme of prevention.68 Educating and training individual managers does not seem to reduce job strain or psychiatric illness.69,70 Alternative preventative approaches have focused on increasing the resilience of individual workers. Two separate systematic reviews have concluded that the heterogeneity of individually focused prevention programmes and the limited methodological quality prevent any definite recommendations being made.68,71 Nevertheless, both reviews reported that stress management programmes might have a modest or short-term impact on a range of variables associated with individual distress.68,71 Other reviews have concluded that interventions which reduce psychological distress among workers will also reduce levels of sickness absence.72 A meta-analysis of 48 experimental studies agreed that individually focused interventions tended to be more effective than organizational interventions74 and cognitive behavioural approaches had the best evidence for effectiveness.71,73
Several employers have instigated general ‘healthy lifestyle’ programmes to improve employee health and work attendance.74 Undertaking regular exercise and maintaining a healthy weight may help prevent psychiatric disorders75,76 but no reliable studies have been able to demonstrate that exercise programmes in the workplace reduce levels of psychiatric illness.71
Screening
A large trial of screening for depression in the workplace77 demonstrated that screening, followed by a systematic programme of telephone outreach and care management (encouraging employees to enter appropriate treatment and monitoring treatment quality) resulted in decreased symptoms, higher job retention and more hours worked. There is also some theoretical evidence that screening programmes may be cost-effective for purchasers,78 however this should be tempered by a body of evidence from medical settings indicating screening for depression is not associated with improved outcomes.79
Preventing or reducing short-term sickness absence
Established guidelines on the treatment of depression and anxiety80,81 are based on the broad research evidence from primary and secondary care trials, few of which have measured occupational outcomes. It is therefore difficult to assess the occupational benefits of interventions recommended in such guidelines, particularly as symptom improvement does not necessarily correlate with return to work.
The Cochrane Collaboration has published a systematic review of all randomized controlled trials of work or worker-directed interventions for depression.82 The authors identified 11 studies, involving 2556 individuals, and concluded there was no evidence that either medication, enhanced primary care, or psychological interventions have any impact on the amount of sickness absence taken by depressed individuals.82 A recent meta-analysis showed that while a range of different treatments can produce significant reductions in symptom severity, the associated gain in labour output was only one-third as large as the reductions in symptoms.83 The lack of an effect of standard treatments on occupational outcomes suggests that additional specific interventions addressing return to work issues may be needed.
Once an employee begins an episode of sickness absence a range of healthcare professionals may become involved in their management. A small number of trials of primary care-based interventions have shown that providing primary care clinicians with the skills and resources to treat psychiatric disorders is effective in helping people to retain employment.84 There will, however, be a proportion of those suffering from psychiatric disorders who do not respond to treatment in the primary care setting or whose cases are too complex to be managed by their general practitioner alone. As most secondary care psychiatric services are focused on caring for those with psychosis, there is currently a gap between primary and secondary services for those with complex or more severe episodes of depression and anxiety.85 When occupational health practitioners are available, training them in cognitive behavioural approaches such as graded activity, can result in employees returning to work more rapidly.86 This approach highlights the advantages of both early intervention and of keeping an individual, and their treatment, as close to the workplace as possible. Our current approach of taking an ill person away from work, trying to make them better, then guessing at when they may be ready to return seems inflexible and unhelpful in comparison.
Employee Assistance Programmes (EAPs) and counselling are common workplace interventions which usually use relatively unstructured psychological support, delivered by individuals from a range of professional backgrounds. There has been a dramatic rise in the number of organizations offering workplace counselling. An English Appeal Court ruling in 2002 suggested the provision of a counselling service was likely to satisfy an employer's duty of care, which may have led many employers to implement a counselling scheme as a form of ‘insurance’87 against stress at work claims. In a 2001 systematic review, the British Association of Counselling and Psychotherapy claimed counselling could reduce sickness absence.88 Others have suggested these conclusions were not justified owing to the poor quality of studies involved.89 Workplace counselling may be helpful for some, but better quality evidence is needed to guide its use.
Managing long-term sickness absence
The longer an employee is absent from work, the less likely they are to return.90 The UK National Institute for Health and Clinical Excellence (NICE) recently published preliminary guidance on the management of individual on long-term sickness absence, which they defined as an absence of four or more weeks.91 This recommended that all employees should undergo an assessment within 12 weeks (ideally 2–6 weeks) of starting an episode of sick leave and highlights the evidence for specific interventions that should be considered, such as cognitive behavioural therapy.91
Psychiatric disorders often occur co-morbidly in those with chronic physical health problems,60 and when present, increases the risk of long-term sickness absence progressing to permanent disability.46 The presence of a psychiatric disorder should therefore be considered in almost all individuals on long-term sickness absence, regardless of the initial reason for the period of absence. A study based within a large French organization (EDF – Gaz de France) suggests that when a simple psychiatric screening programme is added to the usual care of those already on long-term sickness absence, significant numbers of previously undiagnosed psychiatric disorders can be identified and effectively treated.92 However, it remains unclear whether the symptomatic improvements seen in such programmes translate into improved occupational outcomes.
Population-based interventions
Public information campaigns may have a role in tackling the occupational consequences of psychiatric disorders. In 1997 a public health campaign was undertaken in Victoria, Australia, which aimed to educate the population on the importance of staying active and remaining at work when they suffered back pain.93 A research project conducted at the time of this campaign showed progressive changes in attitudes to back pain, with a clear decline in the numbers of workers' compensation claims.94 Although campaigns to reduce stigma associated with psychiatric disorders may improve public attitudes,95 there is a risk that reduced stigma might lead to a greater tendency for distress to be medicalized and false labelling of distress as a psychiatric disorder.
Conclusions
The relationship between work and psychiatric disorder is complex but of increasing interest and importance. It is becoming clear that the decision of some individuals to go on sick leave or seek benefits is the result of a complicated set of factors to which individual perceptions, beliefs and other psycho-social influences contribute.
Secondary care psychiatry has not prioritized the role of work and the nature of impaired occupational function, especially outside psychotic illnesses, and there is too little interface between occupational medicine and psychiatry. A gap in service provision exists whereby a proportion of working age patients with common psychiatric disorders and/or functional somatic syndromes cannot be managed successfully in primary care, yet services which focus largely on psychotic illness have little to offer them. Many of these will languish on long-term benefits at great personal and economic cost.
The psycho-social determinants of the pathway from healthy working to long-term sickness absence are under-researched. Better information is needed on the impact of individual depressive symptoms on work and on individual non-work risk factors for sick leave. More studies are needed on the changing way in which known risk factors impact on occupational impairment over time.
There remains much to be done to develop effective strategies to return, and subsequently retain, an employee who has been off sick with a psychiatric disorder. Getting managers and colleagues to ‘buy in’ to these approaches will in many ways define their success.
DECLARATIONS
Competing interests
None declared
Funding
MJH is supported by the NIHR Biomedical Research Centre for Mental Health BRC Nucleus jointly funded by the Guy's and St Thomas' Charity and the South London and Maudsley Trustees; SBH and MH are funded by the NIHR Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry, King's College London; SØ is funded by the Research Council of Norway; AM was funded by the Research Council of Norway, and is now funded by the Norwegian Institute of Public Health and University of Bergen
Ethical approval
Not applicable
Guarantor
MJH
Contributorship
MJH, SBH and MH initially conceived the review; all authors contributed to the intellectual work of the review process; MJH and SBH drafted the initial manuscript; MH, SØ and AM critically revised the document for important intellectual content; all authors read and approved the final manuscript
Acknowledgements
None
REFERENCES
- 1.Harvey SB, Henderson M, Lelliott P, Hotopf M Mental health and employment: much work still to be done. Br J Psychiatry 2009;194:201–3 [DOI] [PubMed] [Google Scholar]
- 2.OECD Transforming Disability into Ability. Policies to promote work and income security for disabled people. Paris: OECD Publications Service, 2003 [Google Scholar]
- 3.Kessler RC, Ormel J, Demler O, Stang PE Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. J Occup Environ Med 2003;45:1257–66 [DOI] [PubMed] [Google Scholar]
- 4.Savikko A, Alexanderson K, Hensing G Do mental health problems increase sickness absence due to other diseases? Soc Psychiatry Psychiatr Epidemiol 2001;36:310–16 [DOI] [PubMed] [Google Scholar]
- 5.Kooyman I, Dean K, Harvey S, Walsh E Outcomes of public concern in schizophrenia. Br J Psychiatry 2007;50:s29–36 [DOI] [PubMed] [Google Scholar]
- 6.Stansfeld S, Candy B Psychosocial work environment and mental health – a meta-analytic review. Scand J Work Environ Health 2006;32:443–62 [DOI] [PubMed] [Google Scholar]
- 7.Waddell G, Burton A Is work good for your health and well-being? London: The Stationery Office, 2006 [Google Scholar]
- 8.Boardman AP, Grimbaldeston AH, Handley C, Jones PW, Willmott S The North Staffordshire Suicide Study: a case-control study of suicide in one health district. Psychol Med 1999;29:27–33 [DOI] [PubMed] [Google Scholar]
- 9.Claussen B, Bjorndal A, Hjort PF Health and re-employment in a two year follow up of long term unemployed. J Epidemiol Community Health 1993;47:14–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Head J, Ferrie JE, Alexanderson K, Westerlund H, Vahtera J, Kivimaki M Diagnosis-specific sickness absence as a predictor of mortality: the Whitehall II prospective cohort study. BMJ 2008;337:a1469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goldberg D, Huxley P Mental Illness in the Community. London: Tavistock, 1980 [Google Scholar]
- 12.Stansfeld S, Head J, Rasul F, Singleton N, Lee A Occupation and Mental Health: Secondary analyses of the ONS Psychiatric Morbidity Survey of Great Britain. London: Health & Safety Executive, 2003 [Google Scholar]
- 13.Barham G, Begum N Sickness absence from work in the UK. Labour Market Trends 2005;113:149–58 [Google Scholar]
- 14.Sanne B, Mykletun A, Dahl AA, Moen BE, Tell GS Occupational differences in levels of anxiety and depression: the Hordaland Health Study. J Occup Environ Med 2003;45:628–38 [DOI] [PubMed] [Google Scholar]
- 15.Harvey SB, Henderson M Occupational psychiatry. Psychiatry 2009;8:174–8 [Google Scholar]
- 16.Office for National Statistics Labour Force Survey. London: ONS, 2005 [Google Scholar]
- 17.Karasek R, Theorell T Healthy work: Stress, Productivity and the Reconstruction of Working Life. New York, NY: Basic Books, 1990 [Google Scholar]
- 18.Marmot MG Status Syndrome. London: Times Books, 2004 [Google Scholar]
- 19.Stansfeld SA, North FM, White I, Marmot MG Work characteristics and psychiatric disorder in civil servants in London. J Epidemiol Community Health 1995;49:48–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henderson M, Hotopf M, Leon D Childhood temperament and long term sickness absence in adult life. Br J Psychiatry 2009;194:220–3 [DOI] [PubMed] [Google Scholar]
- 21.Stansfeld SA, Fuhrer R, Shipley MJ, Marmot MG Work characteristics predict psychiatric disorder: prospective results from the Whitehall II Study. Occup Environ Med 1999;56:302–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siegrist J Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol 1996;1:27–41 [DOI] [PubMed] [Google Scholar]
- 23.Stansfeld S, Feeney A, Head J, Canner R, North F, Marmot M Sickness absence for psychiatric illness: the Whitehall II Study. Soc Sci Med 1995;40:189–97 [DOI] [PubMed] [Google Scholar]
- 24.Virtanen M, Pentti J, Vahtera J, et al. Overcrowding in hospital wards as a predictor of antidepressant treatment among hospital staff. Am J Psychiatry 2008;165:1482–6 [DOI] [PubMed] [Google Scholar]
- 25.DeSanto Iennaco J, Cullen MR, Cantley L, Slade MD, Fiellin M, Kasl SV Effects of externally rated job demand and control on depression diagnosis claims in an industrial cohort. Am J Epidemiol 2010;171:303–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vingard E, Alexanderson K, Norlund A Chapter 10. Sickness presence. Scand J Public Health 2004;32:216–21 [DOI] [PubMed] [Google Scholar]
- 27.Kessler RC, Greenberg PE, Mickelson KD, Meneades LM, Wang PS The effects of chronic medical conditions on work loss and work cutback. J Occup Environ Med 2001;43:218–25 [DOI] [PubMed] [Google Scholar]
- 28.Sainsbury Centre for Mental Health Mental health and employment. Briefing No. 33. London: SCMH, 2007 [Google Scholar]
- 29.Burton WN, Pransky G, Conti DJ, Chen CY, Edington DW The association of medical conditions and presenteeism. J Occup Environ Med 2004;46 (Suppl. 6):S38–45 [DOI] [PubMed] [Google Scholar]
- 30.Harvey SB, Wadsworth M, Wessely S, Hotopf M The relationship between prior psychiatric disorder and chronic fatigue: evidence from a national birth cohort study. Psychol Med 2008;38:933–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janssen N, Kant IJ, Swaen GM, Janssen PP, Schroer CA Fatigue as a predictor of sickness absence: results from the Maastricht cohort study on fatigue at work. Occup Environ Med 2003;60 (Suppl. 1):71–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lerner D, Adler DA, Chang H, et al. The clinical and occupational correlates of work productivity loss among employed patients with depression. J Occup Environ Med 2004;46 (Suppl. 6):S46–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harvey SB, Wessely S, Kuh D, Hotopf M The relationship between fatigue and psychiatric disorders: Evidence for the concept of neurasthenia. J Psychosom Res 2009;66:445–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mancoso L Reasonable accomodation for workers with psychiatric disabilities. Pscyhosocial Rehabilitation Journal 1990;14:3–19 [Google Scholar]
- 35.Overland S, Glozier N, Mæland J, Aarø L, Mykletun A Employment Status and Perceived Health in the Hordaland Health Study (HUSK). BMC Public Health 2006;6:219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stansfeld SA, Fuhrer R, Head J, Ferrie J, Shipley M Work and psychiatric disorder in the Whitehall II Study. J Psychosom Res 1997;43:73–81 [DOI] [PubMed] [Google Scholar]
- 37.Glozier N Workplace effects of the stigmatization of depression. J Occup Environ Med 1998;40:793–800 [DOI] [PubMed] [Google Scholar]
- 38.Hensing G, Alexanderson K, Allebeck P, Bjurulf P How to measure sickness absence? Literature review and suggestion of five basic measures. Scand J Soc Med 1998;26:133–44 [DOI] [PubMed] [Google Scholar]
- 39.Hensing G. R. Chapter 4. Methodological aspects in sickness-absence research. Scand J Public Health 2004;32:44–8 [DOI] [PubMed] [Google Scholar]
- 40.Unum Limited IfES Towards a Better Understanding of Sickness Absence. Dorking: Unum, 2001 [Google Scholar]
- 41.CBI Attending to absence: CBI / AXA absence and labour turnover survey 2006. London: Confederation for British Industry, 2007 [Google Scholar]
- 42.Spurgeon P, Mazelan P, Barwell F, Flanagan H New directions in Managing Employee Absence: An evidence based approach. London: Chartered Institute of Personnel and Development, 2007 [Google Scholar]
- 43.Vingard E, Alexanderson K, Norlund A Chapter 9. Consequences of being on sick leave. Scand J Public Health 2004;32:207–15 [DOI] [PubMed] [Google Scholar]
- 44.Dekkers-Sanchez PM, Hoving JL, Sluiter JK, Frings-Dresen MH Factors associated with long-term sick leave in sick-listed employees: a systematic review. Occup Environ Med 2008;65:153–7 [DOI] [PubMed] [Google Scholar]
- 45.Mykletun A, Overland S, Dahl AA, et al. A population-based cohort study of the effect of common mental disorders on disability pension awards. Am J Psychiatry 2006;163:1412–18 [DOI] [PubMed] [Google Scholar]
- 46.Knudsen A, Overland S, Aakvaag H, Harvey S, Hotopf M, Mykleltun A Common mental disorder and disability pension award: Seven year follow-up of the HUSK study. J Psychosomatic Research 2010;69:59–67 [DOI] [PubMed] [Google Scholar]
- 47.Mykletun A, Heradstveit O, Eriksen K, et al. Health anxiety and disability pension award: The HUSK study. Psychosom Med 2009;71:353–60 [DOI] [PubMed] [Google Scholar]
- 48.Sivertsen B, Overland S, Neckelmann D, et al. The long-term effect of insomnia on work disability – The HUNT-2 historical cohort study. Am J Epidemiol 2006;163:1018–24 [DOI] [PubMed] [Google Scholar]
- 49.Ejlertsson G, Eden L, Leden I Predictors of positive health in disability pensioners: a population-based questionnaire study using Positive Odds Ratio. BMC Public Health 2002;2:20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Øverland S, Glozier N, Henderson M, Mæland J, Hotopf M, Mykleltun A Health status before, during and after disability pension award. The Hordaland Health Study (HUSK). Occup Environ Med 2008;65:769–73 [DOI] [PubMed] [Google Scholar]
- 51.Overland S, Glozier N, Krokstad S, Mykletun A Undertreatment before the award of a disability pension for mental illness: the HUNT Study. Psychiatr Serv 2007;58:1479–82 [DOI] [PubMed] [Google Scholar]
- 52.Isometsa ET, Katila H, Aro T Disability pension for major depression in Finland. Am J Psychiatry 2000;157:1869–72 [DOI] [PubMed] [Google Scholar]
- 53.Honkonen TI, Aro TA, Isometsa ET, Virtanen EM, Katila HO Quality of treatment and disability compensation in depression: Comparison of 2 nationally representative samples with a 10-year interval in Finland. J Clin Psychiatry 2007;68:1886–93 [DOI] [PubMed] [Google Scholar]
- 54.Brown J, Gilmour WH, Macdonald EB Return to work after ill-health retirement in Scottish NHS staff and teachers. Occup Med (Lond) 2006;56:480–4 [DOI] [PubMed] [Google Scholar]
- 55.Pattani S, Constantinovici N, Williams S Predictors of re-employment and quality of life in NHS staff one year after early retirement because of ill health; a national prospective study. Occup Environ Med 2004;61:572–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Severeijns R, Vlaeyen JW, van den Hout MA, Picavet HS Pain catastrophizing is associated with health indices in musculoskeletal pain: a cross-sectional study in the Dutch community. Health Psychol 2004;23:49–57 [DOI] [PubMed] [Google Scholar]
- 57.Jones J, Huxtable C, Hodgson J Self-reported work-related illness in 2004/2005: results from the Labour Force Survey. London: Health & Safety Executive, 2005 [Google Scholar]
- 58.Mintz J, Mintz LI, Arruda MJ, Hwang SS Treatments of depression and the functional capacity to work. Arch Gen Psychiatry 1992;49:761–8 [DOI] [PubMed] [Google Scholar]
- 59.Glozier N, Hough C, Henderson M, Holland-Elliott K Attitudes of nursing staff towards co-workers returning from psychiatric and physical illnesses. Int J Soc Psychiatry 2006;52:525–34 [DOI] [PubMed] [Google Scholar]
- 60.Harvey SB, Ismail K Psychiatric aspects of chronic physical disease. Medicine 2008;36:471–4 [Google Scholar]
- 61.Hatch SL, Harvey SB, Maughan B A developmental-contextual approach to understanding mental health and well-being in early adulthood. Soc Sci Med 2010;70:261–8 [DOI] [PubMed] [Google Scholar]
- 62.Culpin M, Smith M The Nervous Temperament – A Report for the Industrial Health Research Board. London: His Majesty's Stationery Office, 1930 [Google Scholar]
- 63.Hensing G, Spak F, Alexanderson K, Allebeck P Sick-leave among women and the role of psychiatric disorder. Scand J Soc Med 1997;25:185–92 [DOI] [PubMed] [Google Scholar]
- 64.Sandanger I, Nygard J, Brage S, Tellnes G Occurence of mental health problems and sickness absence with psychiatric diagnoses in general population, gender differences. Oslo: Oslo University, 1997 [Google Scholar]
- 65.Alexanderson K, Norlund A Swedish Council on Technology Assessment in Health Care (SBU). Chapter 12. Future need for research. Scand J Public Health Suppl 2004;63:256–8 [DOI] [PubMed] [Google Scholar]
- 66.Coggon D Occupational medicine at a turning point. Occup Environ Med 2005;62:281–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Totterdell P, Smith L Ten-hour days and eight-hour nights: Can the Ottawa Shift System reduce the problems of shirtwork? Work and Stress 1992;6:139–52 [Google Scholar]
- 68.Graveling RA, Crawford JO, Cowie H, Amati C, Vohra S A review of workplace interventions that promote mental wellbeing in the workplace. Edinburgh: Institute of Occupational Medicine, 2008 [Google Scholar]
- 69.Takao S, Tsutsumi A, Nishiuchi K, Mineyama S, Kawakami N Effects of the job stress education for supervisors on psychological distress and job performance among their immediate subordinates: a supervisor-based randomized controlled trial. J Occup Health 2006;48:494–503 [DOI] [PubMed] [Google Scholar]
- 70.Kawakami N, Takao S, Kobayashi Y, Tsutsumi A Effects of web-based supervisor training on job stressors and psychological distress among workers: a workplace-based randomized controlled trial. J Occup Health 2006;48:28–34 [DOI] [PubMed] [Google Scholar]
- 71.BOHRF Workplace interventions for people with common mental health problems: Evidence review and recommendations. London: British Occupational Health Research Foundation, 2005 [Google Scholar]
- 72.Michie S, Williams S Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med 2003;60:3–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ The benefits of interventions for work-related stress. Am J Public Health 2001;91:270–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harvey SB, Glozier N, Carlton O, et al. Obesity and sickness absence: results from the CHAP study. Occup Med (London) 2010;60:362–8 [DOI] [PubMed] [Google Scholar]
- 75.Rivenes AC, Harvey SB, Mykletun A The relationship between abdominal fat, obesity and common mental disorders: results from the HUNT Study. J Psychosom Res 2009;66:269–75 [DOI] [PubMed] [Google Scholar]
- 76.Wiles NJ, Haase AM, Gallacher J, Lawlor DA, Lewis G Physical activity and common mental disorder: results from the Caerphilly study. Am J Epidemiol 2007;165:946–54 [DOI] [PubMed] [Google Scholar]
- 77.Wang PS, Simon GE, Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA 2007;298:1401–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wang PS, Patrick A, Avorn J, et al. The costs and benefits of enhanced depression care to employers. Arch Gen Psychiatry 2006;63:1345–53 [DOI] [PubMed] [Google Scholar]
- 79.Gilbody S, House AO, Sheldon TA Screening and case finding instruments for depression. Cochrane Database Syst Rev 2005;(4):CD002792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.National Institute for Health and Clinical Excellence Depression: management of depression in primary and secondary care. London: NICE, 2004 [Google Scholar]
- 81.National Institute for Health and Clinical Excellence Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care). London: NICE, 2004 [PubMed] [Google Scholar]
- 82.Nieuwenhuijsen K, Bultmann U, Neumeyer-Gromen A, Verhoeven AC, Verbeek JH, van der Feltz-Cornelis CM Interventions to improve occupational health in depressed people. Cochrane Database Syst Rev 2008;(2):CD006237 [DOI] [PubMed] [Google Scholar]
- 83.Timbie JW, Horvitz-Lennon M, Frank RG, Normand ST A meta-analysis of labour supply effects of interventions for major depressive disorder. Psychiatric Services 2006;57:212–18 [DOI] [PubMed] [Google Scholar]
- 84.Schoenbaum M, Unutzer J, Sherbourne C, et al. Cost-effectiveness of practice-initiated quality improvement for depression: results of a randomized controlled trial. JAMA 2001;286:1325–30 [DOI] [PubMed] [Google Scholar]
- 85.Royal College of Psychiatrists Mental Health and Work. London: The Stationery Office, 2008 [Google Scholar]
- 86.van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med 2003;60:429–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Royal Courts of Justice Supreme Court of Judicature Court of Appeal (Civil Division) on appeal from Liverpool County Court. London: Royal Courts of Justice, 2002 [Google Scholar]
- 88.McLeod J Counselling in the workplace: the facts. A systematic study of the research evidence. Warwickshire: British Association for Counselling and Psychotherapy, 2001 [Google Scholar]
- 89.Henderson M, Hotopf M, Wessely S Workplace counselling. An appeal for evidence. Occup Environ Med 2003;60:899–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Department for Work and Pensions Pathways to work: Helping people into employment. London: Department for Work and Pensions, 2004 [Google Scholar]
- 91.National Institute for Health and Clinical Excellence Managing long-term sickness absence and incapacity for work. London: NICE, 2008 [Google Scholar]
- 92.Godard C, Chevalier A, Lecrubier Y, Lahon G APRAND programme: an intervention to prevent relapses of anxiety and depressive disorders. First results of a medical health promotion intervention in a population of employees. Eur Psychiatry 2006;21:451–9 [DOI] [PubMed] [Google Scholar]
- 93.Buchbinder R, Jolly D, Wyatt M Volvo Award winner in clinical studies: effects of a media campaign on back pain belefs and its potential influence on management of low back pain in general practice. Spine 2001;26:2535–42 [DOI] [PubMed] [Google Scholar]
- 94.Buchbinder R, Jolley D, Wyatt M Population based intervention to change back pain beliefs and disability: three part evaluation. BMJ 2001;322:1516–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Paykel ES, Hart D, Priest RG Changes in public attitudes to depression during the Defeat Depression Campaign. Br J Psychiatry 1998;173:519–22 [DOI] [PubMed] [Google Scholar]