Abstract
The systemic capillary leak syndrome (SCLS), also known as Clarkson’s disease, is a life-threatening disorder of unknown cause. It is characterised by recurrent acute episodes of hypotension, weight gain and generalised oedema with haemoconcentration and hypoproteinaemia caused by paroxysmal capillary hyperpermeability with a shift of plasma fluid from the intravascular to the interstitial space. We report the case of a 40-year-old woman with chronic SCLS treated with high-dose intravenous immunoglobulins, after a prophylactic therapy with theophylline and terbutaline was poorly tolerated and failed to decrease the frequency and severity of the attacks sufficiently.
Background
Idiopathic systemic capillary leak syndrome (SCLS), first described by Clarkson et al in 1960,1 is a rare disorder characterised by episodes of severe hypotension, hypoalbuminaemia and haemoconcentration. About 100 cases have been reported so far. During attacks of SCLS, profound derangement of the vascular endothelium results in leakage of plasma and proteins into the interstitial compartment. These episodes are frequently (about 80%) associated with monoclonal gammopathy.2 3 Attacks of SCLS usually demonstrate three phases: A prodromal phase over 1–2 days with non-specific symptoms is followed by the extravasation phase, lasting 1–4 days, with increased capillary permeability and consequent severe hypovolaemia and hypotension, haemoconcentration and generalised oedema. Serious complications include compartment syndrome and multiple end-organ failure, such as acute tubular necrosis, ischaemic brain injury or ischaemic hepatitis, due to prolonged hypoperfusion. During the recovery phase, extravasated fluids are recruited back into the intravascular space leading to an intravascular volume overload and pulmonary oedema. No prophylactic therapy has been conclusively proven to prevent future episodes of SCLS, furthermore, the rarity of the disorder makes controlled trials unfeasible. However, several case series have shown a prophylactic regimen of theophylline and terbutaline to decrease the frequency of attacks. Nonetheless, treatment of SCLS remains largely empiric. We report the improvement of one patient with SCLS by an alternative therapeutic approach. After a prophylactic therapy with theophylline and terbutaline was poorly tolerated and failed to decrease the frequency of attacks sufficiently, a high dose of intravenous immunoglobulins (IVIG) was repeatedly infused, successfully reducing the frequency and severity of acute attacks.
Case presentation
In 2004, at the age of 35, the patient was admitted to our hospital due to vomiting, light headedness and signs of hypovolaemic shock. Blood laboratory tests revealed leukocytosis of 31.9 g/l, haemoglobin of 239 g/l and haematocrit of 69%. Immediate intensive care treatment using rehydratation and vasopressor therapy was initiated. She developed diffuse oedema, renal insufficiency, a rapid weight gain of 14 kg and a compartment syndrome of the lower limbs. No source of a possible site of infection was found; cardiac and hepatic insufficiency and nephrotic syndrome as well as endocrine disorders and angiooedema related to a deficiency in C1 esterase inhibitor were excluded. Further laboratory analysis revealed a monoclonal gammopathy IgG κ. The clinical manifestation in relation with paraproteinaemia suggested the diagnosis of SCLS.3 After haemodynamic stabilisation of this first attack, the patient was put on a prophylactic regimen of theophylline (400 mg twice daily) and terbutaline (7.5 mg twice daily).4 Further investigations revealed no evidence of multiple myeloma on bone marrow biopsy, and the paraproteinaemia disappeared after 4 years. Clinically insignificant hypogammaglobulinaemia with a marginally low IgG serum level persisted.
During the next 5 years, the patient suffered from about 20 similar episodes of mild to moderate shock, often requiring hospital re-admission and supportive therapy in the form of intravenous fluids and catecholamines, despite prophylactic therapy containing theophylline and terbutaline. Unfortunately, measurement of plasma theophylline level was rarely performed, while the patient repeatedly complained about sympathomimetic side effects. In January 2009, the prophylactic regimen was terminated because of adverse sympathomimetic drug reactions and monthly episodes of mild to moderate shock. Antihistamines, a gestagen-based oral contraceptive and corticosteroids were prescribed, but proved ineffective as well, with episodes of symptomatic shock now recurring every 1–2 weeks in the fall of 2009.
Treatment
During another acute episode with generalised oedema and haemoconcentration, intravenous immunoglobins (IVIG) (1 g/kg/day) were infused over 2 days based on their efficacy in various studies.5–8 Immunoglobulin G levels measured before were only slightly decreased. Dramatic improvement was noted as of the first infusion, with normalisation of haematocrit without having to administer large-volume intravenous fluid, and thus minimising the risk of pulmonary oedema in the recruitment phase (figure 1). Adverse reactions, including headache, were tolerable.
Figure 1.
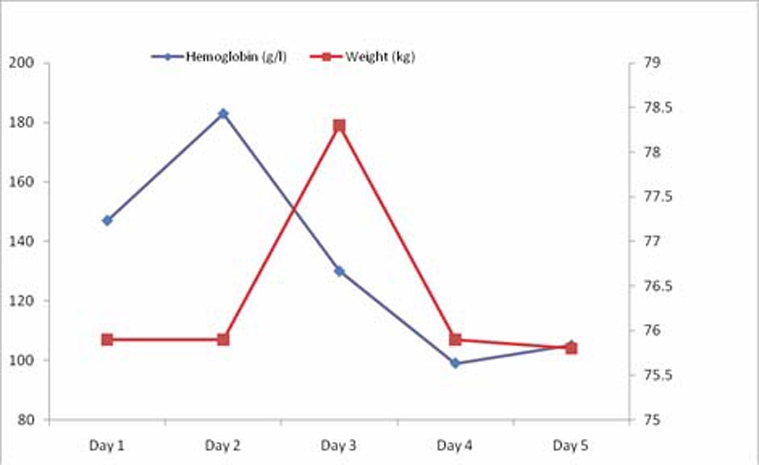
Intravenous immunoglobin administration on days 2 and 3 during acute attack in September 2009. The effect on evolution of weight (kg) and haemoglobin (g/l) during the first 5 days is shown.
Outcome and follow-up
In the absence of any other proven effective prophylactic regimen apart from sympathomimetics, which our patient declined, we continued with monthly IVIG administration (2 g/kg), thus achieving an interval of 4 months without any further attack and dramatic improvement of the quality of life. So far, 10 months of prophylactic therapy resulted in an impressive reduction of intensity and frequency of attacks (figure 2).
Figure 2.
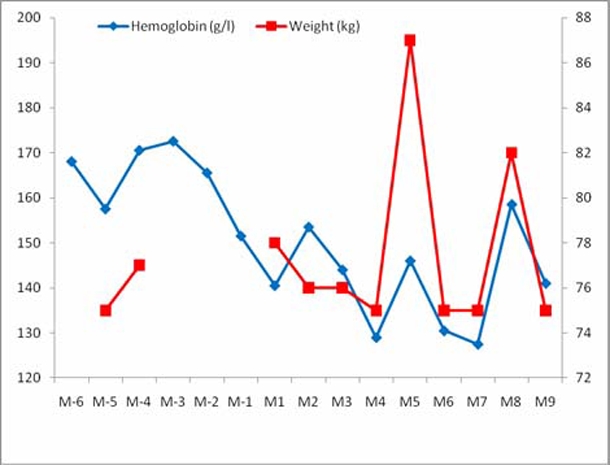
Evolution of weight (kg) and mean haemoglobin (g/l) in the months (M) before (M-6 to M-1) and after (M1 to M9) starting monthly high-dose intravenous immunoglobin administration.
Discussion
Idiopathic SCLS is a rare, but life-threatening, disorder characterised by unexplained episodic capillary hyperpermeability due to a shift of fluid and proteins from the intravascular to the interstitial space. The diagnosis is based on the pathognomonic association of recurrent attacks of hypotension, potentially leading to shock with rapid weight gain and oedema as well as haemoconcentration. Other conditions causing diffuse capillary leak, such as severe infections, allergies, burns or drug and toxin-induced reactions, have to be excluded. The mortality ranges from 30% to 76%.2 9 Seventy per cent of the patients who survived initial attacks were alive a mean of 5 years after diagnosis.9 The pathogenesis of SCLS and the cause of the episodes of capillary leakage remain unclear. A small number of hypotheses have been proposed, but the evidence of any one theory is poor. Contraction of endothelial cells due to apoptosis during attacks of SCLS has been proposed as a mechanism for the increased capillary permeability. A study demonstrated that serum taken from patients with SCLS mediated extensive apoptosis and contraction of endothelial cells in vitro.10 Furthermore, endogenous interleukin-2 (IL) may contribute to the pathogenesis of SCLS. This hypothesis is based on the observation that patients who received high-dose recombinant IL-2 therapy can develop a capillary leak syndrome.11–13 Normal IL-2 plasma levels were measured during one acute attack in our patient. However, only one measurement was carried out, thus a potential participation of IL-2 cannot definitely be excluded. Several studies have found that about 80% of patients with SCLS had a monoclonal gammopathy.2 9 14 15 The role of the paraproteins in the pathogenesis of SCLS has not been determined, but probably they are not directly responsible for vascular endothelial leakage. Zhang et al15 found no detectable cytotoxic effects in healthy endothelial cells, which were exposed in vitro to paraproteins from three patients. However, some reports did show an effect of polychemotherapy for multiple myeloma in SCLS, that of reducing attacks.8 16 Paraproteinaemia in our patient disappeared after 4 years during sympathomimetic therapy, while episodes of capillary leak continued.
So far, no curative treatment is available. A regimen of theophylline (400 mg twice daily) and terbutaline (5 mg five times daily) has been proposed as prophylaxis.2 17 This suggestion is based on the observations that both agents increase intracellular cyclic AMP (cAMP) content and that elevated cAMP inhibits capillary leak.10 18–20 This approach has been used with variable clinical results.2 3 Terbutaline and theophylline can cause sympathomimetic adverse drug reactions, also observed in our patient. Therefore, drug levels of theophylline should be monitored regularly, to achieve serum levels between 10 and 20 mg/l. Breakthrough attacks seem to correlate to subtherapeutic levels of theophylline.2 Unfortunately, in our patient a serum theophylline level was seldom measured. Therefore, recurrent past episodes of SCLS in our patient may also have been associated with subtherapeutic levels of theophylline.
Based on the outcome of three patients in a case report by Lambert et al,6 IVIG were effective against acute-phase SCLS and have been successfully used as prophylaxis in one patient. Vigneau et al7 describe another patient with SCLS and diabetes, benefitting repeatedly from IVIG to reduce the intensity of acute crisis. Early data of a French register, based on a trial of 20 SCLS patients, suggest that IVIG (2 g/kg monthly) may be a promising prophylactic treatment, reducing frequency and severity of the attacks.8 A recent publication adds further evidence to the effectiveness of IVIG as prophylaxis against refractory SCLS.21 Adverse drug reactions may include headache, nausea, hypersensitivity reaction as well as thromboembolic events.
Potential mechanisms of action include an anti-idiotype effect against autoantibodies and induction of Fc-mediated blockade of Fc-receptors on leucocytes.22 By interacting with complement, IVIG prevent it from mediating tissue damage by scavenging its active components and diverting complement attack from cellular targets.23 The prophylactic efficacy might, under special circumstances, be related to the prevention of infections triggering an acute episode of SCLS, as proposed by Lassoued et al5 in a patient with SCLS and concomitant hypogammaglobulinaemia successfully treated with IVIG (0.4 g/kg monthly). Meanwhile, the hypogammaglobulinaemia in our patient was clinically insignificant and cannot have caused repeated attacks by predisposition to recurrent infections.
Several reports demonstrate evidence of an immune-mediated pathogenesis of SCLS, with increased levels of cytokines, including IL-6, IL-10, interferon-γ and tumour necrosis factor-α.24 IVIG possess anticytokine properties and inhibit the synthesis of different ILs, including IL-2,25 and might operate in SCLS through modulation of the immune response.
Based on these promising results and because of intolerance and insufficient effect of β-2 stimulants, we repeatedly administered IVIG (2 g/kg over 48 h) to our patient. We achieved a milder clinical presentation of acute attacks and dramatically reduced the frequency of recurrence.
Learning points.
-
▶
SCLS is a rare disorder, associated with a substantial morbidity and mortality.
-
▶
The diagnosis is based on the pathognomonic findings of diffuse paroxysmal capillary hyperpermeability leading to oedema, hypotension, haemoconcentration and hypoalbuminaemia, frequently associated with monoclonal gammopathy.
-
▶
No evidence-based treatment for SCLS is available, either for acute crisis or prophylaxis. Management of acute episodes is mainly symptomatic. β-2 stimulants are considered the recommended first-line prophylactic measure.
-
▶
Recent research, including our case report, demonstrates IVIG to be a promising alternative treatment strategy for SCLS, functioning possibly through their immunomodulating effects.
-
▶
Further studies are needed to reveal the immunologic characteristics of SCLS and determine the effect of immunomodulatory drugs like intravenous immunoglobulins.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Clarkson B, Thompson D, Horwith M, et al. Cyclical edema and shock due to increased capillary permeability. Am J Med 1960;29:193–216 [DOI] [PubMed] [Google Scholar]
- 2.Tahirkheli NK, Greipp PR. Treatment of the systemic capillary leak syndrome with terbutaline and theophylline. A case series. Ann Intern Med 1999;130:905–9 [DOI] [PubMed] [Google Scholar]
- 3.Amoura Z, Ninet J, Ligout F-C. Le syndrome d′hyperperméabilité capillaire idiopathique. STV 1997;9:179–85 [Google Scholar]
- 4.Bonadies N, Baud P, Peter HJ, et al. A case report of Clarkson’s disease: If you don’t know it, you’ll miss it. Eur J Intern Med 2006;17:363–5 [DOI] [PubMed] [Google Scholar]
- 5.Lassoued K, Clauvel JP, Similowski T, et al. Pulmonary infections associated with systemic capillary leak syndrome attacks in a patient with hypogammaglobulinemia. Intensive Care Med 1998;24:981–3 [DOI] [PubMed] [Google Scholar]
- 6.Lambert M, Launay D, Hachulla E, et al. High-dose intravenous immunoglobulins dramatically reverse systemic capillary leak syndrome. Crit Care Med 2008;36:2184–7 [DOI] [PubMed] [Google Scholar]
- 7.Vigneau C, Haymann JP, Khoury N, et al. An unusual evolution of the systemic capillary leak syndrome. Nephrol Dial Transplant 2002;17:492–4 [DOI] [PubMed] [Google Scholar]
- 8.Gousseff M, Amoura Z. Idiopathic capillary leak syndrome. Rev Med Interne 2009;30:754–68 [DOI] [PubMed] [Google Scholar]
- 9.Dhir V, Arya V, Malav IC, et al. Idiopathic systemic capillary leak syndrome (SCLS): case report and systematic review of cases reported in the last 16 years. Intern Med 2007;46:899–904 [DOI] [PubMed] [Google Scholar]
- 10.Assaly R, Olson D, Hammersley J, et al. Initial evidence of endothelial cell apoptosis as a mechanism of systemic capillary leak syndrome. Chest 2001;120:1301–8 [DOI] [PubMed] [Google Scholar]
- 11.Karatzios C, Gauvin F, Egerszegi EP, et al. Systemic capillary leak syndrome presenting as recurrent shock. Pediatr Crit Care Med 2006;7:377–9 [DOI] [PubMed] [Google Scholar]
- 12.Schwartz RN, Stover L, Dutcher J. Managing toxicities of high-dose interleukin-2. Oncology (Williston Park, NY) 2002;16(11 Suppl 13):11–20 [PubMed] [Google Scholar]
- 13.Rosenberg SA, Lotze MT, Muul LM, et al. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med 1985;313:1485–92 [DOI] [PubMed] [Google Scholar]
- 14.Atkinson JP, Waldmann TA, Stein SF, et al. Systemic capillary leak syndrome and monoclonal IgG gammopathy; studies in a sixth patient and a review of the literature. Medicine (Baltimore) 1977;56:225–39 [DOI] [PubMed] [Google Scholar]
- 15.Zhang W, Ewan PW, Lachmann PJ. The paraproteins in systemic capillary leak syndrome. Clin Exp Immunol 1993;93:424–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Amoura Z, Papo T, Ninet J, et al. Systemic capillary leak syndrome: report on 13 patients with special focus on course and treatment. Am J Med 1997;103:514–19 [DOI] [PubMed] [Google Scholar]
- 17.Droder RM, Kyle RA, Greipp PR. Control of systemic capillary leak syndrome with aminophylline and terbutaline. Am J Med 1992;92:523–6 [DOI] [PubMed] [Google Scholar]
- 18.Casnocha SA, Eskin SG, Hall ER, et al. Permeability of human endothelial monolayers: effect of vasoactive agonists and cAMP. J Appl Physiol 1989;67:1997–2005 [DOI] [PubMed] [Google Scholar]
- 19.Shimura H, Yamaguchi M, Kuzume M, et al. Prevention of reactive oxygen-induced endothelial cell injury by blocking its process. Eur Surg Res 1999;31:390–8 [DOI] [PubMed] [Google Scholar]
- 20.van Nieuw Amerongen GP, van Hinsbergh VW. Targets for pharmacological intervention of endothelial hyperpermeability and barrier function. Vascul Pharmacol 2002;39:257–72 [DOI] [PubMed] [Google Scholar]
- 21.Abgueguen P, Chennebault JM, Pichard E. Immunoglobulins for treatment of systemic capillary leak syndrome. Am J Med 2010;123:e3–4 [DOI] [PubMed] [Google Scholar]
- 22.Fehr J, Kazatchkine MD. Fc receptor blockade. In: Intravenous Immunoglobulins: Clinical Benefits and Future Prospects. Pearl River, NY: Parthenon Publishing Co; 1994:37–8 [Google Scholar]
- 23.Basta M, Fries LF, Frank MM. High doses of intravenous Ig inhibit in vitro uptake of C4 fragments onto sensitized erythrocytes. Blood 1991;77:376–80 [PubMed] [Google Scholar]
- 24.Dowden AM, Rullo OJ, Aziz N, et al. Idiopathic systemic capillary leak syndrome: novel therapy for acute attacks. J Allergy Clin Immunol 2009;124:1111–13 [DOI] [PubMed] [Google Scholar]
- 25.Andersson UG, Björk L, Skansén-Saphir U, et al. Down-regulation of cytokine production and interleukin-2 receptor expression by pooled human IgG. Immunology 1993;79:211–16 [PMC free article] [PubMed] [Google Scholar]


