Abstract
OBJECTIVES
The primary aim was to determine the prevalence of International Classification of Diseases, Ninth Revision (ICD-9), sleep disorders diagnosed by pediatric providers in a large, primary care network. Secondary aims were to examine demographic variables related to these diagnoses and to examine the frequency of prescriptions for medications potentially used to treat sleep disorders.
METHODS
Electronic medical records were reviewed for 154 957 patients (0 –18 years) seen for a well-child visit in 2007. Information collected included ICD-9 sleep diagnoses, demographic variables, comorbid attention-deficit/hyperactivity disorder and autism spectrum disorders, provider type, and medications.
RESULTS
Across all ages, 3.7% of youths had an ICD-9 diagnosis for a sleep disorder. The most-common diagnoses were sleep disorder not otherwise specified, enuresis, and sleep-disordered breathing. Predictors of sleep disorders varied according to developmental age group and included growth parameters, comorbid attention-deficit/hyperactivity disorder or autism spectrum disorder, and provider type. Potential sleep-related medications were prescribed for 6.1% of the sample subjects.
CONCLUSIONS
This study is one of the first to examine comprehensively ICD-9 sleep diagnoses given by primary care providers in a large representative sample of children 0 to 18 years of age. The 3.7% of patients with ICD-9 sleep diagnoses is significantly lower than prevalence rates reported in epidemiological studies, which suggests that primary care providers may be underdiagnosing sleep disorders in children and adolescents. Because sleep disorders are treatable when recognized, the results from this study suggest a significant need for additional education and support for primary care providers in the diagnosis and treatment of pediatric sleep disorders.
Keywords: sleep disorders, children, adolescents, primary care
Sleep disturbances are common in youth,1 including both medically based (eg, obstructive sleep apnea [OSA], restless leg syndrome, periodic limb movement disorder, and narcolepsy) and behaviorally based (eg, behavioral insomnia of childhood) sleep disorders. Common complaints include trouble falling asleep, night waking, snoring, excessive daytime sleepiness, and poor daytime functioning. These complaints often are signs of treatable sleep disorders. However, several studies found that sleep disorders may be underdiagnosed in pediatric practices.2–4 If sleep disorders are not diagnosed and are left untreated, their negative impact on daytime functioning may be significant.5–7
Studies indicated that most parents do not report significant sleep concerns to their pediatricians.2,4,8 One study found that <15% of children with current parent-reported sleep disorder symptoms had chart notes indicating those sleep issues.3 Reasons for this underreporting may include a lack of parent and provider awareness about the serious consequences of insufficient or disrupted sleep and the lack of physician training and comfort with the assessment and diagnosis of pediatric sleep disorders.9
Pediatric sleep disorders fall into multiple categories, with varying prevalence rates. Approximately 1% to 3% of children have OSA, whereas 5% to 27% have primary snoring.10–14 Behavioral insomnia of childhood, which involves bedtime problems and night waking, affects 20% to 30% of infants and toddlers and up to 5% of school-aged children.15–17 Rates of primary or psychophysiological insomnia range between 5% and 20%,11,18,19 with rates being higher among adolescents and youths with developmental disorders. Parasomnia rates range from 5% to 35%, depending on the disorder (eg, sleep terrors versus enuresis) and the child’s age.11,12,20,21 Sleep-related movement disorders (periodic limb movement disorder and restless leg syndrome) are estimated to affect 2% to 8% of youths.12,22–24 Finally, the prevalence rate of narcolepsy among youths is yet to be determined (the prevalence rate among US adults is 1 case per 2000 individuals), although one-half of adult patients report the onset of symptoms before age 20.25
Although some of those prevalence studies used large populations, none examined prevalence rates on the basis of diagnoses given by pediatric primary care practitioners. Therefore, the primary aim of this study was to determine the prevalence of sleep disorders in a large, representative sample of youths seen in pediatric primary care practices. Because sleep disorders may vary according to demographic variables (eg, age, gender, and race), the second aim was to examine the relationship between demographic variables and the diagnosis of sleep disorders. Finally, although no medications have been approved by the Food and Drug Administration for the treatment of sleep disturbances in children, multiple studies have suggested that primary care practitioners frequently prescribe medications to treat sleep difficulties in children.26–28 Therefore, the third aim was to examine the prevalence of medications potentially prescribed to treat sleep difficulties in pediatric primary care practices.
METHODS
Participants and Procedure
An electronic medical record review was conducted for all well-child care visits that occurred between January 1, 2007, and December 31, 2007, in 32 urban or suburban pediatric practices (with 175 physicians and 22 nurse practitioners) affiliated with a large, tertiary care, children’s hospital. The sample included 154 957 children and adolescents (Table 1). For children with >1 well-child care visit, only the most-recent visit was used.
TABLE 1.
Demographic Variables According to Age Group
| Variable | 0–12 mo (N = 22 427) |
12–36 mo (N = 30 208) |
4–5 y (N = 21 661) |
6–12 y (N = 51 810) |
13–18 y (N = 28 851) |
All Ages (N = 154 957 |
|---|---|---|---|---|---|---|
| Patient’s gender, % | ||||||
| Male | 51.4 | 51.9 | 51.0 | 51.9 | 49.1 | 50.5 |
| Female | 48.6 | 48.1 | 49.0 | 48.1 | 50.9 | 49.5 |
| Patient’s age, mean ± SD, y | 0.33 ± 0.30 | 2.14 ± 0.70 | 4.48 ± 0.50 | 8.87 ± 2.02 | 15.06 ± 1.58 | 6.86 ± 5.21 |
| Patient’s race, % | ||||||
| White | 48.7 | 54.4 | 59.8 | 59.7 | 59.0 | 57.0 |
| Black | 28.1 | 27.6 | 24.5 | 26.0 | 27.0 | 26.6 |
| Hispanic | 3.3 | 2.9 | 2.2 | 1.7 | 1.3 | 2.1 |
| Asian | 2.5 | 2.8 | 2.5 | 2.0 | 1.1 | 2.1 |
| Other | 17.3 | 12.4 | 11.1 | 10.7 | 11.7 | 12.2 |
| Median household income, mean ± SD, $ | 50 870 ± 19 466 | 52 364 ± 19 709 | 55 103 ± 20 232a | 55 527 ± 20 596a | 55 495 ± 20 304a | 54 169 ± 20 210 |
Column means were not significantly different (Tukey’s honestly significant difference posthoc test).
Data Extracted
Demographic Characteristics
Participant information was collected through a deidentified, institutional review board-approved query of electronic medical records, including all patients and all patient visits in the network. Demographic variables included age, gender, race, and zip code (used to determine median household incomes on the basis of US Census data). Medical variables included head circumference (for children ≤1 year of age), BMI (for children ≥2 years of age), and provider type (attending physician, fellow/resident, or nurse practitioner).
Sleep Diagnoses
International Classification of Diseases, Ninth Revision (ICD-9), diagnoses and codes were used to identify patients with diagnosed sleep disorders. Both new and existing diagnoses were included (ie, diagnosis might not have been the result of the current well-child visit but was part of the child’s medical record). Sleep diagnoses were grouped into 11 diagnostic categories (see Table 2 for an inclusive list of ICD-9 codes and groupings). Rates of attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorders (ASDs), asthma, and type 1 diabetes mellitus also were collected, for comparison.
TABLE 2.
Rates of Sleep Disorder Diagnoses in Previous and Current Studies
| ICD-9 Diagnostic Codes | Sleep Disorder Grouping | Rates of Diagnosis in Previous Studies, % | Rates in Current Study, % |
|---|---|---|---|
| 327.53 | Bruxism | 5–3511,12,30 | 0.004 |
| 780.55, 307.45, 327.39 | Circadian rhythm disorder | 5–1031 | 0.005 |
| 307.43 | Hypersomnia | Unknown | 0.004 |
| 770.81, 770.82 | Infant apnea | 25–84 (preterm), <0.5–2 (term) | 0.89 (0–12 mo) |
| 307.41, 307.42, 327.02, 327.09, 780.52 | Insomnia | 5–2011,18,19 | 0.05 |
| 347.00, 347.10 | Narcolepsy | Unknown | 0.003 |
| 788.36, 788.30 | Nocturnal enuresis | 15–20 (5 y), 1–2 (≥15 y)20,21 | 1.2 (≥4 y) |
| 307.46 | Parasomnias | 14–3711,32,33 | 0.05 |
| 327.51, 333.94 | Periodic limb movement disorder/restless leg syndrome | 2–822–24 | 0.02 |
| 327.20, 327.21, 327.23, 327.26, 780.51, 780.53, 780.57, 786.03 | SDB | 1–3 for OSA, 5–27 for snoring11–14 | 1.04 (OSA plus snoring) |
| 307.40, 307.47, 780.50, 780.58, 780.59 | SD-NOS | Unknown | 1.4 |
| 314.00, 314.01 | ADHD | 3–836 | 4.2 |
| 299.00, 299.01, 299.80, 299.81, 299.90, 299.91 | ASDs | 0.6737 | 0.9 |
| 430.90, 430.91, 430.92, 100493.901, 100493.902, 100493.903, 100493.904 | Asthma | 13.538 | 14.5 |
| 250.01, 250.03, 250.11, 250.43, 250.91 | Type 1 diabetes mellitus | 0.17–0.2539 | 0.21 |
Medications
Eight classes of medications (including 22 medications) were identified as potential sleep medications on the basis of previous research (see Table 3 for an inclusive list of medication classes and specific medications).26,29 It is important to note that all of these medications might have been prescribed for other reasons.
TABLE 3.
Sleep-Related Medication Classes and Individual Medications Included
| Medication Class | Medications |
|---|---|
| α2-Adrenergic receptor Agonists | Clonidine |
| Guanfacine | |
| Antidepressants | Imipramine hydrochloride |
| Trazadone | |
| Selective serotonin reuptake inhibitors | Citralopram |
| Escitalopram oxalate | |
| Mitrazapine | |
| Antihistamines | Diphenhydramine |
| Hydroxyzine | |
| Promethazine | |
| Antipsychotic agents | Olanzapine |
| Risperidone | |
| Benzodiazepines | Alprazolam |
| Clonazepam | |
| Diazepam | |
| Flurazepam | |
| Lorazepam | |
| Temazepam | |
| Triazolam | |
| Hypnotic agents | Zaleplon |
| Zolpidem | |
| Melatonin | Melatonin |
| Chloral hydrate | Chloral hydrate |
RESULTS
Sample Demographic Characteristics
The overall sample included 154 957 children, with a mean age of 6.86 years (SD: 5.21 years; range: 0 –18 years). For data analyses, the sample was divided into 5 developmentally based subgroups according to age, that is, infants (0 –12.0 months), toddlers (12.1– 47 months), preschool-aged children (4 –5 years), school-aged children (6 –12 years), and adolescents (13–18 years). Detailed demographic information for all participants and all age groups is provided in Table 1.
Frequency of Sleep Disorder Diagnoses
Overall, 3.7% of children (n = 5750) were given an ICD-9 diagnosis of a sleep disorder (Table 2). Sleep disorder not otherwise specified (SD-NOS) was the most-common sleep disorder diagnosis (n = 2193 [1.4%]), followed by nocturnal enuresis (n = 1915 [1.2%]), sleep-disordered breathing (SDB) (n = 1615 [1.0%]), infant apnea (n = 299 [0.2%]), insomnia (n = 76 [0.05%]), restless leg syndrome/periodic limb movement disorder (n = 30 [0.02%]), circadian rhythm disorder (n = 7 [0.005%]), bruxism (n = 6 [0.004%]), and narcolepsy (n = 4 [0.003%]). In comparison, diagnostic rates for ADHD (n = 6440 [4.2%]), ASDs (n = 1380 [0.9%]), asthma (n = 22 547 [14.5%]), and type 1 diabetes mellitus (n = 324 [0.21%]) were similar to those in previous studies.
The χ2 analyses revealed significant differences in sleep diagnoses according to age group, although the effect size was small (; P < .0001; ϕ = .05). Posthoc analyses of standardized residuals suggested that preschool-aged (4.3%; standardized residual: 4.2) and school-aged (4.7%; standardized residual: 11.1) children were more likely to receive a sleep diagnosis.
The most-common diagnosis within the infant age group was SD-NOS (n = 283 [1.3%]), followed by infant apnea (n = 200 [0.9%]) and SDB (n = 113 [0.5%]). SD-NOS also was the most-frequently diagnosed sleep disorder among toddlers (n = 720 [2.4%]), followed by SDB (n = 417 [1.4%]). Preschool-aged children were most likely to receive a diagnosis of SDB (n = 355 [1.6%]), SD-NOS (n = 346 [1.6%]), or nocturnal enuresis (n = 281 [1.3%]). Similarly, school-aged children most-commonly received a diagnosis of nocturnal enuresis (n = 1349 [2.6%]), SD-NOS (n = 598 [1.2%]), or SDB (n = 592 [1.1%]). Adolescents were most likely to receive a diagnosis of nocturnal enuresis (n = 265 [0.9%]), SD-NOS (n = 246 [0.9%]), or SDB (n = 138 [0.5%]).
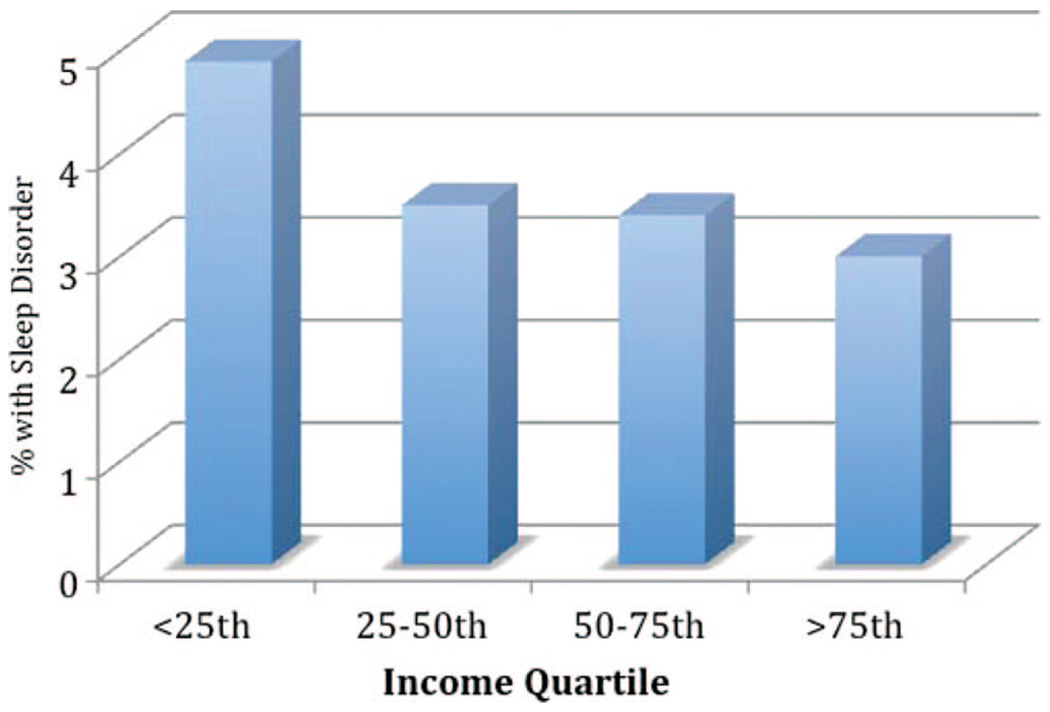
Diagnosed sleep disorders were more common among children from low-income areas (χ2 = 219; P < .0001; Cramer’s V = .038) (Fig 1). Posthoc analyses indicated that children from areas with incomes of <25th percentile were more likely to receive a diagnosis (4.9%; standardized residual: 12.0) than were children from areas with higher income levels (25th to 50th percentile, rate: 3.5%; standardized residual: −1.9; 50th to 75th percentile, rate: 3.4%; standardized residual: −3.6; >75th percentile, rate: 3.0%; standardized residual: −7.1).
FIGURE 1.
Sleep disorder prevalence according to income quartile.
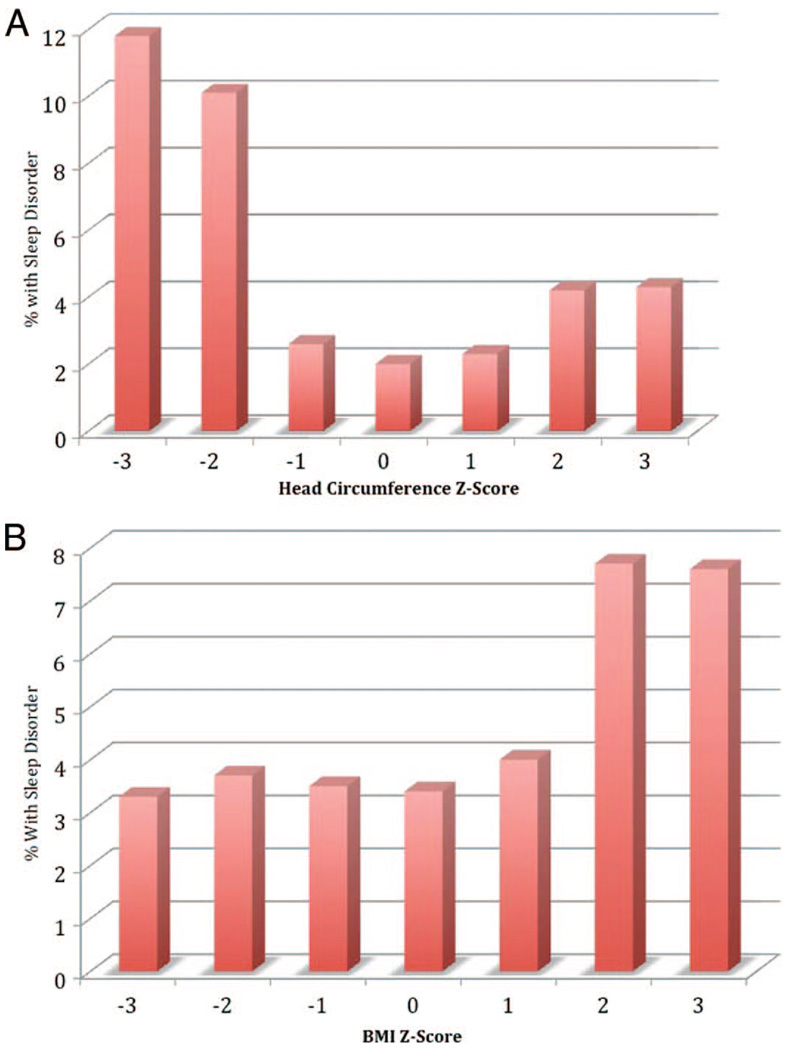
Growth parameters also were closely related to sleep disorder diagnoses (χ2 = 293.2; P < .0001; Cramer’s V = .115) (Fig 2). Among children <1 year of age, small head circumference (≤2 SDs below the mean) was related to increases in diagnosis. Overall, 11.7% (standardized residual: 16.3) of children with small head circumference received a sleep disorder diagnosis, compared with 4.2% (standardized residual: 2.4) of children with large head circumference (≥2 SDs above the mean) and 2.2% (standardized residual: −3.6) of children with normal head circumference. Among children >1 year of age, sleep diagnoses were more common (7.7%; standardized residual: 17.9) for children with higher BMIs (≥2 SDs above the mean) (χ2 = 360.5; P < .0001; Cramer’s V = .054), compared with children with normal (3.6%; standardized residual: −4.9) and low (3.4%; standardized residual: −1.1) BMIs. BMI was not associated with any individual diagnosis (eg, OSA); high BMI values were distributed across the different diagnoses.
FIGURE 2.
Sleep disorder prevalence according to head circumference (0 –1 year of age) (A) and BMI (2–18 years of age) (B).
Logistic Regression Analyses
Models
Logistic regression analyses were performed within each age group to analyze risk factors associated with receiving a sleep disorder diagnosis. Independent variables entered in the initial models included gender, ethnicity (white, black, Hispanic, Asian, or other), income quartile, BMI (children >2 years of age), head circumference (infants only), provider type, and comorbid developmental disorders (ADHD and ASDs). Nonsignificant variables (P≥ .05) were trimmed from the final models (Table 4).
TABLE 4.
Final Logistic Regression Models for Variables That Predicted Sleep Disorder Diagnoses, According to Age Group
| Predictor Variable | B, Estimate ± SE | Odds Ratio (95% Confidence Interval) |
|---|---|---|
| Infants | ||
| Head circumference | ||
| ≤2 SDs below mean | 2.01 ± 0.01 | 7.50 (5.94–9.54)a |
| ≥2 SDs above mean | 0.46 ± 0.22 | 1.59 (1.03–2.44)b |
| Ethnicity | ||
| Black | −0.55 ± 0.11 | 0.58 (0.46–0.72)a |
| Other | −0.42 ± 0.13 | 0.66 (0.51–0.84)a |
| Physician provider | 0.59 ± 0.20 | 1.80 (1.21–2.65)a |
| Toddlers | ||
| Male | 0.23 ± 0.06 | 1.26 (1.12–1.42)a |
| Other ethnicity | −0.42 ± 0.11 | 0.66 (0.53–0.81)a |
| ASD | 0.70 ± 0.29 | 2.01 (1.14–3.56)b |
| Preschool-aged children | ||
| Male | 0.24 ± 0.07 | 1.27 (1.11–1.45)a |
| BMI ≥2 SDs above mean | 0.42 ± 0.12 | 1.52 (1.22–1.91)a |
| Other ethnicity | −0.34 ± 0.13 | 0.71 (0.56–0.92)a |
| Income percentile | ||
| 25th–50th | −0.40 ± 0.11 | 0.67 (0.54–0.84)a |
| 50th–75th | −0.46 ± 0.11 | 0.63 (0.50–0.79)a |
| >75th | −0.37 ± 0.12 | 0.69 (0.55–0.88)a |
| Provider | ||
| Physician | 0.37 ± 0.13 | 1.44 (1.11–1.87)a |
| Fellow/resident | 0.51 ± 0.19 | 1.66 (1.16–2.39)a |
| School-aged children | ||
| Male | 0.36 ± 0.04 | 1.44 (1.32–1.57)a |
| BMI ≥2 SDs above mean | 0.73 ± 0.06 | 2.07 (1.84–2.32)a |
| Ethnicity | ||
| Black | 0.20 ± 0.06 | 1.22 (1.08–1.37)a |
| Hispanic | 0.29 ± 0.14 | 1.33 (1.01–1.77)b |
| Other | −0.32 ± 0.09 | 0.72 (0.61–0.85)a |
| Income percentile | ||
| 25th–50th | 0.18 ± 007 | 1.19 (1.05–1.36)a |
| >75th | −0.30 ± 0.07 | 0.74 (0.65–0.85)a |
| Provider type | ||
| Physician | 0.22 ± 0.08 | 1.25 (1.08–1.44)a |
| Fellow/resident | 0.41 ± 0.11 | 1.50 (1.22–1.86)a |
| Other diagnoses | ||
| ADHD | 0.70 ± 0.06 | 2.00 (1.77–2.27)a |
| ASD | 0.33 ± 0.14 | 1.39 (1.05–1.84)a |
| Adolescents | ||
| Male | 0.24 ± 0.08 | 1.27 (1.08–1.49)a |
| BMI ≥2 SDs above mean | 0.98 ± 0.10 | 2.67 (2.19–1.73)a |
| Ethnicity | ||
| Black | 0.48 ± 0.11 | 1.61 (1.29–2.02)a |
| Other | −0.53 ± 0.18 | 0.58 (0.41–0.84)a |
| Income percentile | ||
| 25th–50th | −0.26 ± 0.13 | 0.77 (0.60–0.99)b |
| 50th–75th | −0.32 ± 0.13 | 0.72 (0.56–0.94)b |
| >75th | −0.40 ± 0.15 | 0.67 (0.50–0.90)a |
| Physician provider | 0.32 ± 0.15 | 1.37 (1.02–1.84) b |
| Other diagnoses | ||
| ADHD | 0.95 ± 0.11 | 2.57 (2.10–3.16)a |
| ASD | 0.56 ± 0.28 | 1.76 (1.02–3.03)b |
Odds ratios are from trimmed logistic regression analyses in which all nonsignificant variables were eliminated from the final models. Only significant results are presented. Odds ratios of >1 represent increased odds of a sleep disorder diagnosis. Odds ratios of <1 represent decreased odds of a sleep disorder diagnosis. B indicates standardized β. Comparison groups for odds ratios were as follows: white, female, nurse provider, income of <25th percentile, and BMI and head circumference within 2 SDs of the mean.
P < .01.
P < .05.
Infants
Logistic regression analysis revealed higher rates of sleep disorders among infants with small or large head circumference. Infants cared for by a physician were 1.8 times more likely to receive a diagnosis than were those cared for by a nurse practitioner. Black and other infants were less likely to receive a sleep disorder diagnosis than were white infants.
Toddlers
Logistic regression analysis revealed higher rates of sleep disorders among boys and toddlers with ASDs. Toddlers of other ethnicities were less likely than white toddlers to receive a diagnosis.
Preschool-aged Children
Results of logistic regression analysis suggested that boys and children with high BMIs were more likely to receive a diagnosis. Preschool-aged children treated by an attending physician or a fellow/resident were more likely to receive a diagnosis than were those treated by a nurse practitioner. Preschool-aged children of other ethnicities were less likely than white preschool-aged children to receive a diagnosis.
School-aged Children
Logistic regression analysis revealed higher rates of diagnoses for boys, children with high BMIs, black or Hispanic children, children with incomes between the 25th and 50th percentiles, children who were treated by an attending physician or fellow/resident, and children with ADHD or ASDs. In contrast, school-aged children of other ethnicities and those with incomes of >75th percentile were less likely to receive a diagnosis.
Adolescents
Logistic regression analyses revealed higher rates of diagnosed sleep disorders for boys, adolescents with high BMIs, black adolescents, adolescents who were treated by an attending physician, and adolescents with ADHD or ASDs. Adolescents of other ethnicities and those with incomes of >25th percentile were less likely to receive a diagnosis.
Frequency of Prescribed Sleep-Related Medications
Overall, potentially sleep-related medications were prescribed for 6.1% of children (n = 9441). Antihistamines were prescribed most commonly (n = 8367 [88.6%]), followed by antipsychotic agents (n = 465 [4.9%]), α-adrenergic receptor agonists (n = 399 [4.2%]), and selective serotonin reuptake inhibitors (n = 159 [0.1%]). The χ2 analyses revealed that boys (n = 4965 [6.3%]) were significantly more likely than girls (n = 4476 [5.8%]) to receive sleep-related medications, although the effect size was small (χ2 = 151.3; P < .0001; ϕ =−.031).
The χ2 analyses also revealed significant differences in sleep-related medications according to age group (χ2 = 847.2; P < .0001; Cramer’s V = .074). Posthoc analyses of standardized residuals indicated that toddlers (7.7%; standardized residual: 11.2), preschool-aged children (7.5%; standardized residual: 8.5), and school-aged children (6.7%; standardized residual: 6.0) were more likely to receive sleep-related medications than were infants (2.3%; standardized residual: −22.7) and adolescents (5.1%; standardized residual: −6.8). Black and Hispanic children were more likely to receive sleep-related medications (χ2 = 5347; P < .0001; Cramer’s V = .186), with medications being prescribed for 13.3% of black children (n = 5492) and 7.9% of Hispanic children (n = 263), compared with only 3.1% of white children (n = 2753), 6.9% of Asian children (n = 223), and 3.8% of other children (n = 710).
DISCUSSION
This study is one of the first to examine comprehensively the prevalence of diagnosed sleep disorders, on the basis of ICD-9 codes, in a large, pediatric, primary care network. Surprisingly, only 3.7% of pediatric patients were given a sleep disorder diagnosis, which is significantly lower than previous reports of sleep disorders in youth. Preschool-aged and school-aged children were more likely to receive a sleep disorder diagnosis than were patients in other age groups, with household income (determined on the basis of Census data), growth parameters (head circumference and BMI), and comorbid developmental disorders (ASDs and ADHD) also being related to whether a patient received a sleep disorder diagnosis.
The low overall prevalence rates found in this study may be attributable to a combination of factors, including primary care providers not asking about sleep and parents not reporting significant sleep problems. The standard review of systems covered in well-child visits often does not include an assessment of sleep. Even if providers inquire about sleep, however, studies have shown a significant lack of education regarding sleep medicine for physicians (with even less education regarding pediatric sleep medicine).9,34–37 Some providers may be reluctant to ask much about sleep, given their lack of confidence in their ability to manage identified sleep issues.9
Overall, the sleep disorder diagnosed most commonly by the health care providers was SD-NOS. It is not clear what symptoms or concerns led to this diagnosis, and they likely varied widely among practitioners, but it has been postulated that this diagnosis includes more-benign sleep disturbances, such as sleep fragmentation and difficulties falling asleep or staying asleep. In prevalence surveys based on parental reports, the sleep problems identified most commonly included bedtime resistance and night waking,4,16,38 which may be consistent with the use of this diagnostic code by health care providers.
The other 2 sleep disorders diagnosed most commonly were SDB and enuresis. The relatively high rate of SDB diagnoses (compared with other diagnoses) likely is a result of the American Academy of Pediatrics recommendation that all children should be screened for snoring.39 However, the overall rate of combined SDB diagnoses we found in this study (~1%) is still below the overall prevalence rates of 1% to 3% for OSA and 5% to 27% for snoring.11–14 The relatively high rate of enuresis is potentially attributable to the significant impact on family and social functioning. However, consistent with the overall findings, the diagnosis of enuresis was still well below known prevalence rates.
One potential explanation for the low prevalence rates for all sleep disorders is that all medical and psychiatric diagnoses are underdocumented, but this does not seem to be the case. We also assessed the prevalence rates of diagnosed ADHD, ASDs, asthma, and type 1 diabetes, comparing the rates for our sample with national rates. ADHD was diagnosed for 4.2% of the children in our sample, which is comparable to rates in epidemiological studies (3%–8%).40 Interestingly, children in the present study were more likely to have documented ASDs (0.9%), compared with national prevalence rates (0.67%).41 For asthma and type 1 diabetes, we found prevalence rates in our sample (asthma, 14.5%; type 1 diabetes, 0.21%) similar to national prevalence rates (asthma, 13.5%; type 1 diabetes, 0.17%–0.25%).42,43 Therefore, it is unlikely that the low prevalence rates of diagnosed sleep disorders that we saw resulted from a general lack of documentation; rather, the findings were specific to sleep disorders.
An interesting finding in this study was the relationship between income levels and diagnosis rates. Overall, children from lower-income families were more likely to be diagnosed as having a sleep disorder, starting at preschool age. This relationship may be compounded by race and ethnicity. Previous studies found that black children were at increased risk for SDB and sleep deprivation.14 Therefore, it is possible that health care providers are more likely to consider sleep disturbances in lower-income and/or ethnic minority families, with sleep issues being missed in other families. Finally, it is possible that the types of sleep problems experienced by children differ across the social strata, with diagnosable sleep disorders such as SDB being experienced more in lower-income families and behaviorally based sleep problems (that may not result in a formal diagnosis) being of greater concern in upper-income families. As we begin to evaluate sleep complaints further, as recorded in the medical records, we should be able to address these issues.
A second interesting risk factor that increased the rates of diagnosed sleep disorders involved growth parameters. In infancy, head circumference was associated with increased risk for a sleep disorder diagnosis. Prematurity, for which data were not available, is likely associated with microcephaly, whereas both microcephaly and macrocephaly may be related to neurologic and developmental concerns,44,45 all of which may result in increased risks for apnea of infancy and other sleep disturbances. For older children, BMI was a risk factor for all sleep disorder diagnoses. Clearly, SDB is related to the increasing rates of obesity, especially in adolescents. Studies indicated that obesity is associated not only with SDB but also with short sleep duration,46–48 which might have contributed to the increased rate of diagnosis of SD-NOS.
Although there are no Food and Drug Administration-approved medications for sleep in youth, the rates of medications potentially used to treat sleep problems are similar to reports of sleep medications used by pediatricians and pediatric psychiatrists and during pediatric hospitalizations.26,29,49–51 It is important to note that, although the proxy method used in this study was based on the paradigm used in previous studies, the current study results may overestimate the use of medications recommended for sleep problems.27,29
This study has several strengths, including the use of a large, representative population of youths and the examination of demographic, growth, and medical factors related to the diagnosis of pediatric sleep disorders. However, there are several limitations that should be noted. First, the use of diagnostic codes precluded identification of “sleep problems” such as bedtime problems/night waking for young children or difficulty waking up for adolescents. Although sleep problems may explain why SD-NOS was the most-common diagnosis, the rates are still far below those in previous reports. Second, sleep problems might have been discussed during the well-child visit but deemed not significant enough to warrant a diagnosis. Third, although we used an approach to the identification of potential sleep medications similar to that used in previous studies, this proxy method may overestimate the use of medications prescribed for sleep disorders. However, the rates also may be underestimates; for example, use of diphenhydramine, which can be obtained without a prescription and is the most-commonly reported medication recommended for the treatment of pediatric insomnia, would not be captured in these records.
Identified future directions include an additional analysis of sleep complaints, which are provided as text within the electronic medical records. This should help elucidate whether sleep problems are being discussed and noted even if diagnoses are not being given. A review of treatment recommendations from text in the electronic medical records would provide additional information on the care of sleep disorders in pediatric practices. Finally, additional research needs to be conducted within the pediatric community regarding reasons for the low rates of documented sleep-related disorders.
The results of this population-based study highlight the need for increased awareness of pediatric sleep disorders, including additional education for health care providers regarding the diagnosis and treatment of pediatric sleep disorders. Education about the importance of sleep is needed for parents and youths of all ages. Because youths spend more than one-third of their lives sleeping, more information about this part of a child’s day needs to become a standard dialogue topic for primary care well-child visits, which would likely result in sleep disorders becoming more widely recognized and treated.
ACKNOWLEDGMENTS
This study was supported in part by National Institutes of Health grant K23 MH077662.
We thank the network of primary care physicians for their contribution to clinical research through the Pediatric Research Consortium at the Children’s Hospital of Philadelphia. We also thank Hannah Benson for her assistance with this project.
ABBREVIATIONS
- ADHD
attention-deficit/hyperactivity disorder
- ASD
autism spectrum disorder
- ICD-9
International Classification of Diseases, Ninth Revision
- OSA
obstructive sleep apnea
- SDB
sleep-disordered breathing
- SD-NOS
sleep disorder not otherwise specified
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
Reprints Information about ordering reprints can be found online: http://www.pediatrics.org/misc/reprints.shtml
REFERENCES
- 1.Owens JA. Epidemiology of sleep disorders during childhood. In: Sheldon SH, Ferber R, Kryger MH, editors. Principles and Practices of Pediatric Sleep Medicine. Philadelphia, PA: Elsevier Saunders; 2005. pp. 27–33. [Google Scholar]
- 2.Blunden S, Lushington K, Lorenzen B, Ooi T, Fung F, Kennedy D. Are sleep problems under-recognised in general practice? Arch Dis Child. 2004;89(8):708–712. doi: 10.1136/adc.2003.027011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chervin RD, Archbold KH, Panahi P, Pituch KJ. Sleep problems seldom addressed at two general pediatric clinics. Pediatrics. 2001;107(6):1375–1380. doi: 10.1542/peds.107.6.1375. [DOI] [PubMed] [Google Scholar]
- 4.Smedje H, Broman JE, Hetta J. Parents’ reports of disturbed sleep in 5–7-year-old Swedish children. Acta Paediatr. 1999;88(8):858–865. doi: 10.1080/08035259950168793. [DOI] [PubMed] [Google Scholar]
- 5.Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: clinical implications. Sleep Med Rev. 2002;6(4):287–306. doi: 10.1053/smrv.2001.0192. [DOI] [PubMed] [Google Scholar]
- 6.Gregory AM, Caspi A, Moffitt TE, Poulton R. Sleep problems in childhood predict neuropsychological functioning in adolescence. Pediatrics. 2009;123(4):1171–1176. doi: 10.1542/peds.2008-0825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quach J, Hiscock H, Canterford L, Wake M. Outcomes of child sleep problems over the school-transition period: Australian population longitudinal study. Pediatrics. 2009;123(5):1287–1292. doi: 10.1542/peds.2008-1860. [DOI] [PubMed] [Google Scholar]
- 8.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107(4) doi: 10.1542/peds.107.4.e60. Available at: www.pediatrics.org/cgi/content/full/107/4/e60. [DOI] [PubMed] [Google Scholar]
- 9.Owens JA. The practice of pediatric sleep medicine: results of a community survey. Pediatrics. 2001;108(3) doi: 10.1542/peds.108.3.e51. Available at: www.pediatrics.org/cgi/content/full/108/3/e51. [DOI] [PubMed] [Google Scholar]
- 10.Ali NJ, Pitson D, Stradling JR. Sleep disordered breathing: effects of adenotonsillectomy on behavior and psychological function. Eur J Pediatr. 1996;155(1):56–62. doi: 10.1007/BF02115629. [DOI] [PubMed] [Google Scholar]
- 11.Archbold KH, Pituch KJ, Panahi P, Chervin RD. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr. 2002;140(1):97–102. doi: 10.1067/mpd.2002.119990. [DOI] [PubMed] [Google Scholar]
- 12.Liu X, Liu L, Owens JA, Kaplan DL. Sleep patterns and sleep problems among school-children in the United States and China. Pediatrics. 2005;115(1) suppl:241–249. doi: 10.1542/peds.2004-0815F. [DOI] [PubMed] [Google Scholar]
- 13.Gregory AM, Rijsdijk FV, Eley TC. A twin-study of sleep difficulties in school-aged children. Child Dev. 2006;77(6):1668–1679. doi: 10.1111/j.1467-8624.2006.00966.x. [DOI] [PubMed] [Google Scholar]
- 14.Redline S, Tishler PV, Schluchter M, Aylor J, Clark K, Graham G. Risk factors for sleep-disordered breathing in children: associations with obesity, race, and respiratory problems. Am J Respir Crit Care Med. 1999;159(5):1527–1532. doi: 10.1164/ajrccm.159.5.9809079. [DOI] [PubMed] [Google Scholar]
- 15.Mindell JA, Kuhn BR, Lewin DS, Meltzer LJ, Sadeh A, Owens JA. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29(10):1263–1276. [PubMed] [Google Scholar]
- 16.Blader JC, Koplewicz HS, Abikoff H, Foley C. Sleep problems of elementary school children: a community survey. Arch Pediatr Adolesc Med. 1997;151(5):473–480. doi: 10.1001/archpedi.1997.02170420043007. [DOI] [PubMed] [Google Scholar]
- 17.Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr. 2000;21(1):27–36. doi: 10.1097/00004703-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 18.Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006;117(2) doi: 10.1542/peds.2004-2629. Available at: www.pediatrics.org/cgi/content/full/117/2/e247. [DOI] [PubMed] [Google Scholar]
- 19.Roberts RE, Roberts CR, Duong HT. Chronic insomnia and its negative consequences for health and functioning of adolescents: a 12-month prospective study. J Adolesc Health. 2008;42(3):294–302. doi: 10.1016/j.jadohealth.2007.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Byrd RS, Weitzman M, Lanphear NE, Auinger P. Bed-wetting in US children: epidemiology and related behavior problems. Pediatrics. 1996;98(3):414–419. [PubMed] [Google Scholar]
- 21.Baskin LS, Kogan BA. Handbook of Pediatric Urology. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 22.Bokkala S, Napalinga K, Pinninti N, et al. Correlates of periodic limb movements of sleep in the pediatric population. Pediatr Neurol. 2008;39(1):33–39. doi: 10.1016/j.pediatrneurol.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 23.Picchietti D, Allen RP, Walters AS, Davidson JE, Myers A, Ferini-Strambi L. Restless legs syndrome: prevalence and impact in children and adolescents: the Peds REST study. Pediatrics. 2007;120(2):253–266. doi: 10.1542/peds.2006-2767. [DOI] [PubMed] [Google Scholar]
- 24.Picchietti DL, Underwood DJ, Farris WA, et al. Further studies on periodic limb movement disorder and restless legs syndrome in children with attention-deficit hyperactivity disorder. Mov Disord. 1999;14(6):1000–1007. doi: 10.1002/1531-8257(199911)14:6<1000::aid-mds1014>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 25.Ohayon MM, Ferini-Strambi L, Plazzi G, Smirne S, Castronovo V. How age influences the expression of narcolepsy. J Psychosom Res. 2005;59(6):399–405. doi: 10.1016/j.jpsychores.2005.06.065. [DOI] [PubMed] [Google Scholar]
- 26.Owens JA, Rosen CL, Mindell JA. Medication use in the treatment of pediatric insomnia: results of a survey of community-based pediatricians. Pediatrics. 2003;111(5) doi: 10.1542/peds.111.5.e628. Available at: www.pediatrics.org/cgi/content/full/111/5/e628. [DOI] [PubMed] [Google Scholar]
- 27.Rappley MD, Luo Z, Brady J, Gardiner JC. Variation in the use of sleep medications for children. J Dev Behav Pediatr. 2003;24(5):394. [Google Scholar]
- 28.Stojanovski SD, Rasu RS, Balkrishnan R, Nahata MC. Trends in medication prescribing for pediatric sleep difficulties in US outpatient settings. Sleep. 2007;30(8):1013–1017. doi: 10.1093/sleep/30.8.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Meltzer LJ, Mindell JA, Owens JA, Byars KC. The use of sleep medications in hospitalized pediatric patients. Pediatrics. 2007;119(6):1047–1055. doi: 10.1542/peds.2006-2773. [DOI] [PubMed] [Google Scholar]
- 30.Sheldon SH, Glaze D. Sleep in neurologic disorders. In: Sheldon SH, Ferber R, Kryger MH, editors. Principles and Practice of Pediatric Sleep Medicine. Philadelphia, PA: Elsevier Saunders; 2005. pp. 269–292. [Google Scholar]
- 31.Herman JH. Circadian rhythm disorders: Diagnosis and treatment. In: Sheldon SH, Ferber R, Kryger MH, editors. Principles and Practice of Pediatric Sleep Medicine. Philadelphia, PA: Elsevier Saunders; 2005. pp. 101–111. [Google Scholar]
- 32.Nguyen BH, Perusse D, Paquet J, et al. Sleep terrors in children: A prospective study of twins. Pediatrics. 2008;122(6):e1164–e1167. doi: 10.1542/peds.2008-1303. [DOI] [PubMed] [Google Scholar]
- 33.Laberge L, Tremble RE, Vitaro F, Montplaisir J. Development of parasomnias from childhood to early adolescence. Pediatrics. 2000;106(1):67–74. doi: 10.1542/peds.106.1.67. [DOI] [PubMed] [Google Scholar]
- 34.Mindell JA, Moline ML, Zendell SM, Brown LW, Fry JM. Pediatricians and sleep disorders: training and practice. Pediatrics. 1994;94(2):194–200. [PubMed] [Google Scholar]
- 35.Rosen R, Mahowald M, Chesson A, et al. The Taskforce 2000 survey on medical education in sleep and sleep disorders. Sleep. 1998;21(3):235–238. doi: 10.1093/sleep/21.3.235. [DOI] [PubMed] [Google Scholar]
- 36.Rosen RC, Rosekind M, Rosevear C, Cole WE, Dement WC. Physician education in sleep and sleep disorders: a national survey of US medical schools. Sleep. 1993;16(3):249–254. doi: 10.1093/sleep/16.3.249. [DOI] [PubMed] [Google Scholar]
- 37.Stores G, Crawford C. Medical student education in sleep and its disorders. J R Coll Physicians Lond. 1998;32(2):149–153. [PMC free article] [PubMed] [Google Scholar]
- 38.National Sleep Foundation. Sleep in America poll 2004: children and sleep. [Accessed May 11, 2007]; Available at: www.sleepfoundation.org/article/sleepamerica- polls/2004-children-and-sleep.
- 39.American Academy of Pediatrics, Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome. Clinical practice guideline: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109(4):704–712. doi: 10.1542/peds.109.4.704. [DOI] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Attention-deficit/hyperactivity disorder: data and statistics. [Accessed June 12, 2009]; Available at: www.cdc.gov/ncbddd/adhd/data.html.
- 41.Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders: Autism and Developmental Disabilities Monitoring Network, 14 sites, United States, 2002. MMWR Surveill Summ. 2007;56(SS-1):12–28. [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. Lifetime asthma prevalence percents by age, United States: National Health Interview Survey. [Accessed June 12, 2009];2006 Available at: www.cdc.gov/asthma/nhis/06/table2-1.htm.
- 43.Centers for Disease Control and Prevention. National diabetes fact sheet, United States. [Accessed June 12, 2009];2005 Available at: www.cdc.gov/diabetes/pubs/pdf/ndfs_2005.pdf.
- 44.Fattal-Valevski A, Toledano-Alhadef H, Leitner Y, Geva R, Eshel R, Harel S. Growth patterns in children with intrauterine growth retardation and their correlation to neurocognitive development. J Child Neurol. 2009;24(7):846–851. doi: 10.1177/0883073808331082. [DOI] [PubMed] [Google Scholar]
- 45.Dementieva YA, Vance DD, Donnelly SL, et al. Accelerated head growth in early development of individuals with autism. Pediatr Neurol. 2005;32(2):102–108. doi: 10.1016/j.pediatrneurol.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 46.Bayer O, Rosario AS, Wabitsch M, von Kries R. Sleep duration and obesity in children: is the association dependent on age and choice of the outcome parameter? Sleep. 2009;32(9):1183–1189. doi: 10.1093/sleep/32.9.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Verhulst SL, Van Gaal L, De Backer W, Desager K. The prevalence, anatomical correlates and treatment of sleep-disordered breathing in obese children and adolescents. Sleep Med Rev. 2008;12(5):339–346. doi: 10.1016/j.smrv.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 49.Owens JA, Rosen CL, Mindell JA, Kirchner LH. Use of pharmacotherapy for insomnia in child psychiatry practice: A national survey. Sleep Medicine. doi: 10.1016/j.sleep.2009.11.015. In press. [DOI] [PubMed] [Google Scholar]
- 50.Owens JA, Babcock D, Blumer J, et al. The use of pharmacotherapy in the treatment of pediatric insomnia in primary care: rational approaches: a consensus meeting summary. J Clin Sleep Med. 2005;1(1):49–59. [PubMed] [Google Scholar]
- 51.Mindell JA, Emslie G, Blumer J, et al. Pharmacologic management of insomnia in children and adolescents: consensus statement. Pediatrics. 2006;117(6) doi: 10.1542/peds.2005-1693. Available at: www.pediatrics.org/cgi/content/full/117/6/e1223. [DOI] [PubMed] [Google Scholar]