Abstract
Background
Differences in the prevalence of cardiovascular disease and associated risk factors have been noted across ethnic groups both within and between countries. The Canadian population is becoming increasingly diverse because of immigration. Understanding ethnic differences in cardiovascular risk factors is critically important in planning appropriate prevention strategies for the country’s rapidly changing population. We sought to examine the prevalence of cardiovascular risk factors in various Canadian ethnic groups.
Methods
We analyzed 3 cross-sectional cycles (for 2000, 2003 and 2005) of the Canadian Community Health Survey of people aged 12 years and older. The surveys were conducted by means of self-reported questionnaires. We used stratified analysis to evaluate the relation between risk factors and ethnicity. The effect of participants’ ethnicity on the prevalence of risk factors was estimated by means of logistic regression, with adjustment for differences in age, sex, marital status, education, household income, language spoken, immigration status, residency type (urban or rural), household size, region (province or territory) and chronic diseases (heart disease, stroke, cancer, bronchitis, chronic obstructive pulmonary disease, bowel disease, arthritis, epilepsy, ulcers, thyroid disease and diabetes mellitus).
Results
We included 371 154 individuals in the analysis. Compared with white people, people from visible minorities (i.e., neither white nor Aboriginal) had a lower prevalence of diabetes mellitus (4.5% v. 4.0%), hypertension (14.7% v. 10.8%), smoking (20.4% v. 9.7%) and obesity (defined as body mass index ≥ 30; 14.8% v. 9.7%) but a higher prevalence of physical inactivity (50.3% v. 58.1%). More specifically, after adjustment for sociodemographic characteristics, people from most visible minorities, in comparison with the white population, were less likely to smoke; were more likely to be physically inactive, with the exception of people of Korean, Japanese and Latin ethnicity; and were less likely to be obese, with the exception of people of black, Latin, Arab or West Asian ethnicity. However, relative to white people, hypertension was more prevalent among those of Filipino or South East Asian background (odds ratio [OR] 1.54, 95% confidence interval [CI] 1.23–1.93) and those of black ancestry (OR 1.69, 95% CI 1.43–2.00).
Interpretation
Cardiovascular risk factors vary dramatically by ethnic group. Health professionals should increase their promotion of physical activity among visible minorities and should prioritize the detection and control of diabetes and hypertension during routine contact with patients of visible minorities, particularly those of South Asian, Filipino and black ethnicity.
Differences in the prevalence of cardiovascular diseases and associated risk factors have been noted across ethnic groups both within and between countries.1-14 The populations of many developed countries are becoming more diverse, so understanding these differences is important for planning appropriate treatment and prevention strategies. Studies in the United States have consistently shown a higher prevalence of cardiovascular risk factors among black and Hispanic people than among white people.3,5,8 Furthermore, the health outcomes of these ethnic populations in the United States have been consistently worse in terms of associated disease prevalence, morbidity and mortality.13-19 Other groups, such as people of South Asian ethnicity, have greater incidence and earlier onset of heart disease and diabetes mellitus, even at lower body mass index (BMI).7 Even though these differences can be largely attributable to disparities in socio-economic status and access to health insurance and care, differences remain after adjustment for these factors.20-25
Canada’s stringent selection process for skilled and healthy immigrants has resulted in a relatively healthy visible minority population (i.e., people who are neither white nor Aboriginal). However, only a few regional studies have examined cardiovascular risk factors such as diabetes, hypertension, smoking, BMI, hyperlipidemia and physical inactivity in Canadian ethnic groups, and each of these studies has considered only a limited number of ethnic groups or risk factors. Anand and colleagues1 reported that South Asian people living in Canada had higher levels of hyperlipidemia and established cardiovascular disease than those of white and Chinese ethnicity. Although rates of hypertension were similar across these 3 groups, BMI was lowest for the Chinese participants. Bryan and colleagues26reported lower levels of physical activity among all visible minority groups relative to white people in Canada. Because the Canadian population is becoming increasingly diverse, and given that the risk factors of today predict the diseases of tomorrow, it is imperative to document cardiovascular risk factors at the national level to allow planning of appropriate preventive strategies. We used data from the nationally representative Canadian Community Health Survey (CCHS) to examine the prevalence of cardiovascular risk factors among various ethnic groups in Canada.
Methods
Data source
We obtained data from the 2000, 2003 and 2005 iterations of the CCHS, a national cross-sectional survey of persons aged 12 years and older in the 10 provinces and 3 territories. We pooled data from these 3 cycles to obtain a sample large enough to allow comparisons of cardiovascular risk factors among various ethnic groups. The surveys excluded people living on Indian reserves and Canadian Forces bases and those in some remote areas. The CCHS used 3 methods for sampling: 50% of respondents were selected from an area frame, 49% from a list frame of telephone numbers and 1% from a random-digit-dialling frame. These multiple sampling techniques were used in lieu of a pure random sample to ensure that data were obtained from across the country. Consequently, certain communities and populations (e.g., youth) were overrepresented in each survey. Therefore, each administrative health region or group of administrative health regions was assigned a calculated sample weight to generate a representative national population. One respondent per household was selected at random for a telephone or in-person interview. Details of the survey methodology are published elsewhere.27
Study variables
We included in our analysis variables for which data were collected using the same survey questions in each of the 3 CCHS cycles. The sociodemographic characteristics were age, sex, marital status, education, household income, language spoken, immigration status, residency type (urban or rural), household size and region (province or territory) at the time of the survey. We categorized household income into 5 groups: less than $30 000, $30 000–$49 999, $50 000–$79 999, $80 000 or higher, or missing. Cardiovascular risk factors were presence of diabetes, presence of hypertension, daily or occasional smoking, physical inactivity and BMI. Presence of diabetes and hypertension was determined from the self-reported answers to the survey questions “Do you have diabetes?” and “Do you have high blood pressure?” The survey collected information on the type, frequency and intensity of physical activity over the previous 3 months. This information was used to estimate the respondent’s average daily energy expenditure during leisure time activities, according to detailed methods reported elsewhere.28 Major chronic medical conditions were heart disease, stroke, cancer, bronchitis, chronic obstructive pulmonary disease, bowel disease, arthritis, epilepsy, ulcers, thyroid disease and diabetes mellitus. Each respondent was asked to report his or her ethnicity according to the following categories: white, Chinese, Japanese, Korean, South Asian, Filipino or South East Asian, Arab, West Asian, Aboriginal and “other.” For the purposes of this study, visible minorities were defined as all ethnic categories other than white and Aboriginal. We excluded all respondents with missing data values for any variable except household income or BMI.
Statistical analysis
Because the CCHS used multistage sampling methods, we calculated descriptive statistics for weighted data. The sample weights assigned to health regions in Canada differed between cycles for 2 main reasons. First, the sample of respondents differed between cycles. Second, the boundaries for several health regions differed between cycles. To combine the data from different cycles, it was necessary to recalculate sampling weights using an equation provided by Statistics Canada. In addition, the data from the 3 cycles were bootstrapped to obtain estimates of the variance. More specifically, the data were resampled 500 times according to the adjusted weights after data from the 3 cycles were pooled. After bootstrapping, we calculated the prevalence of the risk factors. We did not conduct statistical tests for differences in prevalence among ethnic groups. One reason for not conducting such tests is that our large sample size was likely to generate very small p values. Another reason is that we tried to avoid multiple comparisons across ethnicities. We calculated the age-standardized prevalence of each risk factor on the basis of the composition of the survey population by age category (≤ 34, 35–49, 50–64 and ≥ 65 years) and stratified the prevalence by sex. The effect of participants’ ethnicity on the prevalence of risk factors was estimated with logistic regression, while differences in age, sex, marital status, education, household income, language spoken, immigration status, residency type (urban or rural), household size and region (province or territory) were held constant. For household income, the “missing” category was included in the model because of the large number of respondents with missing data for this variable. Statistics Canada approved this study for the purposes of providing access to the survey data. We conducted all analyses at the Prairie Regional Data Centre in Calgary.
Results
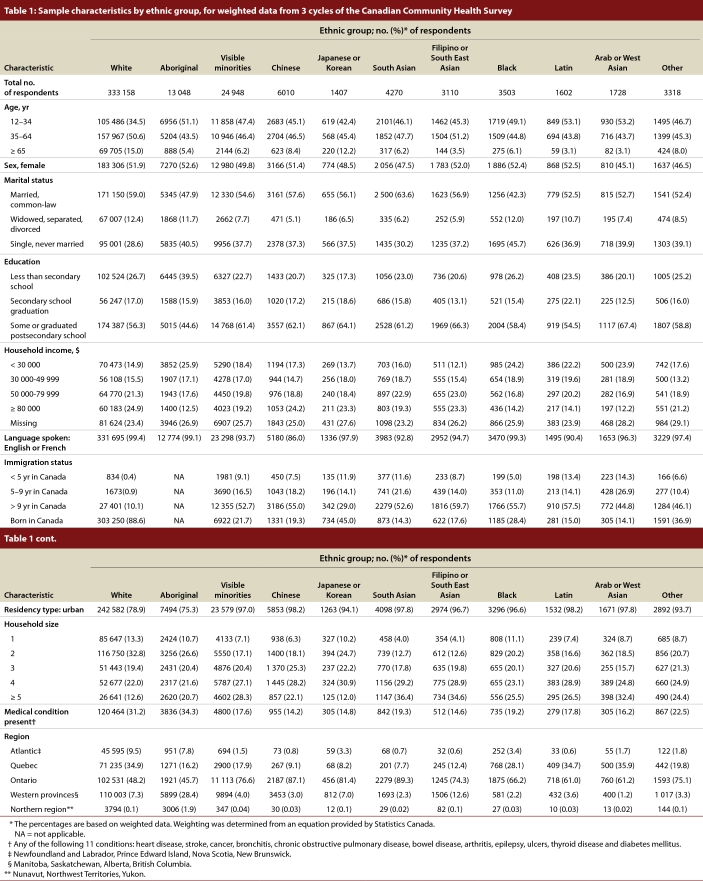
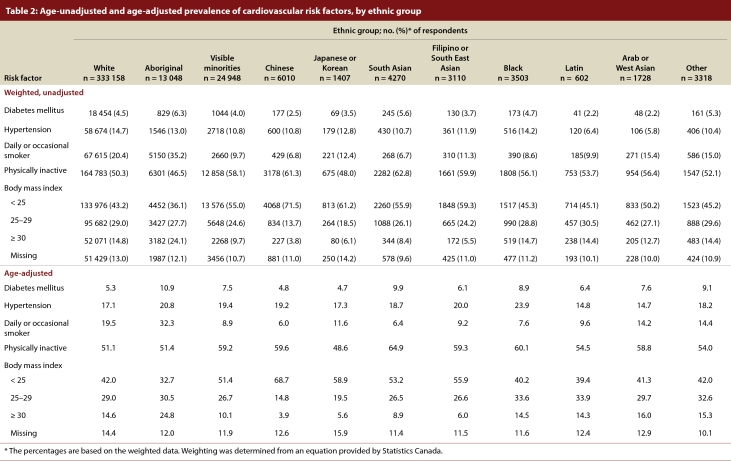
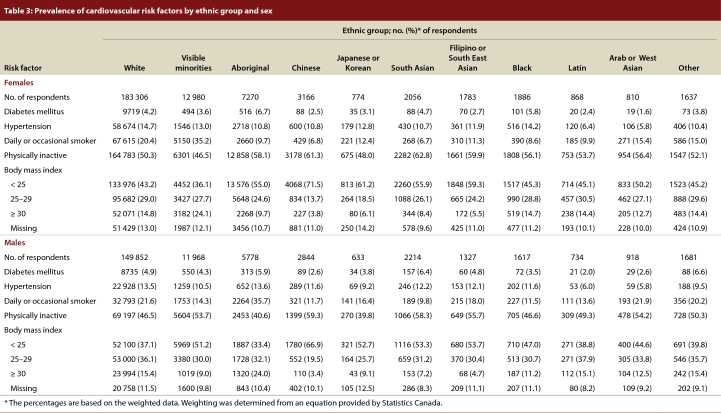
The exclusion of respondents with missing data for variables listed in Table 1 reduced the original sample of 400 055 to 371 154 individuals (92.8% of the original sample). Compared with white people, respondents from visible minorities were younger, had higher educational status, occupied lower tiers of income, resided in urban rather than rural residences, had larger family size and reported fewer chronic medical conditions. Relative to white respondents, members of visible minorities also had lower prevalence of diabetes (4.5% v. 4.0%), hypertension (14.7% v. 10.8%), smoking (20.4% v. 9.7%), and BMI of 30 or higher (14.8% v. 9.7%) and higher prevalence of being physically inactive (50.3% v. 58.1%) (Table 2). When we examined the ethnic groups individually, we found differences for some cardiovascular risk factors. For example, although most members of visible minorities had lower rates of hypertension than white respondents, the rate for black people was similar to that for white people. Most ethnic groups were also less physically active than the white respondents, and people with Chinese and South Asian ethnicity were the least active. The prevalence of these risk factors did not vary significantly across regions for each ethnic population (e.g., Ontario, Quebec and western Canadian provinces; data available upon request). When we adjusted for age composition, we found that, relative to the white respondents, the visible minorities had higher age-standardized prevalence of diabetes (5.3% v. 7.5%) and hypertension (17.1% v. 19.4%) (Table 2). After stratifying the data by sex, we found that the rate of smoking was much higher among white females than among females from visible minorities (19.2% v. 5.1%) (Table 3). Physical inactivity was more prevalent among middle-aged respondents (35–64 years of age, 69.8%) but less prevalent among Chinese respondents aged 65 years or older (46.5%). A high proportion of elderly South Asian respondents were physically inactive (72.6%).
Table 1.
Sample characteristics by ethnic group, for weighted data from 3 cycles of the Canadian Community Health Survey
Table 2.
Age-unadjusted and age-adjusted prevalence of cardiovascular risk factors, by ethnic group
Table 3.
Prevalence of cardiovascular risk factors by ethnic group and sex
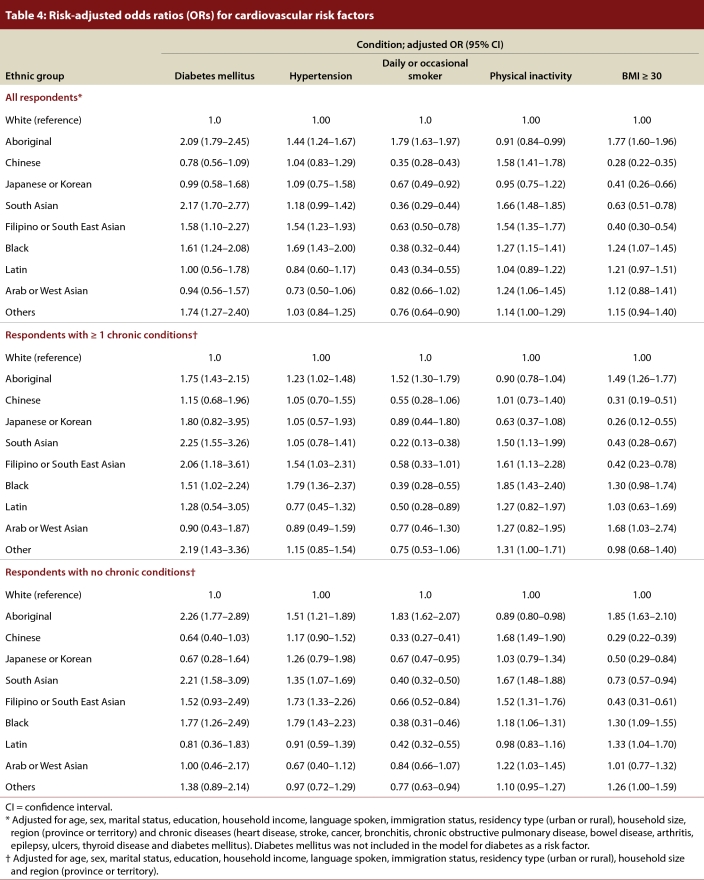
After adjustment for sociodemographic characteristics and chronic conditions, we found that diabetes and hypertension were significantly more prevalent among South Asian respondents (adjusted OR 2.17, 95% confidence interval [CI] 1.70–2.77 for diabetes and adjusted OR 1.18, 95% CI 0.99–1.42 for hypertension), Filipino or South East Asian respondents (adjusted OR 1.58, 95% CI 1.10–2.27 for diabetes and adjusted OR 1.54, 95% CI 1.23–1.93 for hypertension) and black respondents (adjusted OR 1.61, 95% CI 1.24–2.08 for diabetes and adjusted OR 1.69, 95% CI 1.43–2.00 for hypertension) than among white respondents (Table 4). Members of visible minorities, with the exception of Arab or West Asian respondents, were less likely than white respondents to smoke. Compared with white respondents, Chinese, Japanese or Korean, South Asian, and Filipino or South East Asian respondents were less likely to be obese, and Chinese, South Asian or Filipino, South East Asian, black and Arab or West Asian respondents were more likely to be physically inactive.
Table 4.
Risk-adjusted odds ratios (ORs) for cardiovascular risk factors
Interpretation
We found that visible minorities differed in terms of the prevalence of cardiovascular risk factors relative to white respondents. Within the combined visible minority group, the prevalence of these risk factors varied greatly across ethnicities. The prevalences of obesity and smoking were lower in the visible minorities than in the white population, but physical inactivity was more prevalent among the visible minorities. The South Asian, Filipino or South East Asian, and black ethnic groups had significantly higher prevalences of diabetes and hypertension than the white respondents, and the Korean, Japanese and Latin populations were as physically inactive as the white population.
Our findings of high prevalence of cardiovascular risk factors among black people in Canada support findings from the United States. In 2003–2004, black people in the United States had a high prevalence of hypertension, 39.1% of the population.29 Recent data from the Canadian province with the largest population (i.e., Ontario), based on physical measurements, demonstrated a 31.5% prevalence of hypertension in the black population,30 much higher than our finding of 14.2%. This difference indicates that the self-reported survey data used in our study were missing cases of undiagnosed hypertension. Another difference between research from the United States and our study is the prevalence of overweight in the black populations (69.6% in one US study31 v. 43.5% with BMI of 25 or higher in our Canadian study). There are historical differences between the United States and Canada in terms of the pathways of immigration for black people. Many US black people have ancestral roots in slavery, have less education and have social disadvantages that may lead to health inequalities. Although Canadian black people initially emigrated from the United States, many later immigrants have come from the Caribbean and Africa, reflecting Canadian immigration policies, which have tended to increase the number of educated immigrants.32,33 Nevertheless, inequalities in the prevalence of cardiovascular risk factors exist in Canada. The higher prevalences of hypertension and overweight among black respondents relative to other visible minorities may be attributable to different cultural norms regarding lifestyle and health behaviours.34
In our study, people from visible minorities, particularly South Asian respondents, reported high levels of physical inactivity, consistent with findings from similar studies in the United Kingdom and the United States.7,35,36 More interesting was the finding that Chinese respondents with chronic disease were as physically inactive as white respondents with chronic disease (adjusted OR 1.01, 95% CI 0.73–1.40), but Chinese respondents without chronic disease were more likely to be physically inactive than white respondents with chronic disease (adjusted OR 1.68, 95% CI 1.49–1.90). The low prevalence of physical inactivity among Chinese respondents with chronic disease has been reported from the United States37 and from China.38 Two possible reasons are that elderly Chinese people may value health maintenance and disease prevention through physical activity more and may have more time to do exercise than do their younger counterparts. In addition, beliefs about physical activity may play an important role. Kandula and Lauderdale,39 who analyzed data from the California Health Survey, found that physical activity among Asian Americans increased significantly with length of stay in the United States and with ability to speak English. Their findings suggest that acculturation promotes physical activity.
Compared with white respondents, levels of overweight and obesity were lower among Chinese, Japanese or Korean, South Asian, and Filipino or South East Asian respondents. At least one previous study has shown that South Asian people have a greater percentage of body fat than white people, even at low BMI, which results in an increased risk of diabetes, cardiovascular disease and other metabolic disorders.40 There is a need for a lower BMI cutoff to identify overweight Asian people and prevent premature cardiovascular disease in this population.41 Furthermore, with increased duration of residence in developed countries, immigrants tend to become overweight or obese as they become sedentary and adapt to high-calorie diets, which indicates an erosion of the initial healthy immigrant effect.42-45 Thus, although the proportion of people of visible minorities who are obese is currently relatively low, it is likely to increase over time, and the initiation of effective preventive measures is therefore warranted.
Our study had some limitations. First, the reliability and validity of the survey were not assessed. Because the survey responses were self-reported, the level of recall bias and the underreporting of risk factors across ethnic populations were unknown. Physical measurement of hypertension and BMI would provide more accurate data than self-reported values. Leung and colleagues46 conducted a cross-sectional telephone survey of Chinese and white residents in Calgary, Canada, to assess health status in terms of a 5-point Likert-type scale, a health index scale (0–100) and number of chronic conditions. They reported that health status across these 3 measures was inconsistent among the Chinese respondents. In addition, the Chinese respondents were more likely than the white respondents to report values close to the midpoint of the 2 rating scales. However, it is unknown, from that study or others, whether different ethnic groups report health data differently. Second, although the CCHS was conducted in several languages, people with language barriers and sicker people were less likely to be surveyed. Third, our exclusion of individuals with missing values for the variables might have resulted in slight selection bias. However, we excluded only a small number of respondents with missing values, which likely had minimal impact on our large sample. Fourth, we estimated obesity using BMI but lacked important information about waist and hip circumference. Fifth, caution should be exercised in generalizing our findings to ethnic populations outside Canada, because ethnic groups vary across geographic regions for certain risk factors. These differences could result in underestimation of the prevalence of cardiovascular risk factors.
In conclusion, the prevalence of cardiovascular risk factors varied across ethnic groups in Canada. Further research is needed to understand the protective and restrictive factors underlying these variations in prevalence within visible minorities, the Aboriginal population and the white population. The unique risk factor profiles of each ethnic group need to be considered during health promotion activities. Promoting physical activity to specific visible minorities, such as Chinese and South Asian people, should be prioritized in population health programs. In addition, aggressive programs for the prevention, early detection and control of diabetes and hypertension may need to target South Asian, Filipino and black people.
Biographies
Richard Liu, MD, is clinical resident, Faculty of Medicine, Dalhousie University, Halifax, Nova Scotia, Canada.
Lawrence So, PhD, is post-doctoral fellow, Centre for Health Services & Policy Research, University of British Columbia, Vancouver, British Columbia.
Sailesh Mohan, MD, MPH, is post-doctoral fellow, Department of Community Health Sciences, University of Calgary, Calgary, Alberta.
Nadia Khan, MD, MSc, is assistant professor, the Centre for Health Evaluation and Outcome Sciences, University of British Columbia, Vancouver, British Columbia.
Kathryn King, PhD, is professor, Faculty of Nursing, University of Calgary, Calgary, Alberta.
Hude Quan, MD, PhD, is associate professor, Department of Community Health Sciences, University of Calgary, Calgary, Alberta.
Footnotes
Competing interests: None declared.
Funding source: Sailesh Mohan is supported by the Canada-HOPE program of the Canadian Institutes of Health Research (CIHR). Nadia Khan is supported by a New Investigator Award from the CIHR. Hude Quan and Kathryn King are supported by Alberta Innovations – Health Solution Health Scholar Awards.
Contributors: Richard Liu contributed to the data interpretation and drafted the manuscript. Lawrence So contributed to the data analysis and manuscript revision. Sailesh Mohan contributed to the data interpretation and manuscript revision. Nadia Khan and Kathryn King contributed to the study design, data interpretation and manuscript revision. Hude Quan contributed to the study conception and design, data interpretation and manuscript revision. All of the authors reviewed and approved the final version. Hude Quan is the study guarantor.
References
- 1.Anand S S, Yusuf S, Vuksan V, Devanesen S, Teo K K, Montague P A, Kelemen L, Yi C, Lonn E, Gerstein H, Hegele R A, McQueen M. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE. Lancet. 2000;356(9226):279–284. doi: 10.1016/s0140-6736(00)02502-2. [DOI] [PubMed] [Google Scholar]
- 2.Bedi Updesh Singh, Singh Sarabjeet, Syed Asmir, Aryafar Hamed, Arora Rohit. Coronary artery disease in South Asians: an emerging risk group. Cardiol Rev. 2006;14(2):74–80. doi: 10.1097/01.crd.0000182411.88146.72. [DOI] [PubMed] [Google Scholar]
- 3.Bravata DM, Wells CK, Gulanski B, Kernan WN, Brass LM, Long J, Concato J. Racial disparities in stroke risk factors: the impact of socioeconomic status. Stroke. 2005;36:1507–1511. doi: 10.1161/01.STR.0000170991.63594.b6. [DOI] [PubMed] [Google Scholar]
- 4.Fischbacher C M, Bhopal R, Povey C, Steiner M, Chalmers J, Mueller G, Jamieson J, Knowles D. Record linked retrospective cohort study of 4.6 million people exploring ethnic variations in disease: myocardial infarction in South Asians. BMC Public Health. 2007 Jul 05;7:142. doi: 10.1186/1471-2458-7-142. http://www.biomedcentral.com/1471-2458/7/142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hayes D K, Denny C H, Keenan N L, Croft J B, Sundaram A A, Greenlund K J. Racial/ethnic and socioeconomic differences in multiple risk factors for heart disease and stroke in women: behavioral risk factor surveillance system, 2003. J Womens Health (Larchmt) 2003;15(9):1000–1008. doi: 10.1089/jwh.2006.15.1000. [DOI] [PubMed] [Google Scholar]
- 6.Joffres M R, Hamet P, MacLean D R, L’italien G J, Fodor G. Distribution of blood pressure and hypertension in Canada and the United States. Am J Hypertens. 2001;14(11 Pt 1):1099–1105. doi: 10.1016/s0895-7061(01)02211-7. [DOI] [PubMed] [Google Scholar]
- 7.Joshi Prashant, Islam Shofiqul, Pais Prem, Reddy Srinath, Dorairaj Prabhakaran, Kazmi Khawar, Pandey Mrigendra Raj, Haque Sirajul, Mendis Shanthi, Rangarajan Sumathy, Yusuf Salim. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–294. doi: 10.1001/jama.297.3.286. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=17227980. [DOI] [PubMed] [Google Scholar]
- 8.Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–152. [PubMed] [Google Scholar]
- 9.Mohan V, Sandeep S, Deepa R, Shah B, Varghese C. Epidemiology of type 2 diabetes: Indian scenario. Indian J Med Res. 2007;125(3):217–230. http://www.icmr.nic.in/ijmr/2007/March/0302.pdf. [PubMed] [Google Scholar]
- 10.Tillin T, Forouhi N, Johnston DG, McKeigue PM, Chaturvedi N, Godsland IF. Metabolic syndrome and coronary heart disease in South Asians, African-Caribbeans and white Europeans: a UK population-based cross-sectional study. Diabetologia. 2005 Mar 10;48(4):649–656. doi: 10.1007/s00125-005-1689-3. [DOI] [PubMed] [Google Scholar]
- 11.Williams David R. The health of U.S. racial and ethnic populations. J Gerontol B Psychol Sci Soc Sci. 2005;60 Spec No 2:53–62. doi: 10.1093/geronb/60.special_issue_2.s53. [DOI] [PubMed] [Google Scholar]
- 12.Winkleby MA, Kraemer H, Lin J, Jatulis D, Fortmann SP. Sociodemographic influences on Hispanic–white differences in blood pressure. Public Health Rep. 1996;111 Suppl 2:30–32. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=8898768. [PMC free article] [PubMed] [Google Scholar]
- 13.Boltri John M, Okosun Ike S, Davis-Smith Monique, Vogel Robert L. Hemoglobin A1c levels in diagnosed and undiagnosed black, Hispanic, and white persons with diabetes: results from NHANES 1999–2000. Ethn Dis. 2005;15(4):562–567. [PubMed] [Google Scholar]
- 14.Harris M I, Eastman R C, Cowie C C, Flegal K M, Eberhardt M S. Racial and ethnic differences in glycemic control of adults with type 2 diabetes. Diabetes Care. 1999;22(3):403–408. doi: 10.2337/diacare.22.3.403. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=10097918. [DOI] [PubMed] [Google Scholar]
- 15.Herman William H, Ma Yong, Uwaifo Gabriel, Haffner Steven, Kahn Steven E, Horton Edward S, Lachin John M, Montez Maria G, Brenneman Tina, Barrett-Connor Elizabeth Diabetes Prevention Program Research Group. Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program. Diabetes Care. 2007 May 29;30(10):2453–2457. doi: 10.2337/dc06-2003. http://care.diabetesjournals.org/cgi/pmidlookup?view=long&pmid=17536077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hicks LeRoi S, Shaykevich Shimon, Bates David W, Ayanian John Z. Determinants of racial/ethnic differences in blood pressure management among hypertensive patients. BMC Cardiovasc Disord. 2005 Jun 22;5(1):16. doi: 10.1186/1471-2261-5-16. http://www.biomedcentral.com/1471-2261/5/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saydah Sharon, Cowie Catherine, Eberhardt Mark S, De Rekeneire Nathalie, Narayan K M Venkat. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethn Dis. 2007;17(3):529–535. [PubMed] [Google Scholar]
- 18.Seo Dong-Chul, Torabi Mohammad R. Racial/ethnic differences in body mass index, morbidity and attitudes toward obesity among U.S. adults. J Natl Med Assoc. 2006;98(8):1300–1308. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=16916128. [PMC free article] [PubMed] [Google Scholar]
- 19.Sanderson Bonnie K, Mirza Saema, Fry Rachel, Allison Jeroan J, Bittner Vera. Secondary prevention outcomes among black and white cardiac rehabilitation patients. Am Heart J. 2007;153(6):980–986. doi: 10.1016/j.ahj.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 20.Heisler Michele, Faul Jessica D, Hayward Rodney A, Langa Kenneth M, Blaum Caroline, Weir David. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167(17):1853–1860. doi: 10.1001/archinte.167.17.1853. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=17893306. [DOI] [PubMed] [Google Scholar]
- 21.Jones R Huw, Ozanne Susan E. Intra-uterine origins of type 2 diabetes. Arch Physiol Biochem. 2007;113(1):25–29. doi: 10.1080/13813450701318484. [DOI] [PubMed] [Google Scholar]
- 22.Goel Mita Sanghavi, McCarthy Ellen P, Phillips Russell S, Wee Christina C. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–2867. doi: 10.1001/jama.292.23.2860. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=15598917. [DOI] [PubMed] [Google Scholar]
- 23.Robert Stephanie A, Reither Eric N. A multilevel analysis of race, community disadvantage, and body mass index among adults in the US. Soc Sci Med. 2004;59(12):2421–2434. doi: 10.1016/j.socscimed.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 24.Winkleby M A, Gardner C D, Taylor C B. The influence of gender and socioeconomic factors on Hispanic/white differences in body mass index. Prev Med. 1996;25(2):203–211. doi: 10.1006/pmed.1996.0047. [DOI] [PubMed] [Google Scholar]
- 25.Tremblay Mark S, Pérez Claudio E, Ardern Chris I, Bryan Shirley N, Katzmarzyk Peter T. Obesity, overweight and ethnicity. Health Rep. 2005;16(4):23–34. http://www.statcan.gc.ca/studies-etudes/82-003/archive/2005/8041-eng.pdf. [PubMed] [Google Scholar]
- 26.Bryan Shirley N, Tremblay Mark S, Pérez Claudio E, Ardern Chris I, Katzmarzyk Peter T. Physical activity and ethnicity: evidence from the Canadian Community Health Survey. Can J Public Health. 2006;97(4):271–276. doi: 10.1007/BF03405602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Béland Yves. Canadian Community Health Survey — methodological overview. Health Rep. 2002;13(3):9–14. http://www.statcan.gc.ca/studies-etudes/82-003/archive/2002/6099-eng.pdf. [PubMed] [Google Scholar]
- 28.Canadian Community Health Survey, cycle 3.1 (2005). Public use micro data file (PUMF). Integrated derived variable (DV) and grouped variable specifications. Ottawa (ON): Statistics Canada; 2006 Aug. [accessed 2008 Oct 15]. http://www.statcan.ca/english/sdds/document/3226_D5_T9_V3_E.pdf. [Google Scholar]
- 29.Ong Kwok Leung, Cheung Bernard M Y, Man Yu Bun, Lau Chu Pak, Lam Karen S L. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension. 2007 Dec 11;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. http://hyper.ahajournals.org/cgi/pmidlookup?view=long&pmid=17159087. [DOI] [PubMed] [Google Scholar]
- 30.Leenen Frans H H, Dumais Jean, McInnis Natalie H, Turton Penelope, Stratychuk Lori, Nemeth Kathleen, Lum-Kwong Margaret Moy, Fodor George. Results of the Ontario survey on the prevalence and control of hypertension. CMAJ. 2008;178(11):1441–1449. doi: 10.1503/cmaj.071340. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=18490640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flegal Katherine M, Carroll Margaret D, Ogden Cynthia L, Johnson Clifford L. Prevalence and trends in obesity among US adults, 1999-2000. JAMA. 2002;288(14):1723–1727. doi: 10.1001/jama.288.14.1723. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=12365955. [DOI] [PubMed] [Google Scholar]
- 32.Milan A, Tran K. Blacks in Canada: a long history. Ottawa (ON): Statistics Canada; 2004. Catalogue no. 11-008 http://www.statcan.ca/english/freepub/11-008-XIE/2003004/articles/6802.pdf. [Google Scholar]
- 33.Nazroo James, Jackson James, Karlsen Saffron, Torres Myriam. The Black diaspora and health inequalities in the US and England: Does where you go and how you get there make a difference? Sociol Health Illn. 2007;29(6):811–830. doi: 10.1111/j.1467-9566.2007.01043.x. [DOI] [PubMed] [Google Scholar]
- 34.Ricciardelli Lina A, McCabe Marita P, Williams Robert J, Thompson J Kevin. The role of ethnicity and culture in body image and disordered eating among males. Clin Psychol Rev. 2007 Feb 07;27(5):582–606. doi: 10.1016/j.cpr.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 35.Fischbacher C M, Hunt S, Alexander L. How physically active are South Asians in the United Kingdom? A literature review. J Public Health (Oxf) 2004;26(3):250–258. doi: 10.1093/pubmed/fdh158. http://jpubhealth.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=15454592. [DOI] [PubMed] [Google Scholar]
- 36.Kamath S K, Hussain E A, Amin D, Mortillaro E, West B, Peterson C T, Aryee F, Murillo G, Alekel D L. Cardiovascular disease risk factors in 2 distinct ethnic groups: Indian and Pakistani compared with American premenopausal women. Am J Clin Nutr. 1999;69(4):621–631. doi: 10.1093/ajcn/69.4.621. http://www.ajcn.org/cgi/pmidlookup?view=long&pmid=10197563. [DOI] [PubMed] [Google Scholar]
- 37.Taylor Vicky M, Yasui Yutaka, Tu Shin-Ping, Neuhouser Marian L, Li Lin, Woodall Erica, Acorda Elizabeth, Cripe Swee May, Hislop T Gregory. Heart disease prevention among Chinese immigrants. J Community Health. 2007;32(5):299–310. doi: 10.1007/s10900-007-9057-5. [DOI] [PubMed] [Google Scholar]
- 38.Lee Sang-Ah, Xu Wang Hong, Zheng Wei, Li Honglan, Yang Gong, Xiang Yong-Bing, Shu Xiao Ou. Physical activity patterns and their correlates among Chinese men in Shanghai. Med Sci Sports Exerc. 2007;39(10):1700–1707. doi: 10.1249/mss.0b013e3181238a52. [DOI] [PubMed] [Google Scholar]
- 39.Kandula Namratha R, Lauderdale Diane S. Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Ann Epidemiol. 2005;15(4):257–265. doi: 10.1016/j.annepidem.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 40.Razak Fahad, Anand Sonia S, Shannon Harry, Vuksan Vladimir, Davis Bonnie, Jacobs Ruby, Teo Koon K, McQueen Matthew, Yusuf Salim. Defining obesity cut points in a multiethnic population. Circulation. 2007 Apr 09;115(16):2111–2118. doi: 10.1161/CIRCULATIONAHA.106.635011. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17420343. [DOI] [PubMed] [Google Scholar]
- 41.Tremblay Mark S, Bryan Shirley N, Pérez Claudio E, Ardern Chris I, Katzmarzyk Peter T. Physical activity and immigrant status: evidence from the Canadian Community Health Survey. Can J Public Health. 2006;97(4):277–282. doi: 10.1007/BF03405603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koya Deepika L, Egede Leonard E. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007 Mar 09;22(6):841–846. doi: 10.1007/s11606-007-0163-y. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=17503110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lauderdale D S, Rathouz P J. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes Relat Metab Disord. 2000;24(9):1188–1194. doi: 10.1038/sj.ijo.0801365. [DOI] [PubMed] [Google Scholar]
- 44.Yang E J, Chung Hae Kyung, Kim Wha Young, Bianchi Leonard, Song Won O. Chronic diseases and dietary changes in relation to Korean Americans' length of residence in the United States. J Am Diet Assoc. 2007;107(6):942–950. doi: 10.1016/j.jada.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Harding Seeromanie. Mortality of migrants from the Indian subcontinent to England and Wales: effect of duration of residence. Epidemiology. 2003;14(3):287–292. [PubMed] [Google Scholar]
- 46.Leung Brenda, Luo Nan, So Lawrence, Quan Hude. Comparing three measures of health status (perceived health with Likert-type scale, EQ-5D, and number of chronic conditions) in Chinese and white Canadians. Med Care. 2007;45(7):610–617. doi: 10.1097/MLR.0b013e3180331f58. [DOI] [PubMed] [Google Scholar]