Abstract
Posttraumatic growth (PTG) involves personal psychological growth in response to a traumatic or very stressful event. Using theoretical guidance from Tedeschi and Calhoun's cognitive model, this study evaluated the relationship between specific individual, distress, and stress-processing factors and PTG among young adults who experienced an illness-related trauma earlier in life through a relative's serious illness. Sixty individuals with a relative with a serious illness completed measures of PTG, posttraumatic stress symptoms (PTSS), anxiety, and coping. PTG was positively associated with trait anxiety, PTSS, and the use of active, problem-focused coping strategies. Factors associated with PTG development in individuals who have a relative with a chronic illness are similar to that of individuals who had a serious illness themselves. The relationship between PTSS and PTG is moderated by whether the relative's current illness status is resolved versus not resolved.
Keywords: posttraumatic growth, posttraumatic stress, chronic illness, relatives
In recent years, there has been an increased focus on understanding the range of effects that a traumatic medical event can have on an individual. In addition to commonly recognized negative effects such as posttraumatic stress symptoms (PTSS), there may also be positive personal developmental change, including posttraumatic growth (PTG), which occurs in conjunction with or in the aftermath of a traumatic experience. PTG has been defined as “positive psychological change experienced as a result of the struggle with highly challenging life circumstances or traumatic events” (Calhoun & Tedeschi, 1999, p. 1). As an individual attempts to incorporate the reality of a stressful event into their current schema, PTG may develop (Tedeschi & Calhoun, 2004). PTG encompasses several domains, including greater appreciation for life, development of meaningful interpersonal relationships, and a sense of greater personal strength (Tedeschi & Calhoun, 2004). Individuals who develop PTG may have a renewed desire to reconnect with family members, or may experience greater self-efficacy after having survived a traumatic event. PTG may be conceptualized as a process or outcome (Tedeschi & Calhoun, 2004). The development of PTG may occur several years after illness or injury onset and persist for long periods of time once it develops. For instance, PTG has been documented in adults who experienced a spinal cord injury more than 10 years earlier (Chun & Lee, 2008). Additionally, PTG has been associated with lower levels of depression and greater well-being (Helgeson, Reynolds, & Tomich, 2006).
Individuals who indirectly experience a traumatic event, such as the serious physical illness of a relative or close friend, may also develop PTG (Davis, Wohl, & Verberg, 2007; Thornton & Perez, 2006; Weiss, 2004). The reactions of individuals who indirectly experienced a traumatic event are consistent with research on direct exposure to trauma, including PTSS developing after threatened death or injury to another individual (DSM–IV–TR, 2000). Additionally, PTG has been documented among individuals whose relative survived an illness (Mosher, Danoff-Burg, & Brunker, 2006; Thornton & Perez, 2006; Weiss, 2004), as well as individuals whose relative succumbed to an illness (Davis et al., 2007). In fact, in one study of adults who, as children, had a parent with cancer, PTG developed regardless of the parent's survival or death (Wong, Cavanaugh, MacLeamy, Sojourner-Nelson, & Koopman, 2009). Thus, PTG has been documented in individuals whose relative's illness resolved, either through death or survival (i.e., recovery).
There are many factors hypothesized to relate to PTG. To better understand the associations among these factors, Tedeschi and Calhoun (2004) proposed a cognitive model of PTG. This conceptualization emphasizes the central role of the individual's cognitive appraisal (i.e., interpretation of a situation) and processing of the trauma as influencing the potential development of PTG. Tedeschi and Calhoun (2004) emphasize the role of current processing, which occurs through ongoing exposure to a trauma, as an important factor in facilitating greater PTG. The model indicates that an individual's pretrauma characteristics and temperamental vulnerability (e.g., trait anxiety), the nature of the traumatic event (e.g., prolonged exposure to the trauma), and coping processes combine to influence the development of PTG. Studies of individuals with serious illnesses have supported some of these associations, such as trait anxiety being inversely correlated with PTG (Kazak et al., 1997) and use of positive reappraisal (i.e., reframing the stressor to emphasize positives of the situation) as a coping strategy being positively associated with PTG (Garnefski, Kraaij, Schroevers, & Somsen, 2008). In the current study we apply this model to understand the process by which individuals adjust to having a relative with a serious medical condition.
Many of the same correlates of PTG that have been found among illness survivors have also been identified in studies of relatives and caregivers. For example, among relatives, use of positive reframing coping strategies predicted greater PTG in partners of prostate cancer survivors (Thornton & Perez, 2006). Also, the experience of PTSS was positively associated with PTG among bereaved HIV/AIDS patients' caregivers (Cadell, Regehr, & Hemsworth, 2003). A positive association between PTG and PTSS suggests that some stress symptoms may be necessary for PTG to emerge or that both may result from exposure to the trauma.
The goal of the current study was to extend the PTG literature from illness survivors to individuals who experienced an illness-related trauma by having a relative with a serious physical illness. Specifically, we aimed to evaluate the association of factors identified in Tedeschi and Calhoun's (2004) model of PTG in young adults whose relative had an illness earlier in the participants' life. To date, the majority of studies on PTG within the context of serious illness have focused on single, homogeneous illness groups such as breast cancer survivors and their relatives (Cordova et al., 2007). We utilized a noncategorical approach toward having a relative with a serious illness to examine shared factors that are associated with PTG across illness groups. We also sought to expand Tedeschi and Calhoun's model of PTG by examining the impact of the relative's illness status on the development of PTG. Specifically, we assessed current levels of PTG in individuals who had a relative with a serious illness based on whether the relative's illness was resolved (i.e., either cured or resolved through death) or not resolved (i.e., ongoing illness) at the time of the study. Prior research with individuals who themselves had a serious illness revealed that those whose illness was resolved had higher levels of PTG than those whose illness was ongoing (Devine, Reed-Knight, Loiselle, Fenton, & Blount, 2010). The current study sought to further previously published research by examining the association between PTG, PTSS, and whether the illness was resolved, regardless of the outcome (i.e., recovery or death), or ongoing and continuing to influence one's daily life.
Based on previous research and theoretical guidance from the cognitive model of PTG, we hypothesized that PTG would be positively associated with PTSS, greater use of active, problem-focused coping strategies, lower trait anxiety, and the illness being resolved (vs. ongoing). We also explored whether the association between PTG and PTSS differed depending on the relative's illness status (i.e., resolved vs. not resolved).
Method
Participants
Study participants were 60 undergraduate students recruited through the university research pool and flyers posted on campus. Participants were included if they self-reported having a family member with a serious illness during the participant's childhood. Seventy-five people expressed interest in participating; individuals were excluded if their relative's illness resolved before the participant turning 6 years old (n = 9) or if a nonserious (e.g., chicken pox, n = 2) or psychiatric (n = 4) illness was reported.
On average, participants were 20.3 years old (SD = 1.5 years) at the time of the study. About half of the sample was female (51.7%), and participants were predominantly Caucasian (88.3%). At the time of the relative's diagnosis, the participants were a mean age of 9.3 years (SD = 4.5 years). The relatives identified as having an illness were grandparents (28.3%), parents (26.7%), close friends (25%), and other family members (20%). Participants' perceived emotional closeness to their relative was 7.7 (SD = 1.2), out of 10 using a Likert scale from 0 (“Not at all”) to 10 (“Extremely close”). Relatives were primarily diagnosed with cancer (60%); diabetes, pulmonary disease, gastrointestinal disorders, and other serious illnesses comprised the remaining 40%. At the time of participation, 21.7% of the relatives were currently experiencing the serious illness, while 31.7% were recovered and 46.7% were deceased.
Procedure
This study was conducted as part of a larger investigation examining PTG. All aspects of the study were in accordance with the university's Institutional Review Board approval. Participants were first screened using inclusion and exclusion criteria. Eligible individuals then completed informed consent and all study measures. Participants were given university research credit, if applicable, as compensation for their time.
Measures
Information Sheet
A questionnaire created for this study was used to collect demographic and disease-related information including age, gender, and race. Participants were asked to respond to questions regarding their relative's diagnosis, illness status, and treatment. When asked about their relative's illness status, participants indicated whether their relative was currently experiencing the illness, recovered from the illness, or deceased. Based on Tedeschi and Calhoun's cognitive model (Tedeschi and Calhoun, 2004), which emphasizes the role of cognitive processing in the development of PTG, the responses were coded as “resolved” or “not resolved.” The “resolved” category included individuals whose relative was no longer experiencing the daily demands of an illness because of recovery or death, whereas the “not resolved” category included individuals whose relative was currently experiencing the illness. These codes were chosen to categorize individuals based on if they were currently experiencing the demands of a relative's illness, which would require ongoing cognitive processing.
Posttraumatic Growth Inventory
The Posttraumatic Growth Inventory (PTGI; Tedeschi & Calhoun, 1996) is a 21-item self-report measure, which assesses positive outcomes related to traumatic experiences. Participants were asked to rate the degree to which they experienced a certain change in their life as a result of their experience with a relative's illness. Each item is rated on a six-point Likert scale ranging from 0 (“I did not experience this change”) to 5 (“I experienced this change to a very great degree”). Examples of questions include, “I have new priorities about what is important in life” and “I appreciate each day more.” The PTGI contains five subscales including Relating to Others, New Possibilities, Personal Strength, Appreciation of Life, and Spiritual Change and a total scale score, which was used in this study. In the present study, internal consistency for the full scale across participants was excellent (α = .94).
Impact of Event Scale—Revised
The Impact of Event Scale—Revised (IES-R; Weiss & Marmar, 1997) is a 22-item self-report measure of posttraumatic stress symptoms that resulted from a specific life event. For the present study, participants were asked to provide a rating for how distressing each item was during the past seven days with respect to their experience with a relative's illness on a 5-point Likert scale from 0 (“not at all”) to 4 (“extremely”). Examples of questions include “I tried not to talk about,” “I had waves of strong feelings about it,” and “I was jumpy and easily startled.” In the present study, the IES-R full scale had high internal consistency (α = .93).
Ways of Coping
The Ways of Coping (WAYS; Folkman & Lazarus, 1980) is a 66-item self-report measure of how individuals cope with a self-selected specific recent stressful event. Each item was rated on a scale from 0 (“does not apply or not used”) to 3 (“used quite a bit”). The WAYS assesses eight coping factors including Confrontive Coping, Distancing, Self-Controlling, Seeking Social Support, Accepting Responsibility, Escape-Avoidance, Planful Problem Solving, and Positive Reappraisal. In the present study, high internal consistency was found for the WAYS full scale (α = .92). The internal consistencies for the three primary subscales of interest used in analyses, Planful Problem Solving, Positive Reappraisal, and Accepting Responsibility, were α = .76, .81, and .68, respectively.
State–Trait Anxiety Inventory
The State–Trait Anxiety Inventory (STAI; Spielberger, 1983) is a 40-item self-report measure of state and trait anxiety. The trait subscale measures a more stable tendency to experience anxiety whereas the state subscale measures a temporary experience of anxiety or tension. Each item is rated on a 4-point intensity scale. Internal consistency for the current study was good for the State subscale (α = .93) and Trait subscale (α = .92).
Data Analysis
Demographic variables were analyzed using descriptive statistics. Two-tailed Pearson correlations and one-way analyses of variance (ANOVAs) were used to examine the relationship between PTG and demographic and medical outcome variables and factors from the Tedeschi and Calhoun (2004) cognitive model. Hierarchical multiple regression was utilized to predict PTG using Tedeschi and Calhoun's model to determine order of entry for variables.
Results
Demographic and Medical Outcome Variables and Posttraumatic Growth
One-way ANOVAs revealed no significant differences in PTG based on demographic variables such as gender, race, college level, family income, or parent marital status. Further, PTG was not significantly correlated with the participant's age. There were no significant differences in PTG based on the relative's current illness status, with the mean levels of PTG for the three groups being: resolved through recovery (M = 55.16, SD = 27.91), resolved because of death (M = 56.18, SD = 14.64), and not resolved/ongoing illness (M = 53.46, SD = 26.16). The resolved groups were condensed for the remainder of analyses.
Associations Among Factors and Posttraumatic Growth
PTG was significantly and positively related to current posttraumatic stress symptoms from the IES-R, r(60) = .32, p = .01 and the use of the following coping strategies from the WAYS: Planful Problem Solving, r(60) = .41, p < .01, Positive Reappraisal, r(60) = .45, p < .01, and Accepting Responsibility, r(60) = .26, p = .05. Further, there was a significant relationship between trait anxiety (STAI) and PTG, r(60) = −.31, p = .02, in that lower levels of anxious symptoms were associated with greater PTG. PTG was not significantly correlated with state anxiety (see Table 1).
Table 1. Intercorrelations Among Variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | Mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Posttraumatic growth | — | −.31* | −.25 | −.06 | .32* | .41** | .45** | .26* | 55.3 (21.8) |
| 2. Trait anxiety | — | .87** | −.08 | .28* | −.22 | −.19 | .20 | 39.3 (11.1) | |
| 3. State anxiety | — | .25 | −.19 | −.15 | .14 | 37.7 (11.4) | |||
| 4. Current illness statusa | — | −.07 | .08 | .34* | −.05 | 21.7%b | |||
| 5. Posttraumatic stress symptoms | — | .10 | .08 | .21 | 2.1 (2.0) | ||||
| 6. Planful problem solving | — | .51** | .41** | 7.3 (4.4) | |||||
| 7. Positive reappraisal | — | .31* | 5.9 (5.1) | ||||||
| 8. Accepting responsibility | — | 4.4 (3.4) |
Note. Posttraumatic Growth measured with the PTGI. Trait Anxiety and State Anxiety measured with the STAI. Posttraumatic Stress Symptoms measured with the IES-R. Planful Problem Solving, Positive Reappraisal, and Accepting Responsibility measured with the WAYS.
Biserial correlations.
Indicates percentage still experiencing illness.
p < .05.
p < .01.
Hierarchical Regression
Hierarchical regression analysis was performed to evaluate pretrauma, event, enduring distress, and stress-processing factors hypothesized to be associated with overall PTG. The order of entry of variables in the model was guided by Tedeschi and Calhoun's (2004) cognitive model of PTG. Trait anxiety was entered on the first step, which represented the pretrauma qualities of the individual. Trait anxiety accounted for a significant proportion of variance explained (R2 = .10, p < .05). The event factor, current illness status (i.e., resolved vs. not resolved), was entered on the second step, and did not contribute significantly to the model. The stress factor, PTSS, was entered next, and accounted for a significant increase in explained variance (ΔR2 = .16, p < .01). The stress processing factor, Positive Reappraisal, was entered on the last step, and was also associated with a significant increase in R2 (ΔR2 = .13, p < .01). Given the significant intercorrelations among the stress processing factors, we chose to enter only one into the regression equation. Positive Reappraisal was selected based on consistent findings in the literature of its association with PTG. The total model accounted for 39% of the variance in PTG, R2 = .39, adjusted R2 = .35, F(4, 53) = 8.62, p < .001 (see Table 2).
Table 2. Hierarchical Regression Predicting Posttraumatic Growth (N = 60).
| Variable | B | SE B | β | R2 | ΔR2 |
|---|---|---|---|---|---|
| Step 1: Person pretrauma | .10 | .10 | |||
| Trait anxiety | −.59 | .24 | −.31* | ||
| Step 2: Event factor | .11 | .01 | |||
| Trait anxiety | −.61 | .24 | −.32* | ||
| Current illness status | −5.06 | 6.46 | −.10 | ||
| Step 3: Stress | .27 | .16** | |||
| Trait anxiety | −.82 | .23 | −.43** | ||
| Current illness status | −2.88 | 5.93 | −.06 | ||
| Posttraumatic stress symptoms | 4.54 | 1.31 | .42** | ||
| Step 4: Stress processing | .39 | .13** | |||
| Trait anxiety | −.68 | .22 | −.36** | ||
| Current illness status | −7.30 | 5.61 | −.15 | ||
| Posttraumatic stress symptoms | 3.96 | 1.22 | .37** | ||
| Positive Reappraisal | 1.53 | .46 | .38** |
p < .05.
p < .01.
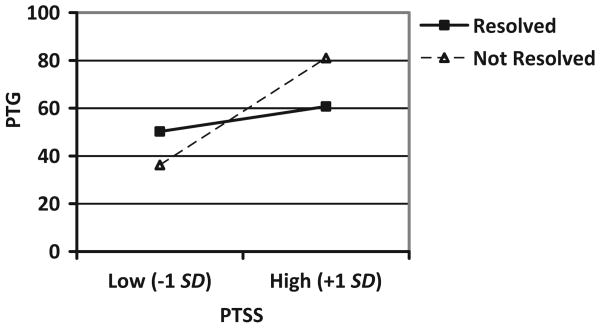
Exploratory Analysis
Following the analysis of Tedeschi and Calhoun's (2004) cognitive model of factors predictive of PTG, we sought to evaluate illness status (i.e., resolved vs. not resolved) as a moderator of the relationship between PTSS and PTG. A significant interaction between PTSS and illness status was found, F(3, 56) = 3.67, p = .01, R2 = .16 (see Table 3). Post hoc probing was conducted to interpret the significant interaction (Holmbeck, 2002). The simple effects of the interaction were examined using simple slope coefficients for individuals with high (+1 SD) and low (−1 SD) levels of PTSS. This interaction is illustrated in Figure 1. Analysis of the slopes for the two groups revealed that the slope for the not resolved group was significant, t(56) = 2.75, p < .01, whereas the slope for the resolved group was not significant. For those whose relative's illness was ongoing or not resolved, a lower level of PTSS was associated with lower PTG and a higher level of PTSS was associated with more PTG, whereas the level of PTG was similar across low and high levels of PTSS in the resolved group. Thus, the relative's current illness status moderated the relationship between PTSS and PTG.
Table 3. Hierarchical Regression Analysis for the Interaction of Variables Predicting Posttraumatic Growth.
| Variable | B | SE B | β | F | R2 |
|---|---|---|---|---|---|
| Illness statusa | 3.15 | 6.68 | .06 | 3.67* | .16 |
| Posttraumatic stress symptoms | 2.67 | 1.46 | .24 | ||
| Illness status × posttraumatic stress symptoms | 8.83 | 4.44 | .27* |
Illness status refers to resolved versus not resolved. Both predictors were centered at their means for the analysis of the interaction effect.
p ≤ .05.
Figure 1.
Interaction of posttraumatic stress symptoms and relative's current illness status to predict posttraumatic growth.
Discussion
The goal of the current study was to evaluate the associations between factors identified in Tedeschi and Calhoun's (2004) cognitive model and PTG in young adults whose relative had an illness earlier in the participants' life. Results from this study illustrate that individuals with an indirect experience with a serious illness experience PTG. As hypothesized, PTG was positively associated with ongoing distress, in the form of posttraumatic stress symptoms, greater use of problem-focused coping strategies, and lower trait anxiety. These results suggest that the factors associated with PTG in individuals who have a relative with a serious illness are similar to factors associated with PTG in individuals who themselves had a serious illness.
The positive relationship between PTG and PTSS found in this study has been documented in the literature (Best, Streisand, Catania, & Kazak, 2001; Cadell et al., 2003; Devine et al., 2010). Results from this study suggest that the relationship between PTSS and PTG for individuals whose relative has an illness may depend on the relative's illness status, as PTSS was associated with greater growth for individuals whose relative had a current illness. On average, participants were not experiencing clinical levels of posttraumatic stress, but endorsed some posttraumatic stress symptoms. It may be that a moderate amount of PTSS is necessary for ongoing processing of the traumatic event and subsequent development of PTG. However, it is possible that the positive association is simply co-occurring, with both resulting from the stressful event. Although not addressed in this study, we expect that the experience of extreme distress or meeting diagnostic criteria for Posttraumatic Stress Disorder (PTSD) would not be positively associated with the development of PTG. In contrast to PTSS, trait anxiety was found to be negatively associated with PTG among individuals who have a relative with serious or chronic illness. It is possible that individuals who are prone to higher levels of trait anxiety have pretrauma cognitive schemas that are more threat-oriented and thus the trauma confirms their already developed schema rather than challenging it, resulting in less potential for growth. This relationship warrants empirical investigation.
Consistent with Tedeschi and Calhoun's cognitive model of PTG, greater use of active coping strategies, such as planful problem solving, positive reappraisal, and accepting responsibility, was associated with greater PTG. These cognitive coping factors play a central role in the model. These findings are important in their implications for the development of intervention programs that might enhance the likelihood of PTG development. Positive reappraisal and the other coping strategies represent trainable skills that may be taught to those coping with a relative's illness or other challenging life event.
Based on prior literature (Devine et al., 2010), we expected greater PTG in individuals whose relative's illness had resolved than those whose relative's illness was ongoing. However, we did not find differences in PTG based on current illness status. On the other hand, there was an interaction between PTSS and relative's illness status in predicting PTG, suggesting that experiencing stress symptoms may facilitate greater PTG among individuals whose relative has an ongoing illness. Although different from our initial hypothesis, this result is consistent with Tedeschi and Calhoun's cognitive model, which acknowledges the influence of ongoing stress processing on promoting PTG. It is likely that mild, persistent symptoms of distress that are associated with a relative's current illness allow for continued processing, during which the potential positive outcomes from the traumatic experience may develop. This relationship between PTSS and PTG was not found for individuals whose relative's illness was resolved. This suggests that the influence of PTSS may be most salient for individuals who have a relative whose illness is not resolved. These correlational results generate hypotheses for further research.
Interpretations of these data must be done within the context of study limitations. First, the sample consisted of predominantly White college students from high income families, which may limit the generalizability of the findings to individuals from other racial or financial backgrounds. Second, the cross-sectional nature of the study prevents causal inferences from being made. Also, participants' reports of details about the relative's illness may have been less explicit or exact because of the retrospective nature of the study. Further, while the noncategorical approach has advantages, the influence of duration, intensity, and developmental timing of the relative's illness was not measured or examined but warrant consideration in future studies. Lastly, it is important to consider the limitation associated with defining the “resolved” group. There are likely notable differences in psychological outcomes, such as the experience of grief, between individuals whose relative died and those whose relative recovered from the illness. Larger studies will help tease apart these potential differences. Future research in this area should use prospective, longitudinal designs to determine causality. Additionally, a more diverse sample should be recruited to determine if these findings extend to other racial groups. Given the nature of chronic and serious illnesses, future research should explore the effects of prolonged and/or repeated trauma (e.g., ongoing medical events), as well as trauma severity, on PTSS and PTG. There should also be further investigation of individual, psychosocial, and illness-related factors that are associated with PTG.
In conclusion, results from this study suggest that individuals who have an indirect experience with serious illness experience ongoing distress as well as PTG. An individual's level of trait anxiety, PTSS, and use of active coping strategies are associated with PTG. It is possible that symptoms of posttraumatic stress facilitate the development of PTG, particularly among individuals whose relative is currently managing the demands of an ongoing serious illness. Future research should continue to elucidate the factors that are predictive of PTG among individuals who have a relative with a serious physical illness.
References
- American Psychiatric Association. Diagnostic and statstical manual of mental disorders (4th ed): DSM–IV–TR. Arlington, VA: American Psychiatric Publishing, Inc.; 2000. [Google Scholar]
- Best M, Streisand R, Catania L, Kazak AE. Parental distress during pediatric leukemia and posttraumatic stress symptoms (PTSS) after treatment ends. Journal of Pediatric Psychology. 2001;26:299–307. doi: 10.1093/jpepsy/26.5.299. [DOI] [PubMed] [Google Scholar]
- Cadell S, Regehr C, Hemsworth D. Factors contributing to posttraumatic growth: A proposed structural equation model. American Journal of Orthopsychiatry. 2003;73:279–287. doi: 10.1037/0002-9432.73.3.279. [DOI] [PubMed] [Google Scholar]
- Calhoun LG, Tedeschi RG. Facilitating posttraumatic growth: A clinician's guide. Mahwah, N. J.: Erlbaum; 1999. [Google Scholar]
- Chun S, Lee Y. The experience of posttrumatic growth for people with spinal cord injury. Qualitative Health Research. 2008;18:877–890. doi: 10.1177/1049732308318028. [DOI] [PubMed] [Google Scholar]
- Cordova MJ, Giese-Davis J, Golant M, Kronenwetter C, Chang V, Spiegel D. Breast cancer as trauma: Posttraumatic stress and posttraumatic growth. Journal of Clinical Psychology in Medical Settings. 2007;14:308–319. [Google Scholar]
- Davis CG, Wohl MJA, Verberg N. Profiles of posttraumatic growth following an unjust loss. Death Studies. 2007;31:693–712. doi: 10.1080/07481180701490578. [DOI] [PubMed] [Google Scholar]
- Devine KA, Reed-Knight B, Loiselle KA, Fenton N, Blount RL. Posttraumatic growth in young adults who experienced serious childhood illness: A mixed-methods approach. Journal of Clinical Psychology in Medical Settings. 2010;17:340–348. doi: 10.1007/s10880-010-9210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. Journal of Health and Social Behavior. 1980;21:219–293. [PubMed] [Google Scholar]
- Garnefski N, Kraaij V, Schroevers MJ, Somsen GA. Post-traumatic growth after a myocardial infarction: A matter of personality, psychological health, or cognitive coping? Journal of Clinical Psychology in Medical Settings. 2008;15:270–277. doi: 10.1007/s10880-008-9136-5. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74:797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Stuber ML. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. Journal of Consulting and Clinical Psychology. 1997;65:120–129. doi: 10.1037//0022-006x.65.1.120. [DOI] [PubMed] [Google Scholar]
- Mosher CE, Danoff-Burg S, Brunker B. Post-traumatic growth and psychosocial adjustment of daughters of breast cancer survivors. Oncology Nursing Forum. 2006;33:543–551. doi: 10.1188/06.ONF.543-551. [DOI] [PubMed] [Google Scholar]
- Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: Measuring the positive legacy of trauma. Journal of Traumatic Stress. 1996;9:455–470. doi: 10.1007/BF02103658. [DOI] [PubMed] [Google Scholar]
- Tedeschi RG, Calhoun LG. Post-traumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry. 2004;15:1–18. [Google Scholar]
- Thornton AA, Perez MA. Post-traumatic growth in prostate cancer survivors and their partners. Psycho-Oncology. 2006;15:285–296. doi: 10.1002/pon.953. [DOI] [PubMed] [Google Scholar]
- Weiss D, Marmar C. The Impact of Event Scale-Revised. In: Wilson T, Keane J, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. pp. 399–411. [Google Scholar]
- Weiss T. Correlates of posttraumatic growth in husbands of breast cancer survivors. Psycho-Oncology. 2004;13:260–268. doi: 10.1002/pon.735. [DOI] [PubMed] [Google Scholar]
- Wong ML, Cavanaugh CE, MacLeamy JB, Sojourner-Nelson A, Koopman C. Posttraumatic growth and adverse long-term effects of parental cancer in children. Families, Systems, & Health. 2009;27:53–63. doi: 10.1037/a0014771. [DOI] [PubMed] [Google Scholar]