Abstract
Multivalent ligands with delta/mu opioid agonist and NK1 antagonist activities have shown promising analgesic potency without detectable sign of toxicities, including motor skill impairment and opioid-induced tolerance. To improve their biological activities and metabolic stability, structural optimization was performed on our peptide-derived lead compounds by introducing 2′, 6′-Dimethyl-L-Tyrosine (Dmt) instead of Tyr at the first position. The compound 7 (Dmt-D-Ala-Gly-Phe-MetPro-Leu-Trp-NH-[3′,5′-(CF3)2-Bzl]) showed improved multivalent bioactivities compared to those of the lead compounds, had more than 6 h half-life in rat plasma, and significant antinociceptive efficacy in vivo. The NMR structural analysis suggested that Dmt1 incorporation in compound 7 induces the structured conformation in the opioid pharmacophore (N-terminus), and simultaneously shifts the orientation of the NK1 pharmacophore (C-terminus), consistent with its affinities and activities at both opioid and NK1 receptors. These results indicate that compound 7 is a valuable research tool to seek a novel analgesic drug.
Keywords: analgesics; bifunctional peptide derivatives; 2′, 6′-Dimethyl-L-Tyrosine; DPC micelle; opioid induced tolerance; opioid receptor agonist; neurokinin-1 receptor antagonist; NMR structure
Introduction
The treatment of pain, especially prolonged and neuropathic pain is a major challenge and millions of people suffer from such pain every day. Opioids remain the mainstay for the treatment of these pain states. However, sustained opioid treatment is associated with serious unwanted effects including somnolence and mental clouding, nausea and vomiting, and constipation. Analgesic tolerance to opioid therapy also develops in many patients with continued use. These side effects significantly decrease the patients' quality of life. The mechanisms for these side effects are still largely unclear. Prolonged pain states lead to neuroplastic changes in both ascending and descending pathways in the spinal column in which there is both an increased release of neurotransmitters (e.g. substance P) that enhance pain and increased expression of the corresponding receptors for those newly released pain-promoting ligands.1-3 Current treatment of prolonged pain generally can only modulate pain and cannot counteract against these induced neuroplastic changes. Thus, it is not surprising that current analgesic drugs do not work well in these pathological conditions.
Recently, co-administrations of a δ/μ opioid agonist and a neurokinin 1 (NK1) antagonist have been tested to study the facilitatory role of the substance P-NK1 system in opioid signal transmission. This combination elucidates several important biological effects such as enhanced potency in acute pain models4, and prevention of opioid-induced tolerance in chronic tests using rats.5 Another study reported that NK1 knockout mice did not show the rewarding properties of morphine.6 Thus, the combination of an agonist at the opioid receptors, and an antagonist at NK1 receptors may have synergistic effects in the treatment of prolonged pain states that involve enhanced substance P activity. Drug cocktails have limitations as therapeutics because of poor patient compliance, complications in drug metabolism, distribution and possible drug-drug interactions. We have taken a new approach to combine these two activities in one ligand which should have simple metabolic and pharmacokinetic properties. The desirable activities of our ligand would include potent analgesic affects in both acute pain and in neuropathic pain states without the development of tolerance.7 Our working drug-design strategy is based on the adjacent and overlapping pharmacophores concept, in which the opioid agonist pharmacophore is incorporated at the N-terminus and the NK1 antagonist pharmacophore locates at the C-terminus of a single peptide derived molecule. The opioid pharmacophore of these chimeric peptides were designed based on the sequence of Biphalin and DADLE,8, 9 while the structures from 3′,5′-(bistrifluoromethyl)-benzyl ester of N-acylated tryptophans were modified with amino acid residues into the NK1 antagonist pharmacophore.10-12 The important fifth residue works as an address region for both pharmacophores as well as a hinge between them (Figure 1).9, 13-16 It should be emphasized that the designed multivalent chimeric molecules have additional advantages over a cocktail of individual drugs for easy administration, a simple ADME property and no drug-drug interaction. A higher local concentration is also expected than in the co-administration of two drugs, since the expressions of the NK1 and opioid receptors show a significant degree of anatomical overlap in the central nervous system, leading to synergies in potency and efficacy.17-19 In fact, our previous results showed that the lead bifunctional compounds, TY005 (Tyr1-D-Ala2-Gly3-Phe4-Met5-Pro6-Leu7-Trp8-O-[3′,5′-Bzl(CF3)2]) and TY027 (1: Tyr1-D-Ala2-Gly3-Phe4-Met5-Pro6-Leu7-Trp8-[NH-3′,5′-Bzl(CF3)2]), have been shown to reverse neuropathic pain in a rodent model with blood brain barrier permeability, no sign of opioid-induce tolerance, and no development of reward liability, validating our hypothesis that a single compound possessing opioid agonist/NK1 antagonist activities is effective against neuropathic pain.7, 20-23 The structural differences between the two lead compounds were in their C-terminus, which was crucial for both opioid and NK1 activities.9 The C-terminal ester (TY005) has a short half life in rat plasma (about 1 min) while C-terminal amide (1) had a half-life of 4.8 hours. The substitution of Met5 with Nle (2) resulted in improved stability (the half-life was more than 6 hours) with nearly equipotent activities at both opioid and NK1 receptors compared to 1.14
Figure 1.
Sequences of multivalent ligands.
In order to perform a lead-to-drug-candidate structural optimization, we sought further improvement in the biological activities and metabolic stability. Extensive studies previously indicated that the substitution of 2′, 6′-dimethyl-L-tyrosine (Dmt) for Tyr1 in opioid peptides produces, in general, a significant increase in opioid receptor affinity,24-26 and thus this modification could be a critically effective strategy to improve opioid agonist activities in the bifunctional peptides, although the influence of Dmt1-introduction for the NK1 activity was not known. Thus, an SAR study was initiated by the incorporation of Dmt1 in compound 2 followed by modification on the C-terminal and fifth position, to optimize both opioid and NK1 activities. Further elucidation of the biological and conformational effect of Dmt1-incorporation was performed using the NMR structure based on distance and φ dihedral angle constraint information.
The bifunctional peptide derivatives 3-7 were synthesized using procedures previously described.13, 15 The biological activities of 3-7 were extensively evaluated on our well-established radioligand binding assays, guanosine 5′-(γ-thio) triphosphate (GTPγS) binding assays, and isolated tissue-based functional assays using guinea pig ileum (GPI) and mouse isolated vas deferens (MVD) tissues.9, 13, 15 The metabolic stabilities of compounds were tested by incubation in rat plasma at 37°C.14 The in vivo antinociceptive potency of the peptide derivative was confirmed using non-injured rats.20, 22, 23
Results and Discussion
Biological activities
The SAR study was initiated by incorporating Dmt at the first position of 2 to yield 3 (Figure 1). Although this modification was made in the opioid-agonist pharmacophore, 3 showed a 10-fold decrease in binding affinity at the human NK1 (hNK1) receptor compared to that of 2, indicating the influence of the N-terminus (Table 1). This implies that the first residues of the peptide sequences work as an address region for the hNK1 receptor. It should be noted that the Dmt1-introduction induced relatively smaller shifts in binding affinity for the rat NK1 (rNK1) receptor, as well as in the functional activity using the GPI (Table 2). 3 had improved binding affinity at the μ opioid receptor (MOR) in the low nanomolar range, while the affinity at the δ opioid receptor (DOR) was 10-fold less than that of 2. This compound has about 9 fold selectivity for the -opioid receptors. Compound 4, which has an N-methylated C-terminus, showed high affinities for both the δ- and μ-opioid receptors, implying that the C-terminus modification has a strong influence on the opioid activities (Ki = 0.46 and 1.8 nM, respectively; Table 1). Thus, the two pharmacophores in our bifunctional compounds do not work independently but interact with each other as a single ligand which can enhance binding at both the opioid and NK1 receptors. Consistent with the binding affinities, the functional activities of 4 in conventional isolated-tissue based assays were improved from those of 2 (14 and 110 nM for MVD and GPI assays, respectively; Table 2). However, the binding affinity of 4 for the hNK1 receptor was not as potent as 2 (Ki = 0.21 nM). We next examined the mono-trifluoromethyl derivative of 3 (5, Figure 1). Compound 5 exhibited decreased NK1 binding affinities (Ki = 1.0 and 140 nM for human and rat NK1 receptors, respectively) and lower functional activity (Ke = 24 nM) compared to those of 3 (Table 1). The affinities of 5 were better at opioid receptors similar to those of 3. The introduction of electron-dominating methoxy groups at the C-terminus was also tested (6, Figure 1). Interestingly, compound 6 had the best opioid affinities among the tested ligands 3-7 with subnanomolar Ki values both at the δ- and μ-opioid receptors (0.15 and 0.34 nM, respectively). GTPγS binding assays (Table 3) also demonstrated that 6 had potent opioid activities at both the δ- and μ- opioid receptors (EC50 = 0.60 and 0.72 nM, respectively; Table 3). Higher potency for opioid activities also was observed in the isolated tissue bioassays using the MVD and GPI (Table 2), suggesting the importance of modification at C-terminus for both μ- and δ- opioid agonist activities. However, the NK1 affinities of 6 were decreased (Ki = 0.95 and 320 nM for human and rat NK1 receptors, respectively).
Table 1.
Binding affinities of bifunctional peptide derivatives at δ/μ opioid receptors and NK1 receptors
| no | hDORa, [3H]DPDPE b |
rMORa, [3H]DAMGO c |
Ki(μ) /Ki(δ) |
hNK1d, [3H]Substance Pe |
rNK1d, [3H]Substance Pf |
Ki(hNK1) /Ki(rNK1) |
||||
|---|---|---|---|---|---|---|---|---|---|---|
| LogIC50g | Ki (nM) | LogIC50g | Ki (nM) | LogIC50g | Ki (nM) | LogIC50g | Ki (nM) | |||
| 1 h | −8.84 ± 0.07 | 0.66 | −7.44 ± 0.05 | 16 | 24 | −10.91 ± 0.10 | 0.0065 | −7.61 ± 0.03 | 7.3 | 1100 |
| 2 i | −8.67 ± 0.05 | 1.0 | −7.17 ± 0.07 | 32 | 32 | −11.57 ± 0.59 | 0.0028 | −7.68 ± 0.03 | 6.8 | 2400 |
| 3 | −7.62 ± 0.10 | 11 | −8.60 ± 0.03 | 1.2 | 0.11 | −9.78 ± 0.04 | 0.075 | −7.28 ± 0.06 | 13 | 170 |
| 4 | −9.01 ± 0.11 | 0.46 | −8.48 ± 0.1 | 1.8 | 3.9 | −9.33 ± 0.04 | 0.21 | −7.51 ± 0.08 | 11 | 52 |
| 5 | −8.07 ± 0.06 | 4.1 | −8.82 ± 0.04 | 0.74 | 0.18 | −8.66 ± 0.04 | 1.0 | −6.41 ± 0.04 | 140 | 140 |
| 6 | −9.50 ± 0.11 | 0.15 | −9.20 ± 0.05 | 0.34 | 2.3 | −8.70 ± 0.03 | 0.95 | −6.05 ± 0.03 | 320 | 340 |
| 7 | −9.42 ± 0.08 | 0.18 | −8.37 ± 0.15 | 2.0 | 11 | −10.74 ± 0.04 | 0.0079 | −8.29 ± 0.35 | 2.3 | 290 |
| Biphalin j | 2.6 | 1.4 | 0.54 | |||||||
| L-732,138 | −8.83 ± 0.02 | 0.73 | −6.40 ± 0.03 | 130 | 180 | |||||
Competition analyses were carried out using membrane preparations from transfected HN9.10 cells that constitutively expressed the DOR and MOR, respectively.
Kd = 0.45 ± 0.1 nM.
Kd = 0.50 ± 0.1 nM.
Competition analyses were carried out using membrane preparations from transfected CHO cells that constitutively expressed rat or human NK1 receptors.
Kd = 0.16 ± 0.03 nM.
Kd = 0.40 ± 0.17 nM.
The logIC50 ± standard error are expressed as logarithmic values determined from the non linear regression analysis of data collected from at least two independent experiments performed in duplicate. The Ki values are calculated using the Cheng and Prusoff equation to correct for the concentration of the radioligand used in the assay.
Reference.13
Reference.14
Reference.38
Table 2.
Functional assay results for bifunctional peptide derivative ligands at opioid and Substance P receptors
| No | Opioid agonist | Substance P antagonist |
|
|---|---|---|---|
| MVD (δ) | GPI (μ) | GPI | |
| IC50 (nM)a | IC50 (nM)a | Ke (nM)b | |
| 1 c | 15 ± 2 | 490 ± 29 | 10 ± 2 |
| 2 d | 14 ± 2 | 460 ± 160 | 10 ± 3 |
| 3 | 2.3 ± 0.6 | 68 ± 10 | 13 ± 4 |
| 4 | 14 ± 1 | 110 ± 27 | 6.1 ± 0.8 |
| 5 | 8.7 ± 2.5 | 22 ± 2 | 14 ± 6 |
| 6 | 8.8 ± 2.1 | 23 ± 3.6 | 24 ± 2 |
| 7 | 1.8 ± 0.6 | 19 ± 5 | 7.5 ± 0.5 |
| Biphalin | 2.7 ± 1.5 | 8.8 + 0.3 | |
| L-732,138 | 250 ± 87 | ||
Concentration at 50% inhibition of muscle contraction at electrically stimulated isolated tissues (n = 4).
Inhibitory activity against the Substance P induced muscle contraction in the presence of 1 μM naloxone, Ke: concentration of antagonist needed to inhibit Substance P to half its activity (n = 4).
Reference.13
Reference.14
Table 3.
Opioid agonist functional activities in [35S]GTPγS binding assays
| No | hDORa | rMORa | ||||
|---|---|---|---|---|---|---|
| LogEC50b | EC50 (nM)c | Emax (%)d | LogEC50b | EC50 (nM)c | Emax (%)d | |
| 1 e | −8.07 ± 0.11 | 8.6 | 60 ± 2 | −8.16 ± 0.17 | 7.0 | 51 ± 3 |
| 2 f | −8.30 ± 0.09 | 5.0 | 120 ± 3 | −7.74 ± 0.14 | 18 | 66 ± 3 |
| 3 | −9.90 ± 0.34 | 0.10 | 41 ± 7 | −9.24 ± 0.14 | 0.57 | 46 ± 2 |
| 4 | −8.15 ± 0.22 | 2.3 | 49 ± 2 | −8.10 ± 0.19 | 8.0 | 29 ± 1 |
| 5 | −9.36 ± 0.16 | 0.20 | 50 ± 3 | −9.08 ± 0.28 | 0.83 | 17 ± 1 |
| 6 | −9.24 ± 0.17 | 0.60 | 42 ± 2 | −9.02 ± 0.15 | 0.72 | 48 ± 2 |
| 7 | −9.01 ± 0.17 | 1.0 | 94 ± 4 | −7.54 ± 0.27 | 29 | 72 ± 4 |
| Biphalin | −8.95 ± 0.17 | 1.1 | 83 | |||
| DAMGO | −7.44 ± 0.19 | 37 | 150 | |||
Expressed from HN9.10 cell.
The log EC50 ± standard error are logarithmic values determined from the non-linear regression analysis of data collected from at least two independent experiments performed in duplicate.
Anti-logarithmic value of the respective EC50.
[Total bound − Basal]/[Basal − Non-specific] × 100
Reference.13
Reference.14
Finally, we introduced Dmt1 on compound 1 which has a Met in the fifth position where the two pharmacophores are connected (7, Figure 1). In contrast with compound 3 with a Nle5 residue, the binding affinity of 7 at the hNK1 receptors was as potent as those of 1 and 2. Compound 7 also showed potent antagonist activity against substance P stimulation in the GPI tissue in the presence of naloxone. At the opioid receptors, the affinities of 7 were improved from those of 1 and 2, showing subnanomolar opioid affinities at the DOR and a potent Ki value at the MOR (Ki = 0.18 and 2.0 nM, respectively) (Table 1). The observed high opioid affinities of 7 were maintained in the GTPγS binding assays with highly efficacious EC50 and Emax values (94 and 72 % for DOR and MOR, respectively, Table 3). The opioid activities of 7 also were improved from those of 1 by 8- and 26-fold in the isolated tissue bioassays using the MVD and GPI, respectively (IC50 = 1.8 and 19 nM, respectively). These results clearly suggest that Nle, which is generally considered as a bioisostere of Met, does not necessarily produce similar activities as derivatives with Met. It is also demonstrated that the fifth position is important for affinities and activities of δ/μ opioid/NK1 bifunctional peptide derivatives possessing Dmt1.
Considering all the biological results for the opioid and NK1 receptors, 7 was found to have the most improved bifunctional affinities and activities compared to the lead compounds 1 and 2.
In vitro metabolic stability
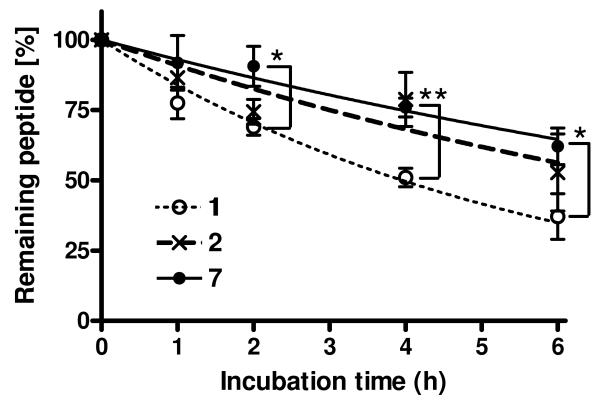
For further biological characterization, the metabolic stability of 7 was tested by incubation in rat plasma at 37 °C.14 The degradation curve of 7 was significantly improved from that of 1, and was as stable as that of 2, suggesting that Dmt1-introduction (7) and Nle5-incorporation (2) in 1 had a similar positive effect against recognition by degrading enzymes (Figure 2). This improved metabolic stability together with the excellent bifunctional activities motivated us to perform in vivo animal studies using compound 7, to confirm its in vivo analgesic efficacy.
Figure 2.
Comparison of the in vitro metabolic stability for 114 (open circle) , 214 (crosses) and 7 (filled circle) incubated in rat plasma at 37°C. Calculated half lives of peptide derivatives (T1/2) were 4.8 h for 1 and > 6 h for 2 and 7. The samples were tested in three independent experiments (n = 3) and the mean values were used for the analysis with the SD. Statistical significance was determined by Kruskal-Wallis test followed by Tukey's test. Asterisks denote significant differences (* p < 0.05; ** p < 0.01).
In vivo antinociceptive effect
Acute intrathecal (i.t.) injection of 7 was given to normal rats, to investigate its antinociceptive properties. A dose of 10 μg of 7 resulted in paw withdrawal latencies of 28 ± 2.6 s, which is significantly higher when compared to baseline values (23 ± 0.9 s) or vehicle treatment (20 ± 2.2 s) alone (p < 0.05; Figure 3). The antinociceptive effect of 7 over baseline at 60 min is 52 ± 22 % whereas vehicle is 7.0 ± 5.7 % over baseline following i.t. administration.23 As reported previously,21 our preliminary result showed that the observed peak effect of 1 occurred between 15 and 30 min after the i.t. injection using the same animal model; in this study compound 7 produced maximal antinociception at 60 min, when 1 showed no significant efficacy. When compared to i.t. morphine, the time of peak effect for similar doses is different (20 min for morphine and 60 min for 7) though the efficacy is similar. These results may have relevance to the observed stabilities of 7 in rat plasma, although existing peptidases in the central nervous system may not be the same as those in plasma.
Figure 3.

Animals underwent intrathecal cannulation and were allowed 5-7 days recovery. Baseline paw withdrawal latencies were obtained 30 min prior to compound or vehicle administration (n = 11) and rats then randomized to a treatment group. 7 (10 μg in 5 μL, n=5) produced maximal antinociception 60 min after the i.t. injection. *p < 0.05 compared to both baseline and vehicle (n=6) paw withdrawal latencies.
In conclusion, 7 showed excellent bioactivities for both the opioid receptors and the NK1 receptors, effective antinociceptive potential in vivo, and had longer half-life than the lead compound 1.
1H-NMR studies in membrane-mimicking circumstances for conformational calculation
In order to elucidate the biological and conformational effect of Dmt1-incorporation, we next performed NMR structural analysis of 7. In fact, numerous SAR studies on Dmt1-enkephalin derivatives have been reported, e.g. 25-27 but little is known about the conformational affect that may result from a Tyr1-to-Dmt1 substitution. Thus, the conformation of 7 in membrane-mimicking micelles was compared with the previously obtained NMR structure of 1 using the same conditions and procedures,13 to evaluate any conformational difference.
The two-dimensional 1H–NMR studies of 7 including total correlation spectroscopy (TOCSY), double quantum filtered correlation spectroscopy (DQF-COSY) and nuclear Overhauser enhancement spectroscopy (NOESY) were performed in pH 4.5 buffer (45 mM CD3CO2Na/HCl, 1 mM NaN3, 90% H2O/10% D2O) with a 40-fold excess of perdeuterated dodecylphosphocholine (DPC) micelles. DPC is a widely used lipid-like surfactant to evaluate the solution NMR structures of membrane-bound proteins and peptides.e.g. 13, 28, 29, 30 The important relevance of membrane-bound conformations of ligands for GPCRs and their biological activities have been extensively discussed recently.e.g. 13, 30, 31 All 1H chemical shift assignments of 7 are found in the Supporting Information.
Conformational analysis
The total number of used nuclear Overhauser enhancement (NOE) restraints for structural calculation of 1 was 155, while that of 7 was 169 including 62 intraresidual NOEs, 67 sequential NOEs, 49 medium-range NOEs (2-4 residues) and 5 long-range NOEs (> 4 residues). The 1H-NMR spectra in 7 showed a negligible amount of the minor cis/trans rotamer at the Pro6 residue. In the structural calculation, the Met5-Pro6 bond of the major rotamer was fixed in the trans configuration based on the observation of Met5 Hα to Pro6 Hδ sequential NOEs together with the absence of sequential Met5 Hα-Pro6 Hα NOEs. The restrained molecular dynamics calculations32, 331 were performed based on the observed NOE restraints, and the calculated 20 lowest-energy structures from this analysis were used for the structural analysis of 7. The calculated 20 structures for 7 showed a very small number of violations for total NOE restraints, maximum NOE distances, and restraint energy based on the Amber force field (details are provided in the Supporting Information).
The conformational effect of Dmt1-incorporation in place of Tyr1 was observed on the obtained NMR structures of 7 in the presence of membrane-mimicking DPC micelles. The calculated superimposed structures of 7 for the alignments on the entire molecule showed smaller root mean square deviation (rmsd) values than those of 1 (0.86 for backbone atoms and 1.91 for all heavy atoms; Table 4 and Figure 5A). Especially, those for the alignment on the residues 1-4 were smaller, indicating that the introduction of Dmt1, possessing two methyl groups on its phenyl ring, provided a more defined N-terminus conformation compared to that of 1 (rmsd = 0.55 for backbone atoms and 1.33 for all heavy atoms). For the C-terminal half of 7, the structural definition of backbone atoms also were improved, while non-hydrogen atoms were rather poorly-defined compared to those of 1 (rmsd = 0.19 for backbone atoms and 1.27 for all heavy atoms).
Table 4.
Atomic rmsd values (Å) for the final 19 conformers compared to the most stable conformer of bifunctional peptide derivatives.
| 1a | 7 | |
|---|---|---|
| Backbone atoms (N, Cα, C′) | ||
|
| ||
| Calculated on whole molecule | 1.14 ± 0.43 | 0.86 ± 0.21 |
| Calculated only on 1-4 res. | 1.05 ± 0.63 | 0.55 ± 0.28 |
| Calculated only on 5-8 res. | 0.45 ± 0.38 | 0.19 ± 0.10 |
|
| ||
| all non-hydrogen atoms | ||
|
| ||
| Calculated on whole molecule | 2.09 ± 0.64 | 1.91 ± 0.54 |
| Calculated only on 1-4 res. | 2.16 ± 0.98 | 1.33 ± 1.01 |
| Calculated only on 5-8 res. and C-terminus | 1.02 ± 0.25 | 1.27 ± 0.41 |
Reference.13
Figure 5.
(A) Ensembles of the best 20 calculated structures in 40-fold DPC micelle / pH 4.5 buffer for 113 (left) and 7 (right) with the lowest restraint energy, aligned on backbone atoms of residues (a) 1-8. The aligned structures are illustrated the backbone atoms with C-terminal benzyl moiety (purple). (b) The most stable conformers are shown with all heavy atoms (C, N, O and F). The superimposed images of obtained NMR structure of 7 (red) with the NMR structure of 1 (blue) at the lowest restraint energy for opioid pharmacophore (residues 1-4; B) and for NK1 pharmacophore (residues 6-C-terminus; C).
The better defined conformation of 7 in the N-terminal region compared to 1 was also confirmed based on the analysis using backbone φ and ψ torsion angles. The residues 2 and 3 in the 20 best structures of 1 had rather scattered plots in the Ramachandran diagram, while those in 7 were highly aggregated (Figures 6A and B). The φ and ψ angular order parameters34 of residues 2 and 3 were close to one in 7, but not in 1 (Figures 6C and D). The Dmt1-introduction also changed a number of β-turn structural elements in the N-terminus. The NMR structure of 1 had two β-turns at the residues 2 to 5 and 6 to the C-terminus.13 These two turn structures also were observed in 7 (Table 5). Additionally, 12 out of 20 of the best structures of 7 showed a distance between the Cα of Tyr1 and the Cα of Phe4 within 7 Å, whereas 1 had the same β-turn structural elements only in three structures. Thus, the N-terminus of 7 manifested the better-defined conformation with more definitive β-turns compared to that in 1.
Figure 6.
The Ramachandran φ,ψ plots for (A) 1 and (B) 7 for residues 2-7 of 20 final structures. Angular order parameters32 for φ (C) and ψ (D) angles calculated from the 20 final structures for 113 (open circle) and 7 (filled square), respectively. For calculating the ψ angles of Trp8, the nitrogen atoms of C-terminal benzyl amide were used instead of N (i + 3), respectively.
Table 5.
Number of β-turn structural elements and the distance between alpha carbons of i th and (i + 3)rd residues.a
| 1b | 7 | |||
|---|---|---|---|---|
| Residues | number of structures with β-turns |
distance (Å) |
number of structures with β-turns |
distance (Å) |
| C1α-C1a | 3 | 7.86 ± 1.21 | 12 | 6.85 ± 0.64 |
| C2α-C5a | 20 | 4.95 ± 0.71 | 20 | 5.93 ± 0.35 |
| C6α-Bzl | 19 | 6.32 ± 0.43 | 20 | 5.45 ± 0.21 |
Out of the best 20 calculated structures. The distance is the mean distance between two alpha carbons ± standard deviation (SD). The sequences with less than 7 Å distance between alpha carbons of i th and (i + 3) rd residues without helical structure were considered as a β-turn.41 Bzl stands for the benzyl moiety at the C-terminus.
Reference.13
These results indicate that 7 clearly has a more structured conformation than 1, especially close to the site of the Dmt1-incorporation, probably due to steric and lipophilic differences between Dmt and Tyr. The introduction of two methyl groups in the first residue plays a crucial role in the molecular structure of opioid pharmacophore, suggesting shifts of affinities and efficacies at the opioid receptors, as observed.
The lowest energy structures of 1 and 7 were next superimposed on alignment with the backbone atoms, to clarify structural differences due to the Dmt-substitutive effect at the first position. The backbone conformation of the opioid pharmacophore of the two molecules showed similar conformations with good overlap that was further improved when the superimposition was performed for the NK1 pharmacophore which showed nearly complete overlap (Figure 5B). It is interesting to note that when the alignment was made for the opioid pharmacophores of 1 and 7, the corresponding NK1 pharmacophores was directed differently in 3D space and thus showed almost no overlap. This result indicates that the Tyr1-to-Dmt1 substitution changes the relative orientation of two pharmacophores which work as an address region with each other, through a conformational change at the fifth residue. The important implication of these results is that the Dmt1 introduction induces orientational shifts of the C-terminus, and these shifts may lead to additional changes in affinities and efficacies at both opioid and NK1 receptors, depending on the amino acid residue at the fifth residue.
Paramagnetic Broadening Studies on 1H NMR
The interactive mode between the bifunctional compound 7 and the cell membrane was examined in order to investigate the effect of Dmt1-substitution at the place of Tyr1 using pseudo-membrane conditions. Mn2+ was used as a paramagnetic ion to eliminate the resonance intensities of solvent-exposed protons in the DPC micelles, based on spin system in TOCSY spectra.13, 16
Interestingly, two major differences were found for the conformations of 7 and 113 (Figure 7 and Supporting Information). First, a cross-peak of NH and Hα protons in D-Ala2 was observed for 7, but not for 1, suggesting that the backbone protons in D-Ala2 of 7 were buried inside of the micelle, while those of 1 were mostly exposed to its surface. This suggests that the Dmt1-incorporation increased the lipophilicity of the opioid pharmacophore, especially around residue 2, to strengthen peptide-membrane interactions. Second, the aromatic side-chain protons of Trp in 1 were mostly maintained after the Mn2+ addition, whereas no corresponding cross-peaks were observed for 7, suggesting that the side-chain of Trp in 1 is located deeper in the micelle than in 7. Thus, Dmt1-incorporation affects the compound-membrane interactions for the side-chains of the C-terminal half, although it is away from the substitution site.
Figure 7.
The paramagnetic effects on TOCSY Spectra of 7. 7 with DPC micelles (top row) and with 200 M Mn2+ (bottom). Preserved resonances (labeled) are in a phase not missed by the phase-specific radical probe (Mn2+). Spectra were compared from the same noise level. X9 represents the cross-peaks derived from the corresponding aromatic protons of benzyl moiety.
As a result, the Tyr1-to-Dmt1 substitution changed backbone conformation of opioid pharmacophore which is modified with an improved β-turn conformation, and strengthened interactions between the ligand and membranes. Whereas, the NK1 pharmacophores of 1 and 7 showed similar backbone conformations, the conformation shift was observed primarily in their side-chains. Therefore, this substitution has a direct structural effect on the opioid pharmacophore, and changes the orientation of NK1 pharmacophore at the fifth residue, with the small conformational shifts in the NK1 pharmacophore. These structural shifts due to the Tyr1-to-Dmt1 substitution may have a strong relationship with the ligand-GPCR docking process assisted by cell-membrane, to critically modulate the affinity and activity of the ligand.
Conclusion
In the search for a drug candidate as a novel type of analgesic, optimization on the C-terminus and fifth residue of a lead compounds 1 and 2 were performed. Among the synthesized derivatives, 7, possessing a Dmt1, a Met5 and NH-[3′,5′-(CF3)2-Bzl] at the C-terminus, was found to have improved opioid agonist activities while maintaining NK1 antagonist activity. Based on the NMR structural analysis in a membrane-mimicking environment, lipophilic and steric effects of a Dmt1-residue induce changes in the conformation and in the membrane-ligand interactive mode, not only in the opioid pharmacophore region, but also in the NK1 pharmacophore region which is some distance from the substitution site. The important finding from these results is that the two pharmacophores do not work independently, but concertedly, and their conformational “balance” has a crucial effect on their biological behaviors. Moreover, 7 showed significant antinociceptive activity in vivo and more than 6 h half-life in rat plasma. These results indicate that compound 7 could be considered as a valuable research tool to develop a novel analgesic drug. Further investigations on 7 are presently underway in our laboratory for further in vivo biological characterization.
Experimental Section
Materials
All amino acid derivatives, coupling reagents and resins were purchased from EMD Biosciences (Madison, WI), Bachem (Torrance, CA), SynPep (Dublin, CA) and Chem Impex International (Wood Dale, IL). Perdeuterated DPC was purchased from C/D/N Isotopes (Quebec, Canada). ACS grade organic solvents were purchased from VWR Scientific (West Chester, PA), and other reagents were obtained from Sigma-Aldrich (St. Louis, MO) and used as obtained. Myo-[2-3H(N)]-inositol; [Tyrosyl-3,5-3H(N)] D-Ala2-Mephe4-glyol5-enkephalin ([3H]-DAMGO); [Tyrosyl-2,6-3H(N)]-(2-D-Penicillamine, 5-D-Penicillamine)enkephalin ([3H]-DPDPE); [3H]-substance P; and [35S]-GTPγS were purchased from Perkin Elmer (Wellesley, MA). Bovine serum albumin (BSA), protease inhibitors, Tris and other buffer reagents were obtained from Sigma (St. Louis, MO). Culture medium, Penicillin/ Streptomycin and fetal calf serum (FCS) were purchased from Invitrogen (Carlsbad, CA).
Preparation and Characterization of peptides
The peptides were prepared and purified using the same method as described previously.9, 13, 15 All the obtained final peptides showed > 98% purity. The purified peptides were characterized by high-resolution mass spectroscopy, TLC, analytical HPLC and 1H-NMR (Supporting Information). Sequential assignment of proton resonances was achieved by 2D-TOCSY NMR experiments.35 High-resolution MS were taken in the positive ion mode using FAB methods at the University of Arizona Mass Spectrometry Facility. TLC was performed on aluminum sheets coated with a 0.2 mm layer of silica gel 60 F254 Merck using the following solvent systems: (1) CHCl3 : MeOH : AcOH = 90 : 10 : 3; (2) EtOAc : n-BuOH : water : AcOH = 5 : 3 : 1 : 1; and (3) n-BuOH : water : AcOH = 4 : 1 : 1. TLC chromatograms were visualized by UV light and by ninhydrin spray followed by heating (hot plate). Analytical HPLC was performed on a Hewlett Packard 1100 or Hewlett Packard 1090m with Waters NOVA-Pak C-18 column (3.9 × 150 mm, 5 μm, 60Å) or Vydac 218TP104 C-18 column (4.6 × 250 mm, 10 μm, 300 Å). 1H-1D-NMR spectra were obtained on Bruker DRX-500 or DRX-600 spectrometer. 2D-TOCSY and 2D-NOESY NMR spectra were performed on a Bruker DRX-600 spectrometer equipped with a 5mm Nalorac triple-resonance single-axis gradient probe. The NMR experiments were conducted in DMSO-d6 solution at 298K. Spectra were referenced to residual solvent protons as 2.49 ppm. The processing of NMR data was performed with the XwinNmr software (Bruker BioSpin, Fremont, CA). In the TOCSY experiments, the TPPI mode36 with MLEV-17 Mixing Sequence37 were used with a mixing time of 62.2 ms, at a spin-lock field of 8.33 kHz. The mixing time for the NOESY spectra was 450 ms for all peptide derivatives. All 2D spectra were acquired in the TPPI mode with 2k complex data points in t2 and 750 real data points in t1, and the spectral processing using shifted sine bell window functions in both dimensions.
In Vitro Stability of peptide derivatives in Rat Plasma.14, 16
Stock solutions of the compound (50 mg/mL in DMSO) were diluted 1000-fold into rat plasma (Lot 24927, Pel-Freez Biologicals, Rogers, AK) to give an incubation concentration of 50 μg/mL of each petpide. All samples were incubated at 37 °C and 200 μL of aliquots were withdrawn at 1 h, 2 h, 4 h, and 6 h. Then 300 μL of acetonitrile was added and the proteins were removed by centrifugation. The supernatant was analyzed for the amount of remaining parent compound by HPLC (Hewlett Packard 1090m with Vydac 218TP104 C-18 column; 4.6 × 250 mm, 10 μm, 300 Å). The samples were tested in three independent experiments (n = 3) and the mean values were used for the analysis with SD.
NMR Spectroscopy in DPC amphipathic media and Conformational Structure Determination
All the conformational determinations were performed by the same methods as previously described,13, 28, 29 based on the NMR spectra using a Bruker DRX600 600 MHz spectrometer.
Briefly, the samples were prepared by dissolving the peptide (3.5 mM) in 0.5 mL of 45 mM sodium acetate-d3 buffer (pH 4.5) containing 40 equivalents of DPC-d38 and 1 mM sodium azide (90% H2O/10% D2O) followed by sonication for 5 min. DQF-COSY, NOESY38 (mixing time = 450 ms) and TOCSY spectra35 (MLEV-17 mixing time = 62.2 ms, spin-lock field = 8.33 kHz) were acquired using standard pulse sequences at 310 K. Coupling constants (3JNH-Hα) were measured from 2D DQF-COSY spectra by analysis of the fingerprint region with a curve-fitting using 5-parameter Levenberg-Marquardt nonlinear least-squares protocol to a general antiphase doublet.
For conformational structure determination, the volumes of the assigned cross-peaks in the 2D NOESY spectrum were converted into upper distance bounds of 3.0, 3.8, 4.8, or 5.8 Å. In addition to the distance constraints, φ dihedral angle constraints derived from 3JHN-Hα coupling constants were set to between −90 and 40° for 3JHN-Hα< 6 Hz and to between −150 and −90° for 3JHN-Hα> 8 Hz. Dihedral angle constraints of 180 ± 5° for peptide bonds (ω) also were used to maintain the planarity of these bonds. Simulated annealing molecular dynamics analysis was done for all the peptides to obtain an ensemble of NMR structures using NOE-derived distance constraints and dihedral angle (φ) constraints, and using the DGII39 program within the software package Insight II 2000 (Accelrys Inc., San Diego, CA). The final 20 conformations with the lowest energies were used for the analysis. All calculations were performed on a Silicon Graphics Octane computer.
Radioligand Labeled Binding Assay, [35S]GTP-γ-S Binding Assay, GPI and MVD in Vitro Bioassay
The methods were carried out as previously described.9, 13, 15 Briefly, the evaluation of the binding affinities of the synthesized bifunctional peptide derivatives at the human δ-opioid receptors (hDOR) and rat μ-opioid receptors (rMOR) were performed on cell (HN9.10) membranes from cells that stably express the corresponding receptors using [3H]-c[D-Pen2, D-Pen5]-enkephalin ([3H]DPDPE) and [3H]-[D-Ala2, NMePhe4, Gly5-ol]-enkephalin ([3H]DAMGO) as the radioligands, for the δ and μ opioid receptors respectively. Receptor density of the opioid cell lines is generally about 1 pmol/mg of membrane proteins. [35S]GTPγS binding assays were used to examine the δ and μ opioid agonist efficacies on the same cell membranes. Isolated tissue-based functional assays also were used to evaluate opioid agonist activities in the GPI (δ) and MVD (μ). For the affinity at the human NK1 (hNK1) receptors, binding assays utilized membranes from transfected CHO cells that stably express hNK1 receptors, using [3H]-substance P as the standard radioligand. The binding affinity assays at the rat NK1 (rNK1) receptors also were performed using transfected CHO cells that stably express rNK1 receptors. For the human and rat NK1 cell lines, the expressions are about 0.5 and 6 pmol/mg protein, respectively. To evaluate antagonistic activities against substance P stimulation, isolated tissue bioassays using GPI were performed in the presence of naloxone to block the opioid activities.
Experimental Procedure: Determination of Antinociceptive Activities in vivo of Bifunctional Peptide 7
Male, Sprague-Dawley rats (200-225g; Harlan; Harlan, IN, USA) were obtained and cared for under the University of Arizona IACUC standards. Food and water were available ad libitum. All preparations and testing were performed in accordance with the policies and recommendations of the International Association for the Study of Pain, National Institute of Health and Animal Care at the University of Arizona. Intrathecal catheter implantation: Rats were anesthetized using ketamine/xylazine (vol/vol: 80/20; 100mg/kg i.p.) and placed in a stereotaxic head holder. The cisternum magnum was exposed and an 8 mm catheter was implanted, as described,40 terminating in the lumbar region of the spinal cord. Animals were allowed to recover for 5-7 days. Compound administration: 5 μL of each treatment was given followed 1 μL air bubble/ 9 μL saline flush over 30 s. Infrared thermal testing (IR, behavioral): Rats were allowed to acclimate within Plexiglas holders for baseline testing (pre- compound administration) for 20 minutes. A mobile radiant heat source was used to direct heat to the left hind paw. Paw withdrawal latencies were measured in seconds, with an automatic shutoff of the heat source at 33.0 seconds. On test days, animals were administered a treatment and tested with radiant heat, 60 minutes after said administration. Paw withdrawal latencies were calculated and expressed as the Mean Withdrawal Latency ± SEM by Graph Pad Prism 4 (GraphPad Software, La Jolla, CA). One-way analysis of variance (ANOVA) was performed in FlashCalc (University of Arizona, Dr. Michael Ossipov) and statistical significance achieved when p ≤ 0.05.
Supplementary Material
Figure 4.
Diagram of HN-Hα coupling constants, NOE connectivities, and Hα chemical shift index (CSI) for 7. The Hα CSI was calculated using the random-coil values reported by Andersen et al.39,40 The residue Bzl stands for the respective C-terminal moieties.
Acknowledgements
The work was supported by grants from the USDHS, National Institute on Drug Abuse, DA-13449 and DA-06284. We thank Dr. Guangxin Lin for kind assistance and advice with the NMR measurements, Dr. Eva Varga and Dr. Edita Navratilova for scientific discussion, Ms. Magdalena Kaczmarska for culturing cells, and the University of Arizona Mass Spectrometry Facility for the mass spectra measurements. We express appreciation to Ms. Margie Colie for assistance with the manuscript.
A List of Abbreviations
Abbreviations used for amino acids and designation of peptides follow the rules of the IUPAC-IUB Commission of Biochemical Nomenclature in J. Biol. Chem. 1972, 247, 977-83. The following additional abbreviations are used:
- BSA
bovine serum albumin
- CHO
Chinese hamster ovary
- DAMGO
[D-Ala2, NMePhe4, Gly5-ol]-enkephalin
- Dmt
2′, 6′-Dimethyl-L-Tyrosine
- DOR
δopioid receptor
- DPC
dodecylphosphocholine
- DPDPE
c[D-Pen2, D-Pen5]-enkephalin
- DQF-COSY
double quantum filtered correlation spectroscopy
- GPI
guinea pig ileum
- GTPγS
guanosine 5′-(γ-thio) triphosphate
- i.t.
intrathecal
- MOR
μ opioid receptor
- MVD
mouse vas deferens
- NK1
neurokinin 1
- NOE
nuclear Overhauser enhancement
- NOESY
nuclear Overhauser enhancement spectroscopy
- rmsd
root mean square deviation
- TOCSY
total correlation spectroscopy
Footnotes
Supporting Information Available: HR-MS, TLC, HPLC and 1H-NMR data of the peptides 3-7 and the metabolic stability studies of peptides 3 in rat plasma are provided. This material is available free of charge via the Internet at http://pubs.acs.org.
References
- 1.Mantyh PW, Allen CJ, Ghilardi JR, Rogers SD, Mantyh CR, Liu H, Basbaum AI, Vigna SR, Maggio JE. Rapid endocytosis of a G protein-coupled receptor: substance P evoked internalization of its receptor in the rat striatum in vivo. Proc. Natl. Acad. Sci. U. S. A. 1995;92:2622–2626. doi: 10.1073/pnas.92.7.2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalso E. Improving opioid effectiveness: from ideas to evidence. Eur. J. Pain. 2005;9:131–135. doi: 10.1016/j.ejpain.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 3.King T, Ossipov MH, Vanderah TW, Porreca F, Lai J. Is paradoxical pain induced by sustained opioid exposure an underlying mechanism of opioid antinociceptive tolerance? Neurosignals. 2005;14:194–205. doi: 10.1159/000087658. [DOI] [PubMed] [Google Scholar]
- 4.Misterek K, Maszczynska I, Dorociak A, Gumulka SW, Carr DB, Szyfelbein SK, Lipkowski AW. Spinal co-administration of peptide substance P antagonist increases antinociceptive effect of the opioid peptide biphalin. Life Sci. 1994;54:939–944. doi: 10.1016/0024-3205(94)00494-3. [DOI] [PubMed] [Google Scholar]
- 5.Powell KJ, Quirion R, Jhamandas K. Inhibition of neurokinin-1-substance P receptor and prostanoid activity prevents and reverses the development of morphine tolerance in vivo and the morphine-induced increase in CGRP expression in cultured dorsal root ganglion neurons. Eur. J. Neurosci. 2003;18:1572–1583. doi: 10.1046/j.1460-9568.2003.02887.x. [DOI] [PubMed] [Google Scholar]
- 6.Ripley TL, Gadd CA, De Felipe C, Hunt SP, Stephens DN. Lack of self-administration and behavioural sensitisation to morphine, but not cocaine, in mice lacking NK1 receptors. Neuropharmacology. 2002;43:1258–1268. doi: 10.1016/s0028-3908(02)00295-2. [DOI] [PubMed] [Google Scholar]
- 7.Hruby VJ. Organic chemistry and biology: chemical biology through the eyes of collaboration. J. Org. Chem. 2009;74:9245–9264. doi: 10.1021/jo901767e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Horan PJ, Mattia A, Bilsky EJ, Weber S, Davis TP, Yamamura HI, Malatynska E, Appleyard SM, Slaninova J, Misicka A, Lipowski AW, Hruby VJ, Porreca F. Antinociceptive Profile of Biphalin, a Dimeric Enkephalin Analog. J. Pharmacol. Exp. Ther. 1993;265:1446–1454. [PubMed] [Google Scholar]
- 9.Yamamoto T, Nair P, Davis P, Ma SW, Navratilova E, Moye M, Tumati S, Vanderah TW, Lai J, Porreca F, Yamamura HI, Hruby VJ. Design, Synthesis and Biological Evaluation of Novel Bifunctional C-terminal Modified Peptides for δ/μ Opioid Receptor Agonists and Neurokinin-1 Receptor Antagonists. J. Med. Chem. 2007;50:2779–2786. doi: 10.1021/jm061369n. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cascieri MA, Macleod AM, Underwood D, Shiao LL, Ber E, Sadowski S, Yu H, Merchant KJ, Swain CJ, Strader CD, Fong TM. Characterization of the interaction of N-acyl-L-tryptophan benzyl ester neurokinin antagonists with the human neurokinin-1 receptor. J. Biol. Chem. 1994;269:6587–6591. [PubMed] [Google Scholar]
- 11.MacLeod AM, Merchant KJ, Cascieri MA, Sadowski S, Ber E, Swain CJ, Baker R. Nacyl-L-tryptophan benzyl esters: potent substance P receptor antagonists. J. Med. Chem. 1993;36:2044–2045. doi: 10.1021/jm00066a015. [DOI] [PubMed] [Google Scholar]
- 12.Millet R, Goossens L, Goossens JF, Chavatte P, Bertrand-Caumont K, Houssin R, Henichart JP. Conformation of the tripeptide Cbz-Pro-Leu-Trp-OBzl(CF3)2 deduced from two-dimensional 1H-NMR and conformational energy calculations is related to its affinity for NK1-receptor. J. Pept. Sci. 2001;7:323–330. doi: 10.1002/psc.326. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto T, Nair P, Jacobsen NE, Davis P, Ma SW, Navratilova E, Lai J, Yamamura HI, Vanderah TW, Porreca F, Hruby VJ. The Importance of Micelle-Bound States for the Bioactivities of Bifunctional Peptide Derivatives for δ/μ Opioid Receptor Agonists and Neurokinin 1 Receptor Antagonists. J. Med. Chem. 2008;51:6334–6347. doi: 10.1021/jm800389v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamamoto T, Nair P, Jacobsen NE, Vagner J, Kulkarni V, Davis P, Ma S-W, Navratilova E, Yamamura HI, Vanderah TW, Porreca F, Lai J, Hruby VJ. Improving metabolic stability by glycosylation: bifunctional peptide derivatives that are opioid receptor agonists and neurokinin 1 receptor antagonists. J. Med. Chem. 2009;52:5164–5175. doi: 10.1021/jm900473p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yamamoto T, Nair P, Vagner J, Davis P, Ma SW, Navratilova E, Moye M, Tumati S, Vanderah TW, Lai J, Porreca F, Yamamura HI, Hruby VJ. A Structure Activity Relationship Study and Combinatorial Synthetic Approach of C-Terminal Modified Bifunctional Peptides That Are δ/μ Opioid Receptor Agonists and Neurokinin 1 Receptor Antagonists. J. Med. Chem. 2008;51:1369–1376. doi: 10.1021/jm070332f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yamamoto T, Nair P, Davis P, Ma S-W, Yamamura HI, Vanderah TW, Porreca F, Lai J, Hruby VJ. The biological activity and metabolic stability of peptidic bifunctional compounds that are opioid receptor agonists and neurokinin 1 receptor antagonists with a cystine moiety. Bioorg. Med. Chem. 2009;17:7337–7343. doi: 10.1016/j.bmc.2009.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hokfelt T, Kellereth JO, Nilsson G. Immunohistochemical studies on the localization and distribution of substance P in cat primary sensory neurons. Brain Res. 1975;100:235–252. doi: 10.1016/0006-8993(75)90481-3. [DOI] [PubMed] [Google Scholar]
- 18.Marchand JE, Kream RM. Substance P and Related Peptides: Cellular and Molecular Physiology. New York Academy of Science; New York: 1990. Substance P and Somatostatin levels in rhumatioid arthesis, molecular physiology; pp. 437–438. [Google Scholar]
- 19.Kondo I, Marvizon JC, Song B, Salgado F, Codeluppi S, Hua XY, Yaksh TL. Inhibition by spinal mu- and delta-opioid agonists of afferent-evoked substance P release. J. Neurosci. 2005;25:3651–3660. doi: 10.1523/JNEUROSCI.0252-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Largent-Milnes TM, Yamamoto T, Davis P, Ma SW, Hruby VJ, Yamamura HI, Lai J, Porreca F, Vanderah TW. Society for Neuroscience. Visceral Pain: Transmitters and Receptors; San Diego, CA.: 2007. Dual acting opioid agonist/NK1 antagonist reverses neuropathic pain and does not produce tolerance. Poster 725. [Google Scholar]
- 21.Largent-Milnes TM, Yamamoto T, Nair P, Navratrilova E, Davis P, Ma S-W, Hruby VJ, Yamamura HI, Lai J, Porreca F, Vanderah TW. International Association for the Study of Pain / 12th World Congress on Pain. Glasgow, Scotland: 2008. Dual acting opioid agonist/NK1 antagonist peptide reverses neuropathic pain in an animal model without demonstrating common opioid unwanted side effects. [Google Scholar]
- 22.Largent-Milnes TM, Yamamoto T, Campos CR, Corral-Frias NS, Andrade-Jimenez JM, Davis P, Ma SW, Mantyh PW, French ED, Davis TP, Lai J, Hruby VJ, Porreca F, Vanderah TW. Society for Neuroscience. Chicago, IL: 2009. Dual acting opioid agonist/NK1 antagonist does not produce antinociceptive tolerance or reward in an animal model of neuropathic pain. Program#/Poster#: 255.10/U7. [Google Scholar]
- 23.Largent-Milnes TM, Yamamoto T, Nair P, Hruby VJ, Yamamura HI, Lai J, Porreca F, Vanderah TW. Spinal or systemic TY005, a peptidic opioid agonist/neurokinin 1 antagonist, attenuates pain with reduced tolerance. Br. J. Pharmacol. 2010;161:986–1001. doi: 10.1111/j.1476-5381.2010.00824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bryant SD, Jinsmaa Y, Salvadori S, Okada Y, Lazarus LH. Dmt and opioid peptides: a potent alliance. Biopolymers. 2003;71:86–102. doi: 10.1002/bip.10399. [DOI] [PubMed] [Google Scholar]
- 25.Lee YS, Petrov R, Park CK, Ma SW, Davis P, Lai J, Porreca F, Vardanyan R, Hruby VJ. Development of novel enkephalin analogues that have enhanced opioid activities at both mu and delta opioid receptors. J. Med. Chem. 2007;50:5528–5532. doi: 10.1021/jm061465o. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sasaki Y, Suto T, Ambo A, Ouchi H, Yamamoto Y. Biological properties of opioid peptides replacing Tyr at position 1 by 2,6-dimethyl-Tyr. Chem. Pharm. Bull. 1999;47:1506–1509. doi: 10.1248/cpb.47.1506. [DOI] [PubMed] [Google Scholar]
- 27.Hansen DW, Jr., Stapelfeld A, Savage MA, Reichman M, Hammond DL, Haaseth RC, Mosberg HI. Systemic analgesic activity and delta-opioid selectivity in [2,6-dimethyl-Tyr1,D-Pen2,D-Pen5]enkephalin. J. Med. Chem. 1992;35:684–687. doi: 10.1021/jm00082a008. [DOI] [PubMed] [Google Scholar]
- 28.Jacobsen NE, Abadi N, Sliwkowski MX, Reilly D, Skelton NJ, Fairbrother WJ. High-resolution solution structure of the EGF-like domain of heregulin-alpha. Biochemistry. 1996;35:3402–3417. doi: 10.1021/bi952626l. [DOI] [PubMed] [Google Scholar]
- 29.Ying J, Ahn JM, Jacobsen NE, Brown MF, Hruby VJ. NMR solution structure of the glucagon antagonist [desHis1, desPhe6, Glu9]glucagon amide in the presence of perdeuterated dodecylphosphocholine micelles. Biochemistry. 2003;42:2825–2835. doi: 10.1021/bi026629r. [DOI] [PubMed] [Google Scholar]
- 30.D'Alagni M, Delfini M, Di Nola A, Eisenberg M, Paci M, Roda LG, Veglia G. Conformational study of [Met5]enkephalin-Arg-Phe in the presence of phosphatidylserine vesicles. Eur. J. Biochem. 1996;240:540–549. doi: 10.1111/j.1432-1033.1996.0540h.x. [DOI] [PubMed] [Google Scholar]
- 31.Deber CM, Behnam BA. Role of membrane lipids in peptide hormone function: binding of enkephalins to micelles. Proc. Natl. Acad. Sci. U. S. A. 1984;81:61–65. doi: 10.1073/pnas.81.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weiner SJ, Kollman PA, Case DA. An all atom force field for simulations of proteins and nucleic acids. J. Comput. Chem. 1986;7:230–252. doi: 10.1002/jcc.540070216. [DOI] [PubMed] [Google Scholar]
- 33.Weiner SJ, Kollman PA, Case DA, Singh UC, Ghio C, Alagona GS, Profeta J, Weiner P. A New Force Field for Molecular Mechanical Simulation of Nucleic Acids and Proteins. J. Am. Chem. Soc. 1984;106:765–784. [Google Scholar]
- 34.Hyberts SG, Goldberg MS, Havel TF, Wagner G. The solution structure of eglin c based on measurements of many NOEs and coupling constants and its comparison with X-ray structures. Protein Sci. 1992;1:736–751. doi: 10.1002/pro.5560010606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Davis DG, Bax A. Assignment of complex proton NMR spectra via two-dimensional homonuclear Hartmann-Hahn spectroscopy. J. Am Chem. Soc. 1985;107:2820–2821. [Google Scholar]
- 36.Marion D, W. K. Application of phase sensitive two-dimensional correlated spectroscopy (COSY) for measurements of 1H-1H spin-spin coupling constants in proteins. Biochem. Biophys. Res. Commun. 1983;113:967–974. doi: 10.1016/0006-291x(83)91093-8. [DOI] [PubMed] [Google Scholar]
- 37.Braunschweiler L, Ernst RR. Coherence Transfer by Isotropic Mixing: Application of Proton Correlation Spectroscopy. J. Magn. Reson. 1983;53:521–528. [Google Scholar]
- 38.Kumar A, Ernst RR, Wüthrich K. A two-dimensional nuclear Overhauser enhancement (2D NOE) experiment for the elucidation of complete proton-proton cross-relaxation networks in biological macromolecules. Biochem. Biophys. Res. Commun. 1980;95:1–6. doi: 10.1016/0006-291x(80)90695-6. [DOI] [PubMed] [Google Scholar]
- 39.Havel TF. An evaluation of computational strategies for use in the determination of protein structure from distance constraints obtained by nuclear magnetic resonance. Prog. Biophys. Mol. Biol. 1991;56:43–78. doi: 10.1016/0079-6107(91)90007-f. [DOI] [PubMed] [Google Scholar]
- 40.Yaksh TL, Rudy TA. Chronic catheterization of the spinal subarachnoid space. Physiol. Behav. 1976;17:1031–1036. doi: 10.1016/0031-9384(76)90029-9. [DOI] [PubMed] [Google Scholar]
- 41.Wagner G, Neuhaus D, Worgotter E, Vasak M, Kagi JH, Wuthrich K. Nuclear magnetic resonance identification of “half-turn” and 3(10)-helix secondary structure in rabbit liver metallothionein-2. J. Mol. Biol. 1986;187:131–135. doi: 10.1016/0022-2836(86)90413-4. [DOI] [PubMed] [Google Scholar]
- 42.Wishart DS, Sykes BD, Richards FM. The Chemical Shift Index: A Fast and Simple Method for the Assignment of Protein Secondary Structure through NMR Spectroscopy. Biochemistry. 1992;31:1647–1651. doi: 10.1021/bi00121a010. [DOI] [PubMed] [Google Scholar]
- 43.Andersen NH, Neidigh JW, Harris SW, Lee GM, Liu ZH, Tong H. Extracting Information from the Temperature Gradients of Polypeptide NH Chemical Shifts. 1. The Importance of Conformational Averaging. J. Am. Chem. Soc. 1997;119:8547–8561. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.