Abstract
Objective
Extend understanding of a rapid response (RR) to treatment by examining its prognostic significance at end-of-treatment (EOT) and 1 year follow-up within two group treatments for binge eating disorder (BED): Dialectical Behavior Therapy for BED (DBT-BED) and an active comparison group therapy (ACGT).
Methods
101 adults with BED randomized to 20-weeks DBT-BED versus ACGT (Safer, Robinson, & Jo, 2010). RR defined as ≥ 65% reduction in the frequency of days of binge eating by week 4. RR across and within treatment conditions used to predict binge eating abstinence and secondary outcomes (e.g., binge eating pathology, treatment attrition) at EOT and 1 year follow-up
Results
(1) Significantly higher binge eating abstinence for rapid responders (RR; n = 41) vs. non-rapid responders (non-RRs; n = 60) at EOT (70.7% vs. 33.3%) and 1 year follow-up (70.7% vs. 40.0%), respectively, as well as improvement on most secondary measures (2) Significantly less attrition among RRs vs. non-RRs (3) Significantly higher binge eating abstinence rates at both time points for DBT-RRs vs. DBT-non-RRs, but not for ACGT RRs vs. ACGT-non-RRs,.
Conclusions
Current study extends prognostic significance of RR to 1 year follow-up. RR more prominent for those randomly assigned to DBT-BED than ACGT. Implications discussed.
Keywords: binge eating disorder, dialectical behavior therapy, rapid response, abstinence
The phenomenon of a rapid response (RR) to treatment by certain patients during therapy is gaining increasing interest and study. Rapid response, an early substantial decline in symptomatology within the first 1 – 4 weeks of treatment found in approximately one third of research subjects, has been described in a number of treatments for depression (Ilardi & Craighead, 1994; Tang & DeRubeis, 1999), alcohol use disorders (Breslin, Sobell, Sobell, Buchan, & Cunningham, 1997), panic disorder (Penava, Otto, Maki, & Pollack, 1998), irritable bowel syndrome (Lackner et al., 2010), bulimia (BN; Fairburn, Agras, Walsh, Wilson, & Stice, 2004; Jones, Peveler, Hope, & Fairburn, 1993; Marrone, Mitchell, Crosby, Wonderlich, & Jollie-Trottier, 2009), and, more recently, binge eating disorder (BED; Grilo, Masheb, & Wilson, 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007; Zunker et al., 2010). There is no accepted explanation as to why some persons have an early substantive treatment response and not others.
Four studies have examined the role of rapid response to BED treatment. Three of these were carried out by Grilo and colleagues, who examined the role of rapid response in BED across various individual psychotherapy treatment conditions including Cognitive Behavioral Therapy (CBT), CBT guided self-help (CBTgsh), and Behavioral Weight Loss guided self-help (BWLgsh) (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007). Psychotherapies were compared to one another (Masheb and Grilo, 2007) as well as in combination with different pharmacotherapies, (e.g., fluoxetine, orlistsat, and placebo) (Grilo et al., 2006, Grilo & Masheb, 2007). To summarize, these three Grilo et al. studies found: (1) no consistently identified differences between rapid responders (RRs) and non-rapid responders (non-RRs) on baseline demographic and clinical characteristics; (2) no difference (when examined) in the rate of treatment attrition; (3) higher rates of BED abstinence for RRs compared to non-RRs at EOT and 3 month follow-up (when reported); and (4) similar percentages of RR rates within BED subgroups, despite receiving quite different psychotherapy and pharmacotherapy treatments.
A recently published fourth study by Zunker and colleagues (2010) examined the role of rapid response among participants receiving CBT for BED in a group format. Randomization was to three active treatments: therapist-led, therapist-assisted, or self-help. Abstinence at the end of treatment (EOT) was best predicted at the end of week 1 among early responders. Interestingly, the week 4 threshold previously utilized by Grilo and colleagues (Grilo, Masheb, & Wilson, 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007) was not predictive of later abstinence.
The current study examines findings for RRs at the end of Dialectical Behavior Therapy adapted for BED (DBT-BED) and at the 12 month, or 1 year, follow-up. The analysis makes use of an existing database from a randomized control trial comparing DBT-BED delivered in a group format with an active comparison group therapy (ACGT). This use of an “active placebo” psychotherapy was to control for the “common factors” in psychotherapy (Frank, 1961; Goldfried, 1980).
Specifically, the current study aims to: (1) examine the prognostic significance of RR in two additional treatments not yet investigated for RR (e.g., DBT-BED and ACGT); (2) extend the assessment of RR as a predictor of outcome at EOT to 1 year follow-up; and (3) assess RR as a predictor of treatment attrition.
METHOD
Participants
The current sample was drawn from a recent study in which 101 patients with BED were randomly assigned to receive twenty 2-hour sessions of one of two group treatment conditions: DBT-BED (n = 50) or ACGT (n = 51). A detailed description of the aims, design, methods, and outcomes of this study has been reported elsewhere (Safer, Robinson, & Jo, 2010), but is briefly described here. Binge eating abstinence and reductions in binge eating frequency at EOT were achieved to a greater degree for DBT than for ACGT (EOT abstinence rate 64% for DBT vs. 36% for ACGT), although these differences did not persist over the 3-, 6-, and 12-month follow-up assessments. (The 12-month follow-up binge eating abstinence rate = 64% for DBT vs. 56% for ACGT).
All participants were 18 years of age or older, met DSM-IV research criteria for BED, and, among those on medication, had been on a stable psychotropic regimen for at least the prior three months. Exclusion criteria were: having a history of bipolar disorder or schizophrenia, meeting current criteria for alcohol or drug dependence, showing evidence of current suicidality, and/or being unwilling to discontinue concomitant weight related medications (e.g., sibutramine, phentermine, amphetamines, insulin, or topiramate)or eating-disorder/weight related psychotherapy treatment. See Safer et al. (2010) for further details.
Procedure
One hundred and one participants were randomly assigned either to DBT adapted for BED or ACGT, as described below. Participants were assessed at pretreatment (which included baseline demographic information), EOT (after 20 weekly sessions), and at the 12-month follow-up. In addition, binge eating frequency was assessed at weekly time points throughout the 20 sessions of treatment.
Measures
The Eating Disorder Examination (EDE), a structured interview that assesses the main behavioral and attitudinal features of eating disorders (Fairburn & Cooper, 1993), was used to document the BED diagnosis and assess the frequency of days on which objective binge episodes (OBE) took place. Its four subscales are: Dietary Restraint, Eating Concern, Weight Concern, and Shape Concern. Items are rated from 0 – 6, with higher scores reflecting greater severity. The Three Factor Eating Questionnaire (TFEQ) is a 51-item questionnaire that measures three dimensions of human eating behavior: (1) cognitive restraint, (2) disinhibition, and (3) hunger (Stunkard & Messick, 1985). The Beck Depression Inventory (BDI; Beck & Steer, 1987) is a 21-item established inventory of the symptoms of depression and negative affect (Beck, Steer, & Garbin, 1998). The Questionnaire on Eating and Weight Patterns (QEWP-R; Spitzer et al., 1992), a self-report instrument, was used to obtain demographic data as well as information on weight history and the onset of binge eating, dieting, and obesity.
Weight and height were measured in lightweight clothing with shoes removed on a balance beam scale. All participants were weighed at baseline, EOT, and at follow-up.
A weekly self-report monitoring form was used toassess the frequency of days on which at least one OBE took place (i.e., OBE days) over the prior week.
A post-randomization questionnaire regarding treatment expectations and suitability was completed at the conclusion of the pre-treatment orientation. Previously participants had received written and verbal rationales for both DBT-BED and ACGT. Post-randomization they were oriented in greater detail to their assigned treatment condition. Using a 10 point visual analogue scale, participants were asked to rate, “How successful do you think your treatment here will be? from 1 (“Not at all successful”) to 10 (“Extremely successful”), and “How suitable do you think the treatment group you were assigned is for your eating problems?” from 1 (“Not at all suitable”) to 10 (“Extremely suitable”).
Psychological Interventions
Dialectical Behavior Therapy for Binge Eating Disorder (DBT-BED)
DBT is an affect regulation behavior therapy initially developed by Linehan (1993a, 1993b) and adapted for BED by Telch and colleagues (Telch et al., 2000; Telch et al., 2001; Wiser & Telch, 1999). Treatment consisted of 20 weekly two-hour sessions of group psychotherapy aimed at teaching emotion regulation skills to reduce binge eating behaviors. A published treatment manual is available (Safer, Telch, & Chen, 2009).
Active Comparison Group Psychotherapy (ACGT)
This manual-based supportive group therapy was expressly developed to control for nonspecific therapeutic factors (e.g., therapeutic alliance, patient expectations, etc.). For more details, see Safer and Hugo (2006). The ACGT condition was matched to the DBT treatment arm on pertinent variables including length of treatment, number of sessions, etc. A supportive psychotherapy manual originally written by Markowitz and Sacks (2002) for chronic depression was used as a model and adapted for BED. In this therapy, binge eating is conceptualized as both the result of low self-esteem and the cause of additional problems. ACGT participants were expected to monitor their binges and self-esteem and complete a weekly diary card (as done by DBT participants). ACGT therapists were provided with explicit instructions to avoid employing any techniques consistent with DBT-BED and other therapeutic approaches such as CBT, IPT, BWL, and psychodynamic psychotherapy.
Overview of Analyses
Determination of Participants in Current Dataset
Of the entire sample of 101 participants, 82 had complete data for every single time point over the first four weeks. Of the 19 participants without data at every single point, only one had dropped out before the first session. Other participants missed treatment sessions sporadically; for example, seven were missing data at week four. Missing data were handled by carrying the baseline observation forward (considered more conservative than last observation carried forward) resulting in a final intent-to-treat sample of 101 participants.
Nineteen (18.8%) of the 101 participants dropped from treatment before completing 20 sessions. Dropping from treatment did not necessarily mean dropping from follow-up. The percentages of participants who completed study assessments on at least the primary outcome variables were: 97% at EOT (n=98/101; DBTBED= 50, ACGT=48) and 87.1% at 12 month follow-up (n=88/101; DBT-BED=49/50, ACGT=39/51).
Defining RR
RR was defined as a 65% or greater reduction in OBE days (as reported on participants’ weekly monitoring forms) between treatment session 1 and session 4, following the guidelines of Grilo and colleagues (Grilo et al., 2006; Masheb & Grilo, 2007).
Primary and Secondary Outcomes
The primary treatment outcome was abstinence from binge eating, defined as no OBE days (per the EDE) over the prior 28 days. Secondary outcomes included binge eating frequency, eating disorder pathology (EDE & TFEQ), depression (BDI), BMI, and weight in lbs. Ratings of treatment expectations and suitability as well as rates of attrition from the 20 session treatment were additional outcomes.
Statistical Analyses
Chi-square analyses of dichotomous outcomes (e.g., 28 day binge eating abstinence, treatment attrition) were used to compare RR and non-RR subjects across treatment conditions, as well as separately within the two treatment conditions, DBT-BED and ACGT. ANOVA was used to investigate differences between RRs and non-RRs on continuous treatment outcomes. In addition, secondary outcomes were analyzed using effect sizes (ES) based on Cohen’s d and were evaluated by the conventions: small =.20, moderate =.50, and large =.80 (Cohen, 1988). SPSS version 17 was used (SPSS Inc., Chicago, Illinois).
We are aware that because RR is a variable identified during treatment and thus affected by treatment assignment, causal inferences regarding outcome cannot be made based on analyses that combine RRs in DBT-BED with RRs in ACGT (Jo, Wang, & Ialongo, 2009). However, these data are included to allow for comparisons with earlier studies that contrasted participants with and without RRto BED treatment.
RESULTS
Sample Characteristics
The baseline characteristics of the total sample are presented in Table 1. Within the entire sample there were more female (n = 86) than male (n = 15) participants. The mean age was 52.1 (SD = 10.6). The majority of the participants were Caucasian (n = 72; 71%), followed by Latino (n = 13; 13%). Most were married (n = 61; 60%) and college-educated (n = 95; 94.5%). Approximately half of the participants (n = 50; 49.5%) were employed, and 19% (n = 19) were retired. The average reported age (in years) for the onset of overweight was 17.4 (SD = 11.2). Participants noted beginning to diet at 17.7 years (SD = 9) and beginning to binge eat at 19.4 years (SD = 12.7). More than half of the sample (n = 64; 63%) had a history of depression, and approximately one third (n = 33; 33%) were currently taking antidepressant medication.
Table 1.
Demographic and Clinical Characteristics of Entire Sample and Rapid Responders and Non-Rapid Responders
| Total (N = 101) | RRs (n = 41) | Non-RRs (n = 60) | |
|---|---|---|---|
| Gender, n (%) | |||
| Female | 86.0 (85.1 %) | 34.0 (82.9 %) | 52.0(86.7%) |
| Male | 15.0 (14.9%) | 7.0 (17.1 %) | 8.0 (13.3 %) |
| Mean age (SD) in years | 52.1 (10.6) | 51.4 (10.3) | 52.6 (10.8) |
| Mean Body Mass Index, kg/m2 (SD) | 36.4 (8.6) | 36.5 (8.9) | 36.3 (8.4) |
| Ethnicity/Race, n (%) | |||
| Caucasian | 72.0 (71.0 %) | 33.0 (80.5 %) | 39.0 (65.0 %) |
| Latino | 13.0 (13.0 %) | 4.0 (9.8 %) | 9.0 (15.0 %) |
| Asian | 5.0 (5.0 %) | 2.0 (4.9 %) | 3.0 (5.0 %) |
| African American | 3.0 (3.0 %) | 1.0 (2.4 %) | 2.0 (3.3 %) |
| More than one race | 4.0 (4.0 %) | 0 | 4.0 (6.7 %) |
| Unknown/Unreported ethnicity | 4.0 (4.0 %) | 1.0 (2.4 %) | 3.0 (5.0 %) |
| Marital status, n (%) | |||
| Married | 61.0 (60.4 %) | 23.0 (56.1%) | 38.0 (63.3 %) |
| Divorced | 19.0 (18.8 %) | 7.0 (17.1 %) | 12.0 (20.0 %) |
| Single/Never married | 17.0 (16.8 %) | 8.0 (19.5 %) | 9.0 (15.0 %) |
| Widowed | 4.0 (4.0 %) | 3.0 (7.3 %) | 1.0 (1.7 %) |
| Educational background, n (%) | |||
| Did not complete high school | 4.0 (4.0 %) | 1.0 (2.4 %) | 3.0 (5.0 %) |
| Have high school degree or equivalent | 2.0 (2.0 %) | 0 | 2.0 (3.3 %) |
| Completed some college/2 year degree | 30.0 (29.7 %) | 8.0 (19.5 %) | 22.0 (36.7 %) |
| Graduated from a 4 year college | 26.0 (25.7 %) | 12.0 (29.3 %) | 14.0 (23.3 %) |
| Completed some graduate school | 9.0 (8.9 %) | 5.0 (12.2 %) | 4.0 (6.7 %) |
| Completed at least one graduate degree | 30.0 (29.7 %) | 15.0 (36.6 %) | 15.0 (25.0 %) |
| Employment status, n (%) | |||
| Employed | 50.0 (49.5 %) | 23.0 (56.1 %) | 27.0 (45.0 %) |
| Retired | 19.0 (18.8 %) | 5.0 (12.2 %) | 14.0 (23.3 %) |
| Homemaker | 14.0 (13.9 %) | 5.0 (12.2 %) | 9.0 (15.0 %) |
| Unemployed | 12.0 (11.9 %) | 6.0 (14.6 %) | 6.0 (10.0 %) |
| Student/Other | 6.0 (5.9 %) | 2.0 (4.9 % ) | 4.0 (6.7 %) |
| Mean age (SD) when first: | |||
| Overweight | 17.4 (11.2) | 17.6 (9.6 ) | 17.2 (12.3) |
| Began dieting | 17.7 (9.0) | 18.0 (7.0) | 17.5 (10.2) |
| Began binge eating | 19.4 (12.7) | 17.3 (10.5) | 20.9 (13.9) |
| Past history of depression, n (%) | 64.0 (63.4 %) | 23.0 (56.1 %) | 41.0 (68.3 %) |
| Current use of antidepressants, n (%) | 33.0 (32.7 %) | 11.0 (26.8 %) | 22.0 (36.7 %) |
RRs = Rapid Responders; Non-RRs = Non-Rapid Responders. No significant differences of p < .05
Comparison of Participants With and Without RR
Of the intent-to-treat sample of 101 participants, 41 (41%) showed a RR (a 65% or greater reduction in OBE days by the 4th week of treatment), and 59 (58.4%) did not evidence a RR to treatment.
No significant differences between RRs and non-RRs were found on any of the baseline demographic characteristics displayed in Table 1.
Table 2 describes baseline eating and clinical characteristics of RRs and non-RRs. Measures included: objective binge eating days per prior month, eating psychopathology as measured by the EDE and TFEQ, depression scores as measured by the BDI, and weight as measured by the BMI and in pounds (lbs.). No significant differences between RRs and non-RRs were found on any of these variables.
Table 2.
Baseline Clinical Characteristics of Rapid Responders and Non-Rapid Responders
| RRs (n = 41) M (SD) | Non-RRs (n = 60) M (SD) | Analysis p | |
|---|---|---|---|
| Objective binge days/month | 15.0 (6.0) | 16.5 (6.4) | .232 |
| Measures of Eating Psychopathology (EDE, TFEQ) | |||
| Dietary restraint (EDE-R) | 1.7 (1.1) | 2.0 (1.3) | .236 |
| Weight concern (EDE-WC) | 3.7 (0.9) | 3.8 (1.1) | .656 |
| Shape concern (EDE-SH) | 3.8 (1.2) | 4.1 (1.1) | .178 |
| Eating concern (EDE-EC) | 2.1 (1.3) | 2.2 (1.4) | .538 |
| Cognitive restraint (TFEQ- CR) a | 8.0 (3.5) | 8.0 (4.0) | .940 |
| Disinhibition (TFEQ-Dis) a | 13.9 (1.8) | 14.0 (1.5) | .673 |
| Hunger (TFEQ-H)a | 10.0 (3.6) | 10.1 (3.4) | .895 |
| Beck Depression Inventory (BDI) | 15.3 (7.4) | 17.5 (8.7) | .183 |
| Body mass index (BMI), kg/m2 | 36.5 (9.0) | 36.3 (8.4) | .873 |
| Weight, lbs | 220.1 (53.6) | 220.8 (56.1) | .950 |
RRs = Rapid Responders; Non-RRs = Non-Rapid Responders. No significant differences of p < .05; EDE = Eating Disorder Examination; TFEQ = Three Factor Eating Questionnaire;
Two participants did not complete the baseline TFEQ. Thus total N = 99 for TFEQ (RRs = 40 and non-RRs = 59); BDI = Beck Depression Inventory.
Treatment Expectations and Suitability
Ratings of expectations for success and treatment suitability were determined after participants had been randomized and oriented to their treatment condition. [Note: Ratings of expectations for success were missing from two participants. Total n = 98.] While there was a trend towards differences in expectations for a successful outcome when comparing participants randomized to DBT-BED (n = 50) vs. ACGT (n = 51), these differences (DBT-BED = 8.1 ± 1.75 vs. ACGT = 7.4 ± 1.75) were not significant (t97= −2.0, p = .054; Effect Size = .40). No significant differences between treatment conditions were found for average ratings of treatment suitability (DBT-BED = 9.2 ± 1.3 vs. ACGT = 8.8 ± 1.7; t99= −1.2, p = .239; Effect Size = .26 ).
When examining the treatment expectation and suitability ratings of RRs vs. non-RRs across treatment conditions, average ratings of expectations for success were significantly higher, p = .039; Effect Size for rapid responders (RRs = 8.1 ± 1.7 vs. non-RRs = 7.4 ± 1.8, t97= −2.10 = .40). There were no significant differences between the two for ratings of suitability of treatment (RRs = 9.3 ± 1.2 vs. non-RRs = 8.8 ± 1.6; t99 = 1.9, p = .060; Effect Size = .35).
RR and Treatment Attrition
Drop-out rates from treatment were significantly higher among non-RRs (n = 16 of 60) compared to RRs (n = 3 of 41). Specifically, non-RRs’ percentage rate of drop out was over three times higher than that of RRs’ [non-RRs = 26.7% vs. RRs = 7.3%; χ2 = 5.97, df = 1, p =.015)].
RR and Treatment Outcome at EOT and 12-Month Follow-up
Primary Treatment Outcome
Across treatment conditions, RRs were significantly more likely than non-RRs to achieve abstinence from binge eating at EOT [RR abstinence rate = 70.7% (n = 29 of 41) vs. non-RR abstinence rate = 33.3% (n = 20 of 60), (χ2 = 13.6, df = 1, p < .001)]. Similarly, at 12-month follow-up, RRs were significantly more likely than non-RRs to achieve abstinence from binge eating [RR abstinence rate = 70.7 % (n = 29 of 41) vs. non-RR abstinence rate = 40.0 % (n = 24 of 60), χ2 = 9.22, df = 1, p = .002. See Figure 1.
Figure 1.
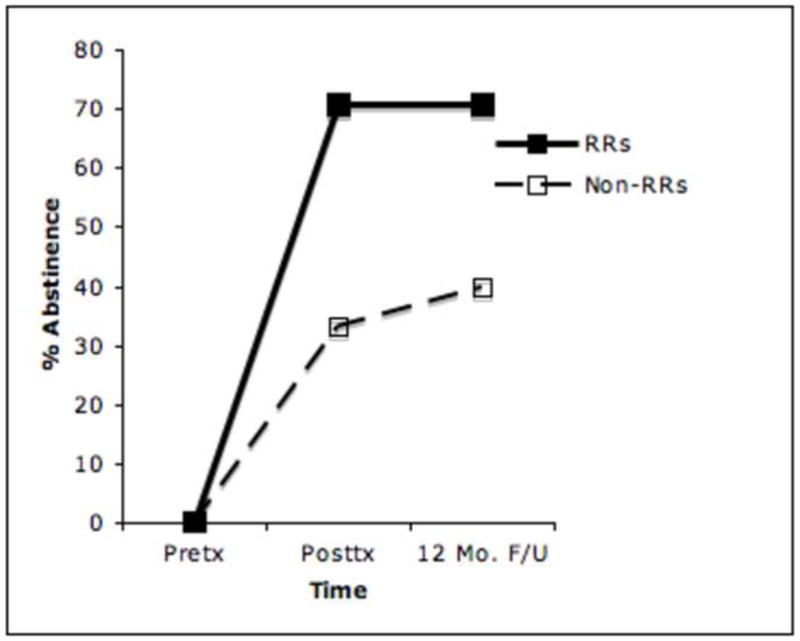
Percent Abstinence among Rapid Responders vs. Non-Rapid Responders at Three Time Points
When only including participants who completed assessments (n=98 at EOT with RRs = 40 and non-RRs= 58; n=88 at 12 month follow-up with RRs= 37, non-RRs= 51), abstinence rates were similar to those of ITT with maintenance of significant differences between RRs and non-RRs. At EOT, the RR abstinence rate = 72.5% vs. non-RRs abstinence rate of 34.5%. At 12 month follow-up, RR abstinence rate = 78.3% vs. non-RR abstinence rate = 47%).
Some of the participants became abstinent at 12-month follow-up who were not abstinent at EOT, and vice versa. For example, of those non-abstinent at EOT, 50% of the RRs and 32.5% of the non-RRs became abstinent at 12-month follow-up. Of those who were abstinent at EOT, 79.3% of the RRs and 55% of the non-RRs remained abstinent at the 12-month follow-up.
Secondary Treatment Outcomes
Table 3 describes eating and clinical characteristics of RRs and non-RRs at EOT as well as at the 12-month follow-up. At EOT, RRs had significantly fewer OBE days (over the prior 28 days) than non-RRs. In addition, they had significantly lower scores on three out of four EDE subscales (eating concern, weight concern, and shape concern). On the TFEQ, RRs had significantly lower scores than non-RRs on two out of three subscales (hunger and disinhibition). RRs also had significantly lower scores on depression (as measured by the BDI) than non-RRs [F(1,100) = 9.97, p =.002)]. Cohen’s d effect sizes were generally medium or small. No significant and no effect size differences were found between RRs and non-RRs on the weight loss-related variables: BMI and weight in pounds.
Table 3.
Secondary Outcomes (Eating And Clinical Characteristics) Between Rapid Responders and Non-Rapid Responders at End-of-Treatment and 12-Month Follow-Up
| End-of-Treatment | 12-Month Follow-up | |||||||
|---|---|---|---|---|---|---|---|---|
| RRs (n = 41) | Non-RRs (n = 60) | Analys is | Effect Size | RRs (n = 41) | Non-RRs (n = 60) | Analy sis | Effect Size | |
| M (SD) | M (SD) | p | Cohen’s d | M (SD) | M (SD) | p | Cohen’s d | |
| Objective binge days (OBE days) per prior month | 1.7 (4.5) | 4.4 (5.3) | < .01* | −.54 | 3.1 (5.8) | 4.4 (6.2) | 0.30 | −.22 |
| Eating psychopathology (as measured by the EDE and TFEQ) | ||||||||
| Dietary restraint (EDE-R) | 1.4 (0.94) | 1.8 (1.3) | 0.12 | −.35 | 1.2 (1.1) | 1.7 (1.4) | 0.04* | −.39 |
| Weight concern (EDE-WC) | 2.5 (1.0) | 3.0 (1.3) | .04* | −.43 | 2.2 (1.1) | 2.9 (1.4) | 0.02* | −.32 |
| Shape concern (EDE-SC) | 2.3 (1.1) | 3.2 (1.3) | < .001* | −.75 | 2.2 (1.3) | 3.1 (1.3) | 0.002 * | −.69 |
| Eating concern (EDE-EC) | 0.4 (0.6) | 1.1 (1.3) | .001* | −.69 | 0.6 (1.3) | 1.3 (1.4) | 0.03* | −.51 |
| Cognitive restraint (TFEQ-CR*) | 10.9 (4.0) | 9.9 (3.8) | 0.21 | .26 | 9.5 (4.3) | 9.6 (4.7) | 0.946 | −.02 |
| Disinhibition (TFEQ-DIS*) | 9.7 (3.8) | 12.2 (3.1) | < .001* | −.72 | 10.4 (3.5) | 12.6 (2.9) | 0.001* | −.68 |
| Hunger (TFEQ-H*) | 6.0 (3.9) | 8.4 (3.8) | .004* | −.62 | 6.9 (4.1) | 9.0 (4.0) | 0.01* | −.52 |
| Depression (BDI) | 7.0 (6.0) | 12.0 (8.8) | .002* | −.66 | 8.0 (8.6) | 13.1 (9.3) | 0.006* | −.57 |
| Body mass index (BMI), kg/m2 | 35.6 (8.3) | 36.1 (8.4) | .780 | −.06 | 36.1 (8.4) | 35.8 (8.4) | 0.876 | .04 |
| Weight, lbs | 214.6 (50.4) | 219.1 (54.8) | .678 | −.09 | 217.4 (50.7) | 218.5 (57.1) | .906 | −.02 |
RRs = Rapid Responders; Non-RRs = Non-Rapid Responders;
p < .05; EDE = Eating Disorder Examination; TFEQ = Three Factor Eating Questionnaire;
Two participants did not complete the TFEQ. Total N = 99 for TFEQ (RRs = 40, non-RRs = 59); BDI = Beck Depression Inventory; Effect Size = Cohen’s d
Twelve-month secondary outcome findings are generally similar to those at EOT (see Table 3). The exceptions were: (1) while binge eating frequency continued to be lower for RRs than non-RRs (3.1 vs. 4.4), this difference was no longer significant at 12 months, F(1, 100)= 1.01, p = 0.30 and (2) unlike at EOT, at the 12-month follow-up RRs had significantly lower scores on the EDE dietary restraint subscale (EDE-R), [F(1, 100)= 4.14, p < .05].
Treatment expectations and suitability as well as rates of attrition from treatment have already been reported.
Abstinence Rates at EOT and 12-Month Follow-Up By Treatment Condition: DBT-BED vs. ACGT
As depicted in Figures 2 and 3, rates of abstinence at EOT and 12 month follow-up differed according to both RR status and treatment condition. When comparing within treatment conditions, DBT-RRs (n = 28; 56%) had significantly higher rates of abstinence than DBT-non-RRs (n = 22; 44%) at both EOT [78.6% vs. 45.5%; (χ2 = 5.86, df = 1, n = 50, p = .015] and at 12-month follow-up [78.6 % vs. 40.9%; (χ2= 7.41, df = 1, n = 50, p = 0.006]. While the ACGT-RRs (n = 13; 25.5%) also reported higher binge eating abstinence rates than ACGT-non-RRs (n = 38; 74.5%) at both EOT (53.8% vs. 26.3%;(χ2 = 3.3, df=1, n = 51, p = .069) and 12 month follow-up (53.8% vs. 39.5%; (χ2= .816, df = 1, n = 51, p = .366), these differences (unlike those for the DBT-RRs) were not statistically significant.
Figure 2.
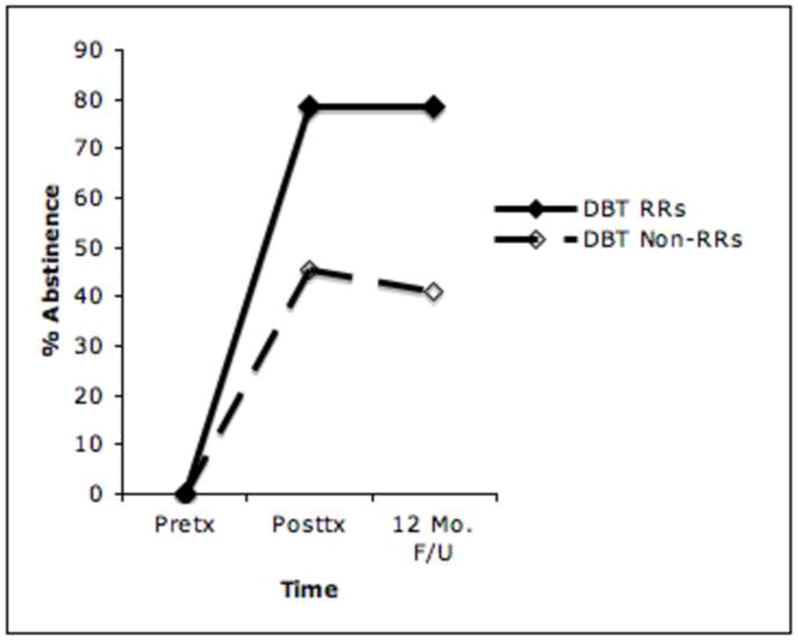
Rates of Binge-Eating Abstinence Between Rapid Responders and Non-Rapid Responders at Three Time Points by Treatment Condition: Dialectical Behavior Therapy adapted for Binge Eating Disorder
Figure 3.
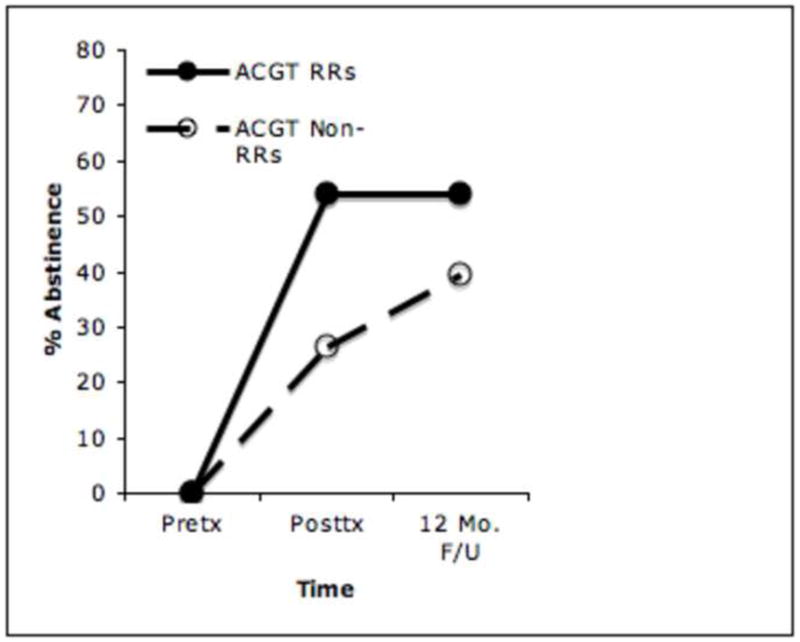
Rates of Abstinence Between Rapid Responders and Non-Rapid Responders by Treatment Condition at Three Time Points: Active Comparison Group Therapy
DISCUSSION
This study aims to further anunderstanding of the role of rapid response (RR) as a predictor of outcome in the treatment of BED. It takes direction from the work of Grilo and colleagues (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007) in defining RR as a reduction in binge eating of at least 65% within the first 4 weeks of treatment. Forty-one percent of the overall sample were rapid responders by this definition, which was similar to percentages found by Grilo and colleagues in the 2006 (% RR = 44%) and the two 2007 studies (% RR = 42% in Grilo & Masheb, 2007; % RR = 55% in Masheb & Grilo, 2007). Also similar is that RRs combined across both treatment conditions evidenced significantly higher rates of abstinence from binge eating (70.7%) compared to non-RRs in the entire sample (33.3%) at EOT.
The current study extends the existing information on RR in three ways. For example, it finds that RR predicts improved outcome not only at EOT but also at the12-month follow-up (RRs = 70.7% abstinence vs. non-RRs = 40.0% abstinence). This holds true for the primary outcome of abstinence from binge eating as well as several secondary measures including binge eating frequency, eating disorder pathology (EDE & TFEQ), and depression (BDI). In addition, the findings of the current study enhance the robustness of the RR construct by showing its prognostic significance within two treatment conditions for BED which had not yet been investigated for RR (e.g., DBT-BED & ACGT), and by replicating the finding of Zunker et al. (2010) regarding the outcome of RR among group therapy participants. Finally, RR was linked to a higher likelihood of remaining in treatment as RRs in this study had only one-third the attrition rate of non-RRs.
However, there were also differences between the findings of the current study and existing studies examining RR in BED (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007; Zunker et al., 2010). For example, in the Zunker et al. (2010) study of participants receiving CBT group therapy for BED, a 65% or greater reduction in binge eating by week 4 was not predictive of remission. Instead, outcome was predicted only when RR was defined as taking place earlier in treatment (e.g., at the end of week 1) and involved a smaller percentage reduction in binge eating (e.g., 15%).
The current study’s findings regarding RR in group therapy were consistent with all other previous studies of BED and BN, which found rapid response to be predictive of remission when examined over a longer time period (e.g., 3–4 weeks) and involving 50% or greater reductions in binge eating and/or purging (e.g., Agras et al., 2000; Fairburn et al., 2004; Grilo et al., 2006; Marrone et al., 2009; Wilson et al., 1999). For example among BN participants: (1) Agras and colleagues (2000) identified RRs as those reporting at least a 70% reduction in purging by week 4 of treatment (2) Fairburn and colleagues (2004) identified those with at least a 51% reduction in purging by week 4 as significantly more likely to be responders at 8 month follow-up; and (3) Wilson and colleagues (1999) identified RRs as those with at least a 50% reduction in binge eating and purging by week 3 (Session 5).
Of interest, when the Zunker et al. (2010) definition of early response as a 15% or more reduction in binge eating by the end of week 1 was applied to data from the current study, RR was not predictive of abstinence at the end of treatment. In their discussion, Zunker and colleagues (2010) note possible explanations for the discrepancy between their findings and the studies by Grilo and colleagues (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007) such as differences in treatment mode (e.g., group vs. individual psychotherapy) and/or treatment delivery (e.g., therapist-delivered vs. self-help). Based on the results of the current study in which RR was predictive of outcome in a group therapy treatment, treatment delivery seems a more likely explanation for discrepant findings than treatment mode.
Within each of the studies by Grilo and colleagues (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007), no significant differences were found in the proportion of participants in each treatment arm who experienced a RR. However, the current study found significantly higher percentages of RRs in the DBT-BED condition (56%, n = 28/50) compared to the ACGT condition (25.5%, n = 13/51). Also, the current study reported significant differences between the outcomes of rapid and non-rapid responders in only one of the two treatment arms, DBT-BED, whereas Grilo and colleagues reported significant differences between RRs and non-RRs in every treatment condition examined (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007).
On a theoretical level, various RR patterns in treatment conditions suggest that RR may be mediated by different mechanisms of action within different treatment conditions (Wilson et al., 1999; Fairburn et al., 1993). One unique aspect of the current study’s examination of RR is its use of a “placebo” psychotherapy comparison control condition instead of a “placebo” pharmacotherapy control condition which was used in two of the three RR studies by Grilo and colleagues (Grilo et al., 2006; Grilo & Masheb, 2007). For example, participants in the placebo control conditions by Grilo and colleagues (Grilo et al., 2006; Grilo & Masheb, 2007) received inert pill placebos that were identical in appearance to the active drug and thus would, at least in theory, generate the same initial expectations regarding treatment effectiveness as the active medication. Unfortunately, treatment expectations were not measured in these studies (Grilo et al., 2006; Grilo & Masheb, 2007).
In this study, the suitability and expectations for success were measured post-randomization. Those who became RRs had significantly higher expectations for success than non-RRs. When comparing participants randomized to DBT-BED vs. ACGT, no significant group differences in suitability or expectations were found, though there was an interesting trend towards lower expectations in those randomized to ACGT (see Results section). It is possible that lower expectations for success among ACGT group participants are related to specific characteristics of a “placebo” psychotherapy control versus an “active” psychotherapy condition. For example, during the first 4 weeks of “active” treatments, such as CBT or DBT, an organized framework is presented with emphasis on learning and practicing specific techniques (Wilson et al., 2002). Because supportive control therapies tend to be less didactic and structured, relatively lower treatment expectations might be generated compared to an active psychotherapy or pill placebo. Expectancy may interact with behavior in an iterative fashion; i.e., those with higher expectations may practice techniques more regularly and thus progress more quickly. Differences in the generation of expectancy may help explain the significantly higher percentage of RRs in DBT vs. ACGT, and shed insight on one of the possible mechanisms of rapid response. Future studies might measure expectancy weekly, along with rates of homework practice, symptom reduction, comprehension of key concepts, etc.
It is important to acknowledge the limitations of this study. While powered to detect treatment effect differences between DBT and ACGT, the sample size (n = 101) may not have afforded adequate statistical power to identify treatment outcomes among RRs and non-RRs. Statistical power was further decreased in comparing RRs and non-RRs within each treatment (e.g., DBT vs. ACGT) condition. The fact that data on treatment suitability and expectations were not gathered pre-randomization limits the ability to assess these variables as potential baseline predictors of RR (and to test some of the speculations listed above). In addition, this study did not originally calculate receiver operating characteristic curves (ROC) to confirm the optimal cut-off point for defining rapid response within this particular sample. At the same time, using an existing definition of RR, as per Grilo and colleagues’ prior work, and producing similar results, lends further support to the external validity of the RR construct in other samples of adults being treated for BED. Of note, when ROC curves were calculated, the ROC curve for percentage change over the first 4 weeks of treatment emerged as the most predictive based on overall area under the curve (AUC). Within that curve, the highest sensitivity and specificity was found for a 59% reduction over the first 4 weeks, which yielded a sensitivity of .61 and a 1- specificity of .31. Given an assumption of some fluctuation between studies regarding the most predictive percentage binge eating reduction, our findings are comparable to those of Grilo, Masheb, & Wilson (2006), who report a reduction of 65% in binge eating by Week 4 as maximizing sensitivity and 1- specificity at .70 and .34, respectively.
In spite of its limitations, this study has important strengths. It represents not only a replication but also an extension of existing studies examining RR in the treatment of BED (Grilo et al., 2006; Grilo & Masheb, 2007; Masheb & Grilo, 2007; Zunker et al., 2010). It found that RR continues to predict improvement in abstinence from binge eating at the12-month follow-up point. It also demonstrates RR to be a significant predictor of outcome in group therapy, replicating the Zunker et al. (2010) findings. Finally, and perhaps most importantly, it shows RR to be a significant predictor of outcome in less established therapeutic treatments for BED, i.e., DBT-BED. As such, the results of this study further support ongoing efforts to personalize therapy through earlier identification of patients less likely to do well for whom additional or alternative treatment options might be of benefit.
Acknowledgments
Funding: This research was funded by a grant from the National Institute of Mental Health, K23MH066330 awarded to Debra Safer
Abbreviations
- RR
rapid response
- RRs
rapid responders
- non-RRs
non-rapid responders
- EOT
end-of-treatment
- BED
binge eating disorder
- DBT-BED
Dialectical Behavior Therapy for BED
- ACGT
active comparison group therapy
- OBE
objective binge eating episode
- EDE
Eating Disorder Examination
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agras WS, Crow SJ, Halmi KA, Mitchell JE, Wilson GT, Kraemer HC. Outcome predictors for the cognitive behavior treatment of bulimia nervosa: Data from a multisite study. American Journal of Psychiatry. 2000;157:1302–1308. doi: 10.1176/appi.ajp.157.8.1302. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer R. Manual for revised Beck Depression Inventory. New York: Psychological Corporation; 1987. [Google Scholar]
- Beck AT, Steer R, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clinical Psychology Review. 1998;8:77–100. [Google Scholar]
- Breslin FC, Sobell MB, Sobell LC, Buchan G, Cunningham CJ. Toward a stepped care approach to treating problem drinkers: The predictive utility of within-treatment variables and therapist prognostic ratings. Addiction. 1997;92:1479–1489. [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Fairburn CG, Agras WS, Walsh BT, Wilson GT, Stice E. Prediction of outcome in bulimia nervosa by early change in treatment. American Journal of Psychiatry. 2004;161:2322–2324. doi: 10.1176/appi.ajp.161.12.2322. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn C, Wilson G, editors. Binge eating: Nature, assessment, and treatment. 12. New York: Guilford Press; 1993. [Google Scholar]
- Fairburn CG, Jones R, Peveler RC, Hope RA. Psychotherapy and bulimia nervosa: Longer-term effects of interpersonal therapy, behavior therapy, and cognitive behavior therapy. Archives of General Psychiatry. 1993;50(6):419–428. doi: 10.1001/archpsyc.1993.01820180009001. [DOI] [PubMed] [Google Scholar]
- Frank JD. Persuasion and healing: A comparative study of psychotherapy. Baltimore: Johns Hopkins University Press; 1961. [Google Scholar]
- Goldfried MR. Toward the delineation of therapeutic change principles. American Psychologist. 1980;35:991–999. doi: 10.1037//0003-066x.35.11.991. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM. Rapid response predicts binge eating and weight loss in binge eating disorder: Findings from a controlled trial of Orlistat with guided self-help cognitive behavioral therapy. Behaviour Research and Therapy. 2007:1–14. doi: 10.1016/j.brat.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Wilson GT. Rapid response to treatment for binge eating disorder. Journal of Consulting and Clinical Psychology. 2006;74(3):602–613. doi: 10.1037/0022-006X.74.3.602. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive- behavior therapy for depression. Clinical Psychology: Science and Practice. 1994;1:138–156. [Google Scholar]
- Jo B, Wang CP, Ialongo NS. Using latent outcome trajectory classes in causal inference. Statistics and its Interface. 2009;2:403–412. doi: 10.4310/sii.2009.v2.n4.a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R, Peveler RC, Hope RA, Fairburn CG. Changes during treatment for bulimia nervosa: A comparison of three psychological treatments. Behavioral Research and Therapy. 1993;31(5):479–485. doi: 10.1016/0005-7967(93)90128-h. [DOI] [PubMed] [Google Scholar]
- Lackner JM, Gudleski GD, Keefer L, Krasner SS, Powell C, Katz LA. Rapid Response to Cognitive Behavior Therapy Predicts Treatment Outcome in Patients With Irritable Bowel Syndrome. Clinical Gastroenterology and Hepatology. 2010 Feb 17; doi: 10.1016/j.cgh.2010.02.007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment of Borderline Personality Disorder. New York: Guilford Press; 1993a. [Google Scholar]
- Linehan MM. Skills training for borderline personality disorder. New York: Guilford Press; 1993b. [Google Scholar]
- Markowitz J, Sacks M. Manual for brief supportive psychotherapy. 2002. Unpublished. [Google Scholar]
- Marrone S, Mitchell JE, Crosby R, Wonderlich S, Jollie-Trottier T. Predictors of response to cognitive behavioral treatment for bulimia nervosa delivered via telemedicine versus face-to-face. International Journal of Eating Disorders. 2009;42:222–227. doi: 10.1002/eat.20603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb RM, Grilo CM. Binge eating disorder: A need for additional diagnostic criteria. Comprehensive Psychiatry. 2000;41:159–162. doi: 10.1016/S0010-440X(00)90041-5. [DOI] [PubMed] [Google Scholar]
- Penava SJ, Otto MW, Maki KM, Pollack MH. Rate of improvement during cognitive behavioral group treatment for panic disorder. Behaviour Research and Therapy. 1998;36:665–674. doi: 10.1016/s0005-7967(98)00035-7. [DOI] [PubMed] [Google Scholar]
- Safer DL, Hugo EM. Designing a control for a behavioral group therapy. Behavior Therapy. 2006;37:120–130. doi: 10.1016/j.beth.2005.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DL, Robinson AH, Jo B. Outcome from a randomized clinical trial of group therapy adapted for binge eating disorder: Comparing Dialectical Behavior Therapy adapted for binge eating to an active comparison control. Behavior Therapy. 2010;41:106–120. doi: 10.1016/j.beth.2009.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safer DL, Telch CF, Chen E. Dialectical Behavior Therapy for Binge Eating and Bulimia. New York: Guilford Press; 2009. [Google Scholar]
- Spitzer RL, Devlin M, Walsh BT, Hasin D, Wing R, Marcus M, et al. Binge eating disorder: A multisite field trial of the diagnostic criteria. International Journal of Eating Disorders. 1992;11(3):191–203. [Google Scholar]
- Stunkard AJ, Messick S. The Three Factor Eating Questionnaire to measure dietary restraint, disinhibition, and hunger. Journal of Psychosomatic Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive- behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(6):894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Group dialectical behavior therapy for binge-eating disorder: A preliminary, uncontrolled trial. Behavior Therapy. 2000;31:569–582. [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of Consulting and Clinical Psychology. 2001;69(6):1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Wilson GT, Fairburn CG, Agras WS, Walsh BT, Kraemer H. Cognitive-behavioral therapy for bulimia nervosa: Time course and mechanisms of change. Journal of Consulting and Clinical Psychology. 2002;70(2):267–274. [PubMed] [Google Scholar]
- Wilson GT, Loeb KL, Walsh BT, Labouvie E, Petkova E, Liu X, et al. Psychological versus pharmacological treatments of bulimia nervosa: Predictors and processes of change. Journal of Consulting and Clinical Psychology. 1999;67(4):451–459. doi: 10.1037//0022-006x.67.4.451. [DOI] [PubMed] [Google Scholar]
- Wiser S, Telch CF. Dialectical behavior therapy for binge-eating disorder. Journal of Clinical Psychology. 1999;55:755–768. doi: 10.1002/(sici)1097-4679(199906)55:6<755::aid-jclp8>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Cao L, Mitchell JE, Wonderlick SA, Crow S, Crosby RD. A receiver operator characteristics analysis of treatment outcome in binge eating disorder to identify patterns of rapid response. Behaviour Research and Therapy. 2010 Sep 6; doi: 10.1016/j.brat.2010.08.007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]


