Abstract
This is the first study to examine the pathways from environmental stressors to substance use among a sample of South African adolescents (N=2,195). The study objective was to assess how environmental stressors might affect cigarette smoking and alcohol use among South African adolescents, and to focus on one mechanism, low well-being, which might mediate this association. Participants consisted of 2,195 Black, mixed ancestry (“Coloured”), Indian, and White youth, aged 12 to 17 years old (mean age=14.6; SD=1.8), recruited via a multi-stage stratified sampling procedure in Durban, Cape Town, and Johannesburg, South Africa. Data were collected via individual in-person structured interviews, administered by trained interviewers in the participant’s preferred language. Structural equation modeling was used to analyze the interrelationships of environmental stressors (violent victimisation, legal and illegal drug availability) and low well-being (depressive symptoms, low self-esteem, health problems) with respect to adolescent cigarette smoking and alcohol use. The results supported our hypotheses: Environmental stressors were related to low well-being which, in turn, was linked to both adolescent smoking and alcohol use. There were also direct pathways from environmental stressors to both adolescent smoking and alcohol use. Smoking and alcohol use were significantly correlated. The findings suggest that environmental stressors may be associated with diminished psychological and physical well-being, as well as smoking and alcohol use, among South African adolescents. Longitudinal research is warranted to further understand the interrelationship of environmental stressors, low well-being, and adolescent substance use, so that these issues may be addressed by South African programmes and policies.
Keywords: South African adolescents, Adolescent substance use, Environmental Stressors, Adolescent Well-being
INTRODUCTION
Smoking and alcohol use are related to numerous morbidities and mortality (Schneider, et al. 2007; Sitas et al., 2004), illegal drug use (Taylor et al. 2003), and the epidemics of violence, tuberculosis, and HIV/AIDS in South Africa (e.g., Seedat et al., 2009; Simbayi et al., 2004; van Zyl Smit et al., 2010). Worldwide, it is estimated that 6 million people will die in the coming year from tobacco use, and that most of these deaths will occur in low- or middle-income countries (Shafey et al., 2009). While smoking-related mortality occurs mostly in adulthood, smoking is usually initiated during adolescence, and the addictive nature of the habit makes quitting extremely difficult (Shafey et al., 2009). Alcohol use is estimated to be responsible for almost 4% of global mortality (Rehm et al., 2009), and 7% of all deaths in South Africa, e.g., due to cancers, cardiovascular diseases, injuries, and violence (Schneider et al., 2007). Alcohol is also involved in about 44% of both traffic injuries and homicides in South Africa (Schneider et al., 2007). Among adolescents, alcohol use is particularly associated with myriad social problems, such as accidents and injury, interpersonal violence, illegal drug use, school failure, and sexual risk behaviour, as well as later alcohol use disorders (Duncan et al., 1997; Schneider et al., 2007).
South Africa continues to have high socio-economic inequalities, and many communities are characterized by extreme poverty and degradation (Mayosi et al., 2009). Young people, in particular, are exposed to numerous environmental stressors within their communities, many of which have detrimental effects on their health and psychological well-being (Barbarin & Richter, 2001; Ensink et al., 1997). Macrosocial factors within these environments, such as violent victimisation and economic deprivation, have been found to be related to both smoking and alcohol use (Kalichman et al., 2006; Thomas et al., 1999). In a related vein, substance availability (the facility with which legal and illegal drugs can be obtained) also predicts both smoking and alcohol use (Parry et al., 2004).
Most investigations on the relationship between stress induced by macrosocial factors (i.e., environmental stressors) and health-risk behaviours, including substance use, have involved samples outside of South Africa (e.g., Patel, 2001), and few investigations have documented the pathways through which environmental stressors predict smoking and alcohol use. The present study, therefore, examined the relationship between environmental stressors and both smoking and alcohol use among a sample of South African adolescents. We focused on one important mechanism, low well-being (including psychological and physical health problems), which may help explain the association of environmental stressors and adolescent substance use.
Environmental Stressors and Adolescent Substance Use
Several studies of adolescents living outside of South Africa, and a few investigations of South African adults, have confirmed that environmental stressors are associated with both smoking and alcohol use (Kalichman et al., 2006; Lambert et al., 2004). There are several forms of environmental stressors that increase the likelihood of substance use, such as violent victimisation, low socioeconomic status, substance availability, and school-based stressors (Boardman et al., 2001; Thomas et al., 1999). For example, among South African adults, Kalichman et al. (2006) found that community stressors, such as violence and crime, were related to substance use. Furthermore, prior research suggests that neighborhood adversities (e.g., violence and drug availability) often coexist (Ward et al., 2001), such that residents of disadvantaged neighborhoods are often exposed to multiple environmental stressors. There is also some evidence that the association of environmental adversity and substance use may be mediated by psychological factors, such as distress (e.g., Boardman et al., 2001).
Environmental Stressors and Low Well-being
Research on the impact of environmental stressors on well-being in adolescence has rarely focused on physical health, and mostly examined the adverse effects of poverty, violence and/or discrimination on post-traumatic stress disorder (PTSD) or externalizing problems, such as aggression (e.g., Ensink et al., 1997). A study conducted by Ward and colleagues (2001), for instance, found that South African adolescents who reported exposure to community violence had more symptoms of both PTSD and depression (as well as anxiety, when the assailant was known to them). Among South African adults, Myer and colleagues (2008) found that greater social capital (less neighborhood crime and more social cohesion) was related to less psychological distress. In the U.S., Prelow et al. (2004) reported that a combined measure of stressful events and neighborhood disadvantage (e.g., assault, ambient safety) predicted depression and delinquency in Black and White youth.
Little research, however, has examined the relationship of environmental stressors and physical health in adolescence. Among adults, there is a considerable literature which demonstrates that environmental stressors are linked with poorer emotional and physical outcomes, such as PTSD, depressive symptoms, compromised immune response, effects on the neuroendocrine systems, and cardiovascular reactivity and disease (Bird et al., 2010; Hamad et al., 2008; Kaminer et al., 2008; Moch et al., 2003). In a study of South African adults, for instance, Williams and co-investigators (2008) found that negative life events predicted both psychological distress and ill health.
Low Well-being and Substance Use
Low well-being, specifically in the form of depression (or depressive symptoms), low self-esteem, or poor general health, is related to smoking as well as to alcohol use (e.g., Fernander et al., 2006). Although there is a small empirical literature on the association of low well-being and substance use among adults in South Africa (e.g., Ward et al., 2008), there are relatively few such studies among South African adolescents.
Panday and colleagues (2007) found that depressive mood predicted smoking among Black and Coloured South African youth. Fernander et al. (2006) also found that depression was associated with tobacco use among females but not males in a school-based sample of adolescents in Cape Town. Wild et al. (2004) showed that less self-esteem was associated with smoking, drinking, and other drug use among male and female South African adolescents.
Smoking and Alcohol Use
We chose to examine adolescent smoking and alcohol use because of their association with numerous physical and psychosocial sequelae. As noted above, tobacco and alcohol use have been linked with cardiovascular diseases, and cancer (Groenewald et al., 2007; Rehm et al., 2009), and alcohol consumption plays a major role in crime, violence, and injury among young people in South Africa (Schneider et al., 2007). In addition, smoking and alcohol use are interrelated (Morrow et al., 2005), and both may be manifestations of a proposed problem behaviour syndrome (Donovan et al., 1988).
In sum, there is evidence of the role of environmental stressors in adult smoking and alcohol use but the pathways have not been elucidated. Furthermore, little is known about the effect of environmental stressors on substance use among South African adolescents. In the present study, we use structural equation modeling to examine the relationship between perceived environmental stressors, low well-being, smoking, and alcohol use among a cohort of South African adolescents. Based on the previous research, we hypothesized that 1) environmental stressors are directly linked with low well-being (psychological and physical health problems); 2) low well-being, in turn, is related to both adolescent smoking and adolescent alcohol use; 3) there are also direct pathways from environmental stressors to both adolescent smoking and adolescent alcohol use; and 4) there is a reciprocal relationship between smoking and alcohol use.
METHOD
Sample
Individual structured interviews were conducted with 2,195 adolescents (54.3% female). The mean (SD) age of participants was 14.6 years (SD=1.8), and the self-reported ethnicity was: Black (41.9%), Coloured (a term used in South Africa to describe people who are of mixed heritage; 24.3%), Indian (18.1%), and White (15.7%).
Procedure
We used a three stage sampling approach to select the participants. In the first instance, census enumeration areas were randomly selected. We first stratified all census enumerator areas (hereafter called “areas”) by ‘race’/population group and socioeconomic status, using 1996 South African population census data. Specifically, each area was categorized as being of one of the four ‘racial’/population groups listed above, based on the predominant ‘racial’/population group of the residents of that area, according to the 1996 census. We used the rate of employment among the heads of households within each enumeration area as the measure of the socioeconomic status of the areas. For each city, we then categorized all areas as being of low socioeconomic status (high risk) versus medium/high socioeconomic status (low risk). We then randomly selected ten high risk and ten low risk areas with predominantly ‘Black,” “Coloured,” “Indian,” and “White” residents for inclusion in the study.
From within each selected area, we randomly selected households. The adolescent participants were recruited from households within the selected census enumerator areas. A starting point was designated randomly for each area, and every tenth household was visited to determine if an eligible adolescent (aged 12–17 years) resided there. When more than one adolescent in a household qualified for the study, one adolescent was selected at random to participate. We obtained both parental consent and adolescent assent prior to commencing the interviews. The interviewers read the questions aloud from a structured interview schedule, while the adolescents followed along on a separate copy of the interview schedule. For the sensitive questions on tobacco and alcohol use, the adolescents marked their responses on the interview schedules themselves. The parents were not present during the interviews, and the respondents were assured that their answers were confidential. Most participants were interviewed by an interviewer of the same gender and ethnicity. The interviews were conducted in the respondents’ language of choice, including English, Afrikaans, SeSotho, or IsiZulu. The interviews lasted for approximately one hour. At the end of the interviews, the participants were given resource lists with contact details of substance abuse services and programmes in their area. The adolescents did not receive monetary compensation for participation. The consent forms and research protocols were approved by the Institutional Review Board of the New York University School of Medicine in the United States, and by the Ethics Committees of the Medical Research Council and the Faculty of Health Sciences of the University of Pretoria, South Africa.
Measures
There were two independent latent variables: environmental stressors and low well-being. The environmental stressors latent variable consisted of three manifest variables: violent victimisation (5 item scale; alpha=0.54; Chavez et al., 1989), availability of legal drugs (3 item scale; alpha=0.76; Johnston et al., 1987), and availability of illegal drugs (2 items; alpha=0.76; Johnston et al., 1987). We chose to examine these environmental variables because prior research suggests that multiple stressors are more deleterious to well-being than one or two stressors (Evans & English, 2002; Prelow et al., 2004), and because there is evidence that covariates of neighborhood poverty, such as violence and drug availability, may be more predictive of psychosocial well-being and physical health than socioeconomic status per se (Barbarin & Richter, 2001; Bird et al., 2010).
The latent variable of low well-being consisted of three manifest variables: depressive symptoms (5 items; alpha=0.68; Derogatis et al., 1974), self-esteem (3 items; alpha=0.73; Brook et al., 1990), and physical health problems (11 item scale; alpha=0.70; Liu & Kaplan, 1999). Two of the Cronbach’s alphas (for violent victimisation and depressive symptoms) were low. However, these scales have been found to predict poor well-being, as well as smoking and alcohol use, in our own work and that of other investigators (Barbarin & Richter, 2001; Brook et al., 1990; Derogatis et al., 1974; Panday et al., 2007; Ward, et al., 2001). All other Cronbach’s alphas for the manifest variables were satisfactory.
For the outcome variables, the current smoking measure (Brook et al., 1990) asked the participant how often he/she had used tobacco in the past 30 days. The response options were: (1) None, (2) A few cigarettes or less a week, (3) 1–5 cigarettes a day, (4) About half pack a day (5) About one pack a day, and (6) More than one pack a day. The other dependent variable, current drinking (Brook et al., 1990), asked the participant about how often he/she drank beer, wine, spirits, or homebrew. Response options included (1) Never, (2) Less than once a week (3), Once a week to several times a week, (4) 1 or 2 drinks a day, and (5) 3 or more drinks every day.
Data Analysis
Latent variable structural equation models were employed to examine the empirical credibility of the proposed processes associated with adolescent smoking and adolescent alcohol use. In order to account for the influences of the youths’ gender, age, and ethnicity, and the adolescents’ reports of their household amenities and hunger, on the measurement and structural models, we used partial covariance matrices as the input matrices, as suggested by Newcomb & Bentler (1988). This strategy allows one to statistically control for the effects of these variables without hypothesizing exactly where they influence the model. Thus, this strategy should afford us a more generalizable model. Since we used stratification by ethnicity and socioeconomic status (SES) to obtain our data, this strategy also allowed us to partially account for possible spatial dependence among the geographic areas from which our sample was selected. The partial covariance matrices were created by statistically partialing out the effects of the demographic and geographic factors noted above on each of the original manifest variables. The partial Pearson correlations among the variables derived from the covariance matrices, as well as the variable means and standards deviations, are presented in Table 1 (see Table 1).
Table 1.
Partial Pearson Correlation Matrix of the Manifest Variables.
| Variables | Smoking | Alcohol Use | Depression | Self- Esteem | Physical Health Problems | Violent Victimisation | Availability of Legal Drugs | Availability of Illegal Drugs |
|---|---|---|---|---|---|---|---|---|
| Smoking | 1.00 | |||||||
| Alcohol Use | .31 | 1.00 | ||||||
| Depression | .08 | .15 | 1.00 | |||||
| Self-Esteem | −.06 | −.80 | −.21 | 1.00 | ||||
| Physical Health Problems | .06 | .11 | .53 | −.21 | 1.00 | |||
| Violent Victimisation | .20 | .25 | .15 | −.70 | .21 | 1.00 | ||
| Availability of Legal Drugs | .09 | .07 | .01 | −.03 | .01 | .08 | 1.00 | |
| Availability of Illegal Drugs | .12 | .12 | .08 | −.08 | .07 | .11 | .51 | 1.00 |
| X̄ (SD) | 1.3 (.82) | 1.3 (.60) | 9.4 (3.9) | 10.2 (1.9) | 18.4 (6.4) | 5.6 (2.2) | 4.5 (2.0) | 2.0 (2.1) |
Note: Age, gender, ethnicity, household amenities, and hunger were statistically controlled.
We then estimated the measurement and structural models hypothesized above by using Mplus 6.1 (Muthén & Muthén, 2010). The distributions of smoking and alcohol use were skewed and non-normal. The joint distribution between smoking and alcohol use were also skewed. For the joint distribution of smoking and alcohol use, only 3 participants reported both the highest score for smoking (6=more than one pack a day), and the highest alcohol use score (5=3 or more drinks every day). The Pearson correlation between smoking and alcohol use was 0.29 (p<0.001). To account for the non-normal distribution of the model variables, we used the Mplus maximum likelihood with robust standard errors (MLR) as the estimator. Since we used data obtained by stratification, cluster sampling, and sampling with an unequal probability of selection, participants between cluster enumeration areas had an unequal probability of selection, and participants within each area were non-independent. As mentioned above, we controlled for ethnicity and SES to take into account the unequal probability of selection due to stratification. In addition, we used the population size of each area as the sample weight. With sampling weights, as suggested by Stapleton (2006) and by Asparouhov (2005), we used the pseudo-maximum likelihood (PML) estimation method developed by Skinner (1989). Using Mplus, we implemented this approach by specifying TYPE=COMPLEX in the ANALYSIS command in conjunction with the CLUSTER and WEIGHT options of the VARIABLE command (Asparouhov, 2005; Asparouhov & Muthén, 2005).
There were no missing data for the measurement of adolescent smoking or alcohol use. Less than 2% of the data were missing for some of the independent variables. We used the Mplus default option (i.e., full information maximum likelihood approach; Little & Rubin, 2002) to treat missing data. The advantage of this option is that the results are less likely to be biased even if the data are not missing completely at random (Muthén, Kaplan, & Hollis, 1987). We chose two indices to assess the fit of the models: (a) Bentler’s comparative fit index (CFI); and (b) the root mean square error of approximation (RMSEA). For the CFI, values between .90 and 1.0 indicate that the model provides a good fit for the data, while the RMSEA should be below .10.
Results
For the whole hypothesized model (the measurement model and the structural model), the following fit indices were obtained: Bentler’s CFI=0.90, and RMSEA=0.061. The model’s chi-square value was 146.3 with 16 degrees of freedom (df). The scaling correction factor for robust standard errors was 1.733. These results reflect a satisfactory model fit. Table 2 presents the results for the measurement model. All factor loadings were significant (p<0.001). The findings show that the indicator variables were satisfactory measures of the latent constructs. (See Table 2.)
Table 2.
Factor Loadings for the Measurement Model.
| Latent Variables: | ||
|---|---|---|
| Low Well-being | Environmental Stressors | |
| Manifest Variables: | ||
| Depression | b=1.00 | -- |
| Self-Esteem | b=−0.19 z=−8.29*** |
-- |
| Physical Health Problems | b=1.51 z=10.00*** |
-- |
| Violent Victimisation | -- | b=1.00 |
| Availability of legal drugs | -- | b=3.67 z=4.53*** |
| Availability of illegal drugs | -- | b=5.15 z=4.10*** |
p<0.001;
Age, gender, ethnicity, household amenities, and hunger were statistically controlled;
Factor loadings weighted by enumeration area (EA) population size.
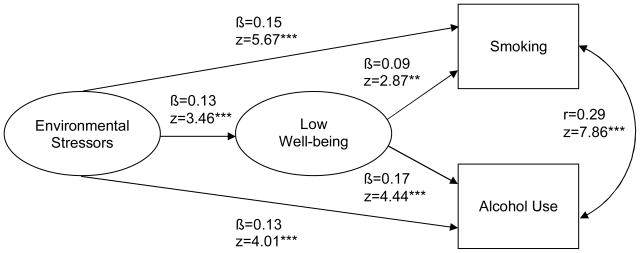
For the structural model, standardized parameter estimates, as well as the associated z-statistics for the sample, are presented in Figure 1. As noted in Figure 1, the data are consistent with the hypothesized model. More specifically, our findings suggest that: 1) environmental stressors were associated with the participants’ low well-being (β=0.13; z=3.46), which in turn was related to both smoking (β=0.09; z=2.87), and alcohol use (β=0.17; z=4.44); 2); environmental stressors had a direct effect on adolescent smoking (β=0.15; z=5.67); and 3) environmental stressors had a direct effect on adolescent alcohol use (β=0.13; z=4.01). In addition, the participants’ smoking and alcohol use were significantly associated (r=0.29; z=7.86). All pathways were statistically significant (p<0.01). (See Figure 1.)
Figure 1.
Structural Equation Model of Environmental Stressors, Low Well-being, Adolescent Smoking, and Adolescent Alcohol Use
Notes:
1. Maximum likelihood parameter estimates with standard errors and a chi-square test statistic (MLR) that are robust to non-normality and non-independence of observations were used as the estimator;
2. CFI=0.90; RMSEA=0.061; df=16;
3. **p<0.01; ***p<0.001;
4. Age, gender, ethnicity, household amenities, and hunger were statistically controlled; Note: Age, gender, ethnicity, household amenities, and hunger were statistically controlled.
An examination of the total effects of each latent variable on adolescent smoking and adolescent alcohol use helps in the interpretation of the structural coefficients. The standardized total effects (z-statistic) of environmental stressors were 0.16 (6.19) for smoking, and 0.15 (4.88) for alcohol use. Low well-being had total effects (z-statistic) of 0.09 (2.87) and 0.17 (4.44) for smoking and alcohol use, respectively. The z values of the total effects of both environmental stressors and low well-being on smoking and on alcohol use were all statistically significant (p<0.01). Thus, our findings showed that environmental stressors and low well-being both had a significant total effect on adolescent smoking and adolescent alcohol use. A test of the indirect effects of environmental stressors on smoking [β=0.01 (z=2.11)] and on alcohol use [β=0.02 (z=2.62)], as partially mediated by low well-being, were also statistically significant (p<0.05). The analyses of both the direct and the indirect effects controlled for age, gender, ethnicity, household amenities, and hunger, and were weighted by enumeration area population size.
Test of Alternative Models
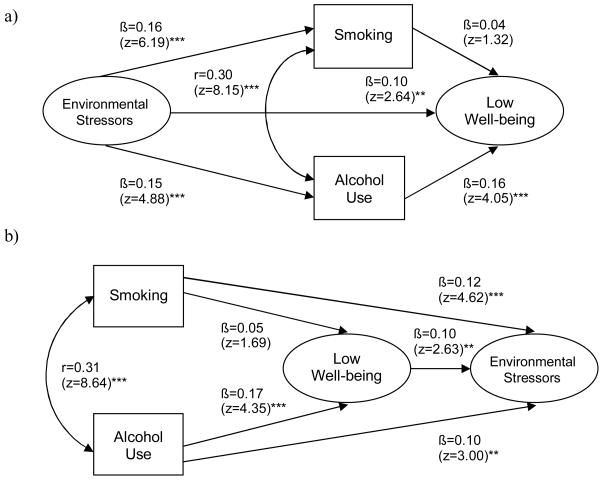
As our cross-sectional data did not allow for the temporal ordering of the constructs, we used the same analytic approach (described above) to test two alternative models. That is, we examined whether there might be statistically significant pathways among the latent constructs other than those supported by our obtained model, shown in Figure 1. For example, smoking and alcohol use were tested as mediators of the relationship between environmental stressors and low well-being. The two alternative models differed from one and other and from the obtained model.
The results of the supplemental path analyses are shown in Figure 2. Although both alternative models had the same CFI and RMSEA as the obtained model, the link between low well-being and smoking was not statistically significant in either alternative model. (See Figure 2.) Because prior research has demonstrated an association between low well-being and adolescent smoking (e.g., Panday et al., 2007; Wild et al., 2004), we decided, therefore, to focus our interpretation on the obtained model in Figure 1.
Figure 2.
Alternative Structural Equation Models of Environmental Stressors, Low Well-being, Adolescent Smoking, and Adolescent Alcohol Use
Notes:
1. Maximum likelihood parameter estimates with standard errors and a chi-square test statistic (MLR) that are robust to non-normality and non-independence of observations were used as the estimator;
2. CFI=.90; RMSEA=.061; df=16;
3. ** p<.01; *** p<.001;
4. Age, gender, ethnicity, household amenities, and hunger were statistically controlled;
5. Analyses were weighted by enumeration area (EA) population size.
DISCUSSION
Overall, our results showed the importance of environmental stressors to lower mental and physical well-being, and to greater substance use, among a cohort of adolescents in three South African cities. Our findings add to the few existing studies on environmental stressors and substance use among South African adolescents, and empirically identify mechanisms which may operate between environmental stressors and smoking and alcohol use among adolescents in South Africa.
Environmental Stressors and Substance Use
The direct pathways shown in our model from environmental stressors to both smoking and alcohol use are consistent with previous studies on some aspects of the environment and South African adults or adolescents residing outside of South Africa. In the U.S., for instance, Lambert et al. (2004) found that adolescents who perceived greater environmental stressors were more likely to use tobacco, alcohol, and marijuana. Although adolescents who have easy access to licit or illicit drugs are more likely to use them (Morojele et al., 2002; Parry et al., 2004), additional factors may underlie the relationship of environmental stressors and adolescent substance use. One such factor, based on social learning theory, is the role modeling of antisocial behaviour present in the broader macro-level environment (e.g., Boardman et al., 2001; Parry et al., 2004). In this vein, King et al. (2003) reported that the most powerful predictor of recent smoking among a cohort of South African adolescents was knowing an adult who engaged in antisocial behaviour. Furthermore, the presence of gang-related violence and drug activity in many South African neighborhoods may lead adolescents to perceive some environmental stressors as normative behaviour (Norman et al., 2007; Ward, 2007). Thus, adolescents in these settings may be not only prone to imitation of deviant behaviours from the broader environment, but also to affiliating with peers who engage in substance use.
Environmental Stressors and Low Well-being
The findings of the present study revealed that environmental stressors were linked to low well-being among the adolescents. Environmental stressors can diminish adolescent well-being by the internalization of a poor self-image, physiological dysregulation, or disrupted social processes (Boardman et al., 2001; McEwan, 2008; Murali & Chen, 2005; Sampson, 1992; Taylor, 2000; Ward, 2007). The adolescent’s perception of greater environmental stressors may also induce less well-being by presenting a threat to their sense of safety (Barbarin & Richter, 2001; Ward et al., 2001). Furthermore, in South Africa, environmental stressors often are associated with other factors that lead to poor physical and mental well-being, such as lack of access to healthcare (Gilson & McIntyre, 2007), cooking fuel pollution (Thomas et al., 1999), and poor diet (Victora et al., 2008). It is not surprising, therefore, that adolescents exposed to stressful neighborhoods are more likely to experience emotional, behavioural, and physical problems (Sampson, 1992).
Low Well-being and Substance Use
Our finding regarding the association of low well-being and substance use is partially consistent with previous studies of South African youth, which have focused on specific components of well-being. In addition, we found that low well-being partially mediated the association between environmental stressors and tobacco and alcohol use. Environmental stressors, may undermine the youth’s ability to cope with adversities, as well as induce both psychological and physiological emotional dysregulation (e.g., McEwan, 2008; Murali & Chen, 2005). Thus, adolescents may turn to cigarettes and/or alcohol in an attempt to temporarily dull the experience of stress, increase well-being, and regain homeostasis (e.g., Dawes et al., 2000).
Alternative Models
The results of the present study also provide support for the alternative models. According to the findings of the first alternate model (Figure 2a), environmental stressors predicted low well-being both directly and indirectly, via the mediation of adolescent alcohol use. This alternative model may suggest that stressful environments present norms and role-models of alcohol use, and facilitate youth access to alcohol (Parry et al., 2004; Morojele et al., 2003). The use of alcohol, in turn, diminishes the youth’s physical and psychological well-being. The findings of this alternative model are consistent with some prior research (e.g., Luthar & Cushing, 1997), which showed that adolescent alcohol use is a predictor of low well-being. However, there is inconsistency in the literature regarding the direction of the relationship between adolescent substance use and low well-being (Saban & Flisher, 2010).
The results of the test of the second alternative model (Figure 2b) suggest that youth who drink alcohol are at-risk for less well-being, and that adolescents who smoke and drink report greater exposure to environmental stressors. These results are consistent with theories which posit that individuals seek out environments that are commensurate with their own behaviours. As noted above, however, previous investigations have reported a statistically significant relationship between smoking and well-being among adolescents (e.g., Mckenzie et al., 2010), which was not supported by either alternative model. In addition, the obtained model shown in Figure 1 is based, in part, on our assumption that personality characteristics, such as low well-being, precede specific behaviours.
Limitations
There are some limitations to the findings. First, we did not assess gender and ethnic differences, which prior research has shown can affect psychological and physical well-being, and substance use (e.g., Fernander et al., 2006; Panday et al., 2007; Read & Gorman, 2006; Ward et al., 2008; Wild et al., 2004). However, we did control for gender and ethnicity in our models. Second, there may be spatial dependence among proximate geographic areas, such as those included in the present study, and we could not take this possible effect into account. However, our model did control for the participants’ enumeration areas as well as their report of household amenities, and hunger. Third, it is unclear whether our results would generalize to adolescents in other urban communities or rural areas in South Africa, although aspects of our model are supported by studies conducted outside of South Africa. Fourth, given the weak evidence for the direction of the pathways in our model, our results would need to be confirmed by longitudinal research.
Conclusion
In sum, we have tried to elucidate some of the mechanisms that may be operative in explaining the pathways from environmental stressors to substance use among South African adolescents. Although our results support the interrelationships of environmental stressors, low well-being, and substance use among South African adolescents in three cities, longitudinal research is warranted to confirm how these constructs are linked. It is possible that there are bidirectional relationships between some of the constructs included in our model, and that, furthermore, these relationships may be age-variant. For instance, low well-being in early adolescence may predict cigarette smoking which, in turn, affects well-being in late adolescence. The identification of additional mechanisms, such as the peer group, also has the potential to afford a greater understanding of processes that mediate the relationship of environmental stressors and adolescent substance use. Nevertheless, our findings suggest that a better understanding of the association between environmental stressors and adolescent substance use could contribute to more effective public policy and prevention programmes that improve the lives of South African youth.
Acknowledgments
The authors wish to thank Ms. S’bonisile Zama, of the Human Sciences Research Council, South Africa, and Ms. Sebenzile Nkosi, of the Medical Research Council, South Africa, for their assistance with accessing the census level data.
References
- Asparouhov T. Sampling weights in latent variable modeling. Structural Equation Modeling. 2005;12:411–434. [Google Scholar]
- Asparouhov T, Muthén B. Multivariate statistical modeling with survey data. Proceedings of the Federal Committee on Statistical Methodology Research Conference; 2005. Retrieved October 28, 2010, from http://www.fcsm.gov/05papers/Asparouhov_Muthen_IIA.pdf. [Google Scholar]
- Barbarin OA, Richter L. Economic status, community danger and psychological problems among South African children. Childhood. 2001;8:115–133. doi: 10.1177/0907568201008001007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird CE, Seeman T, Escarce J, Basurto-Dávila R, Finch BK, Dubowitz T, et al. Neighborhood socioeconomic status and biological “wear & tear” in a nationally representative sample of U.S. adults. Journal of Epidemiology and Community Health. 2010;64:860–865. doi: 10.1136/jech.2008.084814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boardman JD, Finch BK, Ellison CG, Williams DR, Jackson JS. Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior. 2001;42:151–165. [PubMed] [Google Scholar]
- Brook JS, Brook DW, Gordon AS, Whiteman M, Cohen P. The psychosocial etiology of adolescent drug use: A family interactional approach. Genetic, Social, and General Psychology Monographs. 1990;116:111–267. [PubMed] [Google Scholar]
- Chavez EL, Oetting ER, Swaim RC. Dropout and delinquency: Mexican- American and Caucasian Non-Hispanic youth. Journal of Clinical Child Psychology. 1989;23:47–55. [Google Scholar]
- Dawes MA, Antelman SM, Vanyukov MM, Giancola P, Tarter RE, Susman EJ, et al. Developmental sources of variation in liability to adolescent substance use disorders. Drug and Alcohol Dependence. 2000;61:3–14. doi: 10.1016/s0376-8716(00)00120-4. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Donovan JE, Jessor R, Costa FM. Syndrome of problem behavior in adolescence: A replication. Journal of Consulting and Clinical Psychology. 1988;56:762–765. doi: 10.1037//0022-006x.56.5.762. [DOI] [PubMed] [Google Scholar]
- Duncan SC, Alpert A, Duncan TE, Hops H. Adolescent alcohol use development and young adult outcomes. Drug and Alcohol Dependence. 1997;49:39–48. doi: 10.1016/s0376-8716(97)00137-3. [DOI] [PubMed] [Google Scholar]
- Ensink K, Robertson BA, Zissis C, Leger P. Post-traumatic stress disorder in children exposed to violence. South African Medical Journal. 1997;87:1526–1530. [PubMed] [Google Scholar]
- Evans GW, English K. The environment of poverty: multiple stressor exposure, psychophysiological stress, and socioemotional adjustment. Child Development. 2002;73:1238–1248. doi: 10.1111/1467-8624.00469. [DOI] [PubMed] [Google Scholar]
- Fernander AF, Flisher AJ, King G, Noubary F, Lombard C, Price M, et al. Gender differences in depression and smoking among youth in Cape Town, South Africa. Ethnicity & Disease. 2006;16:41–50. [PubMed] [Google Scholar]
- Gilson L, McIntyre D. Post-apartheid challenges: household access and use of health care in South Africa. International Journal of Health Services. 2007;37:673–691. doi: 10.2190/HS.37.4.f. [DOI] [PubMed] [Google Scholar]
- Groenewald P, Vos T, Norman R, Laubscher R, van Walbeek C, Saloojee Y, et al. Estimating the burden of disease attributable to smoking in South Africa in 2000. South African Medical Journal. 2007;97(8 Pt 2):674–681. [PubMed] [Google Scholar]
- Hamad R, Fernald LCH, Karlin DS, Zinman J. Social and economic correlates of depressive symptoms and perceived stress in South African adults. Journal of Epidemiology and Community Health. 2008;62:538–544. doi: 10.1136/jech.2007.066191. [DOI] [PubMed] [Google Scholar]
- Johnston JD, Bachman JG, O’Malley PM. Monitoring the Future Study, 1986. Ann Arbor, Michigan: Institute for Social Research, University of Michigan, Survey Research Center; 1987. [Google Scholar]
- Kalichman SC, Simbayi LC, Kagee A, Toefy Y, Jooste, Cain D, et al. Associations of poverty, substance use, and HIV transmission risk behaviors in three South African communities. Social Science & Medicine. 2006;62:1641–1649. doi: 10.1016/j.socscimed.2005.08.021. [DOI] [PubMed] [Google Scholar]
- Kaminer D, Grimsrud A, Meyer L, Stein DJ, Williams DR. Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in South Africa. Social Science & Medicine. 2008;67:1589–1595. doi: 10.1016/j.socscimed.2008.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King G, Flisher AJ, Mallett R, Graham J, Lombard C, Rawson T, et al. Smoking in Cape Town: Community influences on adolescent tobacco use. Preventive Medicine. 2003;36:114–123. doi: 10.1006/pmed.2002.1128. [DOI] [PubMed] [Google Scholar]
- Lambert SF, Brown TL, Philips CM, Ialongo NS. The relationship between perceptions of neighborhood characteristics and substance use among urban African American adolescents. American Journal of Community Psychology. 2004;34:205–218. doi: 10.1007/s10464-004-7415-3. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. Statistical Analysis With Missing Data. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- Liu X, Kaplan HB. Explaining gender differences in symptoms of subjective distress in young adolescents. Stress Medicine. 1999;15:41–51. [Google Scholar]
- Luthar SS, Cushing G. Substance use and personal adjustment among disadvantaged teenagers: A six-month prospective study. Journal of Youth and Adolescence. 1997;26:353–372. [Google Scholar]
- Mayosi B, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet. 2009;374:934–947. doi: 10.1016/S0140-6736(09)61087-4. [DOI] [PubMed] [Google Scholar]
- McEwan BS. Central effects of stress hormones in health and disease: Understanding the protective and damaging effects of stress and stress mediators. European Journal of Pharmacology. 2008;583:174–185. doi: 10.1016/j.ejphar.2007.11.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie M, Olsson CA, Jorm AF, Romaniuk H, Patton GC. Association of adolescent symptoms of depression and anxiety with daily smoking and nicotine dependence in young adulthood: findings from a 10-year longitudinal study. Addiction. 2010;105:1652–1659. doi: 10.1111/j.1360-0443.2010.03002.x. [DOI] [PubMed] [Google Scholar]
- Moch SL, Panz VR, Joffe BI, Havlik I, Moch JD. Longitudinal changes in pituitary-adrenal hormones in South African women with burnout. Endocrine. 2003;21:267–272. doi: 10.1385/ENDO:21:3:267. [DOI] [PubMed] [Google Scholar]
- Morojele NK, Flisher AJ, Muller M, Ziervogel CF, Reddy P, Lombard CJ. Measurement of risk and protective factors for drug use and anti-social behavior among high school students in South Africa. Journal of Drug Education. 2002;32:25–39. doi: 10.2190/MJDD-PC1G-4KUH-C1YW. [DOI] [PubMed] [Google Scholar]
- Morrow S, Panday S, Richter L. Where we’re at and where we’re going: Young People in South Africa in 2005. Johannesburg: Umsobomvu Youth Fund; 2005. [Google Scholar]
- Muthén B, Kaplan D, Hollis M. On structural equation modeling with data that are not missing completely at random. Psychometrika. 1987;52:431–462. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthen & Muthen; 2010. Retrieved 2 November, 2010, from http://www.statmodel.com/download/usersguide/Mplus%20Users%20Guide%20v6.pdf. [Google Scholar]
- Murali R, Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Annals of Behavioral Medicine. 2005;30:155–163. doi: 10.1207/s15324796abm3002_8. [DOI] [PubMed] [Google Scholar]
- Myer L, Stein DJ, Grimsrud A, Seedat S, Williams DR. Social determinants of psychological distress in a nationally-representative sample of South Africans. Social Science & Medicine. 2008;66:1828–1840. doi: 10.1016/j.socscimed.2008.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb MD, Bentler PM. Impact of adolescent drug use and social support on problems of young adults: A longitudinal study. Journal of Abnormal Psychology. 1988;97:64–75. doi: 10.1037//0021-843x.97.1.64. [DOI] [PubMed] [Google Scholar]
- Norman R, Bradshaw D, Schneider M, Jewkes R, Mathews S, Abrahams N, et al. Estimating the burden of disease attributable to interpersonal violence in South Africa in 2000. South African Medical Journal. 2007;97:653–656. [PubMed] [Google Scholar]
- Panday S, Reddy SP, Ruiter RAC, Bergström E, De Vries H. Determinants of smoking among adolescents in the Southern Cape-Karoo region, South Africa. Health Promotion International. 2007;22:207–217. doi: 10.1093/heapro/dam018. [DOI] [PubMed] [Google Scholar]
- Parry C, Morojele NK, Saban A, Flisher AJ. Brief report: Social and neighborhood correlates of adolescent drunkenness: A pilot study in Cape Town, South Africa. Journal of Adolescence. 2004;27:369–374. doi: 10.1016/j.adolescence.2003.09.005. [DOI] [PubMed] [Google Scholar]
- Patel V. Poverty, inequality and mental health in developing countries. In: Leon D, Walt G, editors. Poverty, inequality and mental health. Oxford: Oxford University Press; 2001. pp. 247–262. [Google Scholar]
- Prelow HM, Danoff-Burg S, Swenson RR, Pulgiano D. The impact of ecological risk and perceived discrimination on the psychological adjustment of African American and European American youth. Journal of Community Psychology. 2004;32:375–389. [Google Scholar]
- Read JG, Gorman BK. Gender inequalities in US adult health: The interplay of race and ethnicity. Social Science & Medicine. 2006;62:1045–1065. doi: 10.1016/j.socscimed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teeawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Saban A, Flisher AJ. The association between psychopathology and substance use in young people: a review of the literature. Journal of Psychoactive Drugs. 2010;42:37–47. doi: 10.1080/02791072.2010.10399784. [DOI] [PubMed] [Google Scholar]
- Sampson RJ. Family management and child development: Insights from social disorganization theory. In: McCord J, editor. Facts, frameworks and forecasts: Advances in criminological theory. Vol. 3. New Brunswick, NJ: Transaction Publishers; 1992. pp. 63–93. [Google Scholar]
- Schneider M, Norman R, Parry C, Bradshaw D, Plüddemann A the South African Comparative Risk Assessment Collaborating Group. Estimating the burden of disease attributable to alcohol use in South Africa in 2000. South African Medical Journal. 2007;97:664–672. [PubMed] [Google Scholar]
- Seedat M, Van Niekerk A, Jewkes R, Suffia S, Ratele K. Violence and injuries in South Africa: Prioritizing an agenda for prevention. The Lancet. 2009;374:1011–1022. doi: 10.1016/S0140-6736(09)60948-X. [DOI] [PubMed] [Google Scholar]
- Shafey O, Eriksen M, Ross H, MacKay J. The Tobacco Atlas. 3. Atlanta, GA: The American Cancer Society; 2009. [Google Scholar]
- Simbayi L, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. Alcohol use and sexual risks for HIV infection among men and women receiving sexually transmitted infection clinic services in Cape Town, South Africa. Journal of Studies on Alcohol. 2004;65:434–442. doi: 10.15288/jsa.2004.65.434. [DOI] [PubMed] [Google Scholar]
- Skinner CJ. Domain means, regression and multivariate analysis. In: Skinner CJ, Holt D, Smith TMF, editors. Analysis of Complex Surveys. New York: John Wiley & Sons; 1989. pp. 59–87. [Google Scholar]
- Sitas F, Urban M, Bradshaw D, Kielowski D, Bah S, Peto R. Tobacco attributable deaths in South Africa. Tobacco Control. 2004;13:396–399. doi: 10.1136/tc.2004.007682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stapleton LM. An assessment of practical solutions for structural equation modeling with complex sample data. Structural Equation Modeling. 2006;13:28–58. [Google Scholar]
- Taylor RD. An examination of the association of African American mothers’ perceptions of their neighborhoods with their parenting and adolescent adjustment. Journal of Black Psychology. 2000;26:267–287. [Google Scholar]
- Taylor M, Junabhai CC, Naidoo K, Kleinschmidt I, Diamini SB. An epidemiological perspective of substance use among high school pupils in rural KwaZulu-Natal. South African Medical Journal. 2003;93:136–140. [PubMed] [Google Scholar]
- Thomas EP, Seager JR, Vilhjoen E, Potgieter F, Rossouw A, Tokota B, et al. Household environment and health in Port Elizabeth, South Africa. 1999 Retrieved 16 September, 2009, from the Medical Research Counsel of South Africa Web site: http://www.mrc.ac.za/healthdevelop/householdpart1.pdf.
- van Zyl Smit RN, Pai M, Yew WW, Leung CC, Zumla A, Bateman ED, et al. Global lung health: the colliding epidemics of tuberculosis, tobacco smoking, HIV and COPD. European Respiratory Journal. 2010;35:27–33. doi: 10.1183/09031936.00072909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet. 2008;371:340–357. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward CL. It feels like it’s the end of the world: Cape Town’s youth talk about gangs and community violence. 2007 Retrieved 14 September, 2009, from South African Human Research Council Web site: http://www.hsrc.ac.za/ResearchPublication-20100.phtml.
- Ward CL, Flisher AJ, Zissis C, Muller M, Lombard C. Exposure to violence and its relationship to psychopathology in adolescents. Injury Prevention. 2001;7:297–301. doi: 10.1136/ip.7.4.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward CL, Mertens JR, Flisher AJ, Bresick GF, Sterling SA, Little F, et al. Prevalence and correlates of substance use among South African primary care clinic patients. Substance Use & Misuse. 2008;43:1395–1410. doi: 10.1080/10826080801922744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wild LG, Flisher AJ, Bhana A, Lombard C. Associations among adolescent risk behaviours and self-esteem in six domains. Journal of Child Psychology and Psychiatry. 2004;45:1454–1467. doi: 10.1111/j.1469-7610.2004.00851.x. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Williams S, Mohammed SA, Moomal H, Stein D. Perceived discrimination, race and health. Social Science & Medicine. 2008;67:441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]