Abstract
Myeloid sarcoma (MS) is a neoplasm of immature granulocytes, monocytes, or both involving extramedullary sites. MS with no evidence of leukemia (nonleukemic MS) is very rare and the initial diagnosis can be difficult. This report describes an unusual case of nonleukemic MS of the liver in a 16-year-old patient presenting as debilitating hepatomegaly. A liver biopsy revealed diffuse infiltration by neoplastic cells of myeloid lineage (CD68, myeloperoxidase). A bone marrow biopsy showed no evidence of medullary involvement. The patient subsequently developed heart failure. Autopsy revealed infiltration of most organs by neoplastic cells but failed to identify abnormal myeloid cells in bone marrow.
Keywords: Myeloid sarcoma, Liver, Leukemia
Introduction
Myeloid sarcoma (MS) is a localized tumor composed of immature myeloid precursor cells in extramedullary sites. Most MS cases are associated with leukemia. On rare occasions, MS may occur without overt leukemia or other myeloproliferative disorders [1, 2]. The most common sites of these so-called nonleukemic MS are skin, central nervous system, lymph nodes, gastrointestinal tract, and gall bladder [2, 3]. Here we present a case of disseminated MS of the liver in a patient without leukemia.
Case report
A 16-year-old girl presented to this hospital for feeling fatigued for a few weeks. On physical examination, the liver was palpable at 3 cm below the right costal margin and the spleen was palpable at 2 cm below the left costal margin. The patient had no history of liver disease and had never smoked or drunk alcohol. Blood tests revealed an elevated alanine aminotransferase at 283 IU/L and alkaline phosphatase (ALP) at 630 IU/L. ALP isoenzyme test revealed that the increase of ALP was due to liver. Blood counts and bilirubin were normal. Hepatitis B surface antigen (HBsAg) and antibodies to hepatitis C virus (anti-HCV) were negative. Antinuclear antibodies and antimitochondrial antibodies were all negative. The serum ceruloplasmin level was normal. Ultrasound examination revealed an enlarged liver with a span of 21.5 cm. The portal vein was in normal size. Computed tomography confirmed enlarged liver with lower density than the spleen.
A liver biopsy revealed generally normal hepatic architecture. However, the sinusoids were profusely infiltrated with large neoplastic cells. The great majority of the infiltrating cells were myeloid precursors with open chromatin, prominent nucleoli, round/oval nuclear contours, and abundant eosinophilic cytoplasm. The neoplastic cells were positive for leukocyte common antigens CD45, CD43, CD20, CD68, and myeloperoxidase (MPO). CD3, CD10, HLA-DR, CD35, CD79a, and chromogranin were negative. Bone marrow aspirate and biopsy were slightly hypercellular with trilineage hematopoiesis. No evidence of leukemia, myelodysplasia, or any type of myeloproliferative disorder was identified. A diagnosis of nonleukemic MS of the liver was made.
One week after the liver biopsy, the patient experienced acute cardiac failure. On Doppler ultrasound, reduced cardiac output and moderate amount of pericardial effusion were noted. A chest X-ray discovered pleural effusion on the left side. Subsequently, the patient experienced severe lung infection with fever and chest pain. She was placed on broad-spectrum antibiotics for pneumonia and dialysis for pulmonary edema. Despite the efforts, the patient’s condition continued to decline and she died before antileukemic chemotherapy could be implemented.
An autopsy revealed grossly enlarged liver and spleen. The lung, spleen, kidney, and intestine were markedly congested. About 700 ml of pleural fluid, 800 ml of ascites, and 120 ml of straw-colored transudate in the pericardial sac were revealed.
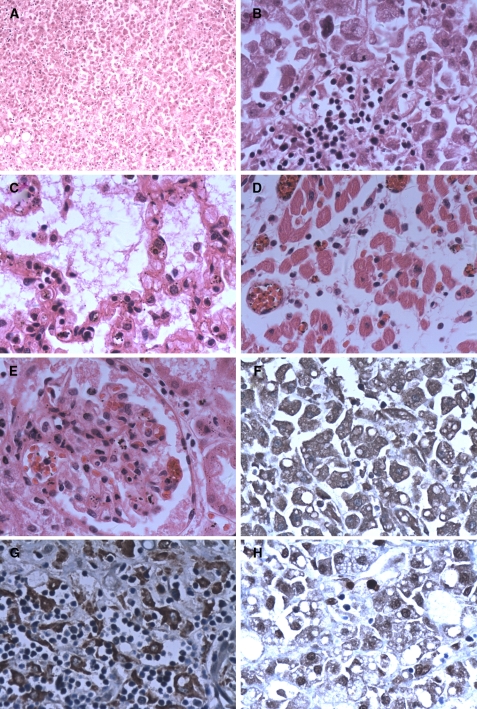
On histological examination, focal myocardial necrosis was noticeable. The liver (Fig. 1a, b), interstitial tissue of lung (Fig. 1c), cardiac ventricles (Fig. 1d), kidneys (Fig. 1e), adrenal glands, intestines, hilar lymph nodes, and mesenteric lymph nodes were diffusely infiltrated by myelocytic leukemic cells. Immunohistochemical stains showed that the tumor cells were positive for CD20 (Fig. 1f), CD68 (Fig. 1g), and myeloperoxidase (Fig. 1h), and negative for CD3 and CD10. Bone marrow in the sternum, humerus, and ilium showed severe myeloid hyperplasia but no abnormal myeloid cells.
Fig. 1.
HE and immunostaining of major organs. a–h: HE staining. a Liver, ×100; b liver, ×400; c lung, ×400; d heart, ×400; e kidney, ×400; f–h: immunohistochemical staining of liver. f CD20 staining, ×400; g CD68 staining, ×400; h MPO staining, ×400
Discussion
We presented a rare case of nonleukemic MS of the liver. No abnormal myeloid cells were found in the bone marrow. Considering the lack of peripheral blood and bone marrow involvement, extensive multiorgan dissemination of MS was surprising.
Due to its rarity, nonleukemic MS is frequently misdiagnosed. The most common sites for the tumor involve skull, axial skeleton, lymph nodes, and skin. Presentation as diffuse infiltration of the liver is very unusual. On reviewing the literature, we found only three similar cases (Table 1) [4–6]. The presenting feature was jaundice in two cases and fever in one. Liver function test of all three patients showed elevation of ALP (145–1,082 IU/L), which may be due to an impairment of the hepatobiliary system. The differential diagnosis includes: [1] hepatobiliary disease: biliary obstruction due to stones, stricture, and tumor; [2] autoimmune: primary biliary cirrhosis and sclerosing cholangitis; [3] infiltrative granulomatous hepatitis, fatty liver, amyloidosis, sarcoidosis, malignancy; [4] medications; and [5] viral hepatitis. Most possibilities in the differential diagnosis can be excluded by the patient’s history and by laboratory studies. To confirm the cause of liver dysfunction, a liver biopsy may be of great help. Of the three cases, diagnosis is established with liver biopsy in two and autopsy in one.
Table 1.
Summary of the reported patients with nonleukemic MS of the liver
| Reference | Age/sex | Clinical presentation | Liver function test | Histological examination | Immunophenotypic features | Methods of diagnosis | Treatment | Outcome (mos) |
|---|---|---|---|---|---|---|---|---|
| [4] | 81/M | Jaundice | NA | Hepatic sinusoides diffuse infiltration | NA | Biopsy | Nothing | 8 days |
| [5] | 84/M | Jaundice | TB 9.5 mg/dL, DB 8.4 mg/dL, ALP 1082 IU/L | MS of the porta hepatic, thickening of the gall bladder wall | CD13+, CD19+, CD33+, CD20+ | Autopsy | ERBD | 50 days |
| [6] | 51/F | Fever | AST 51 IU/L, ALP 145 IU/L | Hepatic blast infiltration | CD68+ | Laparotomy, Biopsy | Nothing | 1 day |
| Present | 16/F | Debilitating hepatomegaly | ALT 283 IU/L, ALP 630 IU/L | Hepatic sinusoides diffuse infiltration | CD45+, CD68+ MPO+ | Biopsy, Autopsy | Nothing | 2 days |
NA not available, TB total bilirubin, ALP alkaline phosphatase, AST aspartate aminotransferase, ALT alanine aminotransferase, ERBD endoscopic retrograde biliary drainage, CHT chemotherapy
Histopathologic and immunohistochemical analysis are critical for establishing correct diagnosis. Morphology in MS varies from well differentiated to poorly differentiated or blastic type. The presence of eosinophilic myelocytes, which have been an important clue to the diagnosis of MS, may not be present in 50–70% of cases [1, 7, 8]. Immunohistochemistry is indispensable to establish a solid diagnosis. Traweek et al. [8] suggested that the vast majority (96%) of myeloid cell tumors can be identified using an immunohistochemical panel that includes CD20, CD43, CD68, and MPO. In our case, the hematological origin was established by CD45, the myeloid lineage was established by MPO and CD68.
In summary, we presented a rare case of disseminated MS of liver without the involvement of bone marrow. Careful morphological analysis of liver biopsy and immunohistochemical staining are vital for diagnosis. Even though nonleukemic MS of liver is rare, its occurrence should never be ignored.
References
- 1.Meis JM, Butler JJ, Osborne BM, et al. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986;58:2697–2709. doi: 10.1002/1097-0142(19861215)58:12<2697::AID-CNCR2820581225>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 2.Sisack MJ, Dunsmore K, Sidhu-Malik N. Granulocytic sarcoma in the absence of myeloid leukemia. J Am Acad Dermatol. 1997;37:308–311. doi: 10.1016/S0190-9622(97)80378-7. [DOI] [PubMed] [Google Scholar]
- 3.Yamauchi K, Yasuda M. Comparison in treatments of nonleukemic granulocytic sarcoma: Report of two cases and a review of 72 cases in the literature. Cancer. 2002;94:1739–1746. doi: 10.1002/cncr.10399. [DOI] [PubMed] [Google Scholar]
- 4.Alama Zaragoza MA, Robles Iniesta A, Roca Adelantado I, et al. Hepatic granulocytic sarcoma: an unusual presentation. An Med Intern. 2003;20:141–144. [PubMed] [Google Scholar]
- 5.Matsueda K, Yamamoto H, Doi I. An autopsy case of granulocytic sarcoma of the porta hepatis causing obstructive jaundice. J Gastroenterol. 1998;33:428–433. doi: 10.1007/s005350050108. [DOI] [PubMed] [Google Scholar]
- 6.Chehensse C, Braun T, Morin AS, et al. Extramedullary blastic transformation revealed by a prolonged fever during the course of a 5q-syndrome. Rev Med Interne. 2009;30:886–889. doi: 10.1016/j.revmed.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 7.Neiman RS, Barcos M, Berard C, et al. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981;48:1426–1437. doi: 10.1002/1097-0142(19810915)48:6<1426::AID-CNCR2820480626>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 8.Traweek ST, Arber DA, Rappaport H. Extramedullary myeloid cell tumours: an immunohistochemical and morphologic study of 28 cases. Am J Surg Pathol. 1993;17:1011–1019. doi: 10.1097/00000478-199310000-00006. [DOI] [PubMed] [Google Scholar]