Abstract
Background
Benign prostatic hyperplasia (BPH), a nonmalignant enlargement of the prostate, can lead to obstructive and irritative lower urinary tract symptoms (LUTS). The pharmacologic use of plants and herbs (phytotherapy) for the treatment of LUTS associated with BPH is common. The extract of the berry of the American saw palmetto, or dwarf palm plant, Serenoa repens (also known by its botanical name of Sabal serrulatum), is one of several phytotherapeutic agents available for the treatment of BPH.
Objectives
This systematic review aimed to assess the effects of Serenoa repens in the treatment of LUTS consistent with BPH.
Search strategy
Trials were searched in computerized general and specialized databases (MEDLINE, EMBASE, and The Cochrane Library), by checking bibliographies, and by handsearching the relevant literature.
Selection criteria
Trials were eligible if they (1) randomized men with symptomatic BPH to receive preparations of Serenoa repens (alone or in combination) for at least four weeks in comparison with placebo or other interventions, and (2) included clinical outcomes such as urologic symptom scales, symptoms, and urodynamic measurements. Eligibility was assessed by at least two independent observers.
Data collection and analysis
Information on patients, interventions, and outcomes was extracted by at least two independent reviewers using a standard form. The main outcome measure for comparing the effectiveness of Serenoa repens with placebo or other interventions was the change in urologic symptom-scale scores. Secondary outcomes included changes in nocturia and urodynamic measures. The main outcome measure for side effects or adverse events was the number of men reporting side effects.
Main results
In this update 9 new trials involving 2053 additional men (a 64.8% increase) have been included. For the main comparison - Serenoa repens versus placebo - 3 trials were added with 419 subjects and 3 endpoints (IPSS, peak urine flow, prostate size). Overall, 5222 subjects from 30 randomized trials lasting from 4 to 60 weeks were assessed. Twenty-six trials were double blinded and treatment allocation concealment was adequate in eighteen studies.
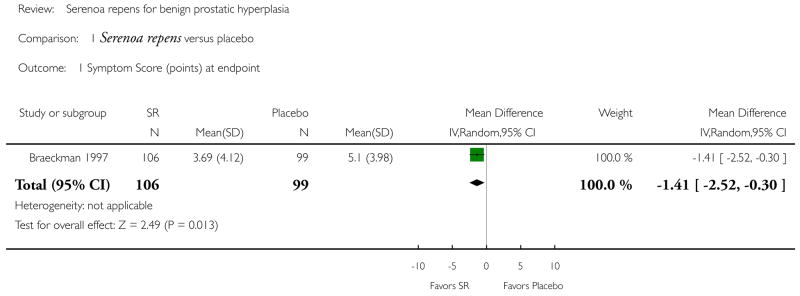
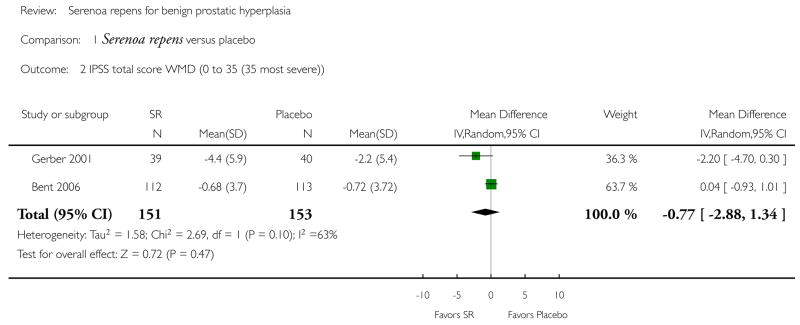
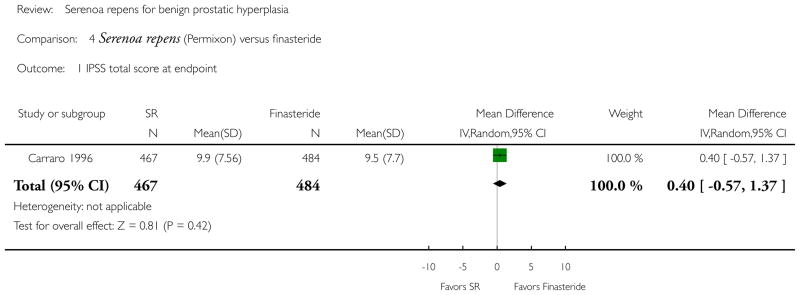
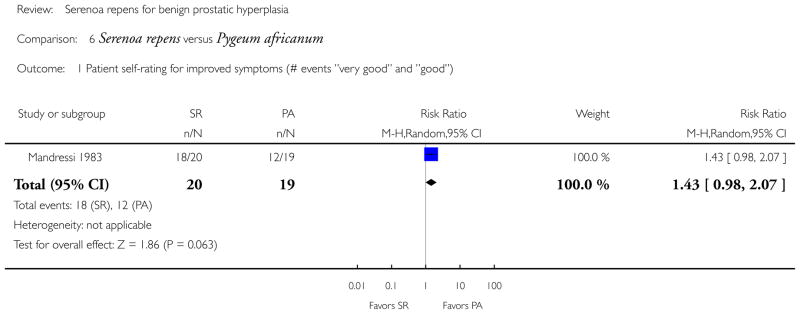
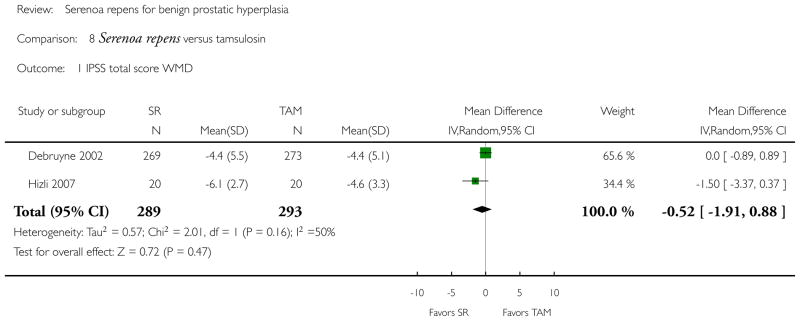
Serenoa repens was not superior to placebo in improving IPSS urinary symptom scores, (WMD (weighted mean difference) −0.77 points, 95% CI −2.88 to 1.34, P > 0.05; 2 trials), finasteride (MD (mean difference) 0.40 points, 95% CI −0.57 to 1.37, P > 0.05; 1 trial), or tamsulosin (WMD −0.52 points, 95% CI −1.91 to 0.88, P > 0.05; 2 trials).
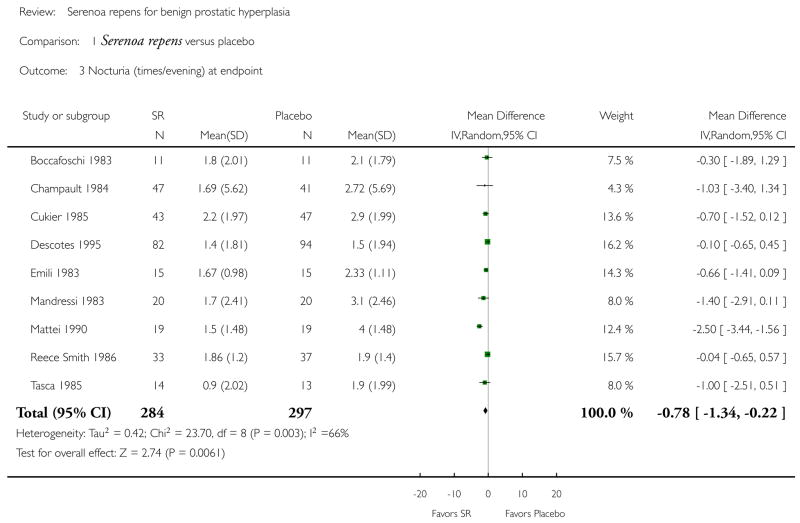
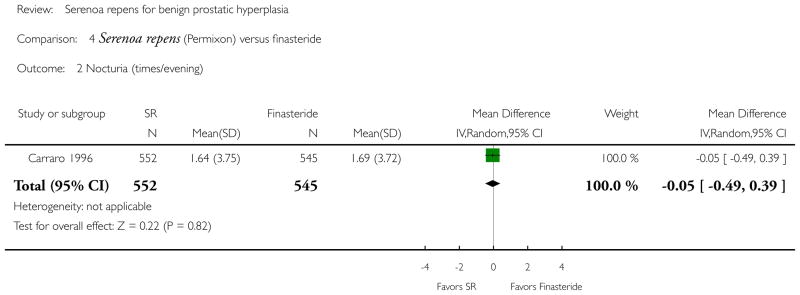
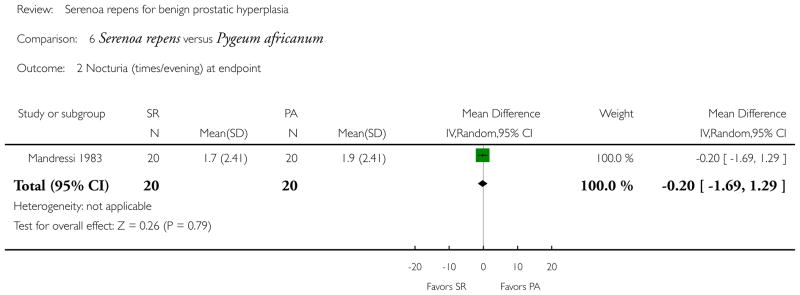
For nocturia, Serenoa repens was significantly better than placebo (WMD −0.78 nocturnal visits, 95% CI −1.34 to −0.22, P < 0.05; 9 trials), but with the caveat of significant heterogeneity (I2 = 66%). A sensitivity analysis, utilizing higher quality, larger trials (≥ 40 subjects), demonstrated no significant difference (WMD −0.31 nocturnal visits, 95% CI −0.70 to 0.08, P > 0.05; 5 trials) (I2 = 11%). Serenoa repens was not superior to finasteride (MD −0.05 nocturnal visits, 95% CI −0.49 to 0.39, P > 0.05; 1 trial), or to tamsulosin (per cent improvement) (RR) (risk ratio) 0.91, 95% CI 0.66 to 1.27, P > 0.05; 1 trial).
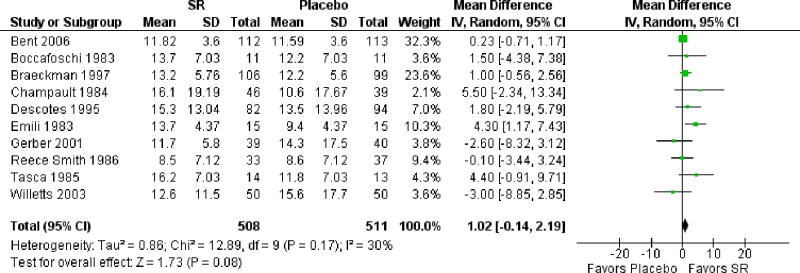
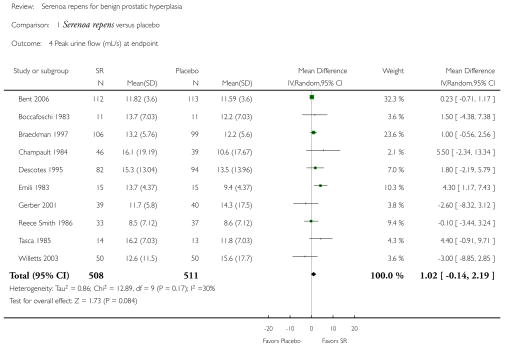
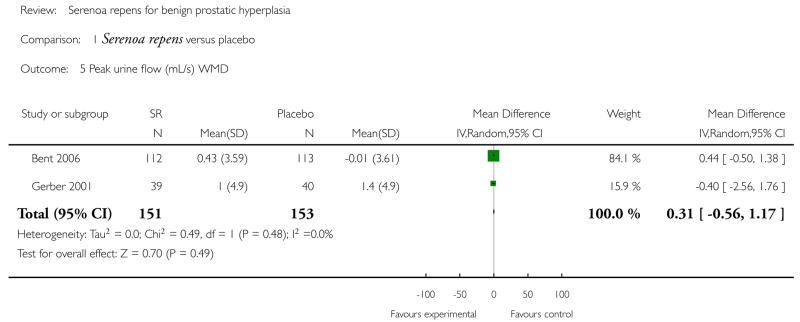
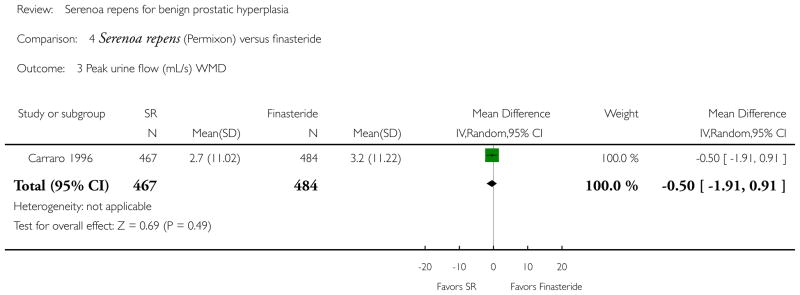
Comparing peak urine flow, Serenoa repens was not superior to placebo at trial endpoint (WMD 1.02 mL/s, 95% CI −0.14 to 2.19, P > 0.05; 10 trials), or by comparing mean change (WMD 0.31 mL/s, 95% CI −0.56 to 1.17, P > 0.05; 2 trials).
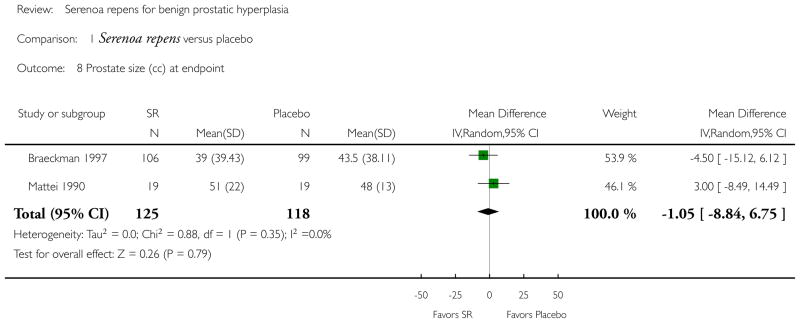
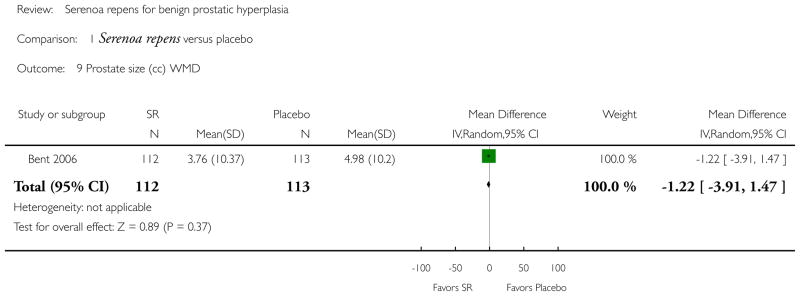
Comparing prostate size at endpoint, there was no significant difference between Serenoa repens and placebo (MD −1.05 cc, 95% CI −8.84 to 6.75, P > 0.05; 2 trials), or by comparing mean change (MD −1.22 cc, 95% CI −3.91 to 1.47, P > 0.05; 1 trial).
Authors’ conclusions
Serenoa repens was not more effective than placebo for treatment of urinary symptoms consistent with BPH.
Medical Subject Headings (MeSH): *Phytotherapy, *Serenoa, Androgen Antagonists [*therapeutic use], Plant Extracts [*therapeutic use], Prostatic Hyperplasia [*drug therapy], Randomized Controlled Trials as Topic, Urination [drug effects]
PLAIN LANGUAGE SUMMARY
Serenoa repens, an herbal medicine, provides no improvement in urinary symptoms and peak urine flow for men with benign prostatic hyperplasia
An enlarged prostate gland, benign prostatic hyperplasia (BPH), can interfere with urination, increasing frequency and urge of urinating, or cause problems emptying the bladder. Surgery and drugs are often used to try to treat BPH. However, using herbal medicines in an attempt to relieve BPH symptoms is common. Serenoa repens is an extremely popular herbal medicine for BPH. This review found that Serenoa repens was well tolerated, but was no better than placebo in improving urinary symptom scores. Nor did Serenoa repens provide noticeable relief - generally considered to be a decrease of 3 points - of urinary symptoms.
At this time there have been relatively few high quality long-term randomized studies evaluating standardized preparations of (potentially) clinically relevant doses. Given the frequent use of Serenoa repens and the relatively low quality of existing evidence, a few more well designed, randomized, placebo-controlled studies that are adequately powered, use validated symptom-scale scores, have a placebo arm and a minimum follow up of one year, are needed to confirm, or deny, our new findings.
BACKGROUND
Benign prostatic hyperplasia (BPH) (see ‘Table of key terms’ (Table 1)) is the nonmalignant enlargement of the prostate gland that is caused by an increase in volume of epithelial and stromal cells into discrete, fairly large nodules in the periurethral region. These nodules in turn can restrict the urethral canal causing partial or complete blockage. Symptoms related to BPH - i.e., lower urinary tract symptoms such as nocturia, incomplete emptying, hesitancy, weak stream, frequency, urgency - are some of the most common problems in older men, and by the seventh decade affect nearly 75% of them (Litwin MS, Saigal CS, editors).
Table 1.
Table of key terms
| AUA | The American Urological Association Symptom Score Index, and the same score as the IPSS. These are self-rated, validated (i.e., symptoms that are confirmed clinically) questionnaires that measure the severity of irritative and obstructive urination symptoms. There are seven questions with each question scaled from 0 to 5. A higher score indicates worse symptoms. There are seven questions with each question scaled from 0 to 5. A higher score indicates worse symptoms. | |
| BPH | Benign prostatic hyperplasia (BPH) is the nonmalignant enlargement of the prostate gland that is caused by an increase in volume of epithelial (top layer of tissue that line cavities and surfaces of the body) and stromal (connective tissue) cells into discrete, fairly large nodules in the periurethral (surrounding the urethra) region. These nodules in turn can restrict the urethral canal causing partial or complete blockage. | |
| Hyperplasia | The proliferation of cells (for BPH, the epithelial and stromal cells) within an organ beyond the ordinary. | |
| IPSS | International Prostate Symptom Score. See AUA. | |
| Peak urine flow | The maximum rate of urine as measured by a uroflowmeter. | |
| Phytosterols | Steroidal alcohols that naturally occur in plants. | |
| Phytotherapy | The use of plants, or plant extracts for medicinal purposes. | |
| Serenoa repens | A small palm native to the American Southeast, Serenoa repens is popularly known as Saw palmetto. When used as a phytotherapy, it is often called Sabal serrulatum. It is the extract of its berries (fatty acids and phytosterols) that is used in the treatment of BPH. | |
| TURP | Transurethral resection of the prostate. A catheter is inserted into the urethra up to the prostate to remove tissue by electrocautery or sharp dissection. |
Histological evidence of BPH is found in more than 40% of men in their fifties and nearly 90% of men in their eighties (Berry 1984), but histologic evidence of BPH, which typically begins in the third decade of life, can be misleading because it does not translate to clinical disease until 20 years later (Litwin MS, Saigal CS, editors). Although absolute prevalence rates differ widely in a number of multinational, longitudinal, population-based studies, they are strikingly consistent in age-related increases that parallel Berry’s (Berry 1984) reporting in his biopsy and cadaver study (Platz 2002; Meigs 2001). In 2000 in the US there were approximately 4.5 million visits to physicians that resulted in a primary diagnosis of BPH; in the same year there were nearly 8 million visits that resulted in a primary or secondary diagnosis (Litwin MS, Saigal CS, editors). In our 2002 update (Wilt 2002), we reported 300,000 prostatectomies for BPH annually (McConnell 1994); in this update we report slightly more than 87,000 prostatectomies for BPH (Litwin MS, Saigal CS, editors). This dramatic decrease in TURPs - formerly the gold standard of practice for severe symptomatic BPH - highlights a trend toward medical management of BPH (Lepor 1996; McConnell 2003). Complementing this trend, phytotherapy has been growing steadily in most countries. Phytotherapeutic agents represent nearly half of the medications dispensed for BPH in Italy, compared with 5% for α-blockers and 5% for 5-ARIs (5α-reductase inhibitors) (Di Silverio 1993). In Germany and Austria, phytotherapy is the first-line treatment for mild to moderate urinary obstructive symptoms and represents more than 90% of all drugs prescribed for the treatment of BPH (Buck 1996). In the United States its use has also markedly increased. In a 2002 survey Serenoa repens (Barnes 2002) was used by 2.5 million adults, “often for BPH.” A recent survey demonstrated that one third of men choosing nonsurgical therapy for benign prostatic hyperplasia were utilizing herbal preparations alone or in combination with prescription medications (Bales 1999).
There are about 30 phytotherapeutic compounds available for the treatment of BPH, and the most widely used of the plant pharmaceuticals is an extract from the berry of the American saw palmetto or dwarf palm plant, Serenoa repens (also known by its botanical name of Sabal serrulatum). While the mechanism of Serenoa repens is unknown, some of those proposed are: alteration in cholesterol metabolism (Christensen 1990); antiestrogenic and antiandrogenic effects (Dreikorn 1990; Marwick 1995), with Serenoa repens (Permixon®) acting as a weak surrogate 5-ARI, inhibiting the conversion of testosterone to dihydrotestosterone (DHT) (Dedhia 2008); anti-inflammatory effects (McGuire 1987; Buck 2004); a decrease in available sex hormone-binding globulin (Di Silverio 1993); pro-apoptotic properties and inhibition of cellular proliferation (Buck 2004; Vacherot 2000; Vela-Navarrete 2005); the dependent inhibition of 5-ARI in the stroma and epithelium of the prostate (Weisser 1996); and the relaxation of smooth muscles via α1-adrenergic receptors.
Despite wide spread use the clinical efficacy of Serenoa repens to improve BPH symptoms and urodynamic measures remains unclear. We conducted and updated a systematic review, first published in 1998 and updated in 2002, to evaluate the efficacy and adverse events of Serenoa repens in men with lower urinary tract symptoms consistent with benign prostatic hyperplasia.
OBJECTIVES
The main outcomes were the efficacy of Serenoa repens versus placebo or control in improving urologic symptom-scale scores or global report of urinary symptoms (improved versus stable or worsened), and side effects. Secondary outcomes included changes in nocturia, prostate size, and peak urine flow.
METHODS
Criteria for considering studies for this review
Types of studies
Randomized, controlled clinical trials.
Types of participants
Men with lower urinary tract symptoms consistent with benign prostatic hyperplasia (BPH).
Types of interventions
Comparison of preparations of Serenoa repens with placebo or medical therapies for BPH with a treatment duration of at least 30 days.
Types of outcome measures
Urologic symptom scores (Boyarsky, American Urologic Association Symptom Index (AUA), and the International Prostate Symptom Score (IPSS)); change in peak urine flow; change in prostate size (measured in cubic centimeters (cc)); nocturia (times/per evening); and overall physician or patient assessment of urinary symptoms, or both. If we could not assess mean change, we compared endpoints between or among arms.
(Note: Both the AUA and IPSS use identical the scale of 0 to 35, with mild symptoms scored 1 to 8, medium 9 to 18, and severe ≧ 19.)
Search methods for identification of studies
-
We searched MEDLINE from 1966 to 2008 by crossing an optimally sensitive search strategy for trials from the Cochrane Collaboration with the following MeSH search terms.
prostatic hyperplasia.mp.
phytosterols.mp.
plant extracts.mp.
sitosterols.mp.
serenoa repens.mp.
sabal serrulata.mp.
or/2–6
or/2–6
1 and 7
limit 9 to randomized controlled trial
limit 10 to yr=“2003 – 2008”
from 11 keep 1–10
from 11 keep 1–10
from 13 keep 1–10
and included all subheadings (Dickersin 1994).
EMBASE (1974 to July 2008) and The Cochrane Library, including the database of the Cochrane Prostatic Diseases and Urologic Cancers Group and the Cochrane Field for Complementary Medicine were searched in a similar fashion.
Reference lists of all identified trials and previous reviews were searched for additional trials.
There were no language restrictions.
Data collection and analysis
Eligibility
In this update one reviewer decided on eligibility.
Extraction
Assessment of study characteristics and data extraction were performed by one reviewer. Missing or additional information was sought from authors/sponsors. Extracted data was reviewed by the principal reviewer and discrepancies resolved by discussion.
Assessment of methodological quality
As a measure of overall methodologic study quality (and bias) we assessed scales and criteria developed by Schulz 1995 and Cochrane (Cochrane Handbook 2008). The five criteria addressed were:
adequate sequence generation (was there an articulated rule for allocating interventions based on chance?);
allocation concealment (was there any foreknowledge of the allocation of interventions by anyone?);
blinding (during the course of the trial were study participants and personnel blinded to the knowledge of who received which intervention?);
incomplete outcome data addressed (did the trial assess all patients, or account for those not assessed?);
free of other bias (selective outcome reporting, differences between/among arms in how outcomes were determined).
Each criterion could be answered by A (’yes’), B (’unclear’), and C (’no’).
Summarizing results of primary studies
Outcomes
We assessed the mean urologic symptom score (IPSS, AUA), nocturia (# times), peak urine flow (mL/s), and prostate size (cc). The number and percent of men reporting specific side effects and/or withdrawing from the study were also evaluated.
Meta-analysis
We assessed for heterogeneity by using the I2 statistic.
For the primary analysis (of the stated primary and secondary outcomes) all trials including Serenoa repens in mono-preparations and in combination were analyzed separately (e.g., Serenoa repens versus placebo or active controls, Serenoa repens + Urtica dioica versus placebo or controls). We pooled studies that were deemed clinically similar and provided sufficient information.
Summary effect estimates were done using a random-effects model to allow for heterogeneity between or among studies. Optimally, we would have liked to compare mean changes and variances at endpoint between or among arms. If that data were not available, we compared intergroup endpoints (with variances). Standard errors (SEM) and confidence intervals (CI) that were needed for input to Revman 5 - the Cochrane statistical and systematic review software - were obtained by the following arguments: SD = CI1-CI2 × √n/1.96 and SD = SEM × √N (Follmann 1992).
For continuous outcomes we also used an inverse variance method, which allowed larger trials with smaller SEM more weight over smaller trials with larger SEM, and thus minimizing the uncertainty of the pooled-effect estimate. To assess the per cent of patients having improved - or worsened - urologic symptoms, a modified ITT was performed (i.e., men who dropped out or were lost to follow up were considered to have had worsening symptoms) (Lavori 1992). The denominator for the modified ITT analysis included the number randomized to treatment at baseline and the numerator included the number completing the trial and showing improvement. For dichotomous outcomes we used the Mantel-Haenszel method because we have small trials with little data. For both dichotomous and continuous outcomes, we used 95% CI, and for statistically significant outcomes a P value of ≦ 0.05.
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
The updated search strategy (2008) identified 12 new trials, of which 9 met inclusion criteria (Preuss 2001; Debruyne 2002; Glémain 2002; Willetts 2003; Lopatkin 2005; Engelmann 2006; Bent 2006; Hizli 2007; Shi 2007). Excluded were Pecoraro 2004, Popa 2005, and Vela-Navarrete 2005. Reasons for exclusion were no clinical outcomes (Pecoraro 2004; Vela-Navarrete 2005), and dual publication (Popa 2005).
In this update a total of 2053 additional participants were randomized in 9 trials (820 in trials of Serenoa repens alone or in combination (Urtica dioica, Cernitin®, B-sitosterol, vitamin E, tamsulosin) versus placebo (Preuss 2001; Willetts 2003; Lopatkin 2005; Bent 2006; Shi 2007), and 1233 men in trials of Serenoa repens alone or in combination versus active control (Debruyne 2002; Glémain 2002; Engelmann 2006; Hizli 2007).
Overall (30 studies), mean follow up was 19.1 weeks, and ranged from 4 to 60 weeks. The weighted mean age of all enrollees was 64.9 years (24 studies). Subjects’ age from reporting studies ranged from 43 to 88 years (21 studies). The per cent of men who dropped out or were lost to follow up was 11% (576/5222) and ranged from 0% to 21.4% (30 studies). Only one trial assessed compliance (Shi 2007), which was, after 12 weeks, 98% for the verum arm, and 100% for the placebo arm.
Fourteen trials - including eight new trials for this update -(Metzker 1996; Carraro 1996; Sökeland 1997; Bauer 1999; Marks 2000; Gerber 2001; Preuss 2001; Debruyne 2002; Glémain 2002; Lopatkin 2005; Engelmann 2006; Bent 2006; Shi 2007; Hizli 2007) provided efficacy outcomes using validated, self-reporting questionnaires (AUA, IPSS), and which were graded on a 0 (’Never’) to 5 (’Almost always’) scale, for a total score of 35 points. Of the 30 included trials, 12 used Permixon®, a commercialized extract of the fruit of Serenoa repens. Of these twelve, seven compared Permixon® to placebo; the remaining compared Permixon®, either alone or in combination (Permixon® + tamsulosin), to finasteride, tamsulosin, and depostat. Five studies compared another standardized combination of Serenoa repens and (160 mg) and Urtica dioica extracts (120 mg), and which is known by the commercial name Prostagutt® forte, or PRO 160/120. Of these, three compared PRO 160/120 to placebo, one to finasteride, and one to tamsulosin. Fourteen trials used generic Serenoa repens alone or in combination with other phytotherapies (pumpkin seeds, vitamins A and E, nettle root, Pygeum africanum).
Twenty-two of the 30 included trials reported racial data. Ninety-seven per cent of (3205/3309) subjects were White, 0.4% (14/3309) were African American, 0.3% (11/3309) were Hispanic, and 0.6% (21/3309) were Asian/Pacific Islanders. All studies reported regional affiliations; accumulatively, all save three could be dichotomized between Europe and the United States. Ninety per cent (4400/4898) of study subjects were European, and 10% (498/4898) were American.
The weighted mean baseline PSA (8 trials) was 2.9 nanograms/millilitres (ng/mL), and ranged from 1.7 ng/mL to 3.4 ng/mL. The weighted mean baseline prostate volume (11 trials) was 43.9 cc, and ranged from 33 cc to 57 cc.
Overall, symptom-scale score results were reported in 21 studies (Mandressi 1983; Champault 1984; Reece Smith 1986; Gabric 1987; Carbin 1990; Descotes 1995; Carraro 1996; Metzker 1996; Braeckman 1997; Sökeland 1997; Bauer 1999; Marks 2000; Gerber 2001; Preuss 2001; Debruyne 2002; Glémain 2002; Willetts 2003; Lopatkin 2005; Bent 2006; Engelmann 2006; Hizli 2007), but only 14 reported the IPSS or AUA validated scores. Results for nocturia were reported in 14 studies (Boccafoschi 1983; Emili 1983; Mandressi 1983; Champault 1984; Cukier 1985; Tasca 1985; Pannunzio 1986; Reece Smith 1986; Carbin 1990; Mattei 1990; Descotes 1995; Carraro 1996; Preuss 2001; Debruyne 2002), but only 11 reported data that permitted pooling. Pannunzio presented per cent with nocturia at baseline and endpoint, but without defining nocturia. Debruyne reported per cent improvement, but did not provide baseline values. Peak urine flow was reported in 25 studies (Boccafoschi 1983; Emili 1983; Champault 1984; Tasca 1985; Pannunzio 1986; Reece Smith 1986; Gabric 1987; Löbelenz 1992; Descotes 1995; Carraro 1996; Metzker 1996; Braeckman 1997; Sökeland 1997; Bauer 1999; Marks 2000; Gerber 2001; Preuss 2001; Debruyne 2002; Glémain 2002; Willetts 2003; Lopatkin 2005; Bent 2006; Engelmann 2006; Shi 2007; Hizli 2007). Data on prostate size were reported in 13 trials (Emili 1983; Pannunzio 1986; Mattei 1990; Roveda 1994; Carraro 1996; Braeckman 1997; Sökeland 1997; Bauer 1999; Marks 2000; Debruyne 2002; Bent 2006; Hizli 2007; Shi 2007). Nine trials reported endpoints (Roveda 1994; Carraro 1996; Sökeland 1997; Braeckman 1997; Braeckman 1997; Mattei 1990; Mattei 1990; Debruyne 2002; Shi 2007; Hizli 2007), one reported mean change (Bent 2006), and two reported per cent change from baseline (Emili 1983; Pannunzio 1986).
(See ’Characteristics of included studies’ and ’Description of studies’).
Serenoa repens alone or in combination versus placebo
There were 21 trials comparing Serenoa repens, alone or in combination, to placebo (Boccafoschi 1983; Emili 1983; Mandressi 1983 (Mandressi was a three-arm trial with placebo and active controls); Champault 1984; Tasca 1985; Cukier 1985; Reece Smith 1986; Gabric 1987; Mattei 1990; Löbelenz 1992; Braeckman 1997; Descotes 1995; Metzker 1996; Bauer 1999; Marks 2000; Preuss 2001; Gerber 2001; Willetts 2003; Lopatkin 2005; Bent 2006; Shi 2007). Eight trials (Metzker 1996; Bauer 1999; Marks 2000; Gerber 2001; Preuss 2001; Lopatkin 2005; Bent 2006; Shi 2007) reported baseline values for IPSS total score for a weighted mean of 16.6 points, indicating moderately severe symptoms. Ten trials reported baseline nocturia in some form (Emili 1983; Boccafoschi 1983; Mandressi 1983; Champault 1984; Cukier 1985; Tasca 1985; Reece Smith 1986; Mattei 1990; Descotes 1995; Preuss 2001); eight trials were poolable (Emili 1983; Boccafoschi 1983; Mandressi 1983; Champault 1984; Cukier 1985; Reece Smith 1986; Mattei 1990; Descotes 1995) for a weighted mean of 2.8 incidents per night. Thirteen trials (Emili 1983; Boccafoschi 1983; Tasca 1985; Descotes 1995; Metzker 1996; Braeckman 1997; Bauer 1999; Marks 2000; Gerber 2001; Willetts 2003; Lopatkin 2005; Bent 2006; Shi 2007) reported baseline peak urine flow for a weighted mean of 11.4 mL/s. This compares closely to Abrams and Griffiths (Abrams 1979) threshold of 10 mL/s or less for intravesical obstruction. The most commonly used dose of Serenoa repens was 160 mg twice daily. Champault reported 80 mg twice daily, Gabric “20 drops” thrice daily, Löbelenz 100 mg once daily, Marks 106 mg twice daily, and Pruess (Serenoa repens + B-sitosterol) 286 mg twice daily.
Serenoa repens alone or in combination versus control
Of ten trials comparing Serenoa repens, alone or in combination, with a control (Mandressi 1983; Pannunzio 1986; Carbin 1990; Roveda 1994; Carraro 1996; Sökeland 1997; Debruyne 2002; Glémain 2002; Engelmann 2006; Hizli 2007), five reported baseline values for IPSS total score (Debruyne 2002; Carraro 1996; Sökeland 1997; Engelmann 2006; Hizli 2007) of 15.3. Three trials reported nocturia at baseline (Mandressi 1983; Pannunzio 1986; Carbin 1990), but only two trials had poolable data (Mandressi 1983; Carbin 1990) for a weighted mean of 1.93 nocturnal visits. The baseline peak urine flow reported in seven trials (Pannunzio 1986; Carraro 1996; Sökeland 1997; Debruyne 2002; Glémain 2002; Engelmann 2006; Hizli 2007) was a weighted mean of 11.0 mL/s. These results indicate that on average men had urinary symptoms consistent with moderate BPH, with moderate defined as IPSS total score 8 to 19.
Most trials reported doses of Serenoa repens equal to 160 mg twice daily, with the exceptions of Carbin (160 mg thrice daily), Roveda (160 mg 4 times daily), and Engelmann (160 mg daily).
Five studies reported baseline prostate volumes (Roveda 1994; Carraro 1996; Sökeland 1997; Debruyne 2002; Hizli 2007), but only four were able to be pooled. The weighted mean baseline prostate size for the four studies (Carraro 1996; Sökeland 1997; Debruyne 2002; Hizli 2007) was 44.5 cc.
Risk of bias in included studies
Treatment allocation concealment was adequate in 18 studies (60%) (Cukier 1985; Reece Smith 1986; Carbin 1990; Löbelenz 1992; Roveda 1994; Braeckman 1997; Carraro 1996; Metzker 1996; Sökeland 1997; Marks 2000; Gerber 2001; Debruyne 2002; Glémain 2002; Willetts 2003; Lopatkin 2005; Engelmann 2006; Bent 2006; Shi 2007), and 26 studies (86.7%) were double blinded (Mandressi 1983; Boccafoschi 1983; Emili 1983; Champault 1984; Cukier 1985; Tasca 1985; Reece Smith 1986; Gabric 1987; Carbin 1990; Mattei 1990; Löbelenz 1992; Descotes 1995; Carraro 1996; Metzker 1996; Sökeland 1997; Braeckman 1997; Bauer 1999; Gerber 2001; Preuss 2001; Debruyne 2002; Glémain 2002; Willetts 2003; Lopatkin 2005; Engelmann 2006; Bent 2006; Shi 2007).
The main comparisons were: Serenoa repens monotherapy versus placebo (Mandressi 1983; Boccafoschi 1983; Emili 1983; Champault 1984; Cukier 1985; Tasca 1985; Reece Smith 1986; Mattei 1990; Löbelenz 1992; Descotes 1995; Braeckman 1997; Bauer 1999; Gerber 2001; Willetts 2003; Bent 2006; Shi 2007); Serenoa repens in combination with other phytotherapeutic agents versus placebo (Mandressi 1983; Gabric 1987; Carbin 1990; Metzker 1996; Marks 2000; Preuss 2001; Lopatkin 2005); Serenoa repens alone versus control, including Pygeum africanum (Mandressi 1983), gestonorone caproate (Pannunzio 1986), finasteride (Carraro 1996), tamsulosin (Debruyne 2002; Hizli 2007), and Serenoa repens + tamsulosin (Hizli 2007); Serenoa repens in combination with other agents versus control, including Serenoa repens + Urtica dioica versus finasteride (Sökeland 1997), Serenoa repens + tamsulosin versus tamsulosin (Glémain 2002), and Serenoa repens + Uritca dioica versus tamsulosin (Engelmann 2006); and Serenoa repens orally versus Serenoa repens rectally, in a therapeutic, bioequivalence study (Roveda 1994).
Effects of interventions
Serenoa repens versus placebo (n = 14)
Urinary symptom scores
Ten trials reported outcomes for urinary symptom-scale scores comparing Serenoa repens alone versus placebo.
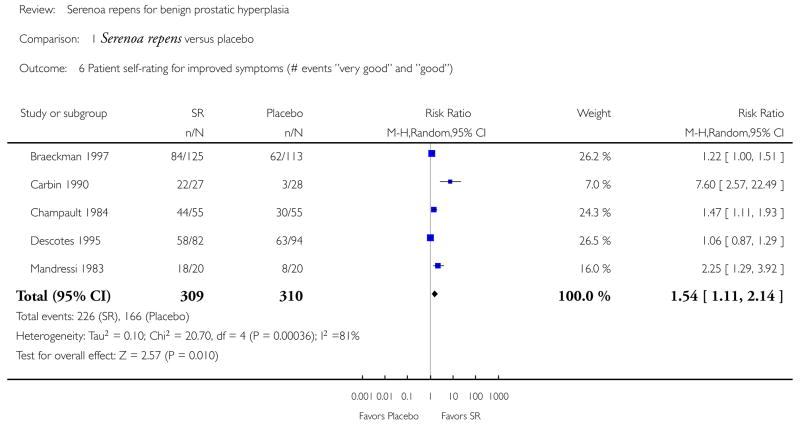
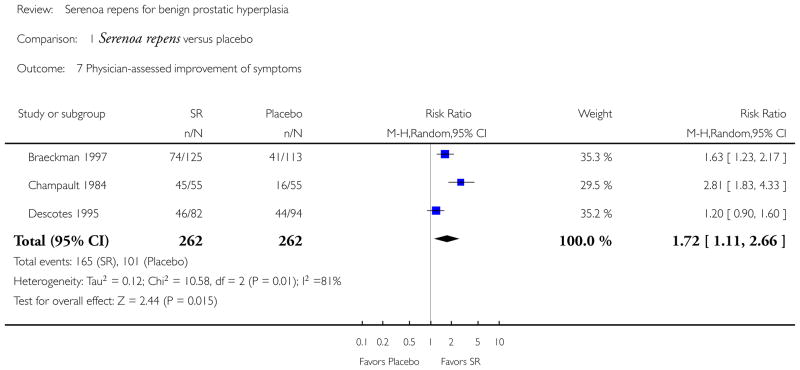
Two trials compared the validated, IPSS total score and found that Serenoa repens was no better than placebo in lowering scores at endpoint (Analysis 1.2). Braeckman 1997 (N = 238), which compared an unidentified, non-validated urinary symptom score (scale 0 to 19) at endpoint, found a significant difference (Analysis 1.1) favoring Serenoa repens. Three trials used a physician-assessed, symptom-improvement score, and found Serenoa repens was significantly better than placebo (Analysis 1.7). In a patient, self-rated survey of improved symptoms, five trials reported Serenoa repens again was significantly better (Analysis 1.6). Reece Smith 1986, in a 12-week trial, compared 11 symptom assessments from both physicians and patients; there were no significant intergroup differences for any symptom in either physician or patient assessments. Willetts 2003 compared IPSS total score from an unequal baseline (t-test, P = 0.028), and reported the Serenoa repens and placebo arms decreased at 12 weeks, but with no significant difference between them (treatment effect 1.74, 95% CI −0.54 to 4.03, P = 0.13).
Gerber did report noticeable relief - considered clinically to be a decrease of three or more points - from symptoms for the Serenoa repens arm (−4.4 points) but not the placebo arm (−2.2 points). Bent found no noticeable relief for either arm (−0.68 points versus 0.72 points, respectively).
Nocturia
Nine trials compared nocturia at endpoint and found Serenoa repens superior to placebo (Analysis 1.3), but with significant heterogeneity (I2 = 66%). A sensitivity analysis, comparing the higher quality, larger trials (N ≧ 40), found no difference (MD −0.31 nocturnal visits, 95% CI −0.70 to 0.08, P > 0.05), and with little heterogeneity (I2 = 11%).
Peak urine flow
Twelve trials (Boccafoschi 1983; Emili 1983; Champault 1984; Tasca 1985; Reece Smith 1986; Löbelenz 1992; Braeckman 1997; Descotes 1995; Bauer 1999; Gerber 2001; Willetts 2003; Bent 2006) presented data for peak urine flow, but only 10 had poolable data. There was no significant difference at endpoint (Analysis 1.4). Gerber 2001 and Bent 2006 compared mean change and found no difference as well (Analysis 1.5).
Three trials reported data that were not poolable (Bauer 1999; Löbelenz 1992; Willetts 2003). Bauer found a 12% absolute improvement for Serenoa repens, and Löbelenz a 5.2% absolute improvement favoring Serenoa repens. Willetts reported a significant difference, favoring placebo (t-test, P < 0.05).
Prostate size
Five trials (Emili 1983; Mattei 1990; Braeckman 1997; Bauer 1999; Bent 2006) reported data for prostate size, but only two were poolable (Mattei 1990; Braeckman 1997). Both trials reported slight decreases for both arms, but nevertheless found no significant difference at endpoint (Analysis 1.8). Bauer (N = 101), with a follow up of six months, reported a slight increase for both arms. For Serenoa repens, the increase was 1.4% (34.5 cc to 35 cc), and for the placebo arm, 1.5% (31.7 cc to 32.2 cc). Emili (N = 30), with a four-week follow up, reported (in a qualitative scale) 26.6% reduction for the Serenoa repens arm, and no change for the placebo arm. Bent (N = 225), with a follow up of 12 months, reported size increases for both arms at endpoint for a mean difference of −1.22 cc (95% CI −3.91 to 1.47, P > 0.05).
Serenoa repens versus finasteride (n = 1)
Urinary symptom scores
Carraro 1996 (N = 1098) found no difference between Serenoa repens and finasteride in the IPSS total score at endpoint (MD 0.40 points, 95% CI −0.57 to 1.37, P > 0.05).
Nocturia
Serenoa repens was not superior to finasteride (−0.05 nocturnal visits, 95% CI −0.49 to 0.39, P > 0.05).
Peak urine flow
There was no difference between Serenoa repens and finasteride (MD −0.50 mL/s, 95% CI −1.91 to 0.91, P > 0.05).
Prostate size
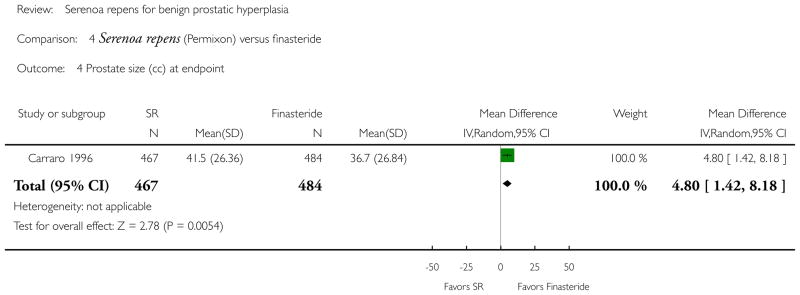
Carraro (mean prostate size 43.5 cc) reported both treatments reduced prostate size over a 13-week follow up. In the Serenoa repens arm, prostate size changed from 43.0 cc to 41.5 cc (−6%) and in the finasteride arm, 44.0 cc to 36.7 cc (−18%). The difference was significant (WMD 4.80 cc, 95% CI 1.42 to 8.18, P < 0.05) and favored finasteride.
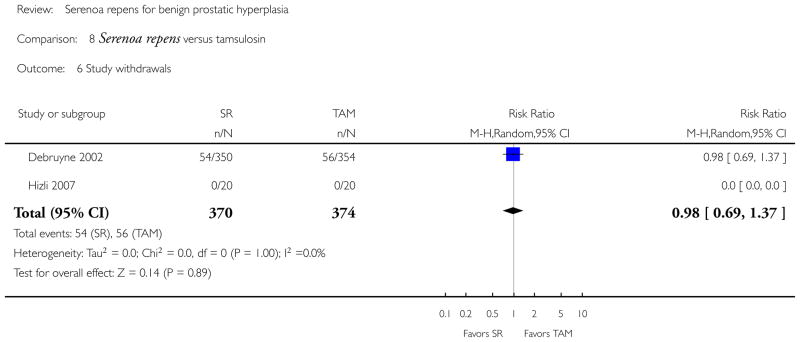
Serenoa repens versus tamsulosin (n = 2)
Urinary symptom scores
There was no significant difference in IPSS total score (tamsulosin dose for both trials was 0.4 mg daily) (Analysis 8.1). In contrast to Serenoa repens versus placebo (P > 0.05), these two trials showed comparable efficacy.
Nocturia
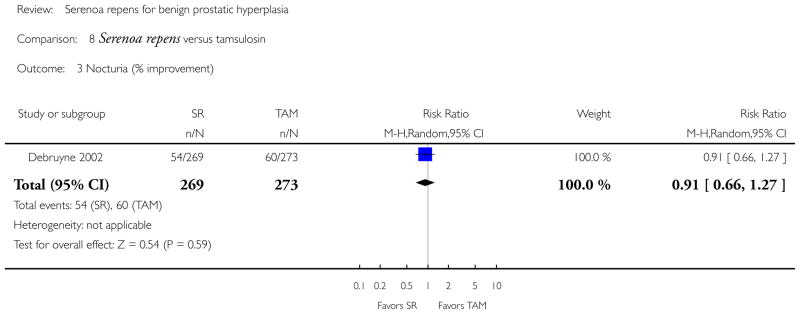
Debruyne 2002 reported no significant difference comparing per cent improvement (RR 0.91, 95% CI 0.66 to 1.27, P > 0.05).
Peak urine flow
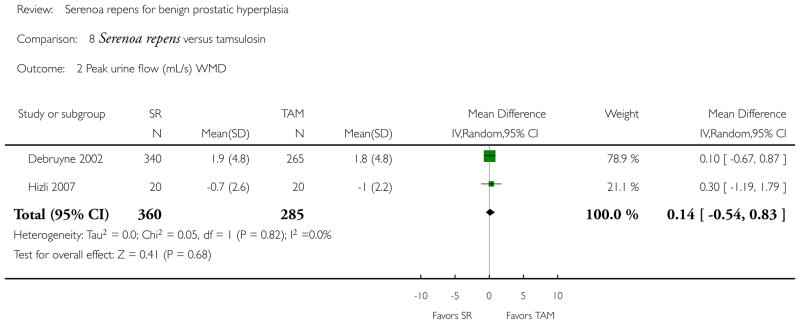
Debruyne found slight increases in peak urine flow and Hizli slight decreases, but in the meta-analysis there was no significant difference (Analysis 8.2).
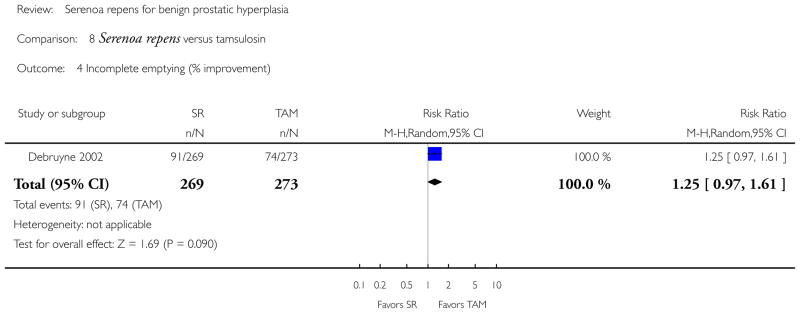
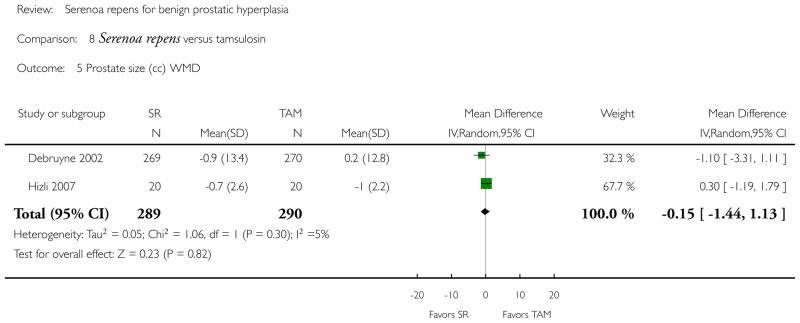
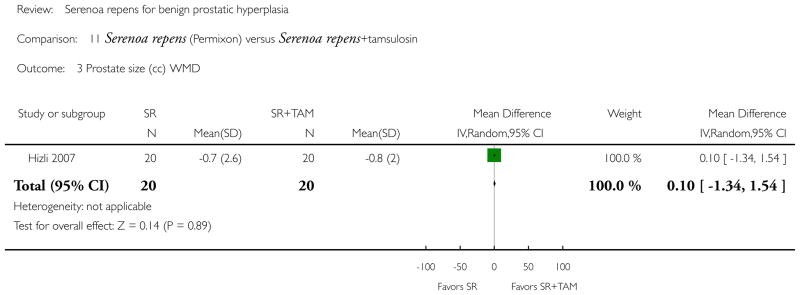
Prostate size
Both trials reported shrinking prostates for all arms save a single tamsulosin arm. No difference was found in the meta-analysis (Analysis 8.5).
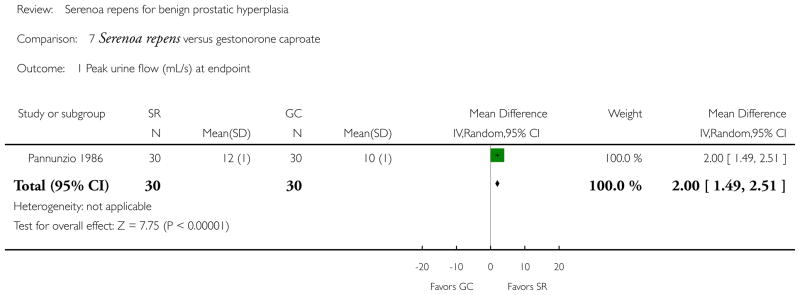
Serenoa repens versus gestonorone caproate (n = 1)
Peak urine flow
Pannunzio (N = 60) reported a significant difference in mean change, favoring Serenoa repens (MD 2.00 mL/s, 95% CI 1.49 to 2.51, P < 0.05).
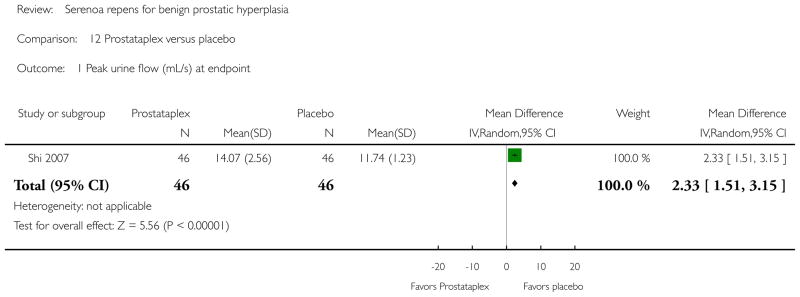
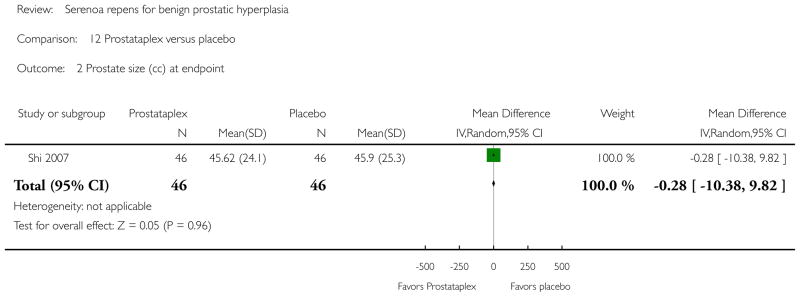
Prostataplex™ (Serenoa repens, soybean oil, beeswax, soy lecithin, gelatin, glycerin, deionized water, titanium dioxide, carmine red, natural vanilla flavor) versus placebo (N = 1)
Urinary symptom score
Shi 2007 (N = 94) considered an a priori intra group decrease of three points of the IPSS total score to be clinically significant. After a three-month follow up, the Prostataplex™ arm decreased a mean of 2.02 points, and the placebo arm decreased a mean of 0.33 (Student’s t-test, P < 0.001). The comparison of endpoints (14.83 versus 14.13, respectively) was not significant (Student’s t-test, P = 0.545).
Peak urine flow
Shi reported a significant difference at endpoint. The WMD was 2.33 mL/s (95% CI 1.51 to 3.15, P < 0.05), favoring Prostataplex™.
Prostate size
Shi reported slight decreases at endpoint (SR = 2.1 cc; placebo = 2.48 cc).
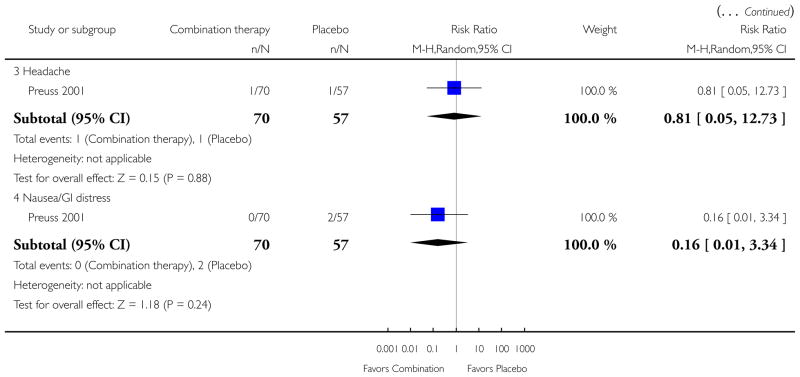
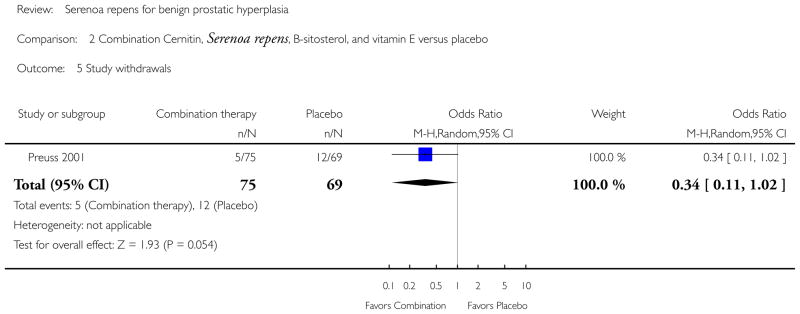
Combination Cernitin®, Serenoa repens, B-sitosterol, vitamin E versus placebo (n = 1)
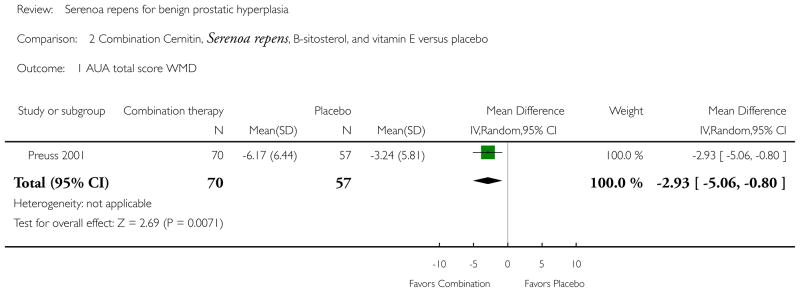
Urinary symptom scores
Preuss 2001 (N = 144) reported a significant difference in the AUA total score (MD −2.93 points, 95% CI −5.06 to −0.80, P < 0.05) in favor of combination therapy.
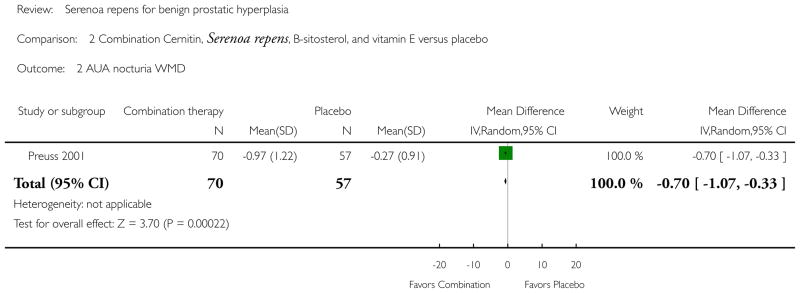
Nocturia
Preuss found a significant difference between the two arms in the AUA nocturia subscale (0 to 5; ’0’ is no trips, ’5’ is 5 trips or more) (MD −0.70, 95% CI −1.07 to −0.33, P < 0.05).
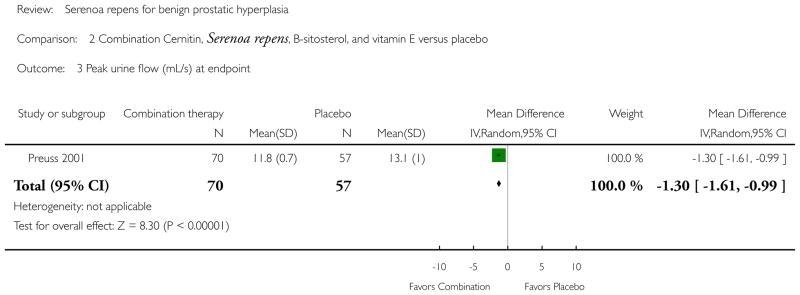
Peak urine flow
Combination therapy was superior to placebo at endpoint (MD −1.30 mL/s, 95% CI −1.61 to −0.99, P < 0.05).
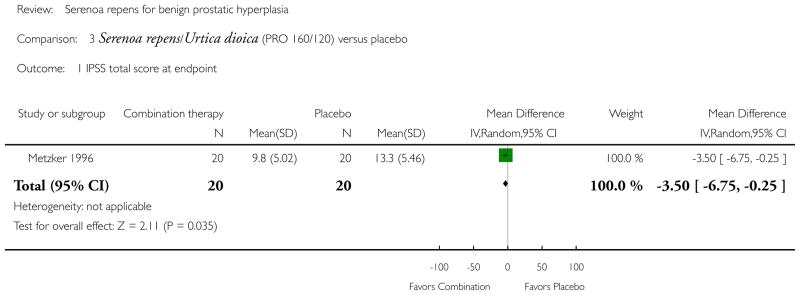
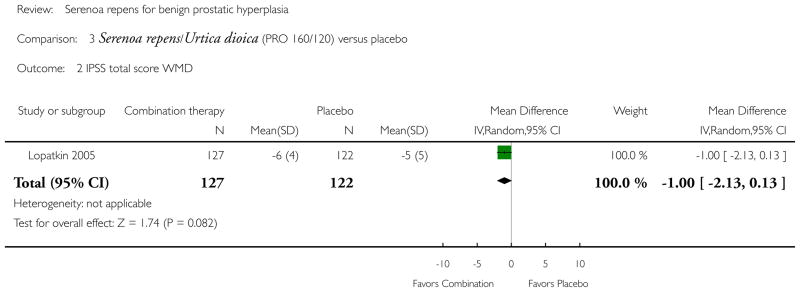
Serenoa repens/Urtica dioica versus placebo (n = 3)
Urinary symptom scores
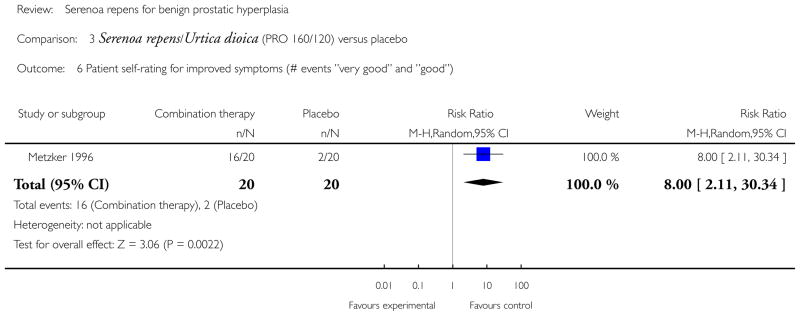
Metzker 1996 (N = 40) found a significant difference in IPSS endpoint (40-week follow up) (MD −3.50 points, 95% CI −6.75 to −0.25, P < 0.05); Lopatkin 2005 (N = 257), comparing mean change, did not (MD −1.00 points, 95% CI −2.13 to 0.13, P > 0.05). Gabric 1987 (N = 30) compared the combination Prostagutt® forte to placebo, and included a physician evaluated global symptom score (scale 1 to 3; 1 = no change, 2 = satisfactory change, 3 = excellent change) at six-week endpoint. The median (extrapolated from graph) for the verum arm was 1.3 and for the placebo arm 2.2 (P < 0.05).
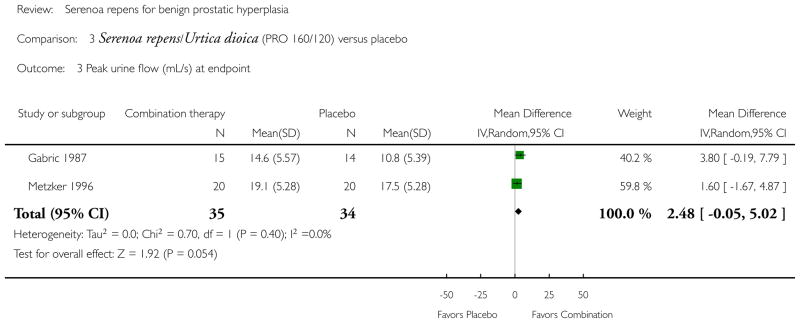
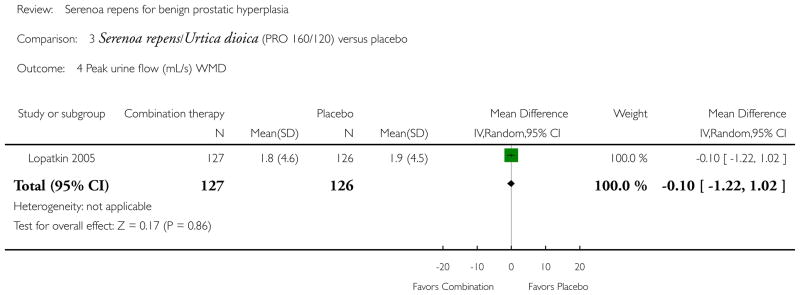
Peak urine flow
Lopatkin, comparing mean change, reported positive mean changes of about 2 mL/s for both arms, but the comparison was not significant (MD −0.10 mL/s, 95% CI −1.22 to 1.02, P > 0.05). Gabric 1987 (N = 30) and Metzker found a significant difference at endpoint (Analysis 3.3).
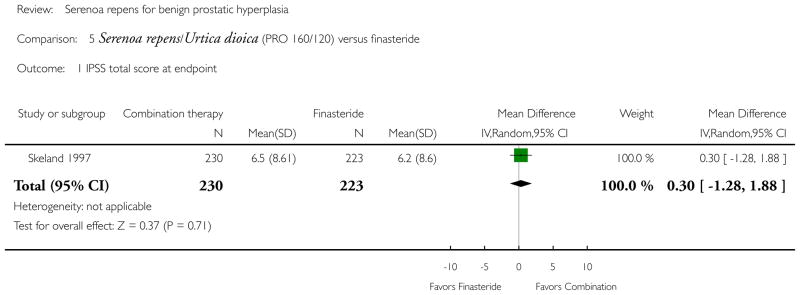
Serenoa repens/Urtica dioica versus finasteride (N = 1)
Urinary symptom scores
Sökeland 1997 (N = 543) found no significant difference in IPSS total score at 12-week endpoint (MD 0.30 points, 95% CI −1.28 to 1.88, P > 0.05).
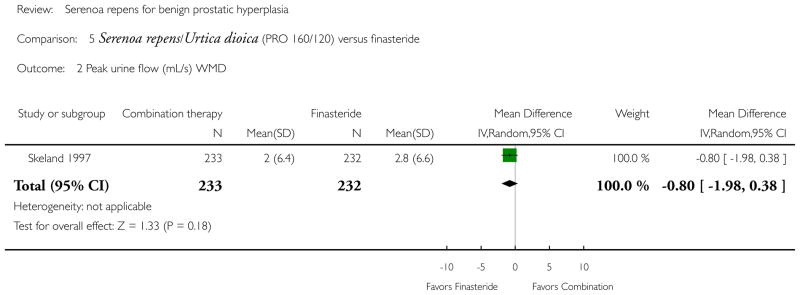
Peak urine flow
Sökeland reported increases of 2.7 mL/s and 3.2 mL/s for Serenoa repens/Urtica dioica and placebo, respectively, but the comparison was not significant (MD −0.80 mL/s, 95% CI −1.98 to 0.38, P > 0.05).
Prostate size
Sökeland (mean prostate size 43.3 cc) reported declines in prostate volume for both arms at the end of 12-week follow up. The PRO 160/120 arm decreased 0.7% (42.7 cc to 42.4 cc), and the finasteride arm, 15.5% (44.0 cc to 37.2 cc), for an absolute improvement of 14.8% favoring finasteride.
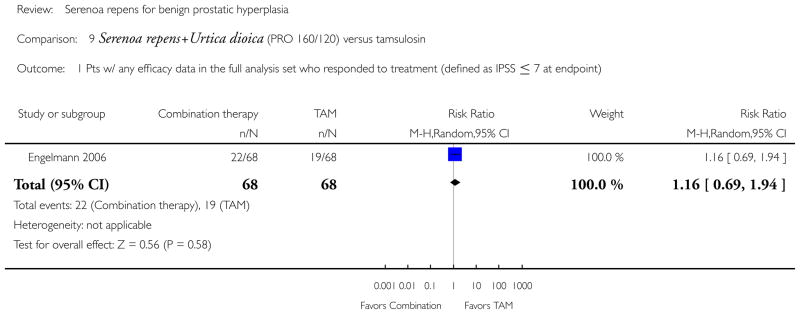
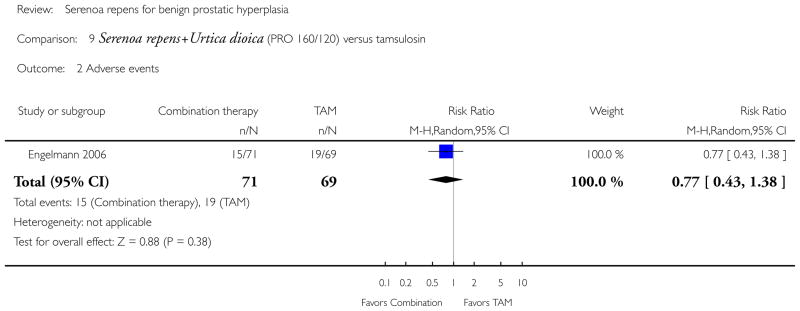
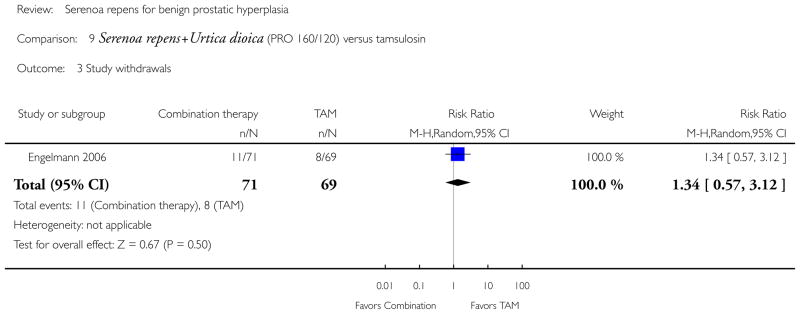
Serenoa repens/Urtica dioica versus tamsulosin (N = 1)
Urinary symptom scores
Engelmann 2006 (N = 140), which reported responders to treatment (defined as IPSS ≧ 7 at endpoint), found no significant difference between the arms (RR 1.16, 95% CI 0.69 to 1.94, P > 0.05).
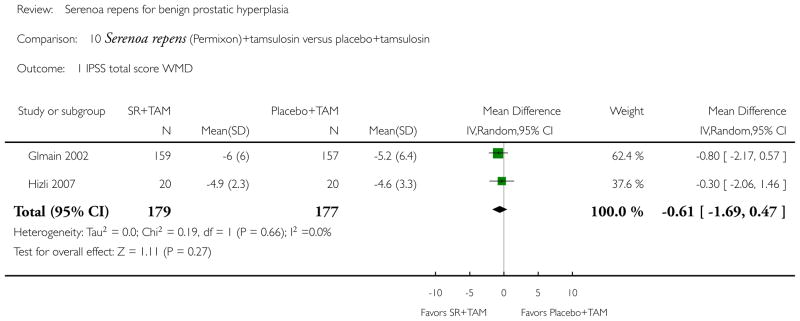
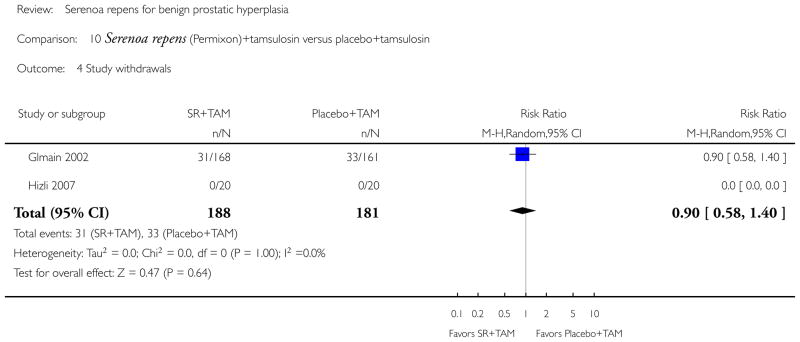
Serenoa repens + tamsulosin versus tamsulosin (dose 0.4 mg daily for both studies) (N = 2)
Urinary symptom scores
Glémain 2002 and Hizli 2007, comparing IPSS total scores, found increases in all arms, but the difference was not significant (Analysis 10.1).
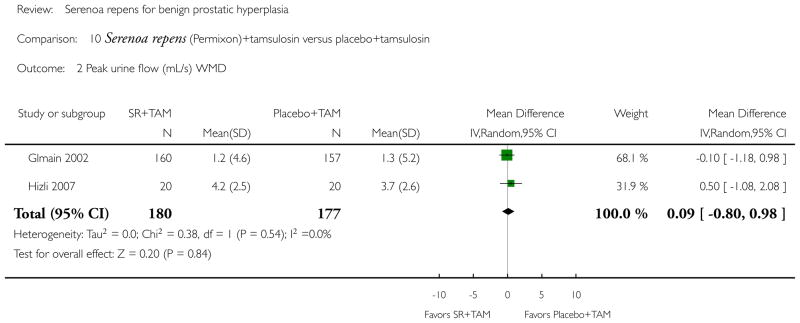
Peak urine flow
Glémain (N = 325) and Hizli (n = 40 in this comparison) reported positive changes in all arms, but no statistical difference (Analysis 10.2).
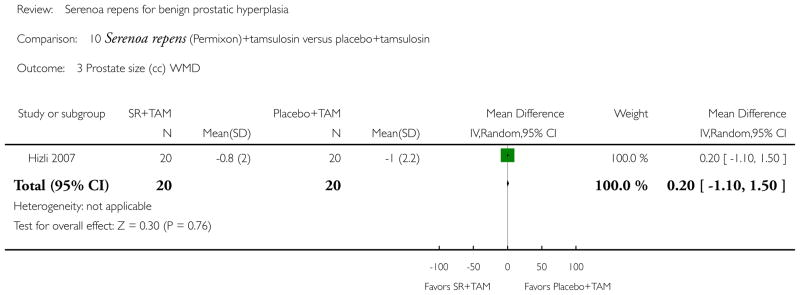
Prostate size
Hizli (n = 40 for these comparisons), in a 24-week study, also reported no significant difference in mean change (MD 0.20 cc, 95% CI −1.10 to 1.50, P > 0.05).
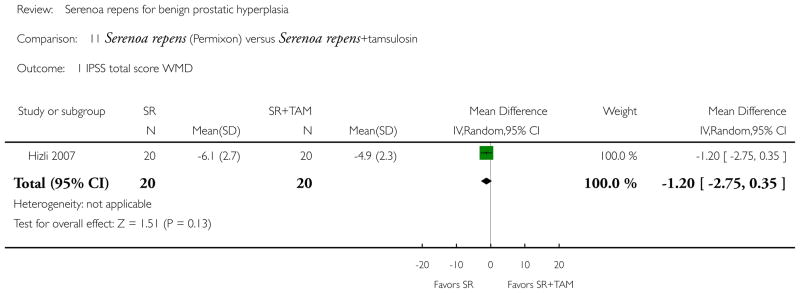
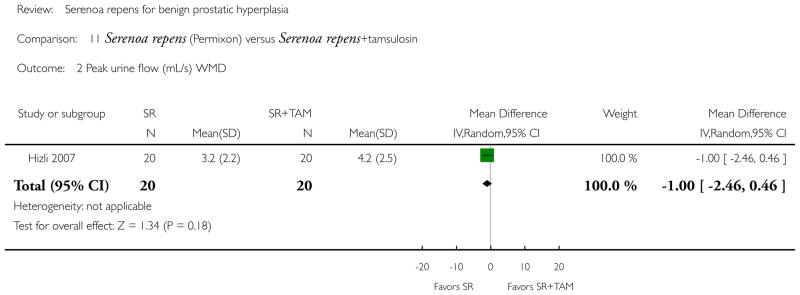
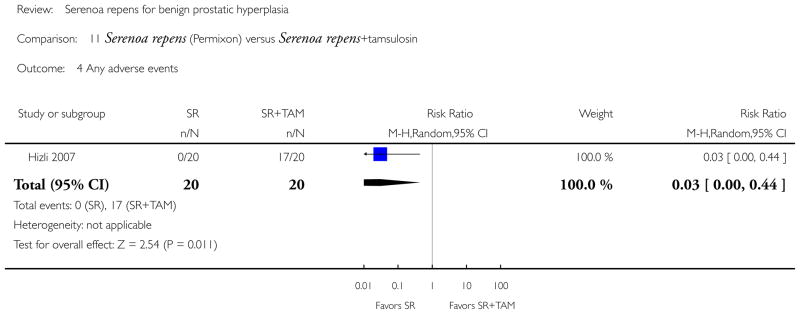
Serenoa repens versus Serenoa repens + tamsulosin (N = 1)
Urinary symptom scores
Hizli 2007 reported no difference in IPSS total score mean change (MD −1.20 points, 95% CI −2.75 to 0.35, P > 0.05).
Peak urine flow
There was no significant difference in mean change (MD −1.00 mL/s, 95% CI −2.46 to 0.46, P > 0.05).
Prostate size
Although both treatments shrank the prostate, Serenoa repens monotherapy was not significantly better than combination therapy (MD 0.10 cc, 95% CI −1.34 to 1.54, P > 0.05).
Peak urine flow
Both arms increased peak urine flow, but monotherapy was not significantly better (MD −1.00 mL/s, 95% CI −2.46 to 0.46, P > 0.05).
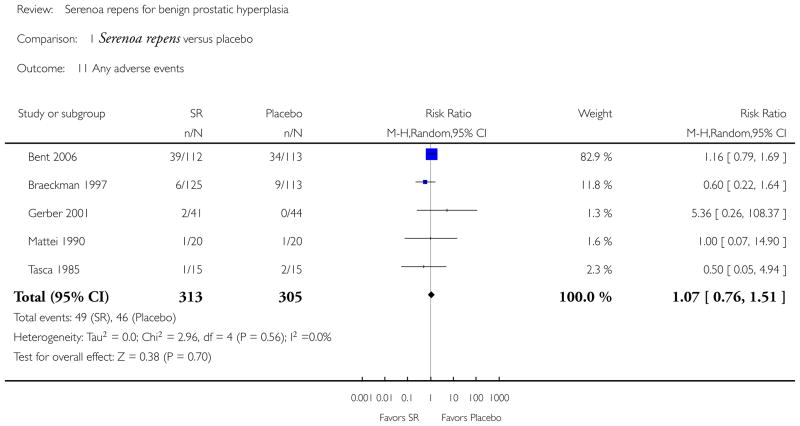
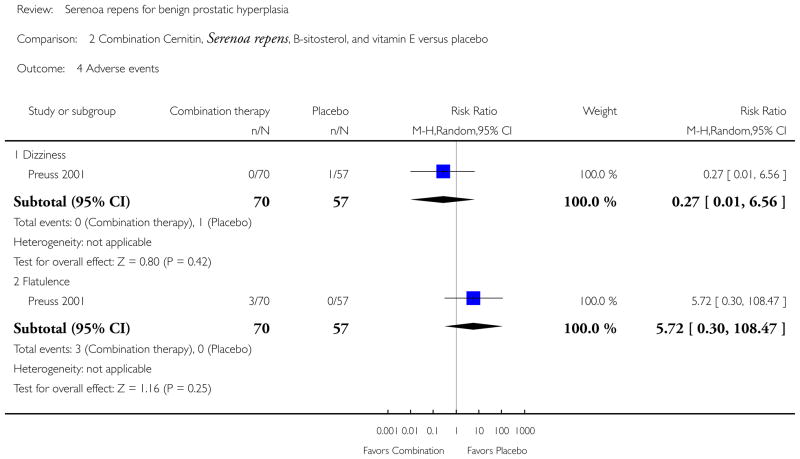
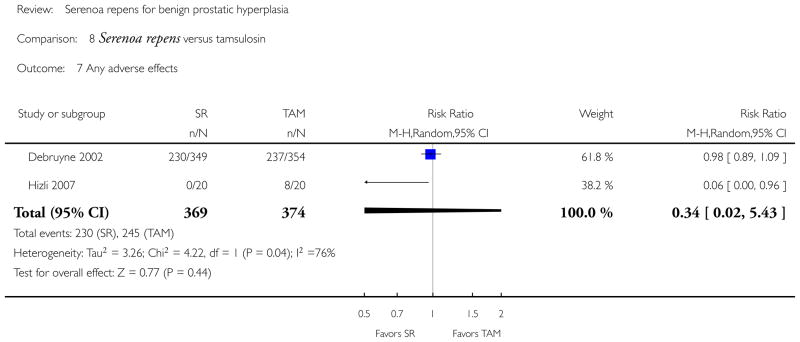
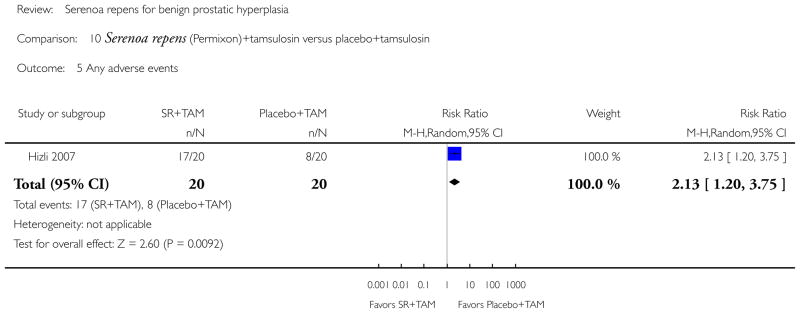
Adverse effects and adverse events
We assessed adverse effects associated with Serenoa repens and active controls (alpha-blockers and 5-alpha reductase inhibitors). For the 19 trials reporting, adverse effects were generally mild. The most common adverse effects associated with Serenoa repens, finasteride, and tamsulosin were asthenia (abnormal loss of strength), decrease in libido, diarrhea, dizziness, ejaculation disorders, gastrointestinal distress, headaches, and postural hypotension. Versus placebo, no arm reported an incidence of adverse effects greater than 5% None of the comparisons was statistically significant (Table 2).
Table 2.
Summary table of adverse effects (SR vs placebo)
| * SR | Placebo | Comparisons P = 0.05 | |
|---|---|---|---|
| n/N (%) | |||
| Dizziness | 10/349 (3) (1 trial) | 1/56 (2) (1 trial) | P = NS |
| Gastrointestinal distress | 30/665 (5) (2 trials) | 3/169 (2) (2 trials) | P = NS |
| Headache | 35/900 (4) (2 trials) | 1/56 (2) (1 trial) | P = NS |
Denominator is number in arm.
Serenoa repens.
Per cents are rounded to the nearest tenth. NS = not statistically significant.
Incidences of asthenia, decrease in libido, dizziness, ejaculation disorders, headache, postural hypotension were most commonly reported in the trials versus tamsulosin. Headache and ejaculation disorders were statistically significantly greater in the tamsulosin arm compared to the Serenoa repens arm (10% versus 4%, and 4% versus 1%, respectively) (Table 3). The RR for any adverse event was 0.34 (95% CI 0.02 to 5.43) (2 studies) (Analysis 8.7).
Table 3.
Summary table of adverse effects (SR vs tamsulosin)
| * SR | § TAM | Comparisons P = 0.05 | |
|---|---|---|---|
| n/N (%) | |||
| Asthenia | 10/349 (3) (1 trial) | 10/354 (3) (1 trial) | P = NS |
| Decrease in libido | 13/890 (1) (2 trials) | 4/354 (1) (1 trial) | P = NS |
| Dizziness | 10/349 (3) (1 trial) | 6/354 (2) (1 trial) | P = NS |
| Ejaculation disorders | 2/349 (1) (1 trial) | 15/354 (4) (1 trial) | P < 0.05 |
| Headache | 35/900 (4) (2 trials) | 37/354 (10) (1 trial) | P < 0.05 |
| Postural hypotension | 4/349 (1) (1 trial) | 3/354 (1) (1 trial) | P = NS |
Denominator is number in arm.
Serenoa repens.
Tamsulosin.
Per cents are rounded to the nearest tenth. NS = not statistically significant.
Compared to finasteride, reported adverse effects included decrease in libido, diarrhea, gastrointestinal distress, and headache. The most common adverse effect reported for Serenoa repens was gastrointestinal distress (5%). The most common adverse effect for finasteride was diarrhea (11%). Only headache was statistically significantly greater in the Serenoa repens arm (4% versus < 1%), (Table 4).
Table 4.
Summary table of adverse effects (SR vs finasteride)
| * SR | ❡FIN | Comparisons P = 0.05 | |
|---|---|---|---|
| Decrease in libido | 13/890 (1) (2 trials) | 16/542 (3) (1 trial) | P = 0.06 |
| Diarrhea | 5/551 (1) (1 trial) | 6/542 (11) (1 trial) | P = NS |
| Gastrointestinal distress | 30/665 (5) (2 trials) | 15/542 (3) (1 trial) | P = NS |
| Headache | 35/900 (4) (2 trials) | 2/542 (< 1) (1 trial) | P < 0.05 |
Denominator is number in arm.
Serenoa repens.
Finasteride.
Per cents are rounded to the nearest tenth. NS = not statistically significant.
Serious adverse events (i.e., events with no necessary causal association with the intervention) were reported in the Bent trial comparing Serenoa repens to placebo (Bent 2006). These events included cardiovascular event, elective orthopedic surgery, gastrointestinal bleeding, bladder cancer, colon cancer, elective hernia repair, hematoma, melanoma, prostate cancer, shortness of breath, and rhabdomyolysis. The Serenoa repens arm had 8 (7%) serious adverse events, and 18 (16%) were reported for the placebo arm (P = 0.05).
In a meta-analysis (5 studies) of ’any’ adverse event, and which included both causal and non-causal harms, there was no difference between the verum and the placebo arms (RR 1.07, 95% CI 0.76 to 1.51 (Analysis 1.11).
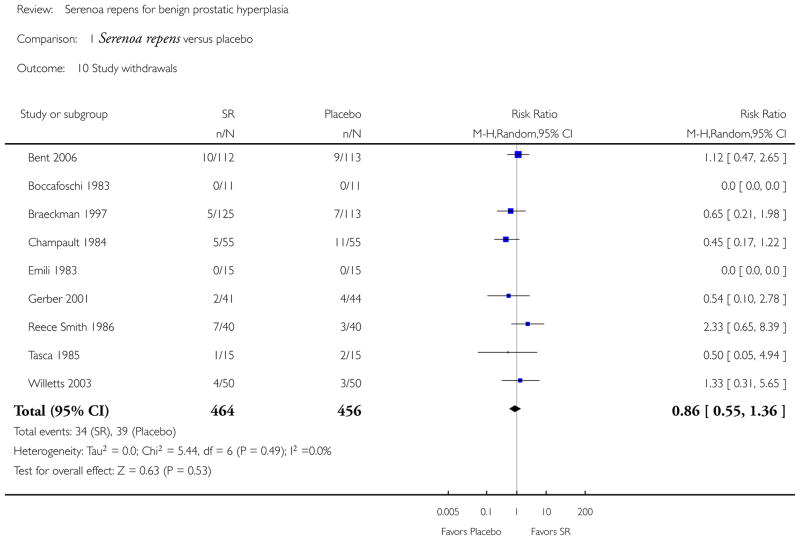
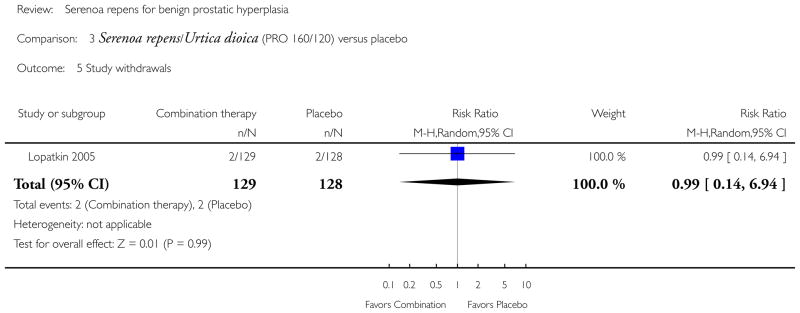
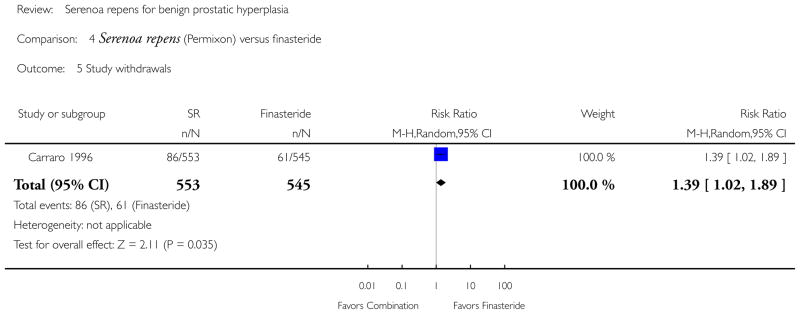
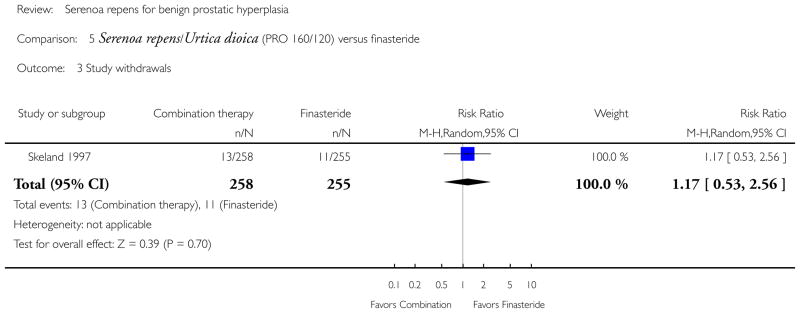
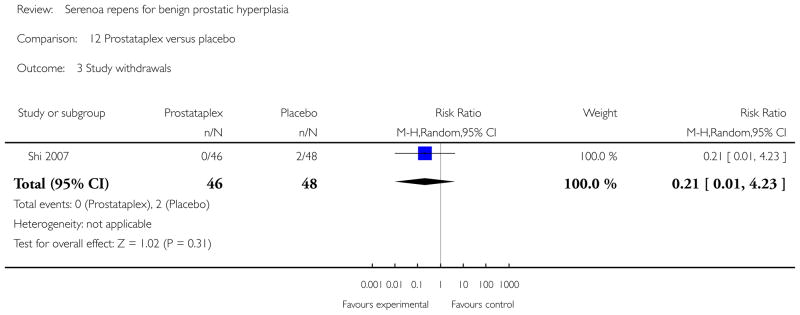
Study withdrawals
All 30 trials reported losses to follow up. The comparison of studies with a Serenoa repens monotherapy arm (n = 15, 175/1483) to trials with a placebo arm (n = 13, 60/721) was 11.8% versus 8.3%, respectively. The RR was 1.42 (95% CI 1.07 to 1.88, P = 0.01), favoring placebo. The tamsulosin (n = 4, 97/624) arms reported a 15.5% withdrawal rate (RR 0.65, 95% CI 0.46 to 0.91, P = 0.01), and favored Serenoa repens monotherapy. Finasteride (n = 2, 72/800) had a 9% rate (RR 1.31, 95% CI 1.01 to 1.70, P = 0.04) and favored finasteride.
DISCUSSION
Summary of main results
We “assess[ed] the effects of Serenoa repens in the treatment of LUTS consistent with BPH” (Wilt 1998). In 1998 and again in 2002 (Wilt 2002), we reported, after evaluating mostly under-powered, short-term trials with variable study design, outcomes, and non-validated symptom-scale scores, that Serenoa repens provided mild improvement of urologic symptoms and flow measures. In this 2008 update we have attenuated our conclusions. In a meta-analysis comparing Serenoa repens to placebo, two trials (Gerber 2001; Bent 2006) reported mean change of the validated IPSS total score. Both trials were well designed and one was adequately powered. Gerber randomized 85 subjects with a follow up of 6 months and a mean age of 65 years. Bent enrolled 225 subjects with a mean age of 63 years in a 12-month trial. The WMD was −0.77 points (95% CI −2.88 to 1.34, P > 0.05). The difference was small and not statistically significant in both studies as well as the pooled analysis. Therefore the two highest quality studies show no substantive benefit versus placebo.
For a consumer looking to see if Serenoa repens offers relief of symptoms for BPH, the evidence is somewhat mixed. In our intra group analysis of the efficacy of Serenoa repens monotherapy, which is generally considered in a clinical setting to be a decrease of three points or greater, we found four trials that reported full data. Three of the four (Gerber; Debruyne; Hizli) reported mean changes of −4.4, −4.4, and −6.1 points for the Serenoa repens arm, respectively. If we discount the two smallest trials (Gerber, N = 79; Hizli, N = 40) with short follow up periods (6 months, respectively), that leaves two large, adequately powered trials, each with 12-month follow ups. Bent shows no clinical efficacy; Debruyne does, but suffers from lack of a placebo arm. At this point we are inclined to accept the evidence of the placebo-controlled Bent trial.
Comparing Serenoa repens to placebo in a meta-analysis of peak urine flow at endpoint (Figure 1), ten trials reported an intergroup WMD of 1.02 mL/s (95% CI −0.14 to 2.19, P = 0.07), an nonsignificant difference and with moderate heterogeneity (I2 = 30%). In a sensitivity analysis including only the four largest, higher quality trials (Bent; Braeckman; Descotes; Willetts), the WMD was 0.43 points (95% CI −0.35 to 1.21, P > 0.05), a non-significant difference with no heterogeneity (I2 = 0%). A second meta-analysis comparing mean change also found no significant difference (WMD 0.31, 95% CI −0.56 to 1.17, P > 0.05; 2 trials).
Figure 1.
Forest plot of comparison: 1 Serenoa repens versus placebo, outcome: 1.4 Peak urine flow (mL/s) at endpoint.
In Bent’s high quality trial comparing ’serious adverse events,’ the relative risk (RR 0.45, 95% CI 0.20 to 0.99, P = 0.05) of a serious event was greater for the placebo arm than the Serenoa repens arm. In a meta-analysis of the relative risk of ’any adverse event’, there was no significant difference between Serenoa repens and placebo (RR 1.07, 95% CI 0.76 to 1.51, P > 0.05; 5 trials).
Overall completeness and applicability of evidence
The overall completeness of the evidence was fairly good in 2008, and much better than it was at the inauguration of this review in 1998. For example, of the 14 trials that were placebo controlled and compared to Serenoa repens monotherapy, 7 utilized the commercialized Permixon®, which assured that the comparators were equivalent. Fifteen of the thirty trials used a validated score - the AUA or IPSS - to assess symptoms. Fourteen of fifteen of those trials provided baseline and endpoint IPSS or AUA scores, although not all gave SD. Nine of the fifteen reporting studies provided mean change with SD for either the IPSS or AUA total score. Of 14 trials with baseline and endpoint data for nocturia, 11 provided means, 1 provided “per cent with nocturia,” and 1 an AUA nocturia grade. Twenty-one trials reported baseline and endpoint data for peak urine flow, and five reported mean differences. Ten of thirty trials provided data at baseline and endpoint for prostate size, and three provided mean change with SD.
In general, the newest trials reported validated symptom scores, provided baseline and endpoint data (with SD, SEM (standard errors), CI) and mean differences. In the future, larger, high quality trials, (and a placebo arm in trials with controls), using validated symptom-scale scores and mean changes for outcome measures, will give us much better data to judge the efficacy of Serenoa repens.
Quality of the evidence
Our first iteration of this review included 18 trials, of which only 6 randomized 100 subjects or more. The other 12 trials ranged from 22 to 80 subjects. In our update of 2002 we added three trials, with subjects of 44, 85, and 101, respectively. This update has added nine trials enrolling subjects ranging from 60 to 704. Of 30 trials, 14 randomized 100 subjects or more (range 100 to 1098). This trend of higher powered trials - and with their corresponding smaller CI - yields statistically better evidence. There has been upward trends in the quality of studies and evidence. As noted above, 15 of 30 (50%) trials used validated symptom-scale scores; in the 1998 review only 3 of 18 (17%) did. Eleven trials reported nocturia data (times/per evening) at baseline and endpoint, but none reported mean change with SD, a statistically better metric, because repeated measures at baseline and endpoint tend to be correlated, leading to smaller SEM and CI, and thus a truer estimate of treatment effect. For prostate size and peak urine flow, there was more data reporting mean change. Four trials reported baselines and endpoints for prostate size, and three reported mean changes. For peak urine flow, the ratio was more lopsided: 13 trials reported baselines and endpoints, and 5 reported mean changes.
Potential biases in the review process
From our very first review in 1998 we were sensitive to biases among trials and their reported outcomes. We decided a priori to report all outcomes using a random-effects model, which is a more conservative estimate of treatment effect. In the 10 years we began this process, there has been a dismaying lack of clarity of descriptions, or even descriptions, of study design, even among top-drawer, peer-reviewed journals. We evaluated five criteria
adequate sequence generation (was there an articulated rule for allocating interventions based on chance?)
allocation concealment (was there any foreknowledge of the allocation of interventions by anyone?)
blinding (during the course of the trial were study participants and personnel blinded to the knowledge of who received which intervention?)
incomplete outcome data addressed (did the trial assess all patients, or account for those not assessed?)
free of other bias (selective outcome reporting, differences between/among arms in how outcomes were determined), and graded them by A (“yes”), B (“unclear”), and C (“no”). For “adequate sequence generation” among the 30 included studies, we reported 30% with “adequate” scores (the other 20 trials scored “unclear”). “Allocation concealment” was “adequate” in 43% (13/30). The other 17 trials reported “unclear” (57%). Eighty-seven per cent of the trials reported “adequate” blinding. Two trials (7%) were “unclear,” and 2 (7%) were not blinded. Twenty-five of thirty trials (83%) reported no “incomplete outcome data.” Ninety-seven per cent reported no “selective [outcome] reporting,” and 93% reported no other sources of bias.
Agreements and disagreements with other studies or reviews
In this update we report that Serenoa repens monotherapy does not improve urinary symptom scores (IPSS, AUA), peak urine flow, or shrink the prostate. In general, these results contradict our two previous findings in 1998 and 2002, as well as - in part - a systematic review performed in 2004 (Boyle 2004). In this analysis Boyle compared Permixon® to placebo with 14 RCTs and three open-label trials for a total of 4280 subjects. Comparing IPSS total scores, Boyle noted an intra group point decrease for both arms (Permixon® 4.78 versus placebo 4.54), but based on only one and two studies, respectively. In the head-to-head comparison, the intergroup difference was not significant (−1.10 points (95% CI −1.66 to 1.46, P > 0.05). In our two-study meta-analysis we found no difference in mean change (−0.77 (95% CI −2.88 to 1.34, P > 0.05), but also with significant heterogeneity (I2 = 63%). These analyses would suggest that there is no benefit to Serenoa repens over placebo.
In Boyle, both arms increased peak urine flow (Permixon® 1.02 mL/s versus placebo 1.20 mL/s) from baseline, but the comparison favored placebo (P = 0.04). In our meta-analysis (10 trials) of endpoints and with minimal heterogeneity (I2 = 30%), there was no significant difference among trials (WMD 1.02 mL/s, 95% CI −0.14 to 2.19, P = 0.08). Comparing mean change (2 trials), our meta-analysis found no significant difference as well (0.31 mL/s (95% CI −0.56 to 1.17, P > 0.05) and no heterogeneity (I2 = 0%). Boyle also noted a significant decrease in nocturnal voids for both arms (Permixon® 0.38 versus placebo 0.63), with the comparison favoring placebo (P < 0.05). In our meta-analysis (Analysis 1.3) of nocturia at endpoint, there was a significant difference (−0.78 nocturnal voids, 95% CI −1.34 to −0.22, P < 0.05) between arms favoring Serenoa repens, but also with considerable heterogeneity (I2 = 66%).
AUTHORS’ CONCLUSIONS
Implications for practice
Serenoa repens is widely used for symptomatic BPH in Europe and the United States, and widely recommended by clinicians in both. Millions of men use it, with little or no evidence of its efficacy or safety. We now have some evidence of both, and the evidence points to a safe product (at current doses) but with little or no efficacy. For both Europe and the US, greater government regulation is needed. Europe, at a national or transnational level, needs to insure that phytotherapeutic agents, such as Serenoa repens, are safe and live up to their scientific claims. In the US the Food and Drug Administration (FDA) needs to revisit the 1994 Dietary Supplement and Health Education Act, which holds herbal remedies to a ’no standard’ compared to pharmaceutical agents. If herbal products make scientific claims, they need to support those claims with scientific evidence that is open to public scrutiny.
Implications for research
In this update we report the efficacy of Serenoa repens is in doubt. Although we acknowledge a certain amount of ambiguity in the evidence, we believe that as future trials of the quality of Bent’s are published, the inefficacy of Serenoa repens will become clearer. These future trials will need to be adequately powered, use validated symptom scores, and be properly randomized and blinded. If Serenoa repens is compared to other interventions, a placebo arm should also be added.
Serenoa repens and other phytotherapies for BPH should be scrutinized and subjected to trials just as are all regulated drugs. For too long these and other homeopathic phytotherapies have been used as accepted remedies without the proper skepticism they deserve. This practice should become a thing of the past.
Acknowledgments
This work was partially funded by Grant Number R24 AT001293 from the National Center for Complementary and Alternative Medicine (NCCAM), and the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Grant Number 1R01 DK063300-01A2. Authors are employees of the US Department of Veterans Affairs. The contents of this systematic review are solely the responsibility of the authors and do not necessarily represent the official views of the NCCAM, the National Institutes of Health, or the Department of Veterans Affairs. We also wish to thank Maurizio Tiso, Margaret Haugh, Rich Crawford, Tatyana Shamilyan, Philipp Dahm, and Joan Barnes for their work in translating and abstracting data from the non-English language studies.
SOURCES OF SUPPORT
Internal sources
Management Decision and Research Center-Department of Veterans Affairs HSRD, USA.
Minneapolis/VISN-13 Center for Chronic Diseases Outcomes Research (CCDOR), USA.
External sources
-
The Cochrane Complementary Medicine Field bursary award, USA.
The Cochrane review group Prostatic Diseases and Urologic Cancers received a one-time payment from the Cochrane Complementary Medicine Field to update this review.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Number of sites unknown Randomization: unclear Patients blinded; providers blinded |
|
| Participants | Geographic region: Germany/Italy Study setting: community N = 101 Baseline IPSS: Sabal extract 9.6, Placebo 8.9 Baseline prostate volume: Sabal extract 34.5 cc, Placebo 31.7 cc Mean age: 66.1 Age range: NA Race: White Diagnostic criteria: confirmed diagnosis of BPH with enlargement of the prostate, symptoms of obstruction and a maximum flow of < 15 mL/s |
|
| Interventions | Control: matching placebo Treatment: Sabal extract (LG166/S) 160 mg twice daily Study duration: 6 months Lost to follow up: 3(?) |
|
| Outcomes | IPSS symptom score Peak urine flow Prostate volume Sexual function Dropouts due to side effects: 0 |
|
| Notes | Exclusions: patients treated for BPH within 1 month of the trial start; prostate cancer; acute urinary tract infection; chronic prostatitis; neurogenic bladder | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Unclear | B - per protocol outcomes |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Unclear | A - Adequate |
| Methods | Dual-site and surrounding community Randomization: computer generated Patients blinded; providers blinded |
|
| Participants | Geographic region: Northern California Study setting: VA Hospital/Kaiser Permanente and community N = 225 Baseline AUA: SR 15.7, Placebo 15.0 Baseline prostate volume: SR 34.7 cc, Placebo 33.9 cc Mean age: 63.0 Age range: NA Race: White 82%; Black 5%; Asian or Pacific Islander 7%; Hispanic 5%; Other 1% Diagnostic criteria: moderate-to-severe symptoms of BPH (AUA ≧ 8); QMAX < 15 mL/s |
|
| Interventions | Control: matching placebo Treatment: Sabal extract 160 mg twice daily Study duration: 12 months Lost to follow up: n = 9 |
|
| Outcomes | AUA symptom score BPH Impact Index Peak urine flow |
|
| Notes | Exclusions: < 49 years old; less than moderate symptoms of BPH (AUA < 8); Qmax < 4 mL/s or residual volume > 250 mL after voiding; hx of prostate cancer; surgery for BPH; urethral stricture; neurogenic bladder; creatinine > 2 mg/dL; PSA > 4 ng/dL; medications known to affect urination; severe concomitant disease | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A -Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: Sealed envelopes Patients blinded; providers blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 22 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 68.0 Age range: 54 to 78 Race: White Diagnostic criteria: Men with symptomatic BPH not in need of surgery |
|
| Interventions | Control: matching placebo Treatment: Permixon® 160 mg twice daily Study duration: 8.5 weeks Lost to follow up: None |
|
| Outcomes | Dysuria (4-point scale) Peak urine flow Mean urine flow Voiding time Total voided volume Pollachiuria Dropouts due to side effects: not reported |
|
| Notes | Exclusions: Cancer; currently on other medication; urinary tract infection | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Unclear | B |
| Free of other bias? | Yes | A - Adequate |
| Methods | Number of sites unknown Randomization: sequentially numbered sealed opaque envelopes Patients blinded; providers blinded |
|
| Participants | Geographic region: Belgium Study setting: community N = 238 Baseline IPSS: NA Baseline prostate volume: Prostaserene™ 44 cc, Placebo 45 cc Mean age: 65 Age range: 57 to 73 Race: White Diagnostic criteria: Peak urine flow 5 to 15 mL/s; residual urine volume less/equal 60 mL; Personal score list 0 to 4; No global physician assessment |
|
| Interventions | Control: matching placebo Treatment: Prostaserene® 160 mg twice daily Study duration: 12 weeks Lost to follow up: 5% |
|
| Outcomes | Symptom improvement Peak urine flow Mean urine flow Total voided volume Bladder residual volume Prostate size Dropouts due to side effects: < 1% |
|
| Notes | Exclusions: Age > 80 years; prostate/other cancers; urine flow < 5mls/sec or > 15mls/sec; residual volume > 60 mL; currently on medications; urinary tract infection | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B - Randomization by each center |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: random allocation according to a centrally controlled code list Patients blinded; providers blinded |
|
| Participants | Geographic region: Sweden and Denmark Study setting: community N = 55 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 61.6 Age range: 51 to 72 Race: White Diagnostic criteria: The presence of BPH on the basis of history, clinical examination of the prostate and acid phosphatase determination |
|
| Interventions | Control: matching placebo Treatment: Combination phytotherapy: Curbicin (Sabal serrulata 80 mg and Cucurbita pepo L. (pumpkin seeds) 80 mg) 2 tablets thrice daily Study duration: 12 weeks Lost to follow up: 4% |
|
| Outcomes | Dysuria Mean urine flow Voiding time Bladder residual volume Nocturia Patient self-evaluation Dropouts due to side effects: 0 |
|
| Notes | Exclusions: Need of imminent surgery due to symptom severity; bladder residual urine > 300 mL; previous treatment with Curbicin | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: computer-generated randomization code Patients blinded; providers blinded |
|
| Participants | Geographic region: Nine European countries Study setting: community N = 1098 Baseline IPSS: Permixon® 15.7, Finasteride 15.7 Baseline prostate volume: Permixon® 43.0 cc, Finasteride 44.0 cc Mean age: 64.5 Age range: 49 to 88 Race: White Diagnostic criteria: BPH diagnosed by digital rectal exam (DRE); International Prostate Symptom Score (IPSS) > 6; Maximun urinary flow between 4 to 15mL/sec (with a urine volume at least 150 mL, and a postvoid residue of < 200 mL); prostate size > 25mL; serum prostate-specific antigen (PSA) < 10 ng/mL (prostates less than or equal to 60 mL) or 15 ng/mL (prostates > 60 mL); good mental and physical condition |
|
| Interventions | Control: finasteride 5 mg (Proscar) plus placebo (morning) and two placebos (evening) Treatment: Permixon® 160 mg plus placebo twice daily Study duration: 26 weeks Lost to follow up: 13.4% |
|
| Outcomes | Symptom improvement - IPSS symptom score (0 to 35 points) Quality of life score (0 to 6 points) Sexual function score (0 to 20 points) Peak urine flow Mean urine flow Total voided volume Bladder residual volume Prostate size (volume) Serum PSA Dropouts due to side effects: 4% (28 Permixon® and 14 finasteride) |
|
| Notes | Exclusions: Prostate cancer; bladder disease; abnormal liver function; diuretics or drugs with antiandrogenic or alpha-receptor properties in the preceding 3 months; urogenital infections; disease potentially affecting micturition | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Number of sites unknown Randomization: unclear Patients blinded; providers blinded |
|
| Participants | Geographic region: France Study setting: community N = 110 Baseline IPSS: NA Baseline prostate size: NA Mean age: NA Age range: NA Race: White Diagnostic criteria: Peak urine flow; mean urine flow; residual urine volume; (No details given) |
|
| Interventions | Control: matching placebo Treatment: Permixon® 80 mg twice daily Average follow up: 4 weeks Lost to follow up: 15% |
|
| Outcomes | Dysuria Mean urine flow Bladder residual volume Nocturia Patient self-rating Physician self-rating Dropouts due to side effects: not reported |
|
| Notes | Exclusions: prostate cancer | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Unclear | B - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: numbered or coded identical containers administered sequentially Patients blinded; providers blinded |
|
| Participants | Geographic region: France Study setting: community N = 168 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 69 Age range: NA Race: White Diagnostic criteria: Patients with “prostatism” or for whom surgery was not indicated (no mechanical or infectious complications) |
|
| Interventions | Control: matching placebo Treatment: Permixon® 160 mg twice daily Study duration: 10 weeks Lost to follow up: 13% |
|
| Outcomes | Symptom score (# of daily mictions) Dysuria (4-point scale) Bladder residual volume Nocturia Dropouts due to side effects: not reported |
|
| Notes | Exclusions: Symptoms for at least 6 months | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Unclear | B - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: not described Patients blinded; providers blinded but not described |
|
| Participants | Geographic region: 98 centers in 11 European countries Study setting: community N = 704 Baseline IPSS: Permixon® 15.5, Tamsulosin 15.2 Baseline prostate size: Permixon® 48.0 cc, Tamsulosin 47.7 cc Mean age: 64.9 Age range: 50 to 85 Race: NA Diagnostic criteria: IPSS ≥ 10; Peak urine flow 5 to 15 mL/s; voided vol at least 150 mL; post-voiding vol < 150 mL; prostate vol ≥ 25 cc; serum PSA < 4 ng/mL (men w/PSA 4 to 10 ng/mL required a free/total PSA ratio of at least 15%) |
|
| Interventions | Control: tamsulosin 0.4 ng daily (capsules were matched in color, smell, size) Treatment: Permixon® 320 ng daily Follow up: 12 months Lost to follow up: n = 110 |
|
| Outcomes | IPSS total score Nocturia Peak urine flow Dropouts due to side effects: tamsulosin n = 8; Permixon® n = 3 |
|
| Notes | Exclusions: hx of bladder disease likely to affect micturition; urethral stenosis; PC; pelvic radiotherapy; repeated infection of the urinary tract; chronic bacterial prostatitis; any disease likely to cause urinary problems; pts w/clinically significant cardiovascular dx; hematuria, insulin-dependent diabetes mellitus; hx severe hepatic failure; abnormal liver function tests; concomitant medication likely to interfere w/study medication; known hypersensitivity to study drugs; participation in other clinical trial in previous 3 months | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Unclear | B |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization:noted but method not stated Patients blinded; providers blinded |
|
| Participants | Geographic region: France Study setting: community N = 215 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 66.3 Age range: NA Race: White Diagnostic criteria: Mild-moderate (stage I or II) BPH; Dysuria: daytime and nocturnal urinary frequency (> 2 nocturnal micturitions, excluding those at bedtime and on awakening) of at least 8 weeks; maximum urinary flow > or equal to 5 mL/s |
|
| Interventions | Control: matching placebo Treatment: Permixon® 160 mg twice daily Study duration: 4 weeks Lost to follow up: 18% |
|
| Outcomes | Dysuria Peak urine flow Mean change in daytime urinary frequency Nocturia Patient-based global efficacy Physician-based global efficacy Dropouts due to side effects: 1 (complaints of fatigue, depression and stomach upset) |
|
| Notes | Exclusions: Excessively mild or severe symptoms of BPH including incontinence, bladder distension, urine flow< 5mls/sec; cancer; prior treatment for BPH; urogenital infection; hematuria; diabetes; any prior surgery that could induce dysuria | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: noted but method not stated Patients blinded; providers blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 30 Baseline IPSS: NA Baseline prostate volume: NA Mean age: NA Age range: 44 to 78 Race: White Diagnostic criteria: Men with manageable BPH |
|
| Interventions | Control: matching placebo Treatment: Permixon® 160 mg twice daily Study duration: 4 weeks Lost to follow up: none |
|
| Outcomes | Peak urine flow Mean urine flow Bladder residual volume Prostate size (qualitative scale used) Nocturia Dropouts due to side effects: none |
|
| Notes | Exclusions: Prior treatment for BPH | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: noted but not described Patients blinded; providers blinded |
|
| Participants | Geographic region: Germany Study setting: private out-patient centers N = 140 Baseline IPSS: Prostagutt® forte 20.0, Tamsulosin 21.0 Baseline prostate volume: NA Mean age: 65.0 Age range: NA Race: NA Diagnostic criteria: maximum urinary flow rate ≤ 12 mL/s at a urinary volume ≥ 150 mL |
|
| Interventions | Control: tamsulosin 0.4 mg daily Treatment: Prostagutt® forte (sabal fruit extract+urtica root extract) twice daily Study duration: 60 weeks Lost to follow up: n = 3 (a total of 121 completed the trial at week 60) |
|
| Outcomes | IPSS total score IPSS QoL CEDQ (Cologne Erectile Dysfunction Questionnaire) Peak urine flow Mean urine flow Mean urine volume Duration of flow increase Ultrasound residual volume |
|
| Notes | Exclusions: Pts whose peak urinary volume changed by more than 3 mL/s during a 2-week period; < 50 yrs old; IPSS < 13 and < 3 for the IPSS QoL; residual urinary volume < 150 mL; congested urinary tract passages; an indication of BPH surgery; urinary tract infection; prostate carcinoma; diabetes; neurogenic or bladder dysfunction; previous treatment w/5ARI; concomitant medication that could interfere w/treatment efficacy | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: unclear Patients blinded; providers blinded |
|
| Participants | Geographic region: Croatia Study setting: community N = 30 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 65.0 Age range: 40 to 82 Race: White Diagnostic criteria: BPH, stage I–II (Vahlensieck) |
|
| Interventions | Control: placebo Treatment: Prostagutt® forte (Serenoa repens and Urtica dioica) 20 drops thrice daily Study duration: 6 weeks Lost to follow up: none |
|
| Outcomes | Physician rating of improvement Peak urine flow Bladder residual volume Dropouts due to side effects: none |
|
| Notes | Exclusions: Stage IV prostate adenoma; bacterial prostatitis; cystitis; urethritis | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Unclear | B |
| Free of selective reporting? | Unclear | A - Adequate |
| Free of other bias? | Unclear | A - Adequate |
| Methods | Multisite or single-site: NA Randomization: computer number table Patients blinded; providers blinded |
|
| Participants | Geographic region: USA Study setting: community N = 85 Baseline IPSS: Serenoa repens 16.7, Placebo 15.8 Baseline prostate volume: NA Mean age: 65.0 Age range: ≥ 45 Race: NA Diagnostic criteria: IPSS score ≥ 8 |
|
| Interventions | Control: placebo Treatment: Serenoa repens 160 mg twice daily Study duration: 6 months Lost to follow up: 7% (2 Serenoa repens, 4 Placebo) |
|
| Outcomes | Symptom improvement - IPSS symptom score Quality of Life score Peak urine flow Dropouts due to side effects: 1% (n = 1, Serenoa repens) |
|
| Notes | Exclusions: prostate surgery; history of prostate cancer or urethral stricture; treated with finasteride, saw palmetto or other alternative therapy (past 6 months); or treated with alpha-blocker (within 1 month) | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization noted but not described Patients and providers blinded; unsure if assessors blinded |
|
| Participants | Geographic region: France Study setting: 47 regional settings N = 329 Baseline IPSS: tamsulosin + Serenoa repens (Permixon®) 16.2, Tamsulosin 16.3 Baseline prostate volume: NA Mean age: 65.0 Age range: NA Race: NA Diagnostic criteria: IPSS ≥ 13, Peak urine flow 7 to 15 mL/s |
|
| Interventions | Control: tamsulosin daily + placebo twice daily Treatment: tamsulosin daily + Serenoa repens (Permixon®) twice daily Study duration: 52 weeks Lost to follow up: n = 64 |
|
| Outcomes | Symptom improvement-IPSS total score IPSS QoL & UROLIFE© BPH QoL9 Peak urine flow Dropouts due to side effects: none |
|
| Notes | Exclusions: previous surgery on the prostate, vesicle collar or pelvic area; residual post-urine volume of >300 mL; prostate cancer; urine infection; α/β-blockers, α-agonists, cholinergics or anticholinergics were prohibited; hepatic insufficiency; cardiovascular event or cerebrovascular event; allergy to intervention drugs Treatments for BPH (such as α-blockers) stopped at least 15 days before randomization; other treatments, such as plant extracts and finasteride, were stopped 1 month before randomization. |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single or multisite: NA Randomization: NA Blinding: not described |
|
| Participants | Geographic region: Turkey Study setting: unknown N = 60 Baseline IPSS: Serenoa repens (Permixon®) 16.2, tamsulosin 18.0, Serenoa repens (Permixon®) + tamsulosin 15.6 Baseline prostate volume: Serenoa repens (Permixon®) 35.2 cc, tamsulosin 38.6 cc, Serenoa repens (Permixon®) + tamsulosin 31.2 cc Mean age: 58.6 Age range: 43 to 73 Race: NA Diagnostic criteria: IPSS ≥ 10; Peak urine flow 5 to 15 mL; prostate volume ≥ 25 cc; PSA ≤ 4 ng/mL |
|
| Interventions | Control 1: tamsulosin 0.4 mg daily Control 2: Serenoa repens (Permixon®) 320 mg daily + tamsulosin 0.4 mg daily Treatment: Serenoa repens (Permixon®) 320 mg daily Study duration: 24 weeks Lost to follow up: none |
|
| Outcomes | IPSS total score IPSS QoL Prostate volume PSA Post-void residual volume |
|
| Notes | Exclusions: cardiovascular disease; hematuria; insulin dependent diabetes; prostate cancer; concomitant meds likely to interfere w/study meds; hypersensitivity to study drugs; concomitant meds likely to interfere w/study meds; hypersensitivity to study drugs; pelvic radiotherapy; UT repeated infection; chronic bacterial prostatitis; any other disease that causes urinary problems; hx of severe hepatic failure; abnormal liver function; hx of bladder disease likely to affect micturition; urethral stenosis; and participating in clinical trial in last 3 months. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Unclear | B |
| Incomplete outcome data addressed? All outcomes |
No | C |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Unclear | B |
| Methods | Multisite study Randomization: random number generator program Patients blinded; Providers blinded |
|
| Participants | Geographic region: Europe Study setting: NA N = 257 Baseline IPSS: PRO 160/120 (Prostagutt® forte) 18.0, Placebo 18.0 Baseline prostate volume: PRO 160/120 (Prostagutt® forte) 44.9 cc, Placebo 46.4 cc Mean age:PRO 160/120 68±7 (n = 127); Placebo 67±7 (n = 126) Age range: NA Race: NA Diagnostic criteria: Peak urine flow (voiding volume): <15 mL/s; change in max urinary flow between screening and of run-in period ? 3 mL/s; urinary output at baseline: > 100 mL; IPSS total score ≥ 14; IPSS QoL ≥ 4 |
|
| Interventions | Control: matching placebo Treatment: PRO 160/120 (Prostagutt® forte) 160 mg Serenoa repens + 120 mg Urtica dioica twice daily Study duration: 24 weeks Lost to follow up: 7 |
|
| Outcomes | IPSS total score IPSS QoL Peak urine flow |
|
| Notes | Exclusions: age < 50; PSA >10 ng/mL; PC; large residual urine > 350 mL; concomitant meds affecting micturition (α-blockers); previous surgery on pelvis, urinary tract, urethral stricture or pelvic radiation; symptomatic urinary tract infection; chronic bacterial prostatitis; serious health risks; diabetes; diabetic neuropathy; mental condition to restrict informed consent. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: computer-generated randomization code Patients blinded; providers blinded |
|
| Participants | Geographic region: Germany Study setting: community N = 60 Baseline IPSS: NA Baseline prostate volume: NA Mean age: NA Age range: 40 to 82 Race: White Diagnostic criteria: BPH, stage I–II; peak urine flow < 20 mL/s |
|
| Interventions | Control: matching placebo Treatment: Sabal extract 100 mg daily Study duration: 6 weeks Lost to follow up: none |
|
| Outcomes | Peak urine flow Mean urine flow Dropouts due to side effects: none |
|
| Notes | Exclusions: NA | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Number of sites unknown Randomization: Identical packaging Patients blinded; providers blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 60 Baseline IPSS: NA Baseline prostate volume: NA Mean age: NA Age range: 50 to 80 Race: White Diagnostic criteria: Men with symptomatic BPH confirmed on rectal examination |
|
| Interventions | Control 1: matching placebo Control 2: Pygeum africanum extract Treatment: Permixon® 320 mg daily Study duration: 4 weeks Lost to follow up: unclear |
|
| Outcomes | Patient self-rating Dysuria (pain on voiding) Urgency Tenesmus Difficult urination Post-voiding residue Pollachiuria Nocturia Dropouts due to side effects: none |
|
| Notes | Exclusions: Details not given | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: table of random numbers Patients blinded |
|
| Participants | Geographic region: USA Study setting: community N = 44 Baseline IPSS: Saw palmetto herbal blend 18.4, Placebo 16.4 Baseline prostate volume: Saw palmetto herbal blend 58.5 cc, Placebo 55.6 cc Mean age: 64.0 Age range: 45 to 80 Race: White 73%, Black 7%, Asian 11% Diagnostic criteria: moderate to severe BPH with enlarged prostate (DRE), IPSS score of 9 or greater, PSA < 15 ng/mL, prostate volume 30 cc or greater |
|
| Interventions | Control: placebo Treatment: Saw palmetto herbal blend (saw palmetto 106 mg, nettle root extract 80 mg, pumpkin seed oil extract 160 mg, vitamin A 190 mg) thrice daily Study duration: 6 months Lost to follow up: 7% |
|
| Outcomes | Symptom improvement - IPSS symptom score Peak urine flow Post-void residual volume PSA Prostate volume Dropouts due to side effects: None |
|
| Notes | Exclusions: concurrent use of α-blockers; use of finasteride, phytotherapy within last 18 months or α-blockers within last month; chronic prostatitis; previous bladder or prostate surgery; neurogenic bladder | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: noted but method not stated Patients blinded; providers blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 40 Baseline IPSS: NA Baseline prostate volume: Talso (Serenoa repens extract) 36 mm (diameter), Placebo 37 mm Mean age: NA Age range: 45 to 72 Race: White Diagnostic criteria: Men with manageable BPH |
|
| Interventions | Control: matching placebo Treatment: Talso (Serenoa repens extract) 160 mg twice daily Study duration: 13 weeks Lost to follow up: 5% |
|
| Outcomes | Dysuria (symptom score 0 to 4) Bladder residual volume (incomplete emptying - symptom score 0 to 4) Discomfort (Pollachiuria - symptom score 0 to 4) Daytime frequency Nocturia Prostate size Dropouts due to side effects: 1 patient from each group due to “stomach pains.” Unclear relation to therapy |
|
| Notes | Exclusions: Urogenital disease; prostate cancer | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: computer-generated randomization code Patients blinded; providers blinded |
|
| Participants | Geographic region: Germany Study setting: community N = 40 Baseline IPSS: Prostagutt® forte 18.6, Placebo 19.0 Baseline prostate volume: NA Mean age: 65.5 Age range: 52 to 84 Race: White Diagnostic criteria: BPH, Alken stage I–II |
|
| Interventions | Control: matching placebo Treatment: Combination phytotherapy: Prostagutt® forte (Serenoa repens 160mg and Urtica dioica 120mg) 1 capsule twice daily Study duration: 48 weeks Lost to follow up: 7.5% |
|
| Outcomes | Symptom improvement-IPSS symptom score Peak urine flow Bladder residual volume Patient self-evaluation Dropouts due to side effects: none |
|
| Notes | Exclusions: Age < 50 years; cancer; taking other prostate medications/contraindicated medications; infections; recent or current urinary tract operations | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: noted but method not stated Patients not blinded; providers not blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 60 Baseline IPSS: NA Baseline prostate volume: NA Mean age: NA Age range: 44 to 78 Race: White Diagnostic criteria: Men with BPH without prior treatment; bladder residual volume of < 150 mL |
|
| Interventions | Control: Depostat (gestonorone caproato 200 mg) intra-muscularly every week for 8 weeks Treatment: Permixon® 160 mg twice daily Study duration: 8 weeks Lost to follow up: none |
|
| Outcomes | Dysuria (% of subjects with symptoms) Pollachiuria Nocturia Peak urine flow Voiding time Prostate size Dropouts due to side effects: none |
|
| Notes | Exclusions: Cancer; urogenital infections | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
No | C |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: by cluster method Patients blinded; providers blinded |
|
| Participants | Geographic region: Washington, DC, Florida, Idaho N = 144 Baseline AUA: Cerniton AF™ 18.9, Placebo 17.7 Baseline prostate volume: NA Mean age: NA Age range: NA Race: NA Diagnostic criteria: dx of BPH; maximal urinary flow rate of 5 to 15 mL/s for a voided volume in excess of 100 mL |
|
| Interventions | Control: Placebo Treatment: Cerniton AF™ (378 mg), saw palmetto complex, phytosterol, B-sitosterol (286 mg), and vitamin E (100 IU) twice daily Study duration: 3 months Lost to follow up: 17 |
|
| Outcomes | AUA emptying frequency hesitancy urgency weak stream straining nocturia Adverse events Bladder volume Mean flow rate Maximal flow rate |
|
| Notes | Exclusions: > 80 yrs old; presence of any tumor, malformation, or infection of the genitourinary tract; any severe or concomitant medical condition that would make it difficult to participate; severe lab abnormalities (WHO grade 2 to 4); medical treatment for BPH w/finasteride within last 4 weeks; pts treated w/antibiotics for genitourinary tract infections | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A- Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Unclear | A - Adequate |
| Free of other bias? | No | C - Cluster randomized method |
| Methods | Single-site study Randomization: random allocation with numbered folders Patients blinded; providers blinded |
|
| Participants | Geographic region: United Kingdom Study setting: community N = 80 Baseline IPSS: NA Baseline prostate volume: NA Mean: 66.6 Age range: 55 to 80 Race: White Diagnostic criteria: Men with symptomatic BPH with symptoms scored by an investigator and symptoms scored with a self-assessment questionnaire |
|
| Interventions | Control: matching placebo Treatment: Permixon® 160 mg twice daily Study duration: 12 weeks Lost to follow up: 12.5% |
|
| Outcomes | Mean urine flow Bladder residual volume Investigator assessment (symptom score 0 to 2) Patient self-assessment data Libido Dropouts due to side effects: 2 patients from the treatment group (nausea and vomiting) |
|
| Notes | Exclusions: Malignant disease or “whose symptoms not fulfilling entry criteria” | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: random allocation using tables of random numbers Patients not blinded; providers not blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 30 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 62.9 Age range: 55 to 76 Race: White |
|
| Interventions | Control: Serenoa repens 640 mg rectal capsule once daily Treatment: Serenoa repens 160 mg oral capsules 4 times daily Study duration: 4 weeks Lost to follow up: none |
|
| Outcomes | Dysuria Bladder residual volume Prostate size Pollachiuria Overall effect of treatment summary Dropouts due to side effects: none |
|
| Notes | Exclusions: Age < 50 and > 80; on current medication; prior treatment for BPH | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
No | C |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: envelope selection Patients blinded; providers blinded |
|
| Participants | Geographic region: Shangai, China Study setting: urology clinic and community hospital N = 94 Baseline IPSS: NA Baseline prostate volume:Prostataplex™ 47.7 cc, Placebo 48.4 cc Mean age: 65.0 Age range: 62 to 68 Race: Chinese Diagnostic criteria: newly diagnosed LUTS associated with BPH based on urological symptoms, including nocturia, incomplete emptying, urinary frequency, intermittence, weak stream, straining and urgency |
|
| Interventions | Control: matching placebo Treatment: Prostataplex™ 2 pills/daily Study duration: 3 months Lost to follow up: 2 |
|
| Outcomes | Maximum urinary flow rate | |
| Notes | ||
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B - Significant difference in baseline inter- group IPSS total score |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Multisite study Randomization: computer-generated randomization code Patients blinded; providers blinded |
|
| Participants | Geographic region: Germany Study setting: community N = 543 (516 therapy trial) Baseline IPSS: PRO 160/120 11.3, Control 11.8 Baseline prostate volume: PRO 160/120 42.7 cc, Finasteride 44.0 cc Mean age: NA Age range: 50 to 88 Race: White Diagnostic criteria: BPH, stage I–II (Alken) |
|
| Interventions | Control: finasteride 5 mg plus placebo (2 capsules per day in a double dummy design) Treatment: Combination phytotherapy: PRO 160/120 (Sabal extract 160 mg and Urtica extract 120 mg) 2 capsules daily Study duration: 12 weeks Lost to follow up: 5% (Data from 489 subjects were used in therapy effect analysis and data from 516 subjects used for side effects analysis) |
|
| Outcomes | Symptom improvement-IPSS symptom score Quality of life - American Urological Association Score Peak urine flow Bladder residual volume Prostate size (volume) Dropouts due to side effects: (no details given) |
|
| Notes | Exclusions: < 50 years of age; BPH III or > (Alken); PSA > 10 ng/mL; cancer; taking other prostate medications; infections; severe concomitant disease that warrants therapy | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | A - Adequate |
| Allocation concealment? | Yes | A - Adequate |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: noted but method not stated Patients blinded; providers blinded |
|
| Participants | Geographic region: Italy Study setting: community N = 30 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 61.5 Age range: 49 to 81 Race: White Diagnostic criteria: Stage I and Stage II prostatic adenomas |
|
| Interventions | Control: matching placebo Treatment: PA109 160 mg twice daily Study duration: 8 weeks Lost to follow up: 10% |
|
| Outcomes | Dysuria (% reporting) Peak urine flow Mean urine flow Total voided volume Pollachiuria-daytime (% reporting) Pollachiuria-nocturnal (% reporting) Urgency (% reporting) Dropouts due to side effects: 1 patient from the treatment group |
|
| Notes | Exclusions: Details not given | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B |
| Allocation concealment? | Unclear | B |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Adequate |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
| Methods | Single-site study Randomization: randomized using balanced-blocks, where each block was for 6 men. Randomization codes were concealed in sealed envelopes and opened only after last man had completed treatment Patients blinded; providers blinded |
|
| Participants | Geographic region: Sydney, Australia Study setting: community N = 100 Baseline IPSS: NA Baseline prostate volume: NA Mean age: 63.9 Age range: NA Race: NA Diagnoxtic criteria: at least 3 symptoms of prostatism: 1) increased frequency; 2) hesitancy; 3) nocturia; 3) hesitancy; 4) dribbling and poor stream |
|
| Interventions | Control: matching placebo (paraffin oil in identical capsules, twice daily) Treatment: Serenoa repens 160 mg of CO2 extract, twice daily Study duration: 12 weeks Lost to follow up: n = 7 |
|
| Outcomes | IPSS Peak urine flow IIEF Questionnaire |
|
| Notes | Exclusions: ≥ 80; no significant medical condition: insulin-dependent diabetes; severe cardiopulmonary disease; significant CNS disease; androgens in previous 4 weeks; 5ARI; α-blockers; herbals for urinary problems; hx of PC or adenomas; urethral, bladder, renal abnormalities; urogenital surgery; renal stones; strictures or scarring; acute urinary retention or allergy to study treatment. | |
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | B - Significant difference between arms in IPSS at baseline |
| Allocation concealment? | Unclear | B - Sequence allocation by blocking; unsure if this process was blinded |
| Blinding? All outcomes |
Yes | A - Adequate |
| Incomplete outcome data addressed? All outcomes |
Yes | A - Per protocol analysis |
| Free of selective reporting? | Yes | A - Adequate |
| Free of other bias? | Yes | A - Adequate |
Characteristics of excluded studies [ordered by study ID]
| Adriazola Semino 1992 | Serenoa repens versus active control (Prazosin). No indication of randomization. |
| Comar 1986 | Study duration unknown. |
| Di Silverio 1992 | Tissue study investigating the antiestrogenic effect of Serenoa repens versus placebo. |
| Gerber 1998 | Open-label study, no control group. |
| Grasso 1995 | Average treatment duration < than 1 month. |
| Pecoraro 2004 | No relevant outcomes. |
| Popa 2005 | Re-analysis of the included study Metzker H, et al. Wirksamkeit eines sabal-urtica-kombinationspraparates bei der behandlung der benignen prostatahyperplasie (BPH). Der Urologe B 1996;36(4):292–300. |
| Sivkov 2001 | Same as Lopatkin 2005 |
| Strauch 1994 | Enzyme study (inhibition of 5 alpha-reductase) comparing Serenoa repens versus finasteride in a 1 week, open, randomized, active-controlled study. |
| Vela-Navarrete 2003a | No clinical outcomes. |
| Vela-Navarrete 2003b | Dual publication. |
| Vela-Navarrete 2005 | No relevant outcomes comparing Permixon® to control. |
| Weisser 1997 | Enzyme study investigating the influence of Sabal serrulata (versus placebo) on epithelial and stromal enzyme activities of BPH tissue. |
DATA AND ANALYSES
Comparison 1.
Serenoa repens versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom Score (points) at endpoint | 1 | 205 | Mean Difference (IV, Random, 95% CI) | −1.41 [−2.52, −0.30] |
| 2 IPSS total score WMD (0 to 35 (35 most severe)) | 2 | 304 | Mean Difference (IV, Random, 95% CI) | −0.77 [−2.88, 1.34] |
| 3 Nocturia (times/evening) at endpoint | 9 | 581 | Mean Difference (IV, Random, 95% CI) | −0.78 [−1.34, −0.22] |
| 4 Peak urine flow (mL/s) at endpoint | 10 | 1019 | Mean Difference (IV, Random, 95% CI) | 1.02 [−0.14, 2.19] |
| 5 Peak urine flow (mL/s) WMD | 2 | 304 | Mean Difference (IV, Random, 95% CI) | 0.31 [−0.56, 1.17] |
| 6 Patient self-rating for improved symptoms (# events ”very good” and “good”) | 5 | 619 | Risk Ratio (M-H, Random, 95% CI) | 1.54 [1.11, 2.14] |
| 7 Physician-assessed improvement of symptoms | 3 | 524 | Risk Ratio (M-H, Random, 95% CI) | 1.72 [1.11, 2.66] |
| 8 Prostate size (cc) at endpoint | 2 | 243 | Mean Difference (IV, Random, 95% CI) | −1.05 [−8.84, 6.75] |
| 9 Prostate size (cc) WMD | 1 | 225 | Mean Difference (IV, Random, 95% CI) | −1.22 [−3.91, 1.47] |
| 10 Study withdrawals | 9 | 920 | Risk Ratio (M-H, Random, 95% CI) | 0.86 [0.55, 1.36] |
| 11 Any adverse events | 5 | 618 | Risk Ratio (M-H, Random, 95% CI) | 1.07 [0.76, 1.51] |
Comparison 2.
Serenoa repens, B-sitosterol, and vitamin E versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 AUA total score WMD | 1 | 127 | Mean Difference (IV, Random, 95% CI) | −2.93 [−5.06, −0.80] |
| 2 AUA nocturia WMD | 1 | 127 | Mean Difference (IV, Random, 95% CI) | −0.7 [−1.07, −0.33] |
| 3 Peak urine flow (mL/s) at endpoint | 1 | 127 | Mean Difference (IV, Random, 95% CI) | −1.30 [−1.61, −0.99] |
| 4 Adverse events | 1 | Risk Ratio (M-H, Random, 95% CI) | Subtotals only | |
| 4.1 Dizziness | 1 | 127 | Risk Ratio (M-H, Random, 95% CI) | 0.27 [0.01, 6.56] |
| 4.2 Flatulence | 1 | 127 | Risk Ratio (M-H, Random, 95% CI) | 5.72 [0.30, 108.47] |
| 4.3 Headache | 1 | 127 | Risk Ratio (M-H, Random, 95% CI) | 0.81 [0.05, 12.73] |
| 4.4 Nausea/GI distress | 1 | 127 | Risk Ratio (M-H, Random, 95% CI) | 0.16 [0.01, 3.34] |
| 5 Study withdrawals | 1 | 144 | Odds Ratio (M-H, Random, 95% CI) | 0.34 [0.11, 1.02] |
Comparison 3.
Serenoa repens/Urtica dioica (PRO 160/120) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score at endpoint | 1 | 40 | Mean Difference (IV, Random, 95% CI) | −3.5 [−6.75, −0.25] |
| 2 IPSS total score WMD | 1 | 249 | Mean Difference (IV, Random, 95% CI) | −1.0 [−2.13, 0.13] |
| 3 Peak urine flow (mL/s) at endpoint | 2 | 69 | Mean Difference (IV, Random, 95% CI) | 2.48 [−0.05, 5.02] |
| 4 Peak urine flow (mL/s) WMD | 1 | 253 | Mean Difference (IV, Random, 95% CI) | −0.10 [−1.22, 1.02] |
| 5 Study withdrawals | 1 | 257 | Risk Ratio (M-H, Random, 95% CI) | 0.99 [0.14, 6.94] |
| 6 Patient self-rating for improved symptoms (# events ”very good” and “good”) | 1 | 40 | Risk Ratio (M-H, Random, 95% CI) | 8.00 [2.11, 30.34] |
Comparison 4.
Serenoa repens (Permixon®) versus finasteride
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score at endpoint | 1 | 951 | Mean Difference (IV, Random, 95% CI) | 0.40 [−0.57, 1.37] |
| 2 Nocturia (times/evening) | 1 | 1097 | Mean Difference (IV, Random, 95% CI) | −0.05 [−0.49, 0.39] |
| 3 Peak urine flow (mL/s) WMD | 1 | 951 | Mean Difference (IV, Random, 95% CI) | −0.5 [−1.91, 0.91] |
| 4 Prostate size (cc) at endpoint | 1 | 951 | Mean Difference (IV, Random, 95% CI) | 4.80 [1.42, 8.18] |
| 5 Study withdrawals | 1 | 1098 | Risk Ratio (M-H, Random, 95% CI) | 1.39 [1.02, 1.89] |
Comparison 5.
Serenoa repens/Urtica dioica (PRO 160/120) versus finasteride
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score at endpoint | 1 | 453 | Mean Difference (IV, Random, 95% CI) | 0.30 [−1.28, 1.88] |
| 2 Peak urine flow (mL/s) WMD | 1 | 465 | Mean Difference (IV, Random, 95% CI) | −0.80 [−1.98, 0.38] |
| 3 Study withdrawals | 1 | 513 | Risk Ratio (M-H, Random, 95% CI) | 1.17 [0.53, 2.56] |
Comparison 6.
Serenoa repens versus Pygeum africanum
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Patient self-rating for improved symptoms (# events ”very good” and “good”) | 1 | 39 | Risk Ratio (M-H, Random, 95% CI) | 1.43 [0.98, 2.07] |
| 2 Nocturia (times/evening) at endpoint | 1 | 40 | Mean Difference (IV, Random, 95% CI) | −0.20 [−1.69, 1.29] |
Comparison 7.
Serenoa repens versus gestonorone caproate
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peak urine flow (mL/s) at endpoint | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 2.0 [1.49, 2.51] |
Comparison 8.
Serenoa repens versus tamsulosin
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score WMD | 2 | 582 | Mean Difference (IV, Random, 95% CI) | −0.52 [−1.91, 0.88] |
| 2 Peak urine flow (mL/s) WMD | 2 | 645 | Mean Difference (IV, Random, 95% CI) | 0.14 [−0.54, 0.83] |
| 3 Nocturia (% improvement) | 1 | 542 | Risk Ratio (M-H, Random, 95% CI) | 0.91 [0.66, 1.27] |
| 4 Incomplete emptying (%improvement) | 1 | 542 | Risk Ratio (M-H, Random, 95% CI) | 1.25 [0.97, 1.61] |
| 5 Prostate size (cc) WMD | 2 | 579 | Mean Difference (IV, Random, 95% CI) | −0.15 [−1.44, 1.13] |
| 6 Study withdrawals | 2 | 744 | Risk Ratio (M-H, Random, 95% CI) | 0.98 [0.69, 1.37] |
| 7 Any adverse effects | 2 | 743 | Risk Ratio (M-H, Random, 95% CI) | 0.34 [0.02, 5.43] |
Comparison 9.
Serenoa repens+Urtica dioica (PRO 160/120) versus tamsulosin
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pts w/any efficacy data in the full analysis set who responded to treatment (defined as IPSS ≤ 7 at endpoint) | 1 | 136 | Risk Ratio (M-H, Random, 95% CI) | 1.16 [0.69, 1.94] |
| 2 Adverse events | 1 | 140 | Risk Ratio (M-H, Random, 95% CI) | 0.77 [0.43, 1.38] |
| 3 Study withdrawals | 1 | 140 | Risk Ratio (M-H, Random, 95% CI) | 1.34 [0.57, 3.12] |
Comparison 10.
Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score WMD | 2 | 356 | Mean Difference (IV, Random, 95% CI) | −0.61 [−1.69, 0.47] |
| 2 Peak urine flow (mL/s) WMD | 2 | 357 | Mean Difference (IV, Random, 95% CI) | 0.09 [−0.80, 0.98] |
| 3 Prostate size (cc) WMD | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.20 [−1.10, 1.50] |
| 4 Study withdrawals | 2 | 369 | Risk Ratio (M-H, Random, 95% CI) | 0.90 [0.58, 1.40] |
| 5 Any adverse events | 1 | 40 | Risk Ratio (M-H, Random, 95% CI) | 2.13 [1.20, 3.75] |
Comparison 11.
Serenoa repens (Permixon®) versus Serenoa repens+tamsulosin
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 IPSS total score WMD | 1 | 40 | Mean Difference (IV, Random, 95% CI) | −1.20 [−2.75, 0.35] |
| 2 Peak urine flow (mL/s) WMD | 1 | 40 | Mean Difference (IV, Random, 95% CI) | −1.0 [−2.46, 0.46] |
| 3 Prostate size (cc) WMD | 1 | 40 | Mean Difference (IV, Random, 95% CI) | 0.10 [−1.34, 1.54] |
| 4 Any adverse events | 1 | 40 | Risk Ratio (M-H, Random, 95% CI) | 0.03 [0.00, 0.44] |
Comparison 12.
™ versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Peak urine flow (mL/s) at endpoint | 1 | 92 | Mean Difference (IV, Random, 95% CI) | 2.33 [1.51, 3.15] |
| 2 Prostate size (cc) at endpoint | 1 | 92 | Mean Difference (IV, Random, 95% CI) | −0.28 [−10.38, 9.82] |
| 3 Study withdrawals | 1 | 94 | Risk Ratio (M-H, Random, 95% CI) | 0.21 [0.01, 4.23] |
Analysis 1.1.
Comparison 1 Serenoa repens versus placebo, Outcome 1 Symptom Score (points) at endpoint.
Analysis 1.2.
Comparison 1 Serenoa repens versus placebo, Outcome 2 IPSS total score WMD (0 to 35 (35 most severe)).
Analysis 1.3.
Comparison 1 Serenoa repens versus placebo, Outcome 3 Nocturia (times/evening) at endpoint.
Analysis 1.4.
Comparison 1 Serenoa repens versus placebo, Outcome 4 Peak urine flow (mL/s) at endpoint.
Analysis 1.5.
Comparison 1 Serenoa repens versus placebo, Outcome 5 Peak urine flow (mL/s) WMD.
Analysis 1.6.
Comparison 1 Serenoa repens versus placebo, Outcome 6 Patient self-rating for improved symptoms (# events “very good” and “good”).
Analysis 1.7.
Comparison 1 Serenoa repens versus placebo, Outcome 7 Physician-assessed improvement of symptoms.
Analysis 1.8.
Comparison 1 Serenoa repens versus placebo, Outcome 8 Prostate size (cc) at endpoint.
Analysis 1.9.
Comparison 1 Serenoa repens versus placebo, Outcome 9 Prostate size (cc) WMD.
Analysis 1.10.
Comparison 1 Serenoa repens versus placebo, Outcome 10 Study withdrawals.
Analysis 1.11.
Comparison 1 Serenoa repens versus placebo, Outcome 11 Any adverse events.
Analysis 2.1.
Comparison 2 Combination Cernitin®, Serenoa repens, B-sitosterol, and vitamin E versus placebo, Outcome 1 AUA total score WMD.
Analysis 2.2.
Comparison 2 Combination Cernitin®, Serenoa repens, B-sitosterol, and vitamin E versus placebo, Outcome 2 AUA nocturia WMD.
Analysis 2.3.
Comparison 2 Combination Cernitin®, Serenoa repens, B-sitosterol, and vitamin E versus placebo, Outcome 3 Peak urine flow (mL/s) at endpoint.
Analysis 2.4.
Comparison 2 Combination Cernitin®, Serenoa repens, B-sitosterol, and vitamin E versus placebo, Outcome 4 Adverse events.
Analysis 2.5.
Comparison 2 Combination Cernitin®, Serenoa repens, B-sitosterol, and vitamin E versus placebo, Outcome 5 Study withdrawals.
Analysis 3.1.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 1 IPSS total score at endpoint.
Analysis 3.2.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 2 IPSS total score WMD.
Analysis 3.3.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 3 Peak urine flow (mL/s) at endpoint.
Analysis 3.4.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 4 Peak urine flow (mL/s) WMD.
Analysis 3.5.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 5 Study withdrawals.
Analysis 3.6.
Comparison 3 Serenoa repens/Urtica dioica (PRO 160/120) versus placebo, Outcome 6 Patient self-rating for improved symptoms (# events “very good” and “good”).
Analysis 4.1.
Comparison 4 Serenoa repens (Permixon®) versus finasteride, Outcome 1 IPSS total score at endpoint.
Analysis 4.2.
Comparison 4 Serenoa repens (Permixon®) versus finasteride, Outcome 2 Nocturia (times/evening).
Analysis 4.3.
Comparison 4 Serenoa repens (Permixon®) versus finasteride, Outcome 3 Peak urine flow (mL/s) WMD.
Analysis 4.4.
Comparison 4 Serenoa repens (Permixon®) versus finasteride, Outcome 4 Prostate size (cc) at endpoint.
Analysis 4.5.
Comparison 4 Serenoa repens (Permixon®) versus finasteride, Outcome 5 Study withdrawals.
Analysis 5.1.
Comparison 5 Serenoa repens/Urtica dioica (PRO 160/120) versus finasteride, Outcome 1 IPSS total score at endpoint.
Analysis 5.2.
Comparison 5 Serenoa repens/Urtica dioica (PRO 160/120) versus finasteride, Outcome 2 Peak urine flow (mL/s) WMD.
Analysis 5.3.
Comparison 5 Serenoa repens/Urtica dioica (PRO 160/120) versus finasteride, Outcome 3 Study withdrawals.
Analysis 6.1.
Comparison 6 Serenoa repens versus Pygeum africanum, Outcome 1 Patient self-rating for improved symptoms (# events “very good” and “good”).
Analysis 6.2.
Comparison 6 Serenoa repens versus Pygeum africanum, Outcome 2 Nocturia (times/evening) at endpoint.
Analysis 7.1.
Comparison 7 Serenoa repens versus gestonorone caproate, Outcome 1 Peak urine flow (mL/s) at endpoint.
Analysis 8.1.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 1 IPSS total score WMD.
Analysis 8.2.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 2 Peak urine flow (mL/s) WMD.
Analysis 8.3.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 3 Nocturia (% improvement).
Analysis 8.4.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 4 Incomplete emptying (% improvement).
Analysis 8.5.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 5 Prostate size (cc) WMD.
Analysis 8.6.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 6 Study withdrawals.
Analysis 8.7.
Comparison 8 Serenoa repens versus tamsulosin, Outcome 7 Any adverse effects.
Analysis 9.1.
Comparison 9 Serenoa repens+Urtica dioica (PRO 160/120) versus tamsulosin, Outcome 1 Pts w/any efficacy data in the full analysis set who responded to treatment (defined as IPSS ≤ 7 at endpoint).
Analysis 9.2.
Comparison 9 Serenoa repens+Urtica dioica (PRO 160/120) versus tamsulosin, Outcome 2 Adverse events.
Analysis 9.3.
Comparison 9 Serenoa repens+Urtica dioica (PRO 160/120) versus tamsulosin, Outcome 3 Study withdrawals.
Analysis 10.1.
Comparison 10 Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin, Outcome 1 IPSS total score WMD.
Analysis 10.2.
Comparison 10 Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin, Outcome 2 Peak urine flow (mL/s) WMD.
Analysis 10.3.
Comparison 10 Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin, Outcome 3 Prostate size (cc) WMD.
Analysis 10.4.
Comparison 10 Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin, Outcome 4 Study withdrawals.
Analysis 10.5.
Comparison 10 Serenoa repens (Permixon®)+tamsulosin versus placebo+tamsulosin, Outcome 5 Any adverse events.
Analysis 11.1.
Comparison 11 Serenoa repens (Permixon®) versus Serenoa repens+tamsulosin, Outcome 1 IPSS total score WMD.
Analysis 11.2.
Comparison 11 Serenoa repens (Permixon®) versus Serenoa repens+tamsulosin, Outcome 2 Peak urine flow (mL/s) WMD.
Analysis 11.3.
Comparison 11 Serenoa repens (Permixon®) versus Serenoa repens+tamsulosin, Outcome 3 Prostate size (cc) WMD.
Analysis 11.4.
Comparison 11 Serenoa repens (Permixon®) versus Serenoa repens+tamsulosin, Outcome 4 Any adverse events.
Analysis 12.1.
Comparison 12 Prostataplex™ versus placebo, Outcome 1 Peak urine flow (mL/s) at endpoint.
Analysis 12.2.
Comparison 12 Prostataplex™ versus placebo, Outcome 2 Prostate size (cc) at endpoint.
Analysis 12.3.
Comparison 12 Prostataplex™ versus placebo, Outcome 3 Study withdrawals.
FEEDBACK
Anna Rita Bilia, et al, 31 August 2009
Summary
Feedback: Quality of a herbal medicinal product is essential. Both the safety profile and the efficacy of a multi-component herbal medicinal product are irrevocably linked to quality. Quality should be assessed according to the monographs reported in the European Pharmacopoeia or in other Pharmacopoeias or pharmaceutical reference books [1, 2]. These record the methods to define the quality of multi-component herbal drugs and also of defined selected extracts, according to classification of active constituents, pharmacologically active markers and quality markers [3,4]. Additionally, pharmacopoeial methods are fully validated to perform correctly under the given analytical proceedings irrespectively of the environment where they are performed [ICH guideline Q2(R1); www.ich.org].
Quality of a defined multi-component herbal extract is strictly related to the quality of the botanical source (herbal drug) defined by the botanical name of the plant according to the binomial system (genus, species, variety and author) and the part used (e.g. leaf, root or fruit). In addition other factors should be considered such as the method of preparation (extraction process, solvents used; solubility and stability of the plant constituents), the drug extract ratio (DER), time and temperature operations, which could be crucial not only for safety but also for the efficacy of the product [5–8]. Ideally, in analogy with the analytical procedures for testing, also the production-process should be fully validated, in order to guarantee consistency of the final product, as far as possible.
For these reasons the final mix of constituents in a multi-component extract may exert different activities and in some circumstances, may even have a different safety profile from another type of extract, that is derived from the identical herb. These facts are taken into consideration and documented for well-defined herbal extracts in a new series of published European Community Monographs, authorised by the EMEA [9]. It is noteworthy that, among the various types of plant products, e.g. food and botanical products, on the world market, only Herbal Medicinal Products are produced under rigid quality systems, such as Good Sourcing Practices (GSP), Good Agricultural Practices (GAP), Good Field Collection Practices (GFCP), Good Processing Practices (GPP), as well as Good Manufacturing Practices (GMP). As a consequence the quality can be assessed and the final product can be considered reproducible. According to the above arguments, it is crucial to realise, that the identical botanical source cannot guarantee the bioequivalence of its various multi-component extracts and of the resulting different Herbal Medicinal Products. The situation in the Cochrane review on Serenoa repens [10] leaves no doubt, that various different Serenoa extracts (not always defined) and their subsequently varying final medicinal products, have been summarised, then analysed, in order to obtain the final conclusions of the review. This left the reader to assume, that both comparable (bioequivalent) and non-comparable products were included and compared in this study, in spite of the fact, that they might have exerted different, e.g. non-comparable safety and/or efficacy profiles.
Considering statements and definitions mentioned above, the Cochrane Review on Serenoa repens [10] has been evaluated by the contributors to the present ’Letter to the editor.’ Four in part-related problems were encountered. In the following four comments, these problems have been addressed.
Comment 1. Problem, missing conclusion regarding studies with a positive control Serenoa alone, was compared in 4 of the 30 investigated clinical trials with known BPH drugs, such as Finasteride, Tamsulosin and Gestonorone caproate as positive controls. Reported in the review were a few minor differences and many comparable results for the various evaluated symptoms and no difference for the overall urinary symptom scores, between treatments with either Serenoa extract or these BPH drugs in different studies with up to 1098 patients. This apparently demonstrated, that the efficacy of these drugs was not different from that of the Serenoa products. Selected results are shown here, to exemplify the commentary: 1 study compared Serenoa to Finasterid (MD, mean difference, −0,40 Points, 95% CI −0.57 to 1.37, p > 0.05); 2 studies compared Serenoa to Tamsulosin (WMD, weighted mean difference, −0.52 Punkte, 95% CI −1.91 to 0.88, p > 0.05).
The reader of the review, even without being in the position to repeat the full statistical analysis, could conclude, that efficacy of Serenoa should be similar or comparable to these BPH drugs. The final statement of the authors, that ?Sereoa is not different from placebo?, is in clear contradiction to these reports. This contradiction has not been addressed, nor discussed, by the authors of the review.
Conclusion to comment 1
Contradictions described here, unless resolved, prohibit a final conclusion about the efficacy of Serenoa repens products.
Comment 2. Problem, chemical complexity of a multi-component plant-extract; ?non-equivalence? of analysed products The authors of the review appear to have treated the various Serenoa fruit preparations, derived from different extracts, used in the 30 clinical trials, which they analysed, as if these extracts were identical single chemical entities. i.e. the authors appear not to have considered in their analysis, that components of different multi-component preparations vary, according to their extraction procedure, the solvent used, the drug-extract-ratio, the total constituents probably vary, the co-active constituents probably vary and the standardization can vary. Thus the doses can vary.
The authors have stated in the review, that “of the 15 trials (in true only 14 appeared to have been actually analysed in the review), that were placebo-controlled and compared to Serenoa repens monotherapy, 7 utilized the commercialized Permixon, which assured that our comparators were equivalent” [page 13]. Thus the reader may conclude, that 7 out of 14 placebo-controlled trials were included in this analysis, that were ’non-equivalent’ (i.e. 50% of the comparators). This causes concern about the validity of the authors’ statement as well as the authors’ conclusions.
Comment 3. Problem, variation of dose
The dosage relates directly to the composition of a multi-component extract (see comment 2 as well). Thus, the dosage between studies can vary, even if identical amounts are given. Naturally, the dosage must also vary, if the administered amount differs. The ’daily dose’ of an extract administered, varied from study to study, in the 30 studies analysed: from 20 drops, 100 mg, 160 mg, 212 mg, 286 mg, 320 mg (a number of studies), 480 mg up to 640 mg, mostly applied in two portions. There was no statistical evaluation in the review, taking these different dosages, that were used in the 30 clinical trials, into account.
The BPH treatments using non-identical Serenoa preparations at strongly varying dosages, were summarized and investigated in the review, as if identical treatments with defined dosages, had been used. This is, as if one would assume, that apples, pears and even lemons will taste the same, merely because they are round.
Conclusion to comments 2 and 3
The statistical comparative analysis by the authors of the review, focuses on clinical symptom-scores of BPH in 30 trials, but they have omitted to fully address the consequences of analysing heterogenous Serenoa preparations administered in heterogenous dosage schemes, in those trials. For example the 7 ’non-equivalent’ placebo-controlled trials should not have been considered as a valid part of a comparative clinical analysis of the placebo-controlled studies.
Comment 4. Problem, studies conducted with Serenoa-containing combination products.
Nine (9) of 30 analysed studies, were conducted with combination products containing Serenoa repens extracts, besides one or more other potentially active phytotherapeutic agent (there was no consideration of the dosage, the various extracts were not defined, in the Cochrane review).
Conclusion to comment 4
These studies do not give evidence concerning the efficacy of Serenoa. Any efficacy or lack of efficacy cannot be attributed to Serenoa, such as would be the case in mono-therapy, but could be influenced by the other plant components in each product. The reader may conclude, that these studies do not qualify for a comparative analysis and cannot support a conclusive statement concerning the activity of Serenoa repens.
Summarising conclusions from comments 1–4
Of 30 analysed studies, 7 placebo-controlled studies with “non-comparable” Serenoa products and 9 studies with combination products, could be deleted for good reasons, possibly leaving 14 studies for a revision of the comparative analysis.
The authors final conclusion in this review “Sereoa is not different from placebo,” does not appear to have been corroborated by rigorous scientific reasoning. Even without repeating the full statistical evaluation (which appears to be necessary as well), the authors final conclusion regarding the efficacy of Serenoa repens, needs to be reconsidered.
Submitter agrees with default conflict of interest statement:
I certify that I have no affiliations with or involvement in any organization or entity with a financial interest in the subject matter of my feedback.
- 1.Saw Palmetto Fruit. Sabalis serrulatae fructus. European Pharmacopoeia. Council of Europe.
- 2.Saw palmetto. USP, United States Pharmacopeia.
- 3.Guideline on declaration of herbal substances and herbal preparations in herbal medicinal products/traditional herbal medicinal products in the SPC (Summary of product characteristics). EMEA adopted guideline. London, 26 July 2007 Doc. Ref: EMEA/HMPC/CHMP/CVMP/287539/2005
- 4.Reflection papers on markers used for quantitative and qualitative analyses of herbal medicinal products and traditional herbal medicinal products. EMEA adopted guideline. London, 15 July 2008. Doc. Ref. EMEA/HMPC/253629/2007
- 5.Gaedcke F, Steinhoff B. Herbal medicinal products. Scientific and regulatory basis for development, quality assurance and marketing authorisation. CRC Press; Boca Raton: 2003. [Google Scholar]
- 6.Guideline on specifications: test procedures and acceptance criteria for herbal substances, herbal preparations and herbal medicinal products/traditional herbal medicinal products. EMEA adopted guideline. London 30 March 2006. CPMP/QWP/2819/00 Rev 1. EMEA/CVMP/814/00 Rev 1
- 7.Guideline on quality of herbal medicinal products/traditional herbal medicinal products. London, 30 March 2006. EMEA adopted guideline. CPMP/QWP/2819/00 Rev 1. EMEA/CVMP/814/00 Rev 1.
- 8.Vlietinck A, Pieters L, Apers S. Legal requirements for the quality of herbal substances and herbal preparations for the manufacturing of herbal medicinal products in the European Union. Planta Med. 2009;75:683–8. doi: 10.1055/s-0029-1185307. [DOI] [PubMed] [Google Scholar]
- 9.a) about European Community Monographs http://www.emea.europa.eu/htms/human/hmpc/hmpcmonographs.htm; b) homepage of HMPC (Herbal Medicinal Product Committee of EMEA) http://www.emea.europa.eu/htms/human/hmpc/index.htm; c) about HMPC documents (Herbal Medicinal Product Committee of EMEA) http://www.emea.europa.eu/htms/human/hmpwp/working.htm.
- 10.Tacklind J, MacDonald R, Rutks I, Wilts TJ. The Cochrane Collaboration, The Cochrane Library. 2. Publishers John Wiley & Sons, Ltd; 2009. Serenoa repens for benign prostatic hyperplasia (Review) pp. 1–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reply
Thank you for your comments.
The reviewer remarks that we are acting non-scientifically by lumping, for example, Permixon and generic Serenoa repens, is mistaken. Others have made claims that Serenoa repens (whether generic or as Permixon) alleviates symptoms associated with BPH. We have merely tested their hypothesis.
The reviewer makes two excellent points on bioequivalency and dosages, and in a forthcoming update we will address both. However, we disagree with the reviewers’ suggestion that we should have utilized only the Permixon trials. We conducted a systematic review of the evidence related to these products.
The Permixon trials, which the reviewer urges us to use exclusively, are of almost uniformly poor quality. For example, the 7 RCTs that compared Permixon to placebo had study populations of 22, 30, 60, 80, 110, 168, and 215. These trials were egregiously underpowered, with the possible exception of the last two. Follow up for the 7 Permixon-versus-placebo trials, measured in weeks, was 4, 4, 4, 4, 8.5, 10 and 12. Only one of the six Permixon trials that were compared to an active control (or combination therapy with either Permixon or the active control) utilized a placebo arm.
The reviewer states: “The reader of the review, even without being in the position to repeat the full statistical analysis, could conclude that efficacy of Serenoa should be similar or comparable to these BPH drugs. The final statement of the authors that ‘Serenoa is not different from placebo,’ is in clear contradiction to these reports.” We are not contradictory, but the evidence is ambiguous, as we put it in the review. For example, Carraro [1] (Permixon versus finasteride) reported a decrease in IPSS symptom scores for both arms (−37% versus −39%, respectively); unfortunately, he did not include a placebo arm. Carraro’s trial was certainly well powered (N = 1098), but follow up was only 26 weeks.
The consequence of the reviewers’ recommendation to use only the Permixon trials would eliminate the highest quality trial of the thirty, and Bent’s NEJM trial [2] (Serenoa repens versus placebo) is methodologically superior to all of the other twenty-nine. Bent writes “these studies [previous RCTs] are limited by the small numbers of subjects enrolled, their short duration, their failure to use standard outcome measures, and the lack of information from participants concerning how effectively the placebo was blinded.” After 12-month follow up Bent reported “[b]oth groups also had a small decrease in the AUASI score …: the score decreased by 0.68 in the saw palmetto group (95 percent confidence interval, −1.37 to 0.01) and by 0.72 in the placebo group (95 percent confidence interval, −1.40 to −0.04) (Table 2). There was, however, no significant difference between groups in the mean change in AUASI scores over time (difference in mean change, 0.04 point; 95 percent confidence interval, −0.93 to 1.01).”
Can these results be extrapolated to European populations using Permixon? We think so. Nevertheless, we welcome an equivalent European trial utilizing Permixon when it becomes available.
References
- 1.Carraro J-C, Raynaud J-P, Koch G, Chisholm GD, Di Silverio F, Teillac P, Da Silva FC, Cauquil J, Chopin DK, Hamdy FC, et al. Comparison of phytotherapy (Permixon) with finasteride in the treatment of benign prostate hyperplasia: a randomized international study of 1,098 patients. The Prostate. 1996;29:231–40. doi: 10.1002/(SICI)1097-0045(199610)29:4<231::AID-PROS4>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 2.Bent S, Kane C, Shinohara K, Neuhaus J, Hudes ES, Goldberg H, Avins AL. Saw palmetto for benign prostatic hyperplasia. The New England Journal of Medicine. 2006;354(6):557–66. doi: 10.1056/NEJMoa053085. [DOI] [PubMed] [Google Scholar]
Contributors
The consumers
Corresponding author: Prof. Dr. Anna Rita Bilia, Phytolab, University of Florence, Department of Pharmaceutical Sciences, via Ugo Schiff 6, I-50019 Sesto Fiorentino (Florence), Italy. E-mail: ar.bilia@unifi.it.
Co-contributors names and addresses:
S. F.A.J. Horsten, PhD., Steenmarteakker 1, NL-3994 GE Houten;
S. Sturm, PhD., University of Innsbruck, Inst. of Pharmacy/Pharmacognosy, A-6020 Innsbruck;
M. Frater-Schröder, PhD., Schwand, CH-9642 Ebnat-Kappel.
The authors
James Tacklind
Rod MacDonald
Indy Rutks
Tim Wilt
WHAT ’S NEW
Last assessed as up-to-date: 20 December 2007.
| 4 March 2010 | Amended | Under ’Feedback/1 Anna Rita Bilia, et al, 31 August 2009/Summary/Reply’, a clause read: “and by 0.72 in the placebo group (95 percent confidence interval, −1.40 to ?0.04) (Table 2).” It has been changed to “and by 0.72 in the placebo group (95 percent confidence interval, −1.40 to −0.04) (Table 2).” |
HISTORY
Protocol first published: Issue 1, 1998
Review first published: Issue 1, 1999
| 29 September 2008 | New citation required and conclusions have changed | We have modified our findings of the efficacy of Serenoa repens. |
| 10 July 2008 | New search has been performed | This is a substantial update with 9 new trials. |
| 25 March 2008 | Amended | Converted to new review format. |
| 21 December 2007 | New citation required and conclusions have changed | Substantive amendment |
Footnotes
CONTRIBUTIONS OF AUTHORS
JT searched for trials and wrote the analysis. RMD and TJW edited the manuscript. IR ran search strategy.
DECLARATIONS OF INTEREST
None.
REFERENCES
*Indicates the major publication for the study
References to studies included in this review
- Bauer 1999{published data only}.Bauer HW, Casarosa C, Cosci M, Fratta M, Blessmann G. Saw palmetto fruit extract for treatment of benign prostatic hyperplasia. Results of a placebo-controlled double-blind study [German] [Sabalfrucht–Extrakt zur Behandlung der benignen Prostatahyperplasie. Ergebnisse einer plazebokontrollierten Doppelblindstudie] MMW Fortschritte der Medizin. 1999;141(25):127–32. [PubMed] [Google Scholar]
- Bent 2006{published data only}.Bent S, Kane C, Shinohara K, Neuhaus J, Hudes E, Goldberg H, Avins AL. Saw palmetto for benign prostatic hyperplasia. The New England Journal of Medicine. 2006;354(6):557–66. doi: 10.1056/NEJMoa053085. [DOI] [PubMed] [Google Scholar]
- Boccafoschi 1983{published data only}.Boccafoschi C, Annoscia S. [Confronto fra estratto di serenoa repens e placebo mediate prova clinica controllata in pazienti con adenomatosi prostatica] Urologia. 1983;50:1257–68. [Google Scholar]
- Braeckman 1997{published and unpublished data}.Braeckman J. A double-blind, placebo-controlled study of the plant extract Serenoa repens in the treatment of benign hyperplasia of the prostate. European Journal of Clinical Research. 1997;9:247–59. [Google Scholar]
- Carbin 1990{published data only}.Carbin BE, Larsson B, Lindahl O. Treatment of benign prostatic hyperplasia with phytosterols. British Journal of Urology. 1990;66(6):639–41. doi: 10.1111/j.1464-410x.1990.tb07199.x. [MEDLINE: 1991091633] [DOI] [PubMed] [Google Scholar]
- Carraro 1996{published data only}.Carraro JC, Raynaud JP, Koch G, Chisholm GD, Di Silverio F, Teillac P, Da Silva FC, Cauqil J, Chopin DK, Hamdy FC, Hanus M, Hauri D, Kalinteris A, Marencak J, Perier A, Perrin P. Comparison of phytotherapy (Permixon) with finasteride in the treatment of benign prostate hyperplasia: a randomized international study of 1,098 patients. The Prostate. 1996;29(4):231–40. doi: 10.1002/(SICI)1097-0045(199610)29:4<231::AID-PROS4>3.0.CO;2-E. [MEDLINE: 1997030765] [DOI] [PubMed] [Google Scholar]
- Champault 1984{published data only}.Champault G, Patel JC, Bonnard AM. A double-blind trial of an extract of the plant Serenoa repens in benign prostatic hyperplasia. British Journal of Clinical Pharmacology. 1984;18:461–2. doi: 10.1111/j.1365-2125.1984.tb02491.x. [MEDLINE: 1985023088] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cukier 1985{published data only}.Cukier J, Ducassou J, Le Guillou M, Leriche A, Lobel B, Toubol J. [Permixon versus placebo; resultats d’une étude multicentrique] Comptes Rendus de Therapeutique et de Pharmacologie Clinique. 1985;4:15–21. [Google Scholar]
- *Debruyne 2002{published data only}.Debruyne F, Koch G, Da Silva FC, Gillenwater JG, Hamdy FC, Perrin P, Teillac P, Vela-Navarrete R, Raynaud JP, Groupe d’etude PERMAL. Comparison of a phytotherapeutic agent (Permixon) with an a-blocker (tamsulosin) in the treatment of benign prostatic hyperplasia: a 1-year randomized international study [Comparaison d’un produit de phytotherapie (permixon) et d’un alphabloquant (tamsulosine) dans le traitement de l’hypertrophie benigne de la prostate: etude internationale randomisee d’une durée de 12 mois] Progrès en Urologie. 2002;41:497–507. [PubMed] [Google Scholar]
- Descotes 1995{published data only}.Descotes JL, Rambeaud JJ, Deschaseaux P, Faure G. Placebo-controlled evaluation of the efficacy and tolerability of Permixon in benign prostatic hyperplasia after the exclusion of placebo responders. Clinical Drug Investigation. 1995;5:291–7. [Google Scholar]
- Emili 1983{published data only}.Emili E, Lo Cigno M, Petrone U. [Risultati clinici su un nuovo farmaco nella terapia dell’ipertofia della prostata (Permixon)] Urologia. 1983;50:1042–8. [Google Scholar]
- Engelmann 2006{published data only}.Engelmann U, Walther C, Bondarenko B, Funk P, Schläfke S. Efficacy and safety of a combination of sabal and urtica extract in lower urniary tract symptoms. A randomized, double-blind study versus tamsulosin. Arzneimittel-Forschung. 2006;56(3):222–9. doi: 10.1055/s-0031-1296714. [DOI] [PubMed] [Google Scholar]
- Gabric 1987{published data only}.Gabric V, Miskic H. [Behandlung des benignen prostata–adenoms und der chronischen prostatatitis] Therapiewoche. 1987;37:1775–88. [Google Scholar]
- Gerber 2001{published data only}.Gerber GS, Kuznetsov D, Johnson BC, Burstein JD. Randomized, double-blind, placebo-controlled trial of saw palmetto in men with lower urinary tract symptoms. Urology. 2001;58(6):960–4. doi: 10.1016/s0090-4295(01)01442-x. [DOI] [PubMed] [Google Scholar]
- Glémain 2002{published data only}.Glémain P, Coulange C, Billebaud T, Gattegno B, Muszynski R, Loeb G the OCOS workgroup. Tamsulosin with or without Serenoa repens in benign prostatic hyperplasia: the OCOS trial [Tamsulosine avec ou sans Serenoa repens dans l’hypertrophie bénigne de la prostate: l’essai OCOS] Progrès en Urologie. 2002;12:395–403. [PubMed] [Google Scholar]
- Hizli 2007{published data only}.Hizli F, Uygur MC. A prospective study of the efficacy of Serenoa repens, tamsulosin, and Serenoa repens plus tamsulosin treatment for patients with benign prostate hyperplasia. International Urology and Nephrology. 2007;39:879–86. doi: 10.1007/s11255-006-9106-5. [DOI] [PubMed] [Google Scholar]
- Lopatkin 2005{published data only}.Lopatkin N, Sivkov A, Walther C, Schläfke S, Medvedev A, Avdeichuk J, Golubev G, Melnik K, Elenberger N, Engelmann U. [Combined extract of sabal palm and nettle in the treatment of patients with lower urinary tract symptoms in the double blind, placebo–controlled trial] World Journal of Urology. 2005;23(2):139–46. doi: 10.1007/s00345-005-0501-9. [DOI] [PubMed] [Google Scholar]
- Löbelenz 1992{published data only}.Löbelenz J. [Extractum Sabal fructus bei benigner prostatahyperplasie (BPH). klinische prufung im stadium I und II] Therapeutikon. 1992;6(1–2):34–7. [Google Scholar]
- Mandressi 1983{published data only}.Mandressi S, Tarallo U, Maggioni A, Tombolini P, Rocco F, Quadraccia Medical treatment of benign prostatic hyperplasia: efficacy of the extract of Serenoa repens (Permixon) compared to that of the extract of Pygeum africanum and a placebo. Urologia. 1983;50(4):752–8. [Google Scholar]
- Marks 2000{published data only}.Marks LS, Partin AW, Epstein JI, Tyler VE, Simon I, Macairan ML, Chan TL, Dorey FJ, Garris JB, Veltri RW, Santos PB, Stonebrook KA, de Kernion JB. Effects of a saw palmetto herbal blend in men with symptomatic benign prostatic hyperplasia. The Journal of Urology. 2000;163(5):1451–6. [PubMed] [Google Scholar]
- Mattei 1990{published data only}.Mattei FM, Capone M, Acconcia A. [Medikamentose therapie der benignen prostatahyperplasie mit einem extrakt der sagepalme] TW Urologie Nephrologie. 1990;2:346–50. [Google Scholar]
- Metzker 1996{published data only}.Metzker H, Kieser M, Holscher U. [Wirksamkeit eines Sabal–Urtica–kombinationspraparates bei der behandlung der benignen prostatahyperplasie (BPH)] Der Urologe B. 1996;36(4):292–300. [Google Scholar]
- Pannunzio 1986{published data only}.Pannunzio E, D’Ascenzo R, Giardinetti F, Civili P, Persichelli E. [Serenoa repens vs. gestonorone caproato nel trattamento dell’ipertofia prostatica benigna: Studio randomizzato] Urologia. 1986;53(5):696–705. [Google Scholar]
- Preuss 2001{published data only}.Preuss HG, Marcusen C, Regan J, Klimberg IW, Welebir TA, Jones WA. Randomized trial of a combination of natural products (Cernitin, saw palmetto, B-sitosterol, vitamin E) on symptoms of benign prostatic hyperplasia (BPH) International Urology and Nephrology. 2001;33:217–25. doi: 10.1023/a:1015227604041. [DOI] [PubMed] [Google Scholar]
- Reece Smith 1986{published data only}.Reece Smith H, Memon A, Smart CJ, Dewbury K. The value of Permixon in benign prostatic hypertrophy. British Journal of Urology. 1986;58:36–40. doi: 10.1111/j.1464-410x.1986.tb05424.x. [DOI] [PubMed] [Google Scholar]
- Roveda 1994{published data only}.Roveda S, Colombo P. [Sperimentazione clinica controllata sulla bioequivalenza terapeutica e sulla tollerabilita dei prodotti a base di Serenoa repens in capsule da 160 mg o capsule rettali da 640 mg] Archivio di Medicina Interna. 1994;46(2):61–75. [Google Scholar]
- Shi 2007{published data only}.Shi R, Xie Q, Gang X, Lun J, Life C, Pantuck A, Rao J. Effect of saw palmetto soft gel capsule on lower urinary tract symptoms associated with benign prostatic hyperplasia: a randomized trial in shanghai, china. The Journal of Urology. 2008;179:610–5. doi: 10.1016/j.juro.2007.09.032. [DOI] [PubMed] [Google Scholar]
- Sökeland J. Combined sabal and urtica extract compared with finasteride in men with benign prostatic hyperplasia: analysis of prostate volume and therapeutic outcome. BJU International. 2000;86:439–42. doi: 10.1046/j.1464-410x.2000.00776.x. [DOI] [PubMed] [Google Scholar]
- *Sökeland 1997{published data only}.Sökeland J, Albrecht J. Combined sabal and urtica extract compared with finasteride in men with benign prostatic hyperplasia: analysis of prostate volume and therapeutic outcome [Kombination aus Sabal– und Urticaestrakt vs. finasterid bei BPH (Stad. I bis II nach Alken); Vergleich der therapeutischen wirksamkeit in einer einjahrigen doppelblindstudie] Urologe A. 1997;36(4):327–33. doi: 10.1007/s001200050106. [MEDLINE: 1997419443] [DOI] [PubMed] [Google Scholar]
- Tasca 1985{published data only}.Tasca A, Barulli M, Cavazzana A, Zattoni F, Artibani W, Pagano F. [Trattamento della sintomatologia ostruttiva da adenoma prostatico con estratto di Serenoa repens. Studio clinico in doppio cieco vs. placebo] Minerva Urologica e Nefrologica. 1985;37:87–91. [MEDLINE: 1986019370] [PubMed] [Google Scholar]
- Willetts 2003{published data only}.Willetts KE, Clements MS, Champion S, Ehsman S, Eden JA. Serenoa repens extract for benign prostate hyperplasia: a randomized controlled trial. British Journal of Urology International. 2003;92:267–70. doi: 10.1046/j.1464-410x.2003.04316.x. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Adriazola Semino 1992{published data only}.Adriazola Semino M, Lozano Ortega JL, Garcia Cobo E, Tejeda Banez E, Romero Rodriguez F. Symptomatic treatment of benign hypertrophy of the prostate. Comparative study of prazosin and serenoa repens [Tratamiento sintomatico de la hipertrofia benigna de prostata. Estudio comparativo entre prazosin y Serenoa repens] Archivos Espanoles de Urologia. 1992;45(3):211–3. [MEDLINE: 1993037631] [PubMed] [Google Scholar]
- Comar 1986{published data only}.Comar OB, Di Rienzo A. Mepartricin versus Serenoa repens: double-blind study in 20 cases of benign prostate hypertrophy. Rivista Italiana di Biologia e Medicina. 1986;6(2):122–5. [Google Scholar]
- Di Silverio 1992{published data only}.Di Siverio F, D’Eramo G, Lubrano C, Flammia GP, Sciarra A, Palma E, Caponera M, Sciarra F. Evidence that Serenoa repens extract displays an antiestrogenic activity in prostatic tissue of benign prostatic hypertrophy patients. European Urology. 1992;21(4):309–14. doi: 10.1159/000474863. [MEDLINE: 1993093014] [DOI] [PubMed] [Google Scholar]
- Gerber 1998{published data only}.Gerber GS, Zagaja GP, Bales GT, Chodak GW, Contreras BA. Saw palmetto (Serenoa repens) in men with lower urinary tract symptoms: effects on urodynamic parameters and voiding symptoms. Urology. 1998;51(6):1003–7. doi: 10.1016/s0090-4295(98)00143-5. [DOI] [PubMed] [Google Scholar]
- Grasso 1995{published data only}.Grasso M, Montesano A, Buonaguidi A, Castelli M, Lania C, Rigatti P, Rocco F, Cesana BM, Borghi C. Comparative effects of alfuzosin versus Serenoa repens in the treatment of symptomatic benign prostatic hyperplasia. Archivos Españoles de Urología. 1995;48(1):97–103. [MEDLINE: 1995251418] [PubMed] [Google Scholar]
- Pecoraro 2004{published data only}.Pecoraro S, Annecchiarico A, Gambardella M-C, Sepe G. Efficacy of pretreatment with Serenoa repens on bleeding associated with transurethral resection of prostate [Effetto del pretrattamento con serenoa repens sul sanguinamento associato a resezione transuretrale della prostata] Minerva Urologica e Nefrologica. 2004;56:73–8. [PubMed] [Google Scholar]
- Popa 2005{published data only}.Popa G, Hägele-Kaddour H, Walther C. [Symptomatische wirksamkeit eines sabal–urtica–kombinationspräparats in der therapie des benignen prostatasyndroms: ergebnisse einer plazebokontrollierten doppelblindstudie] MMW Fortschritte der Medizin. 2005;147(Supp 3):103–8. [PubMed] [Google Scholar]
- Sivkov 2001{published data only}.Sivkov A, Köhler S, Engelmann U, Medvedev A, Lopatkin N. Long-term efficacy and safety of a combination of sabal and urtica extracts in LUTS - a placebo-controlled, double-blind, multicenter trial. Urologe A. 2001;40(Suppl 1):S19. [Google Scholar]
- Strauch 1994{published data only}.Strauch G, Perles P, Vergult G, Gabriel M, Gibelin B, Cummings S, Malbecq W, Malice MP. Comparison of finasteride (Proscar) and Serenoa repens (Permixon) in the inhibition of 5-alpha reductase in healthy male volunteers. European Urology. 1994;26(3):247–52. doi: 10.1159/000475388. [MEDLINE: 1995104266] [DOI] [PubMed] [Google Scholar]
- Vela-Navarrete 2003a{published data only}.Vela Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, López Farré A. BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. European Urology. 2003;44:549–55. doi: 10.1016/s0302-2838(03)00368-3. [DOI] [PubMed] [Google Scholar]
- *Vela-Navarrete 2003b{published data only}.Vela-Navarrete R, Garcia Cardoso JV, Barat A, Manzarbeitia F, Lopez Farre A. BPH and inflammation: pharmacological effects of Permixon on histological and molecular inflammatory markers. Results of a double blind pilot clinical assay. European Urology. 2003;44:549–55. doi: 10.1016/s0302-2838(03)00368-3. [DOI] [PubMed] [Google Scholar]
- Vela-Navarrete 2005{published data only}.Vela-Navarrete R, Escribano-Burgos M, Lopez Farre A, Garcia-Cardoso J, Manzarbeitia F, Carrasco C. Serenoa repens treatment modifies BAX/BCL-2 index expression and CASPASE-3 activity in prostatic tissue from patients with benign prostatic hyperplasia. The Journal of Urology. 2005;173:507–10. doi: 10.1097/01.ju.0000150533.94952.25. [DOI] [PubMed] [Google Scholar]
- Weisser 1997{published data only}.Weissser H, Behnke, Helpap B, Bach D, Krieg M. Enzyme activities in tissue of human benign prostatic hyperplasia after three months’ treatment with the Sabal serrulata extract IDS 89 (Strogen) or placebo. European Urology. 1997;31(1):97–101. doi: 10.1159/000474426. [MEDLINE: 1997184773] [DOI] [PubMed] [Google Scholar]
Additional references
- Abrams 1979.Abrams PH, Griffiths DJ. The assessment of prostatic obstruction from urodynamic measurements and from residual urine. British Journal of Urology. 1979;51(2):129–34. doi: 10.1111/j.1464-410x.1979.tb02846.x. [DOI] [PubMed] [Google Scholar]
- Bales 1999.Bales G, Christiano AP, Kirsh E, Gerber GS. Phytotherapeutic agents in the treatment of lower urinary tract symptoms: a demographic analysis of awareness and use at the University of Chicago. Urology. 1999;54:86–9. doi: 10.1016/s0090-4295(99)00028-x. [DOI] [PubMed] [Google Scholar]
- Barnes 2002.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Advance data from vital and health statistics of the National Center for Health Statistics. 2004;27(343):1–19. [PubMed] [Google Scholar]
- Berry 1984.Berry SL, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. The Journal of Urology. 1984;132:474–9. doi: 10.1016/s0022-5347(17)49698-4. [MEDLINE: 1984292487] [DOI] [PubMed] [Google Scholar]
- Boyle 2004.Boyle P, Robertson C, Lowe F, Roehrborn C. Updated meta-analysis of clinical trials of Serenoa repens extract in the treatment of symptomatic benign prostatic hyperplasia. BJU International. 2004;93(6):751–6. doi: 10.1111/j.1464-410X.2003.04735.x. [DOI] [PubMed] [Google Scholar]
- Buck 1996.Buck AC. Phytotherapy for the prostate. British Journal of Urology. 1996;78(3):325–6. doi: 10.1046/j.1464-410x.1996.00104.x. [MEDLINE: 1997036289] [DOI] [PubMed] [Google Scholar]
- Buck 2004.Buck AC. Is there a scientific basis for the therapeutic effects of serenoa repens in benign prostatic hyperplasia? Mechanisms of action. The Journal of Urology. 2004;172:1792. doi: 10.1097/01.ju.0000140503.11467.8e. [DOI] [PubMed] [Google Scholar]
- Christensen 1990.Christensen MM, Bruskewitz RC. Clinical manifestations of benign prostatic hyperplasia and the indications for therapeutic intervention. Urology Clinics of North America. 1990;17:509–16. [MEDLINE: 1990327595] [PubMed] [Google Scholar]
- Cochrane Handbook 2008.Higgins JPT, Green S, editors. Chapter 8: Assessing risk of bias in included studies. [accessed September 2008];Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 (updated February 2008). The Cochrane Collaboration. 2008 www.cochrane-handbook.org. [: http://www.mrc–bsu.cam.ac.uk/cochrane/handbook/]
- Dedhia 2008.Dedhia RC, McVary KT. Phytotherapy for lower urinary tract symptoms secondary to benign prostatic hyperplasia. The Journal of Urology. 2008;179:2119–25. doi: 10.1016/j.juro.2008.01.094. [DOI] [PubMed] [Google Scholar]
- Di Silverio 1993.Di Silverio F, Flammia GP, Sciarra A, Caponera M, Mauro M, Buscarini M, Tavani M, D’Eramo G. Plant extracts in benign prostatic hyperplasia. Minerva Urologica e Nefrologica. 1993;45:143–9. [MEDLINE: 1994294881] [PubMed] [Google Scholar]
- Dickersin 1994.Dickersin K, Scherer R, Lefebvre C. Indentifying relevant studies for systematic reviews. British Medical Journal. 1994;312:944–7. doi: 10.1136/bmj.309.6964.1286. [MEDLINE: 1995195448] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dreikorn 1990.Dreikorn K, Richter R, Schönhöfer PS. Conservative nonhormonal treatment of patients with benign prostatic hyperplasia. Urologe A. 1990;29(1):8–16. [PUBMED: 1690486] [PubMed] [Google Scholar]
- Follmann 1992.Follmann D, Elliott P, Cutler J. Variance imputation for overviews of clinical trials with continuous response. Journal of Clinical Epidemiology. 1992;45(7):763–73. doi: 10.1016/0895-4356(92)90054-q. [DOI] [PubMed] [Google Scholar]
- Lavori 1992.Lavori PW. Clinical trials in psychiatry: should protocol deviation censor patient data? Neuropsychopharmacology. 1992;6:39–63. [MEDLINE: 1992238968] [PubMed] [Google Scholar]
- Lepor 1996.Lepor H, Williford WO, Barry MJ, et al. The efficacy of terazosin and finasteride, or both in benign prostatic hyperplasia. New England Journal of Medicine. 1996;335:533–9. doi: 10.1056/NEJM199608223350801. [DOI] [PubMed] [Google Scholar]
- Litwin MS, Saigal CS, editors.Wei JT, Calhoun EA, Jacobsen SJ. Benign prostatic hyperplasia. In: Litwin MS, Saigal CS, editors. Urologic Diseases in America. Washington, DC: US Government Publishing Office; 2007. [Google Scholar]
- Marwick 1995.Marwick C. Growing use of medicinal botanicals forces assessment by drug regulators. Journal of the American Medical Association. 1995;273:607–9. [MEDLINE: 1995147312] [PubMed] [Google Scholar]
- McConnell 1994.McConnell JD, Barry MJ, Bruskewitz RC. Benign prostatic hyperplasia: diagnosis and treatment. Agency for Health Care Policy and Research. Clinical practice guideline. Quick reference guide for clinicians. 1994;8:1–17. [PUBMED: 7507389] [PubMed] [Google Scholar]
- McConnell 2003.McConnell JD, Roehrborn CG, Bautista OM, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. New England Journal of Medicine. 2003;349:2387–98. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- McGuire 1987.McGuire E. Detrusor response to obstruction. NIH Publication No. 87–2881. Vol. 221 1987. [Google Scholar]
- Meigs 2001.Meigs JB, Mohr B, Barry MJ, Collins MM, McKinlay JB. Risk factors for clinical benign prostatic hyperplasia in a community-based population of healthy aging men. Journal of Clinical Epidemiology. 2001;54:935–44. doi: 10.1016/s0895-4356(01)00351-1. [DOI] [PubMed] [Google Scholar]
- Platz 2002.Platz EA, Smit E, Curhan GC, Nyberg LM, Jr, Giovannucci E. Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in US men. Urology. 2002;59:877–83. doi: 10.1016/s0090-4295(01)01673-9. [DOI] [PubMed] [Google Scholar]
- Schulz 1995.Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. Journal of the American Medical Association. 1995;273:408–12. doi: 10.1001/jama.273.5.408. [MEDLINE: 1995123716] [DOI] [PubMed] [Google Scholar]
- Vacherot 2000.Vacherot F, Azzouz M, Gil-Diez-de-Medina S, Colombel M, de la Taille A, Lefrere Belda MA, et al. Induction of apoptosis and inhibition of cell proliferation by the lipido-sterolic extract of Serenoa repens (LSESr, Permixon®) in benign prostatic hyperplasia. The Prostate. 2000;45:507. doi: 10.1002/1097-0045(20001101)45:3<259::aid-pros9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Weisser 1996.Weisser H, Tunn S, Behnke B, Krieg M. Effects of the sabal serrulata extract IDS 89 and its subfractions on 5 alpha-reductase activity in human benign prostatic hyperplasia. The Prostate. 1996;28:300. doi: 10.1002/(SICI)1097-0045(199605)28:5<300::AID-PROS5>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Wilt 1998.Wilt TJ, Ishani A, Stark G, Mac Donald R, Lau J, Mulrow C. Saw palmetto extracts for treatment of benign prostatic hyperplasia: a systematic review. Journal of the American Medical Association. 1998;280(18):1604–9. doi: 10.1001/jama.280.18.1604. [DOI] [PubMed] [Google Scholar]
- Wilt 2002.Wilt T, Ishani A, Mac Donald R. Serenoa repens for benign prostatic hyperplasia. Cochrane Database of Systematic Reviews. 2002;(3) doi: 10.1002/14651858.CD001423. [DOI] [PubMed] [Google Scholar]