Abstract
Purpose
To evaluate the effects of toremifene on bone mineral density (BMD), a surrogate for fracture risk, in men receiving androgen deprivation therapy (ADT) for prostate cancer.
Materials and Methods
In an ongoing, multicenter, Phase 3 fracture prevention study, 1392 men ≥ 50 years old with prostate cancer receiving ADT were randomized to toremifene (80 mg/day) or placebo. BMD of lumbar spine, total hip, and femoral neck was assessed using dual-energy x-ray absorptiometry (DXA). This planned interim analysis of the first 197 subjects compared BMD changes from baseline to month 12 between the placebo and toremifene groups.
Results
Compared with the placebo group, men in the toremifene group had significant increases in BMD at each of the evaluated skeletal sites. BMD of the lumbar spine decreased 0.7% in the placebo group and increased 1.6% in the toremifene group (P < 0.001 for between-group comparison). BMD of the total hip decreased 1.3% in the placebo group and increased 0.7% in the toremifene group (P = 0.001). BMD of the femoral neck decreased 1.3% in the placebo group and increased 0.2% in the toremifene group (P = 0.009). The between-group differences for change in BMD from baseline to month 12 were 2.3%, 2.0%, and 1.5% for the lumbar spine, total hip, and femoral neck, respectively.
Conclusions
Toremifene significantly increased BMD of the hip and spine in men receiving ADT for prostate cancer. The effect of toremifene on fracture risk is being assessed in the ongoing randomized controlled trial.
Keywords: prostate cancer, GnRH agonist, orchiectomy, osteoporosis, toremifene, androgen deprivation therapy
INTRODUCTION
Androgen deprivation therapy (ADT), by either bilateral orchiectomy or administration of gonadotropin-releasing hormone (GnRH) agonist, is the mainstay treatment for recurrent, advanced and metastatic prostate cancer and is also frequently used in earlier stage prostate cancer patients to prevent disease progression.1 Short-term and long-term ADT lowers serum testosterone, as well as serum estrogen levels, which leads to bone loss and clinical fractures in men on ADT. 4,5 ADT patients who experience a clinical fracture have on average a 39-month reduction in survival.6 Bone loss and clinical fractures have emerged as important side effects of hormonal therapy that account for significant morbidity and potential mortality in men on ADT. About one-third of the estimated two million prostate cancer survivors in the United States currently receive treatment with a GnRH agonist.7
Estrogens in men are derived by aromatization of testosterone by aromatase. By reducing testosterone, GnRH agonists lower estrogen. In fact, estrogen levels in men on ADT are even lower than estrogen levels in postmenopausal women.5,8 Estrogens play an important role in skeletal homeostasis in both men and women. Estrogen receptors are primarily expressed in osteoclasts.10 By inhibiting osteoclasts, estrogens are antiresorptive on bone.13 Serum estradiol increases BMD and is associated with reduced fracture risk in older men.15
Toremifene is a second-generation selective estrogen receptor modulator (SERM) which is currently in clinical development for the prevention and treatment of osteoporosis in men receiving ADT for hormone-sensitive prostate cancer.17 Toremifene mimics the beneficial effects of estrogen in bone. In an ongoing, multicenter, Phase 3 fracture prevention study, 1392 prostate cancer men receiving ADT for prostate cancer were randomized to receive either placebo or toremifene (80 mg daily) for 24 months. We report herein the results of a planned interim analysis of BMD, a secondary endpoint, for the first 197 subjects to complete one-year follow-up.
MATERIAL AND METHODS
Subjects
The ongoing phase 3 study is a 24-month, double-blind, randomized, placebo-controlled trial of toremifene to prevent incident morphometric vertebral fractures in men receiving ADT for prostate cancer. Between July 2003 and November 2005, 1392 subjects from 140 centers in the United States and Mexico were enrolled in the study. All participants were men ≥ 50 years old with histologically documented prostate cancer, serum prostate-specific antigen (PSA) ≤ 4 ng/mL, and either history of orchiectomy or treatment with a GnRH agonist for at least 6 months, or intermittent treatment with a GnRH agonist for at least 12 months. The study included subjects at increased risk for fracture either by having a low BMD of the lumbar spine or hip, or being ≥ 70 years of age. BMD requirements for subjects younger than 70 years are summarized in Table 1.
Table 1.
BMD Requirements for Study Entry for Subjects Younger Than 70 Years
| Hologic DXA | Lunar DXA | |
|---|---|---|
| BMD, g/cm2 | ||
| Lumbar spine | ≤ 0.926 | ≤ 1.050 |
| Femoral Neck | ≤ 0.717 | ≤ 0.840 |
Subjects receiving prescription treatment for osteoporosis (bisphosphonates, other SERMs, parathyroid hormone, and calcitonin) or treatment with oral glucocorticoids or agents that affect testosterone, such as finasteride, dutasteride, danazol, or testosterone-like supplements, within 45 days were excluded from the study. Subjects with > 4 morphometric vertebral fractures, Paget’s disease of bone, or any history of thromboembolic disease (including deep vein thrombosis or pulmonary embolus) were also excluded.
An institutional review board for each of the participating institutions approved the study. Subjects provided written informed consent prior to study participation.
Study Design
The primary endpoint for the Phase 3 study is the proportion of new morphometric vertebral fractures in the toremifene group versus the placebo group after 24 months. The key secondary endpoints measured were the incidence of clinical fragility fractures; BMD of the lumbar spine and femur; incidence, frequency, and severity of hot flashes; incidence and severity of gynecomastia; safety profile; changes in lipid profile; and quality of life.
For this planned interim analysis, the endpoint was the percentage change in BMD from baseline to month 12 of the lumbar spine, total hip, and femoral neck. The interim analysis was performed in the first 197 subjects (104 in the placebo group and 93 in the toremifene group) who had both a baseline and 12-month BMD assessment of the lumbar spine.
BMD of the posteroanterior lumbar spine (L1–L4), total hip, and femoral neck were determined by dual energy x-ray absorptiometry (DXA) using either Hologic (Hologic, Inc., Waltham, MA) or Lunar (Lunar, Inc., Madison, WI) densitometer. Reviewers, who were blinded to study treatment, summarized all DXA data at a central laboratory (Synarc, Inc., Portland, OR). A Data Safety Monitoring Committee continuously evaluated the clinical trial and reviewed unblinded safety data every 6 months. These safety analyses are not part of the current interim analysis.
Statistical Analysis
The primary efficacy variables for this planned interim analysis were the changes in BMD at lumbar spine, hip, and femur skeletal sites from baseline to month 12. Mean changes in BMD were compared between the groups using an analysis of variance with treatment and study center as the covariates. Statistical analysis was performed using SAS® version 8. Values are reported as means plus-minus standard deviation unless specified otherwise. All p values are two-sided and values < 0.045 are considered significant.
RESULTS
In this planned interim analysis, 197 subjects were randomized to receive either placebo (n = 104) or toremifene 80 mg (n = 93) orally each day for 1 year. Baseline characteristics were similar between the groups (Table 2). Mean (± standard deviation) age was 77.5 ± 6.5 years for men in the placebo group and 76.3 ± 6.9 years for men in the toremifene group. Mean duration of ADT was 3.2 ± 3.1 years in the overall study population.
Table 2.
Baseline Characteristics (± standard error of least square mean)
| Placebo (n = 104) | Toremifene (n = 93) | |
|---|---|---|
| Age, years | 77.5 ± 6.5 | 76.3 ± 6.9 |
|
| ||
| BMD, g/cm2 | ||
| Lumbar spine | 1.0388 ± 0.02040 | 1.1025 ± 0.02157 |
| Total hip | 0.8917 ± 0.01502 | 0.9181 ± 0.01598 |
| Femoral neck | 0.7636 ± 0.01503 | 0.8033 ± 0.0159 |
Plus-minus values are mean ± standard deviation.
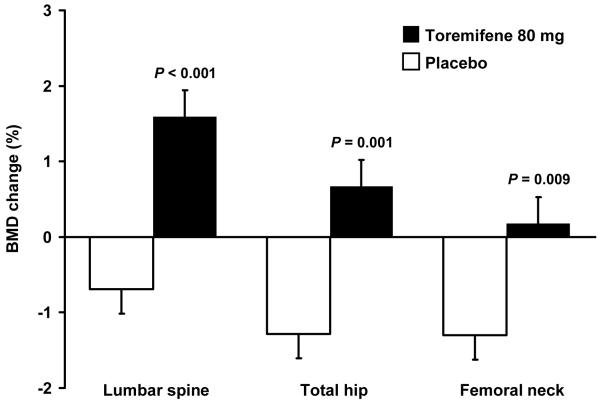
Changes in BMD of the lumbar spine from baseline to month 12 differed significantly between the placebo and toremifene groups (Figure 1). BMD of the lumbar spine decreased by 0.7 ± 0.3% in the placebo group and increased by 1.6 ± 0.4% in the toremifene group (P < 0.001 for between-group comparison). The between-group difference for change in BMD from baseline to month 12 was 2.3%.
Figure 1.
Percentage change in bone mineral density from baseline to month 12 in men receiving androgen deprivation therapy for prostate cancer treated with toremifene (solid boxes) or placebo (white boxes).
Changes in BMD of the hip from baseline to month 12 also differed significantly between the placebo and toremifene groups (Figure 1). BMD of the total hip decreased by 1.3 ± 0.3% in the placebo group and increased by 0.7 ± 0.6% in the toremifene group (P = 0.001). Similarly, BMD of the femoral neck decreased 1.3 ± 0.4% in the placebo group and increased 0.2 ± 0.4% in the toremifene group (P = 0.009). The between-group differences for change in BMD from baseline to month 12 were 2.0% and 1.5% for the total hip and femoral neck, respectively.
DISCUSSION
In this planned interim analysis of a large, randomized, placebo-controlled, Phase 3 fracture prevention study in men on ADT for prostate cancer, toremifene (80 mg/day) significantly increased BMD of the lumbar spine, total hip, and femoral neck. Because low BMD independently predicts fracture risk in men,19 these findings suggest that toremifene may decrease fracture risk in men receiving ADT for prostate cancer by increasing BMD. The magnitude of BMD changes in the subjects in the Phase 3 ADT clinical trial are similar to the reported increases in BMD observed in clinical trials conducted in postmenopausal women treated with another SERM, raloxifene.20 In a randomized, placebo-controlled Phase 3 clinical trial of postmenopausal women, raloxifene significantly increased the BMD of the lumbar spine by 2.0% at 1 year and decreased morphometric vertebral fracture risk by 55% over 3 years.20 In the current study, toremifene increased the BMD of the lumbar spine by 2.3% at 1 year, suggesting that the BMD increases observed in men on ADT should be sufficient to confer a significant decrease in fracture risk.
The effects of toremifene 80 mg on BMD in the current Phase 3 study are also consistent with earlier reports from smaller studies that SERMs increase BMD in men on ADT. In a small, randomized, dose-ranging study of men receiving ADT for prostate cancer, toremifene (60 mg/day) significantly increased BMD of the lumbar spine but only trended (not significantly) to increase BMD of the hip after 6 months,21 suggesting 60 mg may not be the appropriate efficacy dose. In another small, randomized, controlled trial of men receiving GnRH agonist therapy for prostate cancer, raloxifene (60 mg/day) significantly increased BMD of the hip and only trended to increase BMD of the lumbar spine after 12 months.22 In both studies, treatment with a SERM decreased biochemical markers of bone formation and bone resorption.21,22 In postmenopausal women, raloxifene also significantly decreased markers of both bone formation and bone resorption.23,24 These results suggest that the SERMs increase BMD in postmenopausal women and endocrine-induced hypogonadal men to the same degree by similar mechanisms.
This is one of the largest reported prospective analyses of BMD in men receiving ADT for prostate cancer. The interim analysis plan did not allow for detailed comparison of baseline characteristics between the groups and there may have been minor unintended imbalances in baseline characteristics between the groups. Substantial differences between the groups are unlikely, however, based on the large sample size. Moreover, any imbalance between the treatment groups could not readily explain the observed highly significant and consistent treatment effects. In addition, the safety profile of any SERM must be determined in a Phase 3 randomized clinical trial. It cannot be assumed that all SERMs are equipotent for efficacy as the relative estrogenicity of each SERM is different. The degree of estrogenicity for each SERM may also affect the safety profile, as has been previously observed in postmenopausal women.25
ADT has other adverse effects related to its suppression of testosterone and estrogen, such as gynecomastia, mastodynia, vasomotor flushing, increased serum cholesterol, and decreased insulin sensitivity.1,26,27 Consistent with these adverse metabolic effects, GnRH agonists have recently been associated with greater risk of diabetes mellitus and cardiovascular disease.28 Toremifene has the potential to decrease some of these nonskeletal adverse effects of ADT. Toremifene 60 mg (FARESTON®) is antiestrogenic in breast tissue and is approved by the US Food and Drug Administration for the treatment of metastatic breast cancer in postmenopausal women.29 The antiestrogenic activity of toremifene on breast tissue may reduce breast enlargement and tenderness in men on ADT. Toremifene appears to act as a partial agonist and is estrogenic in the hypothalamic-pituitary axis,30 which may decrease vasomotor flushing. Toremifene significantly decreases total cholesterol, low-density lipoprotein cholesterol, and triglycerides in postmenopausal women31 and may have similar beneficial effects on serum lipoproteins in hypogonadal men.21 Accordingly, secondary endpoints being measured in the ongoing Phase 3 clinical study include vasomotor flushing, breast changes, and serum lipoproteins. Evaluation of these endpoints will determine whether toremifene may provide these wider advantages to men on ADT.
CONCLUSIONS
Toremifene (80 mg/day) significantly increased BMD of the hip and spine in men receiving ADT for prostate cancer. Similar improvements in BMD were associated with significant decreases in fracture risk in postmenopausal women treated with raloxifene. Taken together, these observations suggest that toremifene may decrease fracture risk in men receiving ADT for prostate cancer. The final results of the ongoing, multicenter, Phase 3 fracture prevention study in men with prostate cancer on ADT will establish the clinical efficacy of toremifene in this setting.
Standard abbreviations
- ADT
Androgen deprivation therapy
- BMD
Bone mineral density
- DXA
Dual-energy x-ray absorptiometry
- GnRH
Gonadotropin-releasing hormone
- PSA
Prostate-specific antigen
- SERM
Selective estrogen receptor modulator
REFERENCES
- 1.Sharifi N, Gulley JL, Dahut WL. Androgen deprivation therapy for prostate cancer. JAMA. 2005;294:238. doi: 10.1001/jama.294.2.238. [DOI] [PubMed] [Google Scholar]
- 2.Maillefert JF, Sibilia J, Michel F, Saussine C, Javier RM, Tavernier C. Bone mineral density in men treated with synthetic gonadotropin-releasing hormone agonists for prostatic carcinoma. J Urol. 1999;161:1219. [PubMed] [Google Scholar]
- 3.Smith MR, McGovern FJ, Zietman AL, Fallon MA, Hayden DL, Schoenfeld DA, et al. Pamidronate to prevent bone loss in men receiving gonadotropin releasing hormone agonist therapy for prostate cancer. N Engl J Med. 2001;345:948. doi: 10.1056/NEJMoa010845. [DOI] [PubMed] [Google Scholar]
- 4.Oefelein MG, Ricchiuti V, Conrad W, Resnick MI. Skeletal fractures negatively correlate with overall survival in men with prostate cancer. J Urol. 2002;168:1005. doi: 10.1016/S0022-5347(05)64561-2. [DOI] [PubMed] [Google Scholar]
- 5.Barry MJ, Delorenzo MA, Walker-Corkery ES, Lucas FL, Wennberg DC. The rising prevalence of androgen deprivation among older American men since the advent of prostate-specific antigen testing: a population-based cohort study. BJU Int. 2006;98:973. doi: 10.1111/j.1464-410X.2006.06416.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khosla S, Melton LJ, 3rd, Atkinson EJ, O’Fallon WM. Relationship of serum sex steroid levels to longitudinal changes in bone density in young versus elderly men. J Clin Endocrinol Metab. 2001;86:3555. doi: 10.1210/jcem.86.8.7736. [DOI] [PubMed] [Google Scholar]
- 7.Need AG, Horowitz M, Stiliano A, Scopacasa F, Morris HA, Chatterton BE. Vitamin D receptor genotypes are related to bone size and bone density in men. Eur J Clin Invest. 1996;26:793. doi: 10.1046/j.1365-2362.1996.2080554.x. [DOI] [PubMed] [Google Scholar]
- 8.Girasole G, Jilka RL, Passeri G, Boswell S, Boder G, Williams DC, et al. 17β-Estradiol inhibits interleukin-6 production by bone marrow-derived stromal cells and osteoblasts in vitro: a potential mechanism for the antiosteoporotic effect of estrogens. J Clin Investigation. 1992;89:883. doi: 10.1172/JCI115668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khosla S, Melton LJ, 3rd, Atkinson EJ, O’Fallon WM, Klee GG, Riggs BL. Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab. 1998;83:2266. doi: 10.1210/jcem.83.7.4924. [DOI] [PubMed] [Google Scholar]
- 10.Smith MR. Selective estrogen receptor modulators to prevent treatment-related osteoporosis. Rev Urol. 2005;7(Suppl 3):S30. [PMC free article] [PubMed] [Google Scholar]
- 11.Van der Klift M, De Laet CE, McCloskey EV, Hofman A, Pols HA. The incidence of vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res. 2002;17:1051. doi: 10.1359/jbmr.2002.17.6.1051. [DOI] [PubMed] [Google Scholar]
- 12.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282:637. doi: 10.1001/jama.282.7.637. [DOI] [PubMed] [Google Scholar]
- 13.Steiner MS, Patterson A, Israeli R, Barnette KG, Boger R, Price D. Toremifene citrate versus placebo for treatment of bone loss and other complications of androgen deprivation therapy in patients with prostate cancer. Proc ASCO. 2004 (abstract 4597) [Google Scholar]
- 14.Smith MR, Fallon MA, Lee H, Finkelstein JS. Raloxifene to prevent gonadotropin-releasing hormone agonist-induced bone loss in men with prostate cancer: a randomized controlled trial. J Clin Endocrinol Metab. 2004;89:3841. doi: 10.1210/jc.2003-032058. [DOI] [PubMed] [Google Scholar]
- 15.Draper MW, Flowers DE, Huster WJ, Neild JA, Harper KD, Arnaud C. A controlled trial of raloxifene ( LY139481) HCl: impact on bone turnover and serum lipid profile in healthy postmenopausal women. J Bone Miner Res. 1996;11:835. doi: 10.1002/jbmr.5650110615. [DOI] [PubMed] [Google Scholar]
- 16.Delmas PD, Bjarnason NH, Mitlak BH, Ravoux AC, Shah AS, Huster WJ, et al. Effects of raloxifene on bone mineral density, serum cholesterol concentrations, and uterine endometrium in postmenopausal women. N Engl J Med. 1997;337:1641. doi: 10.1056/NEJM199712043372301. [DOI] [PubMed] [Google Scholar]
- 17.Harvey HA, Kimura M, Hajba A. Toremifene: an evaluation of its safety profile. Breast. 2005 doi: 10.1016/j.breast.2005.09.007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 18.Smith MR, Finkelstein JS, McGovern FJ, Zietman AL, Fallon MA, Schoenfeld DA, et al. Changes in body composition during androgen deprivation therapy for prostate cancer. J Clin Endocrinol Metab. 2002;87:599. doi: 10.1210/jcem.87.2.8299. [DOI] [PubMed] [Google Scholar]
- 19.Smith MR, Lee H, Nathan DM. Insulin sensitivity during combined androgen blockade for prostate cancer. J Clin Endocrinol Metab. 2006;91:1305. doi: 10.1210/jc.2005-2507. [DOI] [PubMed] [Google Scholar]
- 20.Keating NL, O’Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2006;24:4448. doi: 10.1200/JCO.2006.06.2497. [DOI] [PubMed] [Google Scholar]
- 21.Toremifene citrate prescribing information. GTx Incorporated; Memphis, Tenn: 2006. [Package insert] [Google Scholar]
- 22.Ellmen J, Hakulinen P, Partanen A, Hayes DF. Estrogenic effects of toremifene and tamoxifen in postmenopausal breast cancer patients. Breast Cancer Res Treat. 2003;82:103. doi: 10.1023/B:BREA.0000003957.54851.11. [DOI] [PubMed] [Google Scholar]
- 23.Joensuu H, Holli K, Oksanen H, Valavaara R. Serum lipid levels during and after adjuvant toremifene or tamoxifen therapy for breast cancer. Breast Cancer Res Treat. 2000;63:225. doi: 10.1023/a:1006465732143. [DOI] [PubMed] [Google Scholar]