Abstract
PURPOSE
The number of effective knee osteoarthritis (OA) interventions, especially those tailored to specific compartmental involvement, is small. The objective of this study was to determine the efficacy of a realigning patellofemoral (PF) brace in improving pain and function among persons with symptomatic lateral patellofemoral OA.
METHOD
We conducted a double blind, randomized crossover trial of a realigning PF brace for persons with lateral PF OA. Participants had lateral PF OA with anterior knee symptoms on most days of the month, lateral PF joint space narrowing, and radiographic evidence of a definite osteophyte in the PF joint. We compared two treatments: A) Control treatment consisting of a BioSkin Q Brace with patellar realigning strap removed; and B) Active treatment consisting of a realigning BioSkin Q Brace with the strap applied. For each participant, the trial lasted 18 weeks, including 6 weeks each of active and control treatment period separated by a 6-week washout period. The order of treatments was randomized. The primary outcome was change in knee pain on the visual analog scale (VAS). Secondary outcomes included WOMAC pain, function, and stiffness. An unstructured correlation matrix for observations within participants was used in generalized estimating equation fitting to derive a linear regression model that expressed the relation between the intervention and change in VAS pain.
RESULTS
80 participants (63 F) with a mean age and body mass index of 61 years and 28 kg/m2, respectively, were randomized by order of treatment. A model examining the main effects for change in VAS knee pain (0–100) demonstrated no significant treatment effect (−0.68 VAS units, 95% CI: −6.2, 4.8 units, p=0.81) and no differential carryover effect. There was also no significant difference between active and control treatments for WOMAC pain, function, or stiffness outcomes.
CONCLUSION
The effects of a specific realigning patellofemoral brace are not of clinical or statistical significance.
Keywords: Patellofemoral osteoarthritis, brace
Introduction
The patellofemoral (PF) joint is involved in approximately 65% of persons with knee OA; predominantly within the lateral PF compartment [1,2]. Relatively little attention has been paid to the PF joint in knee OA, despite suggestions that disease in this compartment may be strongly correlated with lower extremity disability [3], and that involvement of the PF joint is more highly correlated with knee pain in OA than is isolated involvement of the tibiofemoral (TF) joint [4–6]. Unfortunately, the majority of epidemiologic studies examining risk factors for OA have focused on the TF joint with little heed paid to the unique biomechanics of the PF joint [7–9]. This line of research is needed as the designs of the PF and TF compartments reflect unique functions and mechanics [10]. These differences in design and function are likely to have important implications for treatment. Given the heterogeneity of OA as a disease process and its protean symptomatic presentations, therapeutic interventions for knee OA should be guided by an awareness of which joint compartments are involved. At present, there are few effective conservative interventions for relieving pain and improving function in knee OA and even fewer that are specifically targeted to the unique mechanics of the PF compartment.
Patellar malalignment is a translational or rotational deviation of the patella that may lead to an aberrant dispersion of forces transmitted through the PF joint [11]. Patellar malalignment may cause an aberrant dispersion of patellofemoral joint reaction (PFJR) forces and, by this mechanism, predispose to pain and/or structural damage [11–13]. Of primary concern is excessive lateral translation in the coronal plane and excessive lateral tilt in the axial plane [14]. Uncontrolled data suggests that patellae that are well-aligned centrally in the trochlear groove, without lateral coronal or axial malalignment, may be less likely to develop osteoarthritis [15–17]. Conversely, persons with lateral PF OA often present with laterally malaligned patellae and maltracking that is associated with symptoms [18]. Prior studies have demonstrated that patellar taping can lead to marked short-term improvements in knee pain [19,20] although it is not altogether clear that the mechanism involves substantive changes in patellar alignment [21–28]. One possible explanation of the favorable influence that patellar taping has on symptoms is that it leads to sufficient improvements in patellofemoral alignment (by reducing lateral displacement and tilt) to improve joint contact area and consequently impact joint stress. Some evidence suggests that realigning patellofemoral braces can lead to similar short-term improvements in joint contact area [23,24].
Given the increased likelihood of patellar malalignment in people with PF OA and the link between malalignment and symptoms, interventions that aim to improve patellar alignment may be efficacious. If one were able to improve PF alignment with application of a patellofemoral brace with a realigning strap in persons with PF OA, similar improvements in symptoms to those seen in response to patellar taping may be possible [3,29]. Despite its proven efficacy, patellar taping [30] has not been widely adopted clinically for the treatment of patients with knee OA [19,20]. This probably results from the fact that it is complicated to administer and often difficult for older patients to apply independently. Skin irritation occurs in a significant minority of individuals, and removal of the adhesive tape is often uncomfortable for patients with body hair. Furthermore, there are no studies assessing the longer-term efficacy of patellar taping. In contrast, realigning PF braces may accomplish many of the mechanical effects of patellar tape, while avoiding these limitations. More specifically, PF braces are easy to apply during long-term repeated use, and are far less likely to cause skin irritation.
Given the pressing need for effective interventions for PF OA, the specific aim of this trial was to undertake a double-blind, randomized crossover clinical trial among patients with PF OA to determine whether use of a realigning PF brace for 6 weeks leads to greater pain reduction than does an equivalent period of use of the same brace without a patellar realigning strap.
Methods
Participants
From March 2006 to December 2009, we recruited persons with lateral PF OA from previous trial databases in which participants had been originally recruited from community volunteers. Participants were required to have knee pain on most days and either isolated lateral PF OA or mixed lateral PF and TF OA. Participants had skyline and bilateral standing AP radiographs during the screening phase. We used a radiographic definition of PF OA from the skyline view and adopted scoring criteria that have been previously described [31]. Briefly, individual radiographic features and overall grades of OA in the PF compartment were read according to the following schemes using the OARSI atlas; joint space narrowing (JSN) and osteophytes, both on 0–3 scales. A knee was defined as having PF OA if there was an osteophyte of severity grade ≥2 OR if there was moderate to severe JSN (grade ≥2) with concurrent grade 1 osteophyte in the PF joint [31]. We recruited persons with predominantly lateral PF OA; defined as lateral > medial patellofemoral JSN on skyline view.
PF OA was defined as compartment-specific (or isolated) if there was not concomitant TF OA. Radiographic TF OA was defined as a Kellgren and Lawrence (K/L) grade of ≥2 on the AP view [32]. Participants with concomitant TF OA (in addition to radiographic lateral PF OA) were admitted if their source of symptoms for self-reported pain location or physical examination was consistent with PF disease. The judgment was based on consideration of: (1) Which activities brought on the knee pain; pain on stair climbing and/or rising from a chair was considered typical of PF OA, whereas pain walking on level ground was considered more typical of the TF joint; (2) Where the pain was located in the knee; Pain in the posterior aspect of the knee or in the region of the pes anserine bursa was considered unlikely to be from the PF joint; and (3) Where tenderness was located on examination; Tenderness with patellar mobilization was considered typical of PF OA.
For participants in whom both knees met the eligibility criteria, we treated the more symptomatic of the two knees to optimize symptom attribution for self-reported assessments.
Exclusion criteria included:
Bed or wheelchair bound persons or persons who usually used an ambulation aid to walk, such as a cane, crutch, or walker.
Lower extremity pain emanating from the back or hip more than from the knee as determined by screening questionnaire and physical examination.
Low initial pain score on VAS (<4 out of 10) on phone screening and visit 1 screening (Note: bracing commenced after screening and randomization)
Planning to move from area within 10 months of study screening or had any extended vacation plans of more than 1 month during the study period
Symptomatic comorbid disease that limited activities more than knee pain (such as heart or lung problems) per screening questionnaire.
Receiving corticosteriod injection in the month prior to starting the trial, or hyaluronan injection in the 6-month period prior to the trial.
Bilateral total knee replacements or plan for total knee replacement in next 6 months for the signal knee.
Likely difficulty with brace fitting or brace slippage due to knee or thigh dimensions inappropriate for brace fitting (knee circumference > 55cm). Prior prescription brace use or allergies to neoprene.
Other known causes of arthritis, including rheumatoid arthritis, systemic lupus erythema, gout, psoriatic arthritis, or pseudogout as determined by self reported diagnosis.
Skin breakdown at the site where the brace was to be applied.
Failure to pass run-in test or unable to properly fit the brace during the run-in period.
Inability to complete the self-reported forms in English.
Procedures
We performed a randomized, crossover, double-blind (participant and assessor) controlled trial. It was prospectively registered with the NIH Clinical Trials Registry NCT00381563. The Boston University IRB and New England Baptist Hospital Human Research Ethics Committee approved the study and all participants provided written informed consent. IRB approval was obtained on July 13th 2006, the first participant was enrolled in December 2006 and the last participant completed the study on November 3rd 2009.
The trial included a run-in period in which there was a screening phone call, a visit two weeks later (pre-randomization screening visit), and a randomization visit 2 weeks after the initial visit. During the 2-week run-in period, participants wore a circumferential, elastic brace strap with an attached New Lifestyles NL-1000 accelerometer (New Lifestyles, Inc, Lees Summit, MO) to monitor usage. Participants were instructed to wear the brace strap for a minimum of 4 hours per day, and to record their perceived usage in a participant log[33]. After the run-in showed acceptable usage (defined as wearing brace for at least 4 hours per day) and following baseline outcome assessment, patients were randomized to receive either Treatment A or Treatment B first for 6 weeks, followed by a 6 week wash-out period before crossing over to the other treatment group (B or A) for the second 6 week period of treatment.
Randomization was performed outside of the clinic by a biostatistician and concealed from all other study investigators. Randomization was stratified by the presence or absence of x-ray TF OA and by gender, as there may be differences in symptom and disease location by gender [3]. We preserved allocation concealment by having the randomization codes held by the biostatistician external to the clinical trial operations. Group allocation was revealed from a sealed envelope to the research coordinator at the time of the randomization visit.
Intervention
The goal of this study was to evaluate the therapeutic effects of a realigning patellofemoral brace in comparison with a non-realigning placebo brace. The two treatments were: TREATMENT A (CONTROL) a BioSkin Q Brace (Cropper Medical Inc., Ashland, OR) with the realigning T strap removed and TREATMENT B (ACTIVE) the BioSkin Q Brace with the realigning T strap intact (see Figure 1). Participants were asked to wear the assigned knee brace for a minimum of 4 hours per day during the treatment period.
Figure 1.

BioSkin Q Brace with the realigning T strap intact (Figure Left). Positioning and configuration of the T strap overlying the brace delineated in red with patella aperture facing anteriorly and strap cupping the lateral aspect of the patella for application of a force to produce a medial patellar glide (Figure Right).
The Q Brace™ has an anterior aperture to admit the patella. The “T” strap has two arms that adhere medially with Velcro and has one attachment laterally. The application is intended to control the direction of traction on the patella. In particular, the strap aimed to apply a medial glide to minimize lateral movement of the patella. The brace is made of a material trademarked as Bio Skin®. Bio Skin® is an elastic, latex free, hypo-allergenic material that provides compression and moisture vapor transfer. The Q Brace can be purchased off-the-shelf in a range of sizes for different knee and thigh circumferences. In this study, fitting and positioning of the knee brace was performed by a trained investigator (KH) who also positioned and applied the “T” strap. Marks were placed on the brace to indicate where the “T” strap should be reapplied for daily use. The person teaching the participant how to correctly apply the brace was, by necessity, not blinded.
In all other respects, we attempted to conduct a blinded trial. Our description of the treatments to the participants was that we were comparing two types of braces for their PF OA without specifying which one constituted active treatment. The active and control braces were also identical apart from the application of the realigning T strap.
Trial Outcomes
All participants were evaluated by the same blinded assessor. The primary outcome was change in knee pain on the visual analogue scale (VAS) scale. Participants rated the average severity of knee pain over the previous week. Change in pain was measured on a 0–100mm horizontal VAS with terminal descriptors of (0 = no pain; 100 = maximal pain) [34]. This was assessed at baseline and at each follow-up visit (week 1, 3 and 6 of each treatment phase).
Secondary Outcomes included:
Western Ontario and McMaster Universities Arthritis Index (WOMAC) Pain Subscales (Likert form) [35] (primary treated Knee). Pain was assessed using the pain subscale of the Likert version of the WOMAC. This disease-specific measure is reliable, valid and responsive and consists of 5 pain items, 17 function items and 2 stiffness items each using a 5- point scale to score each item, where higher scores indicate worse symptoms [35].
WOMAC Function Subscale. Difficulty with physical function was assessed using the physical function subscale of the Likert version of the WOMAC.
WOMAC Stiffness Subscale Stiffness was assessed using the stiffness subscale of the Likert version of the WOMAC.
Adherence
We used a number of different methods to monitor and improve adherence. First, we screened participants during the run-in after using the brace strap and accelerometer to assess whether they were willing to wear the brace therapy for their PF OA. Second, we inquired in a detailed fashion about adherence with use of bracing and evaluated the participant’s log of brace usage at each visit. We called the participants every week during the active phases of the trial (0–6 weeks; 12–18 weeks).
Statistical Analysis
Analysis of the trial focused on the primary outcome measure, change in pain during treatment. The purpose was to estimate the effect of a realigning strap on pain reduction in comparison with a control brace. Because there were repeated assessments of the VAS and WOMAC pain scores within each treatment period, we averaged the mid-treatment (week 3 of each treatment phase) and end of treatment (week 6 of each treatment phase) pain scores to reduce the variability of assessment [36]. Based on taping studies that showed immediate effects on symptoms, we expected the effects of the PF brace to fully manifest after 3 weeks of treatment, so averaging of mid-treatment and end of treatment pain scores should not have biased estimates of treatment effect.
We performed regression analysis of the pain scale measures using a linear mixed-effect model with unstructured covariance structure for repeated measurements within participants. In these regression models, the baseline score of each phase was used as a predictor in addition to indicators of treatment and period and an interaction of treatment by period. In a two-period crossover trial, the treatment by period interaction is equivalent to the carryover effect, so this provided another method of assessing the carryover effect. The treatment effect in this analysis would have been diminished if there was a carryover effect of the first treatment. However, the washout period of six weeks between treatments was intended to remove any such carryover effect. We also used a formal statistical test to assess for carryover effect [37]. This analysis approximated an intent-to-treat approach with the last observation brought forward for missing values.
The secondary analysis of pain, function and stiffness using the WOMAC subscales proceeded in the same manner as is outlined for the pain scale above. We also performed the crossover analysis stratified by form of OA: participants with isolated PF OA in one stratum and those with TF involvement in the other stratum [38].
All statistical analyses were performed using version 9 of the SAS statistical analysis software package.
Power estimates
Based upon the results from the Hinman [19], Horlick [39] and Kirkley [40] studies of knee taping and bracing, we anticipated a conservative treatment effect difference of 30% in pain and function. We estimated a correlation of 0.6 in the primary outcome measure (VAS pain) for measures taken within a participant. In all of these calculations we used the comparison between the therapeutic tape and control tape groups. Hinman et al[19] found a significant difference between the treatments for VAS pain with a mean difference of 1.3 on a 10 cm scale.
We also planned an a priori stratified analysis for PF OA and mixed PF and TF OA to assess for differences in treatment effect between these two groups. For VAS pain in a crossover analysis, just under 45% of the participants would need to have isolated PF OA to detect a treatment difference of 0.7cm on the VAS (0–10cm scale) with 80% power (2 sided alpha, p = .05). In the analysis of all participants, a treatment difference of 0.46 in VAS pain was detectable with 80% power. To achieve 80% power to detect a difference of 0.7, 43% of participants would need to have isolated PF OA. To achieve 80% power to detect a difference of 0.9, 26% of participants must have isolated PF OA. Thus, in order to be conservative we recruited 40 persons with isolated PF OA
As we were interested in both the crossover design and phase 1 analysis, we assessed the power with 80 participants to assess difference in each. The treatment differences on a 0–10cm VAS where the power reaches 80% were as follows: difference in VAS pain detectable with cross-over analysis approach = 0.46, and difference in VAS pain detectable with period 1 analysis approach = 1.30.
Results
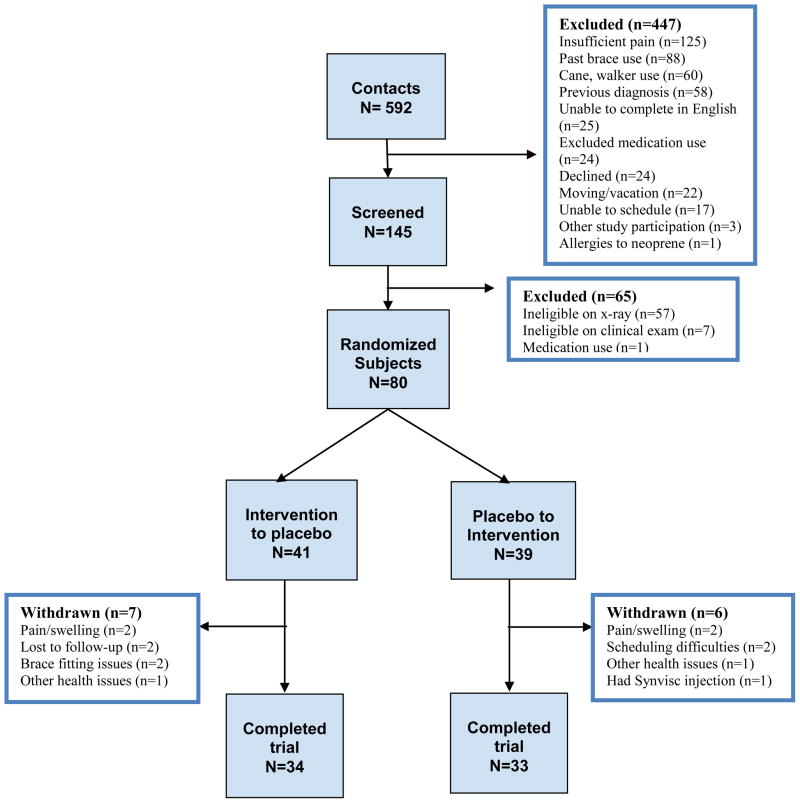
Of the 592 potential participants who were contacted by phone, 145 were eligible for a screening visit. The major reasons for ineligibility on phone screening was insufficient pain (n=125), prior brace use (n=88), current cane or walker use (n=60), and a prior diagnosis of another cause of osteoarthritis (n=58). Of the 145 participants who had a screening visit, 80 (40 with isolated PF OA and 40 with mixed PF and TF OA) were found to be eligible and were randomized. The most common reason for ineligibility at the screening visit was failure to fulfill radiographic entry criteria (n=57). Sixty seven participants (84%) completed the 18-week trial. Figure 2 shows the flow of participants through the trial.
Figure 2.
Flow chart of participants
Forty-one participants were randomized to receive the active brace first and 39 to receive the control brace first. There were no statistically significant differences in age, gender, BMI, radiographic severity or baseline VAS pain or WOMAC pain score between these two treatment order groups (Table 1). The median Kellgren and Lawrence grade and lateral PF JSN grade for the study sample signal knee were both 2. Demographic and clinical characteristics of the 13 participants who withdrew from the study did not differ substantially from those who remained (data not shown).
Table 1.
Baseline participant characteristics according to assigned initial treatment
| Characteristics | Active Brace to Control brace (n=41) | Control brace to Active brace (n=39) |
|---|---|---|
| Age, mean SD years | 60(9.7) | 61(9.1) |
| Male sex, % | 9 (22.5%) | 8 (20.5%) |
| Body mass index, mean SD kg/m2 | 27.7(12.5) | 27.4(14.0) |
| Kellgren/Lawrence grade ≥2, % | 24(58.5%) | 21(53.8%) |
| VAS† pain score, mean SD (0–100 scale) | 45.2(27.4) range: 1–100, Median: 38. |
35.4(24.8) range: 1–87, Median: 26. |
| WOMAC* pain score, mean SD (0–20 scale) | 7.8(3.6) | 7.2(3.9) |
| Kellgren and Lawrence Grade signal knee: Median {range} | 2(0–4) | 2(0–4) |
| n (%) Grade 0 | 7(17%) | 8(21%) |
| n (%) Grade 1 | 10(24%) | 10(26%) |
| n (%) Grade 2 | 6(15%) | 6(15%) |
| n (%) Grade 3 | 13(32%) | 10(26%) |
| n (%) Grade 4 | 5(12%) | 5(13%) |
| Lateral PF Joint Space Narrowing Grade signal knee: Median {range} | 2(0–3) | 2(0–3) |
| n (%) Grade 0 | 3(7%) | 3(8%) |
| n (%) Grade 1 | 17(41%) | 14(36%) |
| n (%) Grade 2 | 11(27%) | 15(38%) |
| n (%) Grade 3 | 10(24%) | 7(18%) |
VAS-Visual Analog Scale pain score at commencement of bracing
WOMAC- Western Ontario and McMaster Universities Osteoarthritis Index.
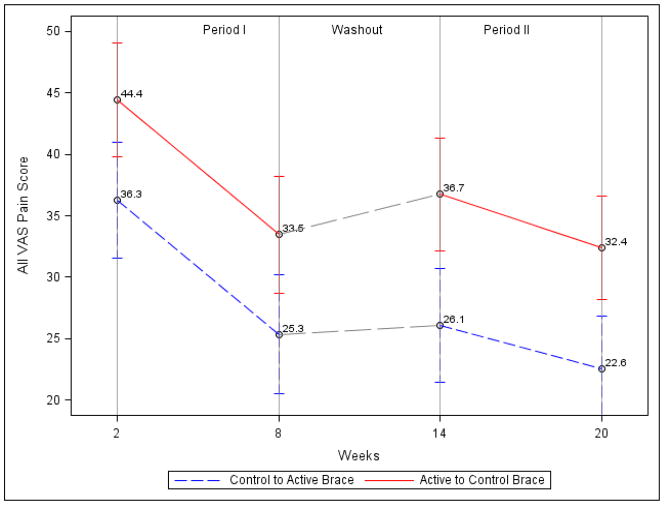
When analyzing the crossover trial findings, we first tested for treatment period and differential carryover effects (Table 2 & Figure 3). The treatment effect of the realigning strap was not significant for VAS pain with a 3.71 unit difference (95% CI−7.23, 14.65). The differential carryover was a 7.7 unit difference in the VAS pain score (P= 0.36), showing that the comparison of treatment efficacy was not significantly different if the patients were randomized to the active or control brace first. Therefore, we removed the carryover term from the model. In Model 2, after excluding the differential carryover effect and adjusting for baseline pain score, the active intervention had no significant effect on VAS pain with a −0.7 unit (−0.07cm) difference (95% CI: −6.2, 4.8 units; p=0.81). The study was powered to detect a 0.7cm on the VAS (0–10cm scale) which is still less than that which is clinically significant [41,42].
Table 2.
| Table 2a. Predictors of VAS pain scores during the crossover trial* | ||
|---|---|---|
| Predictor | Model 1 | Model 2 |
| Baseline VAS pain score (95% confidence interval) | 0.55 (0.41, 0.68) | 0.56 (0.43, 0.69) |
| p-value | <0.0001 | <0.0001 |
| Treatment (95% confidence interval) | 3.71 (−7.23, 14.65) | −0.68 (−6.20,4.84) |
| p-value | 0.5010 | 0.8055 |
| Treatment, period 1 vs. period 2 (95% confidence interval) | 0.89 (−9.33,11.11) | −3.06 (−8.82, 2.71) |
| p-value | 0.8627 | 0.2934 |
| Period by treatment interaction † (95% confidence interval) | 7.70 (−8.89, 24.29) | |
| p-value | 0.3573 | |
| Table 2b. Predictors of WOMAC pain scores during the crossover trial* | ||
|---|---|---|
| Predictor | Model 1 | Model 2 |
| Baseline WOMAC pain score (95% confidence interval) | 0.56 (0.43, 0.69) | 0.58 (0.45, 0.71) |
| p-value | <0.0001 | <0.0001 |
| Treatment (95% confidence interval) | 1.33 (−0.22, 2.88) | 0.11 (−0.66, 0.88) |
| p-value | 0.0912 | 0.7744 |
| Treatment, period 1 vs. period 2 (95% confidence interval) | 1.24 (−0.19, 2.67) | 0.16 (−0.62, 0.94) |
| p-value | 0.0877 | 0.6883 |
| Period by treatment interaction † (95% confidence interval) | 2.17 (−0.24, 4.57) | |
| p-value | 0.0769 | |
| Table 2c. Predictors of WOMAC function scores during the crossover trial* | ||
|---|---|---|
| Predictor | Model 1 | Model 2 |
| Baseline WOMAC function score (95% confidence interval) | 0.80 (0.69, 0.92) | 0.81 (0.70, 0.92) |
| p-value | <0.0001 | <0.0001 |
| Treatment (95% confidence interval) | 0.70 (−4.62, 6.01) | −0.02 (−2.83,2.79) |
| p-value | 0.7943 | 0.9878 |
| Treatment, period 1 vs. period 2 (95% confidence interval) | −1.01 (−5.59, 3.57) | −1.57 (−4.59, 1.46) |
| p-value | 0.6620 | 0.3056 |
| Period by treatment interaction † (95% confidence interval) | 1.10 (−5.74, 7.93) | |
| p-value | 0.7499 | |
| Table 2d. Predictors of WOMAC stiffness scores during the crossover trial* | ||
|---|---|---|
| Predictor | Model 1 | Model 2 |
| Baseline WOMAC stiffness score (95% confidence interval) | 0.65 (0.52, 0.78) | 0.67 (0.54, 0.80) |
| p-value | <0.0001 | <0.0001 |
| Treatment (95% confidence interval) | 0.23 (−0.49, 0.95) | −0.11 (−0.53, 0.32) |
| p-value | 0.5293 | 0.6129 |
| Treatment, period 1 vs. period 2 (95% confidence interval) | 0.26 (−0.39, 0.91) | −0.02 (−0.46, 0.42) |
| p-value | 0.4256 | 0.9314 |
| Period by treatment interaction † (95% confidence interval) | 0.55 (−0.41, 1.51) | |
| p-value | 0.2548 | |
Values for model predictors are beta coefficients. For treatment as a predictor, a value of x means that active treatment was associated with a x lower score on the VAS pain scale compared with control treatment. An unstructured correlation matrix for observations within participants was used in generalized estimating equation fitting of the marginal model (1). Model 2 was conducted with exclusion of the differential carryover effect.
Tests whether treatment effects differed according to use in period 1 or period 2, constituting the differential carryover effect.
Figure 3.
Interaction between treatment and period effect for VAS Pain.
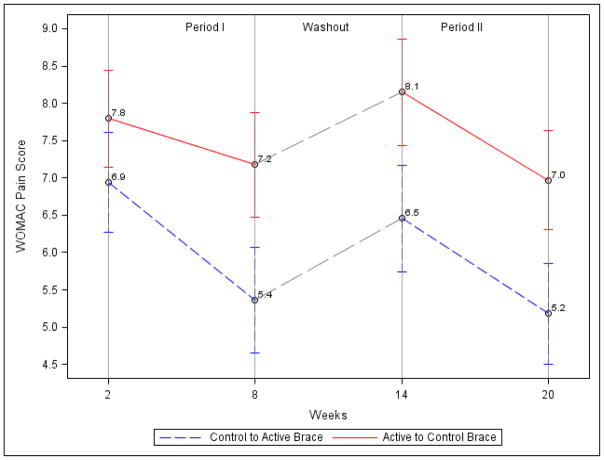
Further examination of the effects of PF bracing on WOMAC pain (Table 2b and Figure 4), WOMAC Function (Table 2c) and WOMAC Stiffness (Table 2d) revealed similar results with no significant carryover effect and no significant treatment effect. In Model 2, after excluding the differential carryover effect and adjusting for baseline WOMAC pain score, the active intervention had no significant effect on WOMAC pain with a −0.11 unit difference (95% CI: −0.66, 0.88 units; p=0.77). Similar effects were seen for WOMAC function −0.02 unit difference (95% CI: −2.83, 2.79 units; p=0.99) and WOMAC stiffness −0.11 unit difference (95% CI: −0.53, 0.32 units; p=0.61).
Figure 4.
Interaction between treatment and period effect for WOMAC Pain.
Table 3 shows that the average participant was adherent (self-reported from diary) with a mean of 4.8 hours per day of use in the active brace and 4.3 hours per day for the control brace. Most participants wore the brace for more than 3 hours per day. The adverse events were generally minimal with no substantive differences between interventions. However, 4 of the people who withdrew from the study cited increased knee pain and/or foot/ ankle swelling and 2 people withdrew due to fitting issues. None of the remaining participants who experienced an adverse event in the trial required either increased analgesia or withdrawal of the brace.
Table 3.
Adherence to and side effects of treatment
| Active brace | Control brace | |
|---|---|---|
| Adherence, mean SD hours of wear/day from self report in diary | ||
| Period 1 Mean(SD) | 4.77(2.07) | 4.32(2.28) |
| n (%) <1 hr | 1(3%) | 3(9%) |
| n (%) 1–2 hrs | 1(3%) | 2(6%) |
| n (%) 2–3 hrs | 3(9%) | 1(3%) |
| n (%) 3–4 hrs | 6(18%) | 9(27%) |
| n (%) 4–5 hrs | 9(27%) | 7(21%) |
| n (%) 5+ hrs | 13(39%) | 11(33%) |
| Period 2 Mean(SD) | 4.36(1.85) | 4.13(1.99) |
| n (%) <1 hr | 1(3%) | 2(6%) |
| n (%) 1–2 hrs | 2(6%) | 2(6%) |
| n (%) 2–3 hrs | 2(6%) | 2(6%) |
| n (%) 3–4 hrs | 9(28%) | 13(40%) |
| n (%) 4–5 hrs | 10(31%) | 4(13%) |
| n (%) 5+ hrs | 8(25%) | 9(28%) |
| Side effect, no. of patients | ||
| Brace slipping | 2 | 2 |
| Brace rubbing/irritation | 3 | 3 |
| Foot/ankle swelling | 4 | 3 |
| Increased knee pain | 4 | 2 |
| Other | 2 | 2 |
Additional analyses limited to phase 1, determining the effect of isolated PF OA vs. mixed PF and TF OA, in addition to effects of gender showed results consistent with those already presented and are not further presented here.
Discussion
The development of efficacious, conservative, non-pharmacologic treatment approaches that are capable of ameliorating the symptoms and improving the structure of knee OA is an important research objective [43]. Despite their current under-emphasis in clinical trials and practice, therapies targeting the pathomechanics of OA are likely to be efficacious [44]. Unfortunately, we have not found any therapeutic clinical effects from the application of a brace with a realigning strap designed to improve PF alignment in persons with lateral PF OA compared with an identical brace without the realigning strap. Although participants were adherent to the intervention in this trial and the application of the brace was generally well-tolerated, there was little therapeutic benefit to be gained by the addition of a realigning strap to the brace.
The underlying aim of this study was to assess the patellar realigning effect of the strap on symptoms. The rationale behind this is that people with lateral PF OA have altered alignment (including lateral displacement and tilt) and that this maltracking is associated with symptoms [18]. Hence if we were to correct maltracking, we should see a reduction in symptoms. This trial demonstrated that the addition of a realigning strap did not lead to a reduction of symptoms compared to the same brace without the strap. There are a number of possible reasons why this may be the case and why we have found no significant treatment effect in this trial.
Prior studies have demonstrated that knee taping improves pain [30], but it is not clear that the mechanism involves a substantive change in patellofemoral alignment. Despite numerous investigations of the potential mechanism of the therapeutic effect of taping and bracing in patellofemoral pain syndrome, a condition thought to result from maltracking of the patella, the reasons for a favorable influence of both taping and bracing on symptoms remains unclear [21–28]. Some of these studies [23,24], using dynamic MRI to visualize PF kinematics in persons with patellofemoral pain syndrome, have suggested that bracing may improve joint contact area and as a consequence reduce PF joint stress. However, these studies [23,24] were in younger persons with patellofemoral pain syndrome and thus they are not immediately generalizable to persons with PF OA. Crossley et al [45] conducted the only study evaluating effects of taping on patella alignment in people with OA and showed that changes in patellar alignment occurred immediately following tape application. Whether these changes persist following prolonged use of the tape when stretching and loosening is likely to occur is not known.
This said, the relation between PF alignment and pain has been demonstrated in a number of studies but is not strong in any of them [18]. Thus if one were able to modify PF alignment with application of a realigning strap (such as in this study) it may have little influence on symptoms.
It may be that the application of the realigning strap was not successful in improving contact area and reducing joint stress. The aperture on this brace for positioning of the patella was quite small. As such, it is possible that the brace alone without the strap actually applied compressive force to the anterior aspect of the patella, increasing retropatellar contact force and, in so doing, mitigating any reduction in symptoms.
It is important that we clearly state that we have demonstrated that the application of this specific brace was no more effective than the control brace in relieving symptoms for people with PF OA. This does not reflect any potential benefit in persons with PF pain from other causes nor for other types of PF braces.
There are a number of limitations of this study that warrant description. There was no control group without a brace for comparison to the intervention because of concerns about unblinding. Prior research has highlighted the difficulty of disentangling the placebo effect in non-pharmacologic clinical trials [46–48]. Consistent with this prior research, participants in our trial demonstrated improvements in symptoms during both the control period (brace without a realigning strap) and the active intervention period (brace with the realigning strap), but we were unable to detect a significant difference between the two treatment periods. 13 (16%) participants dropped out of the study potentially leading to a loss of statistical power and introducing the potential that the null study findings and conclusions may be due to type-2 error. We also lacked sufficient power to stratify based on severity of lateral PF joint space narrowing at baseline to see if there was differential benefit. The variability of the outcomes in this study, reflected in the wide confidence intervals for the main effect indicates some uncertainty in the outcome. The principal finding did not detect a suggestion of a treatment effect with the active intervention having no significant effect on VAS pain with only −0.7 units (0.07cm) difference (95% CI: −6.2, 4.8 units or −0.62cm to 0.48cm). This treatment difference is much smaller than that which is clinically relevant. According to Angst, a clinically relevant difference in VAS pain is 1.2cm or 12 units [41,42]. The attribution of symptoms to the PF or TF joint is challenging and our classification of those with predominant PF involvement could lead to misclassification. Lastly, the daily duration of treatment required to mechanically re-align the patella is unknown, and therefore the prescribed 4 hours of daily use in this study was largely arbitrary. In the clinic, braces are often prescribed for use only during aggravating weight bearing activity as opposed to a set time of 4 hours per day. Furthermore, we do not know if the patient population in this study had PF malalignment.
Another possible reason for not finding an effect of bracing is that the primary outcome measure may not have been responsive enough to detect changes in knee pain among persons with PF OA. Our primary outcome was a global measure of knee pain during the previous week. It is possible that a change in pain would have been more evident if pain had been rated only when people were wearing the brace, or if pain had been rated only during weight-bearing activities when the mechanical effects of the brace are most likely. Further some of the participants pain at the time of study commencement (as opposed to at time of phone and visit screening) was less than 4 on the 0–10 VAS scale potentially mitigating detecting a treatment effect.
Given prior studies demonstrating a positive effect of taping, it is interesting to theorize as to why braces would not work to a similar extent. We assumed that the realigning strap would have a similar mechanical effect to taping (the application of a medially directed force). There are some differences in the studies of taping to our bracing study that may lead to differences in the effects seen during these reported trials [19,20,30,45]. Tape was left on full-time for a week so it is unlikely that there is a lasting force once the tape stretches and loosens within the first day. In contrast, the brace was used ~4 hours per day, during which time the applied force is likely to be nearly continuous with use. Despite educating participants about the appropriate application of the brace and assessing performance at each study visit, repeat donning of the brace at home may not have been consistent. In contrast, once the tape is applied it remains on and in that position until removed. Our study selectively recruited persons with PF OA whereas the prior PF taping studies in OA recruited persons with OA in any portion of the knee joint. However this should have led to a more favorable opportunity for our trial to have detected an effect. Perhaps other features of the application of tape, including the individualized application of tape by a trained therapist and the potential to reduce fat pad impingement by taping may also be helpful.
There are also a number of important strengths of this study that merit mentioning. All participants had meaningful symptoms at baseline, suggesting an opportunity for detecting a real treatment effect if there was a treatment effect to be detected. Similarly, this study was adequately powered to detect a clinically meaningful treatment effect on the primary outcome measure. In addition, we specifically recruited only persons with PF OA into this study cohort using stringent selection criteria. Other studies of patellar taping have recruited persons with tibiofemoral OA. Finally, the crossover design of this trial facilitated both efficient recruitment and strong protection against bias due to patient-related factors.
In conclusion, this study did not demonstrate measurable clinical significance of a realigning strap on a patellofemoral brace in reducing pain among persons with lateral PF OA. This trial represents the results of a test of one brace in persons with lateral PF OA and does not mitigate the potential for other PF braces to have a therapeutic effect on this disease.
Acknowledgments
We would like to thank the participants involved in the study, without whom this trial would not have been possible. We would also like to thank the staff responsible for coordinating the study. We would like to thank Cropper Medical for providing the knee braces used in this trial. Cropper was not involved in study design and played no role in writing or editing this manuscript. The trial was supported by 2 P60 AR047785. Dr Hunter and Dr Bennell are funded by Australian Research Council Future Fellowships.
Supported by NIH AR47785
Footnotes
Conflict of Interest Statement
The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication. The manuscript has not been submitted or is not simultaneously being submitted elsewhere, and no portion of the data has been or will be published in proceedings or transactions of meetings or symposium volumes.
There are no financial interests, direct or indirect, that might affect the conduct or reporting of the work submitted. The manuscript has been read and approved by all the authors, the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
Author Contributions
DJH conceived and designed the study, supervised its conduct, drafted the manuscript and takes responsibility for the integrity of the work as a whole, from inception to finish. KDG, WH, DTF, PM and KB were also involved in the design of the study. All authors contributed to acquisition of the data and its interpretation. All authors critically revised the manuscript and gave final approval of the article for submission.
NIH Clinical Trials Registry NCT00381563
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Ledingham J, Regan M, Jones A, Doherty M. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Annals of the Rheumatic Diseases. 1993;52:520–526. doi: 10.1136/ard.52.7.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duncan RC, Hay EM, Saklatvala J, Croft PR. Prevalence of radiographic osteoarthritis--it all depends on your point of view. Rheumatology (Oxford) 2006;45:757–760. doi: 10.1093/rheumatology/kei270. [DOI] [PubMed] [Google Scholar]
- 3.McAlindon TE, Snow S, Cooper C, Dieppe PA. Radiographic patterns of osteoarthritis of the knee joint in the community: the importance of the patellofemoral joint. Annals of the Rheumatic Diseases. 1992;51:844–849. doi: 10.1136/ard.51.7.844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lanyon P, O’Reilly S, Jones A, Doherty M. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Annals of the Rheumatic Diseases. 1998;57:595–601. doi: 10.1136/ard.57.10.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. How do pain and function vary with compartmental distribution and severity of radiographic knee osteoarthritis? Rheumatology (Oxford) 2008;47:1704–1707. doi: 10.1093/rheumatology/ken339. [DOI] [PubMed] [Google Scholar]
- 6.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage. 2009;17:1151–1155. doi: 10.1016/j.joca.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 7.Cooper C, McAlindon T, Snow S, Vines K, Young P, Kirwan J, et al. Mechanical and constitutional risk factors for symptomatic knee osteoarthritis: differences between medial tibiofemoral and patellofemoral disease. Journal of Rheumatology. 1994;21:307–313. [PubMed] [Google Scholar]
- 8.Elahi S, Cahue S, Felson DT, Engelman L, Sharma L. The association between varus-valgus alignment and patellofemoral osteoarthritis. Arthritis & Rheumatism. 2000;43:1874–1880. doi: 10.1002/1529-0131(200008)43:8<1874::AID-ANR25>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 9.Cicuttini FM, Spector T, Baker J. Risk factors for osteoarthritis in the tibiofemoral and patellofemoral joints of the knee. Journal of Rheumatology. 1997;24:1164–1167. [PubMed] [Google Scholar]
- 10.Hirokawa S. Biomechanics of the knee joint: a critical review. [Review] [119 refs] Critical Reviews in Biomedical Engineering. 1993;21:79–135. [PubMed] [Google Scholar]
- 11.Grelsamer RP, Weinstein CH. Applied biomechanics of the patella. [Review] [39 refs] Clinical Orthopaedics & Related Research. 2001:9–14. doi: 10.1097/00003086-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clinical Orthopaedics & Related Research. 1979:9–15. [PubMed] [Google Scholar]
- 13.Grelsamer RP. Patellar malalignment. [Review] [191 refs] Journal of Bone & Joint Surgery. 2000;82-A:1639–1650. [PubMed] [Google Scholar]
- 14.Ficat RP, Hungerford DS. Disorders of the Patello-femoral Joint. Baltimore: The Williams and Wilkins Co; 1977. [Google Scholar]
- 15.Harrison MM, Cooke TD, Fisher SB, Griffin MP. Patterns of knee arthrosis and patellar subluxation. Clinical Orthopaedics & Related Research. 1994:56–63. [PubMed] [Google Scholar]
- 16.Iwano T, Kurosawa H, Tokuyama H, Hoshikawa Y. Roentgenographic and clinical findings of patellofemoral osteoarthrosis. With special reference to its relationship to femorotibial osteoarthrosis and etiologic factors. Clinical Orthopaedics & Related Research. 1990:190–197. [PubMed] [Google Scholar]
- 17.Fujikawa K, Seedhom BB, Wright V. Biomechanics of the patello-femoral joint. Part II: A study of the effect of simulated femoro-tibial varus deformity on the congruity of the patello-femoral compartment and movement of the patella. Engineering in Medicine. 1983;12:13–21. doi: 10.1243/emed_jour_1983_012_005_02. [DOI] [PubMed] [Google Scholar]
- 18.Kalichman L, Zhu Y, Zhang Y, Niu J, Gale D, Felson DT, et al. The association between patella alignment and knee pain and function: an MRI study in persons with symptomatic knee osteoarthritis. Osteoarthritis Cartilage. 2007;15:1235–1240. doi: 10.1016/j.joca.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 19.Hinman RS, Crossley KM, McConnell J, Bennell KL. Efficacy of knee tape in the management of osteoarthritis of the knee: blinded randomised controlled trial. [see comment] BMJ. 2003;327:135. doi: 10.1136/bmj.327.7407.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cushnaghan J, McCarthy C, Dieppe P. Taping the patella medially: a new treatment for osteoarthritis of the knee joint? BMJ. 1994;308:753–755. doi: 10.1136/bmj.308.6931.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Powers CM, Ward SR, Chen YJ, Chan LD, Terk MR. The effect of bracing on patellofemoral joint stress during free and fast walking. American Journal of Sports Medicine. 2004;32:224–231. doi: 10.1177/0363546503258908. [DOI] [PubMed] [Google Scholar]
- 22.Powers CM, Ward SR, Chen YJ, Chan LD, Terk MR. Effect of bracing on patellofemoral joint stress while ascending and descending stairs. Clinical Journal of Sport Medicine. 2004;14:206–214. doi: 10.1097/00042752-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Powers CM, Ward SR, Chan LD, Chen YJ, Terk MR. The effect of bracing on patella alignment and patellofemoral joint contact area. Medicine & Science in Sports & Exercise. 2004;36:1226–1232. doi: 10.1249/01.mss.0000132376.50984.27. [DOI] [PubMed] [Google Scholar]
- 24.Draper CE, Besier TF, Santos JM, Jennings F, Fredericson M, Gold GE, et al. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J Orthop Res. 2009;27:571–577. doi: 10.1002/jor.20790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Powers CM, Doubleday KL, Escudero C. Influence of patellofemoral bracing on pain, knee extensor torque, and gait function in females with patellofemoral pain. Physiother Theory Pract. 2008;24:143–150. doi: 10.1080/09593980701665793. [DOI] [PubMed] [Google Scholar]
- 26.Bohnsack M, Halcour A, Klages P, Wilharm A, Ostermeier S, Ruhmann O, et al. The influence of patellar bracing on patellar and knee load-distribution and kinematics: an experimental cadaver study. Knee Surg Sports Traumatol Arthrosc. 2008;16:135–141. doi: 10.1007/s00167-007-0428-3. [DOI] [PubMed] [Google Scholar]
- 27.Selfe J, Richards J, Thewlis D, Kilmurray S. The biomechanics of step descent under different treatment modalities used in patellofemoral pain. Gait Posture. 2008;27:258–263. doi: 10.1016/j.gaitpost.2007.03.017. [DOI] [PubMed] [Google Scholar]
- 28.Shellock FG, Mullin M, Stone KR, Coleman M, Crues JV. Kinematic Magnetic Resonance Imaging of the Effect of Bracing on Patellar Position: Qualitative Assessment Using an Extremity Magnetic Resonance System. J Athl Train. 2000;35:44–49. [PMC free article] [PubMed] [Google Scholar]
- 29.Cicuttini FM, Baker J, Hart DJ, Spector TD. Association of pain with radiological changes in different compartments and views of the knee joint. Osteoarthritis & Cartilage. 1996;4:143–147. doi: 10.1016/s1063-4584(05)80323-1. [DOI] [PubMed] [Google Scholar]
- 30.Warden SJ, Hinman RS, Watson MA, Jr, Avin KG, Bialocerkowski AE, Crossley KM. Patellar taping and bracing for the treatment of chronic knee pain: a systematic review and meta-analysis. [Review] [49 refs] Arthritis & Rheumatism. 2008;59:73–83. doi: 10.1002/art.23242. [DOI] [PubMed] [Google Scholar]
- 31.Felson DT, McAlindon TE, Anderson JJ, Naimark A, Weissman BW, Aliabadi P, et al. Defining radiographic osteoarthritis for the whole knee. Osteoarthritis & Cartilage. 1997;5:241–250. doi: 10.1016/s1063-4584(97)80020-9. [DOI] [PubMed] [Google Scholar]
- 32.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis & Rheumatism. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 33.Findings from the aspirin component of the ongoing Physicians’ Health Study. New England Journal of Medicine. 1988;318:262–264. doi: 10.1056/NEJM198801283180431. [DOI] [PubMed] [Google Scholar]
- 34.Huskisson EC. Measurement of pain. Lancet. 1974;2:1127–1131. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 35.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. Journal of Rheumatology. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 36.Pincus T, Koch GG, Sokka T, Lefkowith J, Wolfe F, Jordan JM, et al. A randomized, double-blind, crossover clinical trial of diclofenac plus misoprostol versus acetaminophen in patients with osteoarthritis of the hip or knee. [see comments] Arthritis & Rheumatism. 2001;44:1587–1598. doi: 10.1002/1529-0131(200107)44:7<1587::AID-ART282>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 37.Senn S. Cross-over Trials in Clinical Research. In: Piantadosi S, editor. Clinical Trials: A Methodologic Perspective. New York: Wiley and Sons; 1997. [Google Scholar]
- 38.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. [Review] [6 refs] BMJ. 2003;326(7382):219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Horlick S, Loomer R. Valgus knee bracing for medial gonarthrosis. Clinical Journal of Sport Medicine. 1993;3:251–255. [Google Scholar]
- 40.Kirkley A, Webster-Bogaert S, Litchfield R, Amendola A, MacDonald S, McCalden R, et al. The effect of bracing on varus gonarthrosis. Journal of Bone & Joint Surgery. 1999;81:539–548. doi: 10.2106/00004623-199904000-00012. [DOI] [PubMed] [Google Scholar]
- 41.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45:384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 42.Angst F, Aeschlimann A, Michel BA, Stucki G. Minimal clinically important rehabilitation effects in patients with osteoarthritis of the lower extremities. J Rheumatol. 2002;29:131–138. [PubMed] [Google Scholar]
- 43.Buckwalter JA, Stanish WD, Rosier RN, Schenck RC, Jr, Dennis DA, Coutts RD. The increasing need for nonoperative treatment of patients with osteoarthritis. [Review] [91 refs] Clinical Orthopaedics & Related Research. 2001:36–45. doi: 10.1097/00003086-200104000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Andriacchi TP, Mundermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. A framework for the in vivo pathomechanics of osteoarthritis at the knee. [Review] [101 refs] Annals of Biomedical Engineering. 2004;32:447–457. doi: 10.1023/b:abme.0000017541.82498.37. [DOI] [PubMed] [Google Scholar]
- 45.Crossley KM, Marino GP, Macilquham MD, Schache AG, Hinman RS. Can patellar tape reduce the patellar malalignment and pain associated with patellofemoral osteoarthritis? Arthritis Rheum. 2009;61:1719–1725. doi: 10.1002/art.24872. [DOI] [PubMed] [Google Scholar]
- 46.Boutron I, Tubach F, Giraudeau B, Ravaud P. Blinding was judged more difficult to achieve and maintain in nonpharmacologic than pharmacologic trials. Journal of Clinical Epidemiology. 2004;57:543–550. doi: 10.1016/j.jclinepi.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 47.Boutron I, Guittet L, Estellat C, Moher D, Hrobjartsson A, Ravaud P. Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med. 2007;4:e61. doi: 10.1371/journal.pmed.0040061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148:295–309. doi: 10.7326/0003-4819-148-4-200802190-00008. [DOI] [PubMed] [Google Scholar]