Abstract
Predictors of multiple dimensions of spirituality/religiosity (S/R) and adolescents' preferences for having S/R (e.g., prayer) addressed in hypothetical medical settings were assessed in a sample of urban adolescents with asthma. Of the 151 adolescents (mean age = 15.8, 60% female, 85% African-American), 81% said that they were religious and spiritual, 58% attended religious services in the past month, and 49% prayed daily. In multivariable models, African-American race/ethnicity and having a religious preference were associated with higher levels of S/R (R2 = 0.07–0.25, P < .05). Adolescents' preferences for including S/R in the medical setting increased with the severity of the clinical situation (P < .05).
Keywords: Religion, Spirituality, Asthma, Adolescents, African-American
Asthma is a chronic inflammatory airway disorder that is characterized by airway obstruction, airway inflammation, and airway hyper responsiveness (Guill 2004). As the most common chronic disease in childhood and adolescence, asthma affects an estimated 5 million children under the age of 18 in the United States (United States Environmental Protection Agency 2010). Adolescents with asthma are at greater risk for impaired health-related quality of life (HRQOL), behavioral difficulties, poor school performance, and depression than their healthy peers (Bennet 1994; Forrest et al. 1997; McQuaid et al. 2001; Merikallio et al. 2005). More specifically, African-American adolescents have a disproportionately greater asthma prevalence rate than their counterparts (Akinbami and Schoendorf 2002), have higher rates of hospitalization due to asthma (Akinbami 2006), and as such are at greater risk for adverse outcomes (Akinbami, 2006).
Spirituality/religiosity (S/R) is a multidimensional construct that can incorporate the internal, personal, and emotional expression of the sacred (e.g., peace/comfort derived from faith) and the formal, institutional, and outward expression (e.g., attending religious services) of the sacred (Koenig et al. 2001). Various dimensions of S/R have been differentially related to health outcomes. For example, existential well-being (life's meaning and purpose), more so than religious well-being (one's relationship with God/a Higher Power), has been shown to be correlated with health outcomes (Cotton et al. 2005). Multiple authors have recently called for assessing S/R using a multidimensional approach (Buck et al. 2009; Hill et al. 2002; Nicholson 2010), as it allows for a more precise understanding of how S/R impacts health, ultimately leading to more targeted interventions.
While numerous studies have documented the generally salutary effects of S/R on health outcomes in healthy adolescent samples (Benson et al. 2003; Bridges and Moore 2002; Cotton et al. 2006), few have examined S/R in adolescents with a chronic illness, such as asthma (Benore et al. 2008; Pendleton et al. 2002). Given the greater risk of emotional, behavioral, and school-related problems in adolescents with asthma relative to their healthy peers (McQuaid and Walders 2003), research examining possible protective factors such as S/R in this population is critical. While African-American adults have reported using S/R to find meaning in times of hardship (Mattis 2002) and to help cope with a chronic illness such as cancer (Potts 1996), little is known about how urban African-American adolescents may use S/R to cope with having asthma (Benore et al. 2008). Given the salience of S/R in the African-American community (Koenig et al. 2001) and in urban communities (Koenig et al. 2001), understanding the relevance of S/R in this population is pertinent.
A related issue concerns the role of S/R in the clinical encounter. Studies of adults with a chronic condition have found that some patients want S/R addressed in the medical setting (Ehman et al. 1999; King and Bushwick 1994; MacLean et al. 2003; McCord et al. 2004). Depending on the situation, 33–70% of adults think that physicians should consider the patient's spiritual needs (King and Bushwick 1994; MacLean et al. 2003; Oman and Thoresen 2006). Maclean and colleagues found that the more severe the clinical scenario, the more likely it is for adult patients to prefer that their physician pray with them: 19% in an office visit versus 50% if the patient were dying (MacLean et al. 2003). To our knowledge, these types of data have not yet been reported in any samples of adolescents, though they may be particularly relevant in an urban chronically ill sample. Identifying those patients for whom S/R issues are especially important and relevant will provide health care providers with additional data to inform prevention efforts and clinical interactions.
Therefore, the goals of this study were: (1) to characterize multiple dimensions of S/R in urban adolescents with asthma and to examine associations between S/R and demographic and clinical characteristics and (2) to assess whether these adolescents want to have their S/R issues addressed in various hypothetical clinical scenarios. We hypothesized that greater levels of S/R would be associated with being African-American, being female (The Stronger Sex—Spiritually Speaking 2009), and having greater disease severity. Based on previous studies in adults (Lauckhaupt et al. 2005; MacLean et al. 2003), we also hypothesized that as the intensity of the clinical situation increased, adolescents would be more likely to want S/R incorporated into their encounters with providers. Finally, given the integral role S/R has within the African-American community, we hypothesized that African-Americans would be more likely to endorse wanting their S/R addressed in the medical setting when compared with non-African-Americans.
Methods
Procedure
From January 2008 to November 2009, we recruited 151 adolescents with various levels of asthma severity to participate in a larger longitudinal study about spiritual coping and health-related quality of life. Adolescents were recruited from the teen health center of a large Midwestern children's medical center. The medical center's institutional review board approved all study procedures. Inclusion criteria were a confirmed diagnosis of asthma, ages 11–19, and ability to read English. Eligibility was confirmed by the adolescent's provider and eligible adolescents were approached following their appointment at the teen health center. Prior to study participation, appropriate consent and/or assent was obtained. All 18-year-old participants provided informed consent. For participants under 18, parental consent and adolescent assent were obtained. A research assistant then administered questionnaires to participants following their clinic visit or during another pre-arranged time. Participants were compensated $25 for their time and travel.
Measures
Demographic and clinical data were collected via patient interviews and a clinic provider. Demographic data included age, sex, race/ethnicity, education level, parental education level (for the more highly educated primary caregiver), insurance status (as a proxy for socioeconomic status), and the adolescent's religious preference. Providers rated asthma severity at the time of the study visit according to the National Heart, Lung, and Blood Institute criteria (National Heart Lung and Blood Institute 2007).
Outcome Variables
In order to assess the multidimensional nature of S/R factors in adolescents (Hill et al. 2002), a variety of S/R measures were used. Though developed for use in adults, recent studies have used S/R measures in adolescents and obtained acceptable psychometric properties (Cotton et al. 2009a, b; Harris et al. 2008; The Institute for Social Research University of Michigan 2010).
Spirituality was assessed using the Functional Assessment of Chronic Illness Therapy-Spirituality (FACIT-Sp) scale (Peterman et al. 2002), a 12-item measure of spirituality with validated subscales for Faith (4 items; Cronbach's α = 0.88 in this sample) and Meaning and Peace (8 items; Cronbach's α = 0.81). Responses are scored on a 5-point Likert scale. Total scores can range from 0 to 48, with higher scores indicating greater levels of spirituality. Internal consistency for the overall score in this sample was good (α = 0.78).
Religious/spiritual coping was assessed using the 14-item Brief RCOPE, which consists of 7 positive and 7 negative religious coping items. Positive religious coping includes items such as seeking spiritual support. Negative religious coping includes items such as punishing God reappraisals. Respondents indicated, on a 4-point Likert scale, how much or how frequently they use the particular method of coping with their asthma. Psychometric properties for this sample were adequate (Positive RCOPE, α = 0.88; Negative RCOPE, α = 0.81).
Spiritual well-being was assessed using the 10-item version of the Spiritual Well-Being Scale (SWBS) and its two subscales, religious well-being (RWB), defined as “the strength of one's relationship with God,” and existential well-being (EWB), “a sense of satisfaction and purpose in life” (Paloutzian and Ellison 1991; Rubin et al. 2009). Participants responded to items on a 5-point Likert scale. Possible subscale scores range from 10 to 50, with higher scores representing greater levels of spiritual well-being. In our study, Cronbach's α values for the EWB and RWB subscales were 0.75 and 0.79, respectively.
Daily spiritual experiences and spiritual meaning were assessed using two subscales from the Brief Multidimensional Measure of Religiousness/Spirituality (BMMRS Fetzer Institute/National Institute on Aging Working Group 1999). Both subscales are rated on Likert scales with higher scores indicating stronger endorsement of the construct. Internal consistency for the two subscales in our sample was adequate (daily spiritual experiences, α = 0.91; spiritual meaning, α = 0.72).
Religiosity was assessed via seven items including: religious attendance, frequency of prayer and meditation, importance of religion, belief in God/a Higher Power, and self-rated religiousness and spirituality (Cotton et al. 2005). All items were measured on a 6-point Likert scale.
Clinical encounter preferences (CEP) regarding S/R in hypothetical clinical encounters were assessed using a 25-item questionnaire compiled from previous studies of adults (MacLean et al. 2003; McCord et al. 2004). Items were minimally modified for this study. For example, the McCord et al. (2004) study included several items assessing participant reasons for wanting physician–patient discussion surrounding S/R issues. One such item stated “…so that the doctor can understand how your beliefs influence how you deal with being sick” (p. 359). To make this item and the other items more relevant to adolescents with asthma, the phrase “with being sick” (and “your illness” in similar items) was modified to state “asthma or other illness”. Additionally, the term “doctor” was changed to state “provider” (which was further defined as “your doctor or nurse/nurse practitioner”).
Twelve items asked the adolescent to rate on a 5-point Likert scale (“strongly agree” to “strongly disagree”), how much he or she agreed with the incorporation of S/R issues into hypothetical medical settings. Sample questions included: “My provider should not play a role in my spiritual or religious life”, and “If I am dying, my provider should say a silent prayer for me”. If the participant wanted his/her provider to be aware of his/her S/R beliefs, participants were asked six follow-up questions to better understand his/her answer. These 6 items were also rated on a 5-point Likert scale (“strongly agree” to “strongly disagree”) and included questions such as “Is it so that your provider could understand you better?” The other 6 items were yes/no questions (with blanks provided for participants who answered “yes” to write in more detailed responses) and asked about actual experiences such as: “Can you think of a situation where your spiritual or religious beliefs influenced how you dealt with a health care decision?” Each item was analyzed individually (rather than as part of a sum score).
Statistical Analyses
Descriptive statistics including means and standard deviations were calculated for each variable. Items that were dichotomized for purposes of analyses included: religious affiliation (yes/no), African-American race/ethnicity (yes/no), and insurance status (yes/no). Given our study aims, responses on the clinical encounter preferences questions were collapsed to yield the following three categories: agreement (agree or strongly agree), neutral, and disagreement (disagree or strongly disagree). As we were interested in testing whether race would predict various S/R dimensions in this sample of urban adolescents with asthma, we opted to include both African-American (85%) and non-African-American (15%) participants and dichotomized our race variable as such. In addition, we used analysis of variance (ANOVA) to examine demographic or clinical differences between these two groups. Due to the non-parametric nature of the data, we calculated Spearman rho correlations to assess bivariate relationships between continuous study variables. Responses to the open-ended clinical encounter preferences questions (e.g., “Do you have any S/R beliefs that would influence any future health care decisions?”) were examined for content.
Ten separate multivariable linear regression models were constructed in order to predict each S/R score from a set of demographic and clinical predictors. Multivariable regressions were run first with all of the independent predictor variables, and then again after removing the independent variables that were non-significant (according to the multivariate test). McNemar's tests were used to examine whether preferred level of religious involvement differed by severity of clinical situation. Repeated measures logistic regressions were used to examine differences in responses to CEP items by age, race, or gender. Analyses were performed using SPSS, version 17 (SPSS for Windows 2008) and SAS, version 9.2 (SAS 9.2, 2008).
Results
Description of Sample
The mean (SD) age of the participants was 15.8 (1.8) years; 91 (60%) were female; and 129 (85%) were African-American (Table 1). There were no significant differences in clinical or demographic variables between African-American and non-African-American participants. Specifically, age, sex, insurance status, highest parental education level, asthma severity, and religious preference did not differ between racial groups (P > .05 for all comparisons).
Table 1. Demographic and clinical characteristics.
| Variables | |
|---|---|
| Mean (SD) age, years | 15.8 (1.8) |
| Sex | |
| Male, N (%) | 60 (40) |
| Female, N (%) | 91 (60) |
| Race/ethnicity | |
| White (not Hispanic), N (%) | 13 (9) |
| Black/African-American (not Hispanic), N (%) | 129 (85) |
| Asian or Pacific Islander, N (%) | 1 (1) |
| Native American or Alaskan Native, N (%) | 1 (1) |
| Biracial, N (%) | 4 (3) |
| Other, N (%) | 3 (2) |
| Health insurance* | |
| None, N (%) | 26 (17) |
| Public, N (%) | 101 (66) |
| Private, N (%) | 20 (13) |
| Highest level of participant education† | |
| Grade 6–8, N (%) | 27 (18) |
| Grade 9–12, N (%) | 102 (68) |
| In GED program, N (%) | 6 (4) |
| In college, N (%) | 2 (1) |
| Not currently in school | 12 (8) |
| Home schooled | 1 (1) |
| Highest level of parental education‡ | |
| Did not finish high school, N (%) | 21 (14) |
| Graduated from high school or passed GED exam, N (%) | 44 (29) |
| Received some college education, N (%) | 42 (28) |
| Graduated from college, N (%) | 31 (21) |
| Graduate with an advanced degree, N (%) | 3 (2) |
| Not sure, N (%) | 9 (6) |
| Medications | |
| Inhaled corticosteroids, N (%) | 81 (51) |
| Oral corticosteroids, N (%) | 4 (3) |
| Inhaled beta-agonists, N (%) | 139 (98) |
| Other, N (%) | 10 (7) |
| Asthma severity§ | |
| Intermittent, N (%) | 72 (48) |
| Mild persistent, N (%) | 38 (25) |
| Moderate persistent, N (%) | 36 (24) |
| Severe persistent, N (%) | 5 (3) |
N = 147;
N = 150;
The highest level of parental (mother or father) or caregiver education was used;
According to National Heart Lung and Blood Institute criteria
GED General Equivalency Diploma
One hundred and twenty-two participants (81%) reported being both religious and spiritual, 11 (7%) reported being religious but not spiritual, 6 (4%) reported being spiritual but not religious, and 11 (7%) reported being neither spiritual nor religious. One hundred and sixteen (77%) patients indicated a specific religious preference, most commonly Protestant or Catholic (Table 2). Fifty-seven participants (38%) reported attending religious services at least once a week, 31 (21%) at least once a month, and 63 (42%) reported never attending religious services in the past month. Seventy-four participants (49%) reported praying once a day and 55 (36%) reported praying once a month to once a day; 29 participants (19%) reported having meditated at least once in the last 30 days.
Table 2. Religious and spiritual characteristics.
| Measure | N (%) | ||
|---|---|---|---|
| Religious preference | |||
| Protestant | 97 (64) | ||
| Catholic | 16 (11) | ||
| Jewish | 1 (1) | ||
| No | 35 (23) | ||
| preference | |||
| Other | 2 (1) | ||
| Mean (SD) | Median | Possible range | |
| FACIT-Sp | 34.5 (9.2) | 35 | 0–48 |
| Meaning/peace | 24.0 (5.8) | 24 | 0–32 |
| Faith | 10.5 (4.5) | 11 | 0–16 |
| RCOPE | |||
| Positive religious coping | 11.0 (5.7) | 11 | 0–21 |
| Negative religious coping | 4.1 (4.4) | 3 | 0–21 |
| SWBS | 39.5 (9.9) | 43 | 10–50 |
| Existential well-being | 20.4 (5.0) | 22 | 5–25 |
| Religious well-being | 19.1 (6.2) | 21 | 5–25 |
| BMMRS | |||
| Daily spiritual experiences | 23.4 (6.1) | 24 | 6–30 |
| Spiritual meaning | 7.0 (2.2) | 7 | 2–10 |
FACIT-Sp Functional Assessment of Chronic Illness Therapy-Spirituality, SWBS Spiritual Well-Being Scale, BMMRS Brief Multidimensional Measure of Religiosity and Spirituality
Most participants indicated that spirituality was an important factor in their lives. For example, 114 participants (76%) reported feeling a sense of purpose in their life, and 138 participants (92%) found at least a little comfort in their faith or spiritual beliefs. In addition, 113 participants (75%) reported that their relationship with God/a Higher Power contributed to their well-being, and 125 participants (83%) had a sense of mission or calling in their life.
Sixty-seven participants (45%) indicated that their spiritual or religious beliefs helped them cope with asthma, with most reporting greater use of positive religious coping than negative religious coping. Specifically, positive religious coping strategies most often endorsed with “quite a bit” to “a great deal” of use included: “Asked forgiveness for my sins” (n = 98 [65%]) and “Tried to see how God/a Higher Power might be trying to strengthen me in this situation” (n = 74 [49%]). Negative religious coping strategies most often indicated included: “Questioned God's/a Higher Power's love for me” (n = 29 [19%]), “Decided the Devil made this [asthma] happen” (n = 28 [19%]), and “Wondered what I did for God/a Higher Power to punish me” (n = 27 [18%]).
Predictors of Dimensions of Spirituality and Religiosity
In multivariable models, being African-American and having a religious preference were the only variables associated with higher S/R scores on all S/R measures (R2 ranges 0.07–0.25; P < .05; Table 3), except negative religious coping, with which no variable was statistically significantly associated. Asthma severity, age, sex, insurance status, and parental education were not significant predictors of any of the dimensions of S/R (P > .05).
Table 3. Regression models predicting dimensions of spirituality and religiosity.
| African-American (β) | Having a religious preference (β) | F | R2 | |
|---|---|---|---|---|
| FACIT-Sp overall score | 8.74‡ | 4.37† | 13.60‡ | 0.14 |
| FACIT-Sp meaning/peace | 4.61‡ | 6.64† | 0.07 | |
| FACIT-Sp faith | 4.13‡ | 3.31‡ | 19.37‡ | 0.20 |
| RCOPE-positive | 5.28‡ | 4.73‡ | 22.52† | 0.22 |
| RCOPE-negative | 1.65 | 0.01 | ||
| SWBS | 9.21‡ | 5.80† | 15.47‡ | 0.16 |
| EWB | 4.37‡ | 7.84‡ | 0.08 | |
| RWB | 4.83‡ | 5.14‡ | 19.04† | 0.20 |
| BMMRS-daily spiritual experiences subscale | 4.63‡ | 6.07‡ | 25.24‡ | 0.25 |
| BMMRS-spiritual meaning subscale | 1.14* | 1.35† | 8.63‡ | 0.09 |
FACIT-Sp Functional Assessment of Chronic Illness Therapy-Spirituality, SWBS Spiritual Well-Being Scale, EWB Existential Well-Being Subscale of the Spiritual Well-Being Scale, RWB Religious Well-Being Subscale of the Spiritual Well-Being Scale, BMMRS Brief Multidimensional Measure of Religiosity and Spirituality
P < .05;
P < .01;
P < .001
Clinical Encounter Preferences
Sixty-three participants (42%) felt that their provider should play a role in the patient's spiritual or religious life, and 62 (41%) said that it was important for their provider to have strong spiritual beliefs of their own (Table 4). Although 78 participants (52%) felt that the provider should be aware of S/R beliefs, only 42 (28%) reported actually having told their provider about their S/R beliefs. Of the 78, 55 (71%) said that provider awareness about S/R was important in order for the provider to understand how the adolescent's beliefs influence how they deal with having asthma, and 53 (68%) said it was so that the provider could better understand how the adolescent makes decisions. Of note, 25 (17%) adolescents wanted their provider to discuss spiritual issues with them, even if it meant spending less time on their medical problems. Only 26 adolescents (17%) answered “yes” when asked if they had S/R beliefs that would influence future health care decisions; of those answering yes, write-in examples of such potential future health care decisions involved birth control, abortion, and coping with asthma.
Table 4. Clinical encounter preferences.
| Agree/strongly agree N (%) | Neutral N (%) | Disagree, strongly disagree N (%) | |
|---|---|---|---|
| My provider should not play a role in my spiritual or religious life | 41 (28) | 47 (31) | 63 (42) |
| It is important for me that my provider has strong spiritual beliefs | 62 (41) | 51 (34) | 38 (25) |
| My provider should be aware of my religious or spiritual beliefs | 78 (52) | 51 (34) | 22 (15) |
| If you do believe that your provider should be aware of your religious or spiritual beliefs, is it so that your provider*… | |||
| Could understand you better | 57 (73) | 14 (18) | 7 (9) |
| Could understand how your beliefs influence how you deal with asthma or other illness | 55 (71) | 15 (19) | 8 (10) |
| Would change how you are being treated for asthma or other illnesses | 29 (37) | 22 (28) | 27 (35) |
| Would understand how you make decisions | 53 (68) | 15 (19) | 10 (13) |
| Could be able to take care of you better when you are sick from asthma or other illnesses | 45 (58) | 21 (27) | 12 (15) |
| Can send you to a spiritual advisor if you think you need one | 36 (46) | 24 (31) | 18 (23) |
| Yes N (%) | |||
| Have you ever on your own told your provider about your spiritual or religious beliefs? | 42 (28) | ||
| Has your provider ever asked you about your spiritual or religious beliefs? | 46 (31) | ||
| I want my provider to discuss spiritual issues with me, even if it means spending less time on my medical problems | 25 (17) | ||
| Can you think of a situation where your spiritual or religious beliefs influenced how you dealt with a health care decision?† | 34 (23) | ||
| Do you have any spiritual or religious beliefs that would influence your future health care decisions?‡ | 26 (17) | ||
| Do your spiritual or religious beliefs help you cope with asthma and other illnesses?† | 67 (44) | ||
N= 78;
N = 149;
N = 150
As the severity of the hypothetical clinical situation increased (routine office visit versus hospitalization versus end of life), adolescents more often endorsed wanting their S/R issues addressed (P < .05; Fig. 1). For example, whereas 47 (31%) adolescents reported that their provider (physician or nurse practitioner) should ask about their religious beliefs during an office visit, the number increased to 63 (42%) if the adolescent were to be hospitalized and to 76 (51%) if he/she were dying. Similarly, 47 (32%) of adolescents said their provider should pray with them during an office visit, when compared with 70 (47%) if the patient were hospitalized, and 98 (65%) if the patient were dying. African-American adolescents were more likely than non-African-American adolescents to agree that their providers should say a silent prayer with them in the medical setting (P < .01). Answers to these aforementioned items did not differ by age or sex (P > .05).
Fig. 1.
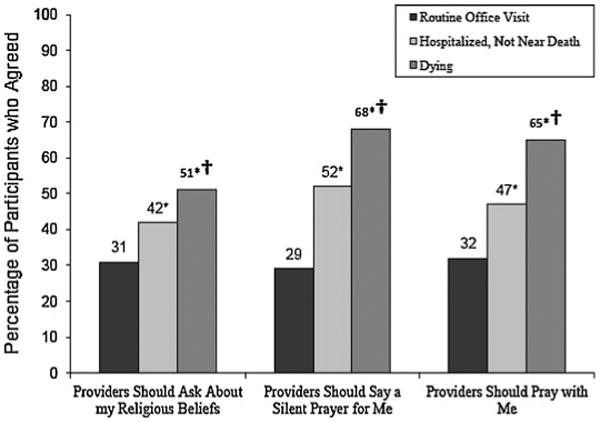
Clinical encounter preferences regarding the role of spiritual/religious practices during various types of clinical situations (N = 151. * Compared with routine office visit (P < .01); † Compared with hospitalized, not near death (P < .05)
Discussion
Issues surrounding S/R are relevant and important to many adolescents including, as our data suggest, urban predominantly African-American adolescents with asthma. Similar to non-chronically ill adolescents (Smith et al. 2005), most adolescents in our study believed in God/a Higher Power, and about half prayed daily. Most adolescents belonged to an organized religion, and approximately half attended religious services at least monthly. These data counter a previous scientific bias in which childhood and adolescence have been viewed as developmental periods in which S/R is not seen as particularly well developed or even important (Hood et al. 2009; Roehlkepartain et al. 2006). Although only a handful of studies exist (Benore et al. 2008; Oman and Thoresen 2006; Pendleton et al. 2002), our findings support the notion that S/R in children and adolescents with a chronic illness is salient, as with chronically ill adults (Cotton et al. 2006; Harvey and Silverman 2007; Koenig et al. 2001; Pargament et al. 2004).
With regard to religious coping, we found that levels of positive religious coping were similar to those found among chronically ill adults (Pargament et al. 2004), reflecting the importance of considering S/R when discussing coping with urban adolescents with asthma. In terms of negative religious coping, when compared with adults in hospice care (Hills et al. 2005) and adult patients with cancer (Balboni et al. 2010), the adolescents in this study utilized negative religious coping more frequently. This finding is concerning as the use of negative religious coping strategies (e.g., “God is punishing me”) in children hospitalized for asthma (ages 8–17, predominantly African-American) has been associated with poorer psychological adjustment during hospitalization and at 1 month follow-up (Benore et al. 2008). Given the rates of negative religious coping, discussions addressing both the potential positive and negative impacts of religious coping may be warranted when caring for urban adolescents with asthma.
Overall, African-American adolescents and those with a religious preference had higher scores on most S/R measures (e.g., used more positive religious coping), even when controlling for other variables such as insurance status, sex, and age. Our findings echo previous research indicating that African-Americans tend to be more religious and spiritual and rely more on faith to cope with adversity when compared with whites (Culver et al. 2002; Koenig et al. 2001; Taylor et al. 1996; Wallace and Williams 1997). Given that the role of S/R in the coping process or in developing meaning during stressful times may be particularly salient to African-American adolescents, providers should be aware of this phenomenon and consider addressing it in the clinical context.
Our study was the first study of its kind to ask urban adolescents about preferences for including S/R in hypothetical medical settings. Over a third of these adolescents wanted their S/R needs addressed in the context of a clinical encounter, and this percentage increased if they were to be hospitalized or dying. Interestingly, although 52% of patients felt that their provider should be aware of their S/R beliefs, only 28% of the total sample had actually told their provider about their S/R beliefs. Perhaps surprisingly, approximately 1 in 6 participants was willing to forgo time discussing medical issues to discuss S/R with his/her provider. The gap between adolescent patient preferences for addressing S/R in the health care setting and previous findings that few physicians actually discuss S/R with their patients is notable (Brooks and Chibnall 2000; Siegel et al. 2002). Whereas previous research has found that many physicians believe that S/R is important to their patients, they often do not have time to discuss such issues, do not feel it is under their professional purview, or do not feel adequately trained in this area (Armbruster et al. 2003; Grossoehme et al. 2007). Although about three-fourths of medical schools in the United States incorporate spirituality and health into their curricula to varying degrees (George Washington Institute for Spirituality and Health 2009) and although a variety of spiritual screening tools have been developed (Anandarajah and Hight 2001; Puchalski and Romer 2000), more work is needed to translate these findings into practical and effective ways to incorporate S/R into the clinical encounter when deemed relevant and appropriate (Fitchett and Risk 2009).
Findings from our study should be viewed in light of several limitations. Our sample of urban, primarily African-American adolescents came from a single Midwestern site and thus may not be generalizable. Further, as our study did not have a control group of healthy urban adolescents, or a control group of adolescents having another chronic disease, we were not able to assess for possible differences in S/R between chronically ill versus non-chronically ill adolescents, or differences between adolescents with asthma versus adolescents with a different chronic illness. In addition, as this sample represents patients from a primary care setting, they likely differ from those seen by a pulmonologist or allergist with regard to various clinical characteristics, especially disease severity. Finally, since the majority of the S/R measures were developed for use in adults, little work has been done on the formal psychometric properties of most S/R measures for use in adolescents (Cotton et al. 2010). Although internal consistency values for all S/R measures in this study exceeded 0.72, the measures as a group may not tap into some key developmental issues relevant to adolescents (e.g., influence of parental or peer religiosity [Cotton et al. 2010]).
Nevertheless, our study has several clinical and research implications. Much like for African-American adults with or without a chronic illness, S/R appears to be important to African-American adolescents (and other urban adolescents) with asthma and may play a role in their coping process. Healthcare providers should consider the role of S/R in the coping process and be open to potentially addressing S/R as it relates to adolescents' medical care and health outcomes. Future research is needed to empirically and practically test specific methods of integrating S/R into health care settings (e.g., incorporating S/R into coping discussions) and assess clinical feasibility of interventions, satisfaction with care, and clinical outcomes of such interventions. Future studies should also examine clinical preferences of addressing S/R in other racial/ethnic samples of chronically ill children and adolescents, as well as preferences of parents/guardians, to best inform clinical encounters.
Acknowledgments
We thank Elizabeth Hesse BS, Jennifer Munafo MA, and Dr. Maria Britto MD, MPH for their involvement on this project. This study was funded by a grant from the National Institute of Child Health and Human Development, #K23HD052639 (Cotton, PI) and a grant from the National Center for Complementary and Alternative Medicine, #K24AT001676 (Tsevat, PI).
Abbreviations
- S/R
Spirituality/religiosity
- FACIT-Sp
Functional Assessment of Chronic Illness Therapy-Spirituality
- SWBS
Spiritual Well-Being Scale
- EWB
Existential Well-Being
- RWB
Religious Well-Being
- BMMRS
Brief Multidimensional Measure of Religiosity and Spirituality
Contributor Information
Sian Cotton, Email: sian.cotton@uc.edu, Department of Family and Community Medicine, University of Cincinnati College of Medicine, P.O. Box 670840, Cincinnati, OH, USA; Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
Jerren C. Weekes, Department of Psychology, University of Cincinnati, Cincinnati, OH, USA
Meghan E. McGrady, Department of Psychology, University of Cincinnati, Cincinnati, OH, USA
Susan L. Rosenthal, Department of Pediatrics, Columbia University College of Physicians and Surgeons, New York, NY, USA
Michael S. Yi, Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA; Division of General Internal Medicine, Department of Internal Medicine, University of Cincinnati College of Medicine, Cincinnati, OH, USA
Kenneth Pargament, Department of Psychology, Bowling Green State University, Bowling Green, OH, USA.
Paul Succop, Division of Epidemiology and Biostatistics, Department of Environmental Health, University of Cincinnati College of Medicine, Cincinnati, OH, USA.
Yvonne Humenay Roberts, Department of Psychology, University of Cincinnati, Cincinnati, OH, USA.
Joel Tsevat, Division of General Internal Medicine, Department of Internal Medicine, University of Cincinnati College of Medicine, Cincinnati, OH, USA; Health Services Research and Development, Veterans Affairs Medical Center, Cincinnati, OH, USA.
References
- Akinbami LJ. The state of childhood asthma, United States, 1980-2005. Advance Data from Vital Health Statistics. 2006;381:1–24. [PubMed] [Google Scholar]
- Akinbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, health care utilization, and mortality. Pediatrics. 2002;110(2 Pt 1):315–322. doi: 10.1542/peds.110.2.315. [DOI] [PubMed] [Google Scholar]
- Anandarajah G, Hight E. Spirituality and medical practice: Using the HOPE questions as a practice tool for spiritual assessment. American Family Physician. 2001;63(1):81–90. [PubMed] [Google Scholar]
- Armbruster C, Chibnall J, Legett S. Pediatrician beliefs about spirituality and religion in medicine: Associations with clinical practice. Pediatrics. 2003;111(3):e227–e235. doi: 10.1542/peds.111.3.e227. [DOI] [PubMed] [Google Scholar]
- Balboni TA, Paulk ME, Balboni MJ, Phelps AC, Loggers ET, Wright AA, et al. Provision of spiritual care to patients with advanced cancer: Associations with medical care and quality of life near death. Journal of Clinical Oncology. 2010;28(3):445–452. doi: 10.1200/JCO.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennet D. Depression among children with chronic medical problems: A meta-analysis. Journal of Pediatric Psychology. 1994;19(2):149–169. doi: 10.1093/jpepsy/19.2.149. [DOI] [PubMed] [Google Scholar]
- Benore E, Pargament KI, Pendleton S. An initial examination of religious coping in children with asthma. International Journal for the Psychology of Religion. 2008;18:267–290. [Google Scholar]
- Benson P, Roehlkepartain E, Rude S. Spiritual development in childhood and adolescence: Toward a field of inquiry. Applied Developmental Science. 2003;7(3):205–213. [Google Scholar]
- Bridges L, Moore K. Religion and spirituality in childhood and adolescence. 2002 From http://www.childtrends.org/Files/Child_Trends-2002_01_01_FR_ReligionSpiritAdol.pdf. Retrieved 15 Jan 2010.
- Brooks C, Chibnall J. Religion in medicine among Salt Lake City pediatricians. Utah Medical Association Bulletin. 2000;47:10–11. [Google Scholar]
- Buck A, Williams D, Musick M, Sternthal M. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Social Science and Medicine. 2009;68(2):314–322. doi: 10.1016/j.socscimed.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Larkin E, Hoopes A, Cromer B, Rosenthal S. The impact of adolescent spirituality on depressive symptoms and health risk behaviors. Journal of Adolescent Health. 2005;36(6):529. doi: 10.1016/j.jadohealth.2004.07.017. [DOI] [PubMed] [Google Scholar]
- Cotton S, Puchalksi C, Sherman SN, Mrus JM, Peterman AH, Feinberg J, et al. Spirituality and religion in patients with HIV/AIDS. Journal of General Internal Medicine. 2006a;21(Suppl 5):S5–13. doi: 10.1111/j.1525-1497.2006.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Zebracki K, Rosenthal S, Tsevat J, Drotar D. Religion/spirituality and adolescent health outcomes: A review. Journal of Adolescent Health. 2006b;38(4):472–480. doi: 10.1016/j.jadohealth.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Cotton S, Grossoehme D, Rosenthal SL, McGrady ME, Roberts Y, Hines J, et al. Religious/spiritual coping in adolescents with sickle cell disease: A pilot study. Journal of Pediatric Hematology Oncology Nursing. 2009a;31(5):313–318. doi: 10.1097/MPH.0b013e31819e40e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Kudel I, Roberts YH, Pallerla H, Tsevat J, Succop P, et al. Spiritual well-being and mental health outcomes in adolescents with or without inflammatory bowel disease. Journal of Adolescent Health. 2009b;44(5):485–492. doi: 10.1016/j.jadohealth.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, McGrady ME, Rosenthal SL. Measurement of religiosity/spirituality in adolescent health outcomes research: Trends and recommendations. Journal of Religion and Health. 2010 doi: 10.1007/s10943-010-9324-0. published online ahead of print February 2 2010. From http://www.springerlink.com/content/a7108178354k8463/fulltext.pdf. Retrieved 14 April 2010. [DOI] [PMC free article] [PubMed]
- Culver J, Arena P, Antoni M, Carver C. Coping and distress among women under treatment for early stage breast cancer: Comparing African Americans, hispanics, and non-Hispanic whites. Psycho-Oncology. 2002;11:495–504. doi: 10.1002/pon.615. [DOI] [PubMed] [Google Scholar]
- Ehman J, Ott B, Short T, Ciampa R, Hansen-Flaschen J. Do patients want their physicians to inquire about their spiritual or religious beliefs if they are gravely ill? Archives of Internal Medicine. 1999;159:1803–1806. doi: 10.1001/archinte.159.15.1803. [DOI] [PubMed] [Google Scholar]
- Fetzer Institute/National Institute on Aging Working Group . Multidimensional measurement of religiousness, spirituality for use in health research: A report of the Fetzer Institute/National Institute on aging working group. 2nd. Kalamazoo, MI: Fetzer Institute; 1999. [Google Scholar]
- Fitchett G, Risk J. Screening for spiritual struggles. Journal of Pastoral Care & Counseling. 2009;63(1,2):1–12. [PubMed] [Google Scholar]
- Forrest CB, Starfield B, Riley AW, Kang M. The impact of asthma on the health status of adolescents. Pediatrics. 1997;99(2):E1. doi: 10.1542/peds.99.2.e1. [DOI] [PubMed] [Google Scholar]
- George Washington Institute for Spirituality and Health 2009 From http://www.gwish.org/. Retrieved 19 Dec 2009.
- Grossoehme D, Ragsdale J, McHenry C, Thurston C, DeWitt T, Vande Creek L. Pediatrician characteristics associated with attention to spirituality and religion in clinical practice. Pediatrics. 2007;119(1):e117–e123. doi: 10.1542/peds.2006-0642. [DOI] [PubMed] [Google Scholar]
- Guill MF. Asthma update: Epidemiology and pathophysiology. Pediatrics in Review. 2004;25(9):299–305. doi: 10.1542/pir.25-9-299. [DOI] [PubMed] [Google Scholar]
- Harris SK, Sherritt LR, Holder DW, Kulig J, Shrier LA, Knight JR. Reliability and validity of the brief multidimensional measure of religiousness/spirituality among adolescents. Journal of Religion and Health. 2008;47(4):438–457. doi: 10.1007/s10943-007-9154-x. [DOI] [PubMed] [Google Scholar]
- Harvey I, Silverman M. The role of spirituality in the self-management of chronic illness among older African and Whites. Journal of Cross Cultural Gerontology. 2007;22(2):205–220. doi: 10.1007/s10823-007-9038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC, Pargament KI, Hood RW, Jr, McCullough ME, Swyers JP, Larson DB, et al. Conceptualizing religion and spirituality: Points of commonality, points of departure. Journal for the Theory of Social Behaviour. 2002;30(1):51–77. [Google Scholar]
- Hills J, Paice J, Cameron J, Shott S. Spirituality and distress in palliative care counseling. Journal of Palliative Medicine. 2005;8(4):782–788. doi: 10.1089/jpm.2005.8.782. [DOI] [PubMed] [Google Scholar]
- Hood R, Jr, Hill P, Spilka B. The psychology of religion: An empirical approach. 4th. New York, NY: The Guilford Press; 2009. [Google Scholar]
- King D, Bushwick B. Beliefs and attitudes of hospital inpatients about faith healing and prayer. The Journal of Family Practice. 1994;39:349–352. [PubMed] [Google Scholar]
- Koenig H, McCullough M, Larson D, editors. Handbook of religion and health. New York, NY: Oxford University Press; 2001. [Google Scholar]
- Lauckhaupt S, Yi M, Mueller C, Mrus JM, Peterman AH, Puchalksi C, et al. Beliefs of primary care residents regarding spirituality and religion in clinical encounters with patients: A study at a midwestern U.S. teaching institution. Academic Medicine. 2005;80(6):560–570. doi: 10.1097/00001888-200506000-00011. [DOI] [PubMed] [Google Scholar]
- MacLean C, Susi B, Phifer N, Schultz MD, Bynum D, Franco M, et al. Patient preference for physician discussion and practice of spirituality. Journal of General Internal Medicine. 2003;18(1):38–43. doi: 10.1046/j.1525-1497.2003.20403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattis JS. Religion and spirituality in the meaning-making and coping experiences of African American women: A qualitative analysis. Psychology of Women Quarterly. 2002;26(4):309–321. [Google Scholar]
- McCord G, Gilchrist V, SD G, King D, McCormick KF, Oprandi AM, et al. Discussing spirituality with patients: A rational and ethical approach. Annals of Family Medicine. 2004;2(4):356–361. doi: 10.1370/afm.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQuaid EL, Walders N. Pediatric asthma. In: Roberts M, editor. Handbook of pediatric psychology. 3rd. New York, NY: The Guilford Press; 2003. pp. 269–285. [Google Scholar]
- McQuaid EL, Kopel SJ, Nassau JH. Behavioral adjustment in children with asthma: A meta-analysis. Journal of Developmental and Behavioral Pediatrics. 2001;22(6):430–439. doi: 10.1097/00004703-200112000-00011. [DOI] [PubMed] [Google Scholar]
- Merikallio VJ, Mustalahti K, Remes ST, Valovirta EJ, Kaila M. Comparison of quality of life between asthmatic and healthy school children. Pediatric Allergy & Immunology. 2005;16(4):332–340. doi: 10.1111/j.1399-3038.2005.00286.x. [DOI] [PubMed] [Google Scholar]
- National Heart Lung and Blood Institute Guidelines for the diagnosis and management of asthma. 2007 From http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. Retrieved 15 July 2010. [PubMed]
- Nicholson A, Rose R, Bobak M. Associations between different dimensions of religious involvement and self rated health in diverse European populations. Health Psychology. 2010;29(2):227–235. doi: 10.1037/a0018036. [DOI] [PubMed] [Google Scholar]
- Oman D, Thoresen C. Religion, spirituality, and children's physical health. In: Roehlke-partain E, Ebstyne-King P, Wagener L, Benson P, editors. The handbook of spiritual development in childhood and adolescence. Thousand Oaks, CA: Sage Pubs Inc.; 2006. p. 399. [Google Scholar]
- Paloutzian R, Ellison C. Manual for spiritual well-being scale. Nyack, NY: Life Advance, Inc.; 1991. [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious coping methods as predictors of psychological, physical and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. Journal of Health Psychology. 2004;9(6):713–730. doi: 10.1177/1359105304045366. [DOI] [PubMed] [Google Scholar]
- Pendleton SM, Cavalli KS, Pargament KI, Nasr SZ. Religious/spiritual coping in childhood cystic fibrosis: A qualitative study. Pediatrics. 2002;109(1):e8. doi: 10.1542/peds.109.1.e8. [DOI] [PubMed] [Google Scholar]
- Peterman A, Fitchett G, Brady M, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy-spiritual well-being scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- Potts RG. Spirituality and the experience of cancer in an African American community. Journal of Psychosocial Oncology. 1996;14(1):1–19. [Google Scholar]
- Puchalski C, Romer A. Taking a spiritual history allows clinicians to understand patients more fully. Journal of Palliative Medicine. 2000;3(1):129–137. doi: 10.1089/jpm.2000.3.129. [DOI] [PubMed] [Google Scholar]
- Roehlkepartain E, Benson P, King D, Wagener L. Spiritual development in childhood and adolescents: Moving to the scientific mainstream. In: Roehlkepartain E, King D, Wagener L, Benson P, editors. The handbook of spiritual development in childhood and adolescence. Thousand Oaks, CA: Sage Pubs Inc.; 2006. pp. 1–15. [Google Scholar]
- Rubin D, Dodd M, Desai N, Pollock B, Graham-Pole J. Spirituality in well and ill adolescents and their parents: The use of two assessment scales. Pediatric Nursing. 2009;35(1):37–42. [PubMed] [Google Scholar]
- SAS 9.2. Cary, NC: SAS Institute; 2008. [Google Scholar]
- Siegel B, Tenenbaum A, Jamanka A, Barnes L, Hubbard C, Zuckerman B. Faculty and resident attitudes about spirituality and religion in the provision of pediatric health care. Ambulatory Pediatrics. 2002;2:5–10. doi: 10.1367/1539-4409(2002)002<0005:faraas>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Smith C, Lundquist-Denton M. Soul Searching: The religious and spiritual lives of American teenagers. Oxford; Oxford University Press; 2005. [Google Scholar]
- SPSS for Windows, Rel 09. Chicago: SPSS Inc.; 2008. [Google Scholar]
- Taylor R, Chatters L, Jayakody R, Levin J. Black and white differences in religious participation: A multi sample comparison. Journal for the Scientific Study of Religion. 1996;35(4):403–415. [Google Scholar]
- The Institute for Social Research University of Michigan Monitoring the future. 2010 From http://monitoringthefuture.org/. Retrieved 9 July 2010.
- The Stronger Sex—Spiritually Speaking 2009 From http://pewforum.org/The-Stronger-Sex—Spiritually-Speaking.aspx. Retrieved 16 July 2010.
- United States Environmental Protection Agency Asthma facts. 2010 From http://www.epa.gov/asthma/pdfs/asthma_fact_sheet_en.pdf. Retrieved 23 July 2010.
- Wallace J, Jr, Williams D. Religion and adolescent health-compromising behavior. In: Schulenberg J, Maggs J, Hurrelmann K, editors. Health risks and developmental transitions during adolescence. New York, NY: Cambridge University Press; 1997. [Google Scholar]


